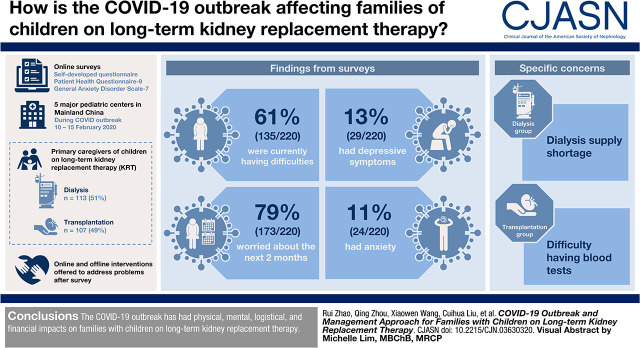
Visual Abstract
Keywords: Renal replacement therapy, COVID-19, SARS-CoV-2, End-stage kidney disease, Caregivers, Families, Mainland China, Children
Abstract
Background and objectives
During the coronavirus disease 2019 outbreak, the treatment of families with children on long-term KRT is challenging. This study was conducted to identify the current difficulties, worries regarding the next 2 months, and mental distress experienced by families with children on long-term KRT during the coronavirus disease 2019 outbreak and to deliver possible management approaches to ensure uninterrupted treatment for children on long-term KRT.
Design, setting, participants, & measurements
A multicenter online survey was conducted between February 10 and 15, 2020, among the families with children on long-term KRT from five major pediatric dialysis centers in mainland China. The primary caregivers of children currently on long-term KRT were eligible and included. Demographic information, severe acute respiratory syndrome coronavirus 2 infection status, current difficulties, and worries regarding the next 2 months were surveyed using a self-developed questionnaire. The Patient Health Questionnaire-9 and the General Anxiety Disorder Scale-7 were used to screen for depressive symptoms and anxiety, respectively.
Results
Among the children in the 220 families included in data analysis, 113 (51%) children were on dialysis, and the other 107 (49%) had kidney transplants. No families reported confirmed or suspected cases of coronavirus disease 2019. Overall, 135 (61%) and 173 (79%) caregivers reported having difficulties now and having worries regarding the next 2 months, respectively. Dialysis supply shortage (dialysis group) and hard to have blood tests (kidney transplantation group) were most commonly reported. A total of 29 (13%) caregivers had depressive symptoms, and 24 (11%) had anxiety. After the survey, we offered online and offline interventions to address their problems. At the time of the submission of this paper, no treatment interruption had been reported.
Conclusions
The coronavirus disease 2019 outbreak has had physical, mental, logistical, and financial effects on families with children on long-term KRT.
Introduction
Coronavirus disease 2019 (COVID-19) has now spread to six continents. Epidemiologic investigations have indicated that all age groups are susceptible to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (1). As the epidemic has evolved, COVID-19 has become a public health emergency of international concern (2). By June 20, 2020, the number of confirmed cases has exceeded 8 million worldwide, with >456,000 deaths (3). To contain the epidemic, in China, strong measures were put in place. On January 23, 2020, Wuhan declared a transportation shutdown. By January 25, 2020, 30 provinces in China had activated the highest level of response to this major public health emergency and had adopted pragmatic tailored measures to address the spread of SARS-CoV-2.
During the COVID-19 epidemic, people with chronic diseases still have continuous medical needs, including patients on long-term KRT. However, during the epidemic, traffic restrictions, the repurposing of medical services, and concerns regarding the risk of SARS-CoV-2 infection may threaten the continuity of life-saving dialysis, immunosuppressant treatment, and regular hospital visits among children with kidney failure.
To the best of our knowledge, no study has focused on the influence of the epidemic on children with kidney failure receiving peritoneal dialysis (PD) or hemodialysis or children with kidney transplants. We conducted this multicenter study to identify the current difficulties, worries regarding the next 2 months, and mental distress experienced by families with children on long-term KRT during the COVID-19 outbreak and to deliver possible management approaches to ensure uninterrupted and proper treatment for children with kidney failure.
Materials and Methods
Study Design and Setting
A multicenter online survey was conducted among families with children on long-term KRT between February 10 and February 15, 2020. It was approved by the Ethics Board of the Children’s Hospital of Fudan University; the ethics number is [2020]-28. Five centers with the largest numbers of current maintenance dialysis cases registered with the International Pediatric Dialysis Network China were selected, including one center in Wuhan. These five centers were Children’s Hospital of Fudan University, Shanghai (Shanghai center); Wuhan Children’s Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei Province (Wuhan center); Affiliated Children’s Hospital of Zhengzhou University, Zhengzhou, Henan Province (Zhengzhou center); Children’s Hospital of Chongqing Medical University, Chongqing (Chongqing center); and The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, Zhejiang Province (Wenzhou center). To recruit more potential respondents, we also used snowball sampling where the caregivers participating in the study also helped distribute the questionnaires to other potential respondents. Informed consent was obtained at the start of the questionnaires, and the respondents could choose to proceed to answer the questions or to leave the page. After summarizing the questionnaire data, an instant action protocol was developed, and immediate interventions were delivered by health care staff at the Shanghai center to the families in need from each center.
Variables and Assessment
Demographic information, SARS-CoV-2 infection status, difficulties, and worries were surveyed using a self-developed questionnaire. The questionnaire was on the basis of interviews with 18 caregivers of children on dialysis or with kidney transplant. These 18 caregivers were selected purposively, with consideration given to ethnicity, treatment modalities, and areas of residence. They were asked about the current difficulties and worries regarding the next 2 months they experienced regarding their children’s current treatment during the COVID-19 outbreak. From the 18 interviews, we identified the current difficulties and future worries that would be surveyed in the questionnaire. The questionnaire included the demographic information of the family, SARS-CoV-2 infection status, treatment modalities, current medical supplies and medication storage, perceived influence of the outbreak on the child’s treatment, the three most common current difficulties in the child’s treatment, and the three most common worries caregivers had regarding the next 2 months. After the respondents submitted their answers, a link and quick response code were provided that gave them access to education about COVID-19 preventative measures. Before extensively distributing the questionnaires, seven caregivers of children on long-term KRT were invited to complete the questionnaires. To identify misunderstandings and to enable the manner of expression of each item to be adjusted for clarity, these seven caregivers were asked to think aloud in response to each question. These seven questionnaires were also included in the final analysis. The questionnaire was translated into English; the details are in Supplemental Material.
The Patient Health Questionnaire-9 (PHQ-9) was a nine-item questionnaire used to screen for depressive symptoms. It scores each of the nine diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, for depression from zero (not at all) to three (nearly every day) over the previous 2 weeks (4). The Chinese version of the PHQ-9 had Cronbach α values of 0.82–0.86 (5,6). In our study, the standard cutoff score of ten and above was used to indicate the occurrence of depressive symptoms (7).
The General Anxiety Disorder Scale-7 (GAD-7) was a seven-item questionnaire widely used to screen for general anxiety disorder. It scores the frequency of anxiety-related symptoms in the past 2 weeks from zero (not at all) to three (nearly every day). The Chinese version of the GAD-7 had a Cronbach α of 0.89. With a cutoff score of ten, it had a sensitivity of 86.2% and a specificity of 95.5% (8).
Patient Selection and Data Collections
Eligibility criteria included families of children with kidney failure currently on long-term KRT. A primary caregiver of children on KRT in each family was eligible and asked to report on each item. Exclusions included families with children aged 19 years and older and families who were not willing or able to participate in the online survey. A researcher from the Shanghai center was responsible for checking the informed consent and the child’s age and removing duplication before recruiting the respondents. An online questionnaire was used to gather the data. This questionnaire was available for distribution via a website link (https://www.wjx.cn/jq/56594212.aspx) and quick response code. In the five aforementioned pediatric centers, the questionnaires were first distributed to each center’s WeChat groups of patients on dialysis and patients with transplants by health care staff. WeChat, with its multipurpose platform, has >1 billion monthly active users and is one of the most important applications in China (9). To reduce the nonresponse rate, from February 10 to 15, health care workers in each center shared links to all members in WeChat groups twice a day. They also texted nonrespondents on February 14 to get more responses. Additionally, to improve the completeness of the questionnaire, each item in the online questionnaire was set to be filled before successfully submitted. No missing data were expected.
Statistical Analyses
All data from the completed electronic questionnaires were first imported into Microsoft Excel for Macintosh, version 15.13.3 (Microsoft Corporation, Washington, WA), and checked for logic errors. Then, we performed all of the statistical tests with SPSS21.0 for Macintosh (IBM SPSS, Chicago, IL). The mean ± SD or median (25th percentile, 75th percentile) was used to describe the quantitative variables, such as age and duration of treatment, depending on the normality of the distribution of the data. Frequency and percentage were used to describe categorical variables, such as sex and treatment modality. Variables in the categories of current difficulties and future worries were sorted to identify the most commonly reported difficulties and worries among different treatment modality groups. For depressive symptoms and anxiety, the Fisher exact test, the chi-squared test, and logistic regression were used to explore factors related to the prevalence of depressive symptoms or anxiety. The binary logistic regression model was also used to adjust the covariates, including caregiver’s sex, caregiver’s age, child’s age, duration on treatment, and medical payment, and to determine the associations of treatment modalities with the prevalence of depressive symptoms and anxiety among the respondents. These associations were further analyzed in participants only from the Shanghai center for sensitivity analyses. Two-sided P values <0.05 were considered statistically significant.
Results
Participant Characteristics
In all, 240 questionnaires were collected from February 10 to 15, 2020. After checking for eligibility, a total of 220 completed questionnaires were finally included in the data analysis, with 211 from five centers and the other 9 from other centers (Figure 1). The number of respondents (overall participation rate) of five centers was 211 (81%), with 110 (73%) in the dialysis group and 101 (92%) in the transplantation group (Table 1). The transplantation respondents were mostly from the Shanghai center because the other four centers do not routinely follow up with children after kidney transplantation.
Figure 1.
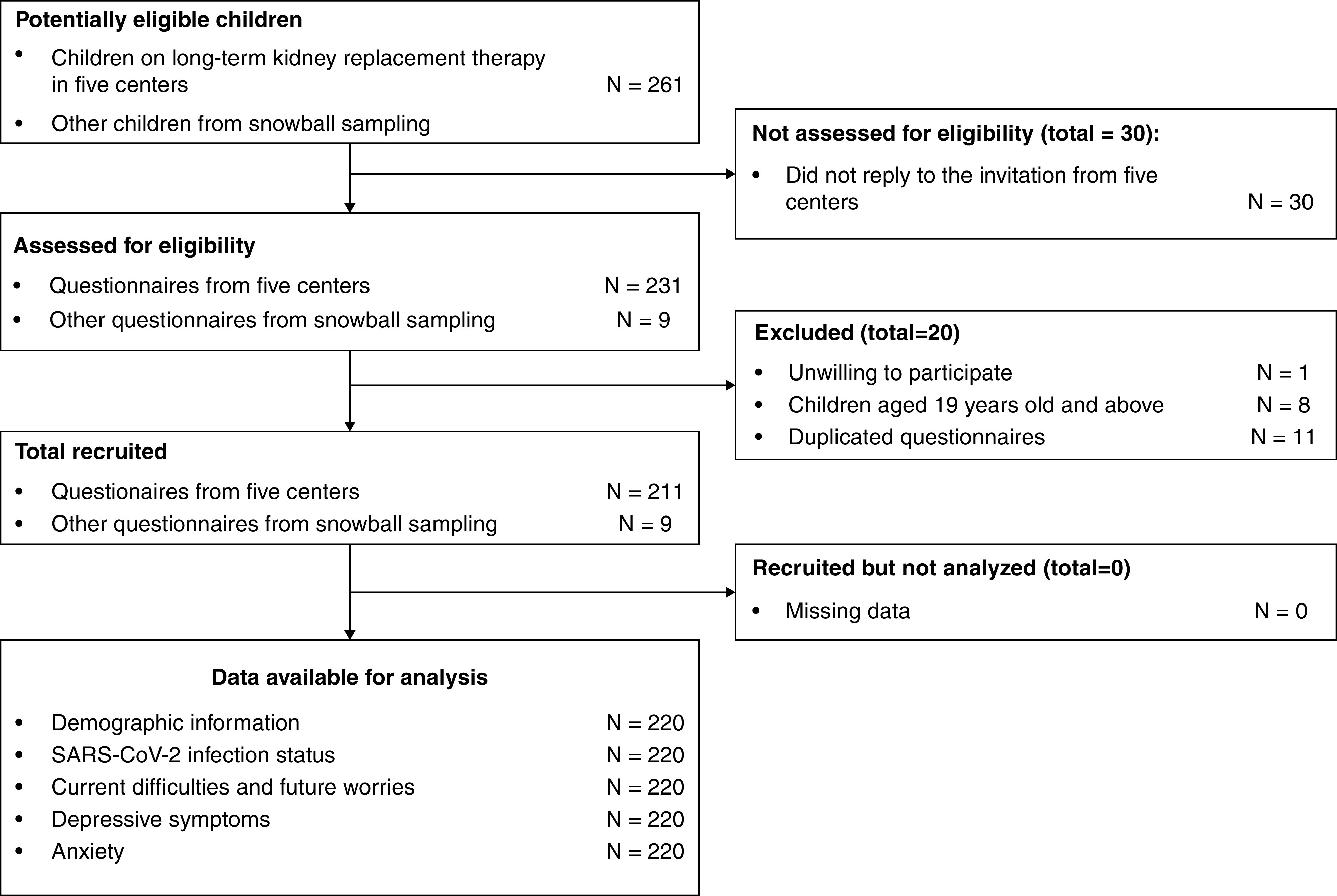
Two hundred twenty eligible caregivers were recruited and available for analysis between February 10 and 15, 2020. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Table 1.
The number of respondents and participation rates overall and by treatment modalities
| Centers | Children Currently on Kidney Replacement Therapy in Each Center, No. | Retrieved Questionnaires and Participation Rate,a No. (%) | |||
|---|---|---|---|---|---|
| Dialysis | Transplantation | Dialysis | Transplantation | Overall | |
| Shanghai | 84 | 110 | 74 (88) | 101 (92) | 175 (90) |
| Wuhan | 11 | 0 | 10 (91) | 0 (0) | 10 (91) |
| Zhengzhou | 17 | 0 | 11 (65) | 0 (0) | 11 (65) |
| Chongqing | 30 | 0 | 10 (33) | 0 (0) | 10 (33) |
| Wenzhou | 9 | 0 | 5 (56) | 0 (0) | 5 (56) |
| Subtotalc | 151 | 110 | 110 (73) | 101 (92) | 211 (81) |
| Othersb | 3 | 6 | 9 | ||
| Totald | 151 | 110 | 113 | 107 | 220 |
Participation rate = (the number of respondents who returned the questionnaires divided by the number of children in the center [percentage]).
These nine questionnaires were from other centers through snowball sampling. The numbers of children on long-term KRT from these centers were unknown.
Number of respondents and participation rates in five centers.
Number of respondents from five centers and through snowball sampling.
The characteristics of the families included are presented in Table 2. Child’s mean age was 11±4 years old. The caregiver's mean age was 40±10 years old. A total of 113 children were on dialysis, including 96 (44%) on automated peritoneal dialysis (APD), 11 (5%) on continuous APD, and 6 (3%) on hemodialysis, and the other 107 children (49%) had kidney transplants. Parents were the child’s primary caregiver in most cases. Among 220 respondents, none of the children or their caregivers had confirmed or suspected cases of COVID-19, nor were they under medical observation for COVID-19.
Table 2.
Characteristics of children on long-term kidney replacement therapy and their caregivers overall and by treatment modalities
| Characteristics | Overall, n=220 | Dialysis, n=113 | Transplantation, n=107 |
|---|---|---|---|
| Child’s age, yra | 11±4 | 10±4 | 12±4 |
| Child’s sex | |||
| Boy | 120 (55) | 62 (55) | 58 (54) |
| Girl | 100 (45) | 51 (45) | 49 (46) |
| Child’s ethnicity | |||
| Han | 210 (94) | 108 (96) | 102 (95) |
| Minority groups | 10 (6) | 5 (4) | 5 (5) |
| Duration on treatment, mob | 19 (8, 34) | 14 (6, 26) | 29 (11, 42) |
| Caregivers | |||
| Parents | 192 (87) | 99 (88) | 93 (87) |
| Grandparents | 12 (6) | 6 (5) | 6 (6) |
| Children by themselves | 13 (6) | 7 (6) | 6 (6) |
| Others | 3 (1) | 1 (1) | 2 (2) |
| Caregiver’s sex | |||
| Man | 37 (17) | 19 (17) | 18 (17) |
| Woman | 183 (83) | 94 (83) | 89 (83) |
| Caregiver’s age, yra | 40±10 | 39±9 | 42±11 |
| Caregiver’s educational background | |||
| Illiterate, primary school, or middle school | 119 (54) | 64 (57) | 55 (52) |
| High school or equivalent | 81 (37) | 38 (34) | 43 (40) |
| Bachelor’s degree and above | 20 (9) | 11 (10) | 9 (8) |
| Caregiver’s working status during the outbreak | |||
| Full-time care | 194 (88) | 103 (91) | 91 (85) |
| Working at home | 21 (10) | 8 (7) | 13 (12) |
| Working at office (need to travel) | 5 (2) | 2 (2) | 3 (3) |
| Medical payment | |||
| Insurance | 191 (87) | 101 (89) | 90 (84) |
| Out of pocket | 29 (13) | 12 (11) | 17 (16) |
The cell contents are N (%) except when noted otherwise.
Mean ± SD.
Median (25th percentile, 75th percentile).
Current Difficulties and Worries Regarding the Next 2 Months
A total of 171 (78%) of the respondents reported that the COVID-19 outbreak had influenced the child’s treatment, with 80 (71%) in the dialysis group and 91 (85%) in the transplantation group, and 64 (29%) of the respondents thought the influence was severe or extremely severe, with 23 (20%) in the dialysis group and 41 (38%) in the transplantation group.
Overall, 135 (61%) and 173 (79%) respondents reported having medical, logistical, and financial current difficulties and future worries regarding the next 2 months, respectively (Table 3). The top three most commonly reported current difficulties and future worries by treatment modalities are described in Figure 2. Dialysis supply shortage in the dialysis group and hard to have blood tests in the kidney transplantation group were most commonly reported both for current difficulties and worries regarding the next 2 months. The two groups had similar worries about contracting COVID-19 during the hospital visits.
Table 3.
Caregivers’ current difficulties and worries regarding the next 2 months overall and by treatment modalities
| Items | No. (%) | ||
|---|---|---|---|
| Overall, n=220 | Dialysis, n=113 | Transplantation, n=107 | |
| Current difficulties | |||
| Hard to have blood tests | 66 (30) | 20 (18) | 46 (43) |
| Face mask shortage | 56 (25) | 22 (19) | 34 (32) |
| Hard to access specialized clinics | 46 (21) | 15 (13) | 31 (29) |
| PD supply shortage | 38 (17) | 38 (34) | 0 (0) |
| Traveling restrictions | 33 (15) | 13 (12) | 20 (19) |
| Lack financial support for treatment | 28 (13) | 14 (12) | 14 (13) |
| Hand hygiene supply shortage | 27 (12) | 11 (10) | 16 (15) |
| Hard to get erythropoietin injected | 22 (10) | 22 (19) | 0 (0) |
| Exit-site care supply shortage | 17 (8) | 17 (15) | 0 (0) |
| Feel fearful or worried | 16 (7) | 6 (5) | 10 (9) |
| Dialysis/transplantation-related medication shortage | 13 (6) | 7 (6) | 6 (6) |
| Delivery service suspended | 12 (5) | 8 (7) | 4 (4) |
| Worries regarding the next 2 mo | |||
| Hard to have blood tests | 69 (31) | 16 (14) | 53 (50) |
| Hard to access specialized clinics | 66 (30) | 29 (26) | 37 (35) |
| PD supply shortage | 64 (29) | 64 (57) | 0 (0) |
| Risk of acquiring COVID-19 during hospital visits | 61 (28) | 33 (29) | 28 (26) |
| Risk of acquiring COVID-19 | 58 (27) | 31 (27) | 27 (25) |
| Face mask shortage | 49 (22) | 23 (20) | 26 (24) |
| Traveling restrictions | 39 (18) | 14 (12) | 25 (23) |
| Lack financial support for treatment | 30 (14) | 12 (11) | 18 (17) |
| Dialysis/transplantation-related medication shortage | 22 (10) | 15 (13) | 7 (7) |
| Hard to get erythropoietin injected | 14 (6) | 14 (12) | 0 (0) |
| Delivery service suspended | 11 (5) | 5 (4) | 6 (6) |
PD, peritoneal dialysis; COVID-19, coronavirus disease 2019.
Figure 2.
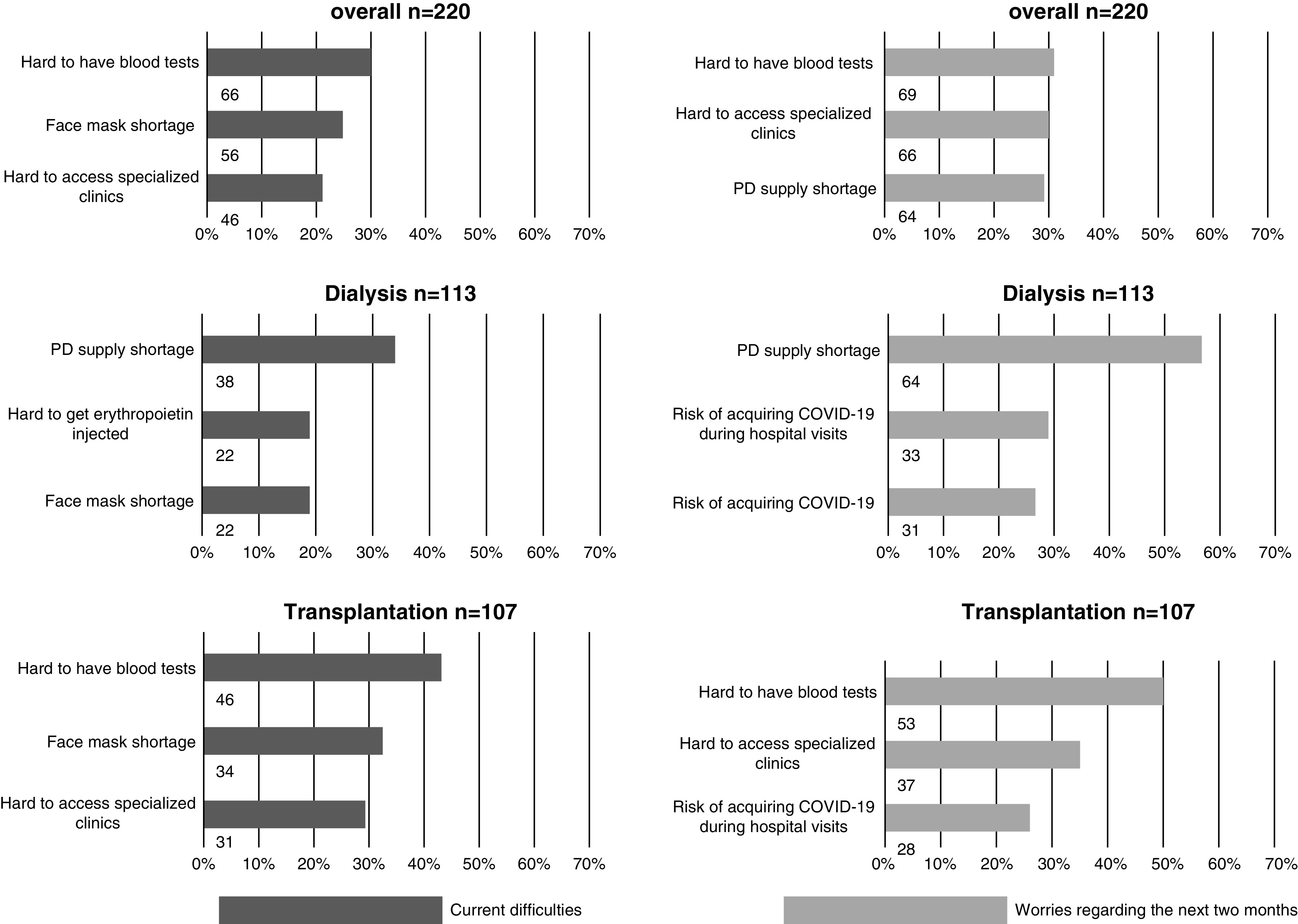
The top three difficulties and worries of caregivers with children on KRT varied across treatment modalities. COVID-19, coronavirus disease 2019; PD, peritoneal dialysis.
In all, 29 (13%) respondents had depressive symptoms, with 20 (18%) in the dialysis group and 9 (8%) in the transplantation group; 24 (11%) respondents had anxiety, with 17 (15%) in the dialysis group and 7 (7%) in the transplantation group. Unadjusted analyses of factors related to the prevalence of depressive symptoms and anxiety are presented in Supplemental Table 1. Treatment modalities were associated with the prevalence of depressive symptoms (odds ratio, 0.43; 95% confidence interval, 0.19 to 0.99; P=0.04) and the prevalence of anxiety (odds ratio, 0.40; 95% confidence interval, 0.16 to 0.99; P=0.04). However, after the adjustment for child’s age, duration on treatment, caregiver’s age, caregiver’s sex, and medical payment, these associations were not significant. Additionally, the results were consistent in the sensitivity analysis in the Shanghai center (Supplemental Table 2).
Management Approaches for Families
In all, 14 (6%) of the families ran out of medication within 2 weeks, including hypertension medication, immunosuppressants, or both. Also, seven families almost ran out of PD supplies, including PD fluids, PD cassettes, or both. Of 14 families who almost ran out of medications, we successfully offered solutions to 13 families, including mailing medication directly from the hospitals, using online pharmacy services, and having the families go to nearby hospitals to obtain prescriptions. We could not make contact with one family from the Shanghai center because they did not answer our phone calls. Of the seven families who almost ran out of PD medical supplies, six families were able to continue their current dialysis modalities by contacting nearby hospitals or contacting PD supply companies. The other child on APD living in Hubei province switched from APD to continuous APD due to the suspension of delivery services and, thus, the inaccessibility of PD cassettes.
On the basis of the data collected, a protocol for caring for children on home PD during the COVID-19 outbreak was developed (10). From February 10 to 24, 2020, in the WeChat groups of patients on dialysis, 77 online consultation questions were answered regarding the child’s general condition changes (n=22), cycler alerts (n=16), medication adjustments (n=13), ultrafiltration changes (n=11), PD supplies (n=10), and potential PD-related infections (n=5).
Considering the caregivers’ willingness to engage in psychologic consultation over the telephone, psychological support was offered to 11 caregivers with depressive symptoms or anxiety. Additionally, health education regarding COVID-19 protective measurements and solutions for refilling medication and medical supplies were shared in patients’ WeChat groups. At the time of the submission of this paper, no treatment interruption had been reported.
Discussion
The COVID-19 outbreak decreased the accessibility of medical supplies and medical visits, making PD supply shortages and hard to have blood tests the main concerns of dialysis and transplantation groups, respectively. Individuals aged 18 years old and younger suffering from SARS-CoV-2 infection tend to have a good prognosis (11,12), but patients with comorbidities, such as cardiovascular disease and hypertension, have a higher COVID-19 fatality rate (13). In pediatric patients with kidney failure, their compromised immune system, exposure to hospitals, and high incidence of nutritional deficiency put them in the high-risk category if they contract COVID-19. Fortunately, no confirmed or suspected cases had been reported from 220 respondents at the time of this survey. Also, the five centers included in the study had not received any report of confirmed or suspected COVID-19 cases from their patients. The reason might be that most of our children had a greater chance of staying at home. They are perceived as being vulnerable to infection, and measures, such as avoiding visits to places with dense populations, wearing face masks outside, and washing hands, are part of their care. Meanwhile, health care staff’s early awareness of the potential spread in hemodialysis centers and adaptation of protection in dialysis centers may also prevent the virus from spreading among children on in-center hemodialysis (14). Certainly, the incidence of the COVID-19 among children with kidney failure might be underestimated in our study due to selection bias and self-report bias.
The results of our survey suggested that the COVID-19 outbreak had a great effect on families with children on long-term KRT. Almost 80% of the participants thought that the COVID-19 outbreak negatively affected their child’s treatment. One third of the participants perceived that the effect was severe or extremely severe. Specifically, the effects included difficulties in accessing medical care, acquiring medical supplies, traveling to hospitals, and acquiring financial support. For children after transplantation, it is challenging to have regular kidney function tests and drug concentration monitoring in specialized clinics. For children on home PD, PD fluids, PD cassettes (for APD), iodine caps, tapes, and dressings are necessities. Unlike medications, these PD supplies are not available to order from hospitals in China. They are usually available from medical supply company stores or online, which means that transportation and delivery services are prerequisites to their accessibility to the patients. With ongoing preventative and control measures, such as transportation control, accessing PD supplies has become very challenging, especially in areas with high COVID-19 caseloads.
We found that caregivers of children on kidney replacement treatment had a higher prevalence of clinically significant depressive symptoms (13%) and anxiety (11%) than those in studies in other Chinese populations. With the same cutoff score, the prevalence of depressive symptoms was 4%–5% (15,16), and the prevalence of anxiety was around 5% (8,17). The possible reasons are that the caregivers of the children on kidney failure treatment during the epidemic have parental, medical, and disease prevention responsibilities and that the physical, logistical, and financial challenges they face in caring for their children make them more vulnerable to mental distress. Additionally, the prevalence of depressive symptoms and anxiety of caregivers in our study did not tend to be higher than in previous studies conducted before COVID-19 in caregivers with children on KRT. For instance, 28% of 32 caregivers of children on maintenance PD had probable depression (18); 19% and 47% of 49 caregivers of children on KRT experienced depression and anxiety, respectively (19). However, with the different tools and small sample sizes, it is hard to ascertain whether the differences in the prevalence of depressive symptoms and anxiety before and after COVID-19 were significant.
During this epidemic, we have combined the traditional modes of delivery of health care, such as phone and online interventions, with novel modes of delivery of health care, such as online pharmacy platforms, to respond to the needs of families while minimizing their chances of contracting COVID-19 during hospital visits and to prevent treatment interruptions. We first contacted the families who used up or almost used up the medications or medical supplies to gain a deeper understanding of the individuals’ situations and to offer information, consultation, guidance in using online pharmacy platforms, or medicine delivery, as appropriate. Most of the difficulties were solved. Notably, caregivers were very aware of COVID-19, as they listed contracting COVID-19 during hospital visits as one of their top concerns. We also encouraged families to self-evaluate and actively report changes in symptoms or testing results, and then, we offered consultations, suggestions, and references online. Additionally, psychological support was offered on the phone to help families better cope with the situation. In this way, we were able to provide remote interventions for children at home and ensure their medical safety when they postponed their regular follow-up visits due to the outbreak. This implies that in regions with COVID-19 outbreaks, both online and offline resources should be available to provide consultation and to manage families with children on long-term KRT. If possible, professional online platforms, such as consulting or pharmaceutical platforms and digital hospital services, should be in place to serve more patients with enhanced privacy and data support.
This study has several limitations. First, with the evolution of the epidemic and the attendant containment measures, the difficulties and worries of families with children on long-term KRT described in the study may be dynamic, and some difficulties and worries may become more or less prominent. Second, we recruited our potential respondents online and collected their data using electronic questionnaires. Therefore, caregivers who were not familiar with the online survey and whose children were in worse physical conditions were less likely to participate in the study and may have more difficulties, worries, and mental distress. Third, we managed to recruit only six patients with hemodialysis, and therefore, the results may fail to reflect the difficulties and worries of this group.
The COVID-19 outbreak has had physical, mental, logistical, and financial effects on families with children on long-term KRT in China. The most commonly reported difficulties and worries were PD supply shortage and difficulty in having blood tests. With online and offline interventions, these difficulties could be generally addressed.
Disclosures
All authors have nothing to disclose.
Funding
This work was supported by Emergency COVID-19 Research Funding of Children’s Hospital of Fudan University grant EKXGZX005.
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03630320/-/DCSupplemental.
Supplemental Material. Questionnaire.
Supplemental Table 1. Unadjusted analysis of the prevalence of caregivers’ depressive symptoms and anxiety.
Supplemental Table 2. Associations of treatment modality with the prevalence of depressive symptoms and anxiety in caregivers with children on long-term KRT.
References
- 1.Wu Z, McGoogan JM: Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention [published online ahead of print February 24, 2020]. JAMA . Available at: 10.1001/jama.2020.264832091533 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization : Novel Coronavirus (2019-nCoV): Situation Report-11, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4. Accessed January 30, 2020
- 3.World Health Organization : Coronavirus Disease (COVID-19) Situation Report-152, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200620-covid-19-sitrep-152.pdf?sfvrsn=83aff8ee_4. Accessed June 20, 2020
- 4.Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 282: 1737–1744, 1999. [DOI] [PubMed] [Google Scholar]
- 5.Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, Zhang G, Zhou Q, Zhao M: Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 36: 539–544, 2014. [DOI] [PubMed] [Google Scholar]
- 6.Yu X, Tam WW, Wong PT, Lam TH, Stewart SM: The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry 53: 95–102, 2012. [DOI] [PubMed] [Google Scholar]
- 7.He C, Levis B, Riehm KE, Saadat N, Levis AW, Azar M, Rice DB, Krishnan A, Wu Y, Sun Y, Imran M, Boruff J, Cuijpers P, Gilbody S, Ioannidis JPA, Kloda LA, McMillan D, Patten SB, Shrier I, Ziegelstein RC, Akena DH, Arroll B, Ayalon L, Baradaran HR, Baron M, Beraldi A, Bombardier CH, Butterworth P, Carter G, Chagas MHN, Chan JCN, Cholera R, Clover K, Conwell Y, de Man-van Ginkel JM, Fann JR, Fischer FH, Fung D, Gelaye B, Goodyear-Smith F, Greeno CG, Hall BJ, Harrison PA, Härter M, Hegerl U, Hides L, Hobfoll SE, Hudson M, Hyphantis TN, Inagaki M, Ismail K, Jetté N, Khamseh ME, Kiely KM, Kwan Y, Lamers F, Liu SI, Lotrakul M, Loureiro SR, Löwe B, Marsh L, McGuire A, Mohd-Sidik S, Munhoz TN, Muramatsu K, Osório FL, Patel V, Pence BW, Persoons P, Picardi A, Reuter K, Rooney AG, da Silva Dos Santos IS, Shaaban J, Sidebottom A, Simning A, Stafford L, Sung S, Tan PLL, Turner A, van Weert HCPM, White J, Whooley MA, Winkley K, Yamada M, Thombs BD, Benedetti A: The accuracy of the Patient Health Questionnaire-9 algorithm for screening to detect major depression: An individual participant data meta-analysis. Psychother Psychosom 89: 25–37, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He XY, Li C, Qian J, Cui HS, Wu WY: Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Jingshen Yixue 22: 200–203, 2010 [Google Scholar]
- 9.Montag C, Becker B, Gan C: The multipurpose application WeChat: A review on recent research. Front Psychol 9: 2247, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinese Medical Doctor Association of Youth Pediatric Nephrology : Mind maps for online medical consultation and advice for children with chronic kidney disease. Chin J Evid Based Pediatr 15: 15–18, 2020 [Google Scholar]
- 11.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Lo SK, Chan KH, Poon VK, Chan WM, Ip JD, Cai JP, Cheng VC, Chen H, Hui CK, Yuen KY: A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 395: 514–523, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization : Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), 2020. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed February 28, 2020
- 13.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention : [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi 41: 145–151, 2020. [DOI] [PubMed] [Google Scholar]
- 14.Shen Q, Wang M, Che R, Li Q, Zhou J, Wang F, Shen Y, Ding J, Huang S, Yap HK, Warady BA, Xu H, Zhang A; Chinese Society of Pediatric Nephrology and Chinese Medical Doctor Association of Pediatric Nephrology : Consensus recommendations for the care of children receiving chronic dialysis in association with the COVID-19 epidemic. Pediatr Nephol 35: 1351–1357, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen TM, Huang FY, Chang C, Chung H: Using the PHQ-9 for depression screening and treatment monitoring for Chinese Americans in primary care. Psychiatr Serv 57: 976–981, 2006. [DOI] [PubMed] [Google Scholar]
- 16.Chin WY, Wan EY, Choi EP, Chan KT, Lam CL: The 12-month incidence and predictors of PHQ-9-screened depressive symptoms in Chinese primary care patients. Ann Fam Med 14: 47–53, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luo Z, Li Y, Hou Y, Zhang H, Liu X, Qian X, Jiang J, Wang Y, Liu X, Dong X, Qiao D, Wang F, Wang C: Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: A validation study and meta-analysis. Gen Hosp Psychiatry 60: 50–56, 2019. [DOI] [PubMed] [Google Scholar]
- 18.Tsai TC, Liu SI, Tsai JD, Chou LH: Psychosocial effects on caregivers for children on chronic peritoneal dialysis. Kidney Int 70: 1983–1987, 2006. [DOI] [PubMed] [Google Scholar]
- 19.Lima AGT, Sales CCDS, Serafim WFL: Burden, depression and anxiety in primary caregivers of children and adolescents in renal replacement therapy. J Bras Nefrol 41: 356–363, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.