ABSTRACT
Background
The COVID-19 pandemic has altered clinical practice and education in manual therapy globally. Social distancing has limited in-person care and changed health-care provision. Education in manual therapy has moved to online platforms with in-person instruction restricted. The global impact on the clinical practice of manual therapy and education has to date not been explored.
Methods
a questionnaire survey methodology was used. A sample of convenience of global leaders in manual therapy practice and education received an electronic link to two surveys: one on clinical practice and one on education. Contributors could complete one or both surveys.
Results
Twenty-five surveys were received on clinical practice and 23 on education in manual therapy, representing the six major continents. Global themes in clinical practice demonstrated a sudden and dramatic shift away from patient contact, with limited modifications to manual therapy in patient care currently adopted. Themes in education were of a major shift to online learning, development of new modes of student instruction including video-based assessment and virtual case-based instruction.
Conclusion
The international perspectives provided demonstrate a major change in manual therapy practice and education globally. Various approaches have been taken in practice and education without a uniform approach being demonstrated.
KEYWORDS: COVID-19, manual therapy, pandemic, clinical practice, education
Background
The coronavirus disease 2019 (COVID-19) pandemic has created profound worldwide changes in society and health-care delivery[1]. At the time of writing (18 May 2020), the total number of global infections and fatalities was estimated at 4,801,943 and 318,481 [2], respectively. Within physiotherapy clinical practice, substantial changes have already occurred globally, with reductions in active practice and a significant shift in clinical roles for practitioners [3–7]. Guidelines for clinical practice have been developed [8,9], but the focus is on personal and patient protection from infection [3], without guidelines for manual therapy practice or education. No published guidelines exist for in-person clinical practice based upon a risk/benefit framework. Recommendations for the use of manual therapy during COVID-19, such as to improve respiratory function through rib cage interventions are very limited [10], with the limited current focus on the acute and critical phases of patient management, where manual chest wall interventions have not been recommended [10].
Graduate and post-graduate physiotherapy education, inclusive of manual therapy, have dramatically changed [11,12], with nearly all education programs moving to online education and all current hands-on training suspended [8]. The impact of these changes on current educational instruction, though unknown, is presumed to be serious. Residency and fellowship education with a focus on manual therapy is also presumed to have predominantly ceased with in-person mentoring and live educational meetings suspended. A shift to online education and various synchronous and asynchronous methods of instruction has been reported anecdotally but perspectives and the impact of such educational shifts are lacking.
Healthcare practice has shifted toward telehealth and online education. Examples include web-based competency approaches for orthopedic surgeons utilized by 55% of physicians seeking recertification in 2019 [13], online case-based and journal club instruction [14] with over 99% of orthopedic residents using some form of web-based instruction before COVID-19 [13]. Virtual conferences are increasing in popularity in some fields such as surgical orthopedic fellowships [15] and psychiatry [16], including virtual reality training [16].
The physiotherapy field has increased the use of simulation in education [17], and there have been advances in the use of simulation to facilitate the development of psycho-motors skills in manual therapy of the lumbar spine [18–20]. Attempts have been made to include additional online education in cardiopulmonary physiotherapy, with no notable reduction in student ability to achieve learning outcomes [21]. No reports are currently available on the formal use of virtual reality in physiotherapy education. Currently, manual therapy focused courses and conventions are either postponed or canceled, including the global manual therapy conference of the International Federation of Orthopedic Manipulative Physical Therapists (IFOMPT) [22].
It is not known if prior roles of physiotherapists within pandemics influence current practice or education. Responses to the COVID-19 pandemic are likely local and determined by government and regulatory directives, with survival instincts for practices to shift into telehealth within a pragmatic clinical decision-making framework. This rapid shift to telehealth [23] and rapid progression in regulatory authority for its use is building on [24] or creating new authority. The impact of virtual care on the future of manual therapy however is unknown.
Historical perspectives of physiotherapists response to pandemics
The role of physiotherapists in this current time of crisis can be determined by our profession and/or associations, or it can be dictated to us. Historically we developed as a profession in large part due to the skilled use of our hands to bring people back to function and movement [25,26]. During the Spanish flu epidemic of 1918, our profession was in its infancy. It was not until after World War One that physiotherapy became more widely known as a rehabilitative profession; one based on experiences of nurses, masseuses, bonesetters, gymnastic instructors and mechanotherapists. [3,5,27]
The polio epidemic of the 1950s changed our profession dramatically with the need to provide hands-on passive mobilization to near flaccid limbs and trunks [28]. The respiratory function of millions was impaired due to severe muscular atrophy and impaired tissue states. The ‘iron lung’ is a well-known term nowadays even after a near eradication of polio, but did we maximize our potential as a hands-on profession to alleviate the impact on chest wall mechanics for millions?
Subsequent influenza pandemics such as the 1957 pandemic, 1968 pandemic, severe acute respiratory syndrome (SARS) pandemic in 2003 and the H1N1 pandemic in 2009 [29,30] saw millions of individuals affected but no specific stratified response from our profession in the approach to rehabilitation for these individuals. Perhaps this is part of the reason only 49% of individuals post SARS were able to return to function in the workplace [31].
Currently, we have a history of pandemics but not the role of manual therapy within the pandemics. We have no structured guidelines to support decision-making in the provision of, or education in manual therapy. This study seeks to initiate an understanding of current perspectives on the delivery of, and education in manual therapy, during and after the COVID-19 pandemic.
Methods
In order to initiate an understanding of the global implications of COVID-19 on manual therapy, international perspectives needed to be obtained. A questionnaire survey process was developed which ideally is a catalyst for future scientific study. Information was sought from a sample of convenience of global leaders in manual therapy recognized either through prior research publication, as national delegates to IFOMPT or as post-professional educators in manual physiotherapy. Contributors were invited through direct e-mails to complete a questionnaire survey on the impact of COVID-19 on manual therapy clinical practice, education, or both in their region.
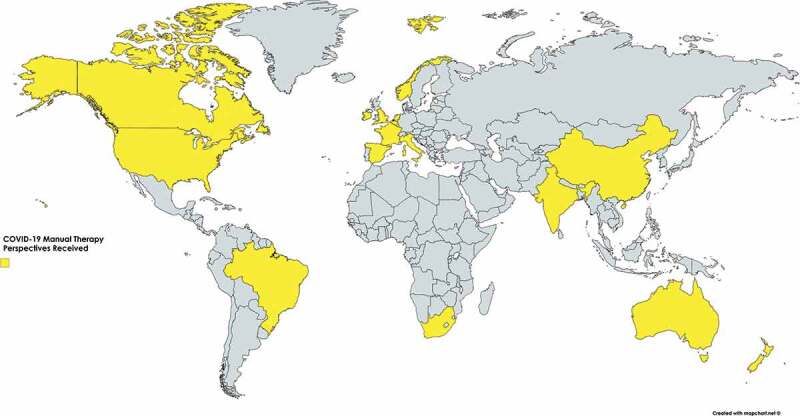
Survey questions were developed and reviewed by the authors, including a trial completion by the authors. Qualitative data for key themes were captured through open-ended questions and quantitative data, via item selection, ranked and scaled responses. Descriptive statistics were utilized to inform an initial understanding of international perspectives. The list of contributors who gave permission to be listed (over 95% of respondents) is provided in Table 1 for Clinical Practice and Table 2 for Education. Global representation is illustrated in Figure 1.
Table 1.
International contributors clinical practice.
| Name | Country |
|---|---|
| Darren Beales | Australia |
| Damien Cummins | Australia |
| Paul Thiry | Belgium |
| Hage Renaud | Belgium |
| Marcelo a. Bracht | Brazil |
| Michael Boni | Canada |
| Xin Zhang | China |
| John Pape | England |
| Frédéric Froment | France |
| Thomas Osinski | France |
| Antoinette Curley | Ireland |
| Filippo Maselli | Italy |
| Firas Mourad | Italy |
| Frédéric Dierick | Luxemburg |
| Svein Kristiansen | Norway |
| César Fernández-de-las-Peñas | Spain |
| Ina Diener | South Africa |
| Jean-Michel Brismee | United States |
| Charalampos Fotiou | United States |
| Steven Kinney | United States |
| Elaine Lonnemann | United States |
| Paul Mintken | United States |
| Ken Olson | United States |
| Louie Puentedura | United States |
Table 2.
International contributors education.
| Name | Country | Affiliation |
|---|---|---|
| Darren Beales | Australia | Australian College of Physiotherapists |
| Darren Rivett | Australia | The University of Newcastle, Australia |
| Peter Osmotherly | Australia | The University of Newcastle, Australia |
| Marcelo a. Bracht | Brazil | Universidade Regional de Blumenau, Brazil |
| Xin Zhang | China | Tong ji University Shangai, China |
| Thomas Osinski | France | efom Boris Dolto-universite, France |
| Senthil P. Kumar | India | Academy of Ortho Man PT, Bethel Medical Mission, India |
| Filippo Maselli | Italy | University of Genova, Campus of Savona, Italy |
| Firas Mourad | Italy | University of Rome Tor Vergata, Italy |
| Duncan Reid | New Zealand | Auckland University of Technology, NZ |
| Svein Kristiansen | Norway | Delegate Norway, IFOMPT |
| Ina Diener | South Africa | CPD Lecturer, Stellenbosch, South Africa |
| César Fernández-de-las-Peñas | Spain | Universidad Rey Juan Carlos, Spain |
| Jean-Michel Brismee | United States | Texas Tech University Health Sciences Center, USA |
| Josh Cleland | United States | Tufts University, USA |
| Chad Cook | United States | Duke University, USA |
| Charalampos Fotiou | United States | Regis University FOMPT, USA + Education in Greece |
| Amy Hammerich | United States | Regis University FOMPT, USA |
| Gary a. Kearns | United States | Texas Tech University Health Sciences Center, USA |
| Elaine Lonnemann | United States | University of St. Augustine, FL |
| Paul Mintken | United States | University of Colorado, USA |
| Louie Puentedura | United States | Baylor University, USA |
Figure 1.
The Institutional Review Board from Des Moines University exempted this study from review. Questionnaires are provided as Appendix A – Clinical Practice and Appendix B – Education.
Clinical practice of manual therapy – Results
Fifty-six percent of respondents were in outpatient practice, 32% in hospital settings and 12% other (combined or academic settings). Societal COVID-19 impact levels, defined as high, medium or low in terms of the societal impact in the region of the contributor, were 56%, 32% and 12%, respectively, with impact levels in regions reported as increasing 24%, stable 44% and decreasing 32%. Forty-four percent of respondents indicated that current approaches were informed in full or partly by prior responses to pandemics. Responses were mainly focused on the use of protective equipment or changing scheduling to limit exposure and 56% of responses indicated physiotherapists are not previously exposed to pandemics.
Decision making for care provision and challenges
The primary screening items for determining if hands-on care was appropriate for individual patients are listed in Table 3. The most frequent items were the presence of cough, potential of exposure, presence of self-quarantine, mask availability and elevated body temperature. Additional reporting found that if screening was completed and no risk identified, hands-on care took place at times without personal protective equipment (PPE), as it was frequently unavailable, or clinicians frequently needed to supply these themselves to provide care outside of hospitals. Clinical reporting from China noted multiple layers of screening such that for patients able to attend a hospital clinic it was stated that ‘… we don’t have any concerns to use manual therapy with our patients’.
Table 3.
Screening items for determining hands-on care during COVID-19 pandemic.
 |
Legend – X-axis, number of contributors reporting the use of each item as a screening tool to determine the ability to provide hands-on care during the COVID-19 pandemic.
Decision-making processes varied among clinicians. One clinician noted that one of the factors that should be considered is ‘to what extent the patient could decline’ as a ‘factor to help the decision-making process’, referring to the medical stability of an individual. It was further stated that ‘ … The challenge is to assess the balance of benefit/risk … we do not know how to evaluate risk factors due to a paucity of background and experience on this topic’. This is supported by only 8% of submissions noting the availability of a risk/benefit approach to clinical decision-making. Additionally, more concern was present when performing upper extremity interventions/techniques when the patient was supine versus prone.
On the topic of whether the current decision-making for the use of manual therapy was optimal, 64% said no, with 48% reporting that physiotherapists were not providing enough manual therapy overall during the COVID-19 pandemic. Examples of challenges were mandates to cease hands-on care, limited access to protective equipment, limiting care to only those patients considered urgent and reporting of political insecurity and social restrictions impacting clinical decisions about care provision. In some circumstances, initial mandates to not provide care were lifted, with urgent cases deemed appropriate with PPE in place, but no PPE was available. Within those reporting optimal manual therapy use, screens between patient and provider glove and mask use were reported.
The clinician was reported as the decision-maker for determining treatment delivery only 27% of the time. Government/regulators were the combined decision-makers 49% of the time, though much overlap in decision-making authority was reported. A decision-making tree based on a risk/benefit approach is provided as an example of a clinical-decision making approach to determine the use of hands-on manual therapy during the COVID-19 pandemic (Figure 2).
Figure 2.
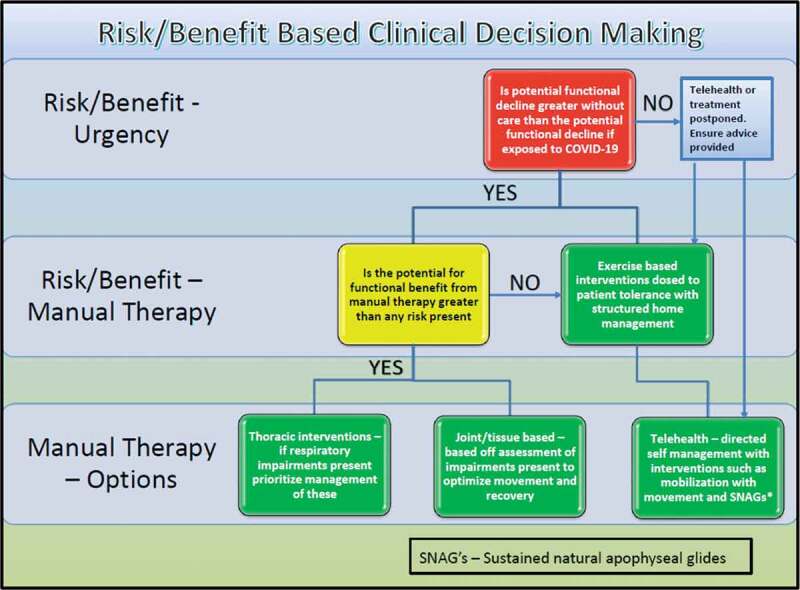
A risk/benefit-based clinical decision-making approach for manual therapy during COVID-19.
Modern ingenuity and critical adaptions in clinical practice
Twenty percent of clinicians reported adapting techniques to the thoracic region, but only in hospital settings to address respiratory impairments. Transfer of physiotherapists from outpatient to inpatient settings for respiratory management was noted in the United Kingdom, USA and Spain. A single reporting of the use of facilitated chest wall mobilization with the use of a home dryer via telehealth for active COVID-19 symptom management was reported.
Eighty-four percent of practitioners reported telehealth was available, with 96% being able to use telehealth, though only 12% before COVID-19. Twelve percent reported not being able to receive telehealth payment, but private pay for this was reported in up to 24%. In the delivery of telehealth, the most frequent mechanism was online or smartphone for over 70%, but 30% were limited to telephone/e-mail. A limited number (20%) reported any form of self-mobilization for patients via telehealth such as self-percussion of the lung fields. Other approaches included self-McKenzie [32] type mobilizations, and self-mobilizations using Mulligan [33] techniques.
In adapting clinical settings, 80% of respondents reported reducing patient volumes in clinics, with 56% removing waiting rooms or directing patients to wait outside in cars. Of concern was that only 8% reported that patients with COVID-19 active symptoms were receiving any management via manual therapy.
Re-envisioning the role of manual therapy with COVID-19
The question of the potential for manual therapy to optimize the human immune system was raised. The very varied response to this question is shown in Figure 3.
Figure 3.
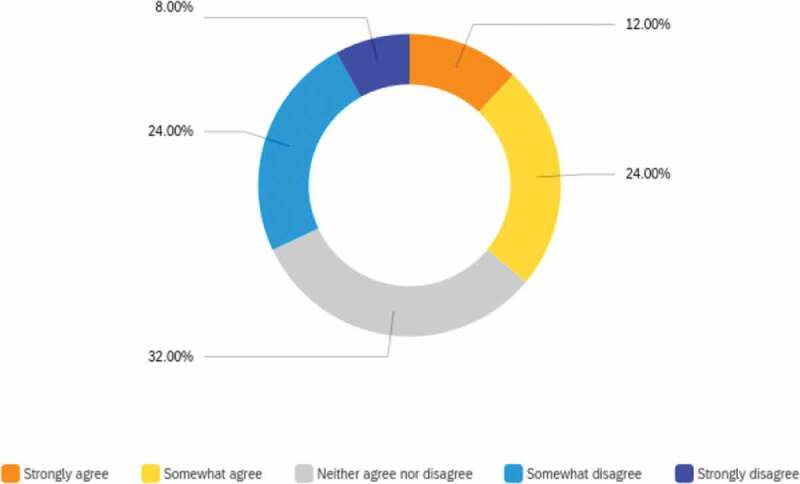
Potential for manual therapy to optimize the human immune system.
In questioning the current and future role of manual therapy, responses included – ‘In Brazil, Physiotherapists can specialize in respiratory and intensive physiotherapy, working in intensive care units to provide mechanical ventilation support to patients with COVID’ and ’Utilization of manual therapy has been helpful at times to help with dyspnea (including thoracic cage mobilization) and pain that would otherwise limit a patient’s participation in exercises and functional mobility training, which are essential for recovery. As sometimes a prone position can significantly help respiratory status, I have found interventions that can make this position more tolerable very valuable ‘.
These responses indicate the potential benefit of manual therapy in managing those with impairments related to COVID-19, but these same individuals reported limited hands-on treatment. It was also noted that there was a ‘… need to redefine … emergency for physiotherapists. The medical world realized that our action was important in order to keep patients active. The risks associated with inactivity are enormous. Painful patients who do not move are very high-risk patients. Not only in terms of musculoskeletal health, but also in terms of cardio-respiratory and general health … and emotional.’
Concerning the overall role of manual therapy within health care, responses emphasized the crucial role manual therapy can take though often ‘underutilized and undervalued’. Of note was the following comment: ‘… manual therapy interventions now have to be considered in a different light in these times. … Inpatient manual therapy … could be an area for growth in manual therapy. Integration of manual therapy will need to occur gradually. Provision of manual therapy will need to occur selectively in situations where a high level of value can be achieved and not at the expense of other best practice standards. Clumsily leaping into this arena likely could set back inpatient manual therapy, so purposeful and deliberate integration needs to occur.’
Finally, it was asked how important it was for a physiotherapist to be involved in the management of an individual with COVID-19 symptoms and how important it was to isolate an individual with COVID-19 from providers and others. On a sliding scale, the first question was scored at a mean of 50% (7–100%) and the second 79% (6–100%). Significant variability was seen in responses.
Education in manual therapy – Results
Critical adaptations in manual therapy education
At the entry level and in post-professional education, repetition in the acquisition of new hands-on skills is considered crucial for developing future clinicians [13]. Questionnaire responses made it very clear that significant challenges are now present for this vital role, and that multiple changes have been and are being made in attempts to address the physical separation between educators and students.
Our respondents were primarily in University/College settings (68%). Fifty to fifty-nine percent reported that changes in education methods included: video review of technique performance, online instruction of techniques, recorded video of techniques for students, while face-to-face instruction was on hold. With the postponement of live instruction, deferral of assessment of hands-on skills and competency has also been put in place in many settings.
Curricular changes have occurred in many settings. An example of the burden of these changes is as follows: ‘We basically take more video for students, and ask students to practice on their family members … instructors view the video and give comments on their performance and feedback periodically … I have a class of 30 students, usually I give them about 4–5 techniques to practice and video for. It took me about 3 hours to review each homework.’ In this circumstance, the workload for technique review was 90 hours!
Another response noted ‘Generally, manual therapy hands-on instruction has been deferred indefinitely … students are being educationally engaged and prepared for the deferred practical classes by provision of access to videotaped instruction in manual therapy techniques with accompanying written resources’. Further, a response spoke to more detail, ‘Delivery of both lab and lecture content is delivered asynchronously. The content is broken into smaller “Ted Talk” videos, i.e. no longer than 10–15 minutes, for easier reference and viewing. Students submit videos of themselves moving through the region-specific assessments, demonstrating selected region-specific special tests and performing selected region-specific manual therapy based on given clinical scenario, i.e. pain relief, improved mobility, etc.’
The crucial development of clinical decision-making skills has been adapted in a variety of ways. Online case reviews and reporting of clinical-decision making have increased, with students submitting videos of their reasoning process. Some processes currently in place have supported the transition to a more virtual educational environment, such as approaches in which ‘… musculoskeletal content always involves asynchronous case studies … each joint complex will have 3 progressively more difficult/complex cases. Once everyone has completed the case studies, we discuss as a group.’
A rapid critical adaption contributed from New Zealand was that ‘We quickly developed a clinical reasoning hypothesis generation sheet that students could work through when we covered the case studies online. a series of power point case studies were developed relevant to the clinical area e.g. Cervical Spine, Thoracic and Lumbar spine conditions. These were delivered … online platform … This can cope with large groups (150+ students), has interactive white board, quizzes, group activities. The case studies were delivered in sections. All these were supported with a hypothesis generation sheet the student had to complete at set intervals in the power point. This made the session more interactive. Following the total class collaborate session, a series of small group labs were set up two days later to answer questions about the lectures and the case studies.’
Student assessment is reported to have changed in some settings ‘Reduced thrust instruction, to one or two techniques. Feel like the introduction is enough, they can specialize later’, or been delayed, or shifted to online assessment via live video interface ‘Students submit videos of themselves moving through the region specific assessments, demonstrating selected region specific special tests and performing selected region specific manual therapy based on given clinical scenario, i.e. pain relief, improved mobility, etc. We assess their techniques on the videos based on a rubric and provide feedback via Zoom call.’ a wide variety of responses made it clear that creativity and a rapid response was in place for many.
New horizons in manual therapy education
Questions to identify areas of success and challenges were presented. In the success domain, it was reported that the use of online courses has allowed for video recording and follow-up student review. Video has allowed for: ’… more individualized feedback for every student. Some students in lab slide by but with the videos we can see ALL students’ performance’. Additionally, ‘much of the feedback from the students has revealed that they’ve had to take more ownership of practicing and critiquing each other (in small groups) than they did in the past’.
In the realm of challenges, responses included: ‘Hands on part is definitely hard. Students needs multi-sensory stimulation to learn. We still planned to give students review class for manual techniques after they return to school.’ Further, ‘Clearly online instruction does not substitute completely for face to face instruction whereby immediate real-time feedback can be provided to an individual student on their handling skills, especially palpatory skills … Students cannot also be expected to practice hands-on skills at home – they do not have the clinically and ergonomically correct set-up (e.g. adjustable plinth) and may live alone without access to a practice partner given social distancing requirements.’ Finally, the acquisition of clinical touch and feel was mentioned by many as a challenge including ‘… the ability to have the student feel a technique or test done by an expert ….’
On the topic of whether or not educational outcomes should be changed due to the COVID-19 pandemic and into the future perspectives were provided including: ’Unfortunately, I think the answer must be YES. If we’re honest, we teach them the correct context for each assessment and how to be as safe and efficient as possible. … Long before COVID-19, I’ve come to realize, my job is to emphasize clinical reasoning to ensure they understand safety, screening and context as much as possible before they get into the clinic where their skills will continue to develop further as they gain context.’ Fifty percent of respondents perceived changes needed to be made in educational outcomes and 50% did not. In addressing current needs, and potential future pandemics it was provided that ‘Hands-on methods needs to be trained with protective gear. Newer types of barrier devices must be evolved. Robotic manual therapy is a viable alternative.’
Perspectives on future methods of instruction in manual therapy included: ‘This COVID situation does bring home the issue that we can do more online than we thought. This could improve costs and time commitments to students. Front loading the theory in line with targeted practical sessions may be the way of the future’. From a similar perspective in seeing new options: ‘We need to teach augmented techniques. Maybe SIM labs have a place’, but caution was also noted ‘… need to gain experience with care during the pandemic and reflect on it. We should not abandon hands-on care if it can be safely provided to patients’.
A final line of inquiry was on the support or challenges from accreditation bodies and regulators in this time of crisis. Sixty-eight percent reported significant support to enable change in educational delivery. A theme in the responses was that the accrediting agencies and regulators have allowed institutions to adapt and been ‘Given scope to implement changes as we see fit. However, further scrutiny to take place upon review after pandemic to ensure requirements and learning outcomes have been met at an appropriate standard.’
Discussion – Conclusion
Physiotherapists are directed, ideally, by individualized clinical decision-making in the delivery of skilled and essential health-care services [34]. Hands-on manual therapy is a critical element in the usual day to day delivery of physiotherapy [35], but now, with the COVID-19 crisis, we are faced with critical decision-making about how we provide care and education in manual therapy. Elements of our profession have moved rapidly, and with minimal training, into providing telehealth-based patient instruction in self-mobilizations and adapted self-management. This may be a temporary fix or an expansion in the value that our profession can provide to address musculoskeletal impairments and develop an increased patient responsibility in their own management, in partnership with their physiotherapist.
In the clinical practice of manual therapy, key findings include that clinicians are bereft in many circumstances of appropriate PPE; or barred from providing care. Clinics are changing entry and exit into buildings, using barriers at times between patients and providers and creating relative isolations in the clinic. Telehealth has become a critical adaptation with self-directed manual interventions provided, but in limited amounts, and many patients being managed with a limited intervention set. Further, a lot of patient care has been deferred at this time with approximately 50% of clinicians concerned that manual therapy care is lacking. The long-term impact of these key findings on individuals with primary musculoskeletal impairments is not known at this time.
Research supports the value of manual therapy for a wide variety of physical impairments [36], but risk/benefit considerations due to COVID-19 raise the question of; what is the current and future value of hands-on care, and how it is prioritized? This is a critical time to reconsider the intent and desired outcome from our manual interventions. An increased emphasis in thoracic interventions to promote respiratory function is indicated, but how it is to be safely provided is not known [10]. If we step away from hands-on care to provide maximal social distancing, do we weaken those who are currently well, and limit their future abilities to fight off the ravages of COVID-19 should they become symptomatically infected?
Key educational findings from this study suggest a new horizon in manual therapy education may be present. Hands-on instruction has declined, virtual instruction and assessment have expanded, and curricula are rapidly evolving with increased focus on clinical reasoning and the defense of reasoning in assessment. We noted increased teaching of manual therapy for respiratory function, instruction for students in patient education virtually for self-mobilization, virtual student mentoring and the use of clinical decision-making self-reflection and virtual case studies [14]. In post-professional residency and fellowship education, the critical role of mentoring in live clinical practice has been severely restricted [37]. These key findings provide an initial frame of reference to ask further key questions going forward about future impacts. It is the task of those who follow to decipher the long-term changes, which will need to be made to optimize future manual therapy education.
Education in manual therapy has been central in the development of physiotherapists since the beginnings of our profession [25,38]. The modes of manual therapy included have varied, from specific joint-based interventions, to more active movement interventions [39]. COVID-19 provides an opportunity in a very challenging time to review our modes of education in manual therapy and re-define what matters. An untested concern is that with reduced hands-on instruction we may graduate clinicians with a reduced skillset; and limit the services that they will be able to provide.
The impact of change in manual therapy instructional methods cannot be determined until the pandemic has subsided; and will then require further research. To optimize telehealth, we will need to provide intentional education and simulations to develop and refine the required skill set in this mode of physiotherapy delivery. Time will need to pass before we are able to assess the impact of these changes in education on manual therapy practice, but in this critical time, we witness adaptations, new ideas, and innovations.
Musculoskeletal impairments are not going away and unfortunately, the current opioid crisis [40,41], which has for the current time been moved from our primary focus, will likely not resolve spontaneously. The crucial role of manual physiotherapy will not be fully replaced by automation, telehealth or a reduction of our profession. Innovative clinical practice and education in manual therapy are happening. Thoughtful reflection on this will inform the future of clinical education and practice in manual therapy.
This study provides international perspectives from the physiotherapy community, but not answers. This study presents primarily rapid-response anecdotal data with limited sample size and formal data analysis, which may limit the interpretation of the results. Further research is needed, with alternative research methods to inform the future of manual therapy in clinical and educational settings as the COVID-19 pandemic continues, matures and ideally recedes. This paper provides perspectives on change; and time will determine which of these we permanently adopt, or set aside, as we find the new normal in manual therapy clinical practice and education.
Acknowledgments
The authors wish to thank the invited contributors to this perspectives paper.
The Institutional Review Boards from Des Moines and Regis Universities exempted this study from review.
Appendix A. Questions – Clinical practice
Q1 – Contributor Information – If your name is included it is your written consent to include your name and geographic location in the manuscript
Name
Location
Q2 – What type of practice setting are you in:
Outpatient private
Outpatient hospital
Other (describe)
Q3 – COVID Impact Level in your region (please chose one)
High
Medium
Low
Q4 – Trend of COVID Impact (please chose one)
Increasing
Stable
Decreasing
Q5 – Are current responses being taken in your region/practice by physiotherapists to manage patients during the COVID-19 pandemic informed by action taken by physiotherapists in prior pandemics?
Yes (describe)
Partially (describe)
No
Q6 – Are physiotherapists in your region/practice adapting manual interventions to the thoracic cage to address respiratory functions during the COVID-19 pandemic? (please briefly describe if yes)
Yes
No
Q7 – Are the current decisions being made in your region/practice optimal for managing patients using orthopedic manual therapy (OMT)? (please provide a brief rationale)
Yes
No
Q8 – As a general statement, have we over-distanced ourselves from patient health-care needs in our OMT response to the COVID-19 pandemic?
No, we have adapted well with our OMT
Yes, we are providing too little OMT patient care
No, we need to be less involved with OMPT
Q9 – What is included in the current decision-making process in your region/practice to determine if hands-on manual therapy can be provided in person? (please check all that apply)
Cough screening
Exposure to COVID positive patients
Exposure to potentially COVID positive patients
Body temperature
Difficulty breathing
Availability of masks
Availability of gloves
Clinician preference
Presence of sore throat
Chills or shaking
Muscle pain
Headaches
Other (describe)
Q10 – What other criteria are you using to determine if hands-on manual therapy should be used for a patient?
Q11 – Who is currently determining whether in-person manual therapy can be provided? (select all that apply)
Government
Regulators
The clinical provider
Professional association
Other (describe)
Q12 – What personal protective equipment is currently available for physiotherapists practicing in outpatient musculoskeletal care in your region/practice? (please check all that apply)
Masks
Gloves
Negative pressure room
Gowns
Face shields
Specialized masks – N95
Other (describe)
Q13 – Is a risk/benefit questionnaire or screening survey available for use in your region/practice to help decide on the use of manual therapy?
Yes
Not sure
No
Q14 – Is telehealth (patient management/treatment via a live video conference) used by manual therapists in your region/practice?
Yes
Not sure
No
Q 15 – If you are using telehealth in your region/practice, for how long have you been able to do this?
2+ years
1–2 years
0–1 years
Only since the COVID-19 pandemic
We cannot use Telehealth
Q16 – Are you able to receive payment for telehealth services?
Yes, since before COVID-19
Yes, since COVID-19
No
Other (describe)
Q17 – What forms of telehealth have you used? (choose all that apply)
Online video
Smartphone
Asynchronous (recorded video or messages)
E-Mail (not pure telehealth)
Telephone (not pure telehealth)
Other (describe)
Q18 – Are patients in your region/practice being instructed in self-mobilization techniques (such as self-percussion of lung fields)?
Yes
Not sure
No
Q19 – Please describe any creative methods of manual therapy performance being utilized in your region/practice to increase patient protections during the pandemic COVID-19.
Q20 – Please indicate different clinical approaches being used to reduce the volume of in-person sessions, or exposure risk, for patients at this time. (select all that apply).
Limited patient numbers in clinic
Reduced number of visits in clinic
Some visits in clinic, some via telehealth
No waiting room in the clinic/wait in car
Staggered schedules for providers/patients
Reduced treatment times
Hands-on interventions (describe)
Other (describe)
Q21 – Are patients with an active diagnosis of COVID-19 receiving in-person manual therapy in outpatient settings in your region/practice?
Yes (describe)
No
Q22 – Are innovations in manual therapy techniques or clinical practice design being created during the COVID-19 pandemic in your region/practice? (examples may be modified manual technique for the chest wall, COVID-19 rehab-specific clinics, etc.)
Yes, new techniques (describe)
Yes, new clinic designs (describe)
No
Q23 – In your opinion, does the use of OMT/manual therapy have a role in improving/optimizing the human immune system to combat disease? (please provide a brief opinion if you wish)
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
Q24 – What is unique in your region/practice that we should consider as it relates to the current and future roles of manual therapy with a health pandemic? (please describe)
Q25 – What is your perspective on the role of a manual therapist in the overall health system? (please describe)
Q26 – On this sliding scales below indicate your opinion as to the importance of physiotherapist management for a symptomatic patient with COVID-19 and the importance of limiting the patient’s interaction with other people (including the provider/PT)?
Level of importance of PT management of a patient with COVID-19 symptoms
Level of importance to not allow a COVID-19 positive individual to be exposed to other people/PT
Appendix B. Questions – Education
Q1 – Contributor Information – If your name is included it is your written consent to include your name and geographic location in the manuscript
Name
Location
Affiliation
Q2 – What type of academic institution/educational setting are you in?
University/College
Private Educational Institution
Other (describe)
Q3 – Within your region/institution, how has education changed for the development of psycho-motor skills in manual therapy? (select all that apply)
Video review of technique performance
Asynchronous instruction being utilized
Online instruction in techniques
Instruction on hold for a period of time
Recorded video of techniques for students
Other (describe)
Q4 – What changes to curriculum have been made in manual therapy programs in your region/institution?
Q5 – What changes have been made to address the development of clinical reasoning skills?
Q6 – How has student manual therapy assessment changed?
Q7 – Where have successes been identified in new approaches?
Q8 – Where have challenges been identified in new approaches?
Q9 – Have accrediting bodies or other institutions provided assistance or guidance for your region/institution?
Yes (describe)
No
Q10 – Should changes be made in the expected educational outcomes in manual therapy to address the impact of COVID-19?
Yes (describe)
No
Q11 – Do we need to change how we educate students in hands-on manual therapy?
Yes (describe)
No
Q12 – Please describe any opportunities that you see for improved manual therapy education due to the impact of the COVID-19 pandemic:
Q13 – Has the COVID-19 pandemic-affected faculty or students from progressing or partaking in scholarly agendas or activities? (select all that apply)
Yes – Faculty
Yes – Students
No
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Velavan TP, Meyer CG.. The COVID-19 epidemic. Trop Med Int Health TM IH. 2020;25(3):278–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].COVID-19 Map . Johns Hopkins Coronavirus Resource Center. [cited 2020 April10]. Available from: https://coronavirus.jhu.edu/map.html
- [3].CGCFE . Spanish Guidelines COVID PT practice PPE. Published online 2020.
- [4].Alpalhão V, Alpalhão M. Impact of COVID-19 on physical therapist practice in Portugal. Phys Ther. Published online Apr 17, 2020. DOI: 10.1093/ptj/pzaa071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pedersini P, Corbellini C, Villafañe JH. Italian physical therapists’ response to the novel COVID-19 emergency. Phys Ther. Published online April 13, 2020. DOI: 10.1093/ptj/pzaa060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Legido-Quigley H, Mateos-García JT, Campos VR, et al. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. Published online Mar 18, 2020;5(5):e251-e252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Haines KJ, Berney S. Physiotherapists during COVID-19: usual business, in unusual times. J Physiother. Published online Apr 2, 2020;66(2):67–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Home page | World Confederation for Physical Therapy . [cited 2018 July8]. Available from: https://www.wcpt.org/
- [9].Landry MD, Tupetz a, Jalovcic D, et al. The novel Coronavirus (COVID-19): making a connection between infectious disease outbreaks and rehabilitation. Physiother Can. Published online March 23, 2020;e20200019. DOI: 10.3138/ptc-2020-0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lazzeri M, Lanza a, Bellini R, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2020;90(1). DOI: 10.4081/monaldi.2020.1285 [DOI] [PubMed] [Google Scholar]
- [11].CAPTE . CAPTE repsone to Covid. [cited 2020 May4]. Available from: http://www.capteonline.org/uploadedFiles/CAPTEorg/Homepage/CAPTEResponsetoCOVID19.pdf
- [12].ABPTRFE . [cited 2020 May4]. Available from:http://www.abptrfe.org/home.aspx
- [13].Rogers MJ, Zeidan M, Flinders ZS, et al. Educational resource utilization by current orthopaedic surgical residents: a nation-wide survey. J Am Acad Orthop Surg Glob Res Rev. 2019;3(4):e041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Clesham K, Piggott RP, Sheehan E. A prospective review of a novel electronic journal club format in an Orthopedic Residency Unit. J Surg Educ. 2020;77(1):115–123. [DOI] [PubMed] [Google Scholar]
- [15].Atesok K, Satava RM, Marsh JL, et al. Measuring surgical skills in simulation-based training. J Am Acad Orthop Surg. 2017;25(10):665–672. [DOI] [PubMed] [Google Scholar]
- [16].Moran J, Briscoe G, Peglow S. Current technology in advancing medical education: perspectives for learning and providing care. Acad Psychiatry J Am Assoc Dir Psychiatr Resid Train Assoc Acad Psychiatry. 2018;42(6):796–799. [DOI] [PubMed] [Google Scholar]
- [17].Mori B, Carnahan H, Herold J. Use of simulation learning experiences in physical therapy entry-to-practice curricula: a systematic review. Physiother Can. 2015;67(2):194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chang J-Y, Chang G-L, Chien C-JC, et al. Effectiveness of two forms of feedback on training of a joint mobilization skill by using a joint translation simulator. Phys Ther. 2007;87(4):418–430. [DOI] [PubMed] [Google Scholar]
- [19].Snodgrass SJ, Odelli RA. Objective concurrent feedback on force parameters improves performance of lumbar mobilisation, but skill retention declines rapidly. Physiotherapy. 2012;98(1):47–56. [DOI] [PubMed] [Google Scholar]
- [20].van Zoest GGJM, Staes FFGM, Stappaerts KH. Three-dimensional manual contact force evaluation of graded perpendicular push force delivery by second-year physiotherapy students during simple feedback training. J Manipulative Physiol Ther. 2007;30(6):438–449. [DOI] [PubMed] [Google Scholar]
- [21].Jones a, Sheppard L. Use of a human patient simulator to improve physiotherapy cardiorespiratory clinical skills in undergraduate physiotherapy students: a randomised controlled trial. Internet J Allied Health Sci Pract. 2011;9(1). Available from:: https://nsuworks.nova.edu/ijahsp/vol9/iss1/12 [Google Scholar]
- [22].IFOMPT . [cited 2020 May4]. Available from: https://www.ifompt.org/
- [23].Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. Published online March 20, 2020;1357633X20916567. DOI: 10.1177/1357633X20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].BIERMAN RT, KWONG MW, CALOURO C. State occupational and physical therapy telehealth laws and regulations: a 50-state survey. Int J Telerehabilitation. 2018;10(2):3–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lonnemann ME, Olson KA, Brismée J-M. The history of IFOMPT: paving the way to global leadership in OMPT excellence. J Man Manip Ther. 2017;25(5):223–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Paris SV. A history of manipulative therapy through the ages and up to the current controversy in the United States. J Man Manip Ther J Man Manip Ther. 2000;8(2):66–77. [Google Scholar]
- [27].Chaitow L. Has osteopathy a role to play in treatment of flu? J Bodyw Mov Ther. 2010;14(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Blum N, Fee E. The polio epidemic in Israel in the 1950s. Am J Public Health. 2007;97(2):218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kilbourne ED. Influenza Pandemics of the 20th Century. Emerg Infect Dis. 2006;12(1):9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].El Zowalaty ME, Järhult JD. From SARS to COVID-19: a previously unknown SARS-related coronavirus (SARS-CoV-2) of pandemic potential infecting humans - Call for a One Health approach. One Health Amst Neth. 2020;9:100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Law RK, Lee EW, Poon PY, et al. The functional capacity of healthcare workers with history of severe acute respiratory distress syndrome (SARS) complicated with avascular necrosis - Case report. Work. 2008;30(1):17–26. [PubMed] [Google Scholar]
- [32].Choi S-Y, Choi J-H. The effects of cervical traction, cranial rhythmic impulse, and Mckenzie exercise on headache and cervical muscle stiffness in episodic tension-type headache patients. J Phys Ther Sci. 2016;28(3):837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Buyukturan O, Buyukturan B, Sas S, et al. The effect of Mulligan mobilization technique in older adults with neck pain: a randomized controlled, Double-Blind Study. Pain Res Manag. 2018;2018:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Jones MA. Clinical reasoning in manual therapy. Phys Ther. 1992;72(12):875–884. [DOI] [PubMed] [Google Scholar]
- [35].Bialosky JE, Beneciuk JM, Bishop MD, et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48(1):8–18. [DOI] [PubMed] [Google Scholar]
- [36].Childs JD, Flynn TW, Fritz JM. A perspective for considering the risks and benefits of spinal manipulation in patients with low back pain. Man Ther. 2006;11(4):316–320. [DOI] [PubMed] [Google Scholar]
- [37].ACGME Response to Pandemic Crisis . [cited 2020 May3]. Available from: https://acgme.org/COVID-19
- [38].Pettman E. A history of manipulative therapy. J Man Manip Ther J Man Manip Ther. 2007;15(3):165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Collins CP, Ling PH. A few words on the curative power of systematized exercises; or the movement cure. Groombridge; London, UK, 1880. [Google Scholar]
- [40].Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharmacol Toxicol. 2018;58:143–159. [DOI] [PubMed] [Google Scholar]
- [41].Zheng P, Kao M-C, Karayannis NV, et al. Stagnant physical therapy referral rates alongside rising opioid prescription rates in patients with low back pain in the United States 1997-2010. Spine (Phila Pa 1976). 2017;42(9):670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]


