SARS-CoV-2 epidemic is moving, shifting its epicenter away from Europe toward the Americas, South Asia and Russia. While in many countries the virus seems to have reached its maximum spread and the number of cases is now decreasing, others are still facing severe epidemics. Interestingly, the disease is showing substantial geographical differences in terms of morbidity and mortality[1]. We investigated whether differences in mortality rates among major Western countries could be associated with the timing of when individual countries’ epidemics began.
We analyzed data from the first 10 European or American countries in terms of population, highest number of documented COVID-19 cases, or the highest number of COVID-19 deaths up to May 20th, 2020[2]. COVID-19 mortality per 1,000,000 population was analyzed 50 days after the beginning of the epidemic in each country[2]. The beginning of the epidemic was defined as the day when the country reached 0.1 deaths per 1,000,000 population [1]. Data were analyzed through a scatter plot, and a line for best fit was identified and presented as Pearson’s R2 coefficient.
Fourteen countries were included in the present report (Figure 1). The mortality rate in the first 50 days of the epidemic ranged between 647 deaths per 1,000,000 population in Belgium (where its epidemic started on March 11th) to 10 deaths per 1,000,000 population in Colombia (where its epidemic began two weeks later). We found an inverse correlation between the date of the beginning of the pandemic and COVID-19 mortality rate (R2 = 0.76).
Figure 1.
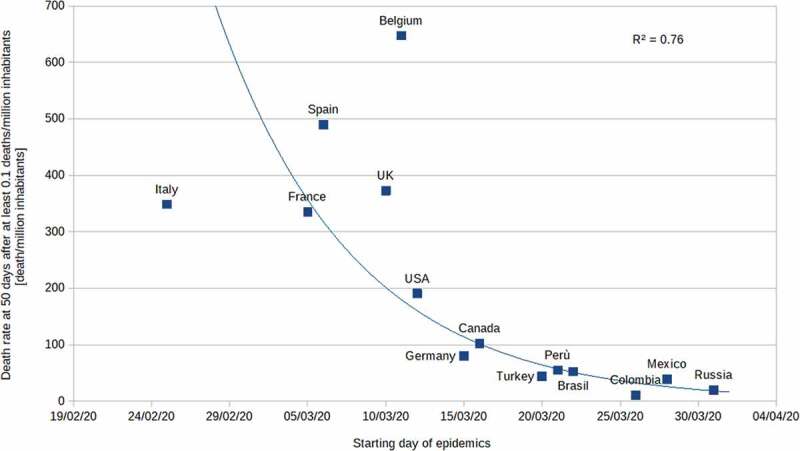
Death at 50 days from fourteen countries.
Scatter plot describing death rate from fourteen countries during 50 days, starting after at least 0.1 deaths per million inhabitants. Presented as Pearson’s R2 coefficient.
Current data hint that the later a specific country was hit by a SARS-CoV-2 epidemic, the softer the impact on mortality during the first 50 days. This interesting epidemiologic finding is open to different speculative explanations. Scientific progress in the pathophysiologic understanding of the disease could play a relevant role, as they might imply a better early medical management including immunomodulatory and anticoagulant therapies [3]. It is also possible that the later the epidemic began, lessons had been learned about bringing lockdown measures in early, and that there was an earlier adoption of ubiquitous personal protections, including facial masks, leading to a reduced viral spread in the community and viral load in the single patient. In fact, fewer undiagnosed cases may have been present in the later countries at the time of lockdown. Moreover, global awareness may have limited COVID-19 diffusion as people at risk (e.g. the elderly, and individuals with comorbidities) were isolated more strictly – or voluntarily decided to do so – in geographical areas that could benefit from others’ experience. We should not forget that unidentified co-factors, including pollution [4], temperature, and coinfection by other viruses, might also have played an unknown role in limiting or facilitating viral spread in determined areas. Lastly, SARS-CoV-2 may have reduced in its lethality, preparing itself to a long-lasting cohabitation with its human hosts. We acknowledge that our work has limitations including countries’ differing COVID-19 death reporting methods (e.g. whether or not countries include out-of-hospital deaths on top of the in-hospital tally).
As a scientific community, every day we are improving our understanding of SARS-CoV-2, and its peculiarities and its pitfalls. Nevertheless, it is evident that what we currently know is preliminary and partial, and further studies are needed to understand the relation between the new virus and the world as we used to know it.
Author’s contributions
Design of the study: Landoni G, Losi D, Fresilli S, Lazzari S, Nardelli P, Puglisi R,
Zangrillo A.
Data collection: Landoni G, Losi D, Fresilli S, Lazzari S.
Statistical analysis: Landoni G, Losi D, Fresilli S, Lazzari S, Nardelli P, Puglisi R,
Zangrillo A.
Manuscript draft and critical review: Landoni G, Losi D, Fresilli S, Lazzari S, Nardelli P, Puglisi R, Zangrillo A.
Administrative support: Landoni G, Zangrillo A.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Roser M, Ritchie H, Ortiz-Ospina E, et al. 2020. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. [cited 2020 June11]. https://ourworldindata.org/coronavirus [Online Resource].
- [2].Worldometer . COVID-19 Coronavirus Pandemic. [cited 2020. June 12]. https://www.worldometers.info/coronavirus/.
- [3].Ciceri F, Beretta L, Scandroglio AM, et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis [published online ahead of print, 2020 Apr 15]. Crit Care Resusc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Frontera A, Cianfanelli L, Vlachos K, et al. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J Infect. 2020. [published online 20th May 2020]. DOI: 10.1016/j.jinf.2020.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]


