ABSTRACT
Background
The aim of this study is to describe the successful emergency plan implemented by Padova University Hospital (AOUP) during the COVID-19 pandemic.
Methods
The emergency plan included early implementation of procedures aimed at meeting the increasing demand for testing and care while ensuring safe and timely care of all patients and guaranteeing the safety of healthcare workers.
Results
From 21 February to 1 May 2020, there were 3,862 confirmed cases of SARS-CoV-2 infection in the Province of Padua.
A total of 485 patients were hospitalized in AOUP, of which 91 were admitted to the ICU; 12 .6% of admitted patients died. The average bed occupancy rate in the ICU was 61.1% (IQR 43.6%:77.4%). Inpatient surgery and inpatient admissions were kept for 76% and 74%, respectively, compared to March 2019.
A total of 123,077 swabs were performed, 19.3% of which (23,725 swabs) to screen AOUP workers. The screening of all staff showed that 137 of 7,649 (1.8%) hospital workers were positive. No healthcare worker died.
Discussion
AOUP strategy demonstrated effective management of the epidemic thanks to the timely implementation of emergency procedures, a well-coordinated effort shared by all hospital Departments, and their continuous adjustment to the ongoing epidemic. Timely screening of all hospital workers proved to be particularly important to defend the hospital, avoiding epidemic clusters due to unknown positive cases.
KEYWORDS: SARS-CoV-2, Covid-19, hospital management, safe care, system capacity, prevent secondary infections, healthcare workers protection, ward reorganization, pharyngeal swab test
Background
The Coronavirus disease 2019 (COVID-19) represents the most serious public health, political, economic emergency of the post-second-war period [1,2]. So far more than 4 million cases of SARS-CoV-2 infection and almost 280,000 deaths have been reported by WHO [3]. Italy became the second country after China for the number of cases and deaths within approximately 20 days after the first case of local transmission was reported on 21 February 2020 in northern Italy and remains one of the most affected countries with 214,103 confirmed cases and 27,955 deaths as of 7 May 2020 [4,5].
Because targeted therapeutic drugs or protective vaccines for COVID-19 do not currently exist, public health and infection control measures are the most effective means to prevent human-to-human transmission. Isolation of confirmed and suspected cases, contact tracing and testing are crucial efforts to slow the spread of the infection and limit epidemiological impact. Healthcare facilities, particularly hospitals, face many challenges to manage the potentially overwhelming burden of illnesses that stresses system capacity while ensuring patient care and preventing adverse effects and infections among healthcare workers [6]. As of 7 May 2020, the number of hospitalized patients with COVID-19 in Italy was 22,793 (15.7% of positive cases), and 1,471 of these (6.4% of positive cases) were admitted to the Intensive Care Unit (information available for 67.7% of the positive cases)[5]. Given the high rate of hospitalization of COVID-19 patients (4.6 per 100,000 population as reported by the Center for Disease Control and Prevention) [7], occupational exposure of healthcare workers represents a major concern that needs to be properly managed. In China, an estimated 3000 healthcare workers were infected and at least 22 have died [6]. Evidence of high transmissibility and hospitalization rate further warns of the importance of vigilance, preparation, active management and protection[6]. In Italy 23,925 positive cases were diagnosed among healthcare professionals, equal to 11.1% of the total reported cases[5]; in Lombardy, the most affected Italian region, at the beginning of the outbreak up to 20% of the hospital workers became infected and some died [4].
As a major point-of-reference hospital for northern Italy and first reference center in Veneto region for COVID-19, Azienda Ospedale Università Padova (AOUP) has promptly implemented an emergency plan to coordinate the management of hospitalized patients – including those with COVID-19, of personal protection and surveillance of healthcare workers and laboratory testing. Here, we report on how the early implementation of such measures has allowed AOUP to provide care effectively for a rapidly increasing number of COVID-19 patients while ensuring the safety of healthcare workers and all patients.
Azienda Ospedale Università Padova (AOUP)
AOUP is recognized as a National Relief Highly Specialized Hospital and is identified as a Regional Reference Center in Veneto region, serving approximately 1 million persons. The medical care provided is of a very high standard and the transplantation activity places the AOUP at the top in Italy for numbers and type of surgery. Volume and type of services provided are very important: 1,700 beds, about 70,000 hospital admission a year and about 60,000 surgical operations a year (about 350 organ transplants). Outpatient facilities count more than 7 million specialist visits every year. A strong focus on teaching and research in collaboration with the University of Padova complement high-level healthcare activities.
Materials and methods
Implementation of the emergency protocol
AOUP had an emergency plan in place already at the beginning of February to manage a possible outbreak of COVID-19 within the Veneto region, even though at that time, the disease appeared to be primarily confined within China, Korea and regions of South-East Asia and in Italy a couple of Chinese tourists had been found positive to COVID-19. The emergency plan included the early implementation of procedures to rapidly identify suspect cases of individuals manifesting COVID-19 symptoms, who were immediately transferred from the Emergency Ward and isolated from other patients requiring attention. A dedicated area of the Infectious Disease Unit was allocated for testing suspect cases and for managing patients with confirmed diagnosis of COVID-19 PCR viral genome detection from pharyngeal swabs. A total of 152 swabs were performed between 1 February and 21 February on patients who presented with respiratory tract symptoms and who had recently returned from China to allow for early detection of positive cases – at a time when infection spread had yet to be reported in Italy. In addition, since the end of January 2020, AOUP started to prepare stockpile of specific equipment and medical devices, including ventilation systems, CPAP machines, other medical devices and personal protective equipment (PPE). The Microbiology Unit rapidly validated an in house rtPCR test that is capable of providing positive/negative results within 3 hours and acquired large quantities of reagents and materials in anticipation of a possible spike in the request of pharyngeal swab test.
With emergency procedures already in place from an early time, we were able to activate the AOUP Crisis Unit as soon as the first positive case of COVID-19 due to local transmission was confirmed on 21 February 2020. The AOUP Crisis Unit included the Infectious Disease Unit, the Microbiology Laboratory, the Emergency Ward, the Intensive Care Unit, the Preventive Medicine Unit and the Safety and Security Unit – all under the guidance of the Hospital Direction. Since its activation, the Crisis Unit has met once or twice daily to provide regular updates of the situation, analyze and solve urgent matters, adjust shorter- and longer-term organizational needs according to the constantly changing epidemiological scenarios, and coordinate healthcare providers and ensure compliance with evolving guidelines at the international, national and regional level.
In order to adapt to the rapid spread of COVID-19, the hospital underwent a reorganization to achieve the following critical objectives:
allocate dedicated spaces to meet the increasing demand for testing and care;
ensure safe and timely care of patients;
ensure safety of healthcare workers.
Each action is briefly described below.
Allocate dedicated spaces to meet the increasing demand of testing and care
The allocation of separated and dedicated areas is considered a crucial measure to avoid possible interactions between infected and non-infected patients, prevent secondary infections and separate contaminated and non-contaminated areas. It also represents an effective means of protecting the safety of healthcare workers and allows more effective use of protective personal equipment according to the working area and specific risk assessment. The areas that were dedicated to this purpose are:
Emergency Ward (EW):
a pre-triage area outside the EW to receive non-hospitalized patients and identify suspect cases;
a dedicated EW area to isolate suspect cases and care for patients with confirmed infection;
twelve outdoor mobile tents raised adjacent to the Infectious Disease Unit used as ‘swab-zone’ for testing of suspect cases as well as for follow-up and management of clinically stable patients.
Upon admission to the EW, patients with respiratory tract symptoms and/or fever were tested for COVID-19 using pharyngeal swabs. As a precautionary measure, swab screening for COVID-19 was performed on all patients admitted to the hospital irrespective of their pathology in order to prevent close contact of asymptomatic patients and other hospitalized individuals and healthcare workers.
Radiology Unit: a mobile CT-scan was installed outside the EW for examining COVID-19 suspect or confirmed patients.
Work schedule in the Microbiology Laboratory was rearranged to ensure testing activities would continue around the clock, 24 hours/day and 7 days/week.
Three isolated hospital wards with dedicated staff were created to care for COVID-19 patients: No-Intensive Care Unit (NICU), Sub-Intensive Care Unit (SICU) and Intensive Care Unit (ICU). We established separate access between the tents, the COVID-19 wards and the hospital areas dedicated to non-infected patients to avoid cross-contamination.
Ensure safe and timely care of patients
The organization of the Medical Department underwent a drastic change to increase hospital bed capacity and staff resources dedicated to COVID-19, with entire hospital floors repurposed for COVID-19 care, existing healthcare providers reassigned to these areas, and new staff members hired to help manage the COVID-19 emergency. Specifically:
Infectious Disease Unit: the entire unit (29 beds, negative pressure rooms) was repurposed for exclusive care of COVID-19 patients. Outpatient services were relocated to make 29 additional beds available.
Internal Medicine Departments: the entire Department was reorganized to dedicate two entire Units (49 beds) for COVID-19 patients non-intensive care.
Respiratory Pathophysiology Unit: 18 beds of sub-intensive care unit (SICU) were activated for COVID-19 patients with respiratory failure undergoing noninvasive ventilation.
Intensive Care Unit: the two general ICUs (29 beds) available at AOUP have both been dedicated to COVID-19 intensive care and the Cardiac Surgery ICU (10 beds) was also re-purposed; then, the total number of ICU beds for COVID-19 patients was 39. A new ICU was created (11 beds) for post-anesthesia care and non-infected patients.
Operating Room: activity was maintained for emergency care, oncological diseases, transplantations and non-deferrable surgery, according to clinical judgment.
Preventive measures were taken to ensure the safety of patients, visitors and healthcare providers:
Non-essential outpatient activities (face-to-face appointments and planned procedures) were postponed. Only urgent non-deferrable visits and procedures were guaranteed, following clinical judgment.
TeleHealth Service was activated where possible to replace in-person appointments.
Online meetings and web conferences replaced in-person meetings, where possible.
The number of patient visitors was limited to one at a time, after visitors were administered a rapid anamnestic interview and their temperature was tested to detect possible infections.
Patients and visitors in clinical settings were supplied with surgical masks.
The cafeteria had restricted schedule and capacity with no tables.
Medical apprenticeships and internal fellowship followed restrictions according to guidelines from the University of Padova.
Frequency of cleaning and disinfection of environmental surfaces was increased, and hypochlorite-based products were used at higher concentrations of 0.5% (5000 ppm), according to international guidelines [8]. Rooms where patients with COVID-19 cared for underwent extraordinary sanitization interventions using no-touch technologies (vaporized hydrogen peroxide and silver salts) to supplement terminal cleaning after a patient had been discharged or transferred. Additional training of outsourcing cleaning staff was implemented to reinforce good practices, standard precautions, safe disinfectant preparation, use of equipment and use of dedicated or single-use supplies for COVID-19 ward. We also organized training sessions for healthcare workers to refresh environmental cleaning procedures and adequate use of PPE. Inside the Hospital, high-touch surfaces such as door and window handles, elevator panels, handrails, bathroom surfaces and work surfaces were identified as priority zones and items for disinfection.
Ensure safety of healthcare workers
Transmission of COVID-19 infection to healthcare workers is a major risk that has the potential to disrupt the continuity of care and to further spread the infection among the vulnerable population of patients and among other members of the healthcare force. The correct use of personal protective equipment (PPE) is a fundamental measure to prevent the risk of infection among the hospital staff. The hospital management prepared and communicated promptly all guidelines related to the use of PPE within 48 hours of the first confirmed case in the Veneto region. All healthcare workers in COVID-19 Unit were provided with FFP2/FFP3 respirators and protective suits and goggles. A high level of coordination was maintained to ensure rapid re-stocking of PPE, their distribution to Clinical Units and adequate training on their correct use to hospital staff members. Following Hospital Direction, the Preventive Medicine Unit activated a dedicated telephone line, available 24 hours/day, for the purpose of answering questions from healthcare workers, for communicating positive swab test results, and for epidemiological investigations. A plan of active surveillance was implemented, according to the Italian ministry’s recommendations, for testing all healthcare workers who were in close contact with confirmed cases or who show signs of respiratory symptoms and/or fever. In case of a positive swab, the worker was required to self-isolate at home for 14 days and could come back to work after two negative swabs. In case of close contact with a positive case, workers were allowed to continue working but was required to repeat the swab test every 5 days for 2 weeks, and to closely self-monitor possible respiratory symptoms, cough and/or fever.
To further strengthen preventive measures, a screening plan for all healthcare providers and employers was implemented: by the beginning of April (less than 40 days from the first confirmed case in Veneto region), all hospital workers were tested at least once with a pharyngeal swab for early detection of possible asymptomatic cases.
Statistical analysis
Continuous data were expressed as medians and interquartile ranges (IQR), and categorical data as numbers and percentages. Continuous and categorical data were compared between ICU and non-ICU groups using the Mann–Whitney test and chi-square test, respectively (a p-value < 0.05 was considered statistically significant).
Data were extracted from AOUP official sources and Regional reports from Azienda Zero also reported in the press and on-line.
Results
Figure 1 reports the daily number of hospitalizations and deaths due to COVID-19 in the Province of Padua: the number of hospitalizations and the number of deaths remained below 250 and 200, respectively. ICU admissions did not follow the increase in non-ICU hospitalizations. Positive cases (not shown in the figure) had a linear increase from approx. 1000 to almost 4000 then followed by a plateaux stage. On 1 May 2020, the fatality rate in the Province of Padua was 6.4%. Similar data patterns in hospitalizations and deaths can be observed from AOUP data (see Figure 2). On May 1, the total number of patients admitted to hospital was 485, of which 91 (18.8%) needed intensive care. Patients admitted to the ICU were primarily males (75.2%), with a median age of 69 years and comorbidities (84.6%) (Table 1). Death was reported in 12.6% (60) of hospitalized patients. The median length of hospital stays of the 434 patients discharged at the time of analysis was 9 days (IQR 5:15).
Figure 1.
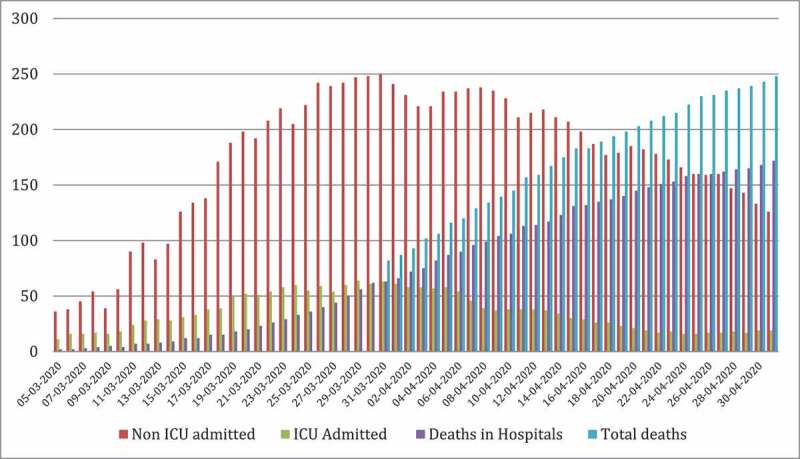
Number of ICU and non-ICU hospitalizations, number of total deaths and hospital deaths from March 5 to 1 May 2020 in the Province of Padua.
Figure 2.
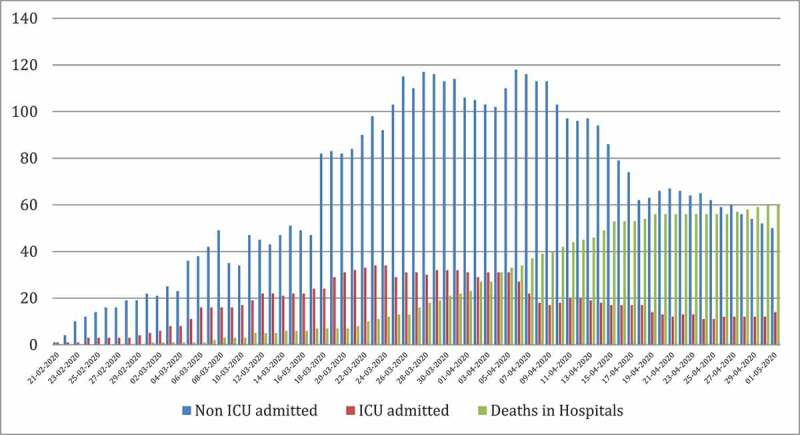
Number of ICU and non-ICU hospitalization and hospital deaths from 21 February to 1 May 2020 in AOUP.
Table 1.
Demographic and clinical data of patients admitted to ICU and Covid-19 ward, from 21 February to 1 May 2020 in AOUP (COPD: chronic obstructive pulmonary disease).
| Total | ICU | Non-ICU | p-value | |
|---|---|---|---|---|
| N | 485 | 91 | 394 | ·· |
| Age (median, IQR) | 65.0 (54.0–77.0) |
69.0 (61.0–77.0) |
64.0 (53.0 − 78.0) |
0.046 |
| Sex (%) M F |
288 (59.4%) 197 (40.6%) |
69 (75.2%) 22 (24.8%) |
219 (55.6%) 175 (44.4%) |
0.0004 |
| Comorbidities Cardiovascular disease Diabetes Malignancy COPD Obesity Others |
384
(79.2%) 161 99 80 69 49 112 |
77
(84.6%) 32 23 16 20 21 24 |
307(77.9%) 129 76 64 49 28 88 |
0.156 |
Figure 3 shows the progressively increasing number of available COVID-19 beds in ICU and the number of positive critical patients admitted in the ICU in AOUP. Note that the number of ICU beds progressively increased with increasing demand, and ICU never reached full capacity. Median bed occupancy rate was 61.1% (IQR 43.6%:77.4%) during the entire period of analysis and 66.7% (IQR 55.6%:79.5%) in the first 50 days of the epidemic outbreak.
Figure 3.
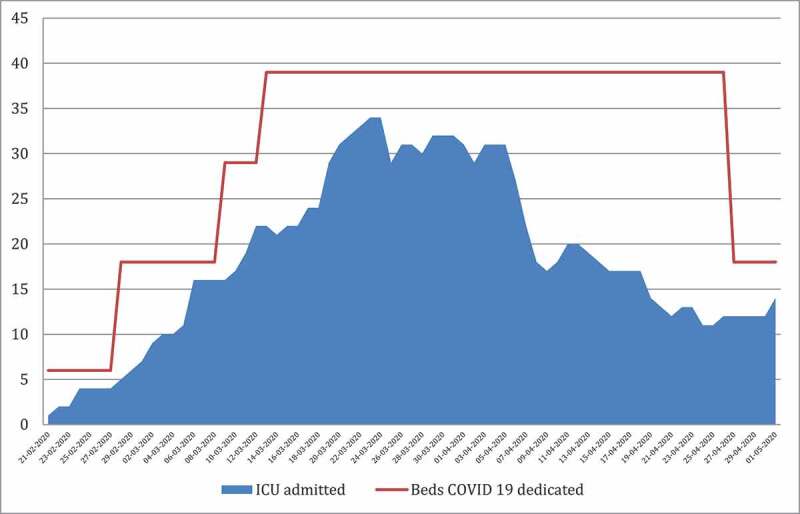
Number of ICU beds dedicated to COVID-19 patients and number of patients admitted in ICU in AOUP from 21 February to 1 May.
Since the time COVID-19 started to spread in Veneto, a large number of pharyngeal swab tests were performed on patients and healthcare workers (see Figure 4). A total of 123,077 swabs (at the time of 1 May 2020) were performed (on average of 1,194 swabs a day), of which 19.3% (23,725 swabs) for screening healthcare workers (in blue). The Microbiology Unit worked 24 hours/day 7 days/week, producing test results consistently throughout the entire day (median number of swab processed per hour every day was 68.1 (IQR 63.6:80.1)). AOUP patients (in red) include inpatients and outpatients referring to AOUP, as well as individuals screened in the AOUP ‘swab-zone’. The green bar represents all swab tests analyzed in AOUP that arrived from other health facilities and hospitals of the Province of Padua and Veneto region.
Figure 4.
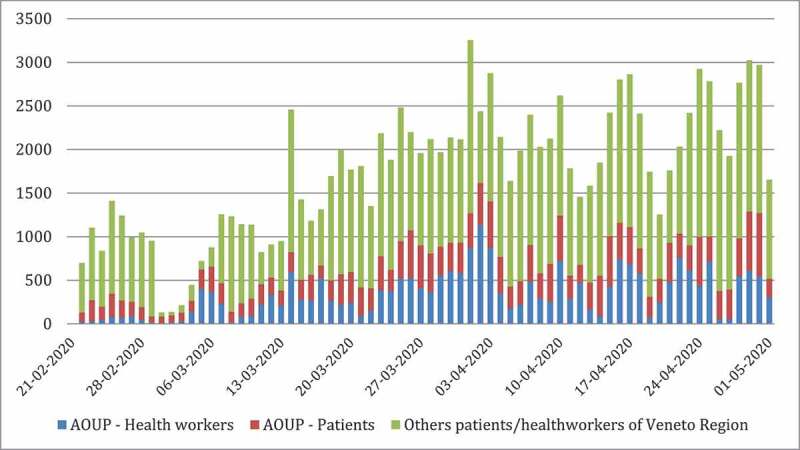
Numbers of swab tests performed in AOUP Microbiology Unit between 21 February to 1 May 2020 in patients and in healthcare workers.
Table 2 reports the number of positive pharyngeal swabs among healthcare workers in AOUP (1.8% of all hospital workers tested). All staff underwent at least two swabs over the period considered. The active surveillance did not include off duty workers, such as people on maternity or prolonged sick leave or junior doctors in training in other healthcare facilities in Italy and abroad (513 workers). The percentage of hospital staff that underwent testing was 93.7%.
Table 2.
Number of positive workers in absolute value (left) and as a percentage of total number of AOUP employees (right) between 21 February and 1 May 2020.
| Positive Cases | Healthcare Workers | Cumulative Incidence | |
|---|---|---|---|
| Physicians | 56 | 2585 | 2.17% |
| Nurses | 42 | 2770 | 1.52% |
| Sanitary Operator | 25 | 971 | 2.57% |
| Others | 17 | 1323 | 1.28% |
| Total | 137 | 7649 | 1.79% |
Figure 5 displays a slight reduction in the number of hospital admissions (ordinary and day hospital) in March 2020, during COVID-19 outbreak (−30.5% compared to March 2019). The number of surgical treatment admissions (outpatients, day hospital, ordinary) in the same period shows a similar decrease (−33%) compared to March 2019.
Figure 5.
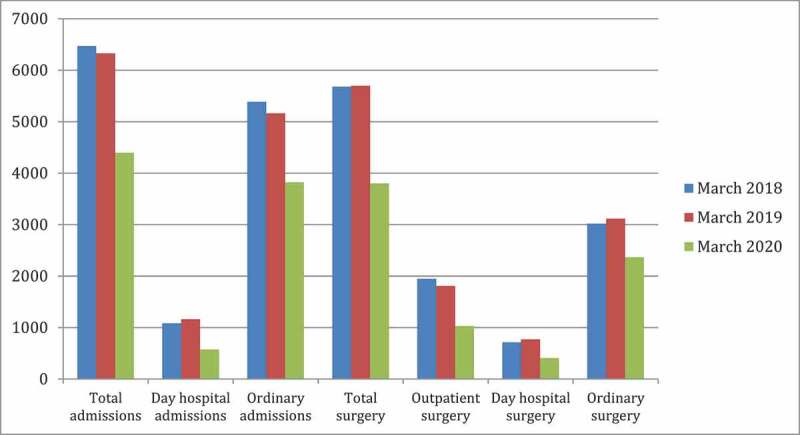
Number of AOUP admissions and surgical treatments (total and for clinical settings) in March in the last 3 years.
Discussion
Recent studies of the COVID-19 epidemic in mainland China [9,10] suggested that rapid and decisive interventions are the most effective means of controlling the spread of the disease in the absence of targeted therapeutic drugs or protective vaccines, even though the long-term effectiveness of these containment measures remains unclear.
In Italy, the National and Regional Governments developed emergency plans to limit the spread of the infection amongst the population [11] immediately after the first case of SARS-CoV-2 infection in the country was reported on 21 February 2020. Despite these efforts, the infection spread first within the Lombardy and Veneto regions in Northern Italy and soon thereafter throughout the entire country.
At AOUP an emergency plan to manage a possible outbreak of COVID-19 was put in place already at the beginning of February 2020, even before the first local positive case in Italy, and then further developed. The plan included extensive measures that proved to be critically important to: (1) deliver effective care to all patients (COVID-19 and non-COVID-19 patients) without disruptions due to increasing demand for intensive care over a short period of time; (2) ensure the safety of healthcare workers; and (3) avoid the spread of the infection within the hospital caused by close-contact of symptomatic or asymptomatic COVID-19 patients, visitors, caregivers and healthcare workers with non-infected individuals.
These measures included the reorganization of hospital infrastructures and the implementation of new management procedures to: (1) create separate paths and dedicated areas for testing, diagnosis and care of COVID-19 patients; (2) increase bed capacity to over 100 beds (107) in the Internal Medicine Departments and to 39 beds in ICU dedicated to COVID-19 care; (3) create new areas for sub-intensive care of COVID-19 patients (18 beds). This important reorganization was implemented in a very short time (2 days) and was continuously re-assessed and adjusted on a day by day basis to adapt the emergency plan according to ongoing developments and possible epidemiological scenarios – a great challenge considering the high volume, variety and complexity of the AOUP hospital activities. The implementation of SICUs for those patients who needed noninvasive ventilation or had been discharged from ICUs proved to be particularly valuable because it allowed to meet the growing demand for intensive care as COVID-19 spread in the general population while providing adequate resources for all patients. As a result of this and other reorganizational efforts, AOUP was able to gradually increase ICU bed capacity in a manner that anticipated the growing demand for intensive care in the hospital. As a matter of fact, ICU median occupancy rate remained around 66.7% even during the first 50 days of the epidemic outbreak. At the same time, AOUP was also able to continue ensuring the highest level of care as the point-of-reference hospital in the region for no-COVID-19 related health issues. Even though the total number of hospital admissions decreased by a third in March 2020 compared to the same month in the previous year, the Surgery Department performed 2,367 high-level treatments, which is 76% of the activity of the previous year, despite the ongoing COVID-19 emergency. Similarly, 24 organ transplants were performed at AOUP during the first 40 days of epidemic.
Another challenge of COVID-19 management consisted of meeting the increasing demand for pharyngeal swab tests to the Microbiology Unit – the regional point-of-reference laboratory for the COVID-19 emergency that was tasked with running tests for the hospital as well as for neighboring provinces. This critically important task was successfully accomplished through a well-coordinated effort that allowed rapid supplies of reagents, materials and new equipment; and the rearrangement of the work schedule to ensure testing activities 24 hours/day 7 days/week. Since the beginning of the epidemic, 123,077pharyngeal swabs have been analyzed by AOUP (of which 23,725 to screen healthcare workers). The high availability of testing was crucial to allow screening of asymptomatic individuals for early detection of positive cases, who were placed in isolation to avoid secondary infections in the hospital and spread of the infection amongst the general population.
It was also remarkable that all hospital staff, both symptomatic and asymptomatic, was tested at least once, unlike other Italian and International situations [12–14]. Screening measures, in conjunction with the prompt and correct use of personal protective equipment (PPE) due to hospital training[15], contributed to a very low prevalence of positive cases amongst healthcare workers (1.8% of the 7,678 AOUP healthcare workers) and no death. These numbers are much lower than those reported in other regions, such as Lombardia [4], and to the general situation in Italy where 23,925 healthcare workers contracted the COVID-19 infection and 79 have died[5]. AOUP infection rates are also significantly lower than those reported amongst Chinese healthcare providers (3,300 infected – 3.8% of the total – and 22 deaths)[6].
The implementation of a overall screening of all workers in AOUP allowed the early detection of asymptomatic positive cases avoiding the presence and spreading of epidemic clusters inside the hospital wards. These early action results have been critical to fight the surge of COVID-19 at AOUP and avoid epidemic clusters within the hospital that are a major cause of infection spreading to patients and other healthcare providers[16]. The implementation of a pharyngeal swab screening plan for all workers also contributed to reduce the anxiety of the staff and mitigate workforce depletion[17].
Overall, AOUP model demonstrated effective management of the epidemic thanks to the timely implementation of emergency procedures that were constantly adjusted according to ongoing spread of the disease and a well-coordinated effort shared by all hospital departments.
Contribution
AOUP COVID-19 Experts Team: Margherita Boschetto, Alfio Capizzi, Annamaria Cattelan, Francesco Causin, Vito Cianci, Luciano Flor, Alberto Friziero, Paolo Navalesi, MariaVittoria Nesoti, AnnaMaria Saieva, Maria Luisa Scapellato, Ivo Tiberio, Roberto Vettor, Andrea Vianello.
Authors’ contribution
All authors have approved the manuscript and have significantly contributed to it.
GC: study conception and design, supervision and drafting of the manuscript. CC: intellectual content, drafting of the manuscript and critical revision. DGB: intellectual content, statistical analyses, interpretation of data and drafting of the manuscript. GB: intellectual content, drafting of the manuscript. SEB: intellectual content, statistical analyses, data interpretation and drafting of the manuscript. SM: supervision and drafting of the manuscript. AOUP COVID-19 ET: drafting of the manuscript and critical revision. RS: intellectual content, statistical analyses, drafting of the manuscript and critical revision. DD: study conception, design, supervision and drafting of the manuscript.
Disclosure statement
None of the authors has any financial support or conflicts of interest to declare.
Ethics committee approval
The manuscript did not require ethics committee approval.
References
- [1].Lai CC, Shih TP, Ko WC, et al. Severe acute respiratory Syndrome coronavirus 2(SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020. DOI: 10.1016/j.ijantimicag.2020.105924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].WHO . Coronavirus disease (COVID-19)-situation report – 112. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200511-covid-19-sitrep-112.pdf?sfvrsn=813f2669_2
- [4].Remuzzi A, Remuzzi G.. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].ISS . Epidemia COVID-19: aggiornamento nazionale 7 Maggio 2020–ore 16:00. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_7-maggio-2020.pdf
- [6].Adams JG, Walls RM.. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. [DOI] [PubMed] [Google Scholar]
- [7].CDC . Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 States, March 1 –30, 2020. Weekly. 2020;69(15):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].WHO . Cleaning and disinfection of environmental surfaces in the context of COVID-19. Interim guidance. 15 May 2020. https://www.file:///C:/Users/a065082/Downloads/WHO-2019-nCoV-Disinfection-2020.1-eng.pdf
- [9].Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5(5):e261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions for containing the COVID-19 outbreak in China. Nature. 2020. DOI: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ordinanza contingibile e urgente del Ministero della Salute e della Regione del Veneto. https://www.regione.veneto.it/documents
- [12].Hunter H, Price DA, Murphy E, et al. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395:10234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Keeley AJ, Evans C, Colton H, et al. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020;25:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Tostmann A, Bradley J, Bousema T, et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Euro Surveill. 2020;25:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].World Health Organization . Rational use of personal protective equipment for coronavirus disease 2019COVID-19. 27 February 2020.
- [16].Friese CR, Mason DJ. Protecting health care workers against COVID-19 and being prepared for future pandemics. Jama. 2020. https://jamanetwork.com/channels/health-forum/fullarticle/2763478 [DOI] [PubMed]
- [17].Black JRM, Bailey C, Przewrocka J, et al. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]


