Abstract
Background
Limited medical facilities are available due to Covid-19 pandemic. Nevertheless, all efforts should be made in planning judicial and possible methods of delivering health care, particularly to pregnant woman with GDM. GDM may play a crucial role in the increasing prevalence of diabetes and obesity and also may be the origin of cardiometabolic diseases.
Methods
It is mandatary to diagnose and care pregnant woman with GDM. The test suggested to diagnose GDM has to be evidence based and in this regard “a single test procedure” evaluated meets this requirement. This doable test has been accepted by the Diabetes in Pregnancy Study Group India (DIPSI) and approved by MHFW-GOI, WHO, International Diabetes Federation, and International Federation of Obstetricians and Gynecologists. MHFW-GOI also recommends testing at first antenatal visit and then at 24–28 weeks of gestation. This opportunity can also be utilized for performing ultrasonography for assessing fetal development.
Result
The first-line management is MNT and life style modifications. Non-responders may require insulin or OHA. The target glycemic control is FPG ~ 5.0 mmol/dl (90 mg/dl) and 2 h PPPG ~ 6.7 mmol/dl (120 mg/dl). The goal is to obtain newborns birth weight appropriate for gestational age between 2.5 and 3.5 kg, a step to prevent offspring developing diabetes.
Conclusion
The essential precaution required during COVID pandemic is to wear face mask, avoid crowded places, and maintain social distancing. Finally, the economical and evidence based “single test procedure” of DIPSI is most appropriate for screening during the COVID pandemic.
Keywords: Gestational diabetes mellitus (GDM), Medical nutrition therapy (MNT), Oral hypoglycemic agent (OHA), Postprandial plasma glucose(PPPG), Fasting plasma glucose (FPG), Ministry of Health and Family Welfare, Government of India (MHFW-GOI)
Introduction
The world has turned topsy-turvy with the COVID-19 pandemic. This will adversely affect the medical profession, particularly in the diagnosis and care of people with diabetes. This is going to result in an epidemic of diabetes. The prevalence of diabetes increasing globally forms 463 million in 2019 to 700 million in 2045, a 51% increase [1]. While several reasons are ascribed for this rising trend including aging population, urbanization, genetic predisposition, nutrition, and lifestyle transition, one factor that has not received adequate attention is glucose intolerance that occurs during pregnancy. GDM may play a crucial role in the increasing prevalence of diabetes and obesity [2]. In 2019, the global prevalence of hyperglycemia in pregnancy (HIP) in the age group 20–49 years was estimated to be 20.4 million or 15.8% of live births [1]. They had some form of hyperglycemia in pregnancy, of which 83.6% were due to GDM [1].Thus, it has become necessary that all women should be screened for GDM even if they have no symptoms [3].
The prevailing opinion is that pregnant women do not appear more likely to contract the infection than the general population [4, 5].It is known that while pregnant women are not necessarily more susceptible to viral illness, pregnancy-related physiological changes influence their immune system and this can be associated with more severe symptoms [6], particularly true in the third trimester.
In the COVID pandemic times, widespread anecdotal evidence suggests that both clinicians and pregnant women are increasingly unwilling to recommend or undergo an OGTT [7]. The problem is the test results are available around 3 h after OGTT and then GDM women have to undergo additional health service visits for diabetes education, glucose monitoring review, and fetal ultrasonography, all of which carry exposure risk during a pandemic. Hence, there is a need for guideline which is universally acceptable [7].
Problems and solutions for screening
There are eleven guidelines to diagnose GDM [1]. The frequently recommended guideline is that of the International Association of Diabetes in Pregnancy Study Group (IADPSG) [8]. Presently, this guideline’s importance is declining because of the comment that even at centers that accepted IADPSG recommendation, the approach varies and needs revision for standardization of the strategy for diagnosing GDM [9]. All the diagnostic criteria require women to be in fasting, but most of the time, pregnant women do not come in the fasting state because of commutation [10]. OGTT which requires three blood samples is resource intensive and many health services are not able to routinely perform an OGTT in pregnant women. Therefore, options which do not involve an OGTT are required. Furthermore, attending the first prenatal visit in the fasting state is impractical in many settings [10]. Even in developed countries (e.g., UK), a fasting blood test at the antenatal booking is often inconvenient [11]. The dropout rate is very high when a pregnant woman is asked to come again for the glucose tolerance test [10].
The guidelines and diagnostic criteria which are simple and feasible on the ground are important [12].A prospective study elucidated a test procedure that would not require a woman to be in the fasting state to diagnose GDM. The outcome of this study was, the 2-h plasma glucose ≥ 7.8 mmol/dl (≥ 140 mg/dl) with 75-g oral glucose administered to a pregnant woman in the fasting or non-fasting state, without regard to the time of the last meal was able to identify a woman with GDM [13–15]. The Diabetes in Pregnancy Study Group India (DIPSI) has accepted this “single test procedure” for diagnosing GDM. The National Institute of Clinical Excellence (NICE) guidelines also recommend 2-h PG ≥ 7.8 mmol/dl as one of the diagnostic criteria for GDM based on the study performed in the multi-ethnic population of UK [16]. This doable procedure is approved by the Ministry of Health & Family Welfare Government of India [17], WHO [10], FIGO [18], and IDF [19]. This procedure is being followed in Sri Lanka [20], Pakistan [21], Bangladesh [22], and may be in many other countries.
Diagnosis of GDM with 2-h PG ≥ 7.8 mmol/dl and treatment is worthwhile with a decreased macrosomia rate, fewer emergency cesarean sections, and serious perinatal morbidity, and may also improve the women’s health-related quality of life [23, 24]. Furthermore, the advantages of this “single test procedure” are
Pregnant women need not be fasting.
It causes the least disturbance in a pregnant woman’s routine activities.
It serves as both screening and diagnostic procedures (universal testing is possible).
Laboratory glucose measurement is often not available and testing with a portable plasma glucose standardized meter is the only option [10].
RCT shows the benefit of treating GDM women identified primarily by postload values [10].
There is no high-quality evidence that women and their fetuses benefit from treatment if only the fasting value is abnormal [10].
-
Fasting glucose measurement is insufficient for reliably ruling out GDM [25], particularly in non-Caucasian population [26].
In view of the above, DIPSI single test procedure may be most appropriate for screening during the COVID pandemic also.
Metabolic management during pregnancy
The guidelines are required to maintain maternal plasma glucose in the normal range by MNT and to recommend OHA or insulin whenever necessary for improved perinatal outcomes. The goal is to maintain fasting plasma glucose (FPG) ~ 90 mg/dl (5.0 mmol/dl) and 2-h postprandial plasma glucose ~ 120 mg/dl (6.7 mmol/dl) in GDM patients so as to avoid perinatal complications [27]. Managing GDM is like primary prevention of the disease for the next generation, as it helps to decrease the incidence of type 2 DM in the generations to come.
Management guiding principles
All pregnant women who test positive for GDM for the first time should be started on MNT and physical exercise for 2 weeks. Dietary intake is foundational to optimal pregnancy outcomes because nutritional quality and quantity have an important impact on the overall growth and development of the fetus.
Women should walk/exercise (which she is used to) for 30 min or perform household work.
Women with normal BMI (19.8–26.0 kg/m2) have been recommended to gain a total of 11.4–15.9 kg; for the ones who are overweight (BMI 26.1–29.0 kg/m2), the weight gain recommendation is 6.8–11.4 kg, whereas obese women with a BMI > 29 kg/m2 are permitted weight gain only up until 7 kg.
For women at high risk for excessive weight gain, interventions need to begin in the first trimester. Research on the pattern of maternal gestational weight gain shows that weight gained in the first trimester is more predictive of infant weight than the weight gained in the third trimester [28]. There was no increase in calories in the first trimester, an additional 340 kcal/day during the second trimester, and 452 kcal/ day during the third trimester [29].
If 2-h postprandial plasma glucose (PPPG) remains > 6.7 mmol/dl with MNT and lifestyle changes, metformin or insulin therapy is recommended.
Medical nutrition therapy
Protein is the most important nutrient and one of the measures in the effort to prevent COVID-19. Protein is also important for immunity as the white blood cells are protein themselves and are the first line of defense mechanism to combat any infection and prevent it from affecting the body. In pregnancy 1.1 g of protein is needed per kilogram of ideal body weight. This would mean 60 to 70 g of protein. This has to come from grains, pulses, legumes, eggs, chicken, fish, and meat. Vitamin C is from Amla, zinc from whole grains, and milk products. Vitamin A is from orange and yellow vegetables, egg fish, and milk products. The sources of vitamin D are fish, egg, milk, and oils which are fortified. The sources of vitamin E are nuts, oils, and oilseeds. Selenium is present in milk, eggs, seafood, and chicken. Ginger, garlic, citrus, spinach, sunflower seeds, and red bell peppers are foods that support the immune system. Garlic can help the body to remove harmful toxins, stimulate immune responses, and reduce inflammation. A balanced meal with an emphasis on whole pulses, eggs, fish, chicken, vegetables, and fruits will provide the required nutrients to prevent COVID-19 in pregnant women and those with gestational diabetes also.
Drug management (metformin or insulin therapy)
Metformin or insulin therapy is the accepted medical management of pregnant women with GDM not controlled on MNT. Insulin is the first drug of choice.
Insulin can be started at any time during pregnancy for GDM if MNT fails.
If a pregnant woman is not willing for insulin, metformin can be recommended provided gestational week is more than 12 weeks [30]. The starting dose of metformin is 500 mg twice daily orally up to a maximum of 2 g/day. If the woman’s blood sugar is not controlled with the maximum dose of metformin (2 g/ day) and MNT, there is no other option but to advise insulin.
Hypoglycemia and weight gain with metformin are less in comparison with Insulin.
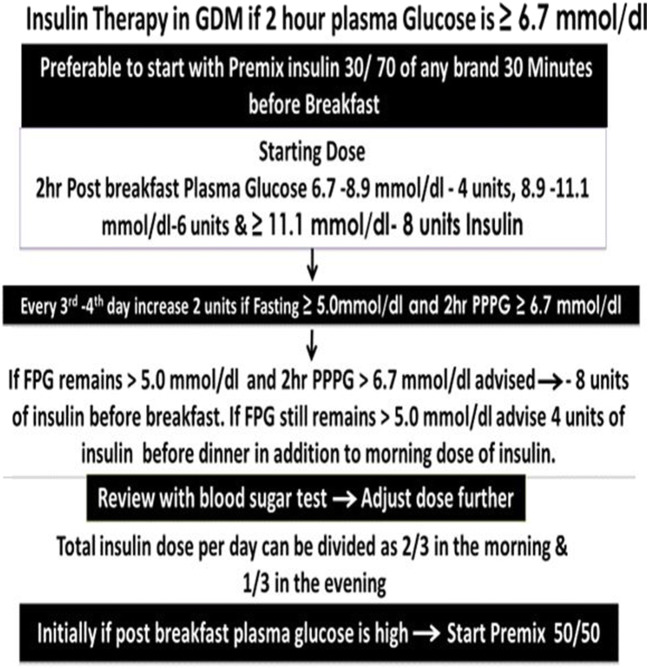
Insulin therapy: (Fig. 1)
Fig. 1.
Insulin therapy
The recommended starting dose of insulin in GDM is 0.1 unit/kg of body weight per day. The dose can be increased on follow-up until 2-h PPPG is around 6.7 mmol/dl.
Rarely, a GDM woman may require more than 20 units of insulin per day. If she requires multiple doses of insulin, she may be referred to a higher center where the physician is available.
Monitoring glycemic control
Fasting and 2-h PPPG can be monitored to adjust the drug dosage. But most importantly, monitoring 2-h PPPG is ideal as when 2-h PPPG is around 6.7 mmol/dl; FPG will never exceed 5.0 mmol/dl.
Laboratory glucose measurement is often not available and testing with a portable plasma glucose standardized meter is the only option.
The WHO (2013) guideline does not include HbA1c as a means of diagnosing diabetes in a pregnant woman and for monitoring [31]?
Ideal will be monitoring as frequently as possible but must be every 2 weeks between the 24th and 28th week of gestation.
After the 28th week every week until delivery.
Treatment modifications in the presence of the COVID-19 pandemic
As alluded earlier, pregnant women experience immunologic and physiologic changes. This might make them more susceptible to viral respiratory infections, including COVID-19. The need to safeguard the fetus adds to the challenge of managing their condition. Antenatal clinics with multiple and traditional face-to-face GDM education sessions now should go for remote delivery, using mobile health tools, interactive webinars, and online resources. If hospital attendance is not possible, blood sugar check-up with standardized glucometers is the alternative choice. After the first check-up and diagnosis of hyperglycemia, where glycemic targets are reached, there are no other risk factors for adverse pregnancy outcomes, and remote obstetric review at 36 weeks allows planning for delivery. But if glycemic and growth parameter targets are not met, or when other risk factors for adverse pregnancy outcomes are present, a face-to-face obstetric review is essential.
The International Federation of Gynecology and Obstetrics (FIGO) has come up with a global interim guidance on COVID-19. This highlights that there is no current evidence that pregnant women are more susceptible to infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or that those infected are more likely to develop severe disease. Poon et al. observed that there is no evidence of vertical transmission [32] (from mother to fetus) but a recent publication documented vertical transmission is possible with no adverse outcome [33].
Special management during the pandemic of COVID 19
Recent publications make it evident about the association of COVID-19 infection in pregnancy with both severe maternal morbidities requiring intensive care and perinatal complications (preterm birth with consequent neonatal morbidity and even perinatal death). Also, the rate of cesarean deliveries among COVID-19 women is very high.
Each pregnant woman should be screened for COVID-19 infection before delivery. For an infected mother, with hyperglycemia, metformin should be continued as it exerts palliative against the infection until any acute complications like ketoacidosis or renal or respiratory failure develop. If not controlled, insulin should be started and will require a higher dosage for COVID-19-positive mothers as the infections damage the glycemic control by its effect on beta cells.
If steroid is used for COVID-19 infection or for fetal lung maturity, insulin dose needs to be increased. Many studies showed that outcomes are worse for patients with COVID-19 infection with corticosteroid use on the outcome of critically ill patients [34].
Antenatal magnesium sulphate given prior to preterm birth (32 gestational weeks) for fetal neuroprotection prevents cerebral palsy (CP) (risk higher with hyperglycemia in pregnancy) and reduces the combined risk of fetal/infant death or CP [35]. Though there is a possibility of a detrimental impact of magnesium sulphate on the respiratory depression in pregnant women with severe COVID-19 disease, appropriate administration with monitoring renal function and maintaining diuresis (≥ 30 mL/h) is not associated with serious maternal adverse effects [36]. Rather, magnesium has also a dilatory effect on bronchodilators, showing even beneficial effects on the pulmonary function in patients with severe asthma and decreasing the production of reactive oxygen species (ROS), which are elevated in patients with acute respiratory distress syndrome, a common complication of COVID-19 infection [37].
Postpartum care
All women who had GDM should be tested for glucose intolerance, 6 weeks after delivery. If FPG is ≥ 5.6 mmol/dl, she should be diagnosed to have impaired fasting glucose (IFG), and if 2-h postglucose is ≥ 7.8 mmol/d, she is diagnosed to have impaired glucose tolerance (IGT) with 75-g oral glucose.
If the GDM woman is on insulin, she may not require insulin immediately after the delivery and in the postpartum period. A GDM woman who was on metformin may be advised to continue if her postpartum blood glucose is ≥ 7.8 mmol/dl. Metformin can be consumed during breastfeeding. It is advisable to continue lactation for 2 to 6 months for delaying the development of diabetes in both the mother and her offspring.
Conclusion
During the COVID-19 pandemic, in order to decrease the risk of infection to pregnant women, it is important to restrict the number of visits to the healthcare facility. She has to take precautionary measures like the use of face masks and hand hygiene while maintaining physical distancing. In order to achieve these objectives, it will be even more pertinent to follow the “single test procedure” for diagnosing GDM. By adopting this procedure, the evaluation for GDM can be done in one visit. Even if the woman comes in the non-fasting state, by administering a 75-g oral glucose load, her plasma glucose can be estimated by taking a blood sample at 2 h. In some situations, the glucose load can also be taken at home and the pregnant woman can visit the hospital 2 h after the glucose ingestion to give a single sample for plasma glucose estimation. If a lab visit is not possible, a plasma glucose standardized glucometer can be used [10]. By this procedure, a prompt diagnosis of GDM can be made, while minimizing the risk of infection to the antenatal women visiting the healthcare facility.
The COVID-19 pandemic is a situation wherein everyone has to provide simple solutions to every problem and the “single test procedure” is ideally suited for screening all pregnant women with minimum contact. Medical nutrition therapy is the sheet anchor in the management of GDM. A woman who does not respond to meal plan and lifestyle modification may be advised insulin or metformin.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.International Diabetes Federation (IDF), Atlas Ninth edition2019. Online version of IDF Diabetes Atlas: www.diabetesatlas.org.
- 2.Ferrara A. Increasing prevalence of GDM. Diab Care. 2007;30(2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 3.Fiore K. United States Preventive Service Task force (USPSTF) backs universal diabetes. Screening. 2014.
- 4.Docherty AB, Harrison EM, Green CA, et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. Med Rxiv. 2020. 10.1101/2020.04.23.20076042.
- 5.Smith V, Seo D, Warty R, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020;15(6):e0234187. doi: 10.1371/journal.pone.0234187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mor G, Cardenas I. The immune system in pregnancy: a unique complexity. Am J Reprod Immunol. 2010;63(6):425–433. doi: 10.1111/j.1600-0897.2010.00836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McIntyreand D, Moses RG. The diagnosis and management of gestational diabetes mellitus in the context of the COVID-19 pandemic. Diabetes Care. 10.2337/dci20-0026. [DOI] [PubMed]
- 8.Boyd E. Metzger. International Association of Diabetes and Pregnancy Study Groups (IADPSG) recommendations on the diagnosis and classification of hyperglycemia in pregnancy. IADPSG consensus panel. Diabetes Care. 2010;33(3):676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lapolla A, Boyd E. Metzger The post-HAPO situation with gestational diabetes: the bright and dark sides. Acta Diabetol. 2018;55:885–892. doi: 10.1007/s00592-018-1146-7. [DOI] [PubMed] [Google Scholar]
- 10.Colagiuri S, Falavigna M, Agarwal MM, Boulvain M, Coetzee E, Hod M, Meltzer S, Metzger B, Omori Y, Rasa I, Inês M, Seshiah V, Simmons D, Sobngwi E, Torloni MR, Yang H-x. Strategies for implementing the WHO diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. DRCP. 2014;103:364–372. doi: 10.1016/j.diabres.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Simmons D, Thompson CF, Engelgau MM. Controlling the diabetes epidemic: how should we screen for undiagnosed diabetes and dysglycaemia? Diabet Med. 2005;22(2):207–212. doi: 10.1111/j.1464-5491.2004.01378.x. [DOI] [PubMed] [Google Scholar]
- 12.Nelison KK, Kapur A, Seshiah V, et al. Factors influencing timely initiation and completion of gestational diabetes mellitus screening and diagnosis. BMC Pregnancy Childbirth. 2017. [DOI] [PMC free article] [PubMed]
- 13.Anajlakshi C, Balaji V, Balaji MS, Ashalatha S, Suganthi S, Arthi T, Thamizharasi V, Seshiah V. A single test procedure to diagnose gestational diabetes mellitus. Acta Diabetol. 2009;46:51–54. doi: 10.1007/s00592-008-0060-9. [DOI] [PubMed] [Google Scholar]
- 14.Franks PW, Looker HC, Kobes S, Touger L, Antonio Tataranni P, Hanson RL, Knowler WC. Gestational glucose tolerance and risk of type 2 diabetes in young Pima Indian offspring. Diabetes. 2006;55:460–465. doi: 10.2337/diabetes.55.02.06.db05-0823. [DOI] [PubMed] [Google Scholar]
- 15.Petit, et al. (12) used the non-fasting 2hour 75 g OGTT Long term effects on offspring. Diabetes. 1991;40(suppl 2):126–130. doi: 10.2337/diab.40.2.S126. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health and Care Excellence. Diabetes in pregnancy: management from preconception to the postnatal period NICE guideline Published: 25 February 2015 nice.org.uk/guidance/ng3. [PubMed]
- 17.Maternal Health Division Ministry of Health & Family Welfare Government of India, www.mohfw.gov.in &www.nhm.gov.in. February 2018.
- 18.Moshe HOD, Kapur A, Sacks DA, Hadar E, Agarwal M, Di Renzo GC, Ruaro LC, Mclyntyre HD, Morris JL, Divakar H. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management and care. Int J Gynaecol Obstet. 2015;131(Supply 3):S173–S211. doi: 10.1016/S0020-7292(15)30033-3. [DOI] [PubMed] [Google Scholar]
- 19.Purandare CN, Sadikot S, Han NC, Hod M. FIGO-IDF Joint Statement and Declaration on Hyperglycemia in Pregnancy. IDF Congress.Abu Dhabi,6th December 2017. www.diabetesatlas.org / atlas@idf.org . [DOI] [PubMed]
- 20.Screening, Diagnosis and Management of Diabetes in Pregnant Women: National Guideline, Sri Lanka. J S Asian Fed Obstet Gynaecol (SAFOG).
- 21.Riaza M, Nawazb A, Masoodc SN, Fawwadde A, Basita A, Shera AS. Frequency of gestational diabetes mellitus using DIPSI criteria, a study from Pakistan. Clin Epidemiol Glob Health. 2019;7(2):218–221. doi: 10.1016/j.cegh.2018.06.003. [DOI] [Google Scholar]
- 22.Sandesh-Panthi, Hasanat MA, Mashfiqul-Hasan, Yasmin-Aktar, Nusrat-Sultana, Sharmin-Jahan, Atiqur-Rahman M, Fariduddin M. Department of Endocrinology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbag, Dhaka, Bangladesh Frequency of gestational diabetes mellitus in Bangladesh impact of WHO 2013 Screening criteria: efficiency of DIPSI and WHO 1999 criteria. JCD 2015;2(2). https://www.researchgate.net/publication/311873204.
- 23.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Effect of treatment of gestational diabetes mellitus on pregnancy outcome. N Engl J Med. 2005;352(24):2477–2486. doi: 10.1056/NEJMoa042973. [DOI] [PubMed] [Google Scholar]
- 24.Gayle C, Germain S, Marsh MS, et al. Comparing pregnancy outcomes for intensive versus routine antenatal treatment of GDM based on a 75 gm OGTT 2- h blood glucose (>7.8 mmol/dl) Diabetologia. 2010;53(Suppl. 1):S435. [Google Scholar]
- 25.Anderson V, Ye C, Sermer M, Connelly PW, Hanley AJG, Zinman B, Retnakaran R. Fasting capillary glucose as a screening test for ruling out GDM. J Obstet Gynaecol Can. 2013;35(6):515–522. doi: 10.1016/S1701-2163(15)30909-9. [DOI] [PubMed] [Google Scholar]
- 26.Wong VW, et al. South-East Asians had the lowest BMI, lowest fasting yet highest 2-hr glucose level on 75-g glucose tolerance test. Diabet Med. 2012;29:366–371. doi: 10.1111/j.1464-5491.2011.03439.x. [DOI] [PubMed] [Google Scholar]
- 27.Seshiah V, Kapur A, Balaji V, Shah SN, Das AK, Diwakar H, et al. Targeting glycemic level in gestational diabetes mellitus to that of normal pregnancy would result in a better maternal-fetal outcome. J Assoc Physicians India. 2019;67. [PubMed]
- 28.Brown JE, Murtaugh MA, Jacobs DR, Jr, Margellos HC. Variation in new-born size according to pregnancy weight change by trimester. Am J Clin Nutr. 2002;76:205–209. doi: 10.1093/ajcn/76.1.205. [DOI] [PubMed] [Google Scholar]
- 29.Food and Nutrition Board . Institute of Medicine: U.S. dietary reference intakes: energy, carbohydrates, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academies Press; 2002. [Google Scholar]
- 30.Singh N, Madhu M, Vanamail P, Malik N, Kumar S. Efficacy of metformin in improving glycaemic control & perinatal outcome in gestational diabetes mellitus: a non-randomized study. Department of Obstetrics & Gynaecology, All India Institute of Medical Sciences, New Delhi, India. Indian J Med Res. 2017;145:623–628. doi: 10.4103/ijmr.IJMR_1358_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Report of a World Health Organization Consultation Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Diabetes Res Clin Pract. 2011;93:299–309. doi: 10.1016/j.diabres.2011.03.012. [DOI] [Google Scholar]
- 32.Poon LC, Yang H, Kapur A, et al. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: information for healthcare professionals. Accessed 12th June 2020. Available from 10.1002/ijgo.13156. [DOI] [PMC free article] [PubMed]
- 33.Susman E. Report: COVID-19 transmitted to babies in utero— Italian researchers confirm two infections at birth, Contributing Writer, Med Page Today July 10, 2020.
- 34.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crowther CA, Middleton PF, Voysey M, et al. Assessing the neuro-protective benefits for babies of antenatal magnesium sulphate: an individual participant data meta-analysis. PLoS Med. 2017;14:e1002398. doi: 10.1371/journal.pmed.1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bain ES, Middleton PF, Crowther CA. Maternal adverse effects of different antenatal magnesium sulphate regimens for improving maternal and infant outcomes: a systematic review. BMC Pregnancy Childbirth. 2013;13:195. doi: 10.1186/1471-2393-13-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shan Z, Rong Y, Yang W, et al. Intravenous and nebulized magnesium sulphate for treating acute asthma in adults and children: a systematic review and meta-analysis. Respir Med. 2013;107:321–30.9. doi: 10.1016/j.rmed.2012.12.001. [DOI] [PubMed] [Google Scholar]