To the Editor:
The risk of HIV transmission is decreased when an HIV-positive individual maintains viral suppression.1 A critical component to maintaining viral suppression is an individual's knowledge of his or her viral load (VL) to make informed decisions around sexual behaviors and reduce the risk of transmission.2 Mounting evidence suggests that limited health literacy is associated with lower HIV knowledge and having a detectable VL.3 Further compounding this challenge is the well-established association of poorer health literacy among people living with HIV (PLWH) from racial/ethnic minority backgrounds.4 Given the disparities in HIV prevalence and outcomes among racial and ethnic minority groups,5 attention to the relationship between health literacy and the knowledge of one's VL has the potential to improve outcomes. The goal of this study was to assess the relationship between health literacy and self-reported VL among racial/ethnic minority PLWH.
This was a cross-sectional analysis of baseline data collected from three research projects aimed to improve outcomes in PLWH. Recruitment was done through flyers and social media websites. Eligibility criteria included those diagnosed with HIV/AIDS, ≥18 years old, able to speak and understand English/Spanish, smartphone ownership, and taking antiretroviral therapy (ART). Exclusion criteria included those who were pregnant, cognitively unable to participate in the study, or having any clinical problems that prevent one to use a smartphone or participate in study activities. All study activities were approved by the Columbia University Irving Medical Center Institutional Review Board.
Sociodemographic covariates were collected through self-report. The shortened version of the Test of Functional Health Literacy in Adults (S-TOFHLA)6 and the Newest Vital Signs (NVSs)7 was used to assess health literacy. Scores on the S-TOFHLA were classified and interpreted as inadequate literacy (scores 0–16), marginal literacy (scores 17–22), and adequate literacy (scores 23–36). The NVS assesses reading and quantitative skills. Scores on the NVS were classified and interpreted as highly limited literacy (scores 0–1), limited literacy (scores 2–3), and adequate literacy (scores 4–6).
Self-reported VL and CD4+ T cell count were obtained during the baseline visit. For VL, participants were asked, “What was the result of your most recent viral load test?” with responses “undetectable,” “detectable,” “I don't know but I think it was undetectable,” or “I don't know but I think it was detectable.” Self-reported viral suppression was defined as “undetectable” or “I don't know but I think it's undetectable.” For CD4+ T cell count, participants were asked, “What was your most recent CD4 or T cell count?” with five options: “less than 200,” “201–349,” “350–499,” “500 or higher,” or “I don't know.”
Biomarker-confirmed measures of VL and CD4 were collected either from serum samples drawn at baseline (n = 140) or from the electronic medical record (EMR; n = 34). Serum samples were sent to the specialty laboratory at Columbia New York Presbyterian Hospital for obtainment of HIV biomarkers. EMR data were the values available at ≤4 months before the baseline visit. All VL values reported undetectable (≤20 copies/mL) and detectable (>20 copies/mL). Using the biomarker-confirmed and self-reported HIV biomarkers, we created variables that reflect accuracy/inaccuracy of VL and CD4.
Descriptive statistics and bivariate analyses were assessed to determine the relationship between sociodemographic characteristics and health literacy as well as their relationship with the inaccuracy of VL. Multi-variable logistic regression was used to assess the association between health literacy and inaccuracy of VL. A two-sided alpha of 0.05 was considered to indicate statistical significance and all analyses used SPSS 25.
Table 1 shows participant characteristics. The mean age for the participants (N = 174) was 49.77 years (23–68 years). Sex was evenly distributed. Most of the participants self-identified as heterosexual/straight (61.5%). Most participants (75.3%) were African American/black, 6.9% were white, and 17.8% were multi-racial or other; 26.4% were Hispanic/Latino ethnicity. Most of our participants completed high school education/General Educational Development (GED) (31.6%). Almost half of the participants (47.7%) reported annual income <$10,000. Most participants (55.2%) had NVS scores that indicate limited literacy, whereas most participants (86.2%) had S-TOFHLA scores that indicate adequate health literacy.
Table 1.
Participant Characteristics by Self-Reported Viral Load Status
| Characteristic | Total |
Accurate VL |
Inaccurate VL |
p |
|---|---|---|---|---|
| N = 174 (100%) | N = 83 (47.7%) | N = 83 (47.7%) | ||
| Race | 0.696 | |||
| White | 12 (6.9) | 4 (4.9) | 7 (8.5) | |
| Black/African American | 131 (75.3) | 62 (75.6) | 63 (76.8) | |
| Other | 29 (16.6) | 16 (19.5) | 12 (14.6) | |
| Hispanic or Latino | 0.298 | |||
| No | 128 (73.6) | 57 (68.7) | 63 (75.9) | |
| Yes | 46 (26.4) | 26 (31.3) | 20 (24.1) | |
| Sex | 0.937 | |||
| Female | 86 (49.4) | 41 (49.4) | 40 (48.8) | |
| Male | 87 (50.0) | 42 (50.6) | 42 (51.2) | |
| Sexual orientation | 0.015 | |||
| Homosexual, gay, or lesbian | 38 (21.8) | 16 (19.3) | 21 (25.3) | |
| Heterosexual or straight | 107 (61.5) | 58 (69.9) | 42 (50.6) | |
| Bisexual | 20 (11.5) | 7 (8.4) | 13 (15.7) | |
| Other | 9 (5.2) | 2 (2.4) | 7 (8.4) | |
| Education | 0.806 | |||
| <High school | 54 (25.3) | 21 (25.3) | 20 (24.1) | |
| High school/GED | 55 (31.6) | 26 (31.3) | 26 (31.3) | |
| Completed some college | 75 (43.1) | 36 (43.3) | 37 (44.5) | |
| Annual income | 0.525 | |||
| <$10,000 | 83 (47.7) | 38 (45.8) | 43 (51.8) | |
| $10,000–19,999 | 46 (26.4) | 22 (26.5) | 20 (24.1) | |
| >$19,999 | 45 (25.9) | 23 (27.7) | 20 (24.1) | |
| On ART | 0.306 | |||
| No | 4 (2.3) | 1 (1.2) | 3 (3.7) | |
| Yes | 169 (97.1) | 82 (98.8) | 79 (96.3) | |
| NVS | 0.644 | |||
| Highly limited literacy | 96 (55.2) | 45 (57.7) | 48 (61.5) | |
| Limited literacy | 50 (28.7) | 26 (33.3) | 21 (26.9) | |
| Adequate literacy | 16 (9.2) | 7 (9.0) | 9 (11.5) | |
| S-TOFHLA | 0.952 | |||
| Inadequate literacy | 13 (7.5) | 7 (8.5) | 6 (7.2) | |
| Marginal literacy | 10 (5.7) | 5 (6.1) | 5 (6.0) | |
| Adequate literacy | 150 (86.2) | 70 (85.4) | 72 (86.7) | |
| Age, mean ± SD | 49.77 ± 9.88 | 49.48 ± 8.87 | 49.43 ± 10.98 | 0.975 |
| Years of HIV diagnosis, mean ± SD | 19.73 ± 8.73 | 20.45 ± 8.51 | 18.51 ± 8.95 | 0.175 |
| NVS, mean ± SD | 1.54 ± 1.45 | 1.59 ± 1.45 | 1.49 ± 1.48 | 0.662 |
| S-TOFHLA, mean ± SD | 30.16 ± 7.16 | 29.98 ± 7.19 | 30.00 ± 7.43 | 0.983 |
ART, antiretroviral therapy; GED, general educational development; NVS, Newest Vital Sign; SD, standard deviation; S-TOFHLA, shortened version of the Test of Functional Health Literacy in Adult; VL, viral load.
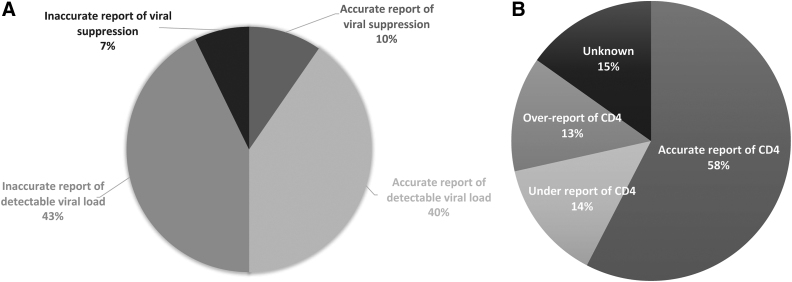
Half of the participants (n = 83) had accurate VL self-report (Fig. 1A). Of those with inaccurate VL, 43% self-reported detectable VL but had biomarker-confirmed measure of viral suppression (n = 71) and 7% self-reported viral suppression but had biomarker-confirmed measure of detectable VL (n = 12). These 12 participants (“transmission risk”) were more likely to inaccurately report their CD4 (χ2 = 6.21, p = 0.013) and have lower NVS score (χ2 = 4.81, p = 0.028) in an unadjusted model. More than half of participants accurately reported their CD4 (Fig. 1B). Of those with inaccurate CD4, 15.2% self-reported “don't know” (n = 24) and 27.3% either over- (n = 21) or under-reported (n = 22) their CD4.
FIG. 1.
(A) Inaccurate report of viral suppression means those who self-reported viral suppression but had biomarker-confirmed measure of detectable VL. Accurate report of viral suppression means those who had both self-reported and biomarker-confirmed measure of viral suppression. Inaccurate report of detectable VL means those who self-reported detectable VL but had biomarker-confirmed measure of viral suppression. Accurate report of detectable VL means those who had both self-reported and biomarker-confirmed measure of detectable VL. (B) Accurate report of CD4 means those who had the same levels of both self-reported and biomarker-confirmed measure of CD4+ T cell count. Under-report of CD4 means those who under-reported their level of CD4+ T cell count but had higher biomarker-confirmed measure of CD4+ T cell count. Over-report of CD4 means those who over-reported their level of CD4+ T cell count but had lower biomarker-confirmed measure of CD4+ T cell count. Unknown means those who self-reported “I don't know” to their CD4+ T cell count. VL, viral load.
Multi-variable logistic regression modeling showed no statistically significant association between health literacy and inaccurate VL. The inaccurate VL was significantly lower among participants who were heterosexuals (odds ratio, 0.28; 95% confidence interval, 0.12–0.68, p < 0.05).
Our results revealed that 50% of our participants inaccurately reported their VL, which is still considerably higher than the inaccuracy levels found in previous studies.8–10 One possible explanation is that our participants may be unaware of their recent VL because they may have significant gaps in care.11,12 Since the contemporary ART regimens are more forgiving in terms of strict adherence and are less likely to show substantial changes in VL, the types of ART and medical visit intervals need to be assessed in future studies.
Half of our participants inaccurately self-reported their CD4. Although there was no relationship between the inaccuracy of CD4 and VL, our findings may suggest that HIV biomarkers are connected to one another and that our participants require more education in HIV biomarkers. In addition, those with potential transmission risk were more likely to inaccurately report their CD4 and have lower NVS score. This highlights the need for education on the dynamic nature of viral suppression and immune function as well as addressing health literacy.
Despite the relationship between health literacy and viral suppression,3 we did not find a significant association between health literacy and inaccurate VL. Heterosexuals were more likely to accurately self-report VL than sexual minority individuals. This finding is surprising since previous studies have reported relatively high levels of accurate VL self-reporting among sexual minority individuals.9,10 One explanation is that our participants with multiple minority identities may face a myriad of minority stress that can exacerbate their understanding of HIV biomarkers, but further study is needed.
This study should be interpreted with limitations. Our use of convenience sampling and the cross-sectional design may not be generalizable to individuals with different demographics and may not explain the causality of relationships. Our sample size was too small for more robust modeling and may have limited statistical power to find associations. Lastly, we were unable to assess some important confounders/covariates such as ART adherence and engagement/gaps in care.
In conclusion, we found that about half of our participants inaccurately reported their VL and that sexual minority individuals were more likely to inaccurately self-report their VL. Further study is warranted to explore how individuals understand their HIV biomarkers, and a more readily available approach in real-time self-testing of VL remains a research priority. There is a need for efforts to address the gap in knowledge of current VL status among racial/ethnic minority PLWH, particularly among sexual minority individuals, to potentially prevent HIV transmission.
Authors' Contributions
M.Y.J. managed the data, conducted the statistical analyses, provided interpretation of findings, and drafted the article. R.S. conceptualized the study, provided the data set, revised the article, and approved submission.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Agency for Healthcare Research and Quality.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported by the National Institute of Nursing Research of the National Institutes of Health and the Agency for Healthcare Research and Quality under the following Award Nos.: T32NR014205, R01NR015737, K24NR018621, and R01HS025071.
References
- 1. Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA 2016;316:171–181 [DOI] [PubMed] [Google Scholar]
- 2. Lampe FC. Sexual behaviour among people with HIV according to self-reported antiretroviral treatment and viral load status. AIDS 2016;30:1745–1759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Perazzo J, Reyes D, Webel A. A systematic review of health literacy interventions for people living with HIV. AIDS Behav 2017;21:812–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Walker RL, Hong JH, Talavera DC, Verduzco M, Woods SP. Health literacy and current CD4 cell count in a multiethnic U.S. sample of adults living with HIV infection. Int J STD AIDS 2018;29:498–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: Social disadvantage and the U.S. HIV epidemic. Am Psychol 2013;68:197–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42 [DOI] [PubMed] [Google Scholar]
- 7. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: The newest vital sign. Ann Fam Med 2005;3:514–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mustanski B, Ryan DT, Remble TA, D'Aquila RT, Newcomb ME, Morgan E. Discordance of self-report and laboratory measures of HIV viral load among young men who have sex with men and transgender women in Chicago: Implications for epidemiology, care, and prevention. AIDS Behav 2018;22:2360–2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sewell J, Daskalopoulou M, Nakagawa F, et al. Accuracy of self-report of HIV viral load among people with HIV on antiretroviral treatment. HIV Med 2017;18:463–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stephenson R, Bratcher A, Mimiaga MJ, Garofalo R, Hidalgo MA, Hoehnle S, et al. Brief report: Accuracy in self-report of viral suppression among HIV-positive men with HIV-negative male partners. J Acquir Immune Defic Syndr 2020;83:210–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rowan SE, Burman WJ, Johnson SC, et al. Engagement-in-care during the first 5 years after HIV diagnosis: Data from a cohort of newly HIV-diagnosed individuals in a large US city. AIDS Patient Care STDS 2014;28:475–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gardner LI, Marks G, Patel U, Cachay E, Wilson TE, Stirratt M, et al. Gaps up to 9 months between HIV primary care visits do not worsen viral load. AIDS Patient Care STDS 2018;32:157–164 [DOI] [PMC free article] [PubMed] [Google Scholar]