Background:
Unicompartmental knee arthroplasty (UKA) is a viable option for patients with symptomatic knee arthritis isolated to 1 compartment. Previous articles have suggested that mobile-bearing UKA should not be performed in patients without bone-on-bone arthritis. The purpose of this study was to compare the clinical outcomes and survivorship of mobile-bearing UKA in patients with severe osteoarthritis with bone-on-bone contact and patients with severe osteoarthritis but without bone-on-bone contact.
Methods:
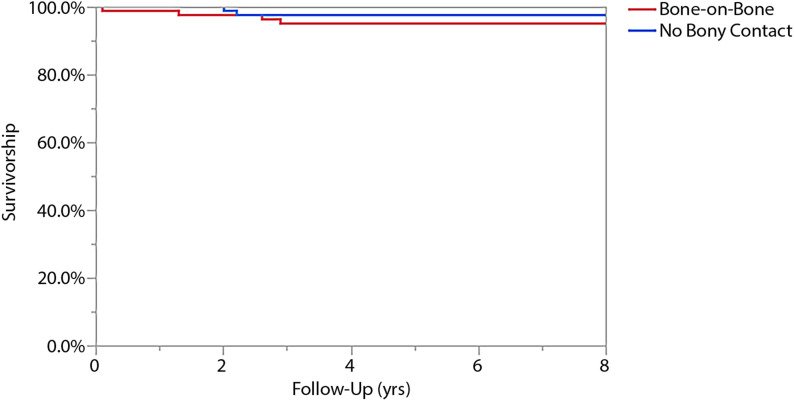
We retrospectively reviewed a single surgeon’s experience with medial compartment mobile-bearing UKA in 219 patients (271 knees) who underwent the procedure between 2007 and 2015. Anteroposterior and posteroanterior radiographs were reviewed, and arthritis was graded using the International Knee Documentation Committee (IKDC) grading system. Only patients with grade D (severe arthritis) were studied. Of the patients who had grade-D arthritis, there were 81 patients (94 knees) with bone-on-bone arthritis and 82 patients (91 knees) without bone-on-bone contact. Functional outcomes were assessed using the Knee Society pain and function scores. Survivorship free of revision in these 2 groups was determined using Kaplan-Meier curves at 8 years.
Results:
There were no significant differences between the 2 groups in terms of age (p = 0.91), sex (p = 0.21), or body mass index (p = 0.63). At the time of the final follow-up, there was no significant difference in Knee Society pain scores (p = 0.59) or Knee Society function scores (p = 0.9) between the 2 groups. There were 5 revisions in the group with bone-on-bone contact and 2 revisions in the group without bone-on-bone contact. The survivorship free of revision at 8 years was 95% for the group with bone-on-bone contact and 98% for the group without bone-on-bone contact (p = 0.45).
Conclusions:
Patients with severe knee arthritis (IKDC grade D) without bone-on-bone contact had similar outcomes of mobile-bearing UKA compared with patients with bone-on-bone contact. UKA is a safe and reliable option in patients with severe osteoarthritis who do not have bone-on-bone contact on preoperative radiographs and it should therefore not be considered a contraindication for mobile-bearing UKA as long as the patient’s symptoms are severe enough to warrant surgical intervention.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Unicompartmental knee arthroplasty (UKA) has emerged as a viable option for patients with symptomatic knee osteoarthritis isolated to either the medial side or the lateral side. The criteria for selecting patients for the surgical procedure have been well described previously and have been expanded in recent years by the Oxford group. Goodfellow and O’Connor published their indications for medial UKA with the Oxford prosthesis in 19861, and Goodfellow et al. followed up with this study in 19882. These criteria included bone-on-bone anteromedial arthritis, a ligamentously normal knee with an intact anterior cruciate ligament (ACL), correctable varus deformity, and a well-maintained lateral joint space1. Despite expanding criteria, the results of UKA have remained satisfactory in the majority of the published series3-8.
The 1 criterion that remains unchanged is that of bone-on-bone anteromedial arthritis, as previous studies have demonstrated inferior outcomes of UKA in patients without bone-on-bone arthritis9,10. As a result, these authors consistently advise against performing UKA in patients without bone-on-bone osteoarthritis. However, these previous studies did not use specific criteria to determine the degree of osteoarthritis prior to the intervention and, instead, incorporated all patients without bone-on-bone arthritis (mild to moderate or severe) into the same group.
The purpose of this study was to compare the clinical outcomes and survivorship of mobile-bearing UKA at a minimum 2-year follow-up in patients with severe osteoarthritis with bone-on-bone contact and patients with severe arthritis without bone-on-bone contact using a standardized osteoarthritis grading system.
Materials and Methods
After institutional review board approval, a retrospective review was performed utilizing our institution’s prospectively maintained total joint registry to identify all consecutive patients who underwent UKA performed by a single senior arthroplasty surgeon (R.J.S.) between January 2007 and December 2015. Surgical indications implemented by the senior author follow a modified version of the Kozinn and Scott criteria11. Patients had degenerative changes limited to a single compartment of the knee, correctable varus deformity of <15°, normal cartilage thickness of the uninvolved contralateral compartment, flexion of at least 100°, and intact cruciate and collateral ligaments. Patients were not offered a UKA if they did not fulfill the aforementioned criteria or if they had 1 of the following exclusion criteria: severe patellofemoral degenerative changes, contralateral compartment involvement (verified radiographically and intraoperatively), fixed flexion contracture of >15°, or a previous diagnosis of inflammatory arthritis. A fluoroscopically aided varus and valgus stress test or a posteroanterior flexion view was used to verify the correction of the varus deformity and full-thickness cartilage on the lateral side.
From November 2007 through December 2015, 271 medial UKAs were performed in 219 patients. The International Knee Documentation Committee (IKDC) validated arthritis grade was then applied to determine the severity of arthritis in each knee12. The IKDC grade is determined radiographically and is divided into 4 separate grades of arthritis. Preoperative anteroposterior, lateral, Merchant, and posteroanterior flexion radiographs were used for grading. Grade A refers to ≥4 mm of joint space without signs of osteoarthritis. Grade B consists of ≥4 mm of joint space with signs of osteoarthritis. Grade C is 2 to 4 mm of joint space with signs of osteoarthritis. Grade D is <2 mm of joint space. There were 185 medial UKAs performed in 163 patients who were classified as grade D, and these were further divided into 2 groups. Two of the authors (S.W.C. and J.S.V.-H.) retrospectively reviewed preoperative radiographs independently for the entire cohort and assigned each patient the appropriate IKDC grade based on digital measurements. When the authors disagreed on a particular grade, the authors reviewed the radiographs and reached a consensus. The first group consisted of 81 patients (94 knees) with radiographic evidence of bone-on-bone unicompartmental osteoarthritis on preoperative anteroposterior or posteroanterior flexion radiographs. The second group consisted of 82 patients (91 knees) with severe, grade-D osteoarthritis, but without radiographic evidence of bone-on-bone contact.
The final medical records of 163 patients were reviewed by 2 of the authors (S.W.C. and J.S.V.-H.). Demographic data, as well as information related to any postoperative complications, were collected from the total joint registry and the electronic medical record. The mean follow-up time was 56 months (range, 24 to 125 months) Demographic data are shown in Table I. There were no significant differences between the 2 groups in terms of age, sex, body mass index (BMI), preoperative knee range of motion, preoperative varus deformity, or the American Society of Anesthesiologists (ASA) physical status classification system, which is used to assess perioperative risk based on a patient’s comorbidities (Table I).
TABLE I.
Demographic Information
| Group with Bone-on Bone Contact (N = 94) | Group without Bone-on-Bone Contact (N = 91) | P Value | |
| Sex* | 0.21 | ||
| Male | 49 | 39 | |
| Female | 45 | 52 | |
| Age at surgery† (yr) | 64.5 (20 to 92) | 64.1 (37 to 89) | 0.91 |
| BMI at surgery† (kg/m2) | 31.3 (16.4 to 45.0) | 32.5 (17.8 to 62.1) | 0.63 |
| Follow up† (mo) | 58.6 (24 to 125) | 56.4 (24 to 122) | 0.96 |
| Preoperative range-of-motion arc† (deg) | 123 (90 to 150) | 120 (90 to 150) | 0.24 |
| Preoperative varus deformity† (deg) | 7.9 (0.5 to 15.2) | 7.4 (0 to 13.8) | 0.33 |
| Implant type* | 0.04 | ||
| Phase III Oxford | 72 | 56 | |
| Oxford Twin Peg | 22 | 35 | |
| ASA score* | 0.56 | ||
| I or II | 71 | 72 | |
| III or IV | 23 | 19 |
The values are given as the number of cases on a per-knee basis.
The values are given as the mean, with the range in parentheses.
All patients underwent medial UKA with the mobile-bearing Phase III Oxford Partial Knee (Zimmer Biomet) or the Oxford Twin Peg Partial Knee Replacement (Zimmer Biomet). In the group with bone-on-bone contact, 72 UKAs were performed with the Phase III Oxford Partial Knee and 22 UKAs were performed with the Oxford Twin Peg Partial Knee Replacement (Table I). In the group without bone-on-bone contact, 56 UKAs were performed with the Phase III Oxford Partial Knee and 35 UKAs were performed with the Oxford Twin Peg Partial Knee Replacement. Patient-reported Knee Society pain and function scores were collected from the electronic medical record and our institution’s total joint registry (Table II)13. There was a significant difference in the implants used between the 2 groups. The senior author (R.J.S.) changed the implant that he used in 2012, resulting in the unequal distribution in this cohort. Survivorship free of revision was calculated using data collected from the electronic medical record and the total joint registry.
TABLE II.
Preoperative and Postoperative Knee Society Pain and Function Scores for Both Groups
| Preoperative Scores* | Postoperative Scores* | P Value | |
| Knee Society pain score | |||
| Group with bone-on-bone contact | 73.1 (47 to 95) | 94.4 (68 to 100) | <0.0001 |
| Group without bone-on-bone contact | 70.0 (45 to 90) | 80.5 (38 to 97) | 0.005 |
| Knee Society function score | |||
| Group with bone-on-bone contact | 68.2 (20 to 100) | 95.2 (15 to 100) | 0.23 |
| Group without bone-on-bone contact | 68.0 (45 to 100) | 90.8 (50 to 100) | <0.0001 |
The values are given as the mean score in points, with the range in parentheses.
Statistical Methods
The mean and the range were used to summarize continuous variables. Categorical variables were presented as absolute numbers and were summarized as percentages. The Student t test was used to compare the mean values of independent continuous variables between the 2 groups. Paired t tests were used to compare the mean preoperative Knee Society pain and function scores with the mean postoperative values in the 2 groups. Categorical variables were analyzed using the chi-square test. Survivorship free of revision was determined with Kaplan-Meier methodology and the log-rank test. Survivorship is reported at 8 years. Significance was set at α < 0.05. All statistical tests were performed with JMP statistical software, version 13 (SAS Institute).
Results
Clinical Outcomes
At a minimum 2-year follow-up, Knee Society scores were available for 46 patients (57%) in the group with bone-on-bone contact and 47 patients (57%) in the group without bone-on-bone contact. For the group with bone-on-bone contact, the mean Knee Society pain score was 94 points (range, 68 to 100 points) and the mean Knee Society function score was 95 points (15 to 100 points), demonstrating a significant improvement from the mean preoperative Knee Society pain scores (73 points [range, 47 to 95 points]; p < 0.0001) and improved Knee Society function scores that did not reach significance (68 points [range, 20 to 100 points]; p = 0.23) (Table II). For the group without bone-to-bone contact, the mean Knee Society pain score was 81 points (range, 38 to 97 points) and the mean Knee Society function score was 91 points (range, 50 to 100 points), demonstrating a significant improvement from the mean preoperative Knee Society pain score (73 points [range, 47 to 95 points]; p = 0.005) and the mean Knee Society function score (68 points [range, 45 to 100 points]; p < 0.0001) (Table II). At the time of the final follow-up, there were no significant differences in the Knee Society pain scores (p = 0.59) and Knee Society function scores (p = 0.9) between the 2 groups.
Survivorship
The survivorship free of revision for the entire cohort was 96% at 8 years. The survivorship free of revision was 95% for those with bone-on-bone contact and 98% for those without bone-on-bone contact (p = 0.45) (Fig. 1). Seven cases (3.8%) in the entire cohort had a revision surgical procedure (Table III). There were 5 revisions (5.3%) in the cases with bone-on-bone contact (Table IV). The mean time to revision was 41 months (range, 0.8 to 125 months) (Table IV). Revisions in this group were for aseptic loosening of the femoral component (n = 2), deep infection (n = 1), polyethylene dislocation (n = 1), and persistent pain (n = 1). Four of these were subsequently converted to a total knee arthroplasty. The UKA with the polyethylene dislocation was treated with revision of the polyethylene. There were 2 revisions (2.2%) in cases without bone-on-bone contact (Table IV). The mean time to revision was 25 months (range, 24 to 26 months). There was no significant difference in the mean time to revision (p = 0.76) or revision rate between the 2 groups (p = 0.42) (Table IV). One revision was for aseptic loosening of the femoral component, and 1 revision was due to tibial component subsidence. Both of these were subsequently converted to total knee arthroplasties.
Fig. 1.
Kaplan-Meier survivorship analysis showing 95% survivorship free of revision for the group with bone-on-bone contact (shown in red) and 98% for the group without bone-on-bone contact (shown in blue) at the 8-year follow-up (p = 0.45).
TABLE III.
Details of the 7 Revisions That Occurred in This Cohort*
| Case No. | Group | Time to Revision (mo) | Reason for Revision | Treatment |
| 1 | Bone-on-bone contact | 0.8 | Postoperative Group-G Streptococcus periprosthetic joint infection | Resection arthroplasty with subsequent conversion to TKA with a stemmed tibial component |
| 2 | Bone-on-bone contact | 15 | Painful left knee that had undergone UKA | Conversion to TKA with a stemmed tibial component |
| 3 | Bone-on-bone contact | 31 | Aseptic loosening of femoral component | Conversion to TKA with stemmed femoral and tibial components |
| 4 | Bone-on-bone contact | 35 | Polyethylene dislocation | Polyethylene bearing exchange with retention of femoral and tibial components |
| 5 | Bone-on-bone contact | 125 | Aseptic loosening of femoral component | Conversion to TKA with stemmed femoral and tibial components |
| 6 | No bony contact | 24 | Tibial component subsidence | Conversion of UKA to TKA with a stemmed femoral component and a stemmed tibial component with a porous sleeve |
| 7 | No bony contact | 26 | Aseptic loosening of femoral component | Conversion of UKA to TKA with a stemmed tibial component |
TKA = total knee arthroplasty.
TABLE IV.
Comparison of Time to Revision and Revision Rate Between the 2 Groups
| Group with Bone-on-Bone Contact | Group without Bone-on-Bone Contact | P Value | |
| Time to revision* (mo) | 41 (0.8 to 125) | 25 (24 to 26) | 0.76 |
| Revision rate† | 5% (5 of 94) | 2% (2 of 91) | 0.42 |
The values are given as the mean, with the range in parentheses.
The values are given as the percentage of knees, with the number of knees in parentheses.
Discussion
The purpose of this study was to assess the clinical outcomes and survivorship of mobile-bearing UKA in patients with evidence of medial compartment bone-on-bone arthritis on preoperative radiographs compared with patients with severe osteoarthritis that did not demonstrate bone-on-bone contact. Previous studies have demonstrated inferior results of UKA in patients without bone-on-bone arthritis. Our data demonstrate that mobile-bearing UKA is an extremely successful operation in patients with severe arthritis (<2-mm joint space according to the IKDC criteria), even in the absence of bone-on-bone contact.
This study must be analyzed considering its limitations. Given the observational and retrospective nature of the study, there is a risk of selection bias and assessment bias. These patients represent a consecutive series of patients of a single surgeon at a large academic institution, and, therefore, these results may not be as generalizable. We excluded patients with milder degrees of osteoarthritis who underwent UKA, intentionally restricting our analysis to specifically examine patients with severe, end-stage osteoarthritis in order to better define this patient population. Furthermore, this study relied on interpretation of knee radiographs to determine the degree of preoperative osteoarthritis, and the ability to determine the amount of joint space is subject to the radiographic measurements made on electronic imaging systems. All of these radiographs were analyzed by the same coauthors, and, therefore, the interpretation of the radiographs remained consistent throughout. In addition, the differences between 2 and 4 mm, as described by the criteria, are broad and easy to apply, making the radiographic analyses reproducible. An additional limitation of this study was that 2 different implants were used throughout the study period. This reflects the primary author changing the implant that he used in 2012 as newer generations of UKA components were developed. Therefore, because there were more patients in this cohort who underwent the surgical procedure prior to 2012, there was an unequal distribution of implant type. A subgroup analysis demonstrates no significant differences in Knee Society pain outcome scores (p = 0.45) and Knee Society function outcome scores (p = 0.31) or survivorship based on implant type (p = 0.62). Therefore, although there was a significant difference in implant type used, this difference had no bearing on patients’ functional outcomes or on the survivorship of the implants in this study period (Table V).
TABLE V.
Subgroup Analysis of Postoperative Clinical Outcomes Scores and Survivorship Free of Revision Based on Implant Type
| Phase III Oxford Partial Knee | Oxford Twin Peg Partial Knee Replacement | P Value | |
| Knee Society pain* | 81 (44 to 98) | 80 (31 to 90) | 0.45 |
| Knee Society function* | 79 (30 to 100) | 87 (50 to 100) | 0.31 |
| Survivorship† | 95.8% | 98% | 0.62 |
The values are given as the mean in points, with the range in parentheses.
The values are given as the percentage of knees with survivorship.
Pandit et al. matched 29 patients with partial-thickness cartilage loss to 29 patients with bone-on-bone arthritis without bone loss and 29 patients with bone-on-bone arthritis with bone loss9. The Oxford Knee Scores for patients with partial-thickness cartilage loss were significantly lower compared with those with bone-on-bone arthritis. There was no difference between the subset of patients with bone-on-bone arthritis with or without bone loss. The authors postulated that patients undergoing UKA with partial-thickness cartilage loss do worse because they could have sources of pain other than arthritis9. In another study, Hamilton et al. matched 94 patients with partial-thickness cartilage loss to 188 patients with bone-on-bone osteoarthritis10. Patients with partial-thickness loss had significantly lower mean Oxford Knee Scores and Knee Society scores at 1, 2, and 5-year follow-ups. Furthermore, outcomes were more variable in patients with partial-thickness cartilage loss compared with patients with bone-on-bone osteoarthritis10. This latter study also reported a higher revision rate with no difference in overall survivorship in patients with partial-thickness cartilage loss compared with patients with full-thickness cartilage loss10. Ultimately, in both of these studies, the authors strictly advised against performing UKA in patients with partial-thickness cartilage loss because of their inferior outcomes. However, both of these series did not follow specific grading criteria for arthritis and seemed to include all patients without bone-on-bone contact into the same group. That is, patients with mild osteoarthritis and full-thickness cartilage may have been included with patients with more severe arthritis but without bone-on-bone contact. More specific details about the severity of osteoarthritis in those studies would be needed to decide whether the lack of bone-on-bone contact is a true contraindication to mobile-bearing UKA.
In contrast to these earlier studies, our current study further used the IKDC validated grading system to classify patients on the basis of the severity of the arthritis. The more severe form, grade D (<2-mm joint space), was subsequently divided into patients with and without bone-on-bone arthritis. This study demonstrated no significant difference in clinical outcomes or survivorship in patients who underwent UKA with bone-on-bone arthritis compared with those who underwent UKA with severe arthritis without osseous contact. Knee Society pain and function scores were nearly identical between the 2 groups. We did not see any differences in revision rates between the groups. Most revisions were performed for mechanical failure of the implants. Within patients without bone-on-bone contact, there were no patients with persistent pain requiring revision. This study did not review the results of patients with IKDC grades A through C, as our intention was to report UKA in patients solely with severe osteoarthritis in the medial compartment.
Patients with severe knee arthritis (IKDC grade D) without bone-on-bone contact had similar outcomes of mobile-bearing UKA compared with patients with bone-on-bone contact. UKA is a safe and reliable option in patients with severe osteoarthritis who do not have bone-on-bone contact on preoperative radiographs, and lack of bone-on-bone contact should therefore not be considered a contraindication for mobile-bearing UKA as long as the patient’s symptoms are severe enough to warrant surgical intervention.
Footnotes
Investigation performed at the Mayo Clinic, Rochester, Minnesota
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSOA/A197).
References
- 1.Goodfellow JW, O’Connor J. Clinical results of the Oxford Knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Related Res. 1986. April;205:21-42. [PubMed] [Google Scholar]
- 2.Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br. 1988. November;70(5):692-701. [DOI] [PubMed] [Google Scholar]
- 3.Riff AJ, Sah AP, Della Valle CJ. Outcomes and complications of unicondylar arthroplasty. Clin Sports Med. 2014. January;33(1):149-60. Epub 2013 Aug 28. [DOI] [PubMed] [Google Scholar]
- 4.Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty. 2012. September;27(8)(Suppl):86-90. Epub 2012 May 4. [DOI] [PubMed] [Google Scholar]
- 5.Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res. 1991. December;273:151-6. [PubMed] [Google Scholar]
- 6.Yang KY, Wang MC, Yeo SJ, Lo NN. Minimally invasive unicondylar versus total condylar knee arthroplasty—early results of a matched-pair comparison. Singapore Med J. 2003. November;44(11):559-62. [PubMed] [Google Scholar]
- 7.Lombardi AV, Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res. 2009. June;467(6):1450-7. Epub 2009 Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012. January;470(1):84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pandit H, Gulati A, Jenkins C, Barker K, Price AJ, Dodd CA, Murray DW. Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee. 2011. June;18(3):168-71. Epub 2010 Jun 2. [DOI] [PubMed] [Google Scholar]
- 10.Hamilton TW, Pandit HG, Inabathula A, Ostlere SJ, Jenkins C, Mellon SJ, Dodd CA, Murray DW. Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss: a medium-term follow-up. Bone Joint J. 2017. April;99-B(4):475-82. [DOI] [PubMed] [Google Scholar]
- 11.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989. January;71(1):145-50. [PubMed] [Google Scholar]
- 12.Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226-34. [DOI] [PubMed] [Google Scholar]
- 13.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989. November;248:13-4. [PubMed] [Google Scholar]