Abstract
Three-dimensional imaging is a useful tool to evaluate liver structure and surrounding vessels for preoperative planning. In this study, we compared two methods of visualizing vascular maps on computed tomography including maximum intensity projection (MIP) and 3D volume rendered (VR) imaging. We compiled important imaging components of pre-surgical planning, and developed criteria for comparison. The imaging techniques were compared based on colorization, volume quantification, rotation, vessel delineation, small vessel clarity, and segmental liver isolation. MIP had more overall limitations due to reduced differentiation of superimposed structures, motion artifact, and interference from calcifications. We determined that because 3D quantitative volume rendered imaging can provide more detail and perspective than MIP imaging, it may be more useful in preoperative planning for patients with liver malignancy. Advanced 3D imaging is a useful tool that can have profound clinical implications on cancer detection and surgical planning.
1. INTRODUCTION
The use of 3D imaging for liver surgeries allows better anatomical visualization for preoperative planning. It provides valuable information that can save the time and resources during the surgical procedures [1]. Liver cancer is a leading cause of death worldwide [2], with secondary metastatic disease being more common than primary liver cancer [3]. The dual blood supply from portal and systemic circulation, the permeability of fenestrated hepatic sinusoidal epithelium, and the liver microenvironment are implicated in development of secondary liver cancers [4]. Among primary liver cancers, the most common form is hepatocellular carcinoma, followed by cholangiocarcinoma. Other less common types of primary liver cancer include fibrolamellar carcinoma, hepatoblastoma, angiosarcoma, and epithelioid hemangioendothelioma [3].
The management approach to hepatocellular carcinoma involves assessment of tumor size and location, extrahepatic metastasis, and underlying liver function. Surgical resection is the only curative treatment. Preoperative assessment depends on radiographic studies to quantify the extent of tumor involvement and assess invasion of vasculature and local structures. This study compares the ability of 3D volume rendering and MIP to define vascular details of the liver.
Multiphase-enhanced CT and dynamic-enhanced MRI are the most effective imaging techniques to detect hepatic tumors less than 2 cm, but can still underdiagnose 25-30% of cases [5,6]. Advanced imaging is useful for delineating vasculature and calculating volume prior to surgery. Advances in CT imaging using unique post-processing techniques, including the utilization of artificial intelligence, have increased its diagnostic accuracy and clinical application [7]. Maximum intensity projection (MIP) is a volume rendering technique based on projecting a volume of interest onto a 3-dimensional viewing plane based on high-intensity structures on CT [8]. The ability of MIP images to preserve attenuation information independent of thresholds makes it widely applicable for visualizing simple anatomic structures. However, MIP is limited by lack of differentiation between foreground and background for superimposed structures, motion artifact from vessel pulsation and respiration, and visual interference from calcifications within atherosclerotic vessels [9].
Three-dimensional volume rendering (3D VR) is a powerful imaging tool that reconstructs 2D CT data into a 3D model with high fidelity. Compared to conventional CT, the longer acquisition times achievable with newer spiral CT can generate more images with higher resolution. The volume data is then resampled based on a series of software algorithms, and manually edited to isolate the region of interest from surrounding structures. Manual segmentation of images is a time-consuming process that involves detailed analysis of size, shape, intensity, location, texture, and proximity to surrounding structures [10]. The automation of this process for 3D imaging continues to be an evolving area of research [11].
The complex vascularity of the liver increases the risk of surgical approaches. Accurate, detailed, and reproducible imaging modalities that highlight subtle anatomic features are essential in preoperative evaluation especially in liver tumor & transplant cases [13]. This study compares the performance of MIP and 3D VR in preoperative imaging for patients with primary and secondary liver malignancies. It delineate more detailed information in a short period of time using the advanced imaging technology specially using one click MIP technique. The overall idea is to define the quickest and more precise method to get maximum information in a limited period of time so the surgeons can review the images for better understanding.
2. MATERIALS AND METHODS
This study examined the utility of 3D VR and MIP for anatomic delineation of hepatic vascularity. Contrast-enhanced abdominal CT images from patients with malignancies involving the liver who were undergoing surgical evaluation at the City of Hope Helford Hospital (Duarte, CA) between 2009-2015 were initially reviewed by experienced academic radiologists. All initial images had been obtained as part of routine care. Of the studies from 128 patients, only 38 were done with multiphase protocols including both arterial and venous phases. Images were reconstructed into 0.625 x 1.25 mm slices for post-processing, and uploaded to General Electric (GE) Advanced Workstation (AW) Server 3.2 for analysis.
3D MIP images were generated by merging arterial and venous phase images with a “drag and drop” tool. 2D images were registered using non-rigid automatic registration. Studies with limited MIP clarity due to motion artifact and suboptimal contrast enhancement were excluded from further analysis. The Volume Computer Assisted Reading (VCAR) software within the AW Server was used to generate scaled 3D images of the 13 studies that had suitable MIP images.
3D color-enhanced volume rendering was performed using the CT arterial and venous phase images. The images were imported in to GE AW workstation, and quantitative volumetric assessment was performed using the automatic hepatic VCAR tool with manual edits when needed. The hepatic artery, hepatic vein, and portal vein were extracted manually based on Hounsfield unit thresholds, and colored individually. Liver lobes were segmented using the virtual scalpel, and color enhancement was applied.
The MIP and 3D volumetric images for each study was compared based on these criteria (Table 1). A multidisciplinary team including radiologists, oncologists, and surgeons determined six consensus criteria based on the visual characteristics and features deemed most clinically useful for preoperative planning. The criteria reflected how both imaging modalities could provide information regarding vascular anatomy, volume quantification, and lobe segmentation. All images were reviewed by two experienced radiologists. MIP and 3D VR images were compared for each individual study, and scored by the radiologists based on which modality had better clarity. All scores were averaged and qualitatively summarized in Table 2.
Table 1.
Criteria used to compare MIP and 3D VR imaging modalities.
| Colorization | Ability to highlight structures and vessels with different colors |
| Volume calculation | Ability to calculate volume of structures within the liver, including parenchyma and blood vessels |
| Rotation | Ability to manipulate images to view additional angles and perspectives |
| Vessel delineation | Ability to distinguish overlapping vessels |
| Small vessel clarity | Ability to visualize small capillaries |
| Segmental liver isolation | Ability to separate target regions from surrounding tissue |
Table 2.
Comparison of MIP and 3D VR techniques*.
| Colorization | -- | +++ |
| Volume calculation | -- | +++ |
| Rotation | +++ | +++ |
| Vessel delineation | + | +++ |
| Small vessel clarity | ++ | ++ |
| Segmental liver isolation | -- | +++ |
| Overall performance | ++ | +++ |
(--) Unable to perform technique
(+) Able to use technique in < 25% of images
(++) Able to use technique in 25-50% of images
(+++) Able to use technique in > 90% of images
3. RESULTS
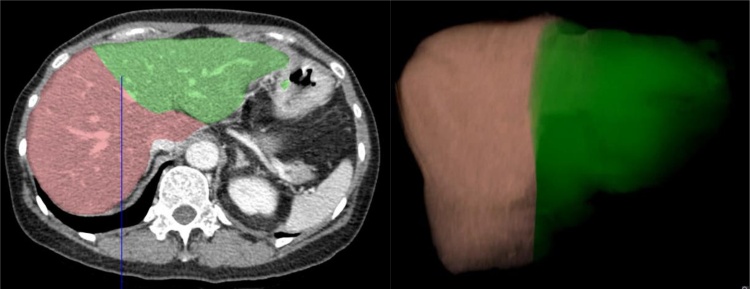
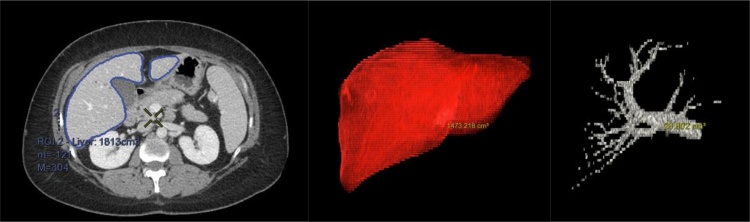
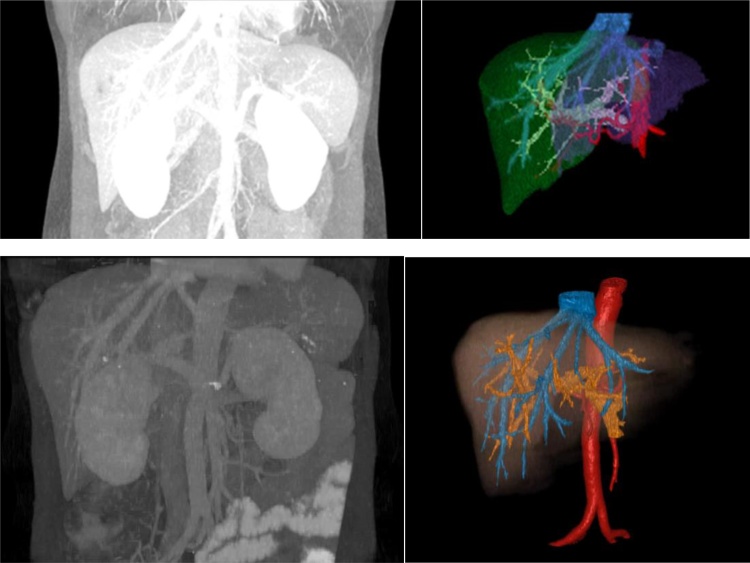
The performance of MIP and 3D VR in several areas was compared. In 3D volume rendered images, anatomic structures were isolated and enhanced with color using the AW Server platform (Fig. 1, Fig. 2). Analysis of individual pixels could be performed with 3D VR images but not MIP images. Voxel analysis allowed volumetric analysis of individual liver segments (Fig. 3) which can be highlighted and isolated. Both 3D VR and MIP images supported quantification of not only the total liver volume, but also the volume of individual structures (Fig. 4).
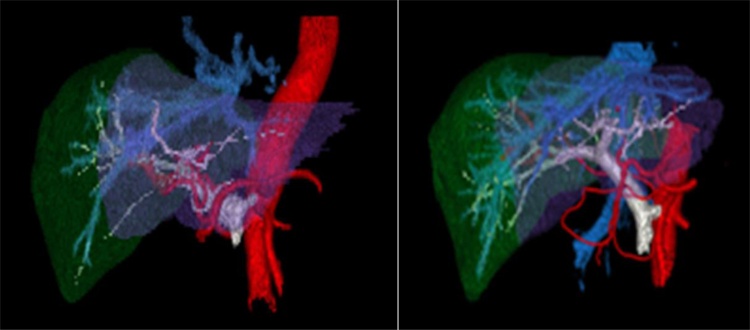
Fig. 1.
Color-enhanced 3D VR images of the liver in two patients with hepatic malignancy.
Red, hepatic arteries arising from the aorta; blue, hepatic veins leading to the inferior vena cava; grey, portal venous system; green, right lobe liver parenchyma; purple, left lobe liver parenchyma.
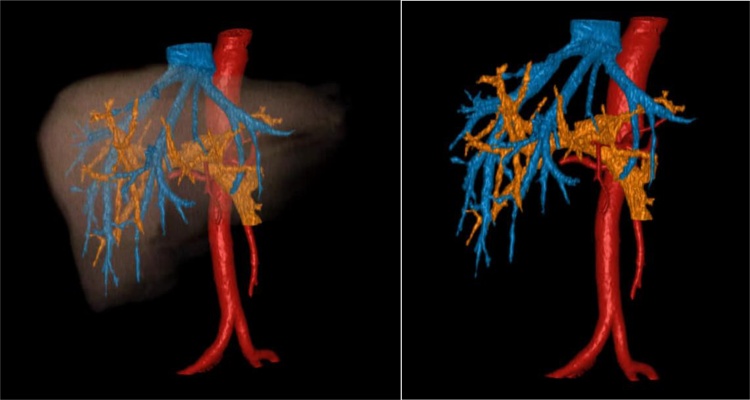
Fig. 2.
Color-enhanced 3D VR images of the liver in a patient with hepatic malignancy (A), with isolation of vascular structures (B).
Red, hepatic arteries arising from the aorta; blue, hepatic veins leading to the inferior vena cava; orange, portal venous system; brown, liver parenchyma
Fig. 3.
Color-enhanced 3D VR images of the liver highlighting individual segments. (A and B) Liver sectioned into right and left lobes.
Fig. 4.
Volume calculation on 3D VR images.
The liver is defined as the region of interest (a), and the VCAR software extrapolates the defined region to additional CT slices. The VR Compare application can then calculate the volume of the entire liver (b) or an individual structure such as the portal vein (c).
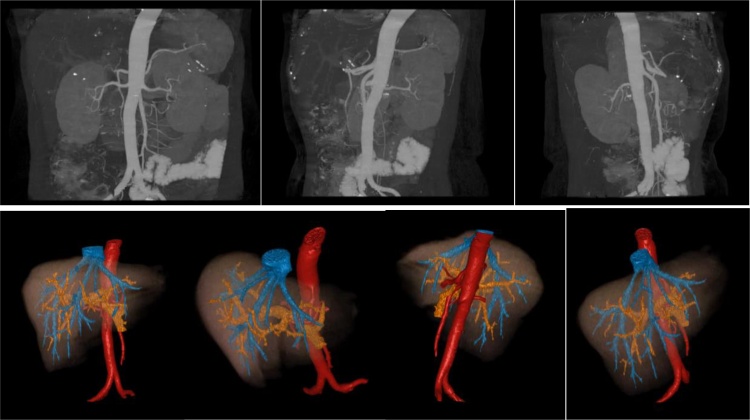
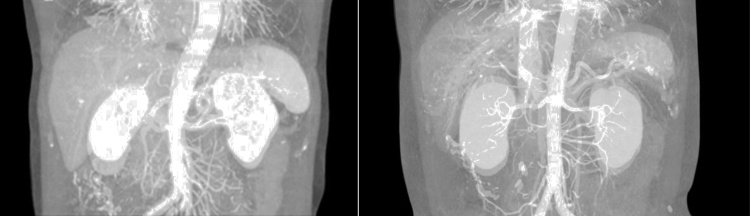
The monochromatic MIP images could not be enhanced with color. Because individual regions of interest could not be highlighted and isolated from surrounding structures, volume calculation was not feasible. Both MIP and 3D VR images could be rotated and manipulated to view structures from multiple perspectives (Fig. 5), though structures in rotated views were visualized more clearly with 3D VR. Overlapping blood vessels were more readily distinguished using 3D VR compared to MIP (Fig. 6). Smaller blood vessels were readily visualized using both modalities. A summary of overall performance is provided in Table 2.
Fig. 5.
Rotation of MIP (top) and 3D VR (bottom) images.
Fig. 6.
Comparison MIP and 3D VR images from two patients with hepatic malignancy.
(a,c) The borders of the overlapping portal and hepatic vessels are the same intensity in the monochromatic MIP image, but smaller vessels can be clearly visualized. (b,d) The overlapping hepatic and portal veins and their branches can be delineated on the color-enhanced 3D VR image.
Overall, color enhancement could only be applied with 3D VR imaging and not MIP imaging. Volume calculation and isolation of liver segments were also possible with 3D VR but not MIP imaging. Image rotation in the superior to inferior, the anterior to posterior, and the lateral view was achieved with both modalities. Vessel delineation was better visualized with 3D VR imaging. The clarity of individual small vessels was suitable with both modalities. The overall performance shows that 3D VR is more superior methodology to delineate the anatomical features compare to the MIP.
4. DISCUSSION
Imaging is an essential component of the preoperative evaluation. MRI has high soft-tissue resolution and can detect hepatic lesions without radiation exposure. However, it is limited by slow scanning speed, and motion artifact [5]. Multiphase CT is routinely used in diagnosis, preoperative planning, and treatment monitoring for hepatic malignancy. Two-dimensional CT and MRI used to detect hepatic tumors underrepresent 25-30% of cases [5]. Three-dimensional or perfusion imaging techniques may provide additional information with increased accuracy in the clinical setting.
MIP creates a 3D perspective by projecting images onto a viewing plane while preserving attenuation information. While it is useful in visualizing simple anatomic structures, it lacks the ability to depict spatial depth and differentiate superimposed structures. On arterial phase-dominant images, venous structures can appear more posteriorly than they actually are in relation to arterial structures [9]. MIP is limited by motion artifact from vessel pulsation and respiration, which also rendered many of our initial images for this study inadequate (Fig. 7).
Fig. 7.
MIP images from two patients showing motion artifact.
3D volume rendering is a useful technique for tumor staging and surgical mapping. As this study illustrates, individual structures can be highlighted and quantified on 3D volume rendered images. However, 3D VR requires manual editing individual CT slices to ensure accurate isolation of the region or structure of interest. This time-consuming task can be a barrier to routine utilization. Automating this process is an evolving area of research that make 3D imaging more efficient and readily available [11].
The application of quantitative 3D color mapping can increase the sensitivity and diagnostic performance of multiphase CT [12]. Recent studies suggest quantitative perfusion analysis also increases the sensitivity and specificity of CT for detection and anatomic delineation of hepatocellular carcinoma [13]. There is no added radiation exposure with post processing 3D VR, and its application can offer greater anatomic visualization at the cost of the computer software [10].
5. CONCLUSION
In conclusion, both 3D volume rendering and maximum intensity projection are useful imaging modalities for visualizing complex anatomy, but 3D VR provides additional features absent from MIP. 3D VR outperformed MIP in its ability to isolate individual structures with color enhancement and calculate the volume of defined regions of interest. Image rotation and small vessel clarity was adequate with both modalities.
3D VR has broad applications in the identification of imaging biomarkers such as perfusion, textural analysis, and density variations. Integration of artificial intelligence with advance imaging can increase its efficiency. While MIP is also useful for quickly generated images, the additional features of 3D imaging such as color enhancement and volumetric analysis make it more widely applicable for precise anatomic reconstruction. The quality of images generated by both modalities are influenced by contrast quality and software capabilities, which should be optimized for high quality images. Further developments in the field of advanced 3D imaging can have profound clinical implications on surgical planning and tumor mapping.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Piccoli G., Smania S., Toso F., Borghese L., Pozzi Mucelli R., Vergendo M. Multislice CT anatomy of hepatic artery in patients undergoing liver transplantation using 3D reconstructions. Radiol Med. 2004;108(4):372–379. [PubMed] [Google Scholar]
- 2.Collaboration GBoDLC. The Burden of Primary Liver Cancer and Underlying Etiologies From 1990 to 2015 at the Global, Regional, and National Level: Results From the Global Burden of Disease Study 2015. JAMA Oncology. 2017;3(12):1683–1691. doi: 10.1001/jamaoncol.2017.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ananthakrishnan A., Gogineni V., Saeian K. Epidemiology of primary and secondary liver cancers. Seminars in interventional radiology. 2006;23(1):47–63. doi: 10.1055/s-2006-939841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brodt P. Role of the Microenvironment in Liver Metastasis: From Pre- to Prometastatic Niches. Clinical Cancer Research. 2016;22(24):5971–5982. doi: 10.1158/1078-0432.CCR-16-0460. [DOI] [PubMed] [Google Scholar]
- 5.Li X.-H., Liang Q., Chen T.-W., Wang J., Zhang X.-M. Diagnostic value of imaging examinations in patients with primary hepatocellular carcinoma. World journal of clinical cases. 2018;6(9):242–248. doi: 10.12998/wjcc.v6.i9.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nowicki T.K., Markiet K., Szurowska E. Diagnostic Imaging of Hepatocellular Carcinoma - A Pictorial Essay. Current medical imaging reviews. 2017;13(2):140–153. doi: 10.2174/1573405612666160720123748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coşkun M., Kayahan E.M., Ozbek O., Cakir B., Dalgiç A., Haberal M. Imaging of hepatic arterial anatomy for depicting vascular variations in living related liver transplant donor candidates with multidetector computed tomography: comparison with conventional angiography. Transplant Proc. 2005;37(2):1070–1073. doi: 10.1016/j.transproceed.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Prokop M., Shin H.O., Schanz A., Schaefer-Prokop C.M. Use of maximum intensity projections in CT angiography: a basic review. RadioGraphics. 1997;17(2):433–451. doi: 10.1148/radiographics.17.2.9084083. [DOI] [PubMed] [Google Scholar]
- 9.Fishman E.K., Ney D.R., Heath D.G., Corl F.M., Horton K.M., Johnson P.T. Volume Rendering versus Maximum Intensity Projection in CT Angiography: What Works Best, When, and Why. RadioGraphics. 2006;26(3):905–922. doi: 10.1148/rg.263055186. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun P.S., Kuszyk B.S., Heath D.G., Carley J.C., Fishman E.K. Three-dimensional Volume Rendering of Spiral CT Data: Theory and Method. RadioGraphics. 1999;19(3):745–764. doi: 10.1148/radiographics.19.3.g99ma14745. [DOI] [PubMed] [Google Scholar]
- 11.Gao L., Heath D.G., Kuszyk B.S., Fishman E.K. Automatic liver segmentation technique for three-dimensional visualization of CT data. Radiology. 1996;201(2):359–364. doi: 10.1148/radiology.201.2.8888223. [DOI] [PubMed] [Google Scholar]
- 12.Kim K.W., Lee J.M., Klotz E., Park H.S., Lee D.H., Kim J.Y. Quantitative CT Color Mapping of the Arterial Enhancement Fraction of the Liver to Detect Hepatocellular Carcinoma. Radiology. 2009;250(2):425–4s34. doi: 10.1148/radiol.2501072196. [DOI] [PubMed] [Google Scholar]
- 13.Fischer M.A., Kartalis N., Grigoriadis A., Loizou L., Stål P., Leidner B. Perfusion computed tomography for detection of hepatocellular carcinoma in patients with liver cirrhosis. European Radiology. 2015;25(11):3123–3132. doi: 10.1007/s00330-015-3732-1. [DOI] [PubMed] [Google Scholar]