Abstract
The coronavirus disease (COVID-19) affected virtually all countries. Uncertain about the health risk and an increasing financial loss will contribute to widespread emotional distress and an increased risk of psychiatric disorders shortly. Posttraumatic, anxiety, and depression disorders are expected during and aftermath of the pandemic. Some groups, like children, have more susceptibility to having long term consequences in mental health. Herein, we made a comprehensive and non-systematic search in four databases (PubMed, Scopus, SciELO, and Google Scholars) to answer the question: What are children's and adolescents' mental health effects of the pandemic? Furthermore, which features are essential for mental health in a pandemic? Results: Seventy-seven articles were selected for full text read, and 51 were included. Children answer stress differently, depending on the development stage. High rates of anxiety, depression, and post-traumatic symptoms were identified among children. Discussion: Symptoms were as expected. New supportive strategies have appeared during this pandemic, but there is no measure of its effectiveness. Some groups seem to be more vulnerable to the mental health burden of the COVID-19 pandemic, and the mitigation actions should prioritize them. The school's role appears to be revalued by society. This review seems to pick good targets to prioritize mitigation actions aiming to spare children not only from the severe cases of COVID-19 but also to help them to deal with the mental health burden of the pandemics.
Keywords: Mental health, Pediatric, Children, Adolescent
1. Introduction
The newly identified human infection caused by the new coronavirus, the SARS-CoV-2, is spreading rapidly across the globe, posing a significant threat to the health of the population and creating a significant challenge for health systems. The coronavirus disease 2019 (COVID-19) affected virtually all countries. Unknown diseases with an uncertain prognosis and associated with a scarcity of medical and protective equipment have led to the imposition of measures that restrict individual freedoms. In addition to these factors, an increasing financial loss will contribute to widespread emotional distress and an increased risk of psychiatric disorders shortly [1] (see Fig. 1, Fig. 2 ).
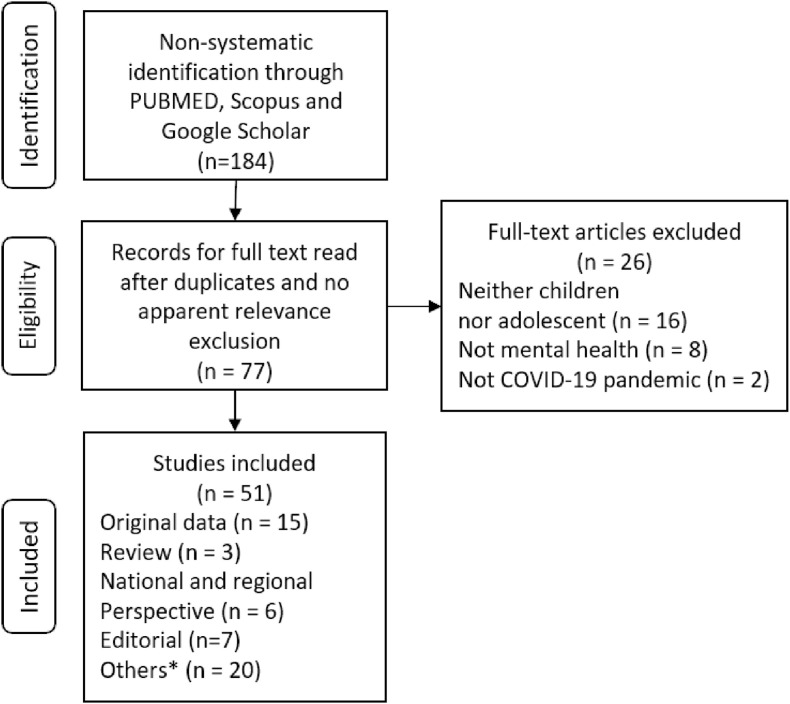
Fig. 1.
Selection of studies flowchart, *Comments, Viewpoints, Position Papers, Letters to the Editor, etc.
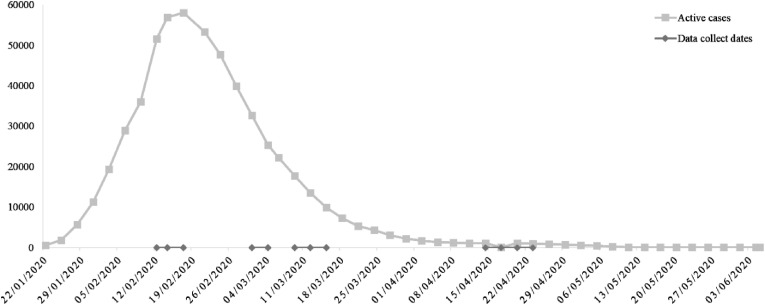
Fig. 2.
Active COVID-19 cases in China from February 22 to June 5, 2020 and surveys dates.
Some groups may be more vulnerable than others to the psychosocial effects of pandemics. Because they are in a critical period of development, children and adolescents deserve special care to preserve and promote their mental health. The history of this pandemic has experienced unparalleled changes in recent world history. Among them, the drastic modification of children's routines. They suppressed the classes at learning and moved all children activities for home. Classes have been routinely offered by distance education systems or even by television stations [2], or simply suppressed.
Physical exercise has been reduced or suppressed. The presence of parents and children's involvement in home activities helps in the child's routine and autonomy. However, isolation imposes more significant contact between parents and children, consisting on opportunities for play and friction [3]. Not all homes are safe places, and some children might be more exposed to varied types of abuses. Although screen time can be relaxed in this quarantine period, the lack of supervision over internet access increases vulnerability to online offenders, attempted fraud, and access to sexually inappropriate content [4]. Adolescents may feel frustrated with events and encounters that they have not experienced or at least postponed. Problems such as worsening school performance, increased agitation, aggression, and regression may arise or become more pronounced [5].
In this scenario, the study of mental status becomes even more critical since the impact of the environment that favors or impairs the child's mental health conditions can be modified by several initiatives. In this study, we review the literature about: How is the Mental Health of Children and adolescents during the COVID-19 pandemic? Furthermore, which features are essential for mental health in a pandemic?
2. Methods
Data was obtained independently by two authors, who carried out a comprehensive and non-systematic search in PubMed, Scopus, SciELO, and Google Scholars databases. Search strategies included Medical Subject Heading terms as: "COVID-19", "SARS-CoV-2", "mental health", "children", "depression", "anxiety", and "adolescent". The search emphasized recent articles, consensus statements, guidelines, and prospective cohort studies, critically reviewed and selected by the authors. Research has also been done in an informative official website public domain and the references contained in the previous data collected.
The choice for a non-systematic review was associated with the circumstances: our search was carried out in an early phase of the pandemic, when much fewer original data addressing pediatric mental health during the COVID-19 pandemic was available. In fact, our findings in the literature were as few as they were heterogeneous: mental health assessment criteria, age ranges, signs and symptoms screened, among other aspects analyzed. Besides, some of the original data obtained were not published as original articles, but as research letters and even editorials. Therefore, it was not possible to conduct a formal systematic review and meta-analysis. Despite that, we have constructed tables that allow comparison and analysis of collected data.
Seventy-seven articles were selected for full text read, and 51 were included. Fifteen of the selected articles presented original data from surveys, cross-sectional and longitudinal studies, and included editorials [6], research letters [7], and original papers. Most articles were from China (n = 11). The review also included articles from the United States of America (n = 2), Europe (n = 1), and South America (n = 1). Most of the original papers were cross-sectional studies. We have found only one longitudinal study [8].
Although all the studies included addressed mental health during the COVID-19 pandemic, they differed in several aspects including aim, age range of the sample, control groups, and mental health assessment criteria. Age ranges of the samples analyzed varied throughout studies. Six studies also included adults [6,[8], [9], [10], [11], [12]] (adults' data were only used for comparison) and nine original studies included only the pediatric population [7,[13], [14], [15], [16], [17], [18], [19], [20]].
Pediatric population encompassed both children and adolescents, however there was no consistency between studies in providing a milestone in years for the end of childhood and the beginning of adolescence. The classification given by the original articles was respected in this review: children age range were 6–15 years old and adolescents, 12–21 years old. The overlap of children and adolescent age ranges is due to that inconsistency. Also, when school grades were provided instead of age, the correspondent age in years was considered for comparison matters [7,19].
The remaining selected papers were editorials, letters to the editor, commentary, and literature addressing mental health concerns and solutions during and after the pandemic, such as commentary, letters to the editor, and position papers, although did not contain original research data on children's mental health during the pandemic.
3. Results
The mental health state was assessed in several different ways in the selected studies. Most of the included studies (n = 10) have utilized the detection of anxiety and depression symptoms as a benchmark for mental health and screened it through different diagnostic criteria [[7], [8], [9], [10], [11], [12], [13], [14], [15], [16]]. Table 1 shows the data found on the frequency of anxiety and depression symptoms in children and adolescents.
Table 1.
Depression and anxiety prevalence in children and adolescents.
| Authors | Country of origin | Data collect date | Sample size | Ages (years) |
Anxiety Symptoms |
Depression Symptoms |
||
|---|---|---|---|---|---|---|---|---|
| Criteria | Presence | Criteria | Presence | |||||
| M. Z. Ahmed et al. | China | 02/12/20–02/18/20 | 62a | 14–20 | BAI | 12,90% | BDI | 27,30% |
| X. Xie et al. | China | 02/28/20–03/05/20 | 2330 | 7–11b | SCARED | 18.9% | CDI-S | 22.6% |
| S.-J. Zhou et al. | China | 03/08/20–03/15/20 | 8079 | 12–18 | GAD-7 | 37,40% | PHQ-9 | 43,70% |
| F. Chen et al. | China | 04/14/20–04/23/20 | 1036 | 6–15 | SCARED | 18,92% | DSRS-C | 11.78% |
| C. M. Rios-González et al. | Paraguay | 03/17/20–03//20/20 | 92* | 18–19 | EADG | 46.74% | EADG | 47.83% |
Study included adults. Only data regarding the sample of interest were included.
Students in grades 2 through 6, BAI beck anxiety inventory, BDI beck depression inventory, CDI-S children's depression inventory–short form, DSRS-C depression self-rating scale for children, EADG goldberg anxiety and depression, GAD-7 generalized anxiety disorder, PHQ-9 patient health questionnaire, SCARED screen.
Three studies assessed the presence of Post-Traumatic Stress Symptoms (PTSS) [[8], [9], [10]] through different Post-Traumatic Stress scales: IES-R (Impact Event Scale revised) [8,10] and Post Traumatic Stress Disorder Checklist-Civilian Version (PLC-C) [9]. Some studies have measured mental health conditions, including the General Health Questionnaire - 12 (GHQ -12) [9]; or the COVID-19 Peritraumatic Distress Index (CPDI), that inquires "about the frequency of anxiety, depression, specific phobias, cognitive change, avoidance, and compulsive behavior, physical symptoms and loss of social functioning" [14]. Other mental health scale utilized were stress levels, through the Stress Subscale from Depression, Anxiety and Stress Scale (DASS-21) [8] and Coping Styles, that were measured by the Simplified Coping Style Questionnaire (SCSQ) [9].
Feelings and subjective impressions were assessed, such as changes in behavior [17,18]; and feelings of belongingness and burdensomeness [13,14]. In these studies, researchers have asked participants' thoughts about themselves [13,14] or their caregivers to report about them [17,18].
To understand and to analyze the effect of pandemic on pediatric mental health, most studies compared symptoms rates from children and adults during the pandemic [6,[8], [9], [10], [11], [12]]. A single study that included only children and adolescents comparing their results with data from previous systematic reviews and meta-analysis [15]. Two studies compared depressive and anxiety symptoms according to parameters such as engagement in social distancing [13] and prosocial experiences [14].
Most of included studies have highlighted the fact that the way the pandemic affects mental health depends on protective and risk factors that must be considered and assessed. Therefore, we have decided to address these variables in this review to allow a more profound and specific analysis.
3.1. Age
Age was an important variable in several studies to analyze mental health. In different researches, children's and adolescents' mental health were compared to adults' mental health.
Four studies [6,8,10,11] found that adolescents are generally less depressed and stressed than adults, although results are similar for depression when compared with the ≥50 years-old groups [11]. Results for anxiety differ, as two studies [6,11] show that the ≤20 years old group is less anxious, while according to two others [8,10], the 12 to 21,4 years-old group was the most anxious. Another study showed that the 14 to 20 years-old group had the highest tendency toward psychological problems in a comparison upon the 21 to 35 years-old group [9].
Depression and anxiety occurrence throughout different childhood and adolescence phases were available in three different studies, as shown in Table 3. Three papers [7,15,16] showed that older adolescents exhibit more depressive symptoms than younger ones and children. However, the analysis came to different conclusions when it comes to anxiety: while two studies [7,16] showed no significant difference between ages (even though it was higher in the older ones), one [15] reported higher anxiety with the increase of age. A single study compared primary school and college students, and it reported more depressive, anxiety, and somatic symptoms among college students [19].
Table 3.
Depression and anxiety prevalence throughout different childhood and adolescence genders.
| Author | Age (years) | Depression |
Anxiety |
||||
|---|---|---|---|---|---|---|---|
| Criteria | Male (%) | Female (%) | Criteria | Male (%) | Female (%) | ||
| S.-J. Zhou et al., 2020 | 12–18 | PHQ-9 | 41,7 | 45,50 | GAD-7 | 36,20 | 38,40 |
| F. Chen et al., 2020 | 6–15 | DSRS-C | 9,04 | 14,65 | SCARED | 15,82 | 22,18 |
| X. Xie et al., 2020 | 7–11a | CDI-S | 22,5 | 22,70 | SCARED | 18,40 | 19,60 |
Students in grades 2 through 6, PHQ-9 patient health questionnaire, CDI-S children's depression inventory–short form, DSRS-C depression self-rating scale for children, GAD-7 generalized anxiety disorder, PHQ-9 patient health questionnaire, SCARED screen for child anxiety related disorders.
As mentioned, not only anxiety and depression were used to describe mental health among children and adolescents. A children specific study [18] showed that all age groups (3-18 year-olds) showed more clinging, inattention, and irritability. However, 3-6 year-olds children were more likely to manifest clinginess and fear that family members might contract the infection, while 6-18 year-olds were more likely to show inattention and persistent inquiry.
Studies do not identify if the pandemic results in Post-Traumatic stress symptoms mean a presence of functional compromise. Adolescents (12–21.4 years-olds) showed higher scores in comparison to older groups in one study [10] and no statistical difference in another study [9].
3.2. Gender
Gender was an essential factor in the analysis of the general mental health state during the pandemic. Regarding the original papers that included only the pediatric population, studies with both children and adolescents show that adolescent girls are more likely to present anxiety and depressive symptoms [15,16]. However, a study with children between 7 and 11 years old showed no differences in those subjects [7] (Table 2 ).
Table 2.
Depression and anxiety prevalence throughout different childhood and adolescence ages.
| Age (years) | Author |
X. Xie et al., 2020 |
S.-J. Zhou et al., 2020 |
F. Chen et al., 2020 |
|||
|---|---|---|---|---|---|---|---|
|
Illness |
Depression |
Anxiety |
Depression |
Anxiety |
Depression |
Anxiety |
|
| Criteria | CDI-S | SCARED | PHQ-9 | GAD-7 | DSRS-C | SCARED | |
| 6–7 | NS | NS | NS | NS | 3.21% | 12.54% | |
| 7–8 | 13.7% | 18.8% | NS | NS | |||
| 8–9 | 21.0% | 18.8% | NS | NS | |||
| 9–10 | 24.1% | 19.0% | NS | NS | 9.68% | 20.32% | |
| 10–11 | 23.2% | 19.1% | NS | NS | |||
| 11–12 | 30.7% | 18.8% | NS | NS | |||
| 12–13 | NS | NS | 32.0% | 28.3% | |||
| 13–14 | NS | NS | 36.5% | 33.6% | 21.15% | 23.50% | |
| 14–15 | NS | NS | 45.8% | 39.3% | |||
| 15–16 | NS | NS | 45.0% | 36.1% | |||
| 16–17 | NS | NS | 49.7% | 41.0% | NS | NS | |
| 17–18 | NS | NS | 59.9% | 53.2% | NS | NS | |
CDI-S children's depression inventory–short form, DSRS-C depression self-rating scale for children, GAD-7 generalized anxiety disorder, NS not studied, PHQ-9 patient health questionnaire, SCARED screen for child anxiety related disorders.
Nonetheless, results from studies that included both adolescents and adults presented several differences. Regarding depression, anxiety, and stress, two studies [10,14] found that women are more likely to exhibit symptoms, while two other studies suggest the opposite [8,9]. Results also differ in what concerns PTSS, as one study states a lower risk for males [8] and another does otherwise [9]. One study [11] did not find interactions between gender with anxiety or depression.
3.3. Metropolitan areas and interior
Anxiety [12,15] and depression [15] were found lower in metropolitan areas compared to rural regions. Children in highly epidemic areas scored more fear, anxiety, and other emotions [18].
3.4. School closure, physical, and mental health
School closure influences children and adolescents' behavior in various ways. Several articles expressed concerns about food nutrition and physical activity for children and adolescents. Different articles argued that schools are the primary source of consistent daily caloric intake and addressed concerns about children's nutritional needs [2,[21], [22], [23], [24], [25], [26]].
School activities are also responsible for providing structure and routine to children and adolescents' daily lives, and their interruption and its consequences concern several authors [[27], [28], [29], [30]], especially when the subjects are ADHD patients [27,28]. On the other hand, ADHD children's parents from Ireland reported an improvement in their children's behavior and mood since schools had closed [28].
Additionally, many articles postulated the importance of physical activity [2,30,31] and the maintenance of physical health [32,33] during the quarantine. Not surprisingly, regular physical exercise associated with less depression and anxiety cases [16] and parents considered it the second most effective action to mitigate children's (3-18 years-olds) psychological burden during quarantine [18], only below the effect of media entertainment. Despite that, physical exercise was the less used technique among parents (compared with media and reading entertainment) to mitigate psychological problems during quarantine [18]; and a reduction in youth exercise practice has been reported: only 14,8% of the subjects in the European study practice ≥60min, and before quarantine that percentage reached 54.1% [17].
3.5. Knowledge and expectations about COVID-19
Expectations about the pandemic may impact children's and adolescents' mental health in several ways. Pessimistic perspectives towards the pandemic, fear of being infected or having a relative infected, for instance, might result in behavioral changes [28]. Being optimistic about the pandemic and not worried about being infected resulted in lower depression scores [7,19]. However, finding expectations misplaced or having them frustrated (e.g., quarantine lasting longer than expected) can also lead to anxiety and depression [34].
Access to information and knowledge about COVID-19 is also meaningful when it refers to mental health. Association between knowledge about the pandemic and mental health was found in two studies [10,15]. In these studies, individuals with higher scores of knowledge about COVID-19 [15] or satisfied with the amount of information about the pandemic [10], were less likely to present anxiety, depression and PTSS. A single study [9], however, did not find an association between information and mental health.
3.6. Community and family relationships
Family and community bonds and relationships also play an essential role in mental health outcomes during the pandemic. For many individuals, the presence of a supportive family can be protective against mental distress [26,34]. In contrast, an original study shows that adolescents left alone during workdays were more likely to show depression and anxiety [16].
Relationships with the community, prosocial action, and sense of social responsibility also matter when it deals with mental health. Youths with prosocial behavior reported greater belongingness [14,34], though also more significant anxiety and feelings of burdensomeness [14]. However, those who were recipients of prosocial action [14] reported less anxiety and depressive symptoms.
Social relations and friendships were also found relevant when associating mental health and quarantine motivation among youths. The ones who were social distancing because they prefer to stay home reported less anxiety and depressive symptoms. Those who were in quarantine to avoid judgement or because they did not want to get sick personally presented higher anxiety symptoms, while those who were in quarantine because their friends told them to, higher depressive symptoms [13]. Staying home due to parental command was correlated with greater belongingness [13].
3.7. Screen time
The quarantine has increased the time spent in front of screens [17,18] for many reasons and purposes. Children and adolescents have been using it for learning - due to school closures -, but also for entertainment and social interaction [29]. The selected literature addresses the positive and negative mental health impacts of such an increase.
Two papers [18,29] state that entertainment media has become, for many families, a tool for coping with distress, boredom, and lack of social interaction caused by the pandemic. In that sense, especially for adolescents, social media use can be helpful in protecting mental health, as it allows access to information, social connection, identity development, and self-expression [32].
Despite those benefits, authors have also highlighted their concerns about the increase in screen time due to its potentially harmful effects. Although electronic entertainment poses risks, regardless of the pandemic [32,[34], [35], [36]], we have decided to highlight, in this review, only new potential threats that might arise with the COVID-19 outbreak. Some of those risks are significant exposure to fake news and misinformation about COVID-19, for some youths may not have enough knowledge to assess the accuracy of information [32,34]; disruption in sleep and circadian rhythms, and an increase in anxiety [32].
We have found a single study that presented original data on this subject [16]. It endorses the positive association between the presence of electronic entertainment with depression (16% vs. 9,38%) and anxiety (27,73% vs. 13,92%). The paper, however, does not specify what kind, amount, or frequency of electronic entertainment associate with these disorders.
Included papers also provide guidelines to orient parents and caregivers about screen time management during the pandemic [29,32,37]. The main points brought out are the importance of parents' being a role model for digital media use, as well as negotiating and limiting screen time and contents - especially those that are anxiety-provoking (e.g., COVID-19 media coverage).
3.8. Risk factors and main concerns
Reviewed literature also states that children from specific groups or exposed to some risk factors are more vulnerable to developing mental health disorders during the pandemic. Fragile groups identified were children with preexisting health conditions and in vulnerable socioeconomic contexts. Risk factors were exposure to domestic violence or child maltreatment and infection by COVID-19.
3.8.1. Domestic violence
Many authors were concerned about children suffering or witnessing domestic violence or sexual abuse [21,25,33,[38], [39], [40]]. Some argued that the in-home scenario produced by the pandemic could erupt to those abuses [21,22,26,35,38]. However, during quarantine, complaints might not be as frequent, for there is no escape from perpetrators [26]. Furthermore, school closure exacerbates that problem since school is a safe space where children can report problems and where signs of abuse can be detected [38].
3.8.2. Children with preexisting health conditions
Children and adolescents with preexisting - mostly mental - health disorders may be more susceptible to new mental health conditions during the pandemic [26,28,31,33,[41], [42], [43]] and have specific needs that must be met. So far, a single study found that the history of chronic illness was associated with higher stress, anxiety, depression, and Post-Traumatic Stress Symptoms [10].
One of the main concerns pointed is the risk of deterioration of their condition due to the pandemic [26,28]. Derangement of mental health services, as well as regulations on travels and quarantine, might prevent patients from attending evaluations or group interventions, obtaining prescriptions or medicines [26,28,31,34,42]. Therefore, it is essential to ensure the maintenance of access to those services through telephone or online support [27] and online pharmacies [31].
It is still not yet clear how the COVID-19 pandemic and its consequences - social distancing, school closures, lockdown - will affect psychiatric disorders' features including symptom severity, relapses, need for increased frequency of assistance, and intensity of mental healthcare [41]. Reviewed literature exemplifies mental health outcomes of the pandemic mainly with disorders like PTSD [26,34,44], eating disorders [45], Attention Deficit Hyperactivity Disorder (ADHD), and Autism Spectrum Condition (ASC) [[25], [26], [27], [28],46]. Individuals with PTSD may experience exacerbations of their symptoms in the new crisis scenario [34], while adolescents with eating disorders such as anorexia nervosa may be prevented from getting meal supervision and have their weight control affected [45]. Moreover, children with neurodevelopmental disorders, including Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Condition (ASC) might struggle with the lack of structure and routine caused by the pandemic, what may impact mental health [25,27,28]. In fact, one original study measured children's ADHD behaviors during the COVID-19 outbreak and found them worse compared with their normal state, showing increased irritability and more challenging behaviors. However, children and adolescents that suffer from social anxiety might benefit from the reduction of face to face interactions [25,46]. These findings might support evidence (51) of the effectiveness of telepsychiatry for ADHD and ASC assessment and management, although results in that matter vary [26].
3.8.3. Children infected with COVID-19
Infection with COVID-19 also must be considered a risk factor for mental health disorder among children and adolescents. One of the main reasons for that is that children necessarily face separation from parents and caregivers when isolated. A Chinese paper [31] reported that insomnia and separation anxiety were the most common mental health problems presented by those children. It also highlights the importance of screening for PTSD in patients who show nightmares, avoidance behaviors, heightened reactions, and other symptoms.
3.8.4. Vulnerable socioeconomic condition
The pandemic may have a more substantial impact on the mental health of children and adolescents from lower socioeconomic conditions [21,26,31,38,41,47]. Children from low-income families might rely only on school for healthy meals, mental health support, and playgrounds for physical exercise [22,33]. Therefore, school closures and quarantine prevent children from accessing these services and activities, which may cause a decrease in mental health and general wellbeing. Besides, those children are less likely to have appropriate access to the Internet [33] for remote learning, and interaction with peers, that can be somehow protective of mental health [32].
Additionally, the pandemic leads to an economic recession that brings several consequences, especially for low-income families and their children's health and wellbeing [26,48,49]. Financial distress and unemployment, for instance, increase the chances of child maltreatment [21,22,38].
Despite literature addressing lower socioeconomic conditions as a risk factor for children's mental health during the pandemic, a single original study [14] approached this subject. According to expectations in literature, researchers found that adolescents that come from families in more significant financial difficulties are more likely to show higher depressive symptoms and lower belongingness.
3.9. Online and telephone support
Due to social isolation, loneliness, and income reduction, children and adolescents reported a decrease in mental health in general. Therefore, the need for mental health services increased during the pandemics [22,33]. However, the lack of mental health services during the pandemic has been reported [33,38]. Furthermore, school closure exacerbates this problem, since it is the primary source of mental health service for numerous children and adolescents, as reported in the United States of America [22].
Online and telephone support were the leading solutions reported in the articles for the lack of mental health face-to-face services [38,50,51]. It has been applied in different countries; among the included articles China, Australia, Italy, the USA, Turkey, India, and Nepal applied online or telephone support for children and adolescents [2,26,31,34,47,52,53]. Moreover, the online solution was considered efficient during the pandemic as an emergency matter [21,22,50,54].
4. Discussion
A pandemic might be considered a disaster-like because a disaster consists of the non-routine character that exceeds the local capacity to respond to it, and changes community, government, and in individual support and infrastructure and affecting the region's stability [55]. Besides recruiting many resources from all instances of support, it does not stop other catastrophes from happening, and it even amplifies their effects by the lack of enough response [56]. It is evident in this revision when many modern pediatric problems are maximized, and some new problems and perspectives emerge [57].
In this review, we diagnosed the mental health scenario caused by pandemic and social distancing. As expected, we have a different response to stress in diverse stages of development. However, children from all development phases had high rates of depression, anxiety, and pos-traumatic symptoms as expected in the aftermath of any disaster [[7], [8], [9], [10], [11], [12], [13], [14], [15], [16],58]. The mental health evaluation was retrieved in different moments of the infective curve in the different studies (Table 1), which might reflect differences in knowledge about the disease and social disorganization or social distancing. Children are highly affected by family and community conditions, such as family stress, conflict related to finances, parental psychopathology and their practices [[59], [60], [61], [62]]. The ideal is to evaluate the data following the timing and intensity of social distancing measures and time from the beginning of the local epidemic. New features including social distancing and the disruptive role over face-to-face social relationships were not directly approached. Like any natural disaster, the effects are of cumulative stress and dependent on individual susceptibility to stressful events [63]. The interaction of individuals and the environment should be better explored to be individually understood about the potential impacts.
The study at the point of this review consists of preliminary evidence; however, some points might be highlighted to reinforce children's mental health. There is a need for social support and early psychological and psychiatric assistance for children, parents, and caregivers feeling distressed during these pandemics. When possible open-air physical activities should be kept to preserve mental health. Daily routine and the more rigorous time to go to bed might help with the organization. Social media and online games might be a useful tool to allow some socialization with peers. As a society, we must be aware of the vulnerabilities to minimize their effects, especially poverty, food insecurity, and domestic violence risks.
The new technological devices and strategies come as "the possibility for the moment" for school settings, health access, or entertainment, but there are very few initiatives up to the moment to understand the related effects and quality of these strategies. Homeschooling was never tried in too many diverse scenarios, and it recruits more presence and organization from the parents. There is a clear need to understand if it is more a burden for families or if it works as an organizing strategy not only for kids but also for parents. The side effects of homeschooling and of the cumulative use of screens must be addressed. The kind of screen used, for how long, the content watched, and its potential to change sleep patterns and disrupt the routine, and mental health are also features important to know not only to apply knowledge in disasters events but also as worldwide events that might enlight the psychopathological role of screens use.
In China, children quarantined could communicate with their parents via mobile devices, and in lack of them, someone from the local community assumed the childcare until their parents would recover from infection [24]. Some countries open 24-h, telemental health services for psychological counseling. As an attempt to provide children daily needs, psychological counseling has been considered a measure that can minimize the short- and long-term impacts of the pandemics [24]. Telehealth assistance has been used as a strategy to promote health care access, especially in remote places. However, nowadays, it has gained scale and must be evaluated for its effectiveness. During the pandemics, only emergency situations have been addressed. In the aftermath of a disaster, the implementation of a supportive network and trained pediatricians in screening for mental health problems might improve the early identification and referral of children and adolescents to proper interventions [64]. The use of standardized screening tools for mental health might make the process easier, while mental health professionals should make available evidence-based guidelines for parents to improve coping with mental health problems in children [64]. In the aftermath, the offer of quick access to children and families for treatments that might mitigate the long-term effects on mental health disorders related to pandemics is of utmost importance [64].
The school has emerged in studies as a structure able to keep routine habits including nutrition [2,[21], [22], [23], [24],26], daily activities [[27], [28], [29], [30]] and even avoiding mortality [65]. It should be mentioned that teaching academic knowledge for children and adolescents seems to be a successful measure in keeping health professionals working and in avoiding unnecessary deaths [65]. The importance of schools has been revalued by societies. In the time to return to regular activities, schools will have an important structural role again. The intense participation of parents in homeschooling scenarios might result in changes in parental involvement with school activities.
We are aware that several important points regarding children and adolescent's mental health during pandemics remains to be further investigated. Important issues as age, gender, school attendance and emotional repercussions of the pandemics have been investigated. However, the designs of the studies, up to now, are not so robust, thus precluding definitive conclusions. Nevertheless, our study summarizes important and available data on children and adolescents' mental health during COVID-19 pandemic. We also discuss the impact of the school activities, even in a remote way, in this scenario.
In conclusion, mental health is a critical concern in a pandemic's scenario. Children and adolescents are considered a vulnerable subgroup and there is a need to reduce the mental health burden of this pandemic.
Funding
We acknowledge the public governmental research agencies which funded the research (CAPES, CNPQ and FAPEMIG).
Dark gray represents the dates the online surveys were available, respectively: M. Z. Ahmed et al. [11], X. Xie et al. [7], S.-J. Zhou et al. [15], and F. Chen et al. [16].
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2008017. NEJMp.2008017. [DOI] [PubMed] [Google Scholar]
- 2.Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Europol . 2020. Catching the Virus Cybercrime, Disinformation and the COVID-19 Pandemic. [Google Scholar]
- 5.Mohammadinia L., Ardalan A., Khorasani-Zavareh D., Ebadi A., Malekafzali H., Fazel M. Domains and indicators of resilient children in natural disasters: a systematic literature review. Int. J. Prev. Med. 2018;9:54. doi: 10.4103/ijpvm.IJPVM_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33:19–21. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xinyan X., Qi X., Yu Z., Qi L., Jiajia Z., Ranran S. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in hubei province, China. Jama Pediatrics. 2020;7:2–4. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. 2020. A Longitudinal Study on the Mental Health of General Population during the COVID-19 Epidemic in China, Brain, Behavior, and Immunity. 0–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020 doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian Journal of Psychiatry. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rios-González C.M., Palacios J.M. 2020. Symptoms of Anxiety and Depression during the Outbreak of COVID-19 in Paraguay. [Google Scholar]
- 13.Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents' motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J. Adolesc. Health. 2020 doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvis L., Douglas R., Shook N.J., Oosterhoff B. 2020. Adolescents' Prosocial Experiences during the COVID-19 Pandemic: Associations with Mental Health and Community Attachments Lauren, PROSOCIAL BEHAVIOR and ADOLESCENT HEALTH. [DOI] [Google Scholar]
- 15.Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatr. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. 2020. Depression and Anxiety Among Adolescents during COVID-19: A Cross-Sectional Study, Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orgilés M., Morales A., Delveccio E., Mazzeschi C., Espada J.P. 2018. Immediate Psychological Effects of the COVID-19 Quarantine in Youth from Italy and Spain. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020;221 doi: 10.1016/j.jpeds.2020.03.013. 264-266.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatr. Res. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., Cao X., Xia W., Wang Y., Chen R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian Journal of Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Witt A., Ordóñez A., Martin A., Vitiello B., Fegert J.M. Child and adolescent mental health service provision and research during the Covid-19 pandemic: challenges, opportunities, and a call for submissions. Child Adolesc. Psychiatr. Ment. Health. 2020;14:19. doi: 10.1186/s13034-020-00324-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 23.Thakur K., Kumar N., Sharma N. Effect of the pandemic and lockdown on mental health of children. Indian J. Pediatr. 2020 doi: 10.1007/s12098-020-03308-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. The Lancet Child & Adolescent Health. 2020;4:347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wright B., Spikins P., Pearson H. Should autism Spectrum conditions Be characterised in a more positive way in our modern world? Medicina. 2020;56:233. doi: 10.3390/medicina56050233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chatterjee S.S., Barikar C M., Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian Journal of Psychiatry. 2020;51:102071. doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cortese S., Asherson P., Sonuga-Barke E., Banaschewski T., Brandeis D., Buitelaar J., Coghill D., Daley D., Danckaerts M., Dittmann R.W., Doepfner M., Ferrin M., Hollis C., Holtmann M., Konofal E., Lecendreux M., Santosh P., Rothenberger A., Soutullo C., Steinhausen H.C., Taylor E., van der Oord S., Wong I., Zuddas A., Simonoff E. ADHD management during the COVID-19 pandemic: guidance from the European ADHD Guidelines Group. The Lancet Child and Adolescent Health. 2020;4642:412–414. doi: 10.1016/S2352-4642(20)30110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee J. Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vanderloo L.M., Carsley S., Aglipay M., Cost K.T., Maguire J., Birken C.S. Applying harm reduction principles to address screen time in young children amidst the COVID-19 pandemic. J. Dev. Behav. Pediatr. 2020;41:335–336. doi: 10.1097/dbp.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 30.Lambrese J.v. Helping children cope with the COVID-19 pandemic. Cleve. Clin. J. Med. 2020:13. doi: 10.3949/ccjm.87a.ccc010. [DOI] [PubMed] [Google Scholar]
- 31.Cui Y., Li Y., Zheng Y. Mental health services for children in China during the COVID-19 pandemic: results of an expert-based national survey among child and adolescent psychiatric hospitals. Eur. Child Adolesc. Psychiatr. 2020;29:743–748. doi: 10.1007/s00787-020-01548-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamilton J.L., Nesi J., Choukas-Bradley S. 2020. Teens and Social Media during the COVID-19 Pandemic: Staying Socially Connected while Physically Distant. [Google Scholar]
- 33.Crawley E., Loades M., Feder G., Logan S., Redwood S., Macleod J. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatrics Open. 2020;4 doi: 10.1136/bmjpo-2020-000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharma V., Reina Ortiz M., Sharma N. Risk and protective factors for adolescent and young adult mental health within the context of COVID-19: a perspective from Nepal. J. Adolesc. Health. 2020;67:135–137. doi: 10.1016/j.jadohealth.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poitras V.J., Gray C.E., Janssen X., Aubert S., Carson V., Faulkner G., Goldfield G.S., Reilly J.J., Sampson M., Tremblay M.S. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0–4 years) BMC Publ. Health. 2017;17:868. doi: 10.1186/s12889-017-4849-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radesky J.S., Schumacher J., Zuckerman B. Mobile and interactive media use by young children: the good, the bad, and the unknown. Pediatrics. 2015;135:1–3. doi: 10.1542/peds.2014-2251. [DOI] [PubMed] [Google Scholar]
- 37.Király O., Potenza M.N., Stein D.J., King D.L., Hodgins D.C., Saunders J.B., Griffiths M.D., Gjoneska B., Billieux J., Brand M., Abbott M.W., Chamberlain S.R., Corazza O., Burkauskas J., Sales C.M.D., Montag C., Lochner C., Grünblatt E., Wegmann E., Martinotti G., Lee H.K., Rumpf H.-J., Castro-Calvo J., Rahimi-Movaghar A., Higuchi S., Menchon J.M., Zohar J., Pellegrini L., Walitza S., Fineberg N.A., Demetrovics Z. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr. Psychiatr. 2020;100:152180. doi: 10.1016/j.comppsych.2020.152180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clemens V., Deschamps P., Fegert J.M., Anagnostopoulos D., Bailey S., Doyle M., Eliez S., Hansen A.S., Hebebrand J., Hillegers M., Jacobs B., Karwautz A., Kiss E., Kotsis K., Kumperscak H.G., Pejovic-Milovancevic M., Christensen A.M.R., Raynaud J.-P., Westerinen H., Visnapuu-Bernadt P. Potential effects of “social” distancing measures and school lockdown on child and adolescent mental health. Eur. Child Adolesc. Psychiatr. 2020;29:739–742. doi: 10.1007/s00787-020-01549-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Green P. Risks to children and young people during covid-19 pandemic. BMJ. 2020;369:m1669. doi: 10.1136/bmj.m1669. [DOI] [PubMed] [Google Scholar]
- 40.Cuartas J. Heightened risk of child maltreatment amid the COVID-19 pandemic can exacerbate mental health problems for the next generation. Psychological Trauma: Theory, Research, Practice, and Policy. 2020 doi: 10.1037/tra0000597. [DOI] [PubMed] [Google Scholar]
- 41.Kaufman K.R., Petkova E., Bhui K.S., Schulze T.G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open. 2020;6 doi: 10.1192/bjo.2020.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yao H., Chen J.-H., Xu Y.-F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tracy M., Norris F.H., Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress. Anxiety. 2011;28:666–675. doi: 10.1002/da.20838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davis C., Ng K.C., Oh J.Y., Baeg A., Rajasegaran K., Chew C.S.E. Caring for children and adolescents with eating disorders in the current coronavirus 19 pandemic: a Singapore perspective. J. Adolesc. Health. 2020;67:131–134. doi: 10.1016/j.jadohealth.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bandyopadhyay G., Meltzer A. Let's unite against COVID-19 - a New Zealand perspective. Ir. J. Psychol. Med. 2020 doi: 10.1017/ipm.2020.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carbone S.R. Flattening the curve of mental ill-health: the importance of primary prevention in managing the mental health impacts of COVID-19. Mental Health & Prevention. 2020;19:200185. doi: 10.1016/j.mhp.2020.200185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wade M., Prime H., Browne D.T. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatr. Res. 2020;290:113143. doi: 10.1016/j.psychres.2020.113143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. The Lancet Public Health. 2020;5:e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prime H., Wade M., Browne D.T. American Psychologist; 2020. Risk and Resilience in Family Well-Being during the COVID-19 Pandemic. [DOI] [PubMed] [Google Scholar]
- 51.McGrath J. ADHD and Covid-19: current roadblocks and future opportunities. Ir. J. Psychol. Med. 2020 doi: 10.1017/ipm.2020.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Öğütlü H. Turkey's response to COVID-19 in terms of mental health. Ir. J. Psychol. Med. 2020:1–4. doi: 10.1017/ipm.2020.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sani G., Janiri D., di Nicola M., Janiri L., Ferretti S., Chieffo D. Mental health during and after the COVID-19 emergency in Italy. Psychiatr. Clin. Neurosci. 2020;74 doi: 10.1111/pcn.13004. 372–372. [DOI] [PubMed] [Google Scholar]
- 54.Franic T., Dodig-Curkovic K. Covid-19, child and adolescent mental health – Croatian (in)experience. Ir. J. Psychol. Med. 2020:1–4. doi: 10.1017/ipm.2020.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.de Anda H.H., Braithwaite S., EMS . 2020. Criteria for Disaster Declaration.http://www.ncbi.nlm.nih.gov/pubmed/30969625 [PubMed] [Google Scholar]
- 56.Sandifer P.A., Walker A.H. Enhancing disaster resilience by reducing stress-associated health impacts. Frontiers in Public Health. 2018;6 doi: 10.3389/fpubh.2018.00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dube A., Moffatt M., Davison C., Bartels S. Health outcomes for children in Haiti since the 2010 earthquake: a systematic review. Prehospital Disaster Med. 2018;33:77–88. doi: 10.1017/S1049023X17007105. [DOI] [PubMed] [Google Scholar]
- 58.Rajkumar A.P., Mohan T.S.P., Tharyan P. Lessons from the 2004 Asian tsunami: epidemiological and nosological debates in the diagnosis of post-traumatic stress disorder in non-Western post-disaster communities. Int. J. Soc. Psychiatr. 2013;59:123–129. doi: 10.1177/0020764011423468. [DOI] [PubMed] [Google Scholar]
- 59.Conger R.D., Ge X., Elder G.H., Lorenz F.O., Simons R.L. Economic stress, coercive family process, and developmental problems of adolescents. Child Dev. 1994;65:541. doi: 10.2307/1131401. [DOI] [PubMed] [Google Scholar]
- 60.McLoyd V.C., Jayaratne T.E., Ceballo R., Borquez J. Unemployment and work interruption among african American single mothers: effects on parenting and adolescent socioemotional functioning. Child Dev. 1994;65:562. doi: 10.2307/1131402. [DOI] [PubMed] [Google Scholar]
- 61.Pilowsky D.J., Wickramaratne P., Nomura Y., Weissman M.M. Family discord, parental depression, and psychopathology in offspring: 20-year follow-up. J. Am. Acad. Child Adolesc. Psychiatr. 2006;45:452–460. doi: 10.1097/01.chi.0000198592.23078.8d. [DOI] [PubMed] [Google Scholar]
- 62.Solantaus T., Leinonen J., Punamäki R.-L. Children's mental health in times of economic recession: replication and extension of the family economic stress model in Finland. Dev. Psychol. 2004;40:412–429. doi: 10.1037/0012-1649.40.3.412. [DOI] [PubMed] [Google Scholar]
- 63.Belsky J., Pluess M. Beyond diathesis stress: differential susceptibility to environmental influences. Psychol. Bull. 2009;135:885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- 64.Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatr. Ment. Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bayham J., Fenichel E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. The Lancet Public Health. 2020;5:e271–e278. doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]