Abstract
Introduction
The ongoing pandemic of COVID-19 brought to the fore prone positioning as treatment for patients with acute respiratory failure. With the increasing number of patients in prone position, both spontaneously breathing and mechanically ventilated, cardiac arrest in this position is more likely to occur.
This scoping review aimed to summarize the available evidence on cardiopulmonary resuscitation in prone position (‘reverse CPR’) and knowledge or research gaps to be further evaluated. The protocol of this scoping review was prospectively registered on 10th May 2020 in Open Science Framework (https://osf.io/nfuh9).
Methods
We searched PubMed, EMBASE, MEDLINE and pre-print repositories (bioRxiv and medRxiv) for simulation, pre-clinical and clinical studies on reverse CPR until 31st May 2020.
Results
We included 1 study on manikins, 31 case reports (29 during surgery requiring prone position) and 2 nonrandomized studies describing reverse CPR. No studies were found regarding reverse CPR in patients with COVID-19.
Conclusions
Even if the algorithms provided by the guidelines on basic and advanced life support remain valid in cardiac arrest in prone position, differences exist in the methods of performing CPR. There is no clear evidence of superiority in terms of effectiveness of reverse compared to supine CPR in patients with cardiac arrest occurring in prone position. The quality of evidence is low and knowledge gaps (e.g. protocols, training of healthcare personnel, devices for skill acquisition) should be fulfilled by further research. Meanwhile, a case-by-case evaluation of patient and setting characteristics should guide the decision on how to start CPR in such cases.
Keywords: Prone CPR, Reverse CPR, Prone position, COVID-19
Abbreviations
- AHA
American Heart Association
- COVID-19
Coronavirus disease 2019
- CPR
Cardiopulmonary resuscitation
- ERC
European Resuscitation Council
- EtCO2
End-tidal carbon dioxide
- FiO2
Inspired fraction of oxygen
- ICU
Intensive care unit
- PEA
Pulseless electric activity
- PPE
Personal protective equipment
- RCT
Randomized clinical trial
- ROSC
Return of spontaneous circulation
- UK
United Kingdom
- VF
Ventricular fibrillation
1. Introduction
Cardiopulmonary resuscitation (CPR) is the cornerstone of the treatment of cardiac arrest, improving patients' chances of defibrillation and eventual survival [1]. The algorithms of cardiopulmonary resuscitation include the provision of high-quality chest compressions and rapid defibrillation [1]. Manual chest compressions are described as effective when delivered ‘in the centre of the chest’, with a depth of 5–6 cm, and at a rate of 100–120 min−1, with less interruptions as possible and complete chest recoil after each compression [1].
These algorithms can be applied in most settings, with specific indications for special circumstances (e.g. drowning, hypothermia or hostile environments) [2]. Among the possible scenarios, cardiac arrest occurring in prone positioned patients may slightly increase the complexity of the procedures, with additional pitfalls.
The main aim for starting CPR in prone position, also known as ‘reverse CPR’, may be the reduction of the no flow time (blood flow to the heart or brain), since turning a prone patient into the supine position requires additional time and focusing (e.g. not to disconnect the patient from the ventilator during supination) and may delay resuscitation.
Prone position as treatment for acute respiratory distress syndrome (ARDS) has been firstly described in 1976 [3]. During the current coronavirus disease 2019 (COVID-19) pandemic, it has been widely used in both spontaneously breathing and mechanically ventilated patients with acute respiratory failure [4,5]. An increasing number of cardiac arrests [6] is expected during COVID-19 era in the prone position. Furthermore, coronavirus diseases 2019 (COVID-19) has resulted in the emergence of new clinical challenges in the context of cardiac arrest, as the time required for personal protective equipment (PPE) donning, the need to clamp endotracheal tubes or to temporarily stop mechanical ventilation to reduce rescuers' exposure. These issues add complexity to the procedure [7].
This scoping review aimed to summarize the available evidence on the cardiopulmonary resuscitation in prone position (‘reverse CPR’) and to highlight possible knowledge or research gaps to be further evaluated.
2. Methods
2.1. Search strategy
For the purpose of this review, we searched PubMed, EMBASE, and MEDLINE for pre-clinical and clinical studies on prone CPR. Our search included the keywords “resuscitation”, “CPR”, “chest compression”, “cardiopulmonary”, “resuscitation”, “prone position” as exact phrases and a combination of broad subject headings according to databases syntax. Specifically, the EMBASE engine was used with the following query: (‘resuscitation’ OR ‘cpr’ OR ‘chest compression’/exp. OR ‘chest compression’ OR cardiopulmonary OR ‘resuscitation’/exp. OR resuscitation) AND (‘prone position’/exp. OR ‘prone position’ OR ‘prone positioning’/exp. OR ‘prone positioning’ OR ‘prone’ OR ‘proning’) AND ([embase]/lim OR [medline]/lim OR [pubmed-not-medline]/lim).
A search was also conducted on main pre-print repositories (bioRxiv and medRxiv) from inception to 31st May 2020 for relevant studies. No limitations were imposed for specific contexts, with the aim of including surgical, medical and intensive care settings. Articles on animals or on manikins were also eligible. Randomized controlled trials (RCTs), nonrandomized studies (both prospective or retrospective), case series and case reports were included. Abstracts and conference proceedings were excluded. Snowballing search on the references of selected articles was also performed.
After the exclusion of duplicates and abstracts, two authors (AM, PI) independently screened full-text papers to include the most relevant on the topic and independently charted data using an electronic standardized form. In case of case reports or series describing more than one patient, we collected data only on patients meeting inclusion criteria (i.e. cardiac arrest occurring in prone position and CPR performed).
We collected data regarding the type of study (e.g. design and country), population characteristics at baseline (e.g. age, main disease), setting (e.g. operatory room, ICU), occurred events (e.g. rhythm and cause of the cardiac arrest), intervention (e.g. prone or standard CPR) and outcomes (e.g. mortality, return of spontaneous circulation - ROSC). Data were then tabulated for presentation, as appropriate.
The protocol of this scoping review was prospectively registered on 10th May 2020 (https://osf.io/nfuh9).
The scoping review was conducted following PRISMA statement extension for scoping reviews [8].
3. Results
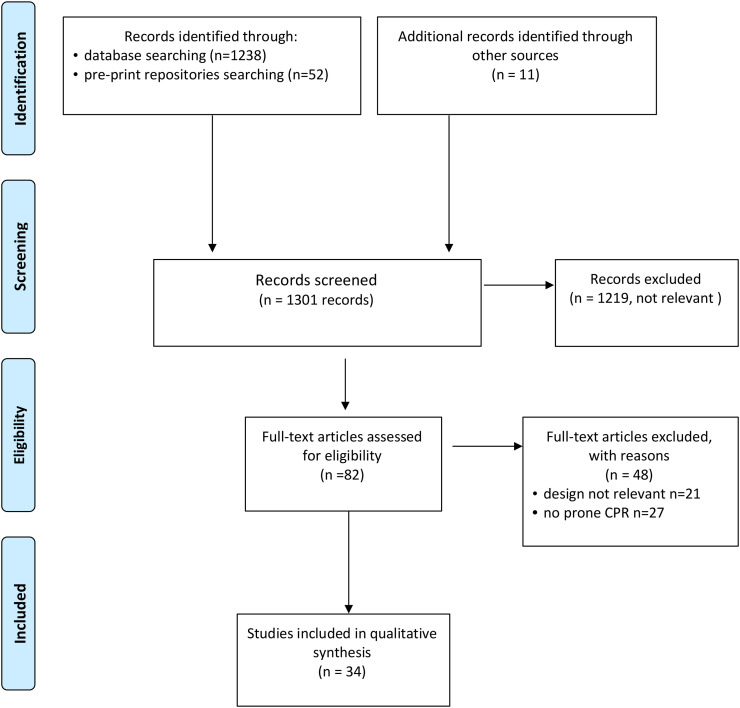
The initial search identified 1301 results from EMBASE, PubMed and other sources. Following screening of titles and abstracts and removing duplicates, we evaluated 82 articles in full text. Among these, we selected and included 34 articles. The search from pre-print repositories (bioRxiv and medRxiv) resulted in 52 records screened, none included. The details on the inclusion/exclusion process are provided in the PRISMA flow diagram (see Fig. 1 ).
Fig. 1.
PRISMA flow diagram.
The figure shows the inclusion/exclusion process with details, as appropriate.
We found no RCT comparing prone to standard supine CPR. Three of the included studies [[9], [10], [11]] had a nonrandomized design and 31 were case reports [[12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42]]. In this section, the included nonrandomized studies are described; a complete description of all the studies, including case reports, is provided with details in Table 1 .
Table 1.
Characteristics of the included studies.
| Author (Year) | Design | Setting; Country | Patients | Event and cause | Intervention | Results |
|---|---|---|---|---|---|---|
| Al Harbi et al. (2020) [12] | Case report | Operating room (Posterior spinal fusion with laminectomy); Saudi Arabia | 80 years old male patient at intermediate cardiac risk | Two episodes of PEA at about 6 h from anesthesia induction. The latter in supine position. Cause: massive pulmonary embolism | First episode: CPR in prone position Second episode: CPR in supine position | First episode: ROSC, supination and second episode of cardiac arrest; Second episode: ROSC and ICU admission |
| Mishra et al. (2019) [13] | Case report | Operating room (Laminectomy and excision of a C2–C3 intradural extra-medullary meningioma); India | 35 years old female patient | Intraoperative cardiac arrest, due to cardiac tamponade | 1 min prone position CPR, followed by supination and standard CPR | ROSC, ICU admission with pericardial catheterism and negative suction; extubation at day 3 |
| Mayorga-Buiza et al. (2018) [14] | Case report | Operating room (Excision of a large tumour in the posterior fossa); Spain | 10 years old patient | Pulseless VT, then VF during mobilization and resection of the tumour | CPR in prone position | ROSC followed by spinal hematoma, then surgically drained. Survived without sequelae at 24 months |
| Burki et al. (2017) [15] | Case report | Operating room (Fourth ventricle tumour excision); Pakistan | 6 years old female patient | Intraoperative cardiac arrest, due to massive bleeding (estimated blood loss 2 l) | CPR in prone position | ROSC and ICU admission. Death at day 5 after surgery |
| Kaloria et al. (2017) [16] | Case report | Operating room (Tethered cord release and removal of bony spur); India | 1 year old girl | Electromechanical dissociation, possibly due to venous air embolism | CPR in prone position | ROSC, surgery completion, discharge at day 6 |
| Lee-Archer and Chaseling (2017) [17] | Case report | Operating room (Posterior spinal fusion C5 to L4, for severe kyphoscoliosis); Australia | 10 years old girl | Cardiac arrest during attempts to locate the epidural space with a loss of resistance air technique, possibly due to air embolism | Supination and standard CPR | ROSC, completion of surgery at day 4, right-sided brain infarction and left upper limb weakness, recovered after two weeks |
| Pinheiro et al. (2017) [18] | Case report | Operating room (Esthetic lipoplasty) | 25 years old female patient | Asystole | Supination and standard CPR | ROSC, surgery cancelled, ICU admission, discharge |
| Taylor et al. (2013) [19] | Case report | Operating room (Craniotomy for metastatic melanoma); New Zeland | 69 years old male patient with hypertrophic cardiomyopathy and impaired (34%) ejection fraction | Pulseless VT, then VF. | CPR in prone position | ROSC. Discharged home in stable neurological condition |
| De Souza Gomez et al. (2012) [20] | Case report | Operating room (Excision of highly vascularized parietal-occipital meningioma on the right side); Brazil | 77 years old female patient | Cardiac arrest, due to rupture of sagittal sinus and subsequent hemorrhagic shock | CPR in prone position | ROSC, ICU admission, discharge at day 3 |
| Pan et al. (2012) [22] | Case report | Endoscopic room (ERCP) | 61 years old female patient | Intraprocedural cardiac arrest, due to venous air embolism | Supination and standard CPR | Death |
| Dooney (2010) [21] | Case report | Operating room (L4-L5 microscopic discectomy); South Australia | 43 years old male patient | Asystole | CPR in prone position | ROSC |
| Dumont et al. (2010) [23] | Case report | Operating room (Arthrodesis for atlantoaxial instability) | 38 years old male patient | Asystole, due to air embolism | Supination and standard CPR | ROSC, surgery completion, ICU admission and discharge without sequelae |
| Haffner et al. (2010) [24] | Case report | Operating room (Emergency craniotomy for cerebellar hemorrhage) | 81 years old | Intraoperative cardiac arrest, possibly due to right heart failure | Prone CPR | ROSC; ICU admission; death at day 28 |
| Almazan et al. (2009) (personal communication reported by Brock-Utne in “Case Studies of Near Misses in Clinical Anesthesia”) [25] | Case report | Operating room (Open reduction internal fixation for multiple pelvic fractures); NA | 28 years old male patient | PEA due to pulmonary embolism | CPR in prone position | ROSC, ICU admission; surgery completion three days later; discharged from the hospital with intact neurological status |
| Beltran and Mashour (2007) [26] | Case report | Operating room (Skullbase craniotomy for tumour debulking); USA | 21 years old female patient with neurofibromatosis type 2 | PEA due to sigmoid sinus disruption, leading to significant blood loss | Supination and standard CPR | Intraoperative death |
| Wei et al. (2006) [9] | Single-centre nonrandomized study | ICU/healthy volunteers; Taiwan | a. 11 patients who had died in ICU b. 10 alive and healthy volunteers |
a. Death b. None |
a. One minute precordial cardiac massage followed by one minute thoracic massage in prone position; b. Back thoracic compressions with spontaneous breathing held and nose clipped |
a. Mean blood pressure (invasively monitored) achieved with standard precordial compressions was 55 ± 20 / 13 ± 7 vs. 79 ± 20 / 17 ± 10 in prone position compression. b. Mean tidal volume with back thoracic compression was 399 ± 110 ml |
| Smelt (2005) [27] | Case report | Operating room (Scoliosis correction); The Netherlands | 16 years old male patient with Duchenne muscular dystrophy and cardiomyopathy with EF 25% | VT, then pulseless VF | Supination and standard CPR | ROSC, ICU admission, discharge at day 10 |
| Mazer et al. (2003) [10] | Single-centre nonrandomized study | ICU; USA | 6 patients with cardiac arrest, enrolled after failed standard CPR | 4 PEA; 1 pulseless VF; 1 pulseless VT | 30 min of prone position CPR after standard CPR failure declared | Systolic blood pressure mean improvement 23 ± 14 mmHg from standard to reverse CPR; calculated MAP mean improvement of 14 ± 11 mmHg from standard to reverse CPR; diastolic blood pressure mean improvement of 10 ± 12 mmHg from standard to reverse CPR |
| Chen et al. (2002) [28] | Case report | Operating room (L2 and L4 percutaneous vertebroplasty); Taiwan | 75 years old female patient with minor diastolic dysfunction and pulmonary hypertension | PEA, possibly due to pulmonary embolism | Supination and standard CPR | Intraoperative death |
| Miranda and Newton (2001) [29] | Case report | Operating room (Palliative debulking of metastatic tumour at T3 and internal fixation of the thoracic spine); UK | 39 years old female patient | Intraoperative pulseless VF, possibly due to altered potassium levels | Sharp thump in prone position, followed by CPR | ROSC, completion of surgery and discharge home at 1 week from the event |
| Brown et al. (2001) [30] | Case report | Operating room (Thoracic spine decompression surgery for an invasive tumour between T11 and L1 vertebral levels); UK | 60 years old female patient | Broad complex tachycardia followed by VT. Suspected cause: venous air embolism | Defibrillation in prone position | ROSC, completion of surgery, extubation on the following day, full recovery without sequelae |
| Atkinson (2000) [11] | Single-centre nonrandomized study | Mannequin based simulation | 36 nurses trained in performing advanced life support | Simulation with prone positioned mannequin on standard examination coach, with gel-pad under the sternum | 100 midline compressions | 3376 registered by the skillmeter (91.8% of the total possible). 1168 (34.6%) effective, 1370 (40.6%) partially effective and 838 (24.6%) ineffective |
| Reid and Appleton (1999) [31] | Case report | Operating room (Spinal surgery to correct progressive scoliosis) | 15 years old boy with Duchenne muscular dystrophy | Pulseless VF | Left posterior thoracotomy and direct cardiac massage, then defibrillation | ROSC, full recovery after ICU stay |
| Sutherland and Winter (1997) [32] | Case report | Operating room (a. T1-sacrum posterior spinal fusion with sublaminar wiring for a progressive scoliosis; b. T2-sacrum posterior spinal fusion with sublaminar wiring for a progressive scoliosis); UK |
|
|
CPR begun in prone position and continued in supine position | Intraoperative death |
| Dequin et al. (1996) [33] | Case report | ICU; France | 48 years old male patient with CAP | Asystole, occurred few minutes after prone positioning | CPR in prone position | ROSC, recovery at day 7 from the event |
| Gueugniaud et al. (1995) [34] | Case report | Operating room (Surgical correction of a right dorsal and left lumbar scoliosis); France | 15 years old boy | Intraoperative pulseless electromechanical dissociation followed by asystole, probably due to myocardial ischaemia | CPR in prone position, then supination | ROSC, surgery postponed, full recovery without neurological sequelae |
| Kelleher and Mackersie (1995) [35] | Case report | Operating room (Elective foramen magnum decompression); UK | 6 months old achondroplastic baby with small patent foramen ovale and a left to right shunt | Multifocal ventricular ectopics, bradycardia and asystole (two episodes). Suspected cause: venous air embolism and estimated total blood loss of 1.1 l | CPR with fingers of one hand in prone position (two episodes) | ROSC, ICU admission, discharge at day 7 |
| Tobias et al. (1994) [36] | Case report | Operating room (Spinal fusion for progressive scoliosis); USA | 12 years old boy with severe spastic quadriplegia | Asystole, possibly due to large amount of blood loss | CPR in prone position | ROSC, ICU admission, uneventful postoperative course |
| Loewenthal et al. (1993) [37] | Case report | Operating room (Excision of a meningioma of the posterior fossa); France | 53 years old female patient | Asystole, possibly due to large amount of blood loss | CPR in prone position | ROSC, ICU admission, recovery and completion of surgery during the day of the event |
| Sun et al. (1992) [38] | Case report | Operating room (a. posterior fossa craniotomy for intracerebral hematoma; b. emergency decompression laminectomy); Taiwan |
|
|
CPR in prone position | ROSC, surgery completion and uneventful recovery |
| Albin et al. (1991) [39] | Case report | Operating room (a. Lumbar laminectomy with fusion L3–4; b. lumbar laminectomy with fusion L5-S1); USA |
|
|
Supination and standard CPR | Intraoperative death |
| Ewah and Calder (1991) [40] | Case report | Operating room (Surgical treatment of prolapsed lumbar intervertebral disc at L4–5); UK | 26 years old female patient | Cardiac arrest, due to laceration of the aorta and subsequent retroperitoneal and peritoneal hemorrhage | Supination and standard CPR | Intraoperative death |
| Lang et al. (1989) [42] | Case report | Operating room (Posterior spinal fusion for progressive scoliosis); Canada | 16 years old male patient with Duchenne muscular dystrophy | Cardiac arrest, due to venous air embolism | Supination and standard CPR | Intraoperative death |
| Kalenda and Greuter (1982) [41] | Case report | Operating room (excision of a cerebellar and fourth ventricle ependymoma); The Netherlands | 1-year old boy | Circulatory arrest | CPR in prone position | ROSC, surgery completion and recovery |
The table shows the characteristics of the included studies, as reported by the authors.
Data are reported as percentages, fractions, mean ± standard deviation or median (IQR), as appropriate.
CPR, cardiopulmonary resuscitation; EF, ejection fraction; ICU, intensive care unit; NA, not available; PEA, pulseless electric activity; ROSC, return of spontaneous circulation; UK, United Kingdom; USA, United States of America; VF, ventricular fibrillation; VT, ventricular tachycardia.
The first study evaluating the feasibility of reverse CPR was a simulation study using Laerdal ‘ResusciAnne’ manikins, posed in prone position on a standard examination coach, with a gel pad under the sternum. Thirty-six trained nurses were asked to perform 100 compressions on the manikin with no breaks for respirations. Using a skillmeter, a total of 3376 compressions (91.8% of the 3600 total possible) were registered, but only 1168 (34.6%) were effective (4–5 cm compression depth), with 1370 (40.6%) partially effective (2–4 cm compression depth) and 838 (24.6%) ineffective (<2 cm compression depth) compressions. Only 9/36 nurses were able to perform 70% or more adequate compressions (usually considered as the acceptable threshold). An important insight was provided by the authors, discussing that all the nurses had judged CPR in the prone position as more tiring than in the standard position. This, in addition to the light weight of the manikin and the position of the nurses (left-hand side of the manikin), may explain the low rate of successful compressions and the number of compressions performed off the midline (11.2% to the right of midline, 4.1% too high, 6.1% too low, none to the left of the midline). None of the eligible studies were conducted on animals.
Among the nonrandomized studies on humans, one was conducted on 11 cadavers and 10 healthy volunteers, evaluating indirect outcomes (blood pressure and tidal volume) [9]. Mean arterial pressure (MAP) was invasively measured in cadavers both during standard and consecutive back chest compressions (55 ± 20/13 ± 7 vs. 79 ± 20/17 ± 10 p = 0.028) performed at a rate of 60 per minute. Healthy volunteers' tidal volume was then measured using a mouthpiece connected to a spirometer, while they were receiving back chest compressions (60 min−1). Spontaneous breathing was held, and a nose clip applied on the volunteers. Mean registered tidal volume was of 399 ± 110 ml. The authors highlighted that their findings may support prone CPR in non-intubated patients, since airways open spontaneously, and adequate ventilation seems achievable with compressions only. Nonetheless, the study has limited external validity, especially for the finding regarding tidal volume (e.g. possibly not generalizable to patients with a compromised pulmonary function), requiring further investigations.
Another nonrandomized study enrolled six ICU patients in cardiac arrest, after the declared failure of standard CPR [10]. Main results included a systolic blood pressure mean improvement of 23 ± 14 mmHg, a calculated MAP mean improvement of 14 ± 11 mmHg and a diastolic blood pressure mean improvement of 10 ± 12 mmHg from standard to reverse CPR, but no cases of ROSC.
Despite such a limited basis, we retrieved a total of 31 case reports described in literature from 1982 (date of the first retrieved report) to date, for a total of 34 patients.
Among the included case reports, 29 described cardiac arrests occurred during surgery. Surgeries included spinal surgery in 20 patients (e.g. discectomies, scoliosis correction, vertebral metastases), craniotomy in 10 patients (e.g. primitive or metastatic cancer, hemorrhage), and cases of pelvic fracture and dorsal lipoplasty. One occurred in the ICU [33] in a prone positioned mechanically ventilated patient, admitted for community acquired pneumonia and acute respiratory failure. Another article reported a case of cardiac arrest during endoscopic retrograde cholangiopancreatography procedure [22]. Fifteen of the described patients were children (≤16 years old), and three were infants (≤1 year old).
No studies were found regarding reverse CPR in patients with COVID-19.
4. Discussion
The feasibility of CPR in prone position has been under investigated. Its use has been described in the settings of both operatory rooms (e.g neurosurgery, orthopedics) and ICUs (e.g. mechanically ventilated patients with respiratory failure), mainly on case reports.
The main finding of this scoping review is that there is insufficient evidence on the topic and further evidence is needed, considering that an increasing number of cardiac arrests in prone position are expected during the COVID-19 pandemic.
Many aspects, both decisional and technical, have been described but remain controversial and need to be investigated with adequately designed studies.
4.1. Available evidence
To date, evidence on reverse CPR comes from case reports and small sized nonrandomized studies conducted on manikins, cadavers, healthy volunteers or patients with previously failed standard CPR. Among the included reports, ROSC after reverse CPR occurred in 23 out of 31 cases, demonstrating that the technique may be effective and deserves further investigations. Nevertheless, publication bias may exist, potentially overestimating the rate of favorable outcomes in prone CPR, and potentially limiting our findings. We did not find any RCT on the topic and nonrandomized studies only provide preliminary and indirect data to support the technique. Despite prone CPR may be a feasible and safe option in specific settings, further literature is needed, with many aspects remaining uninvestigated.
4.2. Causes of cardiac arrest in prone position
From the evaluated articles, it can be argued that a frequent cause of cardiac arrest in prone position is air embolism, a potentially fatal event, often occurring in neurosurgery and closely related to the position of the patient and the presence of a pressure gradient allowing air flow into the vessels. Other causes are linked with the specific patient positioning, which can sometimes lead to vessel occlusion and reduced venous return. Hypovolemia in combination with reduced venous return can quickly lead to reduced cardiac output.
The rhythm presentation is various, ranging from asystole to pulseless electrical activity (PEA), or ventricular fibrillation (VF).
4.3. Pro and contra of reverse and standard CPR
In the event of a cardiac arrest in a prone positioned patient, the clinicians have limited time to decide whether to turn the patient into supine position, before starting CPR, or immediately start a reverse CPR. There is no clear evidence of superiority in terms of effectiveness of reverse compared to supine CPR in patients with cardiac arrest occurring in prone position. Thus, clinicians should take into account several factors when deciding how to start CPR in such cases. Turning the patient into supine position before starting CPR could be very difficult for several reasons: i) this maneuver is time consuming, and can potentially increase the no-flow time to the brain; ii) it may need at least 3–4 operators, not always available in surgical or ICU settings; iii) it could be dangerous for the patients, due to the presence of an open wound, protruding metal work, an unstable spine and fixed head to a Mayfield Skull Clamp potentially causing neurologic injuries, or iv) it could cause the dislodgment of the endotracheal tube and the loss of monitoring. Furthermore, the decision to perform supination and proceed with a standard CPR entails other risks, such as a difficult hemorrhage control (e.g. during spinal surgery) [30]. On the other hand, healthcare personnel might be reluctant to perform reverse CPR as a first option, especially due to the lack of specific training and knowledge of the procedure. Other concerns may regard the presence of an open surgical field, the limited surface to perform compressions, the need for a counterforce under the sternum and the risks of spinal damages. Notwithstanding, cardiac massage in this position is less likely to cause rib fractures, injury to the heart and aspiration pneumonia [9].
4.4. Practical aspects and guidelines recommendations
Since 2005, the American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care recommended that CPR in the prone position might be reasonable when the patient cannot be replaced in the supine position without prejudice, particularly in hospitalized patients with an advanced airway in place [1].
AHA interim guidance for CPR in patients with COVID-19 recommends to attempt to place in the supine position for continued resuscitation of patients with suspected or confirmed COVID-19 who are in a prone position without an advanced airway, and to avoid turning the patient to the supine position if an advanced airway is secured, unless able to do so without risk of equipment disconnections and aerosolization [7]. Similar recommendations are also supported by the European Resuscitation Council (ERC) in its COVID-19 guidelines [43], suggesting to turn patient supine in case of ineffective compressions (arterial line and aim for diastolic pressure greater than 25 mmHg), airway problems or unrestored circulation (after minutes) [43].
A recent joint position statement from Brazilian societies of cardiology, intensive care medicine, anesthesiology and emergency medicine recommends to turn into supine position the patients once safely possible, due to insufficient evidences on reverse CPR and suggests monitoring using partial pressure of end-tidal carbon dioxide partial (EtCO2 > 10 mmHg) and diastolic pressure (>20 mmHg) [44].
An early planning of supination is recommended, since it may require additional help [30,44]. For the specific setting of neurosurgery, UK Resuscitation Council suggests that there is no immediate need to turn the patient to the supine position once cardiac arrest has occurred in the prone position, suggesting to start CPR in the prone position [45]. If the aforementioned techniques are not rapidly feasible or become unsuccessful, thoracotomy and direct internal cardiac massage and/or defibrillation are available options [30].
Once a cardiac arrest is detected in a prone positioned patient, first of all it is important to make sure that airway is secured and the tube is not kinked, obstructed or displaced, in case of intubated patients. Then, it is needed to ensure that the ventilator is connected to the patient with 100% FiO2 concentration and that there is no unidentified loss of blood [12]. If venous air embolism is suspected, the patient's head should stay down, to increase venous pressure, and the surgical field should be flooded with saline. After that, chest compressions should be started.
Unfortunately, only general indications are provided by the guidelines on how to perform cardiac massage in prone position [46].
Some are provided in AHA recent interim guidance for patients with COVID-19 [7], specifying that “if unable to safely transition the patient to a supine position, place the defibrillator pads in the anterior-posterior position and provide CPR with the patient remaining prone with hands in the standard position over the T7/10 vertebral bodies”.
Chest compressions can be performed on the posterior thoracic spine at levels between the scapulae, using either a one or two-handed technique, with or without a counterpressure on the sternum. A two-handed technique for chest compressions over the mid-thoracic spine located between the two scapula and the use of a counter-pressure applied by a second person is recommended by Intensive Care Society [47].
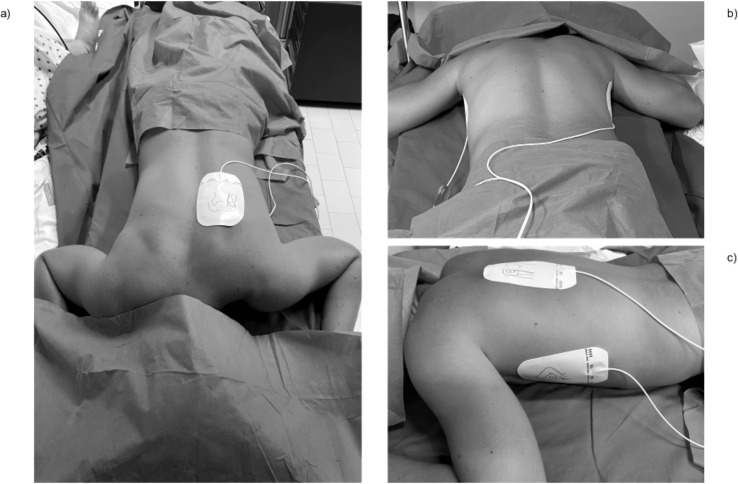
ERC provides some other practical indications [43], suggesting compressing between the scapulae (shoulder blades) at the usual depth and rate (5 to 6 cm at 2 compressions per second) and placing defibrillator pad in anterior-posterior (front and back) or bi-axillary (both armpits) position (Fig. 2 ). Alternatively, defibrillator pads can be applied in posterolateral position [29], i.e. one pad in the left mid-axillary line and a second one over the right scapula, or over the left scapula (Fig. 2) [19].
Fig. 2.
Suggested positions for defibrillator pads placement.
The figure shows the positions of defibrillator pads, as described in available literature. Panel a) antero-posterior placement; panel b) bi-axillary placement; panel c) postero-lateral placement.
A study by Min-Ji Kwon found that in prone position, the largest LV cross-sectional area is located 0 to 2 vertebral segments below the line crossing both the inferior angles of the scapula in at least 86% of patients [48].
Some patients will be positioned prone with the aid of a pillows allowing free movement of the chest and abdomen and preventing the reduction of venous return during surgery. Sternal counterpressure may increase the effectiveness of chest compressions in these circumstances, with beneficial effects on both cardiac-pump and thoracic-pump at each compression. Sandbags, fluid bags or gel pads may be used as sternal counterpressure.
The effectiveness of reverse CPR also depends on the greater strength of thoracic costovertebral joints as compared to sternal costochondral junction and on the absence of abdominal contents displaced anteriorly and dissipating the compression force [15].
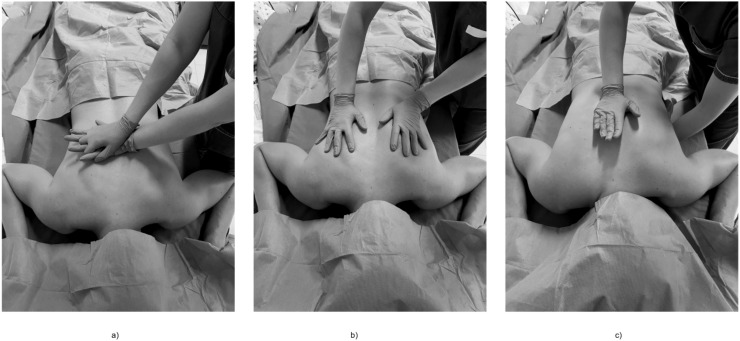
Several options have been described regarding hands position during back chest compressions. An option involves the use of two hands together at the midline at the midthoracic level (Fig. 3, panel a). If sternal support is present, rescuer's hands can be placed on either side of the eventual incision at the midthoracic level, with the palms placed over the patient's scapulae, thus preserving the sterility of the surgical field (Fig. 3, panel b).
Fig. 3.
Suggested position of rescuer's hands in reverse cardiopulmonary resuscitation.
The figure shows the position of rescuer's hands, as described in available literature, for compressions during reverse cardiopulmonary resuscitation. Panel a) midline position; panel b) lateral position; c) one-hand technique with sternal counterpressure.
A one-handed technique can be performed without sternal supports, with the flat of one hand (or with the hand clinched into a fist) on the lower third of the sternum used as counter pressure and the second one on the thoracic spine, and could be performed by one or two physicians (Fig. 3, panel c) [33].
In the pediatric population cardiac massage can be started in the prone position using the fingers of one hand over the thoracic vertebral column at the level of the scapulae [35] with the same rate and force as they were delivered during supine position.
4.5. Issues related to COVID-19
The COVID-19 pandemic represents a new challenge for clinicians in many fields, including CPR. Among various concerns, the increasing number of prone patients under mechanical ventilation carries along a likely increasing number of cardiac arrests occurring in this position. Hypoxemic respiratory failure secondary to acute respiratory distress syndrome, myocardial injury, ventricular arrhythmias, and shock are common in critically ill patients and put them at high risk of cardiac arrest. Plus, many pharmacological treatments proposed for COVID-19, such as hydroxychloroquine and azithromycin, can prolong the QTs potentially leading to cardiac arrests in high risk patients [49].
A critical point is the risk of viral transmission to healthcare workers during CPR, classified as an aerosol-generating procedure and requiring adequate personal protective equipment [50]. The general principles for resuscitation in COVID-19 patients [7,43] are: i) all the rescuers should wear personal protective equipment (PPE) before beginning CPR; ii) minimize the number of personnel in the room and use a negative-pressure room whenever possible; iii) may use a mechanical device for chest compression if available; iv) use HEPA filter and tight seal for bag-mask ventilation and mechanical ventilation, v) emphasize early intubation performed by the most expert provider, using video laryngoscopy if resources and expertise are available; vi) avoid prolonged resuscitation efforts, since available reports estimate high 30-day mortality rates (97%) in adult COVID-19 patients experiencing cardiac arrest, with low ROSC rates (13%) [51].
All these aspects, together with the issues related to prone position, make the resuscitation of patients with COVID-19 a complex procedure, even for experienced personnel. For all these reasons, healthcare workers need periodical training on manual prone positioning CPR techniques. Simulation training could improve comfort and competence in the procedure and in managing potential complications. To date, no studies have evaluated the efficacy of training for reverse CPR or the use of feedback systems, used to maximize the quality of standard CPR. Furthermore, currently available manikins are not validated for the use in prone position, thus limiting training opportunities. Therefore, there is an urgent requirement for best practice guidance to performing CPR in prone positioned, intubated and non-intubated patients with COVID-19 during the pandemic.
4.6. Future research
Controversial aspects about reverse CPR need to be further investigated with adequately designed studies, to support clinicians with evidence-based indications (e.g. best compressions rate, best thoracic level for compressions, best sternal counterpressure, need for ventilation, decisional algorithm for supination, reverse CPR and thoracotomy with direct cardiac massage). Plus, the preliminary evidence of reverse compressions potentially determining adequate ventilation and tidal volume should be further addressed and has potential implication in other clinical contexts. Healthcare personnel involved in the care of prone positioned patients would also benefit of specific protocols for periodical training on how to perform CPR in a prone patient.
Meanwhile, the available CPR guidelines should be followed.
5. Conclusions
Reverse CPR has been performed and described in several settings, but evidence is based on case reports and preliminary small sized nonrandomized studies. The procedure has been described in settings such as neurosurgery and prone position mechanical ventilation, and an increasing number of cardiac arrests in prone positioned patients is expected in the COVID-19 era. The quality of available evidence is low and knowledge gaps should be fulfilled by further adequately designed studies that are urgently needed. Meanwhile, a case-by-case evaluation of patient and setting characteristics should guide the decision on how to start CPR in such cases.
Authors' contribution
Conceptualization: Alessandra Moscarelli, Pasquale Iozzo, Mariachiara Ippolito, Andrea Cortegiani.
Data curation: Alessandra Moscarelli, Pasquale Iozzo, Mariachiara Ippolito, Giulia Catalisano, Cesare Gregoretti, Antonino Giarratano, Enrico Baldi, Andrea Cortegiani.
Writing - original draft: Alessandra Moscarelli, Pasquale Iozzo, Mariachiara Ippolito, Enrico Baldi, Andrea Cortegiani.
Writing - review and editing: Giulia Catalisano, Cesare Gregoretti, Antonino Giarratano.
All the authors approved the final version of the manuscript and agreed to be personally accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
Acknowledgements
We would like to thank Dr. Salvatore Castello for his contribution to the creation of Fig. 1 and Fig. 2.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2020.08.097.
Appendix A. Supplementary data
Supplementary material
References
- 1.Link M.S., Berkow L.C., Kudenchuk P.J., Halperin H.R., Hess E.P., Moitra V.K., et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 2.Truhlář A., Deakin C.D., Soar J., Khalifa G.E.A., Alfonzo A., Bierens J.J.L.M., et al. European resuscitation council guidelines for resuscitation 2015. Section 4. Cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201. doi: 10.1016/j.resuscitation.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Piehl M., Brown R. Use of extreme position changes in acute respiratory failure. Crit Care Med. 1976;4:13–14. doi: 10.1097/00003246-197601000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Longhini F., Bruni A., Garofalo E., Navalesi P., Grasselli G., Cosentini R., et al. Helmet continuous positive airway pressure and prone positioning: a proposal for an early management of COVID-19 patients. Pulmonology. 2020;26:186–191. doi: 10.1016/j.pulmoe.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coppo A., Bellani G., Winterton D., Di Pierro M., Soria A., Faverio P., et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi E., Maria Sechi G., Mare C., Canevari F., Brancaglione A., Primi R., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edelson D.P., Sasson C., Chan P.S., Atkins D.L., Aziz K., Becker L.B., et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19. Circulation. 2020;141:e933–e943. doi: 10.1161/circulationaha.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 9.Wei J., Tung D., Sue S.H., Van Wu S., Chuang Y.C., Chang C.Y. Cardiopulmonary resuscitation in prone position: a simplified method for outpatients. J Chin Med Assoc. 2006;69:202–206. doi: 10.1016/S1726-4901(09)70219-9. [DOI] [PubMed] [Google Scholar]
- 10.Mazer S.P., Weisfeldt M., Bai D., Cardinale C., Arora R., Ma C., et al. Reverse CPR: a pilot study of CPR in the prone position. Resuscitation. 2003;57:279–285. doi: 10.1016/S0300-9572(03)00037-6. [DOI] [PubMed] [Google Scholar]
- 11.Atkinson M.C. The efficacy of cardiopulmonary resuscitation in the prone position. Crit Care Resusc. 2000;2:188–190. [PubMed] [Google Scholar]
- 12.Al Harbi M., Alattas K., Alnajar M., Albuthi M. Prone cardiopulmonary resuscitation in elderly undergoing posterior spinal fusion with laminectomy. Saudi J Anaesth. 2020;14:123–126. doi: 10.4103/sja.SJA_165_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mishra N., Singh S., Elayat A., Kaushal A. Cardiac arrest in the prone position caused by central venous cannulation-induced cardiac tamponade. Korean J Anesthesiol. 2019;72:394–395. doi: 10.4097/kja.19105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayorga-Buiza M.J., Rivero-Garvia M., Gomez-Gonzalez E., Marquez-Rivas J. Cardiac pulmonary resuscitation in prone position. The best option for posterior fossa neurosurgical patients. Paediatr Anaesth. 2018;28:746–747. doi: 10.1111/pan.13448. [DOI] [PubMed] [Google Scholar]
- 15.Burki A.M., Mahboob S., Fatima T. CPR in prone position during neurosurgery. Anaesth Pain Intensive Care. 2017;21:275–278. [Google Scholar]
- 16.Kaloria N., Bhagat H., Singla N. Venous air embolism during removal of bony spur in a child of split cord malformation. J Neurosci Rural Pract. 2017;8:483–484. doi: 10.4103/jnrp.jnrp_508_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee-Archer P.F., Chaseling B. Air embolism during posterior spinal fusion in a 10-year-old girl: a case report. A A Case Reports. 2017;8:307–309. doi: 10.1213/XAA.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 18.Pinheiro L.C., Carmona B.M., Fascio M.de.N.C., de Souza I.S.D., de Azevedo R.A.A., Barbosa F.T. Cardiac arrest after epidural anesthesia for a esthetic plastic surgery: a case report. Brazilian J Anesthesiol (English Ed) 2017;67:544–547. doi: 10.1016/j.bjane.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Taylor J.C.L., Buchanan C.C.R., Rumball M.J. Cardiac arrest during craniotomy in prone position. Trends Anaesth Crit Care. 2013;3:224–226. doi: 10.1016/j.tacc.2013.02.015. [DOI] [Google Scholar]
- 20.De Souza Gomes D.de.S., CDA Bersot. Cardiopulmonary resuscitation in the prone position. Open J Anesthesiol. 2012;02:199–201. doi: 10.4236/ojanes.2012.25045. [DOI] [Google Scholar]
- 21.Dooney N. Prone CPR for transient asystole during lumbosacral spinal surgery. Anaesth Intensive Care. 2010;38:212–213. [PubMed] [Google Scholar]
- 22.Pan Y., Qiu B., Yu F., Hu B. Fatal air embolism during endoscopic retrograde cholangio-pancreatography (ERCP): a case report. J Med Coll PLA. 2012;27:239–243. doi: 10.1016/S1000-1948(12)60024-0. [DOI] [Google Scholar]
- 23.Dumont T.M., Stockwell D.W., Horgan M.A. Venous air embolism: an unusual complication of atlantoaxial arthrodesis: case report. Spine. 2010;35:E1238–E1240. doi: 10.1097/BRS.0b013e3181f62600. [DOI] [PubMed] [Google Scholar]
- 24.Haffner E., Sostarich A.M., Fösel T. Erfolgreiche kardiopulmonale Reanimation in Bauchlage. Anaesthesist. 2010;59:1099–1101. doi: 10.1007/s00101-010-1785-8. [DOI] [PubMed] [Google Scholar]
- 25.Brock-Utne J.G. 2011. Case Studies of Near Misses in Clinical Anesthesia. [DOI] [Google Scholar]
- 26.Beltran S.L., Mashour G.A. Unsuccessful cardiopulmonary resuscitation during neurosurgery: is the supine position always optimal? Anesthesiology. 2008;108:163–164. doi: 10.1097/01.anes.0000296716.56374.49. [DOI] [PubMed] [Google Scholar]
- 27.Smelt W.L.H. Cardiac arrest during desflurane anaesthesia in a patient with Duchenne's muscular dystrophy. Acta Anaesthesiol Scand. 2005;49:268–269. doi: 10.1111/j.1399-6576.2004.00596.x. [DOI] [PubMed] [Google Scholar]
- 28.Chen H., Wong C., Ho S., Chang F., Hsu C., Wu C. A lethal pulmonary embolism during percutaneous Vertebroplasty. Anesth Analg. 2002;95:1060–1062. doi: 10.1213/01.ANE.0000025591.86476.F2. [DOI] [PubMed] [Google Scholar]
- 29.Miranda C.C., Newton M.C.M. Successful defibrillation in the prone position. Br J Anaesth. 2001;87:937–938. doi: 10.1093/bja/87.6.937. [DOI] [PubMed] [Google Scholar]
- 30.Brown J., Rogers J., Soar J. Cardiac arrest during surgery and ventilation in the prone position: a case report and systematic review. Resuscitation. 2001;50:233–238. doi: 10.1016/S0300-9572(01)00362-8. [DOI] [PubMed] [Google Scholar]
- 31.Reid J., Appleton P. A case of ventricular fibrillation in the prone position during back stabilisation surgery in a boy with Duchenne's muscular dystrophy. Anaesthesia. 1999;54:350–371. doi: 10.1046/j.1365-2044.1999.00835.x. [DOI] [PubMed] [Google Scholar]
- 32.Sutherland R., Winter R. Two cases of fatal air embolism in children undergoing scoliosis surgery. Acta Anaesthesiol Scand. 1997;41:1073–1076. doi: 10.1111/j.1399-6576.1997.tb04839.x. [DOI] [PubMed] [Google Scholar]
- 33.Dequin P.F.P., Hazouard E., Legras A., Lanotte R., Perrotin D. Cardiopulmonary resuscitation in the prone position: Kouwenhoven revisited. Intensive Care Med. 1996;22:1272–1282. doi: 10.1007/BF01709349. [DOI] [PubMed] [Google Scholar]
- 34.Gueugniaud P., Muchada R., Bertin-Maghit M., Griffith N., Petit P. Non-invasive continuous haemodynamic and PETCO 2 monitoring during peroperative cardiac arrest. Can J Anesth. 1995;42:910–913. doi: 10.1007/BF03011039. [DOI] [PubMed] [Google Scholar]
- 35.Kelleher A., Mackersie A. Cardiac arrest and resuscitation of a 6-month old achondroplastic baby undergoing neurosurgery in the prone position. Anaesthesia. 1995;50:348–350. doi: 10.1111/j.1365-2044.1995.tb04615.x. [DOI] [PubMed] [Google Scholar]
- 36.Tobias J., Mencio G., Atwood R., Gurwitz G. Intraoperative cardiopulmonary resuscitation in the prone position. J Pediatr Surg. 1994;29:1537–1538. doi: 10.1016/0022-3468(94)90208-9. [DOI] [PubMed] [Google Scholar]
- 37.Loewenthal A., De Albuquerque A., Lehmann-Meurice C., Otteni J. Efficacit du massage cardiaque externe chez une patiente en ddcubitus ventral. Ann Fr Anesth Reanim. 1993;12:587–589. doi: 10.1016/s0750-7658(05)80627-6. [DOI] [PubMed] [Google Scholar]
- 38.Sun W., Huang F., Kung K., Fan S., Chen T. Successful cardiopulmonary resuscitation of two patients in the prone position using reversed precordial compression. Anesthesiology. 1992;77:202–204. doi: 10.1097/00000542-199207000-00027. [DOI] [PubMed] [Google Scholar]
- 39.Albin M., Ritter R., Pruett C., Kalff K. Venous air embolism during lumbar laminectomy in the prone position: report of three cases. Anesth Analg. 1991;73:346–349. doi: 10.1213/00000539-199109000-00021. [DOI] [PubMed] [Google Scholar]
- 40.Ewah B., Calder I. Intraoperative death during lumbar discectomy. Br J Anaesth. 1991;66:721–723. doi: 10.1093/bja/66.6.721. [DOI] [PubMed] [Google Scholar]
- 41.Kalenda Z., Greuter P.N. Sitting or prone? Another argument for the latter. Acta Neurochir. 1982;61:173–179. doi: 10.1007/BF01740082. [DOI] [PubMed] [Google Scholar]
- 42.Lang S., Duncan P., Dupuis P. Fatal air embolism in an adolescent with Duchenne muscular dystrophy during Harrington instrumentation. Anesth Analg. 1989;69:132–134. [PubMed] [Google Scholar]
- 43.Lott C., Carmona F., Van de Voorde P., Lockey A., Kuzovlev A., Breckwoldt J., et al. Education: European resuscitation council COVID-19 guidelines. Notfall Und Rettungsmedizin. 2020;23:260–262. doi: 10.1007/s10049-020-00723-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guimaraes H., Timerman S., Rodrigues R., Polastri F., Fachini Vane M., Bittencourt Couto T., et al. Posicionamento Posicionamento para Ressuscitação Cardiopulmonar de Pacientes com Diagnóstico ou Suspeita de COVID-19-2020. Arq Bras Cardiol. 2020;114:1078–1087. doi: 10.36660/abc.20200548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.North T.H., Square T. Management of cardiac arrest during neurosurgery in adults. 2014. https://www.sbns.org.uk/index.php/download_file/view/805/559/ Available from.
- 46.Douma M.J., MacKenzie E., Loch T., Tan M.C., Anderson D., Picard C., et al. Prone Cardiopulmonary Resuscitation: A Rapid Scoping and Expanded Grey Literature Review for the covid-19 Pandemic. MedRxiv. 2020 doi: 10.1101/2020.05.21.20109710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bamford P., Denmade C., Newmarch C., Shirley P., Singer B., Webb S., et al. Guidance for: prone positioning in adult critical care. 2019. https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf Available from.
- 48.Kwon M.J., Kim E.H., Song I.K., Lee J.H., Kim H.S., Kim J.T. Optimizing prone cardiopulmonary resuscitation: identifying the vertebral level correlating with the largest left ventricle cross-sectional area via computed tomography scan. Anesth Analg. 2017;124:520–523. doi: 10.1213/ANE.0000000000001369. [DOI] [PubMed] [Google Scholar]
- 49.Cortegiani A., Ippolito M., Ingoglia G., Iozzo P., Giarratano A., Einav S. Update I. A systematic review on the efficacy and safety of chloroquine/hydroxychloroquine for COVID-19. J Crit Care. 2020 doi: 10.1016/j.jcrc.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ippolito M., Vitale F., Accurso G., Iozzo P., Gregoretti C., Giarratano A., et al. Medical masks and respirators for the protection of healthcare workers from SARS-CoV-2 and other viruses. Pulmonology. 2020 doi: 10.1016/j.pulmoe.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shao F., Xu S., Ma X., Xu Z., Lyu J., Ng M., et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material