Abstract
Purpose
To report the clinical outcomes after implantation of a pinhole supplementary implant (Xtrafocus, Morcher GmbH, Stuttgart, Germany) to correct fluctuating residual refraction after cataract surgery in a patient with a history of radial keratotomy (RK).
Observations
A 62-year-old patient who had radial keratotomy 22 years earlier, underwent uneventful bilateral cataract surgery using the ASCRS IOL-Calculator for post-RK. Postoperatively, the patient showed fluctuating subjective manifest refraction (MR) on both eyes. To correct the large fluctuating residual refractive error and subjectively worse visual acuity, Xtrafocus IOL was implanted in the right eye. One week later, the uncorrected distance visual acuity (UDVA) was already 0.1 logMAR and the patient stated to have stable vision. Three months after Xtrafocus implantation, the UDVA was −0.04 logMAR which did not improve with MR and the patient expressed high satisfaction, good subjective binocular contrast sensitivity, comparable visual field outcomes, and an elongated depth of focus.
Conclusions and Importance
The pinhole sulcus implant not only helped eliminate the fluctuation in residual refraction after cataract surgery, but also provided an elongated depth of focus without greatly affecting the visual field. The supplementary implantation of the Xtrafocus lens can offer an effective option for the treatment of instable refractive errors after cataract surgery in patients with a history of corneal surgery.
Keywords: Pinhole sulcus lens, Residual refraction, Radial keratotomy
1. Introduction
Radial keratotomy (RK) is a corneal refractive technique that was developed by Fyodorov et al.1 in the 1970s, but today the procedure is seldom performed. It involved placement of up to 16 radial incisions on the cornea to achieve a central flattening and reduction of the corneal power, thereby treating refractive errors. However, as the surgery was associated with a number of postoperative complications,2,3 it became replaced by more modern and predictable refractive procedures such as laser-assisted in situ keratomileusis (LASIK), laser epithelial keratomileusis (LASEK), or implantation of phakic intraocular lenses (PIOLs).
Today, surgeons face a particular challenge when patients who had been previously treated with RK present with symptomatic cataracts. The cornea's impaired stability may result in an intraoperative RK scar dehiscence4 or in a postoperative fluctuation in refractive error despite careful IOL power calculation.5
In cases of residual refraction, treatment options are also rather limited as the cornea had already been treated.6,7 Supplementary implantation of a sulcus-fixated supplementary IOL can be an option in such patients.8 In this study, we report the clinical outcomes after implantation of a sulcus-fixated pinhole lens to address the fluctuating residual refractive error after cataract surgery in a patient who had previously received bilateral RK.
1.1. Case report
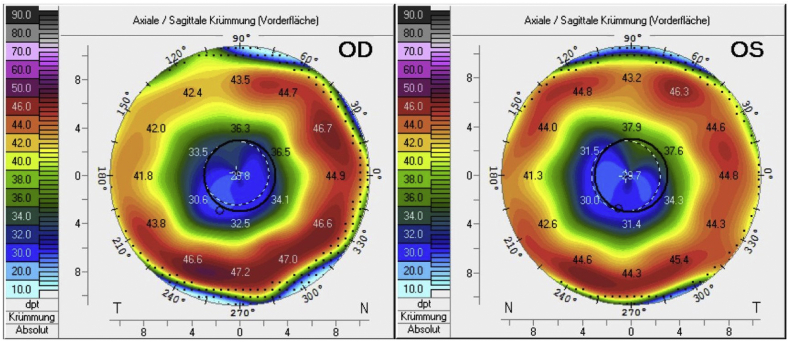
A 62-year-old male patient presented to our clinic with progressive worsening of vision in both eyes. He reported undergoing RK 22 years ago to correct myopia (initially approximately −6.0 D). On the right eye, UDVA was 0.6 logMAR and CDVA 0.4 logMAR with a MR of +4.00 DS/-2.00 DC x 82°. On the left eye, UDVA was 1.7 logMAR and CDVA 0.1 logMAR with a MR of +7.50 DS/-2.00 DC x 162°. The biometry data are presented in Table 1. Bilateral slit-lamp examination of the anterior segment revealed eight radial corneal incisions and cortico-nuclear cataract. Other than glaucomatous excavation of the optic nerves (cup-to-disc ratio of 0.6–0.7), the posterior segment did not show any pathological findings. Ocular dominance testing showed left eye dominance. The corneal topography using Pentacam (Version 6.09r39, OCULUS Optikgeräte GmbH, Wetzlar, Germany) (Fig. 1) showed central flattening of the cornea on both eyes.
Table 1.
Biometry data before cataract surgery.
| Right Eye | Left Eye | |
|---|---|---|
| Keratometry (D) | ||
| D1 | 29.97 at 49° | 30.66 at 166° |
| D2 | 32.17 at 139° | 32.35 at 76° |
| Cylinder (D) | −2.20 at 49° | −1.69 at 166° |
| Anterior Chamber Deptha(mm) | 3.00 | 3.22 |
| Axial Length (mm) | 26.45 | 26.52 |
From corneal epithelium to lens.
Fig. 1.
Corneal topography of both eyes with considerably flattened central cornea after radial keratotomy.
Cataract surgery was recommended and performed on both eyes with no intraoperative complications. The ASCRS IOL Calculator (Version 4.8) for post-RK eyes was used to calculate the appropriate IOL power. On the right eye, the mean IOL power suggested by the ASCRS IOL Calculator was 29.38 D (Table 2) and a monofocal aspheric IOL (TECNIS® PCB00, Johnson&Johnson Vision, Jacksonville, FL, USA) with a power of 29.0 D (target refraction of +0.18 D) was implanted. On the left eye, the mean IOL power suggested by the ASCRS IOL Calculator was 29.25 D (Table 2) and the same monofocal lens with a power of 29.0 D (target refraction of −0.32 D) was implanted.
Table 2.
Calculated intraocular lens powers.
| IOL Power (D) |
||
|---|---|---|
| Right Eye | Left Eye | |
| ASCRS IOL-Calculator | ||
| based on IOLMaster | 29.71 | 28.87 |
| based on Barrett-True K | 29.05 | 29.64 |
| Mean IOL Power | 29.38 | 29.25 |
| IOLMaster 700 | ||
| Holladay 1 | 26.50 | 25.50 |
| SRK/T | 25.50 | 25.00 |
| Holladay 2 | 26.50 | 26.00 |
| Haigis | 29.00 | 28.50 |
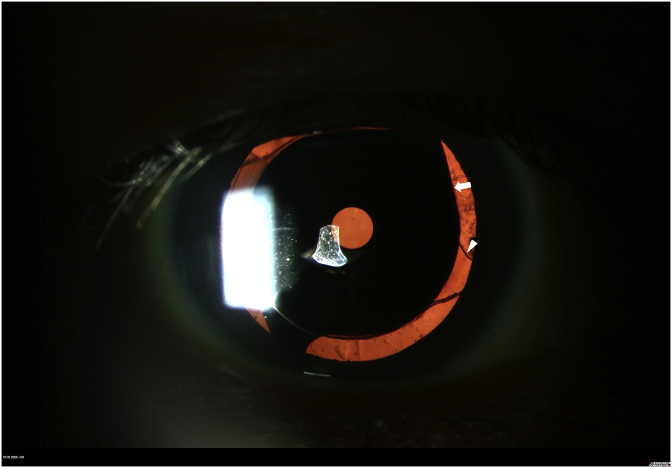
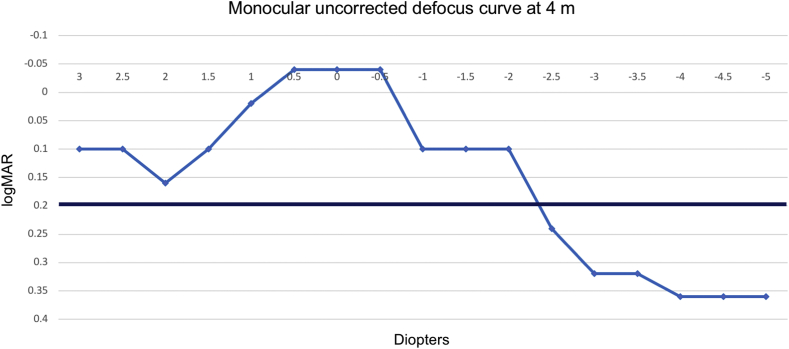
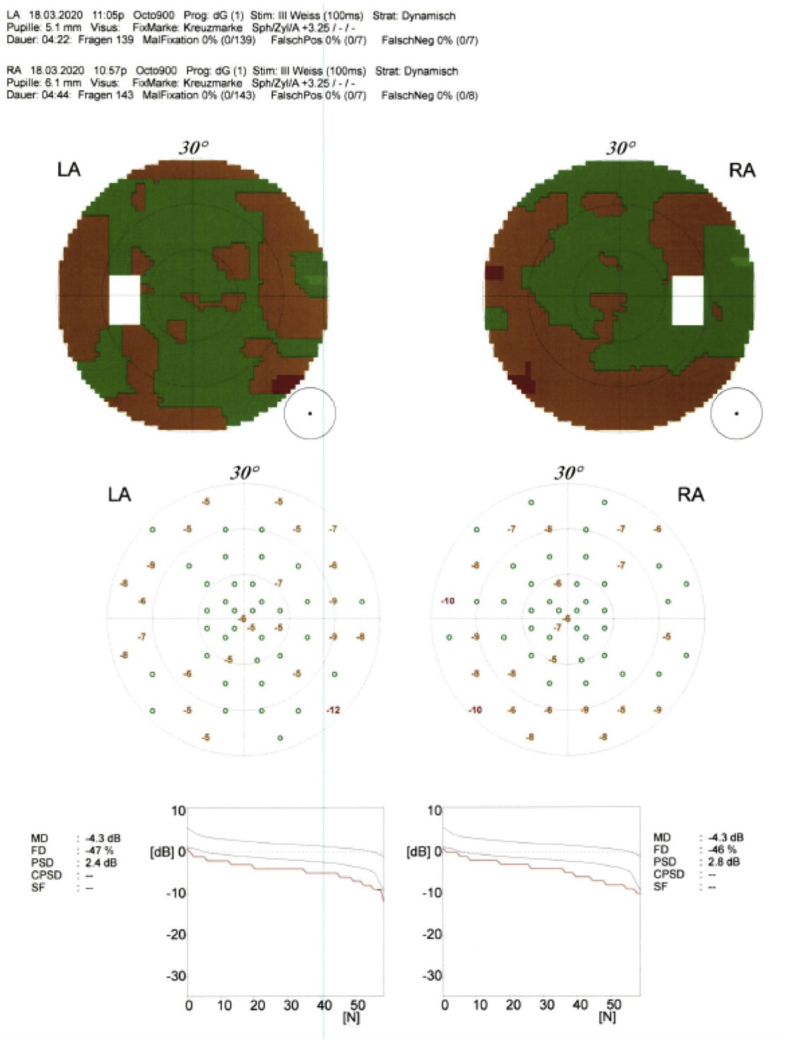
Four months after cataract surgery, the UDVA values were 0.34 and 0.38 logMAR on right and left eyes, respectively. However, both eyes showed considerable fluctuation in subjective refraction (Table 3). Implantation of a monofocal or toric supplementary IOL was planned to address the subjectively worse visual acuity and the considerable fluctuation in manifest refraction on the right eye. As the subjective refraction did not stay stable over more than three consecutive attempts at several different time periods, an accurate secondary IOL power calculation could not be performed. Therefore, we recommended a secondary implantation of the sulcus-fixated pinhole Xtrafocus lens (Morcher GmbH, Stuttgart, Germany), for which a stable MR is not needed as the pinhole lens has no power. This was performed without any intraoperative complications. Following the manufacturer's recommendations, the supplementary lens was implanted in a vertical position, with points of maximum haptic extension at 6 and 12 o'clock (Fig. 2). Three-months after the Xtrafocus lens implantation, the UDVA on the right eye was −0.04 logMAR and subjective refraction did not improve the visual acuity. The posterior segment could be visualized without any difficulty (Fig. 3). Fig. 4 shows the monocular uncorrected defocus curve of the right eye. The visual field examination results using the Octopus 900 perimeter (PeriData for Windows 3.5; Haag-Streit Deutschland GmbH, Wedel, Germany) at 3-months postoperatively are shown in Fig. 5. The contrast sensitivity testing outcomes using the CSV-1000E (VectorVision, Greenville, OH, USA) at 3-months postoperatively are shown in Fig. 6.
Table 3.
Fluctuation in manifest refraction after cataract surgery.
| Time after cataract surgery | Manifest Refraction with Visual Acuity (logMAR) |
|
|---|---|---|
| Right Eye | Left Eye | |
| 4 Months | +1.00–1.00 × 30° (0.16) | +1.50–3.75 × 165° (0.04) |
| 7 Months | +0.75–1.00 × 70° (0.10) | +1.00–1.00 × 30° (0.10) |
| 9 Months | +2.00–1.00 × 63° (0.10) | +1.75–3.00 × 165° (0.10) |
| 11 Months | +2.00–1.00 × 63° (0.10) | +1.00–2.00 × 167° (0.10) |
| 12 Months | +0.75–1.50 × 58° (0.10) | +1.00–2.75 × 168° (0.10) |
Fig. 2.
Slit-lamp photograph of the Xtrafocus supplementary implant (white arrow) in front of a monofocal intraocular lens (white arrowhead).
Fig. 3.
Fundus photograph of the right eye three months after implantation of the Xtrafocus supplementary implant.
Fig. 4.
Monocular uncorrected defocus curve three months after implantation of the Xtrafocus implant.
Fig. 5.
Visual field results of both eyes three months after Xtrafocus implantation.
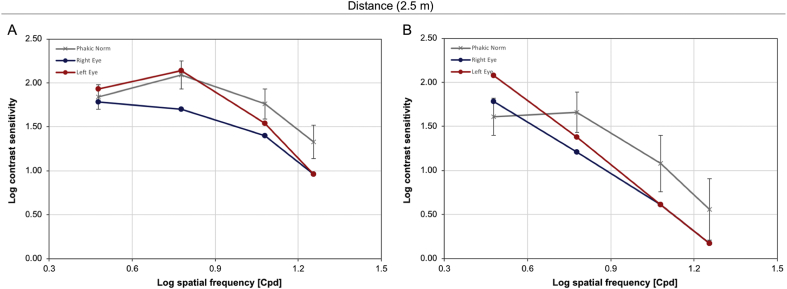
Fig. 6.
Photopic (A) and mesopic (B) contrast sensitivity levels of both eyes compared to normative values of phakic population three months after Xtrafocus implantation in the right eye. Cpd = cycles per degree.
Overall, the patient expressed high satisfaction and good binocular uncorrected visual acuity, stating that he no longer desires a correction for the left eye.
2. Discussion
We implanted the Xtrafocus lens to address the fluctuating residual refractive error after cataract surgery in a patient who had undergone RK.
Residual refractive errors are frequently seen after RK5,7,9 and numerous studies have looked into the possible causes. There are reports of post-RK patients showing diurnal variations in refraction, which would mean that multiple refraction attempts at different time of the day would be necessary to achieve accurate results.10 Delayed wound healing or intraoperative opening of the radial incisions have also been discussed as possible factors.9,11 The radial incisions are intended to alter (and flatten) the cornea and the resulting structural instability and can induce higher-order aberrations, undermining the visual quality.12 In addition, performing a cataract surgery may further flatten the central cornea and amplify the hyperopic shift.11,13
The main challenge, however, lies in the biometric inaccuracy of measuring a cornea with surgically altered curvature.7,11,12 As the radial incisions cause central flattening of the cornea, the corneal refractive power is often overestimated, leading to underestimation of the IOL power which in turn can lead to hyperopic surprises.7,11, 12, 13 Likewise, a precise prediction of the effective lens position can be difficult.11, 12, 13 Therefore, usage of the correct IOL formula is crucial in achieving optimal refractive results. The ASCRS post-RK calculator7,14 or the Holladay II formula based on the Holladay IOL Consultant software12 have proved useful. While biometry data prior to RK can help optimize the IOL power estimation, often these are not available.7 In this study, we used the ASCRS post-RK calculator to calculate the appropriate lens power, and it suggested 29.38 D and 29.25 D, respectively, for right and left eyes. These were higher values than those indicated by the Holladay 1, SRK®/T, Holladay 2, or the IOL-Master 700 formulae; suggesting that these calculations would have led to a greater postoperative hyperopic shift (Table 2). Interestingly, the Haigis formula provided values that were similar to those suggested by the ASCRS calculator (Table 2).
Despite meticulous preoperative planning, surgeons may still be confronted by residual, postoperative refractive errors and it was the case in this patient, who showed a considerable fluctuation in refraction on both eyes even one year after cataract surgery (Table 3). There are different approaches to address this complication. One may consider a laser refractive surgery for a corneal “touch-up”.6,14 This is deemed to be accurate, has high predictability and as it is not an intraocular procedure it avoids the risks of an invasive procedure.14,15 However, in post-RK patients, considering the fact that the cornea had already been treated this option is possible yet challenging.16 This leaves the options of IOL exchange or secondary implantation of a supplementary lens into the sulcus.7,14 While the former always remains a possibility, it is more invasive and bears the risk of intraoperative complications such as capsular bag rupture or zonular damage.17 The latter, in contrast, is relatively easy perform, more accurate, and even reversible.14,17
In contrast to “piggybacking” of IOLs, the idea of which was to implant a second standard IOL in the capsule anterior to an already-implanted IOL,18,19 supplementary IOLs are designed to be implanted into the sulcus and not the capsular bag.20 In Europe, such supplementary IOLs have been already available for ten years21 and they are specifically intended to avoid complications that were related to piggyback IOLs, such as glaucoma, pigmentary dispersion, or inter-lenticular opacification (ILO), thanks to their convex-concave optic configuration to broaden the space between the two IOLs for ILO prevention, large diameter to avoid optic capture or decentration, and rounded edge profile to minimize the risk of contact between the iris and the IOL.20
Studies have reported the clinical efficacy of such supplementary IOLs.7,22, 23, 24, 25 Basarir et al. implanted sulcus-fixated supplementary IOLs in 10 eyes of 10 patients to correct pseudophakic refractive errors and reported that all were within ±0.50 D of emmetropia and showed stable refraction in a follow-up period of up to 15 months.22 We implanted a Rayner 653L supplementary IOL to treat a residual refractive error of +5.00 DS/-1.00 DC x 45° after cataract surgery in an RK patient and observed good results, achieving CDVA of 0.10 logMAR with a MR of 0.00 DS/-0.50 DC x 60° at 3 months postoperatively.7 Multifocal supplementary IOLs can also be an option for patients who desire to be spectacle-independent after cataract surgery with monofocal IOLs.23, 24, 25, 26 Khan et al. implanted a bifocal Sulcoflex IOL in pseudophakic patients and reported UDVA of 0.1 logMAR or better and UNVA of N6 (Jaeger 4) or better (four eyes of four patients).23 As part of a duet-procedure,25 we implanted monofocal IOLs together with trifocal supplementary Sulcoflex IOLs in an 18-year-old patient who had bilateral cataract due to hyperferritinemia cataract syndrome and observed uncorrected binocular far (6 m), intermediate (80 cm), and near visual acuity (40 cm) values of 0.0 logMAR, 0.0 logMAR, and 0.0 logMAR, respectively, at 3-months postoperatively.26
In the present case, we corrected the residual refractive error by implanting the Xtrafocus lens, which is an open-loop lens with an optic-haptic angulation of 14°, and a 6.00 mm black occluded optic that has a pinhole 1.3 mm central opening. The lens is based on the well-established optical principles of a pinhole, which prevents the peripheral light rays from entering the eye and minimizes the effects of optical aberrations, increasing the visual quality and depth of focus.27 As a supplementary lens, the Xtrafocus lens also has specific features to prevent complications related to piggyback IOLs, which were elaborated in detail in a previous study.28
Trindade et al. implanted the Xtrafocus sulcus implant in pseudophakic patients with irregular corneal astigmatism resulting from keratoconus, traumatic corneal laceration, RK, and penetrating keratoplasty, and observed statistically significant improvement of median CDVA from 20/200 (range 20/800 to 20/60) preoperatively to 20/50 (range 20/200 to 20/20) in mean follow-up period of 22.1 months (24 eyes of 21 patients).28 In our case, the Xtrafocus IOL was chosen for this patient for two main reasons: first, while implantation of other supplementary multifocal lenses would also have been possible, stable MR values are necessary to calculate the exact IOL power. Implanting such lenses in a patient with unstable refraction may lead to another postoperative residual refractive error. A pinhole lens, on the other hand, has no dioptric power and is therefore less dependent on the stability of subjective refraction. Secondly, a pinhole optic's high tolerance to corneal aberrations and astigmatism can also be advantageous in cases of fluctuating refraction.28, 29, 30, 31
Three months after implantation of the Xtrafocus lens, our patient no longer showed any residual refractive error, with UDVA of −0.04 logMAR. The pinhole IOL also provided an elongated depth of focus, with visual acuity of 0.2 logMAR or better from +3.0 to −2.0 D (Fig. 4). There are currently no peer-reviewed studies with visual field results after implantation of the Xtrafocus IOL. In a video presented at the Annual Meeting of the ASCRS in 2017, Trindade et al. reported that the Xtrafocus lens led to a slight reduction of overall sensitivity of approximately 2 dB, which was of no clinical relevance (24 eyes with mean follow-up time of 22 months).32 Tsaousis et al. hypothesized that the size of the central opening in Xtrafocus IOL may not be small enough to cause significant visual field loss.33 Our results did not show any apparent changes in the visual field secondary to the pinhole lens implantation, with equal mean defect (MD) values of −4.3 dB on both eyes (Fig. 5). In our patient, the central 1.3 mm opening allowed for a good visualization of the posterior segment (Fig. 3). However, it cannot be ruled out that a pinhole implant may hinder detailed assessment of pathologies in peripheral retina.
Our patient's photopic (Fig. 6A) and mesopic (Fig. 6B) contrast sensitivity levels were partially below the normative values of phakic population in both eyes. While reduced contrast sensitivity is also a known complication after RK,34 it has been reported that objective measurement of contrast levels after RK does not always reflect the patients' actual visual perception in daily life.34 There are also no studies that assessed the contrast sensitivity levels after Xtrafocus lens implantation in pseudophakic patients after RK for comparison. Agarwal et al. reported implanting the Xtrafocus lens in a pseudophakic patient for correction of residual irregular astigmatism and traumatic mydriasis.35 At one-week postoperatively, the UDVA improved from 20/100 preoperatively to 20/30, and uncorrected intermediate and near visual acuities were to 20/40 and J4, respectively.35 However, the patient complained of such poor vision in dim illumination, so that the sulcus implant had to be explanted again.35 In our study, the patient did indicate monocularly reduced vision on the right eye especially at night, but he stated that he can still see well binocularly and did not wish an explantation.
3. Conclusions
The supplementary implantation of the Xtrafocus pinhole device not only led to correction of postoperative fluctuation in residual refraction after cataract surgery, but also provided an elongated depth of focus without greatly affecting the visual field or contrast sensitivity. Therefore, this technique presents an effective option for treatment of instable refractive errors after cataract surgery in patients with a history of corneal refractive surgery.
Patient consent
Patient consent to publish this case report was not obtained. This report does not contain any information that could lead to identification of the patient. Retrospective review of this case report was done in accordance with the Declaration of Helsinki.
Acknowledgements and disclosures
The authors thank D. J. Munro for his contributions to the review of the pre-publication report. All authors report no relevant financial disclosures. All authors attest that they meet the current ICMJE criteria for Authorship. The project was funded by the Klaus Tschira Foundation, Heidelberg, Germany.
Contributor Information
Hyeck-Soo Son, Email: HyeckSoo.Son@med.uni-heidelberg.de.
Ramin Khoramnia, Email: Ramin.Khoramnia@med.uni-heidelberg.de.
Christian Mayer, Email: Christian.Mayer@med.uni-heidelberg.de.
Grzegorz Labuz, Email: Grzegorz.Labuz@med.uni-heidelberg.de.
Timur M. Yildirim, Email: Timur.Yildirim@med.uni-heidelberg.de.
Gerd U. Auffarth, Email: http://www.ivcrc.com, http://www.djapplelab.com, Gerd.Auffarth@med.uni-heidelberg.de.
References
- 1.Fyodorov N.N., Durnev V.V. Anterior keratotomy method application with the purpose of surgical correction of myopia. In: Fyodorov S.N., editor. Pressing Problems of Ophthalmosurgery. Moscow Research Institute of Ocular Microsurgery; Moscow: 1977. pp. 47–48. [Google Scholar]
- 2.Deitz M.R., Sanders D.R., Raanan M.G. Progressive hyperopia in radial keratotomy. Long-term follow-up of diamond-knife and metal-blade series. Ophthalmology. 1986;93:1284–1289. [PubMed] [Google Scholar]
- 3.Waring G.O., 3rd, Lynn M.J., McDonnell P.J. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994;112:1298–1308. doi: 10.1001/archopht.1994.01090220048022. [DOI] [PubMed] [Google Scholar]
- 4.Freeman M., Kumar V., Ramanathan U.S., O'Neill E. Dehiscence of radial keratotomy incision during phacoemulsification. Eye. 2004;18:101–103. doi: 10.1038/sj.eye.6700526. [DOI] [PubMed] [Google Scholar]
- 5.Potvin R., Hill W. New algorithm for post-radial keratotomy intraocular lens power calculations based on rotating Scheimpflug camera data. J Cataract Refract Surg. 2013;39:358–365. doi: 10.1016/j.jcrs.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Sáles C.S., Manche E.E. Managing residual refractive error after cataract surgery. J Cataract Refract Surg. 2015 Jun;41(6):1289–1299. doi: 10.1016/j.jcrs.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Son H.S., Auffarth G.U., Xia A., Yildirim T.M., Mayer C.S., Khoramnia R. [Solutions for IOL-calculation and implantation in patients after radial keratotomy]. [Article in German] Klin Monbl Augenheilkd. 2019 Jul 2 doi: 10.1055/a-0916-8816. [DOI] [PubMed] [Google Scholar]
- 8.Meyer J.J., McGhee C.N.J. Supplementary, sulcus-fixated intraocular lens in the treatment of spherical and astigmatic refractive errors in pseudophakic eyes after keratoplasty. Cornea. 2015;34:1052–1056. doi: 10.1097/ICO.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 9.Turnbull A.M.J., Crawford G.J., Barrett G.D. Methods for intraocular lens power calculation in cataract surgery after radial keratotomy. Ophthalmology. 2020;127:45–51. doi: 10.1016/j.ophtha.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Geggel H.S. Intraocular lens power selection after radial keratotomy: topography, manual, and IOLMaster keratometry results using Haigis formulas. Ophthalmology. 2015;122:897–902. doi: 10.1016/j.ophtha.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Koch D.D., Liu J.F., Hyde L.L., Rock R.L., Emery J.M. Refractive complications of cataract surgery after radial keratotomy. Am J Ophthalmol. 1989 Dec 15;108(6):676–682. doi: 10.1016/0002-9394(89)90860-x. [DOI] [PubMed] [Google Scholar]
- 12.Baartman B.J., Karpuk K., Eichhorn B. Extended depth of focus lens implantation after radial keratotomy. Clin Ophthalmol. 2019 Jul 30;13:1401–1408. doi: 10.2147/OPTH.S208550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen L., Mannis M.J., Salz J.J., Garcia-Ferrer F.J., Ge J. Analysis of intraocular lens power calculation in post-radial keratotomy eyes. J Cataract Refract Surg. 2003 Jan;29(1):65–70. doi: 10.1016/s0886-3350(02)01693-0. [DOI] [PubMed] [Google Scholar]
- 14.Abdelghany A.A., Alió J.L. Surgical options for correction of refractive error following cataract surgery. Eye Vis (Lond) 2014;1:2. doi: 10.1186/s40662-014-0002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernández-Buenaga R., Alió J.L., Pérez Ardoy A.L., Quesada A.L., Pinilla-Cortés L., Barraquer R.I. Resolving refractive error after cataract surgery: IOL exchange, piggyback lens, or LASIK. J Refract Surg. 2013 Oct;29(10):676–683. doi: 10.3928/1081597X-20130826-01. [DOI] [PubMed] [Google Scholar]
- 16.Chhadva P., Cabot F., Galor A., Yoo S.H. Long-Term outcomes of radial keratotomy, laser in situ keratomileusis, and astigmatic keratotomy performed consecutively over a period of 21 years. Case Rep Ophthalmol Med. 2015;2015:592495. doi: 10.1155/2015/592495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El Awady H.E., Ghanem A.A. Secondary piggyback implantation versus IOL exchange for symptomatic pseudophakic residual ametropia. Graefes Arch Clin Exp Ophthalmol. 2013;251(7):1861–1866. doi: 10.1007/s00417-013-2283-x. [DOI] [PubMed] [Google Scholar]
- 18.Gayton J.L., Sanders V.N. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993;19:776–777. doi: 10.1016/s0886-3350(13)80349-5. [DOI] [PubMed] [Google Scholar]
- 19.Holladay J.T., Gills J.P., Leidlein J., Cherchio M. Achieving emmetropia in extremely short eyes with two piggyback posterior chamber intraocular lenses. Ophthalmology. 1996 Jul;103(7):1118–1123. doi: 10.1016/s0161-6420(96)30558-7. [DOI] [PubMed] [Google Scholar]
- 20.Manzouri B., Dari M., Claoué C. Supplementary IOLs: monofocal and multifocal, their applications and limitations. Asia Pac J Ophthalmol (Phila) 2017;6:358–363. doi: 10.22608/APO.2017110. [DOI] [PubMed] [Google Scholar]
- 21.Kahraman G., Amon M. New supplementary intraocular lens for refractive enhancement in pseudophakic patients. J Cataract Refract Surg. 2010;36(7):1090–1094. doi: 10.1016/j.jcrs.2009.12.045. [DOI] [PubMed] [Google Scholar]
- 22.Basarir B., Kaya V., Altan C., Karakus S., Pinarci E.Y., Demirok A. The use of a supplemental sulcus fixated IOL (HumanOptics Add-On IOL) to correct pseudophakic refractive errors. Eur J Ophthalmol. 2012 Nov-Dec;22(6):898–903. doi: 10.5301/ejo.5000156. [DOI] [PubMed] [Google Scholar]
- 23.Khan M.I., Muhtaseb M. Performance of the Sulcoflex piggyback intraocular lens in pseudophakic patients. J Refract Surg. 2011 Sep;27(9):693–696. doi: 10.3928/1081597X-20110512-01. [DOI] [PubMed] [Google Scholar]
- 24.Huerva V. Piggyback multifocal IOLs for a hyperopic-presbyopic surprise after cataract surgery in high myopic patients. Contact Lens Anterior Eye. 2014;37:57–59. doi: 10.1016/j.clae.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 25.Yildirim T.M., Auffarth G.U., Son H.S., Mayer C.S., Tandogan T., Khoramnia R. Klin Monbl Augenheilkd; 2019 Jul 2. [Duet Procedure in High Myopia to Achieve Reversible Multifocality]. [Article in German] [DOI] [PubMed] [Google Scholar]
- 26.Khoramnia R., Yildirim T.M., Son H.S., Labuz G., Mayer C.S., Auffarth G.U. [Duet procedure to achieve reversible trifocality]. [Article in German] Ophthalmologe. 2020 Apr 15 doi: 10.1007/s00347-020-01096-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Charman W.N. Pinholes and presbyopia: solution or sideshow? Ophthalmic Physiol Optic. 2019;39:1–10. doi: 10.1111/opo.12594. [DOI] [PubMed] [Google Scholar]
- 28.Trindade C.C., Trindade B.C., Trindade F.C., Werner L., Osher R., Santhiago M.R. New pinhole sulcus implant for the correction of irregular corneal astigmatism. J Cataract Refract Surg. 2017;43:1297–1306. doi: 10.1016/j.jcrs.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 29.Son H.S., Yildirim T., Khoramnia R., Labuz G., Mayer C., Auffarth G.U. Implantation of a small-aperture intraocular lens and a partial aniridia implant in eyes with traumatic iris defects. Am J Ophthalmol Case Rep. 2020;18:100673. doi: 10.1016/j.ajoc.2020.100673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ang R.E. Comparison of tolerance to induced astigmatism in pseudophakic eyes implanted with small aperture, trifocal, or monofocal intraocular lenses. Clin Ophthalmol. 2019;13:905–911. doi: 10.2147/OPTH.S208651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Son H.S., Khoramnia R., Yildirim T.M., Baur I., Labuz G., Auffarth G.U. Functional outcomes and reading performance after combined implantation of a small-aperture lens and a segmental refractive bifocal lens. J Refract Surg. 2019;35:551–558. doi: 10.3928/1081597X-20190806-02. [DOI] [PubMed] [Google Scholar]
- 32.Trindade C.L.C., Trindade F.C., Trindade B.C. Tiny hero against the evil axis. Video presented at the annual meeting of the American society of cataract and refractive surgery (ASCRS) 2017. , Los Angeles, CA, USA. Available at: http://ascrs2017.conferencefilms.com/abstractawards.wcs.
- 33.Tsaousis K.T., Werner L., Trindade C.L.C., Guan J., Li J., Reiter N. Assessment of a novel pinhole supplementary implant for sulcus fixation in pseudophakic cadaver eyes. Eye. 2018;32:637–645. doi: 10.1038/eye.2017.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghaith A.A., Daniel J., Stulting R.D., Thompson K.P., Lynn M. Contrast sensitivity and glare disability after radial keratotomy and photorefractive keratectomy. Arch Ophthalmol. 1998;116:12–18. doi: 10.1001/archopht.116.1.12. [DOI] [PubMed] [Google Scholar]
- 35.Agarwal P., Navon S.E., Subudhi P., Mithal N. Persistently poor vision in dim illumination after implantation of Xtrafocus small-aperture IOL (Morcher) BMJ Case Rep. 2019;12(11) doi: 10.1136/bcr-2019-232473. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]