Abstract
Research shows that schools can make a positive impact on children’s nutritional outcomes. However, it is also reported that schools and teaching staff note many barriers, which may restrict nutritional education programming and delivery. This is concerning, considering the view that teachers are the key agents for promoting health and nutrition within schools. The purpose of the updated systematic review and meta-analysis was to ascertain the impact that nutrition education programs have on elementary-aged students’ energy intake, fruit, vegetable, sugar consumption and nutritional knowledge. A systematic literature search was conducted using electronic databases (The Cochrane Central Register of Controlled Trials (CENTRAL); A + Education; ERIC; PsycINFO; MEDLINE; ProQuest Central, Journals@Ovid and SAGE Health Sciences Full-Text Collection) from 1990 to 31st October 2018. This process yielded 34 studies for inclusion in this systematic review and meta-analysis. Of these studies, seven studies had a focus on energy intake, five had a focus on sugar consumption, 21 of the studies looked at fruit and vegetable consumption and 13 studies focused on nutritional knowledge. The results suggest that the teaching of nutrition education in elementary schools by qualified teachers can make an important contribution to the knowledge and dietary habits of children. The small and medium effect sizes indicate that prudent, evidence-based decisions need to be made by policy makers and pedagogues as to the teaching strategies employed when delivering nutrition education programs to elementary-aged students.
The review is reported in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (van Sluijs et al., 2007).
Abbreviations: CI, Confidence Interval; ERIC, Education Resources Information Center; ES, Effect Size; RCT, Randomised Control Trial; SD, Standard Deviation; SE, Standard Error
Keywords: Nutrition review, Meta-analysis, Elementary students
1. Introduction
Nutrition‐related health conditions, such as obesity, Type 2 diabetes, and hypertension are becoming prevalent in children (Goran et al., 2003, Kelsey et al., 2014). Children with these conditions often suffer physical discomfort, ill-health, lower self‐esteem, poorer academic outcomes and negative socio-emotional (van Geel et al., 2014, Reilly and Kelly, 2011). Furthermore, the risk of these conditions tracking into adulthood is high (United Nations Educational Scientific and Cultural Organization, 2013). As such, there have been international calls to focus on prevention through nutrition education in schools (World Health Organization, 2012, Story et al., 2009). Schools are ideal settings for preventive nutrition education efforts targeting children due to their reach, structure and cost effectiveness (Graziose et al., 2017, Dudley et al., 2015). Two recent systematic reviews and meta-analysis suggests nutrition education programs delivered in elementary schools can positively influence children's energy intake, fruit and vegetable consumption, sugar consumption and nutritional knowledge, particularly those programs embedding experiential learning strategies and cross-curricular approaches, engaging parents by means of face-to-face sessions and assuring fidelity by training teachers or recruiting trained experts to support the delivery of the intervention (Murimi et al., 2018, Peralta et al., 2016).
Despite research showing that schools can make a positive impact on children’s nutritional outcomes, it is also reported that schools and teaching staff note many barriers that restrict nutritional education programming and delivery. First, nutrition education is often seen as unnecessary because the content is not included on standardized tests. Second, elementary school teaching staff do not have access to appropriate resources and may not have the expertise, motivation or capacity to deliver evidence-based nutrition education (Dudley et al., 2015). Third, preservice teachers only receive limited training in nutrition education during their tertiary studies (de Vlieger et al., 2019). Finally, providing professional learning for teachers is time consuming and often requires financial investment that may not align with the school’s professional learning goals (Porter et al., 2018). To overcome these barriers, schools and teachers have sought community organizations, who are experts in nutrition education, to deliver nutrition education programs in elementary schools (Moher et al., 2009). This is concerning, considering the educative view that qualified teachers are the key agents for promoting health and nutrition within schools (World Health Organization, 2012).
To emphasise the importance and effect of elementary school nutrition education programs on children’s energy intake, fruit, vegetable and sugar consumption and nutritional knowledge, and to capture the exponential growth of studies reporting on elementary school nutrition education programs in the previous five years, an updated systematic review and meta-analysis was undertaken (Murimi et al., 2018). The purpose of the updated systematic review and meta-analysis was to ascertain the impact that nutrition education programs have on elementary-aged students’ energy intake, fruit, vegetable, sugar consumption and nutritional knowledge by widening the search through increasing the number of inclusion criteria and reviewing data from more recent studies.
2. Materials and methods
A systematic literature search was conducted using electronic databases (The Cochrane Central Register of Controlled Trials (CENTRAL); A+ Education; ERIC; PsycINFO; MEDLINE; ProQuest Central, Journals@Ovid and SAGE Health Sciences Full-Text Collection) from 1990 to 31st October 2018.
The search strategy included the use of terms in four broad categories: (i) participants; (ii) delivery; (iii) strategies; and (iv) design. The title and abstract fields were searched using the following terms:
-
1.
primary student* or primary school* or elementary student* or elementary school* or child* or school-based* and
-
2.
teach* or class* or health educ* or nutrition educ* or healthy eat* or curricul* or reward* or nutritional intervention or education program* and
-
3.
nutrition* or energy or cook* or food* or fruit* or vegetable* or sugar* or kilojoule* or calorie* or eating or diet* and
-
4.
test or RCT or randomi* or control or trial or evaluat* or quasi-exper* or cluster or intervention*.
Reference lists of included studies were manually searched for additional articles.
2.1. Inclusion and exclusion criteria
Studies were included if they: (1) targeted elementary-aged children’s nutritional consumption or knowledge; (2) employed a nutritional education program taught by an elementary school teacher; and (3) reported nutritional consumption and/or knowledge outcomes using independent group difference values.
2.2. Study selection, data extraction and analysis
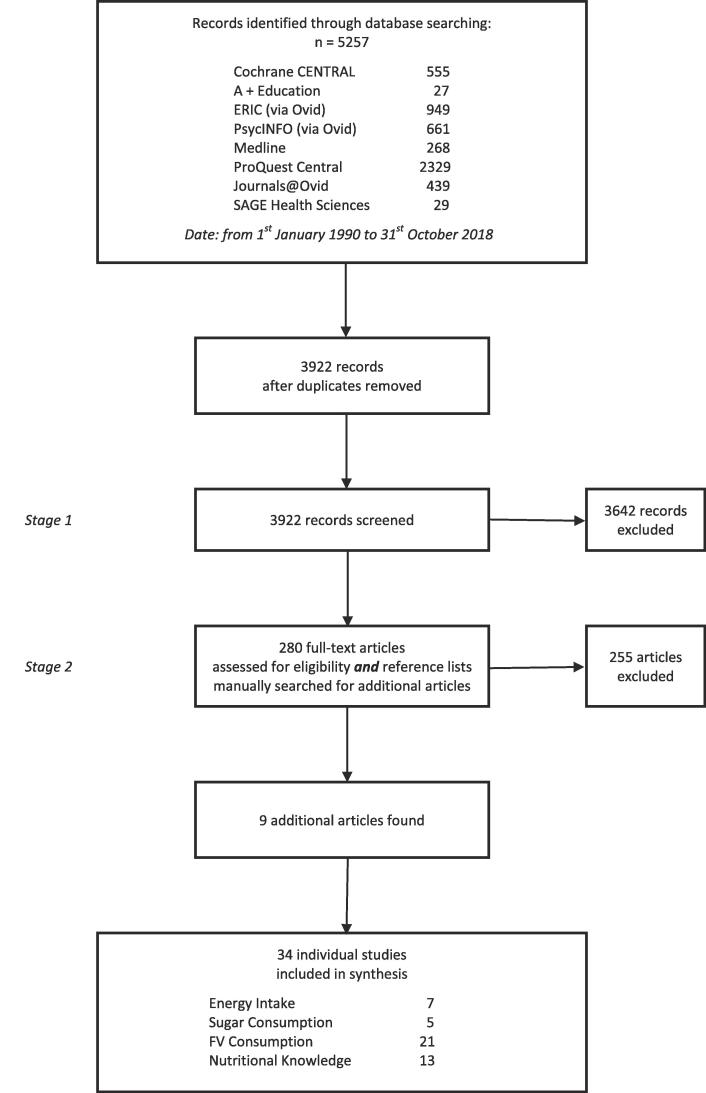
After duplicate deletion, one author (TW) initially screened all articles based on title and abstracts for preliminary inclusion (Stage 1); before screening remaining articles by full text based on inclusion criteria (Stage 2). In cases where there was uncertainty, a second reviewer (DD) assessed the article and consensus was reached by discussion. See Fig. 1 for an overview of this process.
Fig. 1.
Flow of information through the different phases of the systematic review.
The standardised mean difference score was calculated for each stated variable by using Cohen’s d. The pooled ES was estimated by using a random-effects model based on the DerSimonian and Laird (van Sluijs et al., 2007) method. We assessed and reported heterogeneity across studies by using the following statistical analyses. 1. The Q-statistic provided a test of the null hypothesis as to whether all studies share a common effect size; 2.the I2 statistic reports the proportion of the observed variance that are indicative of changes in true effect sizes rather than sampling error; 3.T2 is the variance of true effect sizes; and 4. Prediction interval is range of true effect size for 95% of all samples observed.
Classic Fail Safe N and Trim and Fill (Collaboration and Fail-safe, 2011) methods were used to assess publication bias. Studies were only included in the meta-analysis if they provided complete data for pre- and post-intervention measurements and included a control or comparison group.
In addition, the following statistical assumptions were applied: (1) when two cohorts were included in studies, their data were investigated as combined samples; (2) when two or more tests measuring the same variable were included in the studies, the combined effect size at the study level was used; (3) when two or more learning outcomes were used, the results were treated as independent samples; and (4) when two or more follow-up measurements were reported, only the last measurement was considered.
Comprehensive Meta-Analysis software, version 3 (Biostat, New York, NY) was used to perform all Statistical analyses.
2.3. Data collection process and data items
Characteristics and results of studies were extracted by all authors. Studies with multiple published articles were reported as a single group. For meta-analysis, final mean and standard deviation (SD) or change in mean and SD were extracted energy intake, sugar consumption, fruit and vegetable consumption and nutritional knowledge. In some studies, the required statistics for meta-analysis were not reported. If available, other statistics e.g., 95% confidence interval (CI) or standard error (SE) were converted to the required form according to the calculations outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Section 7.7 and 16.1.3.2) (DerSimonian and Laird, 1986).
2.4. Quality assessment
The methodological quality of the individual studies were assessed using an assessment scale derived from van Sluijs and colleagues (van Sluijs et al., 2007) (See Table 1). For each included article, three reviewers (WC, LP & TW) independently assessed whether the assessed item was present or if the assessed item was absent. If an item was not described sufficiently it was allocated an absent score. For each article, agreement between reviewers for each article was set a priori at 80% (DerSimonian and Laird, 1986) (i.e., reviewers were required to agree that the items were either present or absent for eight of the 10 items). If this did not occur, further discussions were conducted until consensus was reached.
Table 1.
Methodological quality assessment items (Adapted from (van Sluijs et al., 2007).
| Item | Description |
|---|---|
| A | Key baseline characteristics are presented separately for treatment groups (age, and one relevant outcome (food consumption/energy intake; fruit and vegetable consumption or preference; reduced sugar consumption or preference; nutritional knowledge) and for randomised controlled trials and controlled trials, positive if baseline outcomes were statistically tested and results of tests were provided. |
| B | Randomisation procedure clearly and explicitly described and adequately carried out (generation of allocation sequence, allocation concealment and implementation) |
| C | Validated measures of food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge (validation in same age group reported and/or cited) |
| D | Drop out reported and ≤20% for <6-month follow-up or ≤30% for ≥6-month follow-up |
| E | Blinded outcome variable assessments |
| F | Food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge assessed a minimum of 6 months after pre-test |
| G | Intention to treat analysis for food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge outcomes(s) (participants analysed in group they were originally allocated to, and participants not excluded from analyses because of non-compliance to treatment or because of some missing data) |
| H | Potential confounders accounted for in outcome analysis (e.g. baseline score, group/cluster, age) |
| I | Summary results for each group + treatment effect (difference between groups) + its precision (e.g. 95% confidence interval) |
| J | Power calculation reported, and the study was adequately powered to detect hypothesized relationships |
The standardized effect sizes (Cohen, 1988) were interpreted as minimal (<0.02), small (0.2), medium (0.5), and large (0.8).
3. Results
The combined search retrieved 5257 peer-reviewed articles published in English from the 1st January 1990 to the 31st October 2018. After removing duplicates, 3922 individual articles were ready for the initial review. Decisions were made about the inclusion of articles in two stages. In Stage 1, one author (TW) scanned the titles and abstracts for relevance (i.e., did they have a nutrition education focus in elementary schools).
This resulted in a subgroup of 280 remaining articles. In Stage 2, three authors (TW, LP & WC) conducted full text reviews of remaining articles, including reference lists. This process yielded 34 studies for final inclusion in this systematic review and meta-analysis. Of these 34 studies, seven studies had a focus on energy intake, five had a focus on sugar consumption, 21 of the studies looked at fruit and vegetable consumption and 13 studies focused on nutritional knowledge.
Fig. 1 shows a diagrammatic overview of the review process.
An overview of methodological quality of the studies are reported in Table 2.
Table 2.
Methodological quality assessment.
| Paper Author (Year) |
Methodological Quality Assessment Items |
No. of criteria met | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | ||
| Amaro et al. (2006) | √ | x | x | √ | x | √ | x | √ | √ | √ | 6 |
| Anderson et al. (2005) | √ | x | x | x | x | √ | x | x | √ | x | 3 |
| Auld et al. (1998) | √ | x | √ | x | x | √ | x | √ | √ | x | 5 |
| Baranowski et al. (2000) | √ | x | √ | √ | x | √ | x | √ | √ | √ | 7 |
| Battjes-Fries et al. (2015) | √ | x | √ | √ | x | √ | √ | √ | √ | x | 7 |
| Bere et al. (2006) | √ | x | √ | x | x | √ | x | √ | √ | x | 5 |
| Campbell et al. (2012) | x | x | √ | x | x | x | x | x | √ | x | 2 |
| Cooke et al. (2011) | √ | x | x | √ | x | x | x | x | √ | √ | 4 |
| Day et al. (2008) | √ | x | √ | √ | x | x | x | √ | √ | x | 5 |
| Evans et al. (2010) | √ | √ | √ | √ | x | x | x | √ | √ | √ | 7 |
| Fahlman et al. (2008) | √ | x | √ | x | x | x | x | x | x | x | 2 |
| Francis et al. (2010) | √ | √ | √ | x | x | √ | x | √ | √ | √ | 7 |
| Friel et al. (1999) | √ | x | √ | √ | x | x | x | x | √ | x | 4 |
| Gatto et al. (2017) | √ | √ | √ | x | x | x | x | x | √ | x | 4 |
| Gibbs et al. (2013) | √ | x | x | √ | √ | √ | x | √ | √ | √ | 7 |
| Gortmaker et al. 1999) | √ | √ | √ | x | x | √ | √ | x | √ | x | 6 |
| Govula et al. (2007) | √ | x | √ | x | x | x | x | x | √ | x | 3 |
| Horne et al. (2004) | √ | x | √ | x | x | x | x | x | √ | x | 3 |
| Katz et al. (2011) | √ | x | √ | x | x | x | √ | √ | x | x | 4 |
| Kipping et al. (2014) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | 10 |
| Kristjansdottir et al. (2010) | √ | x | x | √ | x | √ | x | √ | √ | x | 5 |
| Lakshman et al. (2010) | √ | x | √ | √ | x | x | √ | √ | √ | x | 6 |
| Liquori et al. (1999) | x | x | √ | x | x | √ | x | x | x | x | 2 |
| Manios et al. (2002) | √ | x | √ | √ | x | √ | x | √ | √ | x | 6 |
| McAleese and Rankin (2007) | √ | x | x | x | x | x | x | x | √ | x | 2 |
| Morgan et al. (2010) | √ | x | √ | √ | x | √ | x | √ | √ | √ | 7 |
| Parmer et al. (2009) | √ | x | x | x | x | √ | x | √ | √ | x | 4 |
| Prelip et al. (2012) | √ | √ | √ | x | x | x | x | x | √ | x | 4 |
| Ransley et al. (2007) | √ | √ | √ | √ | √ | x | x | x | √ | √ | 7 |
| Rosário et al. (2012) | √ | √ | √ | √ | x | x | √ | x | √ | x | 6 |
| Simons-Morton et al. (1991) | √ | x | x | x | x | √ | x | x | x | x | 2 |
| Struempler et al. (2014) | √ | x | √ | x | x | x | x | √ | √ | √ | 5 |
| van de Gaar et al. (2014) | √ | √ | √ | √ | x | x | √ | x | √ | √ | 7 |
| Viggiano et al. (2015) | √ | √ | √ | x | x | √ | x | x | √ | √ | 6 |
| Percentage/Mean | 94% | 29% | 76% | 47% | 9% | 50% | 21% | 50% | 88% | 35% | 5 |
(N.B. √ = criteria met; x = criteria not met).
Results of the included studies are reported in Table 3.
Table 3.
An overview of the studies found in the systematic review and included in the meta-analysis.
| Author (Year), Country, Funding agency | Design/Dominant Theory Framework* | Sample | Treatment Length | Teaching Strategy/Approach | Relevant Outcome Categories | Statistical Significance (p value/95% CI) |
|---|---|---|---|---|---|---|
| Amaro et al. (2006), Italy, Amici di Raoul Follereau (AIFO) | CT / NR |
241 × students Mean age: 12yrs |
24 weeks | Kalèdo Board Game (15-30mins play time p/w) | Nutritional knowledge (31 items) BMI (z-score) |
<0.05 NS |
| Anderson et al. (2005), UK, Food Standards Agency | CT / TPB |
129 × Grades 1–6 students Mean age: 8yrs |
36 weeks | (Curriculum approach) based on experiential learning, video & literary abstraction Marketing and canteen provisions |
Cognitive & attitudinal (Likert scale) - Diet heart disease knowledge - Preference for HFSS foods 3-day food diary - FV consumption (g) - Energy (kJ) - Sucrose (g) |
0.001 0.034 0.617 0.327 0.578 |
| Auld et al. (1998), USA, Kraft Foods, Inc., USDA Food and Consumer Services Cooperative, National Institute of Health/Centers for Disease Control and Prevention 5 A Day Evaluation Grant, and The Lindsay Trust. | QE / SCT |
760 students in grades 2–4. Mean age: NR |
16 weekly sessions | (Curriculum approach) Nutrition education sessions |
FV knowledge FV consumption -Fruits -Vegetables Plate wastage -Fruits -Vegetables -FV Attitudes to food -School lunches -Wholegrains Self-Efficacy scores |
< 0.001 < 0.05 < 0.05 < 0.01 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 |
| Baronowski et al. (2000), USA, NR. | RCT / SCT |
1172 children in grades 3–5. Mean age: NR |
6 weeks with 12 sessions | (Curriculum approach) Nutrition education sessions. Videotapes, point of purchase education |
Fruit Vegetable and Juice consumption -Vegetables intake -FVJ eaten at weekday lunch -Knowledge of FVJ Fruit and Vegetable self-efficacy |
< 0.05 < 0.01 < 0.10 < 0.05 < 0.10 |
| Battjes-Fries et al. (2015), The Netherlands, Ministry of Economic Affairs of the Netherlands. | QE / NR |
1183 children aged between 9 and 12 years. Mean age: 9yrs. |
10–12 sessions | (Curriculum design) nutrition education Experiential Learning (cooking and tasting food) |
Determinants of taste acceptance -Number of foods known -Positive taste -Number of foods tasted -Willingness to taste food Determinants of target behaviours -Knowledge -Awareness -Attitude |
< 0.05 NS < 0.05 NS < 0.01 NS NS |
| Bere et al. (2006), Norway, Norwegian Research Council. | CT / SCT |
369 × Grade 6 students Mean age: 11yrs |
28 weeks | (Curriculum approach) National Curriculum Experiential learning (Cooking/Food Prep) |
24hr recall of Daily Dietary Intake - FV consumption (Servings per day) Curriculum enjoyment (Likert scale) |
0.41 0.004 |
| Campbell et al. (Campbell et al., 2012), Canada, the Provincial Health Service Authority (PHSA) and by the Child and Family Research Institute (CFRI). | RCT / NR |
873 students in grades 3–7. Mean age NR |
21 lessons spanning 1 year | (Curriculum design) nutrition education, peer to peer instruction |
Healthy behaviours -Grades K to 3 -Grades 4 to 7 Health knowledge -Grades K to 3 -Grades 4 to 7 Healthy habits -Grades K to 3 -Grades 4 to 7 |
< 0.001 NS < 0.001 < 0.001 < 0.001 < 0.001 |
|
Cooke et al. (2011), UK, Medical Research Council National Prevention Research Initiative |
CT / mixed |
442 × Kindergarten students Mean age: 6yrs |
2 weeks | Contingent reinforcement for vegetable tasting | Liking of vegetables (Likert scale) Intake of vegetables |
0.001 0.001 |
| Day et al. (Day et al., 2008), Canada, NR | CT / NR |
444 × Grades 4–5 students Mean age: 10yrs |
12 weeks | Integrates classroom learning, environmental change strategies, and a family/community component to promote the consumption of FV |
24hr recall of Daily Dietary Intake - Fruit consumption (Servings) - Vegetable consumption (Servings) - F V consumption (Servings) - Variety of FV consumption (Servings) |
<0.05 NS <0.05 <0.05 |
| Evans et al. (Evans et al., 2010), UK, NR. | Meta-analysis / NR |
Trials of children aged 5 to 11 years. Mean age NR |
NR | NR |
FV schemes -Fruit portions -Vegetable portions |
Significant Significant |
| Fahlman et al. (Fahlman et al., 2008) USA, NR | QE / NR |
576 × students Mean age: 12yrs |
4 weeks | (Curriculum approach) adapted Health Belief Model |
24hr recall of Daily Dietary Intake - Grain consumption (Servings/day) - Fruit consumption(Servings/day) - Vegetable consumption(Servings/day) - Dairy consumption (Servings/day) - Meat consumption (Servings/day) Self-Efficacy (Likert scale) - Eat more FV - Eat less fat - Drink less SLB - Eat healthy at FF restaurants |
NS 0.047 0.018 NS NS NS NS NS NS |
| Francis et al. (Francis et al., 2010) Trinidad & Tobago, Self-funded |
RCT / NS |
579 × Grade 6 students Mean age: 10yrs |
32 weeks | (Curriculum approach) Bloom’s mastery learning model | Children’s Eating Attitude Test-26 (M) Self-Report SLB consumption (Servings/wk) Fried food consumption (Servings/day) HFSS food consumption (<502 kJ/day) |
<0.05 NS 0.04 NS |
| Friel et al. (Friel et al., 1999), Ireland, the Department of Health. | QE / SLT |
821 children aged 8–10 years. Mean age NR |
20 sessions over 10 weeks | (Curriculum approach) Worksheets, homework tasks. Aerobic exercise regimen. |
Food Behaviour Food Preference Food Knowledge |
< 0.01 < 0.01 NS |
| Gatto et al. (Gatto et al., 2017), USA, The NIH and a Community Benefit grant from the Keck School of Medicine. | RCT / Self-Efficacy |
375 elementary school students. Mean age: 9yrs | 12x weekly sessions of 90 min | School gardening and cooking lessons |
FV consumption -Fruit -Vegetables |
<0.05 NS |
| Gibbs et al. (Gibbs et al., 2013), Australia, NR | CT / mixed |
764 × Grades 3 to 6: Mean age: NR | 2 years | (Curriculum approach) Stephanie Alexander’s Kitchen Garden Program. Experiential (gardening and cooking classes) |
Parent-proxy questionnaire - Fruit consumption /d - Vegetable consumption /d |
0.11 0.59 |
| Gortmaker et al. (Gortmaker et al., 1999), USA, Walton Family Foundation. | QE / SCT BCT |
336 × Grades 4–5 students. Mean age: 9yrs |
2 years | Cross-curricular (Math, science, language, social studies, physical education) coupled with a Social Marketing Approach |
24 hr recall of Daily Dietary Intake - Energy from fat (%) - FV consumption (Servings/4184 kJ) |
0.04 0.01 |
| Govula et al. (Govula et al., 2007), USA, NR | QE / NR |
33 × Grade 3 students Mean age: NR |
6 weeks | (Curriculum approach) MyPyramid and Medicine Wheel Nutrition for Native Americans Culturally appropriate lessons |
Block Kids Fruit/Vegetable recall - F&V consumption (Servings/per day) - Fruit consumption (Servings/per day) - Vegetable consumption (Servings/per day) - Knowledge Questionnaire (% correct) |
0.10 0.519 <0.001 <0.001 |
| Horne et al. (Horne et al., 2004) UK, Horticultural Development Council, Fresh Produce Consortium, ASDA, Co-operative Group, Safeway, Sainsbury, Somerfield, Tesco, Bird’s Eye | QE / SLT |
749 × Grades K-6 students Mean age: NR |
16 weeks | Animation abstraction and contingent reinforcement for F&V consumption |
Consumption based on teacher visual estimates − 5–7 yr/old fruit (%) − 5–7 yr/old vegetable (%) − 7–11 yr/old fruit (%) − 7–11 yr/old vegetable (%) |
<0.002 NR <0.002 NR |
| Katz et al. (2011), USA, NR | RCT / NR |
1180 × Grades 2–4 students. Mean age: NR |
3 months | (Curriculum approach) developed with teachers and supported by homework, letters to parents and information evenings with parents. |
Nutrition Knowledge - Food label quiz score Youth and Adolescent Questionnaire Calories (kcal) Carbohydrates (g) |
0.04 0.51 0.51 |
|
Kipping et al. (2014), UK, UK National Institute for Health Research (NIHR) Public Health Research Programme |
RCT / SCT |
2121 × Grade 5 students. Mean age: 9yrs |
12 months | (Curriculum approach) Active For Life Year 5 intervention. Included teacher training, provision of lesson and child-parent interactive homework plans, all materials required for lessons and homework, and written materials for school newsletters and parents. |
A Day in the Life Questionnaire - F&V consumption (no./day) |
0.42 |
| Kristjansdottir et al. (2010), Iceland, The University of Iceland, The Icelandic Centre for Research, Brim Seafood | CT / NR |
171 × Grade 2 students Mean age: NR |
2 years | (Curriculum approach) co developed with teachers and supported by homework, letters to parents and meetings with parents |
Food record by parents - FV consumption (g/day) - Fruit consumption (g/day) - Vegetable consumption (g/day) |
<0.001 0.001 <0.001 |
| Lakshman et al. (2010), UK, Health Enterprise East, NHS innovations hub for East of England. | RCT / NR |
2519 × Grades 5–6 students. Mean age: NR |
9 weeks | (Curriculum approach) Healthy eating curriculum + Top Grub card game to be implemented in classroom and at home. |
Healthy eating quiz - Knowledge |
0.042 |
| Liquori et al. (Liquori et al., 1998) USA, NR. | QE / SCT |
590 × Grades K-6 students Mean age: NR |
1 year | Experiential learning (Cooking, environment and community garden) |
Food intake based on teacher visual estimates (%) Self-report - Preference for plant food - Attitudes - Knowledge - Self efficacy in cooking - Food intentions - Paired food choice |
<0.01 <0.001 NS <0.05 NS <0.01 <0.01 |
| Manios et al. (2002), Greece, Kellogg’s, Greek Ministry of Sport, Greek Ministry of Education. | QE / NR |
1006 × Grade 1 students Age range: 5.5–6.5yrs Mean age: NR |
6 years | (Curriculum approach) Literary abstraction |
Parental reporting (Food Diary) - Energy (kJ) - Total fat (g) - Protein (g) - Carbohydrate (g) |
<0.05 <0.05 <0.05 NS |
| McAleese & Rankin (McAleese and Rankin, 2007), USA, NR. | QE / NR |
99 × Grade 6 students Mean age: 11yrs |
12 weeks | (Curriculum approach) Nutrition in the Garden Experiential learning (School garden) |
24hr recall of Daily Dietary Intake - Fruit (Servings/day) - Vegetables (Servings/day) - Vitamin A (µg/day) - Vitamin C (mg/day) - Fibre (g/day) |
<0.001 <0.001 0.004 0.016 0.001 |
| Morgan et al. (Morgan et al., 2010) Australia, Hunter Medical Research, Coles. | QE / SCT |
127 × Grades 5–6 students Age range: 11-12yrs Mean age: NR |
10 weeks | (Curriculum approach) Nutrition in the Garden – Modified Experiential learning (School garden) |
FV knowledge (Gimme 5 Questionnaire) 24hr recall of Daily Dietary Intake - Vegetable intake (Servings/day) - Fruit intake (Servings/day) |
<0.02 0.22 0.23 |
| Parmer et al. (2009), USA, NR | CT / ELT |
115 × 2nd Grade students Mean age: 7yrs |
28 weeks | (Curriculum approach) Nutrition lessons + school garden Experiential Learning (Gardening + Food Prep) |
FV Survey (Likert Scale) - MyPyramid food groups - Nutrient–food association - Nutrient–job association - F V identification Researcher Observed Lunch Choices - Vegetable choice (Servings) - Vegetable consumption (Servings) |
NS < 0.001 < 0.001 < 0.01 <0.01 <0.01 |
| Prelip et al. (Prelip et al., 2012), USA, the Network for a Healthy California through the United States Department of Agriculture. | QE / SCT,TPB |
399 × Grades 3–5. Age range: 8-11yrs Mean age: NR |
1 year of schooling | (Curriculum approach) National curriculum and teacher training workshops |
FV Recall - Fruit intake - Vegetable intake - Fruit availability - Vegetable availability FV Questionnaire - Food grp knowledge - FV related attitudes - FV attitude influence from parent - FV influence from teacher |
< 0.01 NS NS NS <. 05 < 0.01 NS < 0.05 |
| Ransley et al. (Ransley et al., 2007), United Kingdom, NR. | QE / NR |
3703 × Children Age range: 4 – 6yrs. Mean age 6 yrs |
11 months | Provision of fruit and vegetables at school |
Fruit intake - At reception age - In year 1 - In year 2 Vegetable portions - At reception age - In year 1 - In year 2 Fruit and vegetable intake - At reception age - In year 1 - In year 2 Energy intake - At reception age - In year 1 - In year 2 |
95% CI (7mth follow up) 0.2 (0.1–0.4) 0.3 (0.1 – 0.6) 0 (-0.2 – 0.3) −0.2 (-0.5 – 0.1) −0.2 (-0.5–0.2) −0.3 (-0.6 – 0.1) 0.2 (0.3 – 0.1) 0.2 (−0.2 – 0.6) −0.2 (−0.5 – 0.2) −0.03 (-0.25 – 0.19) 0.03 (-0.35 – 0.4) −0.63 (-1.01 – 0.25) |
| Rosário et al. (2012), Portugal, NR | RCT / SCT, Health Promotion Model |
464 × Grades 1–4. Mean age: 8yrs | 6 months of lessons | (Curriculum approach) Nutrition lessons |
FV Intake - Fruit (grams) - Vegetables (grams) - Fruits and vegetables (grams) - BMI - Weight control |
< 0.01 <0.05 < 0.001 < 0.01 < 0.05 |
| Simons-Morton et al. (1991), USA, NHLBI funded | RCT / SCT |
Total sample size NR. Children in kindergarten – 4th grade. Mean age NR |
3x spring sessions spanning 3 years | (Curriculum approach) Classroom nutrition lessons, Physical activity, School lunches |
Nutrient Intake - Energy (kcal) [School 3] - Energy (kcal) [School 4] |
Value (95% CI range) 849.3 (816.8 – 881.8) 840.9 (800.7 – 881.1) |
| Struempler et al. (Struempler et al., 2014), USA, Alabama Cooperative Extension System and the US Department of Education SNAP | QE / Experiential Learning Theory |
2477 × third graders. Mean age NR |
17 weeks | (Curriculum approach) Nutrition lessons |
FV intake - Fruit intake (weekly servings) - Vegetable intake (weekly servings) |
< 0.001 < 0.001 |
| van de Gaar et al. (2014), The Netherlands, ZonMw, the Netherlands Organization for Health Research and Development and The Netherlands Organization for Scientific Research (NWO) | RCT / NR |
1288 × Grades 2 – 7. Mean age NR |
1 year | (Curriculum based) Healthy lifestyle promotion, Physical activity |
Sugar sweetened beverage consumption (parent report) - SSB consumed daily (% of cohort) - SSB consumption (Litres) - SSB servings Sugar sweetened beverage consumption (child report) - SSB consumed daily (% of cohort) - SSB consumption (Litres) - SSB servings SSB brought to school |
0.79 (0.47 – 1.34) −0.19 (−0.28 - −0.10) −0.54 (-0.82 - −0.26) 1.32 (0.78 – 2.24) 0.04 (-0.10 – 0.19) 0.05 (-0.36 – 0.47) 0.51 (0.36 – 0.72) |
| Viggiano et al. (2015) Italy, Second University of Naples, Associazione Culturale Kaledo, Regione Campania (Assessorato all’Istruzione), Provincia di Napoli, Provincia di Salerno Assessorato allo Sport, Comune di Cercola (Assessorato all’istruzione) and Fondazione per l’Assistenza all’Infanzia | RCT / NR |
3110 × 9–19 year olds. Mean age 13yrs. |
20 weeks | Board game based education |
Adolescent Food Habit Checklist − 6 month follow up score − 18 month follow up score Nutrition Knowledge Questionnaire − 6 month follow up score − 18 month follow up score Healthy and Unhealthy Diet and Food Questionnaire − 6 month follow up score − 18 month follow up score Food Habits Questionnaire − 6 month follow up score − 18 month follow up score |
< 0.001 NS < 0.001 NS < 0.001 NS < 0.001 NS |
(N.B. TPB = Theory of Planned Behaviour; SCT = Social Cognitive Theory; SLT = Social Learning Theory; BCT = Behavioural Choice Theory; RCT = Randomised controlled trial; QE = Quasi-experimental; CT = Cluster-controlled trial; NR = Not reported; NS = Not significant; FV = Fruit and vegetable; SLB = Sugar-laden beverages; HFSS = High fat, sugar & salt; HFF = High Fat Food; FF = Fast food, BMI = Body Mass Index).
3.1. Studies included in energy intake Meta-Analysis
In the seven studies included in the energy intake meta-analysis (Anderson et al., 2005, Evans et al., 2010, Gatto et al., 2017, Gortmaker et al., 1999, Liquori et al., 1998, Manios et al., 2002, Simons-Morton et al., 1991), the researchers reported the energy intake of elementary school-aged children as taught through a curriculum approach, experiential learning activities or provision of food at school through lunches or the school canteen. In these studies, researchers included information on energy intake using food diaries that were completed by: (1) parents of children in the study; (2) self-reported; or (3) teacher estimates.
3.1.1. Study quality
Of the seven studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. (2007), only three of the six papers met five or more of the assessment criteria (Evans et al., 2010, Gortmaker et al., 1999, Manios et al., 2002). One paper met four of the criteria (Gatto et al., 2017), one met three criteria (Anderson et al., 2005) and two studies met only two of the prescribed criteria (Liquori et al., 1998, Simons-Morton et al., 1991). All seven papers reported their findings using validated measures.
3.1.2. Summary
The analysis is based on seven studies that evaluated the effect of teaching-based interventions on energy intake of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a reduction of energy intake teaching intervention or their regular curricular and the researchers recorded their energy intake at the conclusion of the intervention period. The effect size is the standardised mean difference and is reported using Cohen’s d. The Cohen’s d effect size estimate is calculated using a relative weight assignment to each of the included studies based on the precision of the effect reported. In other words, studies that reported higher degrees of precision (i.e. less variance around the mean) contribute more to the overall Cohen’s d that those with less precision (i.e. greater variance around the mean).
The studies in this analysis were sampled from a universe of possible studies defined by the inclusion/exclusion criteria defined earlier in the paper. For this reason, the random-effects model was employed for analysis. The conclusion (below) applies to that universe.
3.1.3. Do teaching-based interventions affect student energy intake?
The standardised difference in means is d = 0.396. On average, students receiving the teaching-based intervention reduced their energy intake by over a third of a standard deviation than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.042 to 0.751, which tells us that the mean effect size in the universe of studies could fall anywhere in this range.
The Z-value for testing the null hypothesis (that d is 0.0) is 2.190, with a p = 0.029. Thus, we can reject the null that teaching-based interventions have no effect on student energy intake with greater than 95% certainty.
3.1.4. How much does the effect size vary across studies (Heterogeneity)?
To test the null hypothesis that all studies in the analysis share a common effect size the Q-statistic was used in conjunction with the I2 statistic (what proportion of the observed variance reflects differences in true effect sizes rather than sampling error), T (the standard deviation of true effects) and T2 (the variance of true effect sizes). The Q-value is 71.783 with 6 degrees of freedom and p < 0.001. Thus, we reject the null hypothesis that the true effect size is identical in all studies. The I2 is 91.681%, T2 is 0.184 and T is 0.429 indicating considerable heterogeneity among the included studies.
The prediction interval is −0.8009 to 1.5929. We would expect the true effect size for 95% of all populations receiving the interventions to fall within this range.
3.1.5. To what extent would publication bias or the small-study effect alter these findings?
Publication bias suggests that not all completed studies are published, instead studies that have large effects are more likely to be submitted and/or accepted for publication than studies that do not have such large effect sizes. As the treatment effect estimated was calculated from a potentially biased collection of studies, the following analyses were applied to assess the extent of that bias.
Initially, the Classic fail-safe analysis was undertaken. The results showed that the incorporated data from seven studies yielded a z-value of 5.59397 and corresponding 2-tailed p < 0.0001. The fail-safe N in this case is 51. This suggests that 51 ‘null’ studies would need to be included for a combined 2-tailed p > 0.05 i.e., for the effect to be nullified.
Next, we applied Duval and Tweedie’s (Duval and Tweedie, 2000) ‘Trim and Fill’ method that looks for missing studies in a symmetric funnel plot. This method looks for missing studies to the left side of the mean effect. The result suggests that no studies should be trimmed from the left or right of the mean to reduce the potential publication bias in this instance.
3.2. Studies included in sugar consumption Meta-Analysis
Five studies (Anderson et al., 2005, Evans et al., 2010, Fahlman et al., 2008, Francis et al., 2010, van de Gaar et al., 2014) were included that investigated the sugar intake of elementary school- aged children as taught through a curriculum approach, experiential learning and provision of fruits and vegetables at school. The sugar consumption was reported through the variables of: (1) sugar-sweetened beverage consumption; (2) 24-hour dietary recalls; and (3) self-reported intake of sugary foods.
3.2.1. Study quality
Of the five studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. (van Sluijs et al., 2007), three of the five studies met seven of the assessment criteria (Evans et al., 2010, Francis et al., 2010, van de Gaar et al., 2014). One study met three criteria (Anderson et al., 2005) and the last met only two of the criteria (Fahlman et al., 2008). All five papers reported their findings using validated measures.
3.2.2. Summary
The analysis is based on five studies that evaluated the effect of teaching-based interventions on sugar consumption of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a reduction of sugar consumption teaching intervention or their regular curricular and the researchers recorded their sugar consumption at the conclusion of the intervention or follow-up period (whichever was the latter).
3.2.3. Do teaching-based interventions affect student sugar consumption?
The standardised difference in means is d = 0.144. On average, students receiving the teaching-based intervention reduced their sugar consumption by an eighth of a standard deviation than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.004 to 0.284. This range does not include an effect size of zero, which tells us that the true effect size is probably not zero.
In addition, for testing the null hypothesis, the Z-value is 2.023, with a p = 0.043. Thus, we can reject the null that teaching-based interventions have no effect on student sugar consumption with greater than 95% confidence.
3.2.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 23.919 with 4 degrees of freedom and p = 0.004. We reject the null hypothesis that the true effect size is identical in all studies. I2 is 71.630%, T2 is 0.017 and T is 0.130. The prediction interval is −0.3291 to 0.6171. We concluded that here is substantial heterogeneity across these studies.
3.2.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis that showed this meta-analysis incorporated data from five studies and yield a z-value of 3.76678 and corresponding 2-tailed p < 0.0002. The fail-safe N in this case is 14, indicating that there would need to be less than three missing studies for every observed study for the effect to be nullified.
The ‘Trim and Fill’ method suggests that no studies are missing to the left of the mean, but one study is potentially missing from the right of the mean. If three studies were to be trimmed to account for this bias, the adjusted standardised difference in means would be d = 0.181.
3.3. Studies included in FV consumption Meta-Analysis
The fruit and vegetable consumption of elementary school aged children was reported in 21 studies (Fahlman et al., 2008, Anderson et al., 2005, Evans et al., 2010, Gatto et al., 2017, Gortmaker et al., 1999, Amaro et al., 2006, Auld et al., 1998, Baranowski et al., 2000, Bere et al., 2006, Cooke et al., 2011, Day et al., 2008, Fairclough et al., 2013, Gibbs et al., 2013, Govula et al., 2007, Horne et al., 2004, McAleese and Rankin, 2007, Morgan et al., 2010, Prelip et al., 2012, Ransley et al., 2007, Rosário et al., 2016, Struempler et al., 2014) included in this meta-analysis through experiential learning in schools, curricular approaches, the use of board games, and providing fruits and vegetables to children at school. The 21 studies included information on fruit and vegetable intake using the following variables: (1) 24-hour dietary recalls; (2) teacher estimates of consumption; (3) nutrition knowledge test scores; (4) scales measuring how much children like fruits and vegetables; and (5) parent surveys.
3.3.1. Study quality
Of the 21 studies whose quality was assessed using the methodological quality assessment items adapted from van Sluijs et al. (van Sluijs et al., 2007), 13 had between 5 and 7 of the assessment criteria (Bere et al., 2006, Morgan et al., 2010, Day et al., 2008, Fairclough et al., 2013, Gibbs et al., 2013, Ransley et al., 2007, Rosário et al., 2016, Struempler et al., 2014), 6 had between 3 and 4 of the assessment criteria (Anderson et al., 2005, Gatto et al., 2017, Cooke et al., 2011, Govula et al., 2007, Horne et al., 2004, Prelip et al., 2012) and 2 studies had only 2 of the assessment criteria (Fahlman et al., 2008, McAleese and Rankin, 2007). All 21 papers reported their findings using validated measures.
3.3.2. Summary
The analysis is based on 21 studies that evaluated the effect of teaching-based interventions on the fruit and vegetable consumption of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a nutrition focussed teaching intervention or their regular curricular and the researchers recorded their fruit/vegetable consumption at the conclusion of the intervention period.
3.3.3. Do teaching-based interventions affect fruit and vegetable consumption?
The standardised difference in means is d = 0.228. On average, students receiving the teaching-based intervention consumed almost a quarter of a standard deviation more fruit and vegetables than those students who did not receive a teaching intervention. The confidence interval for the standardised difference in means is 0.141 to 0.315.
Similarly, the Z-value for testing the null hypothesis (that d is 0.0) is 5.127, with a p < 0.001. We can reject the null that teaching-based interventions have no effect on student fruit and vegetable consumption.
3.3.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 129.223 with 20 degrees of freedom and p < 0.001. We reject the null hypothesis that the true effect size is identical in all studies. I2 is 84.523%, T2 is 0.029, and T = 0.169 indicating that considerable heterogeneity exists across the included studies. The prediction interval is −0.1403 to 0.5963.
3.3.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis showed this meta-analysis incorporated data from 21 studies and yield a z-value of 10.70147 and corresponding 2-tailed p < 0.0001 for observed studies. The fail-safe N in this case is 606. There would need to be 29 missing studies for every observed study for the effect to be nullified.
The ‘Trim and Fill’ method based on a random effects model suggests that no studies were missing from the left of the mean and three studies from the right of the mean. If three studies were to be trimmed to account for this bias, the adjusted standardised difference in means would only slightly decrease to d = 0.272.
3.4. Studies included in nutritional knowledge Meta-Analysis
Thirteen studies were included (Anderson et al., 2005, Liquori et al., 1998, Fahlman et al., 2008, Francis et al., 2010, Govula et al., 2007, Morgan et al., 2010, Prelip et al., 2012, Amaro et al., 2006, Auld et al., 1998, Baranowski et al., 2000, Campbell et al., 2012, Friel et al., 1999, Lakshman et al., 2010), with researchers reporting on elementary school children’s level of nutrition knowledge as taught through curriculum approaches in the classroom, the use of board games and experiential learning tasks including school gardens. Knowledge of nutrition was measured using: (1) eating attitude tests; (2) self efficacy scales; (3) nutrition knowledge questionnaires; and (4) attitudes to food questionnaires.
3.4.1. Study quality
Of the 13 studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. (van Sluijs et al., 2007), only six of the 13 papers met five or more of the assessment criteria (Francis et al., 2010, Morgan et al., 2010, Lakshman et al., 2010, Amaro et al., 2006, Auld et al., 1998, Baranowski et al., 2000) and seven studies met between two and four of the assessment criteria (Anderson et al., 2005, Liquori et al., 1998, Fahlman et al., 2008, Govula et al., 2007, Prelip et al., 2012, Campbell et al., 2012, Friel et al., 1999). All 13 papers reported their findings using validated measures.
3.4.2. Summary
The analysis is based on 13 studies that evaluated the effect of teaching-based interventions on nutritional knowledge of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a nutrition focussed teaching intervention or their regular curricular and the researchers recorded their nutritional knowledge at the conclusion of the intervention period.
3.4.3. Do teaching-based interventions affect student nutritional knowledge?
The standardised difference in means is d = 0.224. On average, students receiving the teaching-based intervention scored nearly a quarter of a standard deviation higher in terms of nutritional knowledge than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.142 to 0.305. Similarly, the Z-value for testing the null hypothesis (that d is 0.0) is 5.384, with a p < 0.001. We can reject the null that teaching-based interventions have no effect on student nutritional knowledge.
3.4.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 29.446 with 12 degrees of freedom and p < 0.001. The I2 statistic reflecting the proportion of the observed variance differences in true effect sizes rather than sampling error is 59.248%, T2 is 0.010 and T = 0.102. The prediction interval is −0.0142 to 0.4662. Again, in this instance we are led to conclude that substantial heterogeneity exists across the studies included in this analysis.
3.4.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis that showed this meta-analysis incorporated data from 13 studies and yield a z-value of 9.18895 and corresponding 2-tailed p < 0.0001. The fail-safe N in this case is 3246. There would need to be 21 missing studies for every observed study for the effect to be nullified.
Secondly, the ‘Trim and Fill’ method using a random effects model suggests that six studies are missing to the left of the mean but none from the right. It suggests six studies could be trimmed from the left of the mean to reduce bias which would decrease the observed effect to d = 0.156.
4. Discussion
The main findings of this review and meta-analysis indicate that nutrition education programs in elementary schools that are delivered by teachers can have modest effects on a child’s nutritional knowledge and eating behaviours. It appears that elementary school teachers and nutritional education programs can have a small to medium effect on reducing children’s energy intake (d = 0.396), followed by smaller effects on increasing fruit and vegetable consumption (d = 0.228) and nutritional knowledge (d = 0.224). The smallest effect was found on reducing children's sugar consumption, with teachers and nutritional education programs having a very small effect (d = 0.144).
Previous research focusing on elementary school-based nutritional education programs shows that effectiveness depends on the duration of the program, having a few focused nutrition-related outcomes, the appropriate use of theoretical frameworks, fidelity of nutritional education programs, support from school leadership and policy makers, changes in the food school environment, provision of professional learning alongside the delivery of the nutritional education program for teachers, and strategies embedded to engage parents and families (Murimi et al., 2018, Peralta et al., 2016, Dudley et al., 2015, Australian Bureau of Statistics. Australian health survey: nutrition first results – foods and nutrients, 2014, Colley et al., 2018).
In regards to energy intake, unhealthy foods, such as sugary, salty snacks and sugar-sweetened beverages, can contribute up to 40% of 2- to 13-year-old children’s total energy intake, with the greatest increase in this intake occurring with children aged 3 to 4 years and 5 to 8 years (Department of Health FSA, 2012, Keast et al., 2013, Van Cauwenberghe et al., 2010). When these behaviours are targeted through multifaceted school-based nutrition education programs, with regular curricular and non-curricular lessons, delivered by nutritionists or teachers, and engaged parents (Micha et al., 2018), energy intake can be reduced, and reduced substantially as shown through this meta-analysis.
When focusing on increasing fruit and vegetable consumption only, findings of two previous reviews (Murimi et al., 2018, Savoie-Roskos et al., 2017) emphasise that multifaceted interventions that include improved availability of fruit and vegetables, a nutrition education curriculum delivered by teachers with embedded experiential learning experiences, and parental involvement can improve intake of fruits and vegetables. As such, it is not surprising that there has been a proliferation of elementary school nutrition education programs that have used these findings and assessed the impact of gardening and curriculum programs on elementary school children’s fruit and vegetable consumption. A systematic review of gardening interventions (World Health Organization. Guideline: Sugars intake for adults and children. Geneva, Switzerland;, 2015) found that 10 of the 14 articles reviewed produced statistically significant increases in fruit or vegetable consumption among children. Due to many of the 10 studies being limited by the use of convenience samples, small sample sizes, and self-reported measurements of fruit and vegetable consumption, it is important to note that the evidence is not yet clear, with future studies needing to include control groups, randomized designs, and assessments of fruit and vegetable consumption over at least 1 year to advance the literature.
Estimates on sugar consumption suggests that approximately 5% of energy is attributed to sugar sweetened beverage consumption (Bleich and Vercammen, 2018). This is concerning, as it would appear that sugar sweetened beverage consumption alone is already meeting the new World Health Organization's guidelines for maximum free-sugar consumption (Bleich and Vercammen, 2018) and therefore should be a prime target for reducing sugar consumption in children. Despite the clear and consistent evidence that consumption of sugar sweetened beverage consumption increases obesity risk and dental caries among children, and emerging evidence supporting an association with insulin resistance and caffeine-related effects (Nathan et al., 2019), reducing children’s sugar consumption seems to be challenging and complex. A recent systematic review and meta-analysis focusing on the effectiveness of lunchbox interventions in elementary and pre-schools (Nathan et al., 2019), found that removing items that are less healthy from students’ lunchboxes may be more difficult than adding healthier options like fruit and vegetables. Consequently, the researchers suggested that greater formative evaluation with the lunch box packers (i.e., the parents) may be required to improve the shape and impact of future interventions that target high sugar foods.
Only one study included in our meta-analysis included parental engagement as a teaching strategy but reported the second largest effect size recorded (van de Gaar et al., 2014; d = 0.144). A qualitative paper interviewing elementary school-aged children and their perceptions of sugar sweetened beverage consumption, reported that children had a high level of awareness of beverages, the sugar content and health effects (Battram et al., 2016). Hence, children highlighted that they made choices based on taste, parental control practices, accessibility, and advertising, and offered suggestions or strategies for school nutrition education programs that focused on sugar consumption. These included limiting advertising of sugar sweetened beverage consumption, providing incentives to purchase healthy options, and increasing the cost of sugar sweetened beverages or lowering the cost of healthy beverage choices, more education at school and education for parents (Battram et al., 2016).
A limitation of this study was that only one author screened the articles based on titles and abstracts (stage 1) and that a second author was only used in cases of uncertainty in stage 2. This could increase the risk of bias (Cooper, 2015).
5. Conclusion
The findings of this systematic review and meta-analysis suggest that the teaching of nutrition education in elementary schools by teachers can make an important contribution to the knowledge and dietary habits of children. A subsequent finding also suggests that parents and caregivers have an important role to play. The small and medium effect sizes indicate that prudent and evidence-based decisions need to be made by policy makers and pedagogues as to the teaching strategies they employ however not all nutrition education approaches render the same effect. Future intervention research in this field would be well served by augmenting strategies that demonstrate higher effects in nutritional knowledge, reducing energy intake, and increasing fruit and vegetable consumption. New, and a greater number of studies, need to be employed that reduce sugar consumption by children.
Funding
The University of Sydney’s Research Recognition and Incentive Fund partly funded this study. The funding was used to employ a research assistant to conduct, record and collate initial literature searches.
CRediT authorship contribution statement
Wayne Cotton: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Validation, Supervision, Project administration, Funding acquisition. Dean Dudley: Conceptualization, Methodology, Formal analysis, Writing - original draft. Louisa Peralta: Conceptualization, Writing - original draft, Writing - review & editing, Validation. Thea Werkhoven: Data curation, Resources, Investigation, Writing - original draft, Visualization, Writing - review & editing.
Contributor Information
Wayne Cotton, Email: wayne.cotton@sydney.edu.au.
Dean Dudley, Email: dean.dudley@mq.edu.au.
Louisa Peralta, Email: louisa.peralta@sydney.edu.au.
Thea Werkhoven, Email: thea.werkhoven@sydney.edu.au.
References
- Amaro S., Viggiano Alessandro, Di Costanzo Anna, Madeo Ida, Viggiano Andrea, Baccari Maria Ena, Marchitelli Elena, Raia Maddalena, Viggiano Emanuela, Deepak Sunil, Monda Marcellino, De Luca Bruno. a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Eur. J. Pediatr. 2006;165(9):630. doi: 10.1007/s00431-006-0153-9. [DOI] [PubMed] [Google Scholar]
- Anderson A.S., Porteous L.E.G., Foster E., Higgins C., Stead M., Hetherington M. The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutr. 2005;8(6):650–656. doi: 10.1079/phn2004721. [DOI] [PubMed] [Google Scholar]
- Auld G.W., Romaniello C., Heimendinger J., Hambidge C., Hambidge M. Outcomes from a school-based nutrition education program using resource teachers and cross-disciplinary models. J. Nutr. Educ. 1998;30(5):268–280. [Google Scholar]
- Australian Bureau of Statistics. Australian health survey: nutrition first results – foods and nutrients, 2011–12: Australian Government; 2014 [Available from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.007main+features12011-12.
- Baranowski T., Davis M., Resnicow K., Baranowski J., Doyle C., Lin L.S. Gimme 5 Fruit, Juice, and Vegetables for Fun and Health: Outcome Evaluation. Health Educ. Behavior. 2000;27(1):96–111. doi: 10.1177/109019810002700109. [DOI] [PubMed] [Google Scholar]
- Battjes-Fries M.C.E., Haveman-Nies A., Renes R.-J., Meester H.J., van't Veer P. Effect of the Dutch school-based education programme 'Taste Lessons' on behavioural determinants of taste acceptance and healthy eating: a quasi-experimental study. Pub. Health Nut. 2015;18(12):2231–2241. doi: 10.1017/S1368980014003012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battram D.S., Piche L., Beynon C., Kurtz J., He M. Sugar-Sweetened Beverages: Children's Perceptions, Factors of Influence, and Suggestions for Reducing Intake. J. Nutr. Educ. Behav. 2016;48(1):27–34.e1. doi: 10.1016/j.jneb.2015.08.015. [DOI] [PubMed] [Google Scholar]
- Bere E., Veierød M.B., Bjelland M., Klepp K.-I. Outcome and process evaluation of a Norwegian school-randomized fruit and vegetable intervention: fruits and Vegetables Make the Marks (FVMM) Health Educ. Res. 2006;21(2):258. doi: 10.1093/her/cyh062. [DOI] [PubMed] [Google Scholar]
- Bleich S.N., Vercammen K.A. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obesity. 2018;5(1):6. doi: 10.1186/s40608-017-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A.C., Barnum D.B., Ryden V.B., Ishkanian S.B., Stock S., Chanoine J.P. The Effectiveness of the Implementation of Healthy Buddies™, a School-Based, Peer-Led Health Promotion Program in Elementary Schools. Can. J. Diabetes. 2012;36(4):181–196. [Google Scholar]
- Cohen J. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- The Cochrane Collaboration. Fail-safe N 2011 [updated March 2011. 5.1.0: [Available from: https://handbook-5-1.cochrane.org/index.htm#chapter_10/10_4_4_3_fail_safe_n.htm.
- Colley P., Myer B., Seabrook J., Gilliland J. The impact of Canadian school food programs on children's nutrition and health: a systematic review. Can. J. Dietetic Practice and Res. 2018;80(2):79–86. doi: 10.3148/cjdpr-2018-037. [DOI] [PubMed] [Google Scholar]
- Cooke L.J., Chambers L.C., Anez E.V., Croker H.A., Boniface D., Yeomans M.R. Eating for pleasure or profit: The effect of incentives on children's enjoyment of vegetables. Psychol. Sci. 2011;22(2):190–196. doi: 10.1177/0956797610394662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H. Sage publications; London: 2015. Research Synthesis and Meta-Analysis: A Step-by-Step Approach. [Google Scholar]
- Day M.E., Strange K.S.P., McKay H.A.P., Naylor P.-J.P. Action Schools! BC - Healthy Eating: Effects of a Whole-school Model to Modifying Eating Behaviours of Elementary School Children. Can. J. Public Health. 2008;99(4):328–331. doi: 10.1007/BF03403766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vlieger N., Riley N., Miller A., Collins C., Bucher T. Nutrition education in the Australian New South Wales primary school curriculum: an exploration of time allocation, translation and attitudes in a sample of teachers. Health Promot. J. Austr. 2019;30(1):94–101. doi: 10.1002/hpja.188. [DOI] [PubMed] [Google Scholar]
- Department of Health FSA . Department of Health; England, UK: 2012. National diet and nutrition survey headline results from years 1, 2 and 3 (combined) of the rolling programme (2008/2009–2010/11) [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dudley D.A., Cotton W.G., Peralta L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Activity. 2015;12 doi: 10.1186/s12966-015-0182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudley D., Peralta L., Cotton W., Baxter D. NSW Department of Education and Communities,; Sydney, Australia: 2015. Teaching healthy eating to primary school students: A review of evidence and best practice. [Google Scholar]
- Duval S., Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Evans C.E.L., Greenwood D.C., Cade J.E. 068 Systematic review and meta-analysis of school-based interventions to improve fruit and vegetable intake. J. Epidemiol. Community Health. 2010;64 [Google Scholar]
- Fahlman M.M., Dake J.A., McCaughtry N., Martin J. A Pilot Study to Examine the Effects of a Nutrition Intervention on Nutrition Knowledge, Behaviors, and Efficacy Expectations in Middle School Children. J. Sch. Health. 2008;78(4):216–222. doi: 10.1111/j.1746-1561.2008.00289.x. [DOI] [PubMed] [Google Scholar]
- Fairclough S.J., Hackett A.F., Davies I.G., Gobbi R., Mackintosh K.A., Warburton G.L. Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health. 2013;13:626. doi: 10.1186/1471-2458-13-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis M., Nichols S.S.D., Dalrymple N. The effects of a school-based intervention programme on dietary intakes and physical activity among primary-school children in Trinidad and Tobago. Public Health Nutr. 2010;13(5):738–747. doi: 10.1017/S1368980010000182. [DOI] [PubMed] [Google Scholar]
- Friel S., Kelleher C., Campbell P., Nolan G. Evaluation of the Nutrition Education at Primary School (NEAPS) programme. Public Health Nutr. 1999;2(4):549–555. doi: 10.1017/s1368980099000737. [DOI] [PubMed] [Google Scholar]
- Gatto N.M., Martinez L.C., Spruijt-Metz D., Davis J.N. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatric Obesity. 2017;12(1):28–37. doi: 10.1111/ijpo.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs L., Staiger P.K., Johnson B., Block K., Macfarlane S., Gold L. Expanding Children's Food Experiences: The Impact of a School-Based Kitchen Garden Program. J. Nutr. Educ. Behavior. 2013;45(2):137–146. doi: 10.1016/j.jneb.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Goran M.I., Ball G.D., Cruz M.L. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J. Clin. Endocrinol. Metab. 2003;88(4):1417–1427. doi: 10.1210/jc.2002-021442. [DOI] [PubMed] [Google Scholar]
- Gortmaker S.L., Cheung L.W.Y., Peterson K.E., Chomitz G., Cradle J.H., Dart H. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch. Pediatr. Adolesc. Med. 1999;153(9):975–983. doi: 10.1001/archpedi.153.9.975. [DOI] [PubMed] [Google Scholar]
- Govula C., Kattelman K., PhD R.D., Ren C. Culturally appropriate nutrition lessons increased fruit and vegetable consumption in American Indian children. Top Clin Nutr. 2007;22(3):239–245. [Google Scholar]
- Graziose M.M., Koch P.A., Wang Y.C., Lee Gray H., Contento I.R. Cost-effectiveness of a nutrition education curriculum intervention in elementary schools. J. Nutr. Educ. Behav. 2017;49(8):684–969. doi: 10.1016/j.jneb.2016.10.006. [DOI] [PubMed] [Google Scholar]
- Horne P.J., Tapper K., Lowe C.F., Hardman C.A. Increasing children's fruit and vegetable consumption: A peer-modelling and rewards-based intervention. Eur. J. Clin. Nutr. 2004;58(12):1649–1660. doi: 10.1038/sj.ejcn.1602024. [DOI] [PubMed] [Google Scholar]
- Katz D.L., Katz C.S., Treu J.A., Reynolds J., Njike V., Walker J.…Michael J. Teaching healthful food choices to elementary school students and their parents: the nutrition detectives[TM] program. J. School Health. 2011;81(1):21–28. doi: 10.1111/j.1746-1561.2010.00553.x. [DOI] [PubMed] [Google Scholar]
- Keast D.R., Fulgoni V.L., 3rd, Nicklas T.A., O'Neil C.E. Food sources of energy and nutrients among children in the United States: National Health and Nutrition Examination Survey 2003–2006. Nutrients. 2013;5(1):283–301. doi: 10.3390/nu5010283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelsey M.M., Zaepfel A., Bjornstad P., Nadeau K.J. Age-related consequences of childhood obesity. Gerontology. 2014;60(3):222–228. doi: 10.1159/000356023. [DOI] [PubMed] [Google Scholar]
- Kipping R.R., Howe L.D., Jago R., Campbell R., Wells S., Chittleborough C.R.…Lawlor D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ: British Medical Journal. 2014;348 doi: 10.1136/bmj.g3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristjansdottir A.G., Johannsson E., Thorsdottir I. Effects of a school-based intervention on adherence of 7-9-year-olds to food-based dietary guidelines and intake of nutrients. Pub. Health Nut. 2010;13(8):1151–1161. doi: 10.1017/S1368980010000716. [DOI] [PubMed] [Google Scholar]
- Lakshman Rajalakshmi R., Sharp Stephen J., Ong Ken K., Forouhi Nita G. A novel school-based intervention to improve nutrition knowledge in children: cluster randomised controlled trial. BMC Public Health. 2010;10:123. doi: 10.1186/1471-2458-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liquori T., Koch P.D., Contento I.R., Castle J. The Cookshop Program: Outcome evaluation of a nutrition education program linking lunchroom food experiences with classroom cooking experiences. J. Nutr. Educ. 1998;30(5):302–313. [Google Scholar]
- Manios Y., Moschandreas J., Hatzis C., Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br. J. Nutr. 2002;88(3):315. doi: 10.1079/BJN2002672. [DOI] [PubMed] [Google Scholar]
- McAleese J.D., Rankin L.L. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J. Am. Diet. Assoc. 2007;107(4):662–665. doi: 10.1016/j.jada.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Micha R., Karageorgou D., Bakogianni I., Trichia E., Whitsel L.P., Story M. Effectiveness of school food environment policies on children's dietary behaviors: A systematic review and meta-analysis. PLoS ONE. 2018;13(3) doi: 10.1371/journal.pone.0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., The P.G. Preferred Reporting Items For Systematic Reviews And Meta-Analyses: The PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan P.J., Warren J.M., Lubans D.R., Saunders K.L., Quick G.I., Collins C.E. The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students. Public Health Nutr. 2010;13(11):1931–1940. doi: 10.1017/S1368980010000959. [DOI] [PubMed] [Google Scholar]
- Murimi M.W., Moyeda-Carabaza A.F., Nguyen B., Saha S., Amin R., Njike V. Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr. Rev. 2018;76(8):553–580. doi: 10.1093/nutrit/nuy020. [DOI] [PubMed] [Google Scholar]
- Nathan N., Janssen L., Sutherland R., Hodder R.K., Evans C.E.L., Booth D. The effectiveness of lunchbox interventions on improving the foods and beverages packed and consumed by children at centre-based care or school: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019;16(1):38. doi: 10.1186/s12966-019-0798-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmer S.M., Salisbury-Glennon J., Shannon D., Struempler B. School gardens: an experiential learning approach for a nutrition education program to increase fruit and vegetable knowledge, preference, and consumption among second-grade students. J. Nut. Edu. Behav. 2009;41(3):212–217. doi: 10.1016/j.jneb.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Peralta L.R., Dudley D.A., Cotton W.G. Teaching Healthy Eating to Elementary School Students: A Scoping Review of Nutrition Education Resources. J. Sch. Health. 2016;86(5):334–345. doi: 10.1111/josh.12382. [DOI] [PubMed] [Google Scholar]
- Porter K.J., Koch P.A., Contento I.R. Why and how schools make nutrition education programs “Work”. J. Sch. Health. 2018;88(1):23–33. doi: 10.1111/josh.12577. [DOI] [PubMed] [Google Scholar]
- Prelip M., Kinsler J., Thai C.L., Erausquin J.T., Slusser W. Evaluation of a school-based multicomponent nutrition education program to improve young children's fruit and vegetable consumption. J. Nutr. Educ. Behavior. 2012;44(4):310–318. doi: 10.1016/j.jneb.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Ransley J.K., Greenwood D.C., Cade J.E., Blenkinsop S., Schagen I., Teeman D. Does the school fruit and vegetable scheme improve children’s diet? A non-randomised controlled trial. J. Epidemiol. Community Health. 2007;61(8):699. doi: 10.1136/jech.2006.052696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly J.J., Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int. J. Obesity 2014. 2011;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- Rosário R., Oliveira B., Araújo A., Lopes O., Padrão P., Moreira A.…Moreira P. The impact of an intervention taught by trained teachers on childhood overweight. Int. J. Environ. Res. Public Health. 2012;9(4):1355–1367. doi: 10.3390/ijerph9041355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosário R., Araújo A., Padrão P., Lopes O., Moreira A., Abreu S., Vale S., Pereira B., Moreira P. Impact of a school-based intervention to promote fruit intake: a cluster randomized controlled trial. Public Health. 2016;136:94. doi: 10.1016/j.puhe.2016.03.013. [DOI] [PubMed] [Google Scholar]
- Savoie-Roskos M.R., Wengreen H., Durward C. Increasing Fruit and Vegetable Intake among Children and Youth through Gardening-Based Interventions: A Systematic Review. J. Acad. Nutr. Dietetics. 2017;117(2):240–250. doi: 10.1016/j.jand.2016.10.014. [DOI] [PubMed] [Google Scholar]
- Simons-Morton B.G., Parcel G.S., Baranowski T., Forthofer R., O'Hara N.M. Promoting physical activity and a healthful diet among children: results of a school-based intervention study. Am. J. Public Health. 1991;81(8):986. doi: 10.2105/ajph.81.8.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M., Nanney M.S., Schwartz M.B. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. The Milbank Quarterly. 2009;87(1):71–100. doi: 10.1111/j.1468-0009.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struempler B.J., Parmer S.M., Mastropietro L.M., Arsiwalla D., Bubb R.R. Changes in fruit and vegetable consumption of third-grade students in body quest: Food of the warrior, a 17-class childhood obesity prevention program. J. Nutr. Educ. Behavior. 2014;46(4):286–292. doi: 10.1016/j.jneb.2014.03.001. [DOI] [PubMed] [Google Scholar]
- United Nations Educational Scientific and Cultural Organization . UNESCO; Paris: 2013. Making Education a Priority in the Post-2015 Development Agenda. [Google Scholar]
- Van Cauwenberghe E., Maes L., Spittaels H., van Lenthe F.J., Brug J., Oppert J.M. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and 'grey' literature. Br. J. Nutr. 2010;103(6):781–797. doi: 10.1017/S0007114509993370. [DOI] [PubMed] [Google Scholar]
- van de Gaar V., Jansen W., Grieken A., Borsboom G., Kremers S., Raat H. Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: A controlled trial. Int. J. Behav. Nutr. Phys. Activity. 2014;11(1):98. doi: 10.1186/s12966-014-0098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Geel M., Vedder P., Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int. J. Obesity 2014. 2014;38(10):1263–1267. doi: 10.1038/ijo.2014.117. [DOI] [PubMed] [Google Scholar]
- van Sluijs E.M.F., McMinn A.M., Griffin S.J. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ (Clinical research ed). 2007;335(7622):703–707. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viggiano A., Viggiano E., Di Costanzo A., Viggiano A., Andreozzi E., Romano V.…Amaro S. Kaledo, a board game for nutrition education of children and adolescents at school: cluster randomized controlled trial of healthy lifestyle promotion. Euro. J. Ped. 2015;174(2):217–228. doi: 10.1007/s00431-014-2381-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva, Switzerland: 2012. Population-Based Approaches to Childhood Obesity Prevention. [Google Scholar]
- World Health Organization. Guideline: Sugars intake for adults and children. Geneva, Switzerland; 2015 31 March. [PubMed]