Abstract
Introduction:
The aim of the current study was to assess the levels of anxiety and depression and to determine relationships between perceived social support and other factors in migraine patients and to compare with the control group.
Methods:
The study was a cross-sectional study with 37 migraine patients and 40 control patients. The diagnosis of migraine was established according to the International Headache Society criteria. Patients completed a questionnaire comprised of sociodemographic characteristics, migraine severity (frequency and visual analogue scale score) and scales which are used for the determination of depression, anxiety and social support.
Results:
Correlation analyses revealed that Beck Depression Inventory (BDI) scores were positively correlated with anxiety scores; however, they were not correlated with the clinical characteristics of migraine. Whereas, anxiety scores were correlated with the number of days with migraine pain and the number of migraine attacks in a month. However, VAS scores were not correlated with anxiety scores. Furthermore, social support scores were found to be negatively correlated with depression and anxiety scores. In the migraine group, median BDI score was 10.0 (0.0–44.0), median STAI score was 81.0 (44.0–131.0), in the control group, median BDI score was 6.0 (0.0–24.0), median STAI score was 75.0 (62.0–95.0). BDI, STAI-Trait and STAI-Total scores were higher in the migraine group than in the control group. The MSPSS score was found to be lower in the migraine group than in the control group.
Conclusions:
Depression and anxiety scores higher in the migraine group than control group. We believe our results support the suggestion that anxiety and depression are associated with migraine. Additionally, social support may be critical in the prevention or reduction of migraine attacks as it was found to affect the anxiety and depression scores of patients with migraine.
Keywords: Migraine, depression, anxiety
INTRODUCTION
Migraine is one of the most common diseases worldwide; in 2016, global age-standardized prevalence was reported to be 14.4% in the general population, 18.9% in women and 9.8% in men (1). Migraine usually begins in the adolescence and is characterized by lifelong and recurrent episodes of pain (2). It is an important cause of disability for individuals as it has been associated with significant comorbidities such as severe depression and anxiety in addition to its detrimental effects on work and school life (3).
Like many psychiatric disorders (4), anxiety and mood disorders are among the primary psychiatric disorders that affect the prevalence, prognosis, treatment process and clinical results of migraine. Studies have reported that anxiety and mood disorders are two to ten times more common in migraine patients than the general population (5). Furthermore, people suffering from pain conditions (including headache) also experience depression and its symptoms at a higher frequency than both the general population and matched controls. In addition to being associated with pain variance and disability in migraine (6), these psychiatric conditions have also been shown to contribute to the development and identification of migraine attacks in effected individuals (7). The presence of anxiety and depression may be a trigger of migraine attacks via increasing pain perception or lowering pain threshold (8).
Social support has been shown to be effective in protecting individuals from the adverse affects of disease and disability, as it may promote healthy behavior and could increase compliance with treatment (9). Studies have shown that individuals with headaches receive more social support from their friends and family compared to those who do not have headaches (10, 11). Increasing social support plays an important role in migraine patients, both in order to prevent excessive drug use and also to direct patients to take measures which could have prophylactic effects (9). Therefore, assessing depression, anxiety and perceived social support levels in migraine patients and determining their relationship with each other could provide critical data as to how migraine sufferers cope with their disease and how pain can be managed or prevented in these patients.
The aim of the current study was to assess the levels of anxiety and depression and to determine relationships (or lack thereof) between perceived social support and other factors in patients with migraine, and to compare with control group.
METHODS
This was a cross-sectional study including 37 patients with migraine (migraine group) and 40 healthy individuals without migraine or any other type of chronic headache (control group) who applied to the neurology clinic of İstanbul Yeni Yuzyil Universty School of Medicine, Gaziosmanpaşa Hospital between July 2018 – November 2018. Migraine diagnosis was established according to the criteria put forth by the International Headache Society in 2018 (12). The criteria for inclusion into the study were: being over 18 years of age and accepting to participate in the study. Patients who did not agree to participate in the study and those who were under 18 years of age were excluded.
Patients were asked to fill a questionnaire which included the following sections: sociodemographic characteristics, Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI), Multidimensional Scale of Perceived Social Support (MSPSS) and Visual Analogue Scale (VAS) for pain.
The BDI was used to determine the level of depression in individuals. It was developed by Beck in 1961 and the Turkish validity and reliability study of the scale was performed by Hisli in 1989 (13). The scale consists of 21 items that evaluate common symptoms of depression. Higher scores (from a possible 63) indicate worse depression (14).
State-Trait Anxiety Inventory is used to assess the ‘state’ and ‘trait’ anxiety levels of individuals and was developed by Spielbeier et al. (15). The Turkish validity and reliability study of the scale was performed by Öner and Le Compte (16). The scale has two sections consisting of 20 items. While one section focuses on determining current anxiety (state, STAI-S), the other section focuses on determining the overall anxiety propensity of the individual (trait, STAI-T). Total score varies between 20–80 points in both sub-scales of the scale, and the level of anxiety is proportional to the score (15).
The MSPSS is used to evaluate the perceived social support levels of individuals, and was developed by Eker et al. (17). There are three sub-dimensions (family, friends and a special/significant person) in the scale, each consisting of 4 items. The total score that can be obtained from the scale varies between 12–84, and perceived social support increases as the score increases (17).
Visual Analogue Scale (VAS) was used to determine the subjective pain level of subjects. In VAS, 0 indicates no pain, 5 is the moderate severity of pain and 10 is the worst pain imaginable (sometimes referred to as the worst pain the patient has ever suffered) (18). Patients were given a paper incremented from 0 to 10 at equal intervals and were asked to mark their perceived pain level during their last attack.
Patients who were admitted to our outpatient clinic with migraine were informed about the aim and subject of the study and their verbal consent was obtained. Ethics committee approval and necessary permissions were obtained for the study. The questionnaire forms were filled by the patients themselves under observation by a physician who was not their immediate healthcare provider. Each questionnaire form took about 25–30 minutes to complete.
All data obtained during the study were evaluated in SPSS (Version 15.0) (IBM, Armonk, NY). In the evaluation of descriptive data, number (n), percentage (%), mean, standard deviation (SD), median, minimum (min) and maximum (max) values were used. The chi-square test was used to compare the sociodemographic characteristics of migraine and control groups. Mann Whitney U test was used to compare the BDI and STAI scores of the groups. Spearman correlation analysis was used to evaluate the relationship between the parameters studied. The level of statistical significance was accepted as p<0.05.
RESULTS
The study group consisted of 37 patients with migraine (29 females; 78.4%) with a mean age of 39.5±9.0 years, and 40 controls (33 females; 82.5%) with a mean age of 32.4±11.7 years. When the sociodemographic characteristics of the migraine group were examined, we found that 27.0% were unemployed, 94.6% were married and 86.5% had at least one child. When the sociodemographic characteristics of the control group were examined, 10.0% were unemployed, 62.5% were married and 40.0% had at least one child. The sociodemographic characteristics of the study group are given in Table 1.
Table 1.
Sociodemographic characteristics of the study group
| Sociodemographic Characteristics | Migraine group n (%) | Control group n (%) | p |
|---|---|---|---|
| Sex | |||
| Male | 8 (21.6) | 7 (17.5) | 0.776 |
| Female | 29 (78.4) | 33 (82.5) | |
| Age Group | |||
| ≤30 age | 5 (13.5) | 20 (20.0) | 0.001 |
| >30 age | 32 (86.5) | 20 (50.0) | |
| Working Status | |||
| Working | 27 (73.0) | 36 (90.0) | 0.076 |
| Not working | 10 (27.0) | 4 (10.0) | |
| Marital Status | |||
| Married | 35 (94.6) | 15 (37.5) | <0.001 |
| Single or divorced | 2 (5.4) | 25 (62.5) | |
| Having Children | |||
| Yes | 32 (86.5) | 16 (40.0) | <0.001 |
| No | 5 (13.5) | 24 (60.0) | |
| Total | 37 (100.0) | 40 (100.0) | |
No differences were found between the BDI and STAI scores of those in the migraine group with regard to gender, age group, working status, marital status and having children. The comparison of BDI and STAI scores of migraine group according to sociodemographic characteristics are given in Table 2.
Table 2.
Comparison of BDI and STAI scores of migraine group according to sociodemographic characteristics
| BDI Median (Min-Max) | p | STAI Median (Min-Max) | p | |
|---|---|---|---|---|
| Gender | ||||
| Male | 8.5 (5.0–29.0) | 0.814 | 79.0 (70.0–99.0) | 0.550 |
| Female | 10.0 (0.0–44.0) | 82.0 (44.0–131.0) | ||
| Age Group | ||||
| ≤30 age | 17.0 (6.0–23.0) | 0.197 | 89.0 (76.0–113.0) | 0.286 |
| >30 age | 9.0 (0.0–44.0) | 79.0 (44.0–131.0) | ||
| Working Status | ||||
| Working | 10.0 (0.0–44.0) | 0.801 | 82.0 (44.0–131.0) | 0.533 |
| Not working | 9.5 (5.0–23.0) | 75.5 (65.0–113.0) | ||
| Marital Status | ||||
| Married | 10.0 (0.0–44.0) | 0.589 | 80.0 (44.0–131.0) | 0.589 |
| Single or divorced | 15.0 (7.0–23.0) | 87.0 (85.0–89.0) | ||
| Having Children | ||||
| Yes | 9.5 (0.0–44.0) | 0.328 | 79.0 (44.0–131.0) | 0.350 |
| No | 17.0 (6.0–29.0) | 89.0 (76.0–99.0) | ||
There was a positive correlation between BDI score and STAI-S, STAI-T and STAI scores in the migraine group. When the associations between clinical characteristics and scores were evaluated, we found that STAI and STAI-S scores were positively correlated with the number of days with migraine pain in a month and number of migraine attacks in one month. Additionally, there was a positive correlation between STAI-T scores and the number of migraine attacks in a month. Finally, when we evaluated scores in regard to social support as measured by MSPSS, we found that MSPSS scores were negatively correlated with BDI, STAI and STAI-T scores. The results of Spearman correlation analyses are given in Table 3.
Table 3.
Results of correlation analyses among the parameters examined in the study group
| BDI | STAI-State | STAI-Trait | STAI total | |||||
|---|---|---|---|---|---|---|---|---|
| r | p | R | p | r | p | r | p | |
| Migraine VAS score | 0.104 | 0.540 | -0.130 | 0.444 | -0.210 | 0.212 | -0.184 | 0.276 |
| Number of days with migraine/month | 0.241 | 0.150 | 0.432 | 0.008 | 0.312 | 0.060 | 0.432 | 0.008 |
| Number of migraine attacks/month | 0.213 | 0.206 | 0.473 | 0.003 | 0.333 | 0.044 | 0.474 | 0.003 |
| BDI | 0.470 | p<0.001 | 0.510 | p<0.001 | 0.535 | p<0.001 | ||
| STAI-State | 0.470 | p<0.001 | 0.447 | p<0.001 | 0.841 | p<0.001 | ||
| STAI-Trait | 0.510 | p<0.001 | 0.447 | p<0.001 | 0.816 | p<0.001 | ||
| STAI Total | 0.535 | p<0.001 | 0.841 | p<0.001 | 0.816 | p<0.001 | ||
| MSPSS | -0.250 | 0.028 | -0.181 | 0.115 | -0.341 | 0.002 | -0.313 | 0.006 |
VAS, Visual Analogue Scale; BDI, Beck Depression Inventory; STAI, State and Trait Anxiety Inventory; MSPSS, Multidimensional Scale of Perceived Social Support.
There were significant differences between the patients and controls in terms of BDI, STAI, STAI-T and MSPSS results, whereas STAI-S scores were similar (Table 4). BDI, STAI-T and STAI scores were higher in the migraine group than in the control group. The MSPSS score was found to be lower in the migraine group than in the control group. Box-plot graphs showing the comparison of BDI, STAI and MSPSS scores of patients and controls are given in Figures 1, 2 and 3.
Table 4.
Comparison of BDI, STAI-State, STAI-Trate, STAI-Total and MSPSS scores of migraine and control groups
| Migraine group | Control group | p | |
|---|---|---|---|
| BDI | 10.0 (0.0–44.0) | 6.0 (0.0–24.0) | 0.002 |
| STAI-State | 39.0 (8.0–65.0) | 37.0 (23.0–49.0) | 0.332 |
| STAI-Trait | 43.0 (31.0–66.0) | 39.0 (31.0–49.0) | 0.009 |
| STAI-Total | 81.0 (44.0–131.0) | 75.0 (62.0–95.0) | 0.028 |
| MSPSS | 57.0 (24.0–84.0) | 69.5 (35.0–84.0) | 0.001 |
Figure 1.
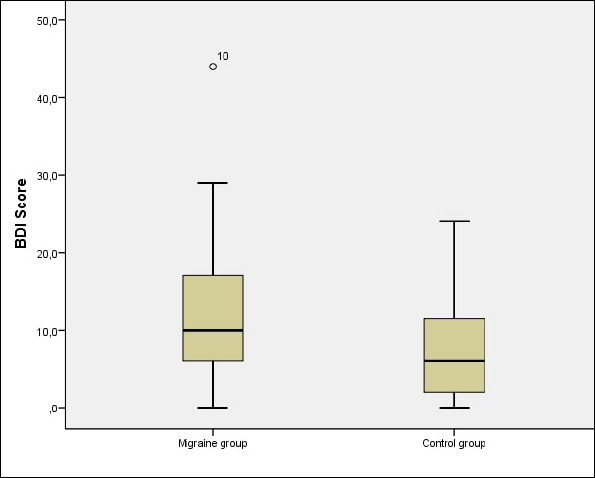
Comparison of BDI scores of migraine and control groups.
Figure 2.
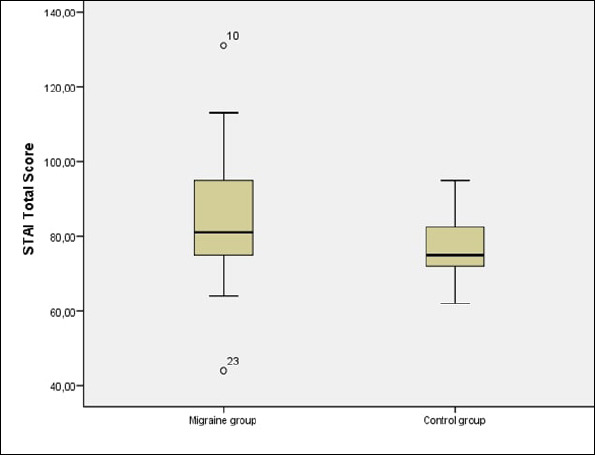
Comparison of STAI-Total scores of migraine and conrol groups.
Figure 3.
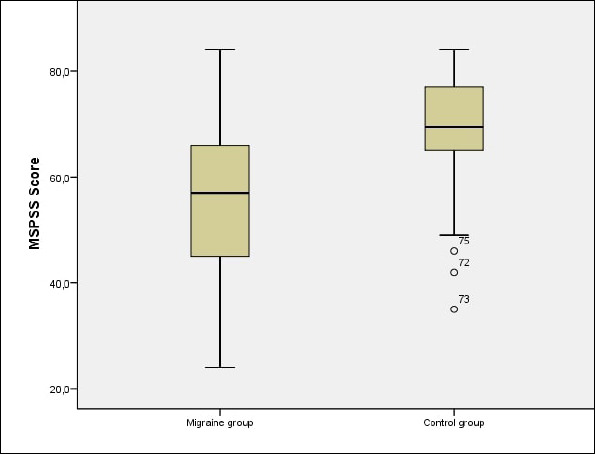
Comparison of MSPSS scores of migraine and control groups.
DISCUSSION
In addition to the increased frequency of depression and anxiety in patients with migraine, these conditions have also been suggested to have a role in migraine development and severity (19). In the current study, mean BDI score was 12.35±8.55 in the migraine group. Previous studies have reported varying results: 15.10±8.87 by Karaca et al., 9.68±8.67 by Yaşar et al. and 7.50±5.80 by Perozzo et al. (20–22). Mean STAI score was 84.14±16.26 (mean STAI-S and STAI-T scores were 39.68±10.00 and 44.46±8.62), which are similar to those reported in a previous study Perozzo et al. (STAI-S: 36.9±9.00 and STAI-T: 37.80±9.50) (22). Overall, our results were generally similar to those found in other studies involving patients with migraine.
We did not find any relationships between BDI scores and parameters such as gender, age group, working status, marital status and having children. Song et al., also reported that depression scores were not associated with gender in patients with migraine (23). Similarly, it was reported that BDI score did not change according to gender and age group, but was higher in married patients (24). In a study from Iran, BDI scores were found to be higher among females (25).
In our patients, the STAI scores were not found to be related with gender, age group, working status, marital status and having children. In contrast, according to a study conducted by Yong et al., the risk of anxiety was higher in migraine patients under 30 years of age (26). In another study, it was reported that there was no difference in terms of anxiety according to sex (24). Although our results seem contradictory in terms of sex and age, the fact that the majority of patients in our study were female, may have caused a lack of statistical significance for these comparisons.
The relationship between migraine and depression has been the subject of many clinical and community-based studies. The incidence of depression/anxiety in migraine patients and the incidence of migraine in patients with depression or anxiety have led to researchers suggesting that migraine attacks may contribute to the development of said conditions. According to another view, migraine is argued to be a somatic symptom of depression. It has been reported that the risk of depression in persons with migraine increases by 2.4 to 5.8–fold (27, 28, 7). In the current study, no correlations were found between BDI scores and migraine VAS score, number of days with migraine pain and the number of migraine attacks per month. However, in the study by Baldacci et al., the presence of depression symptoms were reported to be positively correlated with the frequency of headache attacks (8). Additionally, Song et al. reported that the frequency of migraine attacks and VAS scores were higher when patients with migraine had depression (29). In the current study, only MSPSS score was found to be associated (negatively) with BDI score. Similarly, in other studies, the increase in perceived social support has been reported to be associated with lower symptoms of depression in diffrent patient groups (25, 30–34). Although we did not find any association between BDI scores and the clinical characteristics of migraine patients in the current study, we showed a relationship between social support and depressive symptoms, which is similar to the majority of studies on this topic.
Anxiety disorders have been reported to be associated with migraine, and the risk of anxiety disorder is reported to increase up to 5.3-folds in those with migraine (7). In the current study, no correlation was found between VAS scores and STAI, STAI-S and STAI-T scores. Conversely, Song et al., reported that the frequency of migraine attacks and migraine VAS scores were higher in patients with anxiety (29). Although we did not find any relationship between VAS scores and anxiety in the current study, we did find that STAI-S and STAI scores were positively correlated with the number of days with migraine pain per month and the number of migraine attacks per month, indicating a clinically relevant relationship. Similarly, Baldacci et al. reported a positive correlation between the presence of anxiety symptoms and the frequency of migraine attacks (8).
In a study examining the relationships between migraine and various psychiatric disorders, it was reported that the relationship between anxiety disorder and migraine was stronger than other psychiatric disorders (35). In another study, it was reported that anxiety symptoms are more strongly associated with migraine than the symptoms of depression (5). According to a study in Korea, migraine attack frequency and VAS scores were found to be higher in those who had both anxiety and depression. The authors also found that attack frequency and VAS scores were higher in those who only had anxiety compared to those who only had depression (36). In the current study, BDI was not correlated with clinical characteristics, while STAI scores were associated with the number of days with migraine pain and the number of migraine attacks in a month; therefore, our findings suggest that anxiety is more closely associated with the clinical results of migraine compared to depression. This suggestion is supported by studies showing strong associations between anxiety disorders and various chronic pain conditions including migraine (8). When our findings are evaluated in the context of the literature on this topic, it may be feasible to suggest that the relationship between depression and anxiety is more pronounced in those with migraine. However, several previous studies have also reported higher rates of depressive findings in migraine patients compared to controls (6, 22, 37–39). Thus, further studies are necessary to evaluate the relationships between these conditions, and to determine whether the relationship between anxiety and migraine is indeed stronger than other conditions such as depression.
In regard to social support and its effects on migraine, we found that MSPSS scores were negatively correlated with STAI-T and STAI scores. Similarly, in the results of various studies, the increase in the level of perceived social support has been reported to reduce the level of anxiety (34, 40, 41). In the light of our findings and the results of previous studies, we believe that social support has a significant effect on the anxiety scores of patients with migraine. Therefore, providing adequate social support to these patients may be instrumental in preventing migraine attacks or at least reducing their frequency.
Limitations
The main limitation of our study is that it is a cross-sectional study. The cross-sectional research design does not allow us to precisely define causal relationships. Our second limitation was that the study was conducted with a limited number of patients who applied to the outpatient clinic. If we could have performed a community-based research, we could have obtained stronger evidence.
CONCLUSIONS
This study examined the relationship between depression, anxiety and social support in migraine patients. We found a positive correlation between anxiety and migraine severity, number of migraine days per month and number of migraine attacks per month, but no correlation was found between these values and depression. This result adds to the literature data suggesting that the relationship between migraine and anxiety is stronger than depression. We also found that perceived social support demonstrated significant negative correlations with depression and anxiety scores in patients with migraine. The inclusion of a control group also showed that BDI, STAI-T and STAI scores were higher, while MSPSS score was lower in patients compared to controls.
In the light of these results, it was concluded that it would be useful to evaluate depression and especially anxiety more closely in patients with migraine. Furthermore, increasing social support in patients with migraine could be instrumental in preventing or reducing the clinical severity of migraine. We believe our findings contribute to the literature in terms of providing data for the improvement of the management of migraine patients.
Footnotes
Ethics Committee Approval: Ethics committee approval was received by İstanbul Yeni Yüzyıl University, Science, Social and Non-Interventional Health Sciences Research Ethics Committee, decision number 2018/7.
Informed Consent: Patients who were admitted to our outpatient clinic with migraine were informed about the aim and subject of the study and their verbal consent was obtained.
Peer-review: Externally peer-reviewed
Author Contributions: Concept – ÜFD; Design – OB; Supervision – ÜFD; Data Collection and/or Processing – ÜFD; Analysis and/or Interpretation –OB; Literature Search – ÜFD; Writing Manuscript – ÜFD, OB.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: No financial support has been received from any institution or person for this study.
REFERENCES
- 1.Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, Ansha MG, Barac A, Bensenor IM, Doan LP. GBD 2016. Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache 1990–2016:a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–976. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobayashi K, Tha KK, Terae S, Iijima Y, Katabami K, Minami Y, Uegaki S, Gando S, Shirato H. Improved detection of heat stroke-induced brain injury by high b-value diffusion-weighted imaging. J Comput Assist Tomogr. 2011;35:498–500. doi: 10.1097/RCT.0b013e3182220082. [DOI] [PubMed] [Google Scholar]
- 3.Burstein R, Noseda R, Borsook D. Migraine:multiple processes, complex pathophysiology. J Neurosci. 2015;35:6619–6629. doi: 10.1523/JNEUROSCI.0373-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sengul Y, Sengul HS, Tunc A. Psychoform and somatoform dissociative experiences in migraine:relationship with pain perception and migraine related disability. Ideggyogyaszati Szemle. 2018;71:385–392. doi: 10.18071/isz.71.0385. [DOI] [PubMed] [Google Scholar]
- 5.Peres MFP, Mercante JP, Tobo PR, Kamei H, Bigal ME. Anxiety and depression symptoms and migraine:a symptom-based approach research. J Headache Pain. 2017;18:37. doi: 10.1186/s10194-017-0742-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bag B, Hacihasanoglu R, Tufekci F. Examination of anxiety, hostility and psychiatric disorders in patients with migraine and tension-type headache. Int J Clin Pract. 2005;59:515–521. doi: 10.1111/j.1368-5031.2005.00522.x. [DOI] [PubMed] [Google Scholar]
- 7.Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. 2006;46:1327–1333. doi: 10.1111/j.1526-4610.2006.00576.x. [DOI] [PubMed] [Google Scholar]
- 8.Baldacci F, Lucchesi C, Cafalli M, Poletti M, Ulivi M, Vedovello M, Giuntini M, Mazzucchi S, Del Prete E, Vergallo A, Nuti A, Gori S. Migraine features in migraineurs with and without anxiety-depression symptoms:A hospital-based study. Clin Neurol Neurosurg. 2015;132:74–78. doi: 10.1016/j.clineuro.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 9.D'amico D, Grazzi L, Bussone G, Curone M, Di Fiore P, Usai S, Leonardi M, Giovannetti AM, Schiavolin S, Raggi A. Are Depressive Symptomatology, Self-Efficacy, and Perceived Social Support Related to Disability and Quality of Life in Patients With Chronic Migraine Associated to Medication Overuse?Data from a Cross-Sectional Study. Headache. 2015;55:636–645. doi: 10.1111/head.12534. [DOI] [PubMed] [Google Scholar]
- 10.Teoh H, Tam C. A comparison of headache and non-headache sufferers on measures of social support and mental health problems. Malays Fam Physician. 2008;3:82–86. [PMC free article] [PubMed] [Google Scholar]
- 11.Martin PR, Soon K. The relationship between perceived stress, social support and chronic headaches. Headache. 1993;33:307–314. doi: 10.1111/j.1526-4610.1993.hed3306307.x. [DOI] [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd Edition Cephalalgia. 2018 Jan;38(1):1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 13.Hisli Şahin N. A reliability and validity study of Beck Depression Inventory in a university student sample. Türk Psikoloji Derg. 1989;7:3–13. [Google Scholar]
- 14.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 15.Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR. State-trait anxiety inventory (STAI) BiB. 2010;1970:180. [Google Scholar]
- 16.Öner N, Le Compte A. Durumluluk-sürekli kaygıenvanteri elkitabı. İstanbul: Boğaziçi Üniversitesi Matbaası; 1983. [Google Scholar]
- 17.Eker D, Arkar H. Factorial Structure, Validity, and Reliability of the Multidimensional Scale of Perceived Social Support. Türk Psikoloji Derg. 1995;34:45–55. [Google Scholar]
- 18.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain:Visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), mcgill pain questionnaire (MPQ), short-form mcgill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63:S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 19.Tan HJ, Suganthi C, Dhachayani S, Mohd Rizal A, Raymond A. The coexistence of anxiety and depressive personality traits in migraine. Singapore Med J. 2007;48:307–310. [PubMed] [Google Scholar]
- 20.Karaca S, Demir F, Herken H, Demir O, Aşkın R. Kronik Ağrılıve Migrenli Hastalarda Depresyon Düzeyleri ve Ağrıile Başaçıkma Becerileri 1. Düşünen Adam. 1999;12:31–33. [Google Scholar]
- 21.Yaşar H, Balıbey H, Alay S, Tekeli H, Türker T, Bayar N. Migren hastalarında anksiyete, depresyon ve obsesif-kompulsif belirti düzeyleri. J Mood Disord. 2013;3:156–161. [Google Scholar]
- 22.Perozzo P, Savi L, Castelli L, Valfrè W, Giudice RL, Gentile S, Rainero I, Pinessi L. Anger and emotional distress in patients with migraine and tension-type headache. J Headache Pain. 2005;6:392–399. doi: 10.1007/s10194-005-0240-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadeghniiat K, Rajabzadeh A, Ghajarzadeh M, Ghafarpour M. Sleep quality and depression among patients with migraine. Acta Med Iran. 2013;51:784–788. [PubMed] [Google Scholar]
- 24.Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Sex Differences in Prevalence, Symptoms, Impact, and Psychiatric Comorbidities in Migraine and Probable Migraine:A Population-Based Study. Headache. 2019;59:215–223. doi: 10.1111/head.13470. [DOI] [PubMed] [Google Scholar]
- 25.Korkmaz T, Tel H. KOAH'lıhastalarda anksiyete, depresyon ve sosyal destek durumunun belirlenmesi. Anadolu Hemşirelik ve Sağlık Bilimleri Derg. 2010;13:79–86. [Google Scholar]
- 26.Yong N, Hu H, Fan X, Li X, Ran L, Qu Y, Wang Y, Tan G, Chen L, Zhou J. Prevalence and risk factors for depression and anxiety among outpatient migraineurs in mainland China. J Headache Pain. 2012;13:303–310. doi: 10.1007/s10194-012-0442-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dworkin SF, Von Korff M, LeResche L. Multiple pains and psychiatric disturbance:an epidemiologic investigation. Arch Gen Psychiatry. 1990;47:239–244. doi: 10.1001/archpsyc.1990.01810150039007. [DOI] [PubMed] [Google Scholar]
- 28.Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms:a prospective study of depression as a risk factor. Pain. 1993;55:251–258. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- 29.Song TJ, Cho SJ, Kim WJ, Yang KI, Yun CH, Chu MK. Anxiety and depression in probable migraine:A population-based study. Cephalalgia. 2017;37:845–854. doi: 10.1177/0333102416653235. [DOI] [PubMed] [Google Scholar]
- 30.Yoo H, Shin DW, Jeong A, Kim SY, Yang HK, Kim JS, Lee JE, Oh JH, Park EC, Park K. Perceived social support and its impact on depression and health-related quality of life:a comparison between cancer patients and general population. Jpn J Clin Oncol. 2017;47:728–734. doi: 10.1093/jjco/hyx064. [DOI] [PubMed] [Google Scholar]
- 31.Eom CS, Shin DW, Kim SY, Yang HK, Jo HS, Kweon SS, Kang YS, Kim JH, Cho BL, Park JH. Impact of perceived social support on the mental health and health-related quality of life in cancer patients:results from a nationwide, multicenter survey in South Korea. Psychooncology. 2013;22:1283–1290. doi: 10.1002/pon.3133. [DOI] [PubMed] [Google Scholar]
- 32.Billedo CJ, Kerkhof P, Finkenauer C, Ganzeboom H. Facebook and Face-to-Face:Examining the Short-and Long-Term Reciprocal Effects of Interactions, Perceived Social Support, and Depression among International Students. J Computer-Mediated Communication. 2019;24:73–89. [Google Scholar]
- 33.Hann D, Baker F, Denniston M, Gesme D, Reding D, Flynn T, Kennedy J, Kieltyka RL. The influence of social support on depressive symptoms in cancer patients:age and gender differences. J Psychosom Res. 2002;52:279–283. doi: 10.1016/s0022-3999(01)00235-5. [DOI] [PubMed] [Google Scholar]
- 34.Shafaie FS, Mirghafourvand M, Rahmati M, Nouri P, Bagherinia M. Association between psychological status with perceived social support in pregnant women referring to Tabriz health centers. J Matern Fetal Neonatal Med. 2018;31:1554–1560. doi: 10.1080/14767058.2017.1319934. [DOI] [PubMed] [Google Scholar]
- 35.Merikangas KR, Angst J, Isler H. Migraine and psychopathology:results of the Zurich cohort study of young adults. Arch Gen Psychiatry. 1990;47:849–853. doi: 10.1001/archpsyc.1990.01810210057008. [DOI] [PubMed] [Google Scholar]
- 36.Oh K, Cho S-J, Chung YK, Kim J-M, Chu MK. Combination of anxiety and depression is associated with an increased headache frequency in migraineurs:a population-based study. BMC Neurol. 2014;14:238. doi: 10.1186/s12883-014-0238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nicholson RA, Gramling SE, Ong JC, Buenevar L. Differences in anger expression between individuals with and without headache after controlling for depression and anxiety. Headache. 2003;43:651–663. doi: 10.1046/j.1526-4610.2003.03108.x. [DOI] [PubMed] [Google Scholar]
- 38.Dikmen PY, Yavuz BG, Aydinlar EI. The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Acta Neurol Belg. 2015;115:117–122. doi: 10.1007/s13760-014-0312-0. [DOI] [PubMed] [Google Scholar]
- 39.Chu HT, Liang CS, Lee JT, Yeh TC, Lee MS, Sung YF, Yang FC. Associations between depression/anxiety and headache frequency in migraineurs:a cross-sectional study. Headache. 2018;58:407–415. doi: 10.1111/head.13215. [DOI] [PubMed] [Google Scholar]
- 40.Glazier R, Elgar F, Goel V, Holzapfel S. Stress, social support, and emotional distress in a community sample of pregnant women. J Psychosom Obstet Gynecol. 2004;25:247–255. doi: 10.1080/01674820400024406. [DOI] [PubMed] [Google Scholar]
- 41.Çavuşoğlu H, Sağlam H. Examining the perceived social support and psychological symptoms among adolescents with leukemia. J Spec Pediatr Nurs. 2015;20:76–85. doi: 10.1111/jspn.12101. [DOI] [PubMed] [Google Scholar]


