Abstract
BACKGROUND
Hypertension guidelines recommend home blood pressure monitoring (HBPM) to help achieve blood pressure (BP) control. We hypothesized that HBPM use with a physician recommendation would be associated with lower BP and greater medication adherence.
METHODS
We used data from 6,320 adults with hypertension in the National Health and Nutrition Examination Survey 2009–2014 to characterize the association of (i) provider recommendation for HBPM and (ii) HBPM use on 2 outcomes: measured BP (linear regression) and medication adherence (logistic regression). Provider recommendation, HBPM use, and medication use were self-reported.
RESULTS
Among adults with hypertension, 30.1% reported a physician recommendation for HBPM, among whom 82.0% reported using HBPM. Among those who did not report a physician recommendation for HBPM, 28.3% used HBPM. Factors associated with a physician recommendation were having health insurance, higher education attainment, hypertension awareness, and having a prescription for antihypertensive medication. Among those who reported receiving a physician recommendation, those who used HBPM had a mean BP that was 3.1/4.5 mm Hg lower than those who did not. Those who reported having a physician recommendation and using HBPM were more likely to report hypertension medication adherence (odds ratio 2.9; 95% confidence interval: 2.0, 4.4).
CONCLUSIONS
HBPM use was associated with lower BP and higher medication adherence. Use of HBPM was higher among those with a physician recommendation. These results support a role for physicians in counseling and partnering with patients on HBPM use for BP management.
Keywords: blood pressure, home blood pressure monitoring, hypertension, NHANES
Accurate blood pressure (BP) measurement is a critical component of hypertension treatment and management. While BP measured in clinic office settings have conventionally dictated treatment decisions, there is growing evidence that the quality and accuracy of clinic-based measurements varies substantially.1–3 Because of these concerns, professional societies and practice guidelines, both in the United States4–7 and abroad,8,9 increasingly advocate for the use of home blood pressure monitoring (HBPM) to assist in the diagnosis and management of hypertension. These recommendations are based on clinical trials showing a short-term benefit of HBPM in lowering BP10 and improving patient engagement with treatment.5 Larger effects on BP lowering have been observed when HBPM was coupled with clinical action such as medication titration,11 highlighting the complementary roles of the health provider and patient in HBPM use and interpretation.
Prior studies in US adults have assessed population characteristics associated with HBPM, and found that a physician recommendation for HBPM was more common among HBPM users compared with those who did not report using HBPM.12,13 Furthermore, US adults using HBPM were more likely to have diagnosed, treated, or controlled hypertension.12,13 Complementing HBPM with additional clinician support has been shown to have a more robust impact on BP control compared with HBPM alone.14 Therefore, we assessed whether having a physician recommendation modified the association of HBPM and measured BP or self-reported medication use among US adults with hypertension.
The objectives of our study are (i) to characterize sociodemographic and clinical factors associated with self-reported HBPM and physician recommendation for HBPM and (ii) to assess the associations of HBPM and physician recommendation with measured BP and medication use among those who recalled having been told to take BP lowering medication. We hypothesized that physicians would be more likely to recommend HBPM to higher risk patients (e.g., older, with comorbidities), and that HBPM use would be associated with lower BP and higher medication adherence, particularly among those who reported a physician recommendation for HBPM.
METHODS
Study population
The continuous National Health and Nutrition Examination Survey (NHANES) 2009–2014 are a program of surveys, conducted by the National Center for Health Statistics over 3, 2-year cycles. The NHANES employ a multistage sampling approach to select a nationally representative sample of participants. In these 3 survey cycles, a total of 17,547 adults over the age of 20 underwent a home interview, physical examination, and laboratory testing. Hypertension status was defined by a self-report of a prior diagnosis of hypertension (N = 6,426) or a systolic BP ≥140 or diastolic BP ≥90 mm Hg at the NHANES examination without a prior diagnosis (N = 968). We excluded participants who self-reported being pregnant or who had a positive lab pregnancy test.15–17 Among this population of nonpregnant adults with hypertension, complete data were available for 6,366 participants, who comprised our analytic population.
Definition of main exposure
Provider recommendation and HBPM use were self-reported in response to the questions “Did a doctor tell you to take your blood pressure at home? (yes/no)” and “Did you take your blood pressure at home during the past 12 months? (yes/no),” respectively.18–20
Outcome definitions
All systolic and diastolic BP measurements were obtained at the NHANES mobile examination clinic by trained physicians using calibrated mercury sphygmomanometers. Participants were asked to rest for 5 minutes, after which their maximum inflation level was determined and triplicate measurements were made, separated by 30 seconds each.21 Mean BP was defined based on an average of up to 3 BP measurements at the NHANES examination visit. Hypotension status was defined as a mean BP <90/60 mm Hg.22
A subgroup of 4,637 participants self-reported ever having been told to take prescription medication for high BP, based on a “yes” response to the question, “Because of your (high BP/hypertension), you ever been told to take prescribed medicine?” Among this subgroup, antihypertensive medication adherence was defined based on a “yes” response to the question, “Are you now taking prescribed medication?” 18–20
Covariate definitions
Age was modeled categorically in 10-year intervals from 20 to 80+ years. Race was self-reported and classified as non-Hispanic White, non-Hispanic Black, Mexican American, non-Mexican Hispanic, and Other (includes non-Hispanic Asians, who were oversampled starting in 2011). We examined the following additional self-reported factors: marital status (single, never married; married/living with partner; widowed/divorced/separated), current smoking status (yes/no), education (less than high school, high school/General Education Development, some college, beyond college), income–poverty ratio (not in poverty, >1.3, borderline poverty, 1.0–1.3, poverty, <1.0; 7.2% were unknown), having health insurance (yes, no), having a usual health care site (yes, no), and diabetes status (yes, no). Stage 3–5 chronic kidney disease (CKD) status was defined as an estimated glomerular filtration rate of <60 ml/min/1.73 m2, calculated using the Chronic Kidney Disease Epidemiology Collaboration equation23 based on laboratory standardized creatinine measurements. Hypertension duration was derived based on the difference between participant age at the NHANES visit and self-reported age at hypertension diagnosis. Those detected at the examination were assigned a duration of 0 years. Frequency of HBPM was based on self-report in response to the question: “How often did you check blood pressure at home during the last 12 months?” 18–20 and categorized as following: less than monthly (<12), monthly to weekly (12 to <52), weekly to daily (52 to <365), and more than once a day (≥365).
Statistical analysis
The NHANES mobile examination clinic weights were used to account for the multilevel survey design and participant nonresponse. Variance was estimated using Taylor series linearization. Multivariable linear regression was used in analyses with systolic or diastolic BP as the outcome. Multivariable logistic regression was used to model current medication use among the subset of participants who reported ever having been told to take prescription medication. Models were unadjusted (Model 0), adjusted for age, sex, and race (Model 1), and additionally adjusted for income:poverty ratio, education, marital status, current smoking, body mass index category, insurance, having a regular healthcare site, self-reported health, diagnosed diabetes, diagnosed hypertension, stage 3–5 CKD, and hypertension duration (Model 2). Interactions between HBPM and having received a doctor’s recommendation were assessed using Wald’s test of the interaction term and the following categories: (i) Using HBPM and reporting a doctor’s recommendation; (ii) using HBPM and not reporting a doctor’s recommendation; (iii) not using HBPM and reporting a doctor’s recommendation; and (iv) not using HBPM and not reporting a doctor’s recommendation. All analyses were conducted using the survey package in Stata 15.1 (College Station, TX).24
RESULTS
Among US adults over the age of 20 with hypertension and with complete demographic and socioeconomic data, 30.1% reported receiving a physician recommendation for HBPM, among whom 82.0% of this group reported performing HBPM at least once in the past year. Of the 70.2% who did not report receiving a recommendation for HBPM, 28.3% reported HBPM use at least once in the past year. Several demographic and socioeconomic factors differed among subgroups defined by having a physician recommendation and HBPM use, including age, body mass index, having a regular healthcare site, self-reported diabetes status, and hypertension duration (Table 1).
Table 1.
Characteristics of US adults with hypertension by self-reported home blood pressure monitoring status
| Characteristic | Unweighted N overall | Overall | Use home blood pressure monitoring | Do not use home blood pressure monitoring | ||
|---|---|---|---|---|---|---|
| Doctor recommendation | No recommendation | Doctor recommendation | No recommendation | |||
| Unweighted N | 6,366 | 1,542 | 1,242 | 346 | 3,236 | |
| Weighted N | 76,120,230 | 18,857,590 | 15,143,959 | 4,175,825 | 37,942,857 | |
| Age, weighted % | ||||||
| 20–29 | 244 | 4.8 | 2.0 | 3.4 | 3.9 | 6.9 |
| 30–39 | 533 | 9.3 | 7.5 | 6.0 | 10.2 | 11.4 |
| 40–49 | 879 | 15.8 | 15.7 | 12.1 | 20.0 | 16.9 |
| 50–59 | 1,224 | 23.5 | 21.0 | 22.0 | 25.2 | 25.1 |
| 60–69 | 1,624 | 22.3 | 21.9 | 26.0 | 21.0 | 21.1 |
| 70–79 | 1,151 | 15.1 | 20.2 | 20.3 | 12.2 | 10.9 |
| 80+ | 711 | 9.2 | 11.7 | 10.2 | 7.5 | 7.8 |
| Female, weighted % | 3,190 | 50.6 | 55.1 | 51.7 | 50.3 | 47.9 |
| Race, weighted % | ||||||
| Non-Hispanic White | 2,815 | 69.7 | 72.1 | 72.9 | 65.2 | 67.8 |
| Non-Hispanic Black | 1,707 | 14.1 | 13.6 | 12.8 | 17.7 | 14.4 |
| Mexican American | 723 | 5.8 | 4.5 | 3.5 | 5.6 | 7.4 |
| Non-Mexican Hispanic | 550 | 4.4 | 3.5 | 3.5 | 5.1 | 5.1 |
| Other | 571 | 6.0 | 6.3 | 7.3 | 6.4 | 5.3 |
| Education, weighted % | ||||||
| Less than high school | 1,811 | 19.6 | 17.4 | 17.9 | 21.2 | 21.2 |
| High school/GED | 1,550 | 24.2 | 23.0 | 24.1 | 23.1 | 25.0 |
| Some college | 1,817 | 31.8 | 31.4 | 34.3 | 29.4 | 31.4 |
| Beyond college | 1,188 | 24.3 | 28.2 | 23.7 | 26.3 | 22.5 |
| BMI, weighted % | ||||||
| <25 | 1,258 | 18.5 | 18.7 | 19.0 | 14.3 | 18.6 |
| 25–30 | 2,037 | 32.3 | 30.8 | 35.2 | 27.6 | 32.3 |
| 30+ | 3,071 | 49.3 | 50.6 | 45.8 | 58.1 | 49.1 |
| Hypertension awareness, weighted % | 5,440 | 85.6 | 97.5 | 86.4 | 93.3 | 78.5 |
| Antihypertensive prescription, weighted % | 4,685 | 72.0 | 92.6 | 76.6 | 82.7 | 58.7 |
| Income–poverty ratio, weighted % | ||||||
| Not in poverty (>1.3) | 3,790 | 71.3 | 74.7 | 74.2 | 70.4 | 68.5 |
| Borderline poverty (1.0–1.3) | 722 | 8.2 | 6.7 | 6.7 | 11.6 | 9.3 |
| Poverty (<1.0) | 1,321 | 13.8 | 11.4 | 12.1 | 14.5 | 15.7 |
| Unknown | 533 | 6.7 | 7.2 | 7.0 | 3.6 | 6.6 |
| Current smoker, weighted % | 1,422 | 22.0 | 16.3 | 21.9 | 23.7 | 24.7 |
| Any health insurance, weighted % | 5,353 | 87.2 | 92.9 | 88.6 | 88.2 | 83.7 |
| Have regular health site, weighted % | 5,803 | 91.9 | 97.3 | 93.0 | 93.0 | 88.6 |
| Self-reported health status, weighted % | ||||||
| Excellent/very good | 1,745 | 34.5 | 31.1 | 35.9 | 28.7 | 36.2 |
| Very good | 2,465 | 39.0 | 40.3 | 38.4 | 37.8 | 38.8 |
| Fair/poor | 2,156 | 26.5 | 28.6 | 25.7 | 33.5 | 25.0 |
| Marital status, weighted % | ||||||
| Single, never married | 742 | 11.0 | 6.4 | 7.8 | 13.0 | 14.4 |
| Married, living with partner | 3,647 | 62.7 | 68.1 | 68.1 | 57.7 | 58.5 |
| Widowed, divorced, separated | 1,977 | 26.2 | 25.5 | 24.1 | 29.3 | 27.1 |
| Self-reported diabetes, weighted % | 1,453 | 19.1 | 24.5 | 17.9 | 21.3 | 16.7 |
| Stage 3–5 chronic kidney disease, weighted % | 1,019 | 14.1 | 18.1 | 16.3 | 14.7 | 11.2 |
| Hypertension duration, mean (SE) years | 6,366 | 9.6 (0.2) | 11.8 (0.3) | 10.1 (0.4) | 10.6 (0.7) | 8.1 (0.2) |
| Frequency of HBPM, weighted % | ||||||
| Less than monthly | 4,128 | 65.5 | 13.4 | 29.6 | — | — |
| Monthly to weekly | 793 | 13.9 | 27.8 | 34.1 | — | — |
| Weekly to daily | 864 | 12.6 | 33.4 | 25.6 | — | — |
| At least daily | 581 | 8.0 | 25.4 | 10.7 | — | — |
Abbreviations: BMI, body mass index; GED, General Education Development; HBPM, home blood pressure monitoring.
The following sociodemographic and clinical factors were independently associated with HBPM: age, non-Hispanic Black race, income:poverty ratio, education status, and self-reported having a prescription for antihypertensive medications (Supplementary Table S1 online). Meanwhile, having insurance (odds ratio (OR) 1.3; 95% confidence interval (CI): 1.1, 1.7), higher educational attainment (beyond college OR 1.5; 95% CI: 1.2, 1.9), hypertension awareness (OR 2.0; 95% CI: 1.3, 3.2), and having a prescription for antihypertensive medication (OR 3.8; 95% CI: 2.8, 5.3) were independently associated with having received a physician recommendation for HBPM (Table 2). With adjustment for demographic characteristics, those with diabetes were more likely to report having received a recommendation for HBPM (OR 1.5; 95% CI 1.3, 1.7), but those with CKD (OR 1.2; 95% CI 1.0, 1.5) did not (Table 2, Model 1). Neither remained associated with reported HBPM recommendation with adjustment for other covariates (Table 2, Model 2).
Table 2.
Odds ratio (95% CI) of factors associated with receiving a physician recommendation for home blood pressure monitoring, unweighted N = 6,366
| Factor | Unadjusted | Model 1a | Model 2b |
|---|---|---|---|
| Age | |||
| 20–29 | REF | REF | REF |
| 30–39 | 2.0 (1.1, 3.6)* | 2.0 (1.1, 3.7)* | 1.1 (0.6, 2.1) |
| 40–49 | 2.7 (1.5, 4.6)** | 2.6 (1.5, 4.6)** | 1.1 (0.6, 1.9) |
| 50–59 | 2.3 (1.3, 3.8)** | 2.2 (1.3, 3.7)** | 0.8 (0.4, 1.4) |
| 60–69 | 2.4 (1.5, 4.1)** | 2.4 (1.4, 4.0)** | 0.7 (0.4, 1.4) |
| 70–79 | 3.5 (2.0, 6.0)*** | 3.3 (1.9, 5.8)*** | 1.0 (0.5, 1.9) |
| 80+ | 3.2 (1.9, 5.5)*** | 3.1 (1.8, 5.2)*** | 0.9 (0.5, 1.8) |
| Female | 1.2 (1.0, 1.5)* | 1.2 (1.0, 1.4)* | 1.1 (0.9, 1.3) |
| Race/ethnicity | |||
| Non-Hispanic White | REF | REF | REF |
| Non-Hispanic Black | 1.0 (0.8, 1.2) | 1.1 (0.9, 1.3) | 1.1 (0.9, 1.3) |
| Mexican American | 0.7 (0.5, 1.0) | 0.8 (0.6, 1.1) | 0.9 (0.7, 1.3) |
| Non-Mexican Hispanic | 0.8 (0.6, 1.1) | 0.8 (0.6, 1.1) | 0.9 (0.7, 1.2) |
| Other | 1.1 (0.7, 1.5) | 1.1 (0.8, 1.6) | 1.2 (0.8, 1.7) |
| Have insurance | 2.0 (1.7, 2.4)*** | 1.8 (1.5, 2.2)*** | 1.3 (1.1, 1.7)** |
| Have regular health site | 3.1 (2.2, 4.5)*** | 2.6 (1.8, 3.8)*** | 1.5 (1.0, 2.3) |
| Income–poverty ratio | |||
| Not in poverty (>1.3) | REF | REF | REF |
| Borderline poverty (1.0–1.3) | 0.8 (0.7, 1.0) | 0.8 (0.7, 1.0) | 0.9 (0.8, 1.2) |
| Poverty (<1.0) | 0.8 (0.6, 0.9)** | 0.8 (0.7, 1.0)* | 0.9 (0.7, 1.2) |
| Unknown | 0.9 (0.7, 1.3) | 0.9 (0.6, 1.3) | 0.9 (0.7, 1.3) |
| Marital status | |||
| Single, never married | REF | REF | REF |
| Married, living with partner | 1.8 (1.2, 2.6)** | 1.5 (1.1, 2.3)* | 1.4 (1.0, 2.1) |
| Widowed, divorced, separated | 1.6 (1.2, 2.4)** | 1.3 (0.9, 1.8) | 1.2 (0.9, 1.7) |
| Education | |||
| Less than high school | REF | REF | REF |
| High school/GED | 1.0 (0.8, 1.3) | 1.1 (0.8, 1.3) | 1.1 (0.9, 1.3) |
| Some college | 1.1 (0.9, 1.3) | 1.1 (0.9, 1.4) | 1.1 (0.9, 1.4) |
| Beyond college | 1.4 (1.1, 1.7)** | 1.5 (1.2, 1.8)** | 1.5 (1.2, 1.9)** |
| Current smoker | 0.7 (0.6, 0.8)*** | 0.7 (0.6, 0.9)** | 0.8 (0.7, 1.0) |
| BMI | |||
| <25 | REF | REF | REF |
| 25–30 | 1.0 (0.8, 1.2) | 1.0 (0.8, 1.2) | 0.8 (0.6, 1.0) |
| 30+ | 1.1 (0.9, 1.4) | 1.2 (1.0, 1.5) | 0.9 (0.7, 1.1) |
| Self-reported health | |||
| Excellent/very good | REF | REF | REF |
| Good | 1.2 (1.0, 1.5) | 1.2 (1.0, 1.5) | 1.2 (0.9, 1.5) |
| Fair/poor | 1.4 (1.1, 1.7)** | 1.4 (1.1, 1.7)** | 1.3 (1.0, 1.7) |
| Self-reported diabetes | 1.5 (1.3, 1.8)*** | 1.5 (1.3, 1.7)*** | 1.2 (1.0, 1.4) |
| Self-reported diagnosed hypertension | 7.1 (5.0, 10.0)*** | 6.9 (4.9, 9.8)*** | 2.0 (1.3, 3.2)** |
| Prescription for hypertension medication | 5.6 (4.5, 7.0)*** | 5.7 (4.4, 7.5)*** | 3.8 (2.8, 5.3)*** |
| Stage 3–5 chronic kidney disease | 1.5 (1.2, 1.8)*** | 1.2 (1.0, 1.5) | 1.1 (0.9, 1.3) |
| Hypertension duration, per 5 years | 1.1 (1.1, 1.2)*** | 1.1 (1.1, 1.1)*** | 1.0 (1.0, 1.0) |
Abbreviations: BMI, body mass index; CI, confidence interval; GED, General Education Development.
aAdjusted for age, sex, and race/ethnicity.
bAdjusted for all covariates.
*P < 0.05.
**P < 0.01.
***P < 0.001.
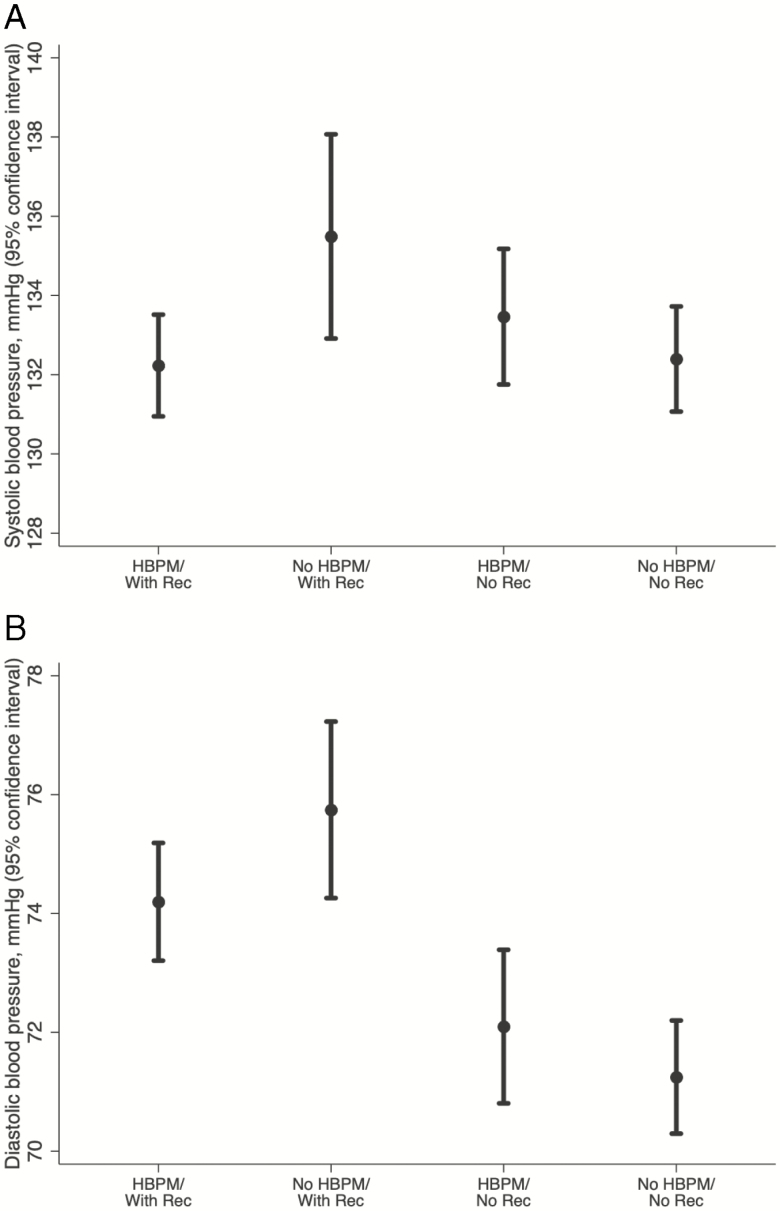
Among those who did not report receiving a physician recommendation for HBPM, HBPM use was not associated with a difference in systolic BP (1.2 mm Hg; 95% CI: −0.7, 3.2), but was associated with lower diastolic BP (−2.0 mm Hg; 95% CI: −3.6, −0.6). Among those who reported a physician recommendation, HBPM was associated with a lower systolic (−3.1 mm Hg; 95% CI: −5.7, −0.5) and diastolic (−4.5 mm Hg; −6.2, −2.8) BP (Figure 1). Compared with those who did not use HBPM and did not recall a physician recommendation for HBPM, those with a recommendation, who did not report HBPM use had a higher average BP, even after adjustment for demographic and health characteristics (Table 3). However, those who received a recommendation and engaged in HBPM did not have a significant difference in measured BP compared with those who did not use HBPM and did not recall a physician recommendation for HBPM (Table 3). The prevalence of hypotension was rare (0.4%; 95% CI: 0.2%, 0.7%) and was not associated with either HBPM (crude OR 1.5; 95% CI: 0.5, 4.9) or having a doctor’s recommendation for HBPM (crude OR 1.1; 95% CI: 0.3, 4.3).
Figure 1.
Mean (a) systolic and (b) diastolic blood pressure (mm Hg) by home blood pressure monitoring (HBPM) and physician recommendation status.
Table 3.
Differences in mean measured blood pressure among participants based on use home blood pressure monitoring and recall of physician recommendation for home blood pressure monitoring
| Outcome | Unweighted N | Unadjusted | Model 1 | Model 2 |
|---|---|---|---|---|
| SBP, β (95% CI) | 6,366 | |||
| No physician recommendation/no HBPM | 0 (reference) | 0 (reference) | 0 (reference) | |
| No physician recommendation/HBPM | 1.2 (−0.7, 3.2) | 0.0 (−2.0, 2.0) | 1.7 (0.1, 3.3) | |
| Physician recommendation/no HBPM | 3.3 (0.8, 5.7) | 3.0 (0.7, 5.3) | 6.3 (4.3, 8.3) | |
| Physician recommendation/HBPM | 0.2 (−1.2, 1.6) | −1.1 (−2.5, 0.4) | 3.1 (1.7, 4.5) | |
| Interaction term P value | 0.009 | 0.013 | 0.001 | |
| DBP, β (95% CI) | 6,366 | |||
| No physician recommendation/no HBPM | 0 (reference) | 0 (reference) | 0 (reference) | |
| No physician recommendation/HBPM | −2.1 (−3.6, −0.6) | −0.3 (−1.6, 1.0) | 0.4 (−0.9, 1.6) | |
| Physician recommendation/no HBPM | 1.5 (0.1, 3.0) | 1.5 (0.1, 3.0) | 3.1 (1.7, 4.4) | |
| Physician recommendation/HBPM | −2.9 (−4.0, −1.9) | −1.3 (−2.3, −0.3) | 0.6 (−0.3, 1.5) | |
| Interaction term P value | 0.014 | 0.006 | 0.002 |
Model 1: adjusted for age, sex, and race. Model 2: Model 1 + income:poverty ratio, education, marital status, current smoking, BMI category, insurance, having a regular healthcare site, self-reported health, diagnosed diabetes, diagnosed hypertension, stage 3–5 chronic kidney disease, and hypertension duration. Abbreviations: BMI, body mass index; CI, confidence interval; DBP, diastolic blood pressure; HBPM, home blood pressure monitoring; SBP, systolic blood pressure.
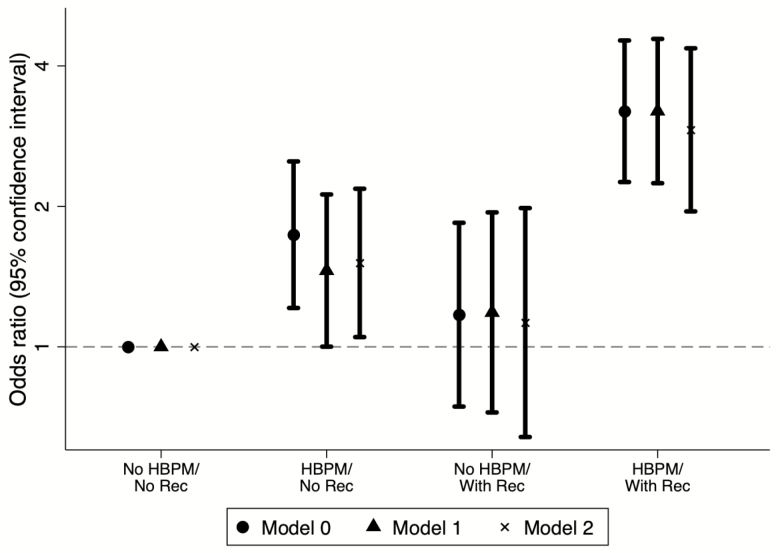
Among those who reported ever having been told to take an antihypertensive prescription (N = 4,685), those who received a physician recommendation and used HBPM were more likely to report currently taking BP medications (OR 2.9; 95% CI: 2.0, 4.4). Those who received a physician recommendation but did not use HBPM were not more likely to report medication use (OR 1.1; 95% CI: 0.6, 2.0), while those who used HBPM without a physician recommendation were modestly more likely to use medications (OR 1.5; 95% CI: 1.0, 2.1) (Figure 2; Model 2).
Figure 2.
Association of hypertension medication use (yes vs. no) in past 12 months with home blood pressure monitoring and physician recommendation for home monitoring among 4,637 participants with a self-reported prescription for hypertension medication. Model 1 was adjusted for age, sex, and race. Model 2 includes additional adjustment for income–poverty ratio categories, educational attainment, marital status, current smoking status, BMI categories, having insurance, having a regular health site, self-reported health category, self-reported diabetes, self-reported hypertension, self-reported prescription for hypertension medication, stage 3–5 chronic kidney disease, and hypertension duration. Abbreviation: HBPM, home blood pressure monitoring.
In our large, representative study of US adults with hypertension, we characterized the relationship between HBPM use and physician recommendations for HBPM with lower BP and antihypertensive medication use. Most US adults in NHANES 2011–2014 with hypertension did not report using HBPM and did not report a physician recommendation for HBPM use. Among the population who have been recommended for HBPM, HBPM use was associated with lower systolic and diastolic BP and a higher odds of self-reported antihypertensive medication use.
Physician recommendation plays an important role in HBPM use. We observed that over half of adults with hypertension who had a physician recommendation for HBPM used HBPM. However, only 30% of all US adults with hypertension had a recommendation for HBPM. Having health insurance, a college education, a hypertension diagnosis, or hypertension treatment were associated with being recommended for HBPM regardless of demographic characteristics, suggesting that a lack of healthcare access may be a barrier for HBPM recommendations. Other barriers that were not assessed in NHANES (e.g., the cost of devices, insurance coverage and reimbursement for HBPM) should be explored in subsequent studies.
Our findings build upon a prior analysis of the full NHANES population, which showed an association of HBPM with age, race, hypertension awareness, diabetes status, and hypertension control.13 Here, we focused on adults with hypertension and assessed whether the relationship between HBPM and measured BP was modified by receiving a physician recommendation for HBPM use. Our findings are consistent with prior studies showing a greater reduction in BP among patients who monitor their BP at home,11,25 and with prior studies suggesting that home monitoring, even in the absence of coupled interventions such as medication titration programs, may be associated with slower decline in medication adherence compared with those who do not self-monitor.26 Our findings show these associations may be applicable to adults with hypertension.
Despite the literature supporting the benefits of home monitoring, this resource may be underutilized, both broadly, as most US adults with hypertension did not report being recommended by their physician to home monitor and did not engage in monitoring, and in high-risk subpopulations, such as those with kidney disease.27 While we observed higher rates of home monitoring among patients with diabetes compared with those without, this association was not seen among CKD patients. This may be partly due to the objective measure of creatinine used to define CKD status as CKD awareness is thought to be low in the United States.28 However, this is consistent with a study of CKD patients by Ye et al. which found the most common reason for not using HBPM was the lack of a recommendation to do so.29 A meta-analysis of prevalence estimates for masked and white coat hypertension in the CKD population suggests that about 40% of those with controlled clinic BP had uncontrolled BP at home, and 30% of those with uncontrolled BP in the clinic were controlled at home, highlighting the substantial discordance of home BP with clinic BP in this population.30 Our findings suggest there may be under-recommendation of HBPM in the CKD population.
There are several limitations to our analyses. Given the cross-sectional nature of NHANES, we are unable to comment on the temporality of the exposure and outcomes. It is possible that HBPM may contribute to improved BP control and medication use. Alternatively, we cannot rule out that those with better controlled hypertension or higher medication adherence might be more likely to engage in HBPM. Second, doctors may be selective in their recommendations for HBPM use. Indeed, we observed and controlled for potential confounders such as hypertension duration, diabetes status, and health care access which were differentially associated with self-reported doctor recommendation. However, there may also be unmeasured confounders such as a doctor’s perception of the compliance of the patient, which may also factor into their willingness to recommend this practice to their patients. This is consistent with the higher medication use among those who received a physician recommendation for home monitoring. Thus, whether providing a recommendation to a broader patient population will have similar effects remains to be seen. Third, our main exposures and covariates of interest were self-reported, and thus susceptible to misclassification. For example, some adults may not recall a diagnosis of hypertension. Finally, with the available data, we are unable to assess how participants were using HBPM and whether participants changed their hypertension management strategies (e.g., titration of medication) as a result of their monitoring. However, this is certainly possible given the higher prevalence of antihypertensive medications among adults using HBPM.
In conclusion, HBPM is associated with lower average BP and higher antihypertensive medication use among adults with hypertension, particularly among those who received a physician’s recommendation for HBPM. Despite the potential benefits of this practice, most adults with hypertension do not use HBPM and have not been told to do so by their physicians. Barriers to receiving a physician recommendation (e.g., heath disparities and insurance status) represent an important area for further intervention to improve both physician recommendation and patient uptake of HBPM.
FUNDING
SPJ supported by a National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute (NHLBI) K23HL135273. OT is supported by NIH/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) F30DK120160. KF is supported by NIH/NHLBI T32HL007024.
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
ACKNOWLEDGMENTS
We are indebted to the NHANES study participants.
REFERENCES
- 1. Campbell NR, Culleton BW, McKay DW. Misclassification of blood pressure by usual measurement in ambulatory physician practices. Am J Hypertens 2005; 18:1522–1527. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad FS, Chan C, Rosenman MB, Post WS, Fort DG, Greenland P, Liu KJ, Kho A, Allen NB. Validity of cardiovascular data from electronic sources: the multi-ethnic study of atherosclerosis and HealthLNK. Circulation 2017; 136:1207–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stergiou G, Kollias A, Parati G, O’Brien E. Office blood pressure measurement: the weak cornerstone of hypertension diagnosis. Hypertension 2018; 71:813–815. [DOI] [PubMed] [Google Scholar]
- 4. Siu AL; U S Preventive Services Task Force . Screening for abnormal blood glucose and type 2 diabetes mellitus: U.S. preventive services task force recommendation statement. Ann Intern Med 2015; 163:861–868. [DOI] [PubMed] [Google Scholar]
- 5. Pickering TG, White WB; American Society of Hypertension Writing Group . ASH Position Paper: home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich) 2008; 10:850–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D; American Heart Association ; American Society of Hypertension; Preventive Cardiovascular Nurses Association. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008; 52:1–9. [DOI] [PubMed] [Google Scholar]
- 7. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 8. Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O’Brien E, Ohkubo T, Padfield P, Palatini P, Pickering TG, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G; ESH Working Group on Blood Pressure Monitoring . European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24:779–785. [DOI] [PubMed] [Google Scholar]
- 9. Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, Tsuchihashi T, Ohkubo T, Kuwajima I, Miyakawa M; Japanese Society of Hypertension Committee for Guidelines for Self-monitoring of Blood Pressure at Home . The Japanese Society of Hypertension Guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res 2012; 35:777–795. [DOI] [PubMed] [Google Scholar]
- 10. Reboussin DM, Allen NB, Griswold ME, Guallar E, Hong Y, Lackland DT, Miller EPR 3rd, Polonsky T, Thompson-Paul AM, Vupputuri S. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:e116–e135. [DOI] [PubMed] [Google Scholar]
- 11. Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension 2011; 57:29–38. [DOI] [PubMed] [Google Scholar]
- 12. Ostchega Y, Berman L, Hughes JP, Chen T-C, Chiappa MM. Home blood pressure monitoring and hypertension status among US adults: the National Health and Nutrition Examination Survey (NHANES), 2009–2010. Am J Hypertens 2013; 26:1086–1092. [DOI] [PubMed] [Google Scholar]
- 13. Ostchega Y, Zhang G, Kit BK, Nwankwo T. Factors associated with home blood pressure monitoring among US adults: National Health and Nutrition Examination Survey, 2011–2014. Am J Hypertens 2017; 30:2011–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med 2013; 159:185–194. [DOI] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention (CDC). DEMO_F. https://wwwn.cdc.gov/nchs/nhanes/2009-2010/DEMO_F.htm. Accessed 14 April 2020.
- 16. Centers for Disease Control and Prevention (CDC). DEMO_G. https://wwwn.cdc.gov/nchs/nhanes/2011-2012/DEMO_G.htm. Accessed 14 April 2020.
- 17. Centers for Disease Control and Prevention (CDC). DEMO_H. https://wwwn.cdc.gov/nchs/nhanes/2013-2014/DEMO_H.htm. Accessed 14 April 2020.
- 18. Centers for Disease Control and Prevention (CDC). BPQ_H. https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/BPQ_H.htm. Accessed 10 April 2020.
- 19. Centers for Disease Control and Prevention (CDC). BPQ_G. https://wwwn.cdc.gov/Nchs/Nhanes/2011-2012/BPQ_G.htm. Accessed 10 April 2020.
- 20. Centers for Disease Control and Prevention (CDC). BPQ_F. https://wwwn.cdc.gov/Nchs/Nhanes/2009-2010/BPQ_F.htm. Accessed 10 April 2020.
- 21. National Center for Health Statistics. Health Tech/Blood Pressure Procedures Manual. 2009. https://wwwn.cdc.gov/nchs/data/nhanes/ 2009-2010/manuals/lab.pdf. [Google Scholar]
- 22. Low Blood Pressure | National Heart, Lung, and Blood Institute (NHLBI). Low Blood Pressure. https://www.nhlbi.nih.gov/health-topics/low-blood-pressure. Accessed 13 May 2020.
- 23. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC, 2017. [Google Scholar]
- 25. Fuchs SC, Ferreira-da-Silva AL, Moreira LB, Neyeloff JL, Fuchs FC, Gus M, Wiehe M, Fuchs FD. Efficacy of isolated home blood pressure monitoring for blood pressure control: randomized controlled trial with ambulatory blood pressure monitoring - MONITOR study. J Hypertens 2012; 30:75–80. [DOI] [PubMed] [Google Scholar]
- 26. Vrijens B, Goetghebeur E. Comparing compliance patterns between randomized treatments. Control Clin Trials 1997; 18:187–203. [DOI] [PubMed] [Google Scholar]
- 27. Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int 2006; 69:406–411. [DOI] [PubMed] [Google Scholar]
- 28. Dharmarajan SH, Bragg-Gresham JL, Morgenstern H, Gillespie BW, Li Y, Powe NR, Tuot DS, Banerjee T, Burrows NR, Rolka DB, Saydah SH, Saran R; Centers for Disease Control and Prevention CKD Surveillance System . State-level awareness of chronic kidney disease in the U.S. Am J Prev Med 2017; 53:300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ye X, Shafi S, Negrete A, Davis WN, Sarac E, Negrete AM, Negrete H. Home blood pressure monitor use in patients with chronic kidney disease. Blood Press 2016; 25:280–285. [DOI] [PubMed] [Google Scholar]
- 30. Bangash F, Agarwal R. Masked hypertension and white-coat hypertension in chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol 2009; 4:656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.