Abstract
We are reporting the imaging findings of the rare entity of critical illness-associated cerebral microbleeds in a COVID-19-positive 66-year-old woman with hypoxic respiratory failure, who was eventually intubated and ventilated. Multiple scattered cerebral microhaemorrhages diffusely distributed in the juxtacortical white matter and internal capsule region, sparing the deep and periventricular white matter, basal ganglia, thalami and cortex were seen, which is a unique imaging finding in critically ill patients with respiratory failure and hypoxemia requiring mechanical ventilation. The mechanism underlying these microhaemorrhages relates to the endpoint of critical illness, rather than a specific underlying disease.
Keywords: COVID-19, critical illness, cerebral microbleeds
Introduction
COVID-19-related neurological imaging features are evolving with increasing frequency of neurological manifestations in COVID-19 patients. Cerebral microbleeds in COVID-19 patients could be attributed to various aetiologies including virus-induced direct neural damage and virus-induced or other systemic causes. We are presenting a patient with the relatively recently described unique entity of critical illness-associated cerebral microbleeds displaying its distinctive distribution pattern as a possible cause of cerebral microbleeds in COVID-19.
Case report
A 66-year-old female patient was brought to our hospital complaining of cough, tachypnoea, chills and weakness, and was found to have reduced oxygen saturation. She had a past medical history of diabetes mellitus, hypertension, dyslipidemia and hypothyroidism. The patient deteriorated to hypoxic respiratory failure and was eventually intubated and ventilated. She had septic shock and acute kidney injury requiring haemodialysis. Laboratory tests showed high white blood cell (WBC) count of 14.5 K/dl, low platelets of 145 K, high activated partial thromboplastin time (APTT) of 64.4 seconds, normal international normalised ratio (INR) of 1, normal prothrombin time (PT) of 11.2 seconds, high fibrinogen of 5 g/l, high D-dimer of 2.6 mg/l, high C-reactive protein of 67.8 mg/l, high creatinine of 217 μmol/L, high alanine aminotransferase (ALT) of 60 U/l, high aspartate aminotransferase (AST) of 40 U/l and high alkaline phosphatase of 175 U/l. She had a history of recent travel and was tested positive for COVID-19 by polymerase chain reaction (PCR).
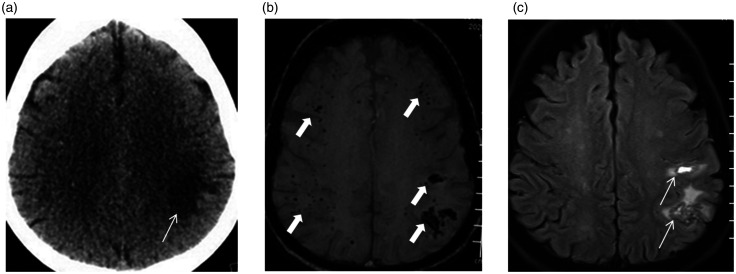
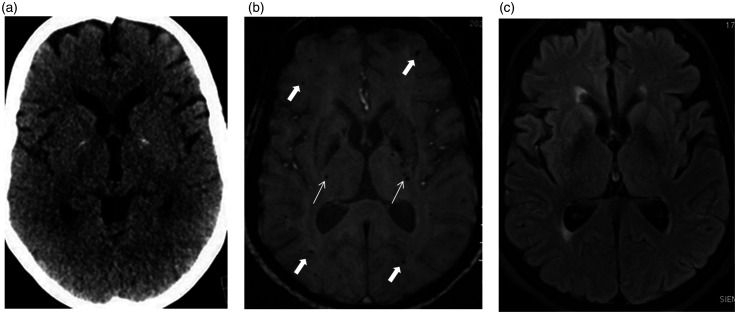
Three weeks later the patient was not improving and a computed tomography (CT) scan of the head was requested as part of a general sepsis work-up as the patient was feverish and there was some drop in the level of consciousness. Non-contrast CT scan of the head (Siemens Somatom Edge Plus; Erlangen, Germany; 128 multislice, kV 120/146 mAs) was performed, which showed focal left parietal centrum semiovale vasogenic oedema that made the emergency radiologist and the intensive care unit (ICU) physician consider the possibility of an underlying evolving abscess. Therefore, on the same day multiplane different pulse sequence magnetic resonance imaging (MRI) head (Siemens 3T MAGNETOM Skyra; Erlangen, Germany) before and after intravenous gadolinium contrast agent injection as well as three-dimensional time of flight intracranial magnetic resonance angiography was performed for further evaluation and better characterization of the CT finding. The MRI showed widespread susceptibility weighted imaging blooming hypointense foci consistent with microbleeds predominantly involving the juxtacortical white matter, sparing the deep and periventricular white matter, thalami and basal ganglia. The larger bleeding foci were in the left parietal region, displaying perilesional oedema which was also seen on the CT scan, but there was no evidence of abscess formation (Figure 1). Tiny foci of microbleeds were seen in the internal capsules (Figure 2). The constellation of these magnetic resonance features along with the clinical status of the patient as described before was consistent with critical illness-associated cerebral microbleeds; the largest one was associated with vasogenic oedema in the left parietal region.
Figure 1.
Axial unenhanced computed tomography (CT) scan (a) shows hypodensity in the left parietal centrum semiovale suggestive of vasogenic oedema (thin arrow). Axial susceptibility weighted imaging (SWI) magnetic resonance imaging (MRI) (b) shows widespread blooming hypointense foci consistent with microbleeds predominantly involving the juxtacortical white matter (thick arrows), sparing the deep white matter. The larger bleeding foci are in the left parietal region, displaying perilesional oedema in the centrum semiovale (thin arrows) in the axial fluid-attenuated inversion recovery (FLAIR) image (c) which was also seen in the CT scan.
Figure 2.
Axial unenhanced computed tomography (CT) scan (a) at the level of the basal ganglia and thalami appear unremarkable, except for physiological-basal ganglia calcifications. Axial susceptibility weighted imaging (SWI) magnetic resonance imaging (MRI) (b) shows widespread blooming hypointense foci consistent with microbleeds predominantly involving the juxtacortical white matter (thick arrows), sparing the deep periventricular white matter, basal ganglia and thalami. Basal ganglia calcifications are hypointense on SWI. Note bilateral tiny microbleeds in the internal capsules (thin arrows). Axial fluid-attenuated inversion recovery (FLAIR) image (c) at this level appears unremarkable.
Discussion
Brain imaging findings in COVID-19 are not yet quite known but are evolving, with ischaemic strokes and haemorrhages, meningoencephalitis, haemorrhagic leukoencephalopathy and acute necrotising encephalopathy reported.1,2
Multiple scattered cerebral microhaemorrhages diffusely distributed in the juxtacortical white matter and callosal region, sparing the deep and periventricular white matter, basal ganglia, thalami and cortex is a unique imaging finding in critically ill patients with respiratory failure and hypoxemia-induced hydrostatic or chemical effects on the blood–brain barrier. The internal capsules, brain stem and middle cerebellar peduncles can also be diffusely involved. Many of these critically ill patients have associated sepsis, disseminated intravascular coagulation, thrombocytopenia, prolonged PT and APTT. Critical illness with hypoxemia/respiratory failure requiring mechanical ventilation in the majority is a common denominator in these cases, and the mechanism underlying these unique microhaemorrhages relates to the endpoint of critical illness, rather than specific underlying diseases.3,4 Similar findings have been described in high altitude cerebral oedema-associated microbleeds.5
Although many neurological symptoms such as headache, dizziness, acute cerebrovascular disease, impairment of consciousness, ataxia and seizures are seen associated with the disease, none of them is specific for it.6 Brain haemorrhage in COVID-19 could be due to many pathophysiological mechanisms, which include both virus-induced direct neural damage and viral-induced or other systemic causes; such as virus-induced acute haemorrhagic leukoencephalopathy, haemorrhagic infarcts, deranged bleeding/clotting parameters and the effects of therapeutic agents,1,7 but the typical pattern of critical illness-associated cerebral microbleeds should be carefully evaluated in patients with hypoxemia and respiratory failure.
Conclusion
Brain haemorrhage in COVID-19 could be due to a variety of causes, both related to the direct effects of virus or other mechanisms. We are presenting a rare entity of cerebral microbleeds in a critically ill patient with COVID-19 infection, due to respiratory failure and hypoxemia requiring mechanical ventilation. Critical illness-associated cerebral microbleeds is a very rare entity, due to respiratory failure and hypoxemia-induced hydrostatic or chemical effects on the blood–brain barrier in any critical illness. Radiologists should be aware of this unique entity in the current COVID era.
Author note
Surjith Vattoth is now affiliated to Radiology Department at University of Arkansas for Medical Sciences in Little Rock, AR, USA.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics and consent
Relevant consents were taken.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Open Access funding provided by the Qatar National Library.
ORCID iD
Surjith Vattoth https://orcid.org/0000-0002-9846-7914
References
- 1.Kandemirli SG, Dogan L, Sarikaya ZT, et al. Brain MRI findings in patients in the intensive care unit with COVID-19 infection. Radiology 2020; 201697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poyiadji N, Shahin G, Noujaim D, et al. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology 2020; 201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fanou EM, Coutinho JM, Shannon P, et al. Critical illness-associated cerebral microbleeds. Stroke 2017; 48: 1085–1087. [DOI] [PubMed] [Google Scholar]
- 4.Hall JP, Minhas P, Kontzialis M, et al. Teaching neuroimages: distinct brain microhemorrhage pattern in critical illness associated with respiratory failure. Neurology 2018; 90: e2011. [DOI] [PubMed] [Google Scholar]
- 5.Riech S, Kallenberg K, Moerer O, et al. The pattern of brain microhemorrhages after severe lung failure resembles the one seen in high-altitude cerebral edema. Crit Care Med 2015; 43: e386–e389. [DOI] [PubMed] [Google Scholar]
- 6.Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci 2020; 11: 116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sachs JR, Gibbs KW, Swor DE, et al. COVID-19-associated leukoencephalopathy. Radiology 2020; 201753. [DOI] [PMC free article] [PubMed] [Google Scholar]