Abstract
Florid cemento-osseous dysplasia (FCOD) is a rare benign fibro-osseous lesion which affects multiple quadrants and predominantly the mandible. This case report presents a successful implant placement with 8-year of follow-up in a 44-yearold woman asking for a fixed restoration in mandibular right posterior edentulous area. Radiographic images showed lobular, irregularly shaped radiopacities and radiolucencies almost symmetrically observed in the premolar-molar area of the right and left regions of the mandible. The findings of Xray images were attributable to FCOD. Minimally invasive two-stage surgery with strict infection control was followed to place two implants in lower right posterior region. The implants demonstrated clinically rigid fixation and restored successfully after 6 months. A direct functional connection between dysplastic bone and the implant load bearing surface was evidenced by the lack of symptoms, and the lack of soft tissues inflammation or peri-implant bone loss up to 8 years follow-up.
Key words: Florid cemento-osseous dysplasia, dental, implant, follow-up
Introduction
Florid cemento-osseous dysplasia (FCOD) is a rare benign fibro-osseous lesion which affects multiple quadrants and predominantly the mandible.1 It is more common in females and has a predisposition for African-Americans.2 The exact etiopathology of FCOD is still unknown, though it is usually considered to be a reactive lesion.3 It involves the replacement of normal bone architecture by fibroblasts and collagen fibers containing different quantities of mineralized material.4 Depending upon its duration, the radiographic appearance may vary, however it may appear firstly as a radiolucent lesion that becomes progressively radiopaque with the deposition of immature bone. The lesion has compromised bone structure characterized with incomplete stromal vasculature that predisposes the affected bone to secondary infection. 5 We describe the success of dental implants osseointegration in areas of florid cemento-osseous dysplasia after 8-year of follow-up.
Case Report
A 44-year-old woman presented to the private dental clinic at Tulkarm for dental treatment. The presenting complaint was to have new fixed restoration in the right lower side to replace the previously failed one in order to eat on that side and to improve the appearance. Her medical history was non-significant. The dental history revealed that the patient had 3-unit metalceramic fixed partial denture (FPD) supported by mandibular right second molar and right second premolar. The reason of failure of this FPD was recurrent caries of second molar up to cemento-enamel junction leading to frequent decementation of FPD (Figure 1).
Orthopantomogram (OPG) showed lobular, irregularly shaped radiopacities and radiolucencies almost symmetrically observed in the incisor, premolar, and molar areas of the right and left regions of the mandible (Figure 2). The opacities were surrounded by a radiolucent zone. The findings of X-ray images were attributable to FCOD.
After discussing with the patient about the available options to replace the missing posterior teeth as well as the pros and cons of each option, the patient decided to have dental implant therapy and provided informed consent.
Strict infection control was ensured to reduce the chance of any secondary infection, as it will be aggressive and difficult to treat. This was assured by prescribing prophylactic antibiotic (amoxicillin/clavulanic acid 500 mg/125 mg) 1 h before surgery and chlorhexidine mouthwash preoperatively and postoperatively, by ensuring sterile environment during the procedure, minimizing periosteal reflection, making the procedure as short as possible, and avoiding overheating the bone using cool sterile saline and sharp drills with intermittent pressure during drilling. Two 4.6 diameter implants with length of 12 mm (internal; BioHorizons, Birmingham, AL, USA) were placed in the mandibular first and second molar area with torque of 40 N-Cm. Submerged two-stage surgery was made to avoid any premature loading during healing and to reduce the incidence of infection. Postoperative panoramic radiograph was taken at end of surgery. After 5 months of submerged healing, the implants were uncovered without noting any vertical or horizontal defects and the two implants revealed rigid fixation clinically. One month later, the implants were restored with cement-retained metal-ceramic splinted crowns. Regular clinical and radiographic follow-up with the patient was maintained.
Radiographically, OPGs were taken before the surgery (Figure 2), immediately after surgery, at prosthesis delivery, 1-year following prosthesis delivery, and every 2 years thereafter. Neither the size of FCOD lesion, nor the peri-implant bone loss were observed; however, a well-defined radiolucency appeared on distal aspect of the apex of the mandibular second molar implant. Furthermore, a cone beam computed tomography (CBCT) was undertaken six years after prosthesis delivery as it has become available, (Figure 3) which showed optimal functional rehabilitation and complete integration of implants. The radiographic examination using OPG and periapical images at 8-year following prothesis delivery showed optimal osseointegration with no remarkable bone problems (Figures 4 and 5). The clinical evaluation of the covering mucosa of the treated region demonstrated non-remarkable presentation (Figure 6). Although the implants were not placed in the correctly prosthetic position, the patient has maintained good oral hygiene leading to stable level of crestal bone and healthy soft tissue up to 8-year follow-up.
Discussion
FCOD is a non-malignant fibro-osseous lesion, having multifocal involvement in the tooth-bearing areas of the mandible.6 Despite several evidences of familial and genetic predilection of some oral lesions,7,8 FCOD has a poor familial and genetic background. 9,10 Clinically, this reactive lesion is asymptomatic, although the probability of dull pain, exposure of alveolar bone into the oral cavity, and alveolar sinus tract arising from secondary infection is quite possible.11 A wide array of terms has been used to report FCOD including multiple cementoossifying fibromas, multiple osteomas, multiple enostosis, periapical cementoblastoma, sclerosing osteomyelitis, gigantiform cementoma. According to the 2nd edition of the World Health Organization’s classification of odontogenic tumors, the term florid cemento-osseous dysplasia replaced gigantiform cementoma.9 A growing body of evidences now suggest that for all lesions visible in radiographs, it is not mandatory to always perform histologic examination. Thereby, only radiographic and clinical investigations may be considered critical to diagnosis of FCOD.12
A more mature FCOD lesion is transformed to dense, acellular, avascular and sclerotic, calcified tissue.3 The regeneration, osseointegration and healing capacity of the affected alveolar bone is reduced.9 It has been reported that dental implant placement in the affected region may produce osteomyelitis.13 During the preparation of osteotomy site, the bony tissue surrounding dental implant might get necrosed due to overheating. The damage to the bone can be increased if drilling is performed without sufficient cooling.14 Necrosis often leads to osteomyelitis if the adjacent inflammatory process is spread into the sclerotic bone.15 Bony sequestrum formation16 and infection are the primarily associated radiological features with chronic osteomyelitis. Infection requires debridement and enucleation and might not respond to antibiotics due to avascular nature of the lesion.3
Figure 1.

Orthopantomogram pre-extraction of mandibular right second molar.
Figure 2.
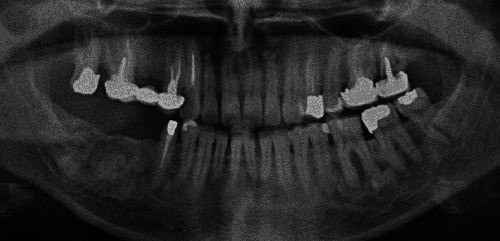
Orthopantomogram before the surgery.
Figure 3.

Cone beam computed tomography taken 6-year following prosthesis delivery.
There is a dearth of literature regarding dental implant survival rate and cementoosseous dysplasia. A recent case report showed a successful implant placement for a 62-year-old Caucasian woman with a chief complaint of mandibular partial edentulous diagnosed with FCOD. A highly conservative step-by-step 2-stage implant surgery was performed. After 6 months, the implants were loaded with fixed prosthesis. The case was followed up to 18 months revealing an optimal functional rehabilitation and complete integration of implants.4 On the other hand, another case report had shown implant failure by fibrous encapsulation after 26 months of function. The patient returned with clinical symptoms of pain, buccal swelling, and the sensation of a loose implant. The case report was diagnosed of 2 distinct disease entities associated with the implant site, a cemento-ossifying fibroma and florid cemento-osseous dysplasia of the mandible. This diagnosis was determined from clinical, surgical, radiographic, and histopathologic evidence after biopsy and removal of the implant.9
In addition, a case report demonstrated successful integration of a dental implant placed into a late-stage focal cementoosseous dysplasia up to 15 years without any complications. However, at the 16-year follow-up, the implant and a sclerotic mass were removed due to peri-implantitis, and the entire specimen was evaluated with conventional histology and microcomputed tomography. The analysis revealed that the sclerotic mass attached to the implant was cementum-like tissue that was free of any intervening soft tissue.17
Regarding the current case, dental implant therapy was opted after taking patient’s request and consent into consideration. If removable partial denture (RPD) was selected, the mandibular right posterior ridge would be prone to resorption since vertical and horizontal alveolar bone resorption was found to be higher in the RPD-wearing patients when comparing the dentate and edentulous sites. However, the implant-supported fixed prosthesis would improve the functional efficiency while maintaining the underlying bone. No surgical excision of these lesions was done before implant rehabilitation because the patient was completely asymptomatic, excision of these lesions would have been very difficult because it is difficult to distinguish between normal or affected bone, and if excision was made, it would result in a large discontinuity defect which may require bony reconstruction at a later stage with a bone graft, and also would expose the inferior alveolar canal.
In terms of oral rehabilitation with implants in FCOD, the avascular nature of these lesions might complicate the osseointegration of the implants and if secondary infection occurs, it will be aggressive and difficult to treat. The main expected complications have been reported as poor healing, risk of infection and fracture of the jaw.12,18,19
Figure 4.

Orthopantomogram taken 8-year following prosthesis delivery.
Figure 5.

Periapical radiograph taken 8-year following prosthesis delivery.
Figure 6.

Clinical photograph of the implant prosthesis and adjacent teeth (frontal view at centric occlusion).
Conclusions
This report concludes that implant rehabilitation of the edentulous area near the FCOD lesions can be considered if strict infection control with minimally invasive submerged two-stage surgery is followed. Since there is insufficient evidence on the long-term or even the short-term success of dental implant rehabilitation in cementosseous dysplasia cases, we recommend regular clinical and radiographic follow-up with the patient maintaining good oral hygiene and attending regularly for followup and prophylaxis every three months.
References
- 1.Daviet-Noual V, Ejeil A-L, Gossiome C, et al. Differentiating early stage florid osseous dysplasia from periapical endodontic lesions: a radiologicalbased diagnostic algorithm. BMC Oral Health 2017;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delai D, Bernardi A, Felippe GS, et al. Florid cemento-osseous dysplasia: a case of misdiagnosis. J Endodontics 2015;41:1923-6. [DOI] [PubMed] [Google Scholar]
- 3.Bencharit S, Schardt-Sacco D, Zuniga JR, Minsley GE. Surgical and prosthodontic rehabilitation for a patient with aggressive florid cemento-osseous dysplasia: a clinical report. J Prosthet Dent 2003;90:220-4. [DOI] [PubMed] [Google Scholar]
- 4.Esfahanizadeh N, Yousefi H. Successful implant placement in a case of florid cemento-osseous dysplasia: a case report and literature review. J Oral Implantol 2018;44:275-9. [DOI] [PubMed] [Google Scholar]
- 5.Aiuto R, Gucciardino F, Rapetti R, et al. Management of symptomatic florid cemento-osseous dysplasia: Literature review and a case report. J Clin Exper Dent 2018;10:e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex a review. Head Neck Pathol 2008;2:177-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Najafi S, Yousefi H, Mohammadzadeh M, et al. Association study of interleukin- 1 family and interleukin-6 gene single nucleotide polymorphisms in recurrent aphthous stomatitis. Int J Immunogenet 2015;42:428-31. [DOI] [PubMed] [Google Scholar]
- 8.Najafi S, Yousefi H, Mohammadzadeh M, et al. Interleukin-2, interferongamma gene polymorphisms in recurrent aphthous stomatitis. Prague Med Rep 2017;118:81-6. [DOI] [PubMed] [Google Scholar]
- 9.Gerlach RC, Dixon DR, Goksel T, et al. Case presentation of florid cementoosseous dysplasia with concomitant cemento-ossifying fibroma discovered during implant explantation. Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:e44-e52. [DOI] [PubMed] [Google Scholar]
- 10.MacDonald-Jankowski D. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol 2008;37:350-60. [DOI] [PubMed] [Google Scholar]
- 11.Lin T-M, Huang W-H, Chiang C-P, et al. Florid cemento-osseous dysplasia (FCOD): case report. J Dent Sci 2010;5:242-5. [Google Scholar]
- 12.de Santana Sarmento DJ, de Brito Monteiro BV, de Medeiros AMC, da Silveira EJD. Severe florid cementoosseous dysplasia: a case report treated conservatively and literature review. Oral Maxillofac Surg 2013;17:43-6. [DOI] [PubMed] [Google Scholar]
- 13.Shin H, Kim B, Lim H, et al. Chronic osteomyelitis induced by the placement of dental implants on cemento-osseous dysplasia. Bri J Oral Maxillofac Surg 2019;57:268-70. [DOI] [PubMed] [Google Scholar]
- 14.Al-Sabbagh M, Bhavsar I. Key local and surgical factors related to implant failure. Dent Clin North Am 2015;59:1-23. [DOI] [PubMed] [Google Scholar]
- 15.Cavalcante MB, de Oliveira Lima AL, Júnior MAB, Santos MBP. Florid cemento-osseous dysplasia simultaneous the chronic suppurative osteomyelitis in mandible. J Craniofac Surg 2016;27:2173-6. [DOI] [PubMed] [Google Scholar]
- 16.Shnaiderman-Shapiro A, Dayan D, Buchner A, et al. Histopathological spectrum of bone lesions associated with dental implant failure: osteomyelitis and beyond. Head Neck Pathol 2015;9:140-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park WB, Han JY, Jang JS, et al. Longterm implant survivability of an implant having direct contact with cementumlike tissue in a preexisting mandibular intraosseous lesion with a 16-year longitudinal follow-up. Int J Periodontics Restorative Dent 2019;39:895-902. [DOI] [PubMed] [Google Scholar]
- 18.Das BK, Das SN, Gupta A, Nayak S. Florid cemento-osseous dysplasia. J Oral Maxillofac Pathol 2013;17:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gündüz K, Avsever H, Karaçayli Ü, et al. Florid cemento-osseous dysplasia: a case report. Braz Dent J 2009;20:347-50. [DOI] [PubMed] [Google Scholar]


