The advent of lumen-apposing metal stents (LAMSs) has led to new endoscopic techniques for the management of numerous complex clinical scenarios. LAMSs are only approved for the management of pancreatic fluid collections, and all other indications are off-label. EUS-guided gastroenterostomy using LAMSs for the treatment of both malignant and benign gastric outlet obstruction (GOO) has been described. Deployment of a LAMS to create a gastrojejunostomy requires multiple steps with significant risk for both proximal and distal maldeployment of the stent. We describe a case demonstrating intraperitoneal salvage of a maldeployed LAMS during EUS-gastroenterostomy to treat malignant GOO.
A 63-year-old man with metastatic bladder cancer presented with malignant GOO. He initially underwent concomitant endoscopic placement of a biliary self-expandable metal stent for biliary obstruction and duodenal self-expandable metal stent placement for GOO. Tumor in-growth occurred within the duodenal stent, and the patient presented again with GOO 3 months later.
A palliative EUS-guided gastroenterostomy was attempted using a cautery-enhanced LAMS. During the initial attempt, the target small bowel was distended via irrigation of dilute contrast and methylene blue through a nasobiliary tube placed in the small bowel. A linear echoendoscope was used, and endosonographic and fluoroscopic views from the stomach identified the dilated and contrast-filled small bowel. A 20- × 10-mm cautery-enhanced LAMS was deployed across the stomach wall into the target small bowel. After deployment of the proximal flange, there was no evidence of blue-tinged fluid refluxing into the stomach. A guidewire was advanced (Video 1, available online at www.VideoGIE.org).
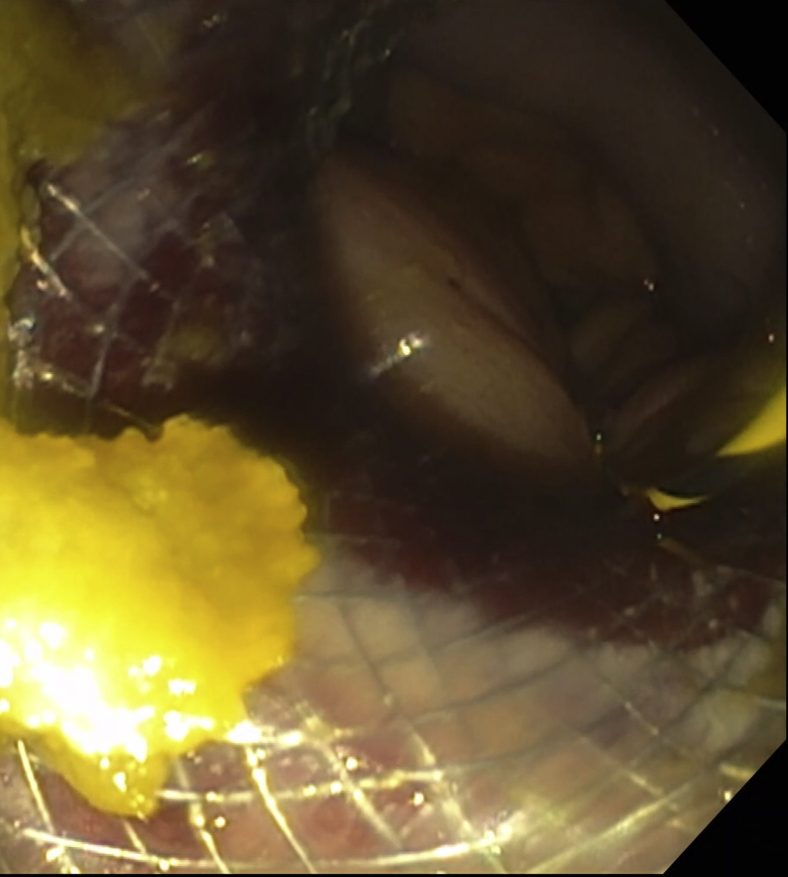
On fluoroscopy, the guidewire appeared extraluminal and intraperitoneal, suggesting maldeployment of the LAMS (Fig. 1). Endoscopic salvage was attempted. The LAMS was successfully balloon dilated to 18 mm. The small-bowel serosa was visualized and appeared healthy without a cautery burn (Fig. 2). The echoendoscope was advanced across the maldeployed LAMS and into the peritoneal cavity. From the peritoneal cavity, a second EUS-guided cautery-enhanced LAMS (15 × 10 mm) was deployed into the target small bowel, and the distal flange was deployed.
Figure 1.
Extraluminal guidewire suggestive of perforation.
Figure 2.
Healthy jejunal serosa without cautery burn.
The echoendoscope and partially deployed LAMS were slowly retracted into the stomach. The proximal flange was released, and the LAMS was nested in the initial LAMS (Fig. 3). Reflux of blue-tinged fluid into the gastric lumen was observed. The nasobiliary drain could be endoscopically visualized through the gastroenterostomy (Fig. 4). To secure the 2 LAMSs to one another, 2 sequential endoscopic sutures were attached to a 19-gauge FNA needle and then deployed through overlapping cells of the nested stents (Fig. 5). Using this technique, we backloaded the blunt end of an endoscopic suture needle into a 19-gauge FNA needle.
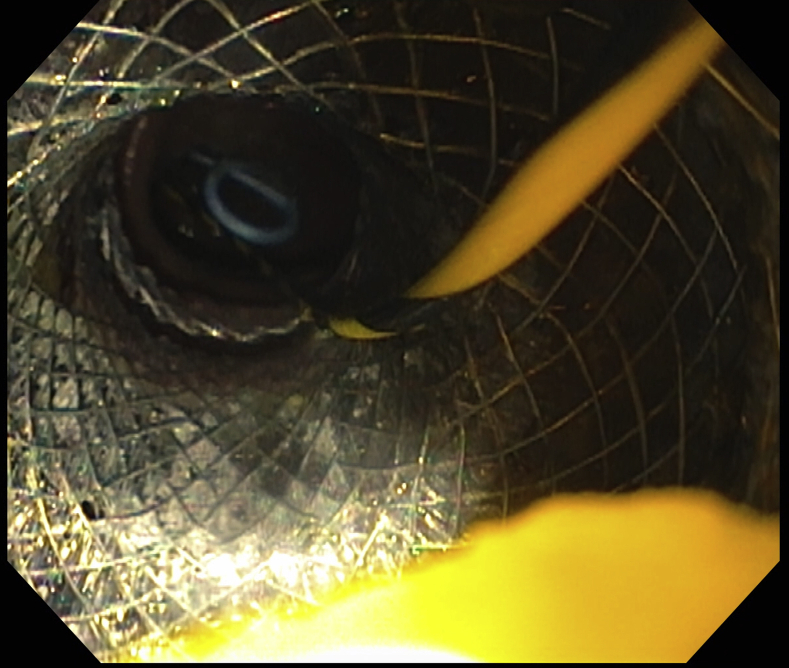
Figure 3.
Nested lumen-apposing metal stents.
Figure 4.
Nasobiliary drain in the jejunum endoscopically visible across the nested lumen-apposing metal stents.
Figure 5.
Suture fixation of the nested lumen-apposing metal stents.
The FNA needle and suture were passed down the working channel of the echoendoscope. The sharp end of the endoscopic suture needle was advanced through the overlapping walls of the nested LAMS. The suture needle was released and cinched. Postprocedurally, the patient remained hemodynamically stable but required needle decompression of capnoperitoneum and experienced mild postprocedure pain. He received a course of empiric antibiotics. He tolerated a stent diet, and his GOO symptoms improved. He was discharged home but died 6 weeks later of progression of his malignancy.
In conclusion, endoscopists performing procedures involving LAMSs should be aware of the risk for maldeployment and of available rescue options. Multiple rescue options have been previously presented.1, 2, 3 In cases in which the “freehand” technique is used and maldeployment occurs, there is often no intraluminal guidewire to work over during the salvage attempt; thus, intraperitoneal endoscopy is often needed in some capacity. Conversely, in cases in which maldeployment occurs but an intraluminal guidewire is secured in the target small bowel, a second LAMS can then be deployed using the over-the-wire technique. In our case, the 20-mm LAMS permitted passage of a linear echoendoscope across the LAMS to perform intraperitoneal salvage using a second LAMS.
Disclosure
Dr Law is a consultant for Olympus America. All other authors disclosed no financial relationships.
Footnotes
This video was selected as an Honorable Mention at Digestive Disease Week 2020.
Supplementary data
Intraperitoneal salvage of an EUS-guided gastroenterostomy using a nested lumen-apposing metal stent.
References
- 1.James T.W., Greenberg S., Grimm I.S. EUS-guided gastroenteric anastomosis as a bridge to definitive treatment in benign gastric outlet obstruction. Gastrointest Endosc. 2020;91:537–542. doi: 10.1016/j.gie.2019.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James T.W., Grimm I.S., Baron T.H. Intraperitoneal echoendoscopy for rescue of a gastrojejunal anastomosis. VideoGIE. 2019;4:528–529. doi: 10.1016/j.vgie.2019.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ligresti D., Amata M., Barresi L. The lumen-apposing metal stent (LAMS)-in-LAMS technique as an intraprocedural rescue treatment during endoscopic ultrasound-guided gastroenterostomy. Endoscopy. 2019;51:E331–E332. doi: 10.1055/a-0924-5408. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraperitoneal salvage of an EUS-guided gastroenterostomy using a nested lumen-apposing metal stent.