Abstract
Policy Points.
This article reconceptualizes our understanding of the opioid epidemic and proposes six strategies that address the epidemic's social roots.
In order to successfully reduce drug‐related mortality over the long term, policymakers and public health leaders should develop partnerships with people who use drugs, incorporate harm reduction interventions, and reverse decades of drug criminalization policies.
Context
Drug overdose is the leading cause of injury‐related death in the United States. Synthetic opioids, predominantly illicit fentanyl and its analogs, surpassed prescription opioids and heroin in associated mortality rates in 2016. Unfortunately, interventions fail to fully address the current wave of the opioid epidemic and often omit the voices of people with lived experiences regarding drug use. Every overdose death is a culmination of a long series of policy failures and lost opportunities for harm reduction.
Methods
In this article, we conducted a scoping review of the opioid literature to propose a novel framework designed to foreground social determinants more directly into our understanding of this national emergency. The “continuum of overdose risk” framework is our synthesis of the global evidence base and is grounded in contemporary theories, models, and policies that have been successfully applied both domestically and internationally.
Findings
De‐escalating overdose risk in the long term will require scaling up innovative and comprehensive solutions that have been designed through partnerships with people who use drugs and are rooted in harm reduction.
Conclusions
Without recognizing the full drug‐use continuum and the role of social determinants, the current responses to drug overdose will continue to aggravate the problem they are trying to solve.
Keywords: substance use, drug use, opioids, addictive behavior
Drug overdose is the leading cause of injury death in the United States, with recent increases in overdose fatalities contributing to national reductions in life expectancy over two consecutive years. 1 In 2017, the United States recorded more than 70,000 drug overdose deaths, an increase of more than 30% since 2015, and 67,367 deaths in 2018. 1 , 2 The current epidemic has been characterized as consisting of three distinct opioid overdose “waves” beginning in the 1990s: the widespread prescription, diversion, and misuse of prescription opioids; their interaction with and amplification of heroin use; and the expansion of synthetic opioids in the drug supply, including illicitly manufactured fentanyl. 3 , 4 Adjacent to the dramatic rates of fatal overdose are the rising burden of nonfatal overdose, polysubstance use, and the health and financial costs they incur. 5 Given the high human resources and monetary costs of managing this epidemic—driven by factors such as rising hospitalization costs and expenditures on treatment and incarceration— the overall economic cost of the opioid epidemic for 2018 will likely exceed $500 billion. 6 , 7
Despite their similar underlying social and economic causes, including poverty and stigma, earlier waves of overdoses driven by heroin (1970s) and crack cocaine (1980s), particularly among urban low‐income communities of color, are less often acknowledged in the public discourse. 8 , 9 , 10 The federal policy response since the early 1900s has been the moral rebuke of people who use drugs (PWUD); expanded drug criminalization laws, particularly following the declaration of the War on Drugs by President Richard Nixon; increased funding of interdiction efforts; and aggressive policing, especially of urban Black communities. Together these factors have led to high incarceration rates, greater overdose risk, and community violence, and have alienated many communities. 11 , 12 The legacy of these punitive approaches continues to manifest today through “drug‐induced homicide” laws and police drug raids, which jeopardize public health efforts to tackle this crisis. 13 , 14
Alternative views of drug use, based on pragmatism and driven by grassroots activists, including PWUD, catalyzed the movement now known globally as harm reduction. The term PWUD was in fact developed by and advocated for by organizations led by PWUD to replace stigmatizing terms like junkie and addict and has been adopted globally. In the United States, the growing demographics of PWUD and the sharp rise in fatalities over the past decade have also galvanized a movement to reframe the overdose crisis as a medical or public health issue rather than a criminal one. Progress has been made in tackling addiction and overdose, such as the expansion of medications for opioid use disorder (OUD) and the increased availability of naloxone. Supply‐reduction strategies have reduced the number of prescription opioids dispensed, even though the decades‐long efforts to stem the flow of illicit opioids have remained largely ineffective.
However, the current response remains too narrow for the scale and scope of this crisis. For example, reforming opioid‐prescribing practices and holding pharmaceutical companies accountable for placing profits over patient safety is necessary but will not be sufficient to reduce overdose rates over the long term because it leaves PWUD ill‐equipped to adapt to the rapidly evolving illicit drug market and to adopt safer drug use practices. 15 , 16 Instead, the focus must shift from reducing supply and interdiction to recognizing, understanding, and addressing the epidemic's root causes. Although the social determinants of health, defined by the World Health Organization as “the conditions in which people are born, grow, live, work and age … shaped by the distribution of money, power and resources,” have been underutilized in addressing the opioid epidemic, they could propel us forward in our response.
In this article, we propose a range of evidence‐based strategies that could be implemented to holistically address the scope and depth of this epidemic. We introduce the “continuum of overdose risk” (COR) framework (Figure 1) to highlight the precursors to overdose, clarify the distinction between drug use and addiction, and identify factors that escalate progression, as well as six strategies that could de‐escalate risk. We developed this framework to promote a comprehensive approach inclusive of the social determinants of health, amid new challenges posed by synthetic opioids and polysubstance use. 17 , 18 , 19
Figure 1.
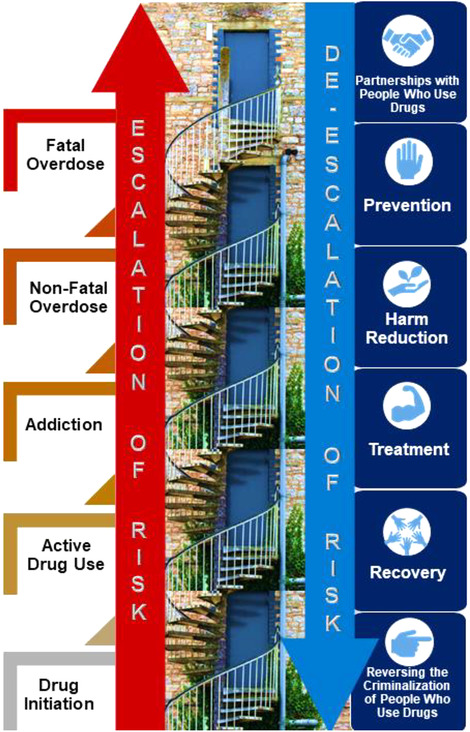
The Continuum of Overdose Risk (COR) Framework Visualized as a Staircase [Color figure can be viewed at wileyonlinelibrary.com]
Higher steps represent increasing risk of a fatal overdose (red step). Six strategies to de‐escalate risk are represented by the blue doors.
The social determinants of health are more important than ever, given the current COVID‐19 pandemic, which has swept through the world and resulted in more than a quarter of a million cases and 36,000 deaths in less than 5 months, 20 causing major and unprecedented disruptions to the global economy. In the United States, this pandemic has exposed the vulnerabilities that many Americans face, from inequities in health insurance and paid sick leave, to constraints in accessing COVID‐19 testing, masks, and ventilators. PWUD, with their unique set of health, social and structural vulnerabilities, including medical comorbidities, homelessness, food insecurity, and violence, are expected to be disproportionately burdened by this pandemic. In addition to interruptions in medications, care, and harm reduction supplies, social distancing is nearly impossible for homeless individuals and incarcerated populations, and detrimental to those with severe mental health disorders or who face abuse at home. It therefore is vital that COVID‐19 policies consider PWUD in their development and implementation.
Through this work, we aim to confront the stigmatization and criminalization of drug use and the abstinence‐centric ideology and racism that endures in public discourse (eg, the media) as well as in medicine, public health, and law. Following others, we argue that these views, laws, and policies impede access to critical opportunities to prevent drug morbidity and mortality. 12 , 21 , 22 A narrow understanding of drug use coupled with punitive drug policies will continue to isolate and harm the millions of Americans who use drugs. Despite leading the development and dissemination of harm reduction interventions (eg, community‐based naloxone, syringe services programs [SSP]), and being directly impacted by the overdose crisis themselves, PWUD continue to be excluded from key policy discussions at local and national levels, even though their inclusion could facilitate pragmatic dialogue, innovation, and action. In later sections, we discuss six strategies to address the epidemic, such as meaningful partnerships with PWUD, harm reduction interventions, and legal reforms, along with the traditional strategies of prevention, treatment, and recovery that are often the guiding framework for responding to the overdose crisis.
The Continuum of Overdose Risk Framework
The COR framework (Figure 1) characterizes key stages that could be effective intervention targets in reducing drug overdose: (1) drug initiation, (2) active drug use, (3) addiction, (4) nonfatal overdose, and (5) fatal overdose. As we will discuss later, we propose six strategies to de‐escalate progression toward higher levels of risk: (1) meaningful partnerships with PWUD, (2) prevention, (3) harm reduction, (4) treatment, (5) recovery, and (6) reversal of the criminalization of PWUD. Because individuals can progress toward higher levels of overdose risk and skip or jump steps, we have applied a staircase analogy in which the stairs represent stages of risk and doors along the way symbolizing strategies that can support the de‐escalation of risk. Drug use is a complex phenomenon, and accordingly, these stages capture the trajectory for many—but not all—PWUD. Throughout this article, we apply the following definition of harm reduction: “a set of practical strategies and ideas aimed at reducing negative consequences associated with drug use … harm reduction is also a movement for social justice built on a belief in, and respect for, the rights of PWUD.” 23
This framework is also informed by our review of the health and policy literature, national guidelines on evidence‐based interventions, existing strategic plans, and our collective experiences. It recognizes a need for shifting investment from supply‐side approaches (ie, controlling prescription opioids and arresting PWUD) to interventions that address the social determinants of health. We reviewed contemporary models, frameworks, and theories commonly applied in the health literature in order to understand the existing views of drug use and overdose, including conceptualizations of drug use spectrums, 24 addiction as a “brain disease,” 25 harm reduction approaches to substance use, 26 a public health strategy to address the crisis, 27 and the social and economic determinants of the opioid epidemic. 10 Some of the tensions among those approaches preferred in medicine, public health, harm reduction, and the law are highlighted. Our comprehensive focus on the entire drug use continuum through a social determinants lens differentiates this framework from existing approaches. We prioritized interventions implemented domestically or internationally that were holistic and evidence based in order to spur cross‐adoption. Throughout, we call attention to some of the implementation barriers and research gaps that require urgent attention.
Unpacking the Continuum of Overdose Risk
The next five sections describe the risk factors associated with each stage of the COR. Strategies to address them are discussed in the second half of this article.
Drug Initiation
The timing and nature of drug use initiation can help determine subsequent trajectories of drug use and misuse. The onset of drug use during childhood or adolescence while the brain remains plastic can have long‐lasting impacts on the modulation of desires, emotions, and behaviors, 25 which in turn influences patterns of future drug use. Early initiation is also linked to subsequent dependence and riskier behaviors like injection, 28 , 29 which can increase the likelihood of infectious diseases, job instability, unintended pregnancies, and suicide. 30 , 31 , 32 Studies specific to opioid initiation show similar trends, with national data linking early initiation with subsequent risks such as poorer clinical outcomes, greater emotional distress, and increased tolerance and withdrawal symptoms relative to adult‐onset users. 33 We next look at several elements that may influence the opioid initiation environment.
Over the last decade, trends in the licit and illicit drug supply have received much attention. 34 , 35 Increased marketing and a greater number of prescriptions for OUD medications have increased the supply of prescription opioids, 36 , 37 resulting a birth cohort of opioid users significantly more likely to initiate use with prescription opioids or nonmedical prescription opioids (NMPO) than with heroin. 38 The availability of pharmaceutical opioids initially occurred in the context of shifts in pain treatment guidelines, along with the targeted marketing and lobbying by pharmaceutical companies to push profits. The resulting outcry concerning opioid dependence led to the formulation of abuse‐deterrent prescription opioids, the leveling of prescribing practices, and the use of prescription drug–monitoring programs (PDMP). However, an unintentional consequence of these interventions was a substantial resurgence of PWUD initiating with heroin, which became more easily available at a lower cost, triggering a second “wave” of the epidemic. 36 , 39 , 40
The emergence of synthetic opioids like illegally manufactured fentanyl and its many related analogues, which was partly due to economic pressures generated by law enforcement “crackdowns” of heroin suppliers, 4 , 16 critically shifted the drug supply and initiation environment for a third time. 41 Fentanyl is estimated to be 50 times more potent than heroin and accounts for 40% of overdose deaths. 42 It is sold as a stand‐alone drug and also contaminates a range of illicit drugs including heroin, counterfeit pills, and (in rare cases) cocaine. 43 , 44 , 45 This makes possible the inadvertent initiation of highly potent opioids and high risk of overdose among low‐frequency users. 46 , 47 , 48 , 49 , 50 Given the increased supply of illicit fentanyl in many states, it is likely that initiation patterns will shift between the current and the future cohorts of PWUD.
Although there has been relatively less attention paid to the epidemic's social roots, several social determinants that drive drug initiation have been identified: (1) microsocial factors, including trauma, social exposure/access to prescription opioids and illicit drugs; 34 and (2) macrosocial factors such as structural racism, income inequality, and affordable housing. 10 , 51 , 52 , 53 , 54 For example, although NMPO initiation and use is often a response to physical pain and injury, it can also be a response to life stressors like unemployment or untreated mental illness. 36 Place‐based factors have been well‐documented as critical to shaping the risk of drug initiation, with neighborhood‐level measures of disadvantage such as income inequality, low educational attainment, and racial segregation associated with an earlier initiation of overall substance use and administration via injection. 55 , 56 , 57 , 58 More broadly, the concept of despair 59 spreading within a geographic community or particular class (eg, an especially vulnerable labor market) is also increasingly thought to influence the likelihood of experiencing harmful outcomes like overdose. The literature on how these factors influence the conditions and age of opioid initiation is sparse, however. An overreliance on supply‐side interventions without a commensurate focus on these social determinants will not be sufficient to curb overdose deaths. 36 , 60 , 61
Finally, although the influence of individual‐level factors (eg, family history, mental illness, early use of alcohol or nicotine) 62 , 63 , 64 on drug initiation has been previously reviewed, 28 considerably less is known specifically about opioid initiation. The data suggest that the initiation of NMPO is concentrated among those between ages 18 and 25, 65 and that early initiation of NMPO is associated with heroin initiation and later‐life dependence on other prescription drugs. 66 , 67 , 68 , 69 , 70 Our recent work 71 shows that PWUD initiating with NMPO are significantly more likely to engage in the nonmedical use of benzodiazepines—a risk behavior that, in conjunction with opioid use, amplifies overdose risk—and illustrates the greater risk of initiation with NMPO among women who are entering the risk population in greater numbers now that NMPO have so fully penetrated street drug markets. 72 Nonetheless, there is insufficient research on ways to detect and intervene 73 to delay opioid initiation at the individual level, and we know very little about the initiation of fentanyl. Research and surveillance to identify actionable targets to delay opioid initiation, incorporating individual as well as the micro‐ and macrosocial elements of the initiation environment, are needed.
From Initiation to Active Drug Use
What happens between opioid initiation and the development of harmful dependent use? Although we often assume that dependence inevitably follows opioid initiation there is a distinction between recreational, nonproblematic drug use for pleasure, and persistent or uncontrollable drug use to relieve psychological, physical, or emotional pain, which impairs social functioning. 25 , 36 This is reflected in US national statistics: In 2019, more than 11 million individuals in the United States reported using opioids for nonmedical reasons, with only a small fraction meeting the definition of an OUD. 74 Notably, the dominant rhetoric in the public health, medical, and legal arenas fails to acknowledge that many people use drugs regularly without the overwhelming physical, psychosocial, individual, and interpersonal harms characteristic of OUD and addiction. The term PWUD has been increasingly adopted as a nonstigmatizing term that acknowledges that drug use exists on a continuum from recreational use to severe dependence, though there is less discourse and research on this topic in the current epidemic.
At the level of individual biology, sustained and dependent patterns of opioid use alter the neurological circuitry that produces fewer returns per episode of consumption (ie, physical tolerance), which can result in the altered regulation of executive processes such as decision making and inhibitory control (ie, resisting “urges”). 25 In addition, the strong relief that opioids provide from states like despair, sadness, anxiety, or physical pain may be “learned” by the mind and body and compound the craving to use them to relieve the symptoms of distress, which include withdrawal. 75 Changes in tolerance can lead to the adoption of higher‐risk practices. Examples are more frequent use and the use of several drugs or high‐risk (but more economical) routes of administration such as injection drug use to achieve the same levels of relief. 76 , 77 , 78 , 79 These practices also confer a greater risk of overdose, particularly during recurring cycles of stopping and resuming use. 80 , 81
Risk factors for progressing to harmful patterns of use overlap with those we described in the previous section. For example, experiences of violence and abuse, particularly during childhood, are linked with the likelihood of increased substance use disorder (SUD). 82 Upstream social and structural segregation and economic disadvantage in both urban and rural environments further increase the likelihood of successive adoption of higher‐risk practices, including binging and injection. 34 , 53 , 83 , 84 Initiation of injection represents a critical shift in risk, as introducing substances directly into the bloodstream increases the PWUD's vulnerability to changing potency and drug formulation and amplifies the risk of overdose 85 , 86 , 87 , 88 , 89 and blood‐borne infections. People who inject drugs also face greater levels of stigma and discrimination, which in themselves are additional barriers to accessing social and medical support, financial stability, housing, and employment and thereby compound the risk factors for progression along the COR. 22 While many of these factors can lead to the adoption of riskier practices, they also are consequences of higher‐risk drug use. For example, the risk of experiencing violence, eviction, or homelessness is higher for individuals progressing further along the COR, cycling through the criminal justice system, and dealing with the ensuing mental, physical, and economic consequences.
Alcohol research and policy clearly distinguish between recreational use and harmful dependence, allowing for a greater focus on tailored prevention and treatment and reserving punitive measures for circumstances when grave harm is caused to others (eg, drunk driving). In contrast, studies of illicit drug use often rely on dichotomous outcomes of success defined by abstinence, with frequency or measures of harm caused rarely used to delineate what is “problematic.” 90 , 91 , 92 This is changing in the cannabis literature, as the legalization of recreational use has created the need for more clearly defined gradations and parameters around consumption, 90 , 93 but this delineation remains largely absent in reference to other drugs. One study has shown that a lower frequency of heroin injection is associated with lower rates of nonfatal overdose. 94 A one‐size‐fits‐all definition of opioid use ignores the likelihood that the trajectory to overdose differs between individuals who use drugs recreationally and those who have a harmful dependence on them. Consequently, we need research, surveillance, and discourse to define the distinct stages of drug use more effectively, in order to allow greater specificity in designing interventions to avert overdose among individuals with fundamentally different relationships to illicit substances.
Addiction
Several theories have tried to explain the sequelae of opioid addiction. Historically, these have varied considerably. The early 19th to late 20th centuries saw broad shifts from the widespread social acceptance and legalization of heroin and morphine for medical and recreational use due to their pain‐relieving and euphoric properties, to the view that heroin use was a moral failing requiring punishment, which still prevails in the United States and abroad. 95 This stigma‐driven view fueled support for the War on Drugs, led by the United States, which resulted in the global mass incarceration of PWUD, particularly in communities of color and among low‐income women, frequently in breach of their constitutional rights, 11 , 96 as well as state‐sponsored mass killings of PWUD and drug dealers in countries like the Philippines. 97 Without legal reform, barriers to accessing vital services will hinder our ability to implement real change and continue to marginalize PWUD.
The brain disease model of addiction centers on the neurobiological and psychological changes caused by chronic opioid use. 25 While this model has been a critical tool in shifting the paradigm away from moral judgment and stigma, its proliferation raises at least three important concerns. First, the model supports a dichotomy that sees abstinence as the only way to recovery and sees a return to drug use as a “relapse” that inherently causes harm. These social norms can create the abstinence violation effect, a set of negative emotional and cognitive responses that perpetuate the drug‐related stigma experienced by the individual after resuming drug use. 98 The second concern focuses on biomedical solutions to addressing opioid addiction, rather than those rooted in the social determinants of health that characterize the lives of many PWUD. Third, by popularizing the idea that addiction “highjacks the brain,” the model threatens to undermine harm reduction efforts by eroding the legal constructs of agency and self‐determination among PWUD. This is already apparent in the proliferation of statutes authorizing involuntary commitment for substance use and the rising number of states actively deploying these mechanisms in order to institutionalize PWUD against their will.
Microsocial factors such as lacking social integration or the support of family and friends, and exposure to interpersonal trauma have been conceptualized as risk factors for addiction and may operate through similar neural pathways as the opioid addiction process does. 99 Adverse childhood experiences (ACE) and traumatic experiences are consistently associated with mental illness and SUD. Substance use may be an attempt to “self‐medicate” from these stressful experiences, 100 , 101 and such maladaptive coping behaviors are hypothesized to drive addiction and relapse. 102 Previous studies corroborating this hypothesis have shown that trauma and mental illness are more likely to occur before rather than after the onset of SUD among women 101 , 103 and to aggravate symptoms over the long term. 104 Stressful life events among individuals in recovery who have developed learned associations between opioid use and relief from negative mental states over time may trigger drug relapse and sustain drug addiction. 75
Stressful life events that place populations at risk of addiction often operate at the macrosocial level. Examples of these life events are homelessness, unemployment, concentrated disadvantage, structural racism, trauma, and hopelessness, which have been discussed in relation to the opioid crisis. 10 In addition to needing to escape the physical effects of drug withdrawal to being triggered by social cues associated with drug use (eg, seeing a dealer), research on drug cessation and relapse shows that patients often develop learned associations between opioid use and relief from the negative mental impact of life stressors. These associations may make it difficult to break the cycle of addiction without broader intervention addressing macrosocial triggers, 75 which may help explain why many people resume using drugs after a period of abstinence. 105 Taken together, this body of literature highlights that overreliance on the brain disease model may serve to disempower affected communities by pathologizing drug use and undercutting the role of individual agency and contextual factors that may lead to addiction.
Nonfatal Drug Overdose
Nonfatal drug overdose, affecting 17% to 68% of PWUD, is a significant risk factor for a fatal overdose and also is associated with a range of health (eg, cognitive and muscular dysfunctions), social (eg, “compassion fatigue”), and economic (eg, emergency room costs) consequences, marking it as a critical target for intervention. 106 , 107 , 108 , 109 , 110 The literature on risk factors exhibits high heterogeneity in the types of nonfatal overdoses examined (eg, any drug versus opioids), the target population (eg, injectors versus noninjectors), and their historical, sociopolitical, and economic contexts. However, several individual‐level risk factors of nonfatal overdose have endured over time, recently highlighted in a systematic review. 106
The risk of a nonfatal overdose is high after periods of abstinence (eg, recent release from detoxification or incarceration without access to MAT) because the tolerance to opioids is lower than normal. 111 Polysubstance use (also known as polydrug use and concomitant use), particularly between multiple opioids, or opioids in combination with depressants such as alcohol or benzodiazepines, can increase overdose risk owing to the compounding effects on the body's metabolic systems. 108 , 110 , 111 Injection drug use is also a strong risk factor for a nonfatal overdose. 112 , 113 , 114 , 115 Documented risk factors include fentanyl injection 116 and the assumption that drugs contain fentanyl. 49 Some studies also point to underlying mental illness, including suicidal behaviors and other medical comorbidities. 108 More research is required to elucidate the risk factors of nonfatal fentanyl overdose among noninjectors, although many risk factors are expected to be comparable for the two populations. 106 , 112
Although the social determinants of nonfatal overdose receive comparably less attention, emerging evidence has documented higher risks associated with incarceration, unstable housing, 49 , 83 , 111 and drug use in public settings 116 , 117 , 118 (which often accompanies homelessness). Homeless PWUD who rely on public spaces to use drugs are at a heightened risk of robbery, stigmatization, and harassment from community members and interactions with police, and these factors can lead to rushed and unsafe levels of drug use and overdose. 117 , 119 , 120
Broader place‐based and macrosocial factors have been explored as important drivers of overdose risk in urban and rural communities at different periods in history, such as deindustrialization, stagnation of economies, population loss, and despair. 121 , 122 Community poverty endures as a condition that elevates the risk of overdose. A recent analysis of overdose hospitalizations in 17 states from 2002 to 2014 found that zip code–level poverty was associated with increased heroin overdose hospitalizations in urban areas. 123 Paradoxically, drug criminalization laws may increase overdose rates among PWUD by creating an environment where safe drug preparation and use is compromised and rushed in order to avoid police harassment, arrest, and incarceration. 111 , 124 , 125 The availability and regulation of opioids also contribute to overdose risk. 108 In settings where the manufacturing, distribution, and marketing of drugs are criminalized and thus unregulated, illegal drug markets may contain products of unknown or unpredictable purity and doses that pose a high risk of fatal and nonfatal overdose, as we describe more fully below. 10 , 108 , 126
Fatal Drug Overdose
Beyond individual‐level factors such as polysubstance use 80 , 127 , 128 and reduced opioid tolerance following abstinence‐based treatment 81 or incarceration, 80 , 127 , 128 , 129 , 130 , 131 , 132 broader risk factors contribute to the lethality of the current epidemic. The major challenge with the current synthetic opioid epidemic is the infusion of illicit fentanyl and related analogues. 4 , 19 These potent drugs come in the form of powders, tablets, and liquids. In the absence of regulation and drug checking programs, the high potency and rapid absorption properties of fentanyl narrow the window of opportunity to revive someone using naloxone and render the drug highly lethal even among chronic opioid users. 126 The penetration of fentanyl into heroin markets has resulted in high rates of overdose mortality among heroin users who may unknowingly use fentanyl that is marketed to them as heroin or who are unaware that the product is contaminated with fentanyl. 46 , 48 , 49 Even among those who knowingly use fentanyl, the purity is often unknown, which makes safe dosing a challenge. Alarmingly, synthetic opioids are involved in deaths attributable to prescription opioid pills (24%), cocaine (40%), benzodiazepines (31%), psychostimulants (14%), and other drugs (27%). 133
A growing number of studies at multiple levels have examined risk factors other than supply‐side factors, although these enduring and fundamental determinants of overdose have received less attention. 10 , 127 For example, PWUD who are witnesses to fatal overdoses frequently state their fear of police arrest as a reason for delaying or refusing to call emergency medical services (EMS). Unsurprisingly, geographic areas with higher rates of police activity (ie, arrest) exhibit higher population‐level overdose mortality, which may be driven by fear of calling for medical help among bystanders. 132 Naloxone coverage remains low among PWUD, many of whom have seen their family and friends die of an overdose. Notably, no national surveillance data are available on naloxone coverage among PWUD and others at a higher risk of witnessing an overdose. 134 Solitary drug use, which is practiced by an estimated 58% of PWUD, lowers the chances of EMS being called or naloxone being administered. 135 , 136 , 137 State‐level income inequality has been shown to be highly correlated with drug overdose deaths in the early 2000s. 127 , 131 , 138
The roles of race, sex, drug, time, geography, and urbanicity in relation to overdose risk require further attention. 122 For example, the disaggregation of national mortality trends has shown that age‐adjusted mortality among women in the southern United States continued to grow between 2000 and 2013, whereas among men it peaked by the mid‐2000s. 139 Urban areas in 2017 faced a higher burden of mortality from heroin, synthetic opioids, and cocaine, but rural areas faced higher mortality from prescription opioids and methamphetamines. 140 In regard to racial disparities, cocaine was the largest contributor of deaths among Black men and women between 2000 and 2015 but not among whites. 141 From 2014 to 2016, mortality among whites from drug overdose was highest in urban areas and associated with both socioeconomic and opioid supply factors. 142 Whether all these trends can be attributed to “despair” or other factors needs further investigation. In any case, tailored interventions that account for these factors will likely be required at the local level. 143
Although the demographic, socioeconomic, and drug supply factors warrant further examination, our review suggests that the risk factors along the COR are multifaceted and necessitate a comprehensive, evidence‐based strategy that is attentive to local needs. We next look at several of these strategies.
Opening Doors to De‐escalate Risk: Six Strategies
Given the nature of the risk factors that drive drug use and overdose (examined in the previous section), we identified and grouped interventions that together could de‐escalate risk over the long run and address drug‐related morbidity and mortality. Our findings are organized around six strategies: (1) meaningful partnerships with PWUD, (2) prevention, (3) harm reduction, (4) treatment, (5) recovery, and (6) reversal of the criminalization of PWUD. We chose interventions that are most likely to have a population‐level impact on addiction and overdose burden, keeping in mind that the implementers should be responsive to local place‐based needs. Many strategies have already been successful in several states, while others have been evaluated internationally. Ensuring that these approaches are applied through a racial, gender, and class equity lens will be critical, given the disproportionate effects of decades of punitive policies and broader economic forces on these populations.
Meaningful Partnerships with People Who Use Drugs
PWUD have been the driving force behind the international harm reduction movement. 144 , 145 In the Netherlands, early SSP, peer education programs, and treatment policies were driven by drug user unions. 146 The emergence of HIV/AIDS, which appeared among US PWUD in New York City in 1981, as well as significant activism by PWUD and their allies, propelled the adoption of SSP as a public health measure against HIV and viral hepatitis transmission in some parts of the country and, later, the scale‐up of community‐based naloxone and other important risk reduction programs. 145 , 147 Nonetheless, despite their pivotal historical role, PWUD are often sidelined in the present‐day development of programs, policy, and research.
Central to a harm reduction approach are the experiences and voices of PWUD when developing opioid strategies. The most direct method involves including PWUD in positions of leadership and decision making 21 , 148 because their involvement brings expertise and humanity, and therefore relevance, to the design and implementation of programs, policies, and laws. Even though PWUD have provided critical input for global health issues such as HIV/AIDS, they have been systematically excluded from influencing drug policy. This includes measures like felon disenfranchisement laws, prison gerrymandering, and other efforts to deprive people who are incarcerated or have a history of incarceration, specifically people of color, from participating in the political process. A key measure to sensible and humane drug policies is dismantling the barriers to political participation for those who are most directly impacted by drug policy.
Throughout history, PWUD have also had a pivotal role in the development and delivery of outreach services, including SSP, naloxone programs, HIV education, counseling, and recovery support. 144 , 149 Peer‐based interventions have been shown to improve harm reduction education and supply distribution and to reduce injection and sexual risk behaviors among PWUD. However, many are precluded from federal and state employment, even though their community relationships and cultural competencies could help these programs succeed. Legal protection from discrimination, like the Americans with Disabilities Act (ADA), which covers individuals with alcohol use disorder, have often not been successful in SUD cases, especially in view of the “illegal use” exception to this statute (42 U.S.C.A. § 12114[b]). Eliminating this exception would provide some legal protections from discrimination.
Being convicted of drug charges and labeled as a felon create far more barriers than most people fully comprehend. These barriers often include, but certainly are not limited to, an inability to obtain gainful employment. Although “ban the box” legislation would prevent employers from investigating past drug convictions and would mitigate future discrimination, these efforts would not fully prevent discrimination because of public criminal records. Even in places where PWUD are engaged in paid work, they risk being arrested if their drug use (past or present) is discovered. In addition, universities regularly bar people with criminal records from employment and often prevent PWUD from receiving student loans and access to college grants and scholarships. Many employment credentials and certifications are not accessible to felons. Drug convictions also pose a barrier for housing and food in the United States, with landlords regularly denying housing applications for people with criminal records, and many states denying government assistance like food stamps to people with drug convictions.
Stigma is another factor that adds to the marginalization of PWUD. 27 , 150 In a national survey, most respondents reported stigmatizing views toward OUD patients (eg, blaming them for having a disorder). 151 Another study found that stigmatizing terms were used to describe PWUD in half of all news stories examined from 2008 to 2018. 152 In addition, the media's negative portrayal of racial minority PWUD, in contrast to holding white suburbanites blameless, has been observed. 153 The enduring stigma towards PWUD in the health care sector also remains a barrier to seeking and receiving compassionate and quality health care. 154 Despite their own lack of experience, most policymakers and academics fail to see PWUD as experts. Although many organizations are led by PWUD (eg, Urban Survivors Union, New England User Union, Bmore POWER, International Network of People Who Use Drugs, Women and Harm Reduction International Network), few researchers and policymakers take the time to create real buy‐in when engaging in opioid work. Albeit rare, participatory approaches in research that draw on the expertise of PWUD can decrease stigmatization and researcher bias. Fostering meaningful partnerships with PWUD to address the opioid response holds great potential in ensuring that policy and research priorities are appropriate and effective.
Prevention
Prevention is a broad term that encapsulates a range of interventions across the life span. Many evidence‐based prevention programs exist,150ranging from early education to public mass‐media campaigns. However, these programs focus heavily on drug use prevention or abstinence rather than overdose prevention, as reflected by the outcomes typically reported in their evaluation. In fact, as the narrative moves away from the “white” prescription opioid crisis, it is reverting to a campaign of scare tactics and misinformation resulting in a revitalization and commitment to America's war on drugs. This is exemplified by the recent rhetoric and policy promoting harsher penalties for the possession or sale of fentanyl, for example, than for other opioids, as well as drug‐induced homicide laws. 13 , 16 Limiting prevention efforts to the deterrence of opioid use rather than harm reduction reflects long‐standing stigma toward PWUD, equating abstinence with recovery, as well as policies aiming for a “drug‐free society” that punishes those who use drugs. Such views and policies continue to hamper prevention efforts by fueling the stigma and marginalization of PWUD.
We argue that society must shift from the model of judgment and punishment of PWUD to one accepting that drug use will likely persist (as it has throughout history). To improve the health of and social outcomes for future generations, interventions should also target the full COR, from initiation to overdose, and follow harm reduction principles. For example, the integration of educational information about opioid awareness, naloxone, Good Samaritan laws, and OUD treatment into existing drug education programs may better equip individuals to prevent drug‐related harms, like overdose, rather than focusing on averting drug use altogether. Avoiding stigmatizing terms like drug abuse and addict in the narrative characterizing PWUD could help shift some key barriers to safer drug use and access to treatment.
Prevention efforts targeting factors upstream of the drug initiation, informed by the social determinants of health model, are an important avenue for research and evaluation. For example, efforts to alleviate neighborhood‐level poverty or blight and the promotion of access to education, employment, and housing would likely bolster overdose prevention efforts. These are often de‐prioritized, however, owing to their scope and the many years before “returns on investment” are measurable, and they therefore lack a solid evidence base.
Increased oversight of opioid prescribing through PDMPs and providers’ greater awareness and restriction of the illegal marketing of opioids through lawsuits have been successful in reducing the supply of pharmaceutical opioids. 106 , 155 But tackling the upstream policy environment that enables poor opioid stewardship, including laws that permit pharmaceutical companies to pay doctors both directly and indirectly and to advertise their products to consumers through the media, is another reform that has not yet been pursued. These approaches also do not address the needs of already opioid‐dependent individuals. Moreover, research suggests that the reduction of prescription opioid supplies through PDMPs may have inadvertently led to increased rates of heroin overdose deaths. 106 , 155 These supply‐based approaches also fail to help those who initiate opioid use through heroin or fentanyl, especially among underserved urban communities of color who have been suffering the effects of this crisis for decades.
Harm Reduction
Naloxone and Good Samaritan Laws
It has been almost 50 years since the US Food and Drug Administration (FDA) approved the use of naloxone, a medication that can reverse the course of an overdose by strongly binding to opioid receptors in the brain in the place of opioids and effectively blocking their effects. Unlike other interventions, naloxone is the only tool that directly prevents fatal overdoses. Although fatal overdoses often occur in the presence of bystanders, the majority do not administer naloxone, indicating a missed opportunity for intervention. 136 Even so, tens of thousands of overdoses have been reversed through the distribution of naloxone in the community. 147
The Centers for Disease Control and Prevention (CDC), among others, recommends that the scale‐up of naloxone programs should target those people who are most likely to experience or witness an overdose, including active PWUD (eg, at SSP, emergency rooms, drug treatment facilities, recovery programs, infectious disease and mental health clinics, and jails/prisons), first responders (eg, EMS and police), and service providers (eg, outreach staff and clinicians). 136 , 156 Training potential bystanders (eg, family and friends of PWUD) has been successful and could have a substantial impact on overdose rates if such programs were scaled‐up. 147 The implementation of coprescribing policies, as well as standing orders permitting over‐the‐counter dispensing of naloxone without a prescription has increased access in some states, like Maryland. Given the current fentanyl crisis, it is imperative that individuals receive at least three doses of naloxone in case a higher dose is required.
The limitations of naloxone programs also should be noted. First, naloxone does not address nonfatal overdoses, which account for a large proportion of social and economic burden, and thus other interventions are always needed. Second, the fear of police involvement often keeps bystanders from calling EMS and intervening. Naloxone programs need to be coupled with a federal Good Samaritan law to provide legal protections to those who try to intervene in the case of an overdose, and implemented effectively. 156 , 157 Third, because of fentanyl's lipophilic nature, overdoses occur rapidly, so waiting for EMS may not be an option. 21 , 36 Finally, even though solitary drug use is common, it is often not addressed. 37 Preventive interventions are needed that target the earlier stages of the overdose trajectory.
Overdose Prevention Sites
Overdose prevention sites (OPS), also known as safe consumption spaces and supervised injection facilities, are places in which PWUD can use previously purchased drugs under trained supervision. 158 , 159 , 160 If scaled‐up, OPS could address many issues regarding naloxone, bystanders, and police. There are more than 110 OPS in 66 cities worldwide. Evidence on the impacts of OPS demonstrates their significant association with reducing overdose fatalities, HIV and HCV transmission, syringe sharing, public injection, ambulance usage, and crime. 161 , 162 , 163 , 164 Furthermore, OPS increase entry into drug treatment, have never housed a fatal overdose, and have been found to be cost‐effective. 165 , 166 , 167 There is one unsanctioned OPS documented in the United States, 168 although many more likely exist, and a number of US jurisdictions, including Maryland, are considering legislation to legalize these potentially lifesaving spaces. In Philadelphia, the nonprofit Safehouse was established with support from the mayor, health commissioner, and private donors. Despite a civil lawsuit (21 U.S.C. §856[a]), a US district judge ruled in favor of Safehouse. Even though they are currently underutilized, OPS hold great potential for saving lives in the United States, particularly in areas of concentrated poverty, drug use, and overdose.
Drug Checking
Drug checking programs enable PWUD, without the risk of arrest, to have their drugs chemically analyzed for the presence of substances like fentanyl and its analogues and for their purity, thereby allowing for more informed decisions about subsequent drug use. 169 , 170 , 171 , 172 These programs, which were pioneered in Europe and are inclusive of laboratory‐based and point‐of‐care models, have the potential to promote product safety in the illicit drug supply in the United States, where its use has been limited to testing drugs at music festivals and some SSP and community‐based organizations. Such services are needed in the context of a large unregulated illicit market in which the quantity and purity of illicit drugs (eg, heroin) remain uncertain. We, among others, have found a high level of interest in drug checking programs among urban PWUD and associated behavior change (eg, obtaining naloxone, using in the presence of others). 72 , 173 , 174 , 175
Legal barriers will need to be overcome in order to scale‐up drug checking programs. The Controlled Substances Act (CSA) prohibits the possession of controlled substances, which includes community‐based collection of drug samples. Consequently, there are barriers to implementing drug checking programs in the community, and the current drug surveillance system relies heavily on drug testing data from law enforcement that may not fully represent the broader drug supply. Reforming the CSA would enable the direct testing of samples collected from the community to strengthen surveillance, improve awareness, and promote safety.
Treatment
The provision of methadone and buprenorphine to manage OUD (also known as medication‐assisted treatment) is an important aspect of a comprehensive overdose reduction strategy. 154 , 176 , 177 The gold standard medical treatment for OUD is maintaining patients on either methadone or buprenorphine/naloxone. As opioid agonists, these drugs reduce cravings, treat withdrawal symptoms, and stabilize the patient. Methadone and buprenorphine/naloxone can be considered harm reduction tools insofar as many patients, despite continuing to take opioids, still receive important health benefits from treatment. A third FDA‐approved drug approved for OUD treatment is extended‐release naltrexone. While opioid agonists occupy the same receptors in the brain that illicit opioids stimulate, naltrexone blocks receptor activity and is therefore an antagonist. Building on decades of evidence, a 2019 report from the National Academies of Science, Engineering, and Medicine concluded that OUD medications are effective at reducing overdoses and promoting recovery and yet are massively underprovided in the United States. 154
Opioid agonists reduce overdose risk by causing people to use illicit opioids less frequently and to stop injecting opioids (and consequently reduce their risk of acquiring infectious diseases) and ultimately to abstain from using illicit opioids. 178 Their protective effect has been demonstrated in clinical trials and cohort studies. 179 Moreover, because patients receiving agonist treatments do not completely lose their tolerance, they also make it less likely that people will overdose if they return to using drugs, compared with medication‐free treatments. 180 For this reason, even though naltrexone is more commonly used in correctional settings, its use for preventing overdoses and providing other health benefits has been demonstrated to be far inferior to opioid agonist treatment. 181
The current paradigm for delivering treatment is fundamentally failing. Most OUD patients are not receiving treatment, and fewer than half the treated patients are receiving agonist medication. 182 Moreover, when they do receive treatment, it is often inadequately short and fragmented. 183 Access to treatment is particularly difficult for the most vulnerable, such as people in the criminal justice system, in which only one in twenty individuals receive OUD medications. 184 Comorbidities such as underlying mental illness (eg, stemming from trauma) are often left untreated as well, even though more than 60% of OUD patients suffer from mental illness and high levels of trauma. 185 Limited access to OUD treatment likely reflects the stigma toward PWUD and OUD medications, including the perception that medications merely “substitute one drug for another.” 186 Drug‐related stigma is pervasive in all sectors—among doctors, law enforcement, and in many segments of the recovery community. 187
Stigma reinforces, and is reinforced by, burdensome regulations that ironically make it more difficult to access OUD treatment than addictive opioid pain relievers. Specifically, since the 1970s, access to methadone has been restricted to certified opioid treatment programs, which themselves are often subject to additional regulation and discriminatory zoning rules. In Canada, Australia, and the United Kingdom, by contrast, methadone can be accessed through primary care. 188 Although buprenorphine is available in primary care settings in the United States, it is limited to providers who have obtained a federal waiver. The number of providers has grown somewhat in recent years, but many areas still do not have an adequate supply of providers, 189 and most treatment is not “on demand.” 190
Expanding treatment across the United States that could achieve widespread public health benefits would require substantial change. It would require the confluence of at least three elements: stigma reduction, increased financing, and regulatory change.
Stigma reduction would focus on normalizing opioid agonist treatment and making OUD a mainstream medical issue, much as diabetes is considered a chronic disease that is appropriately managed in primary care. In particular, stigma reduction in the context of treatment delivery would necessitate fundamental changes in the training of medical professionals and other first responders. Currently, medical professionals receive little to no education in addiction medicine and are sometimes professionally socialized to see people with addiction issues as untrustworthy, dangerous, and unsuitable for treatment in primary care. 191 Creating stronger expectations for medical professionals about how they interact with PWUD and measuring patient satisfaction, as well as promoting further research on this topic in partnership with PWUD will be necessary in addressing the stigma of PWUD in health care.
Much of the current treatment for OUD is derived from public sources, especially Medicaid, which has grown as a payer after the Affordable Care Act (ACA) was passed. 192 The ACA established that covering OUD and mental health services is essential and reinforced that benefits should have parity with other medical conditions. While the growth of funding has been important, available funding is currently failing to meet needs in several ways. First, many states do not comprehensively cover treatment costs or limit the duration of time that publicly insured individuals are able to remain in treatment. 192 Second, many providers still do not accept publicly insured patients, which may reflect the lower reimbursement offered by Medicaid and administrative hurdles, such as prior‐authorization rules. 190 Third, supplemental federal funds (eg, the 21st Century Cures Act) have opened new treatment slots but are time limited without further funding.
Finally, regulatory changes are needed. The long‐term objective should be dismantling the burdensome regulatory framework dating back to such antiquated drug control policies as the 1914 Harrison Narcotics Act, the federal law that forbade doctors from prescribing opiates (including, ultimately, methadone and buprenorphine) to people known to be addicted to drugs. 193 In the shorter term, smaller regulatory changes could boost access to treatment, including removing the patient cap for physicians who prescribe buprenorphine, providing prescribing authority to all prescribers with a DEA license (along with a revamped addiction curriculum), and providing more options for methadone provision offered at nontraditional locations such as mobile vans or jails.
The cumulative effect of these policy changes would be a new framework to treat OUD that combines the resources for treatment with the enabling regulations and a workforce that is more motivated to care for these patients. The ultimate test of this treatment's effectiveness would be measured by the increased number of patients who initiate and stay in treatment and ultimately by fewer overdose deaths.
Recovery
Recovery programs are often included in national and state strategic plans, yet most of them implicitly or explicitly conflate the term recovery with abstinence from drug use. As noted in the Surgeon General's report, it is possible to be in recovery and still use opioids, whether they are medically supervised (eg, MAT) or not (eg, controlled safe use). 150 The federal definition offered by SAMHSA (Substance Abuse and Mental Health Services Administration) demonstrates that recovery involves more than a person's drug use and consists of “a process of change through which people improve their health and wellness, live self‐directed lives, and strive to reach their full potential.”
Many laws, policies, and strategic plans, however, do not reflect this definition of recovery, which paradoxically poses major hurdles for PWUD who seek long‐term recovery. Addressing the social determinants of health (eg, employment, housing), and structural barriers such as the integration of services targeting SUD, along with mental health and general health services, would go a long way in supporting recovery programs. Examples of specific changes are (1) expunging low‐level, nonviolent, drug‐related offenses; (2) instituting a federal “ban the box” law; (3) including PWUD in broader discrimination laws like the ADA to reduce employment discrimination; (4) banning drug testing when it is unrelated to the candidate's ability for the job; (5) creating affordable housing opportunities that are not contingent on maintaining abstinence; and (6) treating SUD as a chronic condition and providing wraparound services (prevention, harm reduction, and mental health services in addition to drug treatment) that are not contingent on maintaining abstinence. Prioritizing interventions based on geography may be warranted in accordance with local needs. For example, homelessness, violence reduction, and structural racism may be more urgent to address in urban areas, whereas health insurance, and treatment of injury‐related pain may be more appropriate in rural areas with economies reliant on mining. 123 , 142
In order to maximize the impact of these interventions, economic policies to reduce community‐level poverty targeting education barriers, wage stagnation, and unemployment, could be implemented by raising the minimum wage, investing in public education (particularly for low‐income communities), and strengthening labor rights. 194 Finally, access to affordable health care is needed to support recovery.
Reversing the Criminalization of PWUD
Activists, academics, and policymakers are increasingly recognizing the harms to individuals and societies that results from drug prohibition and the aggressive enforcement of punitive legislation, including the criminalization of addiction. 11 , 12 These laws and policies have resulted in high incarceration rates among PWUD and low‐level drug dealers but have done little to stem the flow of illicit opioids (including fentanyl) into the United States and have systematically targeted and exploited Black communities for many decades. 11 , 195 The many psychosocial and economic consequences of heavy‐handed law enforcement and repeated incarceration have been shown to amplify the risks associated with drug use—including overdose—and to raise barriers to providing public health resources to prevent overdoses.
The criminal legal system—from initial police encounters to incarceration, parole, and reentry—plays an outsized role in this crisis. An estimated 65% of the 2.3 million people in US prisons and jails have a diagnosable SUD, more than seven times the rate in the general population. 196 Nearly 15% of incarcerated men and 30% of women also have diagnosable mental health disorders. 197 There is broad recognition that in the context of mass incarceration, correctional institutions act as the de facto national substance use and mental health safety net. 198 Even so, correctional health efforts to address these health conditions often fall below medically accepted standards of care.
Each phase of involvement in the criminal legal system—from the point of crisis before arrest, through detention, and after release—is an opportunity to better address SUD and mental health challenges. This means that criminal legal institutions must (1) screen and diagnose, (2) treat, (3) monitor and support, and (4) triage individuals to appropriate health care and prevention services. Other researchers have developed a model for using key inflection points to help provide necessary health care along a five‐phase continuum. 199 Rhode Island is a model state for providing the continuum of OUD care among individuals who enter the criminal legal system. 199 , 200
Even where there is access to treatment, the conditions of community supervision frequently bar returning individuals from obtaining buprenorphine or methadone and then punish them for experiencing relapse. 201 This may be done through parole boards’ policies, judges’ or community supervision staff practices, or conditions imposed by transitional housing and other programs. 202 Reforming community supervision systems to play a supportive rather than a punitive and coercive role can help facilitate recovery and prevent negative outcomes, including death.
Cyclical involvement in the criminal legal system is likely if the social determinants of health are not addressed. Untreated substance use and mental health challenges, poverty, barriers to employment and education, isolation, intrusive government surveillance, and racism are among the factors driving the cycle of vulnerability. To stop this cycle, “off ramps” must be built to divert individuals to supportive structures and services. This begins in the community—at Intercept 0—where measures like Law Enforcement Assisted Diversion (LEAD) programs and opioid agonist treatment can help avoid system involvement now and prevent it in the future. 203 Given the multiple cascades of harm, the ultimate goal must be to minimize system contact whenever possible.
Off ramps should never lead into a ditch, however. In most jurisdictions, policing and criminal legal budgets have long outpaced investment in community‐based services. As a result, many communities lack adequate quality substance use and mental health treatment, affordable housing, meaningful employment, and other supportive mechanisms that can help avert contact with the criminal legal system. This has ensured that the criminal legal sector is not just the safety net of last resort but is the only governmental system that many vulnerable people can reliably access. In the short term, improvements to health and other services in correctional and other criminal legal system components are urgently needed to reduce their harm. This includes the provision of sanitary supplies, testing, screening, and treatment to help prevent the spread of COVID‐19. In the long term, investing in legitimate public health approaches and measures of social support through the decriminalization of low‐level drug possession (as realized in Portugal and several other countries 12 , 204 , 205 ), early‐release efforts, and the reversal of decades of policies that have systematically disenfranchised PWUD from education, employment, and housing will help reduce our reliance on coercive and punitive systems to address the substance use and mental health crisis in our society. 13 There is a precedent in the United States for reversing the criminalization of PWUD, from marijuana decriminalization to the release of nonviolent PWUD from jails because of COVID‐19.
Research Gaps
Too often, the social determinants of health are neglected when examining the COR and developing methods to address the escalation of risk. Public health initiatives would benefit from a more detailed understanding of the social drivers of illicit opioid use initiation (NMPO, heroin, synthetics), decision making that sustains use, transitions between different types of opioids, and how use propels individuals along the COR. Despite the scope of fentanyl‐involved polysubstance use, we have yet to determine whether PWUD have a greater need for stimulants owing to the strength of fentanyl and whether their frequency of use has increased, which may confer greater risks. In addition, despite efforts to research the actual and perceived benefits of substance use (eg, marijuana, alcohol use), as well as ways to minimize harm, research in this area is limited for opioids, particularly fentanyl. Related to this is the need to employ a more diverse set of outcome measures in substance use research, including measures of frequency of use, quality of life, interpersonal relationships, job stability, and de‐escalation of risk through transitioning to other substances (ie, marijuana).
Biomedical research could spur the development of crucial tools for prevention (eg, the link between OUD and mental health) harm reduction (eg, drug checking tools, a naloxone‐equivalent for all drugs involved in overdoses), and treatment (eg, medication‐assisted treatment for cocaine). We also need US‐based proof‐of‐concept research for successful biomedical interventions that are available in other countries (eg, diacetylmorphine “heroin‐assisted” treatment). 206 , 207
The stigma toward PWUD, harm reduction programs, and medications for OUD persists in many parts of the country, including among law enforcement, first responders, providers, researchers, and policymakers, and it threatens public health responses to the opioid epidemic. We urgently need to develop and evaluate effective interventions that reduce stigma and the resultant harms among different populations. 208 In addition to stigma, we need to better understand why evidence‐based public health‐oriented approaches, such as the role of power and interest groups, are widely available in some countries but not others (see the Limitations section).
Finally, new and existing laws, policies, programs, and practices that address drug use should be based on data and rigorously evaluated. We should do more to support real‐world implementation research that evaluates prevention, harm reduction, treatment, and criminal justice approaches to the epidemic, with priorities set in consultation with PWUD. Removing barriers to accessing health data at the county and state levels and increasing funding for community‐ and policy‐based research on the social determinants of health framework would boost this line of work. Future studies could also examine how frequently PWUD are given key roles in drug‐related research (eg, funding decisions, research design, and authorship). Given the scope of the current drug overdose epidemic, it is important that these large gaps in knowledge be addressed to end overdoses.
Limitations
Structures of authority are configured to benefit certain groups. 209 As articulated by historian Elizabeth Hinton, 195 who built on the work of Michelle Alexander and others, 11 the drug control policies in the United States since at least the 1960s cannot be separated from larger efforts to contain perceived threats in American society and win political support from white voters following the civil rights movement, including the changes taking place in American cities and deliberate social and political linkages made between urban Black youth and crime. The work and opinions of scholars contributed to racist beliefs about African Americans, thus perpetuating these harmful policies. Mainstream political coalitions have been built on “tough on crime” policies, which have penalized and disenfranchised urban communities of color, including PWUD. These policies have led to the expansion of the criminal justice system at all levels of government, including law enforcement, courts, prosecutors, and private for‐profit prisons, as well the US Department of Justice (including the Drug Enforcement Agency and the Office of Justice Programs). The conflation between urban policy and drug control policy led to the diversion of federal funding, so that the criminal justice system became, and remains, the de facto public health and social service agencies in many low‐income communities across the country. Scholars have also shown that various industries are reliant on prison labor to be financially viable. Without recognizing and addressing racism and the beneficiaries of the status quo, our efforts regarding prevention, treatment, recovery, and criminal justice reform will fall short.
Conclusions
The tragic toll of the opioid epidemic underscores a pressing and overdue obligation to fundamentally shift public policy from punishment to public health and to adopt more innovative and comprehensive strategies to curb the harms associated with opioid use. First and foremost, PWUD should be represented in leadership and decision making to shape programs, laws, policies, and research pertaining to drug use. For example, a national advisory council could be formed to consult on these activities. Adopting comprehensive harm reduction approaches in partnership with PWUD would help engage the most at‐risk communities and bolster ongoing public health efforts that have centered on the prevention of drug use and treatment. The outcomes that are monitored should be expanded to include the full COR. Without comprehensive legal reform, our successes will be short‐lived. This article has explained several common‐sense policies, such as decriminalizing drug possession, which could de‐escalate risk and improve health for many generations to come, as well as such factors as the underlying racism and vested interests that hinder progress. Without treating all members of society as equal citizens with equal access to resources and opportunities, and addressing the social determinants of health, the United States will continue to see preventable overdoses for the foreseeable future.
Funding/Support: JN Park and SG Sherman were supported by the Johns Hopkins University Center for AIDS Research (1P30AI094189). S Rouhani was supported by the National Institute on Drug Abuse (T32DA007292). L Beletsky was supported in part by the National Institute on Drug Abuse (R01DA039073). B Saloner was supported by the National Institute on Drug Abuse (K01‐DA042139).
Conflict of Interest Disclosures: All authors have completed the ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were reported.
References
- 1. CDC WONDER . Overdose death rates. 2018. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed September 30, 2018.
- 2. Wilson N, Kariisa M, Seth P, Ht Smith, Davis NL. Drug and opioid‐involved overdose deaths—United States, 2017–2018. Morbidity Mortality Weekly Rep. 2020;69(11):290‐297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention . The three waves of opioid overdose deaths. 2019. https://www.cdc.gov/drugoverdose/epidemic/index.html. Accessed December 19, 2019.
- 4. Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107‐111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Florence C, Luo F, Xu L, Zhou C. The economic burden of prescription opioid overdose, abuse and dependence in the United States, 2013. Med Care. 2016;54(10):901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Council of Economic Advisers . The underestimated cost of the opioid crisis. 2017. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/The%20Underestimated%20Cost%20of%20the%20Opioid%20Crisis.pdf. Accessed June 1, 2020.
- 7. Stevens JP, Wall MJ, Novack L, Marshall J, Hsu DJ, Howell MD. The critical care crisis of opioid overdoses in the United States. Ann Am Thorac Soc. 2017;14(12):1803‐1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stobbe M. Today's opioid crisis shares chilling similarities with past drug epidemics. Chicago Tribune. October 28, 2017. [Google Scholar]
- 9. Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361(6408). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alexander M. The New Jim Crow: Mass Incarceration in the Age of colorblindness. New Press, NY; 2012. ISBN: 978‐1‐59558‐103‐7. [Google Scholar]
- 12. Csete J, Kamarulzaman A, Kazatchkine M, et al. Public health and international drug policy. Lancet. 2016;387(10026):1427‐1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Beletsky L. America's favorite antidote: drug‐induced homicide in the age of the overdose crisis. Utah Law Rev. 2019:833. [Google Scholar]
- 14. US Federal Bureau of Investigation . Persons Arrested: Arrests for 2018. Washington, DC: US Department of Justice; 2018. https://ucr.fbi.gov/crime-in-the-u.s/2018/crime-in-the-u.s.-2018/topic-pages/persons-arrested. Accessed July 20, 2020. [Google Scholar]
- 15. Pichini S, Solimini R, Berretta P, Pacifici R, Busardo FP. Acute intoxications and fatalities from illicit fentanyl and analogues: an update. Therapeutic Drug Monitoring. 2018;40(1):38‐51. [DOI] [PubMed] [Google Scholar]
- 16. Beletsky L, Davis CS. Today's fentanyl crisis: Prohibition's iron law, revisited. Int J Drug Policy. 2017;46:156‐159. [DOI] [PubMed] [Google Scholar]
- 17. Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. Morbidity Mortality Weekly Rep. 2019;68(17):388‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid‐involved overdose deaths—United States, 2013–2017. Morbidity Mortality Weekly Rep. 2019;67(5152):1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. US Drug Enforcement Administration . 2018. National Drug Threat Assessment. 2018. https://www.dea.gov/sites/default/files/2018-11/DIR-032-18%202018%20NDTA%20final%20low%20resolution.pdf. Accessed June 1, 2020.
- 20. Johns Hopkins University . Coronavirus COVID‐19 global cases by the Center for Systems Science and Engineering (CSSE). https://coronavirus.jhu.edu/map.html. Accessed March 30, 2020.
- 21. Marlatt GA, Blume AW, Parks GA. Integrating harm reduction therapy and traditional substance abuse treatment. J Psychoactive Drugs. 2001;33(1):13‐21. [DOI] [PubMed] [Google Scholar]
- 22. Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Dependence. 2007;88(2‐3):188‐196. [DOI] [PubMed] [Google Scholar]
- 23. Harm Reduction Coaliation . Principles of harm reduction. 2019. https://harmreduction.org/about-us/principles-of-harm-reduction/. Accessed December 19, 2019.
- 24. McMurran M. The Psychology of Addiction . Book 10. Abingdon, UK: Taylor & Francis; 1994. ISBN 10: 0748401873. [Google Scholar]
- 25. Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363‐371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marlatt GA, Witkiewitz K. Update on harm‐reduction policy and intervention research. Annu Rev Clin Psychol. 2010;6:591‐606. [DOI] [PubMed] [Google Scholar]
- 27. Saloner B, McGinty EE, Beletsky L, et al. A public health strategy for the opioid crisis. Public Health Rep. 2018;133(Suppl. 1):24S‐34S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sussman S, Skara S, Ames SL. Substance abuse among adolescents. Substance Use & Misuse. 2008;43(12‐13):1802‐1828. [DOI] [PubMed] [Google Scholar]
- 29. Trenz RC, Scherer M, Harrell P, Zur J, Sinha A, Latimer W. Early onset of drug and polysubstance use as predictors of injection drug use among adult drug users. Addictive Behav. 2012;37(4):367‐372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Odgers CL, Caspi A, Nagin DS, et al. Is it important to prevent early exposure to drugs and alcohol among adolescents? Psychological Sci. 2008;19(10):1037‐1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cho H, Hallfors DD, Iritani BJ. Early initiation of substance use and subsequent risk factors related to suicide among urban high school students. Addictive Behav. 2007;32(8):1628‐1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Crouse JJ, Chitty KM, Iorfino F, et al. Exploring associations between early substance use and longitudinal socio‐occupational functioning in young people engaged in a mental health service. PLOS ONE. 2019;14(1):e0210877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen C‐Y, Storr CL, Anthony JC. Early‐onset drug use and risk for drug dependence problems. Addictive Behav. 2009;34(3):319‐322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Toumbourou JW, Stockwell T, Neighbors C, Marlatt G, Sturge J, Rehm J. Interventions to reduce harm associated with adolescent substance use. Lancet. 2007;369(9570):1391‐1401. [DOI] [PubMed] [Google Scholar]
- 35. Ciccarone D. Fentanyl in the US heroin supply: A rapidly changing risk environment. Int J Drug Policy. 2017;46:107‐111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cicero TJ, Ellis MS. The prescription opioid epidemic: a review of qualitative studies on the progression from initial use to abuse. Dialogues Clin Neurosci. 2017;19(3):259‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36(1):559‐574. [DOI] [PubMed] [Google Scholar]
- 38. Novak SP, Bluthenthal R, Wenger L, Chu D, Kral AH. Initiation of heroin and prescription opioid pain relievers by birth cohort. Am J Public Health. 2016;106(2):298‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241‐248. [DOI] [PubMed] [Google Scholar]
- 40. Alpert A, Powell D, Pacula RL. Supply‐side drug policy in the presence of substitutes: evidence from the introduction of abuse‐deterrent opioids. Am Econ J: Econ Policy. 2018;10(4):1‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zoorob M. Fentanyl shock: the changing geography of overdose in the United States. Int J Drug Policy. 2019;70:40‐46. [DOI] [PubMed] [Google Scholar]
- 42. Centers for Disease Control and Prevention . Drug overdose deaths in the United States, 1999–2017. 2018. https://www.cdc.gov/nchs/data/databriefs/db329-h.pdf. Accessed June 1, 2020.
- 43. Centers for Disease Control and Prevention . Rising numbers of deaths involving fentanyl and fentanyl analogs, including carfentanil, and increased usage and mixing with non‐opioids. 2018. https://emergency.cdc.gov/han/han00413.asp. Accessed June 1, 2020.
- 44. Centers for Disease Control and Prevention . Notes from the field: unintentional fentanyl overdoses among persons who thought they were snorting cocaine—Fresno, California, January 7, 2019. 2019. https://www.cdc.gov/mmwr/volumes/68/wr/mm6831a2.htm. Accessed June 1, 2020. [DOI] [PMC free article] [PubMed]
- 45. US Drug Enforcement Administration . Deadly contaminated cocaine widespread in Florida. 2018. https://www.dea.gov/sites/default/files/2018-07/BUL-039-18.pdf. Accessed June 1, 2020.
- 46. Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA. Why the FUSS (Fentanyl Urine Screen Study)? A cross‐sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduction J. 2015;12(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sutter ME, Gerona RR, Davis MT, et al. Fatal fentanyl: one pill can kill. Academic Emergency Med. 2017;24(1):106‐113. [DOI] [PubMed] [Google Scholar]
- 48. Mars SG, Ondocsin J, Ciccarone D. Sold as heroin: perceptions and use of an evolving drug in Baltimore, MD. J Psychoactive Drugs. 2018;50(2):167‐176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Park JN, Weir BW, Allen ST, Chaulk P, Sherman SG. Fentanyl‐contaminated drugs and non‐fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduction J. 2018;15(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. US Drug Enforcement Administration . DEA releases 2016 drug threat assessment: fentanyl‐related overdose deaths rising at an alarming rate. 2016. https://www.dea.gov/press-releases/2016/12/06/dea-releases-2016-drug-threat-assessment-fentanyl-related-overdose-deaths. Accessed June 1, 2020.
- 51. Hepburn K, Barker B, Nguyen P, et al. Initiation of drug dealing among a prospective cohort of street‐involved youth. Am J Drug Alcohol Abuse. 2016;42(5):507‐512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hoy C, Barker B, Regan J, et al. Elevated risk of incarceration among street‐involved youth who initiate drug dealing. Harm Reduction J. 2016;13(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fuller CM, Borrell LN, Latkin CA, et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am J Public Health. 2005;95(4):689‐695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Galea S, Annas GJ. Aspirations and strategies for public health. JAMA. 2016;315(7):655‐656. [DOI] [PubMed] [Google Scholar]
- 55. Friedman SR, Tempalski B, Brady JE, et al. Income inequality, drug‐related arrests, and the health of people who inject drugs: Reflections on seventeen years of research. Int J Drug Policy. 2016;32:11‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fite PJ, Wynn P, Lochman JE, Wells KC. The influence of neighborhood disadvantage and perceived disapproval on early substance use initiation. Addictive Behav. 2009;34(9):769‐771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Jensen M, Chassin L, Gonzales NA. Neighborhood moderation of sensation seeking effects on adolescent substance use initiation. J Youth Adolesencec. 2017;46(9):1953‐1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fuller CM, Borrell LN, Latkin CA, et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am J Public Health. 2005;95(4):689‐695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Case A, Deaton A. Mortality and morbidity in the 21(st) century. Brookings Papers Econ Activity. 2017;2017:397‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lankenau SE, Teti M, Silva K, Bloom JJ, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23(1):37‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addictive behav. 2007;32(3):562‐575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Osborne V, Serdarevic M, Crooke H, Striley C, Cottler LB. Non‐medical opioid use in youth: gender differences in risk factors and prevalence. Addictive Behav. 2017;72:114‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Miech R, Johnston L, O'Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136(5):e1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Darke S. Pathways to heroin dependence: time to re‐appraise self‐medication. Addiction. 2013;108(4):659‐667. [DOI] [PubMed] [Google Scholar]
- 65. Rigg KK, McLean K, Monnat SM, Sterner GE III, AM Verdery. Opioid misuse initiation: implications for intervention. J Addictive Diseases. 2018;37(3‐4):111‐122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Banerjee G, Edelman EJ, Barry DT, et al. Non‐medical use of prescription opioids is associated with heroin initiation among US veterans: a prospective cohort study. Addiction. 2016;111(11):2021‐2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cerdá M, Santaella J, Marshall BD, Kim JH, Martins SS. Nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J Pediatr. 2015;167(3):605‐612. e602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Palamar JJ, Shearston JA, Dawson EW, Mateu‐Gelabert P, Ompad DC. Nonmedical opioid use and heroin use in a nationally representative sample of us high school seniors. Drug Alcohol Dependence. 2016;158:132‐138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription‐opioid use and heroin use. N Engl J Med. 2016;374(2):154‐163. [DOI] [PubMed] [Google Scholar]
- 70. McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ. Does early onset of non‐medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction. 2007;102(12):1920‐1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rouhani S PJ, Morales KB, Green TC, Sherman SG. Trends in opioid initiation in 3 U.S. cities. Drug Alcohol Rev. In press. 2020. [DOI] [PubMed] [Google Scholar]
- 72. Rouhani S, Park JN, Morales KB, Green TC, Sherman SG. Harm reduction measures employed by people using opioids with suspected fentanyl exposure in Boston, Baltimore, and Providence. Harm Reduction J. 2019;16(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Cicero TJ, Ellis MS, Kasper ZA. Increased use of heroin as an initiating opioid of abuse. Addictive Behav. 2017;74:63‐66. [DOI] [PubMed] [Google Scholar]
- 74. Substance Abuse and Mental Health Services Administration . Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2017. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.pdf. Accessed July 20, 2020. [Google Scholar]
- 75. Evans CJ, Cahill CM. Neurobiology of opioid dependence in creating addiction vulnerability. F1000Research. 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Griffiths P, Gossop M, Powis B, Strang J. Transitions in patterns of heroin administration: a study of heroin chasers and heroin injectors. Addiction. 1994;89(3):301‐309. [DOI] [PubMed] [Google Scholar]
- 77. Crofts N, Louie R, Rosenthal D, Jolley D. The first hit: circumstances surrounding initiation into injecting. Addiction. 1996;91(8):1187‐1196. [DOI] [PubMed] [Google Scholar]
- 78. Kelley MS, Chitwood DD. Effects of drug treatment for heroin sniffers: a protective factor against moving to injection? Soc Sci Med. 2004;58(10):2083‐2092. [DOI] [PubMed] [Google Scholar]
- 79. Monico LB, Mitchell SG. Patient perspectives of transitioning from prescription opioids to heroin and the role of route of administration. Substance Abuse Treatment, Prevention, Policy. 2018;13(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Darke S, Hall W. Heroin overdose: research and evidence‐based intervention. J Urban Health. 2003;80(2):189‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Strang J, McCambridge J, Best D, et al. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326(7396):959‐960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Walsh K, Keyes KM, Koenen KC, Hasin D. Lifetime prevalence of gender‐based violence in US women: Associations with mood/anxiety and substance use disorders. J Psychiatr Res. 2015;62:7‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Sherman SG, Fuller CM, Shah N, Ompad DV, Vlahov D, Strathdee SA. Correlates of initiation of injection drug use among young drug users in Baltimore, Maryland: the need for early intervention. J Psychoactive Drugs. 2005;37(4):437‐443. [DOI] [PubMed] [Google Scholar]
- 84. Draus P, Carlson RG. Down on main street: drugs and the small‐town vortex. Health Place. 2009;15(1):247‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Des Jarlais DC, Diaz T, Perlis T, et al. Variability in the incidence of human immunodeficiency virus, hepatitis B virus, and hepatitis C virus infection among young injecting drug users in New York City. Am J Epidemiol. 2003;157(5):467‐471. [DOI] [PubMed] [Google Scholar]
- 86. Kral AH, Bluthenthal RN, Erringer EA, Lorvick J, Edlin BR. Risk factors among IDUs who give injections to or receive injections from other drug users. Addiction. 1999;94(5):675‐683. [DOI] [PubMed] [Google Scholar]
- 87. Thomas DL, Shih JW, Alter HJ, et al. Effect of human immunodeficiency virus on hepatitis C virus infection among injecting drug users. J Infect Dis. 1996;174(4):690‐695. [DOI] [PubMed] [Google Scholar]
- 88. Sterrett C, Brownfield J, Korn CS, Hollinger M, Henderson SO. Patterns of presentation in heroin overdose resulting in pulmonary edema. Am J Emergency Med. 2003;21(1):32‐34. [DOI] [PubMed] [Google Scholar]
- 89. Warner‐Smith M, Darke S, Day C. Morbidity associated with non‐fatal heroin overdose. Addiction. 2002;97(8):963‐967. [DOI] [PubMed] [Google Scholar]
- 90. Asbridge M, Duff C, Marsh DC, Erickson PG. Problems with the identification of “problematic” cannabis use: examining the issues of frequency, quantity, and drug use environment. Eur Addict Res. 2014;20(5):254‐267. [DOI] [PubMed] [Google Scholar]
- 91. Andreasson S. Is there an epidemiological paradox for illicit drugs? Addiction. 2011;106(2):248‐249. [DOI] [PubMed] [Google Scholar]
- 92. US Food and Drug Administration . Opioid use disorder: endpoints for demonstrating effectiveness of drugs for medication‐assisted treatment guidance for industry. 2018. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/opioid-use-disorder-endpoints-demonstrating-effectiveness-drugs-medication-assisted-treatment. Accessed June 1, 2020.
- 93. Sznitman SR, Room R. Rethinking indicators of problematic cannabis use in the era of medical cannabis legalization. Addictive Behav. 2018;77:100‐101. [DOI] [PubMed] [Google Scholar]
- 94. Harris JL, Lorvick J, Wenger L, et al. Low‐frequency heroin injection among out‐of‐treatment, street‐recruited injection drug users. J Urban Health. 2013;90(2):299‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Heimer R, Hawk K, Vermund SH. Prevalent misconceptions about opioid use disorders in the united states produce failed policy and public health responses. Clin Infect Dis. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Cooper HL. War on drugs policing and police brutality. Substance Use Misuse. 2015;50(8‐9):1188‐1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Human Rights Watch . Philippines: Duterte's first year a human rights calamity. 2017. https://www.hrw.org/news/2017/06/28/philippines-dutertes-first-year-human-rights-calamity. Accessed August 20, 2017.
- 98. Collins SE, Witkiewitz K. Abstinence violation effect. Encyclopedia of Behavioral Medicine. 2013:8‐9. [Google Scholar]
- 99. Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosci. 2016;17(9):592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta‐analysis. Psychol Bull. 2003;129(1):52‐73. [DOI] [PubMed] [Google Scholar]
- 101. Stewart SH, Pihl RO, Conrod PJ, Dongier M. Functional associations among trauma, PTSD, and substance‐related disorders. Addictive Behav. 1998;23(6):797‐812. [DOI] [PubMed] [Google Scholar]
- 102. Havassy BE, Hall SM, Wasserman DA. Social support and relapse: commonalities among alcoholics, opiate users, and cigarette smokers. Addictive Behav. 1991;16(5):235‐246. [DOI] [PubMed] [Google Scholar]
- 103. Khantzian EJ. The self‐medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am J Psychiatry. 1985;142(11):1259‐1264. [DOI] [PubMed] [Google Scholar]
- 104. Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. 2001;158(8):1184‐1190. [DOI] [PubMed] [Google Scholar]
- 105. Shah NG, Galai N, Celentano DD, Vlahov D, Strathdee SA. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988–2000. Drug Alcohol Dependence. 2006;83(2):147‐156. [DOI] [PubMed] [Google Scholar]
- 106. Martins SS, Sampson L, Cerdá M, Galea S. Worldwide prevalence and trends in unintentional drug overdose: a systematic review of the literature. Am J Public Health. 2015;105(11):e29‐e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Olfson M, Wall M, Wang S, Crystal S, Blanco C. Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug Alcohol Dependence. 2018;190:112‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Elzey MJ, Barden SM, Edwards ES. Patient characteristics and outcomes in unintentional, non‐fatal prescription opioid overdoses: a systematic review. Pain Physician. 2016;19(4):215‐228. [PubMed] [Google Scholar]
- 109. Caudarella A, Dong H, Milloy M, Kerr T, Wood E, Hayashi K. Non‐fatal overdose as a risk factor for subsequent fatal overdose among people who inject drugs. Drug Alcohol Dependence. 2016;162:51‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Darke S, Darke S, Williamson A, et al. Non‐fatal heroin overdose, treatment exposure and client characteristics: findings from the Australian Treatment Outcome Study (ATOS). Drug Alcohol Rev. 2005;24(5):425‐432. [DOI] [PubMed] [Google Scholar]
- 111. Seal KH, Kral AH, Gee L, et al. Predictors and prevention of nonfatal overdose among street‐recruited injection heroin users in the San Francisco Bay Area, 1998–1999. Am J Public Health. 2001;91(11):1842‐1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Silva K, Schrager SM, Kecojevic A, Lankenau SE. Factors associated with history of non‐fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Dependence. 2013;128(1‐2):104‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Havens JR, Oser CB, Knudsen HK, et al. Individual and network factors associated with non‐fatal overdose among rural Appalachian drug users. Drug Alcohol Dependence. 2011;115(1‐2):107‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Kinner SA, Milloy M, Wood E, Qi J, Zhang R, Kerr T. Incidence and risk factors for non‐fatal overdose among a cohort of recently incarcerated illicit drug users. Addictive Behav. 2012;37(6):691‐696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Britton PC, Wines Jr JD, Conner KR. Non‐fatal overdose in the 12 months following treatment for substance use disorders. Drug Alcohol Dependence. 2010;107(1):51‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wallace B, Kennedy MC, Kerr T, Pauly B. Factors associated with nonfatal overdose during a public health emergency. Substance Use Misuse. 2019;54(1):39‐45. [DOI] [PubMed] [Google Scholar]
- 117. Hunter K, Park JN, Allen ST, et al. Safe and unsafe spaces: non‐fatal overdose, arrest, and receptive syringe sharing among people who inject drugs in public and semi‐public spaces in Baltimore City. Inter J Drug Policy. 2018;57:25‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Kerr T, Fairbairn N, Tyndall M, et al. Predictors of non‐fatal overdose among a cohort of polysubstance‐using injection drug users. Drug Alcohol Dependence. 2007;87(1):39‐45. [DOI] [PubMed] [Google Scholar]
- 119. Ickowicz S, Wood E, Dong H, et al. Association between public injecting and drug‐related harm among HIV‐positive people who use injection drugs in a Canadian setting: a longitudinal analysis. Drug Alcohol Dependence. 2017;180:33‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Rhodes T, Watts L, Davies S, et al. Risk, shame and the public injector: a qualitative study of drug injecting in South Wales. Soc Sci Med. 2007;65(3):572‐585. [DOI] [PubMed] [Google Scholar]
- 121. McLean K. “There's nothing here”: deindustrialization as risk environment for overdose. Int J Drug Policy. 2016;29:19‐26. [DOI] [PubMed] [Google Scholar]
- 122. Muennig PA, Reynolds M, Fink DS, Zafari Z, Geronimus AT. America's declining well‐being, health, and life expectancy: not just a white problem. Am J Public Health. 2018;108(12):1626‐1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Pear VA, Ponicki WR, Gaidus A, et al. Urban‐rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Dependence. 2019;195:66‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Jenkins LM, Banta‐Green CJ, Maynard C, et al. Risk factors for nonfatal overdose at Seattle‐area syringe exchanges. J Urban Health. 2011;88(1):118‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Burris S, Blankenship KM, Donoghoe M, et al. Addressing the “risk environment” for injection drug users: the mysterious case of the missing cop. Milbank Q. 2004;82(1):125‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Suzuki J, El‐Haddad S. A review: fentanyl and non‐pharmaceutical fentanyls. Drug Alcohol Dependence. 2017;171:107‐116. [DOI] [PubMed] [Google Scholar]
- 127. King NB, Fraser V, Boikos C, Richardson R, Harper S. Determinants of increased opioid‐related mortality in the United States and Canada, 1990–2013: a systematic review. American J Public Health. 2014;104(8):e32‐e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98(6):739‐747. [DOI] [PubMed] [Google Scholar]
- 129. Binswanger IA, Blatchford PJ, Lindsay RG, Stern MF. Risk factors for all‐cause, overdose and early deaths after release from prison in Washington state. Drug Alcohol Dependence. 2011;117(1):1‐6. [DOI] [PubMed] [Google Scholar]
- 130. Rowell‐Cunsolo TL, Sampong SA, Befus M, Mukherjee DV, Larson EL. Predictors of illicit drug use among prisoners. Substance Use Misuse. 2016;51(2):261‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Dependence. 2011;115(3):221‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Bohnert AS, Nandi A, Tracy M, et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Dependence. 2011;113(1):62‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA. 2018;319(17):1819‐1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Schneider KE, Park JN, Allen ST, Weir BW, Sherman SG. Patterns of polysubstance use and overdose among people who inject drugs in Baltimore, Maryland: a latent class analysis. Drug Alcohol Dependence. 2019;201:71‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Park JN, Sherman SG, Rouhani S, et al. Willingness to use safe consumption spaces among opioid users at high risk of fentanyl overdose in Baltimore, Providence, and Boston. J Urban Health. 2019:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Mattson CL, O'Donnell J, Kariisa M, Seth P, Scholl L, Gladden RM. Opportunities to prevent overdose deaths involving prescription and illicit opioids, 11 states, July 2016–June 2017. Morbidity Mortality Weekly Rep. 2018;67(34):945‐951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Wojcicki JM. Dying alone: the sad irrelevance of naloxone in the context of solitary opiate use. Addiction. 2019;114(3):574‐575. [DOI] [PubMed] [Google Scholar]
- 138. Wilkinson RG, Pickett KE. The problems of relative deprivation: why some societies do better than others. Soc Sci Med. 2007;65(9):1965‐1978. [DOI] [PubMed] [Google Scholar]
- 139. Gelman A, Auerbach J. Age‐aggregation bias in mortality trends. Proc Natl Acad Sci USA. 2016;113(7):E816‐817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Hedegaard H, Minino AM, Warner M. Urban‐rural differences in drug overdose death rates, by sex, age, and type of drugs involved, 2017. Natl Center Health Stat Data Brief. 2019(345):1‐8. [PubMed] [Google Scholar]
- 141. Shiels MS, Freedman ND, Thomas D, de Gonzalez AB. Trends in US drug overdose deaths in non‐Hispanic black, Hispanic, and non‐Hispanic white persons, 2000–2015. Ann Intern Med. 2018;168(6):453‐455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Monnat SM. The contributions of socioeconomic and opioid supply factors to US drug mortality rates: urban‐rural and within‐rural differences. J Rural Stud. 2019;68:319‐335. [Google Scholar]
- 143. Monnat SM. Factors associated with county‐level differences in u.s. drug‐related mortality rates. Am J Prev Med. 2018;54(5):611‐619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Marshall Z, Dechman M, Minichiello A, Alcock L, Harris GE. Peering into the literature: a systematic review of the roles of people who inject drugs in harm reduction initiatives. Drug Alcohol Dependence. 2015;151:1‐14. [DOI] [PubMed] [Google Scholar]
- 145. Des Jarlais DC, Friedman SR, Ward TP. Harm reduction: a public health response to the AIDS epidemic among injecting drug users. Annu Rev Public Health. 1993;14:413‐450. [DOI] [PubMed] [Google Scholar]
- 146. Erickson PG, Riley DM, Cheung YW, O'Hare PA. Harm reduction: A new direction for drug policies and programs. Toronto, ONT: University of Toronto Press; 1997. ISBN: 9780802007568. [Google Scholar]
- 147. Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons—United States, 2014. Morbidity Mortality Weekly Rep. 2015;64(23):631‐635. [PMC free article] [PubMed] [Google Scholar]
- 148. Latkin C, Friedman S. Drug use research: drug users as subjects or agents of change. Substance Use Misuse. 2012;47(5):598‐599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Bassuk EL, Hanson J, Greene RN, Richard M, Laudet A. Peer‐delivered recovery support services for addictions in the United States: a systematic review. J Subst Abuse Treatment. 2016;63:1‐9. [DOI] [PubMed] [Google Scholar]
- 150. US Department of Health and Human Services (HHS) , Office of the Surgeon General. Facing addiction in America: the Surgeon General's report on alcohol, drugs, and health. Washington, DC: US HHS; 2016. https://store.samhsa.gov/product/Facing-Addiction-in-America-The-Surgeon-General-s-Report-on-Alcohol-Drugs-and-Health-Full-Report/SMA16-4991. Accessed July 20, 2020. [PubMed] [Google Scholar]
- 151. Kennedy‐Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health–oriented policies. Psychiatric serv. 2017;68(5):462‐469. [DOI] [PubMed] [Google Scholar]
- 152. McGinty EE, Stone EM, Kennedy‐Hendricks A, Barry CL. Stigmatizing language in news media coverage of the opioid epidemic: implications for public health. Prev Med. 2019;124:110‐114. [DOI] [PubMed] [Google Scholar]
- 153. Netherland J, Hansen HB. The war on drugs that wasn't: wasted whiteness,“dirty doctors,” and race in media coverage of prescription opioid misuse. Cult, Med, Psychiatry. 2016;40(4):664‐686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. National Academies of Sciences E, and Medicine . Medications for Opioid Use Disorder Save Lives. Washington, DC: National Academies Press; 2019. https://www.nap.edu/catalog/25310/medications-for-opioid-use-disorder-save-lives. Accessed July 20, 2020. [PubMed] [Google Scholar]
- 155. Martins SS, Ponicki W, Smith N, et al. Prescription drug monitoring programs operational characteristics and fatal heroin poisoning. Int J Drug Policy. 2019;74:174‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Centers for Disease Control and Prevention . Evidence‐Based Strategies for Preventing Opioid Overdose: What's Working in the United States. Washington, DC: USHHS, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2018. https://npin.cdc.gov/publication/evidence-based-strategies-preventing-opioid-overdose-what%E2%80%99s-working-united-states. Accessed July 20, 2020. [Google Scholar]
- 157. Banta‐Green CJ, Beletsky L, Schoeppe JA, Coffin PO, Kuszler PC. Police officers’ and paramedics’ experiences with overdose and their knowledge and opinions of Washington State's drug overdose—naloxone–Good Samaritan law. J Urban Health. 2013;90(6):1102‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Sherman S. Overdose prevention sites and heroin assisted treatment. BMJ. 2019;366:l5437. [DOI] [PubMed] [Google Scholar]
- 159. Potier C, Laprévote V, Dubois‐Arber F, Cottencin O, Rolland B. Supervised injection services: what has been demonstrated? A systematic literature review. Drug Alcohol Dependence. 2014;145:48‐68. [DOI] [PubMed] [Google Scholar]
- 160. Kennedy MC, Kerr T. Overdose prevention in the United States: a call for supervised injection sites. Am J Public Health. 2017;107(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of North America's first medically supervised safer injecting facility: a retrospective population‐based study. Lancet. 2011;377(9775):1429‐1437. [DOI] [PubMed] [Google Scholar]
- 162. Freeman K, Jones CG, Weatherburn DJ, Rutter S, Spooner CJ, Donnelly N. The impact of the Sydney Medically Supervised Injecting Centre (MSIC) on crime. Drug Alcohol Rev. 2005;24(2):173‐184. [DOI] [PubMed] [Google Scholar]
- 163. Kennedy MC, Hayashi K, Milloy MJ, Wood E, Kerr T. Supervised injection facility use and all‐cause mortality among people who inject drugs in Vancouver, Canada: a cohort study. PLOS Med. 2019;16(11):e1002964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Salmon AM, van Beek I, Amin J, Kaldor J, Maher L. The impact of a supervised injecting facility on ambulance call‐outs in Sydney, Australia. Addiction. 2010;105(4):676‐683. [DOI] [PubMed] [Google Scholar]
- 165. Irwin A, Jozaghi E, Weir BW, Allen ST, Lindsay A, Sherman SG. Mitigating the heroin crisis in Baltimore, MD, USA: a cost‐benefit analysis of a hypothetical supervised injection facility. Harm Reduction J. 2017;14(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Enns EA, Zaric GS, Strike CJ, Jairam JA, Kolla G, Bayoumi AM. Potential cost‐effectiveness of supervised injection facilities in Toronto and Ottawa, Canada. Addiction. 2016;111(3):475‐489. [DOI] [PubMed] [Google Scholar]
- 167. Bayoumi AM, Zaric GS. The cost‐effectiveness of Vancouver's supervised injection facility. CMAJ. 2008;179(11):1143‐1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Kral AH, Davidson PJ. Addressing the nation's opioid epidemic: lessons from an unsanctioned supervised injection site in the U.S. Am J Prev Med. 2017;53(6):919‐922. [DOI] [PubMed] [Google Scholar]
- 169. Harper L, Powell J, Pijl EM. An overview of forensic drug testing methods and their suitability for harm reduction point‐of‐care services. Harm Reduction J. 2017;14(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Barratt M, Kowalski M, Maier L, Ritter A. Global review of drug checking services operating in 2017 (Drug Policy Modelling Program, Bulletin No. 24). Sydney, Australia: National Drug and Alcohol Research Centre; ndarc_med-unsw_ed_au/resource/bulletin-no-24-global-review-drug-checking-services-operating-2017. 2018. Accessed June 1, 2020. [Google Scholar]
- 171. Palamar JJ, Salomone A, Barratt MJ. Drug checking to detect fentanyl and new psychoactive substances. Curr Opinion Psychiatry. March 13, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Green TC, Park JN, Gilbert M, et al. An assessment of the limits of detection, sensitivity and specificity of three devices for public health‐based drug checking of fentanyl in street‐acquired samples. Int J Drug Policy. 2020;77:102661. [DOI] [PubMed] [Google Scholar]
- 173. Sherman SG, Morales KB, Park JN, McKenzie M, Marshall BDL, Green TC. Acceptability of implementing community‐based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. Int J Drug Policy. 2019;68:46‐53. [DOI] [PubMed] [Google Scholar]
- 174. Krieger MS, Goedel WC, Buxton JA, et al. Use of rapid fentanyl test strips among young adults who use drugs. Int J Drug Policy. 2018;61:52‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: Findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122‐128. [DOI] [PubMed] [Google Scholar]
- 176. Krawczyk N, Mojtabai R, Stuart EA, et al. Opioid agonist treatment and fatal overdose risk in a state‐wide US population receiving opioid use disorder services. Addiction. February 24, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Pitt AL, Humphreys K, Brandeau ML. Modeling health benefits and harms of public policy responses to the US opioid epidemic. Am J Public Health. 2018;108(10):1394‐1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. National Institute on Drug Abuse . Medications to treat opioid use disorder. 2018. https://www.drugabuse.gov/publications/research-reports/medications-to-treat-opioid-addiction/efficacy-medications-opioid-use-disorder. Accessed June 1, 2020.
- 179. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Systematic Rev. 2014(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Carter J, Zevin B, Lum PJ. Low barrier buprenorphine treatment for persons experiencing homelessness and injecting heroin in San Francisco. Addiction Sci Clin Pract. 2019;14(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Wakeman SE. Comparing medications to treat opioid use disorder. Harvard Health Blog January 3, 2018. [Google Scholar]
- 182. McCarty D, Priest KC, Korthuis PT. Treatment and prevention of opioid use disorder: challenges and opportunities. Annu Rev Public Health. 2018;39:525‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Saloner B, Daubresse M, Alexander GC. Patterns of buprenorphine‐naloxone treatment for opioid use disorder in a multi‐state population. Med Care. 2017;55(7):669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Krawczyk N, Picher CE, Feder KA, Saloner B. Only one in twenty justice‐referred adults in specialty treatment for opioid use receive methadone or buprenorphine. Health Aff. 2017;36(12):2046‐2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Jones CM, McCance‐Katz EF. Co‐occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Dependence. 2019;197:78‐82. [DOI] [PubMed] [Google Scholar]
- 186. Olsen Y, Sharfstein JM. Confronting the stigma of opioid use disorder—and its treatment. JAMA. 2014;311(14):1393‐1394. [DOI] [PubMed] [Google Scholar]
- 187. McGinty E, Pescosolido B, Kennedy‐Hendricks A, Barry CL. Communication strategies to counter stigma and improve mental illness and substance use disorder policy. Psychiatr Serv. 2018;69(2):136‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Samet JH, Botticelli M, Bharel M. Methadone in primary care—one small step for congress, one giant leap for addiction treatment. N Engl J Med. 2018;379(1):7‐8. [DOI] [PubMed] [Google Scholar]
- 189. Dick AW, Pacula RL, Gordon AJ, et al. Growth in buprenorphine waivers for physicians increased potential access to opioid agonist treatment, 2002–11. Health Aff (Millwood). 2015;34(6):1028‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Beetham T, Saloner B, Wakeman SE, Gaye M, Barnett ML. Access to office‐based buprenorphine treatment in areas with high rates of opioid‐related mortality: an audit study. Ann Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Kennedy‐Hendricks A, Busch SH, McGinty EE, et al. Primary care physicians’ perspectives on the prescription opioid epidemic. Drug Alcohol Dependence. 2016;165:61‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Maclean JC, Saloner B. The effect of public insurance expansions on substance use disorder treatment: evidence from the Affordable Care Act. J Policy Analysis Manage. 2019;38(2):366‐393. [PMC free article] [PubMed] [Google Scholar]
- 193. Courtwright DT. A century of American narcotic policy. In: Treating Drug Problems: Volume 2: Commissioned Papers on Historical, Institutional, and Economic Contexts of Drug Treatment.: Washington, DC: Institute of Medicine; 1992. [PubMed] [Google Scholar]
- 194. Piketty T, Saez E, Zucman G. Distributional national accounts: methods and estimates for the United States. Q J Econ. 2018;133(2):553‐609. [Google Scholar]
- 195. Hinton E. From the war on poverty to the war on crime: The making of mass incarceration in America. Cambridge, MA: Harvard University Press; 2016. ISBN: 9780674737235. [Google Scholar]
- 196. Center of Addiction and Substance Abuse . Behind Bars II: Substance Abuse and America's Prison Population. New York, NY: Center of Addiction and Substance Abuse; 2010. https://www.centeronaddiction.org/addiction-research/reports/behind-bars-ii-substance-abuse-and-america%E2%80%99s-prison-population. Accessed July 20, 2020. [Google Scholar]
- 197. National Alliance on Mental Illness . Jailing people with mental illness. https://www.nami.org/learn-more/public-policy/jailing-people-with-mental-illness. Accessed December 20, 2019.
- 198. Dumont DM, Brockmann B, Dickman S, Alexander N, Rich JD. Public health and the epidemic of incarceration. Annu Rev Public Health. 2012;33:325‐339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Brinkley‐Rubinstein L, Zaller N, Martino S, et al. Criminal justice continuum for opioid users at risk of overdose. Addictive Behav. 2018;86:104‐110. [DOI] [PubMed] [Google Scholar]
- 200. Green TC, Clarke J, Brinkley‐Rubinstein L, et al. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 2018;75(4):405‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Brief on Behalf of the Massachusetts Medical Society et al. as Amici Curiae, Eldred v Massachusetts, 101 N.E.3d 911 (No. SJC‐12279) (2017), available at http://www.massmed.org/advocacy/eldred-amicus-brief-final/.
- 202. Cramer M. Legislators seek to bar judges from sending drug users who relapse to jail, Boston Globe (Mar. 17, 2019), https://www.bostonglobe.com/metro/2019/03/17/legislators-seek-bar-judges-from-sending-drug-users-who-relapse-jail/qNWRWdvmYOL4ETfWBho0VM/story.html
- 203. U.S. Department of Justice National Institute of Corrections, LEAD: Law Enforcement Assisted Diversion, NIC; (2015), https://nicic.gov/lead-law-enforcement-assisted-diversion [Google Scholar]
- 204. European Monitoring Centre for Drugs and Drug Addiction. Portugal, Country Drug Report 2017 . Luxemborg: Publications Office of the European Union; 2017. [Google Scholar]
- 205. Greenwald G. Drug Decriminalization in Portugal: Lessons for Creating Fair and Successful Drug Policies. Cato Institute Whitepaper Series; 2009. https://www.cato.org/publications/white-paper/drug-decriminalization-portugal-lessons-creating-fair-successful-drug-policies. Accessed July 20, 2020. [Google Scholar]
- 206. Kilmer B, Taylor J, Caulkins JP, etal. Considering Heroin‐Assisted Treatment and Supervised Drug Consumption Sites in the United States. Santa Monica, CA: RAND; 2018. https://www.rand.org/pubs/research_reports/RR2693.html. Accessed July 20, 2020. [Google Scholar]
- 207. Ferri M, Davoli M, Perucci CA. Heroin maintenance for chronic heroin‐dependent individuals. Cochrane Database Systematic Rev. 2010(8). [DOI] [PubMed] [Google Scholar]
- 208. Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. 2012;107(1):39‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Blau PM, Scott WR. Formal Organizations: A Comparative Approach. Stanford, CA: Stanford University Press; 2003. ISBN: 9780804748902. [Google Scholar]


