Over the past 3 months, the coronavirus disease 2019 (COVID-19) has rapidly spread from China to Europe and the rest of the world. The pandemic severely hit the central part of Italy, with almost 6000 confirmed cases out of 1.5 million inhabitants in the Marche region as of April 24, 2020.1
Among the common, highly heterogeneous and deadly cardiovascular complications of COVID-19,2 arrhythmias represent a frequent occurrence.3 Furthermore, even during the pandemic, arrhythmias, or device-related issues in patients with heart disease and without COVID-19 are continuing to require evaluation by electrophysiologists. Therefore, electrophysiology laboratories have continued providing highly needed services while adapting to this unprecedented health crisis.3,4 Recently, consensus recommendations for the management of electrophysiology procedures were provided, mandating the cancellation or postponement of elective cases.4 However, little is known about the real-world impact of the COVID-19 pandemic on high-volume electrophysiology laboratories.
We conducted a single-center, retrospective, observational study. We enrolled patients undergoing electrophysiology procedures at the University Hospital “Ospedali Riuniti” in Ancona, Italy, a tertiary-level referral center. Data supporting the findings of this study are available from the corresponding author upon reasonable request. We included all consecutive patients who underwent electrophysiology procedures since March 9, 2020, when novel health care measures were taken in the cardiology department due to the COVID-19 outbreak, until April 26, 2020. These patients were compared with those undergoing electrophysiology procedures in the preceding 6 months (September 9, 2019, to March 8, 2020). During the COVID emergency, only nondeferrable procedures were performed, giving priority to electrical storms (ES), refractory device infections requiring lead/device extraction, pacemaker or defibrillator implantations, and generator changes.4 Each patient was meticulously evaluated for symptoms of COVID-19,4 and polymerase chain reaction tests for the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) on throat swabs were always obtained before proceeding to the electrophysiology laboratory. To reduce the risk of infection’s transmission, the number of healthcare workers involved in each case was reduced to the bare minimum, and every person routinely donned personal protective equipment.4 Patients not undergoing endotracheal intubation donned face masks. In case of procedures on patients with suspected or confirmed COVID-19, operators also put on N95 masks, protective eyewear, and gowns.
The χ2, Fisher exact, or Wilcoxon rank-sum tests were used to analyze data as appropriate, with the software RStudio. The study was performed according to institutional standards, national legal requirements, and the Declaration of Helsinki. Informed consent was obtained by all patients.
During the COVID-19 emergency, 79 electrophysiology procedures were performed (Table). The most common interventions included generator changes, pacemaker implantations (2 with leadless devices), defibrillator implantations, ES catheter ablations (CA, 3 with epiendocardial approach), and device extractions. We did not have results of polymerase chain reaction testing before the electrophysiology procedure in just one patient urgently requiring a pacemaker, who was later found to be negative. In all other 78 cases, results of polymerase chain reaction testing for SARS-Cov-2 were available and excluded infection. In the 6 months before the lockdown, 592 electrophysiology procedures were performed, most commonly pacemaker implantations (three with leadless devices), generator changes, and CAs for atrial fibrillation (Table).
Table.
Procedural Volumes During the COVID Institutional Lockdown as Compared to the Pre-COVID Period
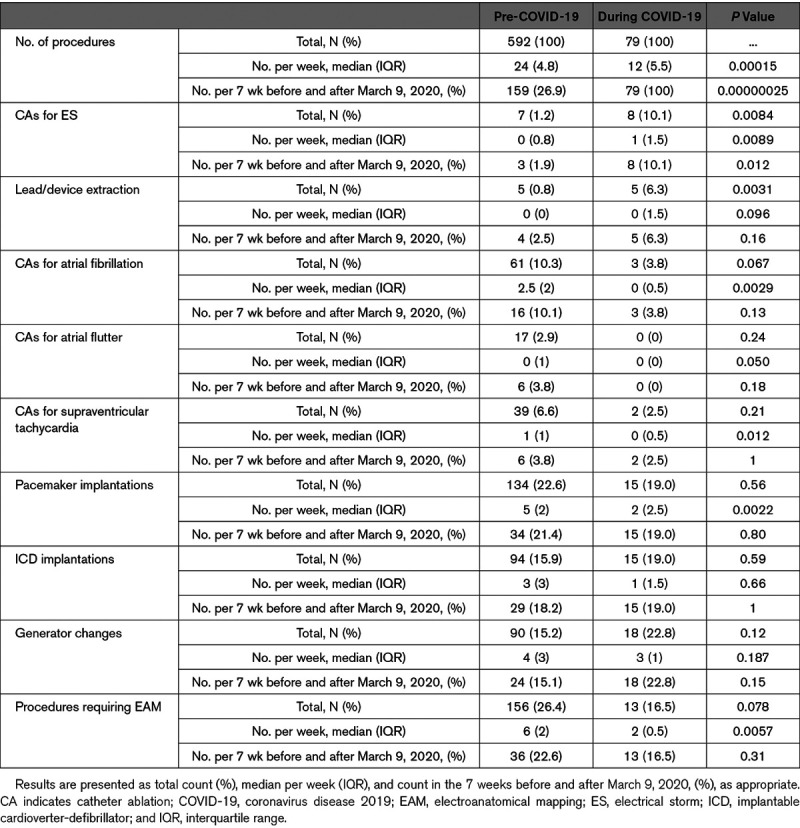
Overall, there was a decrease in absolute procedural volumes in the COVID-19 period. This finding extended to every type of procedure, except generator changes and extractions, whose weekly absolute numbers remained stable, and CAs for ES, whose figures per week increased (Table).
The relative prevalences of some procedural subsets changed with the COVID-19 outbreak: ES CAs and device/lead extractions were relatively more common than before, whereas the relative frequency of other interventions showed nonsignificant changes (Table).
Remarkably, no healthcare personnel developed COVID-19 as a result of working in the electrophysiology laboratory, as assessed by antibody testing in the week of April 20.
Our data clearly illustrate that the COVID-19 emergency set an unprecedented scenario which had a major impact on a tertiary-level electrophysiology laboratory. Our findings suggest 3 key messages: (1) overall, there was a drastic reduction in the numbers of electrophysiology procedures, due to postponement of nonurgent interventions; (2) an electrophysiology laboratory model extensively adopting personal protective equipment and other preventive measures proved safe for healthcare personnel; and (3) weekly rates of ES CAs significantly increased. This latter observation does not seem a direct consequence of COVID-19 (no patients had a personal history of the infection) but could be potentially attributed to patients’ reluctance to come to the hospital, to the lower quality of care of patients with heart disease indirectly brought by the pandemic, or to other unmeasured factors.5
The major limitation of our study lies in the lack of information on whether the COVID-19 pandemic influenced patients’ outcomes, due to the shortness of follow-up.
Our data reinforce the concept that COVID-19 can have major direct as well as indirect effects on the practice of electrophysiology, which need to be further elucidated to better understand the complex interplay between the pandemic and arrhythmias3–5.
Sources of Funding
None.
Disclosures
None.
Nonstandard Abbreviations and Acronyms
- CA
- catheter ablation
- COVID-19
- coronavirus disease 2019
- ES
- electrical storm
- SARS-
- severe acute respiratory syndrome CoV-2 coronavirus-2
For Sources of Funding and Disclosures, see page 1041.
References
- 1.Istituto Superiore di Sanità. Infographic on SARS-CoV-2. https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_24aprile%20ENG.pdf.
- 2.Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani L, et al. COVID-19 and cardiovascular disease. Circulation 20201411648–1655doi: 10.1161/CIRCULATIONAHA.120.046941 [DOI] [PubMed] [Google Scholar]
- 3.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, Brown TS, Nigoghossian C, Zidar DA, Haythe J, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020752352–2371doi: 10.1016/j.jacc.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, Cheung J, Patel P, Sotomonte J, Lampert R, et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation 2020141e823–e831doi: 10.1161/CIRCULATIONAHA.120.047063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guerra F, Bonelli P, Flori M, Cipolletta L, Carbucicchio C, Izquierdo M, Kozluk E, Shivkumar K, Vaseghi M, Patani F, et al. Temporal trends and temperature-related incidence of electrical storm: the TEMPEST Study (Temperature-Related Incidence of Electrical Storm). Circ Arrhythm Electrophysiol. 2017;10:e004634. doi: 10.1161/CIRCEP.116.004634. doi: 10.1161/CIRCEP.116.004634. [DOI] [PubMed] [Google Scholar]


