ABSTRACT
Vaccination is an indisputable intervention that has tremendously mitigated the global burden of vaccine-preventable diseases (VPDs). The number of armed conflicts globally seems to be at an all-time high, with devastating effects on vaccination coverage. This paper will examine how armed conflicts affect childhood vaccination and lead to the reemergence and spread of VPDs. Unarguably, socioeconomic factors, population demographics, the apparent long vaccination timetable, multiple vaccine doses, lack of trust in vaccination processes and the rumor of the adverse effects of some vaccines unnerve some parents and create a puzzle. By bringing under the global floodlight, the impact of armed conflicts which contextually affect vaccination coverage, this article will help strengthen the advocacy for vaccination, and call for the fortification of existing treaties on the rule of engagement during conflicts. In order to eliminate or eradicate VPDs, strategies to reach children that are left behind during conflicts is paramount.
KEYWORDS: Vaccination, benefits, determinants, conflicts, Global Alliance for Vaccination and Immunization (GAVI), immunization, vaccine prventable diseases (VPDs), leave no child behind
1. Introduction
Vaccination is one of the easiest and cost-effective methods of mitigating childhood morbidity and mortality. Irrespective of circumstances, it remains a basic necessity in the provision of universal health services. Prevention is often regarded to be better than cure. The eradication of smallpox in the 80s remains a shred of incredible evidence to show that vaccination is an important disease prevention and control tool. Also, the elimination of wild poliovirus (WPV) transmission and endemic measles across many countries and regions in the world are remarkable testaments.1 However, according to the United Nations International Children Emergency Fund (UNICEF), 30% of deaths among children less than 5 years are caused by VPDs with over 1.5 million deaths recorded in children annually from diseases that can be prevented by vaccination.2 Millions of people die when life-saving vaccines and medicines do not reach those who need them most because they or the countries they live in are too poor to provide them vaccines.3 Increased investment in vaccination services in low-and-middle-income countries alone could prevent 36 million deaths and 24 million cases of impoverishment that result from medical costs.2 Armed conflict is one of the challenging emergencies that disrupt societal function and hampers access to health care. It leads to the destruction of health-care facilities, disruption of vaccine cold chain management, crippling of the healthcare system, killing of health-care personnel, displacement of people internally, into the bushes and across borders, obstruction of humanitarian access, poor hygiene and nutritional status, low immunity, and high susceptibility to infections.4 The administration of vaccines during armed conflicts is very challenging to navigate. Usually, during armed battles, more priority is paid on the treatment and management of casualties involved with less attention on preventive care. Children that are affected by conflict suffer disproportionately from VPD outbreaks. For instance, out of about 3400 cases of polio reported globally between 2010 and 2016, 70% were in conflict-affected countries.5 These include countries in Africa, the Middle East and some parts of Europe where widespread armed conflict has led to the reemergence and spread of poliovirus.6-8 More than two-thirds of children who have not received essential vaccines live in countries that are either partially or entirely affected by conflict.9 In 2015, the six countries (the Central African Republic, Equatorial Guinea, Somalia, South Sudan, Syrian Arab Republic, and Ukraine) that reported a shallow DPT vaccine coverage were all experiencing conflicts or other forms of humanitarian emergencies.1,7
2. Background
Since the establishment of the World Health Organization’s Expanded Program on Immunization (WHO-EPI) in 1974 and the Global Alliance for Vaccination and Immunization at the end of 1999, tremendous successes have been recorded in the reduction of lethal childhood infections.10,11 In some countries, diseases like diphtheria, measles, mumps, pertussis, polio, rubella, smallpox, and tetanus have witnessed an incredible reduction in the number of deaths to about 100% due to vaccines, likewise, hepatitis A and B, Haemophilus influenza, and varicella have experienced a decline in the number of cases, hospitalizations, and deaths by more than 80% except for pneumococcus.12 Another milestone that has been achieved using vaccines is the eradication of smallpox.1,13 Vaccines are not only useful in averting morbidity and mortality but are of economic benefit as well. Following an economic evaluation report on routine childhood immunization programs in the United States, vaccination was established to be one of the most cost-effective strategies that prevents and averts millions of childhood illnesses and deaths yearly.14
According to the WHO, at least 10 million deaths were averted between 2010 and 2015 through vaccination, and many more protected from the sufferings and disabilities associated with VPDs such as pneumonia, diarrhea, whooping cough, measles, and polio.15 This has made the WHO to regard vaccination as one of its most successful public health programs. As of 1974 (when the EPI was established), only 5% of children globally were vaccinated. However, today, it is estimated that about 86% of children worldwide are either partially or fully vaccinated against the six killer diseases with some countries having more than 95% coverage.15 The 2017 GAVI report suggests that about 6 million children were administered vaccines in 2016, and the target is to immunize 300 million more before the year 2020 using the Global Vaccine Action Plan (GVAP).16 For a communicable disease to be effectively eliminated from a community or country, vaccines against that disease must be administered appropriately to a significant number of people over a considerable duration to achieve protection above the herd immunity threshold for that vaccine.17 Even though vaccination has some medical exceptions (like those who are immunosuppressed), a number of countries, however, have made certain vaccines compulsory to improve compliance. This is because children who are not vaccinated also pose a severe risk to those around them. Some governments focus on educating their citizens on the benefits of vaccination; others give financial incentives to improve vaccine coverage.18 Before the creation of GAVI, there was widespread inequality in vaccination coverage. Children in some low-and-middle countries were denied access to vaccination simply because of cost and pharmaceutical companies did not have the interest to invest and supply vaccines to resource-poor countries due to the low incentives in vaccines.19 The birth of GAVI has helped in mitigating inequities that existed in vaccination by bringing both new and underused vaccines closer to the poor. For about two decades now, GAVI has successfully bridged this gap by bringing on board actors in both the public and private sector (public–private partnership) including, governments, multinational organizations, foundations, and non-governmental organizations.19
Childhood vaccination is the gateway to the provision of comprehensive health care to children irrespective of race, socioeconomic status, religion, culture, and geographical location. However, vaccination coverage in some parts of the world is yet to reach an optimal level. According to the WHO,20 by 2017, the global coverage of some vaccine-preventable childhood diseases was as follows: Haemophilus influenza type b (Hib) (72%), hepatitis B (43%), measles (85% received a single dose and 67% double dose), pneumococcal diseases (44%), polio (85%), childhood diarrhea resulting from rotaviruses (28%), rubella (52%) tetanus (85%), and yellow fever (43%) while mumps and meningitis-A vaccines were yet to be included in the national immunization program in many countries. The WHO report further estimated that about 19.9 million infants worldwide were not reached with routine immunization services out of which 60% of them were living in 10 countries including, Afghanistan, Angola, the Democratic Republic of the Congo, Ethiopia, India, Indonesia, Iraq, Nigeria, Pakistan, and South Africa.20 One thing that is common to these countries is conflict, social and political instability. Mathew et al.21 identified and classified the barriers to vaccination under three themes: knowledge barrier and beliefs regarding vaccination, attitudinal barriers, and logistic barriers to the utilization of vaccination services including, lack of access to health care, vaccination hesitancy and insufficient information all of which are directly or indirectly affected by armed conflicts.
3. Purpose
The aim of this paper is to examine how armed conflicts affect vaccination coverage leading to infectious disease outbreaks, and the reemergence and spread of VPDs.
4. Method
This literature review is based on extensive reading of online published papers from the following bibliographic databases: PubMed, Google Scholar, MEDLINE, and the University of Gothenburg library. Only articles published in English between 1974 (when the expanded program on immunization (EPI) was established) to 2019 were considered. Both MeSH and regular keywords were used in the search. Search terms included ‘Conflicts,’ ‘war,’ ‘determinants,’ ‘immunization,’ ‘vaccination,’ ‘childhood.’ These terms were then combined interchangeably using “and.” Abstracts of retrieved articles were read to select papers relevant to the topic. The scale for the assessment of narrative review articles (SANRA)22 was used to guide our selection of quality articles. Following the combination of search terms, 50 papers merited selection; ‘Childhood immunization’ (10 articles), ‘childhood vaccination’ (8 articles), ‘immunization and conflict’ (9 articles), ‘Immunization determinants’ (4 articles), ‘vaccination and conflict’ (7 articles), ‘immunization and war’ (4 articles), ‘vaccination and war’ (3 articles) and ‘determinants of vaccination’ (5 articles). Thirty-three more articles were then gotten by “snowballing” the reference list of selected articles. In total, 83 articles were reviewed in writing this paper. We also followed the SANRA guidelines in writing this paper to address, the topic, and its relevance while focusing on the aims.
5. Discussion
Vaccination and immunization have often been used interchangeably even though both are aimed at improving health and prolonging life, especially in children. The former is the administration of vaccines while the latter is the effects of these vaccines on the immune system. Understanding these two terminologies is essential.
5.1. Vaccination and immunization
Vaccination is the administration of a biological preparation called vaccine to an individual to build his or her immunity against a disease. The purpose is for the individual to develop protection (body defense) against infections caused by the organisms the vaccines are administered against.23 Vaccination is credited to Edward Jenner, who demonstrated that inoculating an individual with material from cowpox (vaccinia) would lead to protection (immunization) against smallpox.24 Immunization is, therefore, the process of acquiring immunity against disease following vaccination. Vaccines usually contain agents that resemble the microorganism it is being administered against.25 These vaccines could be made either from the entire disease-causing organism in its sub-optimal or weakened form (attenuated) or from some of its components, including toxins, surface proteins, and nucleic acids. It could also be from a genetically modified form of the organism that cannot cause the disease. When administered to humans, the vaccine stimulates the immune system of the individual to recognize the agent as foreign, destroy it, and generate antibodies against it. The immune system then keeps a memory of the organism so that, upon subsequent exposure to that type of infectious agent, it is recognized and destroyed. Vaccines have excipients or media (additives, preservatives or adjuvants) added to it to maintain the potency of the vaccine over its shelf-life.25 Preservatives like thimerosal help to prevent contamination while adjuvants like aluminum salts facilitate the stimulation of a stronger immune response and stabilizers (sugars or gelatin), keep the vaccine potent during transportation and storage.26 Some of these excipients are believed to be responsible for the side effects that result from vaccination.26 The routes of administration of vaccines vary (oral or parenteral) and these drugs could come as a single or combined doses and can be administered either once or multiple times.
5.2. The benefits of vaccination
Vaccination remains one of the easiest and cost-effective methods of reducing childhood morbidity and mortality.1 Millions (2–3 million) of lives are saved yearly from VPDs such as diphtheria, hepatitis B, measles, mumps, pertussis (whooping cough), pneumonia, polio, rotavirus diarrhea, rubella, and tetanus.27 The eradication of smallpox, the near eradication of endemic poliomyelitis and the elimination of both measles and rubella from the WHO Region of the Americas in 2002 are some of the glaring benefits of vaccination.28,29 According to Akil and Ahmad30 in the 80s, polio was paralyzing at least 1000 children every day worldwide. However, following the widespread use of the oral polio vaccine (OPV), the number of children that were paralyzed by polio plummeted from 350,000 in 1988 to just 1606 in 2009. Additionally, the health-care costs involved in treating a sick child and the time spent taking care of a child with complications like paralysis (from polio), cirrhosis (from viral hepatitis), and hearing problems, blindness, encephalitis caused by measles can be re-invested into production.
Albeit numerous direct health benefits are associated with vaccination, other advantages include the long-term values of immunization to the community, the country, and the world at large. Vaccines are economic goods regarded by health economists to have positive externalities. This implies that vaccination is vital to both the individuals that are vaccinated and to their community. Therefore, when a substantial number of children in a community are vaccinated against a particular disease, herd immunity develops against that disease such that, even children who did not receive the vaccines become indirectly protected. However, to achieve a significant herd immunity, there must be enough protected individuals in a population whose immunization has exceeded the herd immunity threshold, defined as the fraction of a society that must be immunized to confer herd immunity on those not vaccinated against that disease.17,29 Studies in health economics have also demonstrated that a healthy community leads to high economic growth and development because healthy people work harder, efficiently, attract foreign direct investment and infrastructural development.28 Vaccinated children usually grow to their full potential, have better cognitive skills, improved life expectancy, and are more likely to progress in school and acquire a higher level of education. They can perform complex tasks effectively, leading to high economic productivity.26,31 Figure 1 shows a summarized vicious cycle of economic and health benefits of vaccination.32
Figure 1.
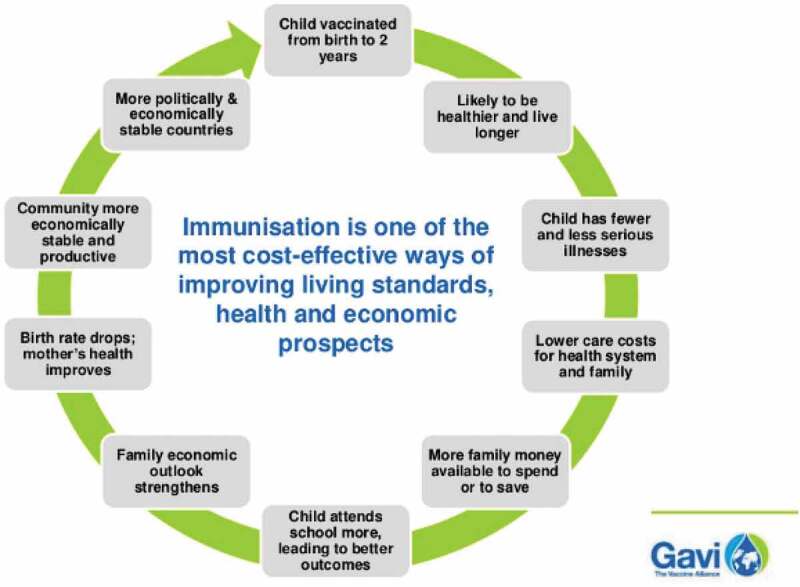
A vicious cycle of economic and health benefits of vaccination32.
5.3. Children’s right to vaccination
Childhood vaccination, irrespective of circumstances, is regarded as essential health-care services.33 Despite numerous pieces of evidence depicting the usefulness of vaccines in averting childhood morbidity and mortality, the debate on whether children should be vaccinated tends to be poignant and divisive. While some health-care professionals are trying to project mind-blowing data and figures on the noble role of vaccines in the prevention of infectious disease epidemics, some parents, on the other hand, are recounting nerve-racking stories of the different adverse reactions they have encountered.34 This has made vaccination to be opposed by some antagonists, who believe that each shot of vaccine is like a “Russian roulette”.35 Left out of this controversial discourse is the right of children to health as enshrined in the United Nations Convention on the rights of the child. All children should benefit from special protection and assistance; should have access to services such as education and health care; can develop their personalities, abilities and talents to the fullest potential; grow up in an environment of happiness, love and understanding; and be informed about their health and participate in achieving their rights in an accessible and active manner.36 Unfortunately, majority of children within the vaccination age bracket cannot make informed decisions about their health, thereby, leaving their fate in the hands of their parents and the government.
So much has been talked about parents regarding vaccine hesitancy (the ability to deny or delay vaccination despite the availability of vaccination services).37,38 However, some public and media debates regarding medical, ethical, and legal issues on vaccinations tend to aggravate vaccine hesitancy. Some parents do lack confidence in vaccination and in the health-care providers especially during conflicts because of suspicion regarding the motives behind vaccincation. For instance, in some parts of Nigeria, some of the reasons behind vaccine hesitancy include rumors about vaccine safety, community suspicions about the motives behind vaccination coupled with preexisting political, religious, and ethnic tensions.39 Similarly, in Abbottabad, Pakistan, the Guardian reported that the Central Intelligence Agency (CIA) organized a fake vaccination program as a means to obtain Osama Bin Ladin’s family member DNA.40 Some people are worried about kidnapping and the fear of being caught in the crossfire during conflicts. Many governments are unable to make vaccines available to children whose parents are willing to get them vaccinated but are unreachable during armed conflicts. These children are denied the highest level of health through vaccination including the opportunities to develop to their fullest potential. According to UNICEF, children in conflict-affected areas are forced to a downward spiral of deprivation that robs them of their health and, by extension, their futures.41 Leaving some children behind is not only a problem for them but also those around them.
5.4. A world full of conflicts
Armed conflicts and violence, whether social or political, continue to cause death, displacement, and suffering globally on a massive scale. Unfortunately, International law does not provide a clear guideline on the precise definition of “armed conflict” in the context of the Charter of the United Nations and the Geneva Conventions.42 However, the International Criminal Tribunal for the former Yugoslavia’s Appeals Chamber indicates that an armed conflict exists whenever there is protracted armed violence between governmental authorities and organized armed groups or between such groups within a State.43
According to the Uppsala Conflict Data Program, armed conflict is believed to occur when an organized actor uses armed force against another organized actor, or against civilians, resulting in at least 25 battle-related deaths in 1 calendar year.45 Based on this, three categories of armed conflicts exist; Firstly, state-based conflict (which involves two states or between one state and one or more rebel groups). Secondly, non-state conflict (this includes two organized, armed actors, of which neither is the government of a state) and thirdly, one-sided armed conflict (caused by an organized militant group, either a state’s military forces or an armed group, against civilians). Irrespective of the type of conflict, just or unjust, disastrous, or victorious, all wars are regarded to be waged against children because armed conflicts often do not demarcate battlefields; instead, residential areas and schools nowadays are battlefields and children and women are the most vulnerable.46
In a recent report by the Save the Children charity organization47 about 357 million children (one in six) worldwide are living in conflict areas and exposed to the most severe forms of violence imaginable. These figures are believed to be up by 75% from previous records in the early 90s. Conflict-affected children are children that reside within conflict zones or in areas within or less than 50 km from where conflict incidents are occurring. These children face killings and maimings, recruitment as “child soldier,” sexual violence, abduction, malnutrition, forceful displacement into the bushes and congested refugee camps, including attacks on schools and hospitals, and the denial of humanitarian access.47 About two-fifths of the children in the Middle East are believed to be living in conflict zones while in Africa, about 20% of the children are living in war-torn areas, and the figures are believed to be far higher due to the challenges involved in getting accurate statistics.48 Majority of these conflict-affected children live in Asia, the Middle East and Africa with Syria, Afghanistan, and Somalia ranked as the most dangerous countries to be a child.48 Figure 2 is a map of the world showing countries with ongoing armed conflicts classified based on of casualties.44
Figure 2.
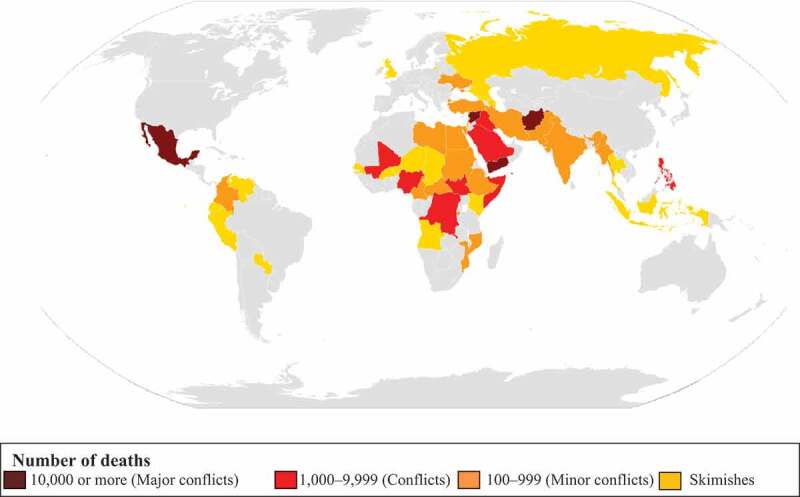
Countries with ongoing armed conflicts classified based on the number of deaths in current or past years.44
5.5. The impact of armed conflict on childhood immunization
The extent to which armed conflict affects vaccination services and child survival strategies seems to be poorly studied and inadequately assessed. However, the impact is believed to be devastating due to the destruction of essential livelihood services such as food, water, shelter, health, and education.49 Conflicts are associated with a dramatic reduction in vaccination coverage.1 Wagner and colleagues conducted a study in Africa and found a substantial increase in the risk of a child dying even after conflicts, which could probably be due to the destruction of infrastructures, malnutrition, and lack of vaccination.50 Despite the numerous successes recorded in immunization programs in some parts of the world, a considerable gap still exists globally, with a significant number of children in conflict zones left behind.
According to the United Nations International Children’s Emergency Fund (UNICEF), out of the 19.9 million children who did not receive the three recommended doses of DTP vaccine in 2017 and the 20.8 million who failed to receive a single dose of measles-containing vaccine, about two-thirds of them were living in countries that are either partially or entirely affected by conflict. This included children in South Sudan that has the highest percentage of unimmunized children (61%), followed by Somalia (58%) and Syria (57%).51,52 In a study conducted by Grundy and Biggs53 to ascertain the impact of conflict on immunization coverage in 16 countries (Afghanistan, Chad, Central African Republic, Cote D’Ivoire, Democratic Republic of Congo, Ethiopia, Kenya, Myanmar, Nigeria, Pakistan, Somalia, the Sudan, South Sudan, Uganda, Ukraine and Yemen), 14 out of 16 of these countries had immunization coverage below the global estimate for DPT3. Even though as of 2015, only 12.1% the global population were living in these 16 countries; however, between 2010 and 2015, they were home to 67% and 39% of all polio and measles cases, respectively.53
Polio is a highly infectious disease that mainly affects young children and leads to paralysis. It has almost been eliminated globally except in countries like Pakistan, Afghanistan, and Nigeria, where conflict has made the disease endemic.54 Before the ongoing conflict in Syria, polio was near elimination but re-surfaced in 2013 (14 years after being polio-free). Similarly, in Yemen, between the years 2014 to 2015, according to the WHO report, DPT3 coverage plunged from 73% to 47% as a result of conflict.55 Likewise, in South Sudan, there was a drop in DPT coverage from 75% to 46% in 2012 and 2014, respectively.53 In Ukraine, immunization coverage was about 76% for DPT3 between 2012 and 2013, but following the conflict in 2014, it crashed down to about 23% and then further to 19% 2 years after.56 In Syria, the proportion of children vaccinated against DPT was observed to have decreased significantly from 80% to 41% within 5 years of conflict.1 Recently in Cameroon, since the worsening of the ongoing armed conflict in the Northwest and Southwest Regions of the country between government forces and the restorationist fighters (also known as amba boys), the number of vaccinated children from 2018 has started to show a decline from previous years.57
5.6. How armed conflict affects childhood vaccination
The rhetoric regarding armed conflicts, the rule of engagement, human rights, and humanitarianism seems to be futile as the number of armed conflicts skyrocket globally, and the impacts on civilians, especially women and children, remain on a geometric increase. The Geneva Conventions and other Protocols (Rome Statute) demand that health-care systems, including health workers, should be neutral and be protected from attacks during conflict. However, these attacks still go on with little or no active response from the international community.58 The mechanism through which childhood vaccination services are affected by armed conflict, causing the emergence and spread of VPDs is multifaceted. Prevailing factors include the destruction of health-care facilities, crippling of the healthcare system, killing of health-care workers, displacement of people into the bushes, obstruction of humanitarian access, overcrowding in camps, poor hygiene conditions and poor nutritional status all causing a low immunity and high susceptibility to infection among displaced individuals.4 When people are forcibly displaced into the bushes and across national and international boundaries, VPDs outbreak and the reemergence of VPDs in these settings could be devastating and even spread to other areas. All of these contribute to inflicts more suffering on the vulnerable population who are predominantly children.59
5.6.1. Attacks on health-care facilities and workers
Attacks on health-care facilities and personnel seem to be another instrument of war. According to a 2018 report by the Safeguarding Health in Conflict Coalition Organization, there were at least 973 attacks on health workers, health facilities, health transports in 23 countries experiencing conflict.60 The report also showed that over 167 health workers were killed and 710 more injured. Amongst those wounded and killed were vaccination workers, paramedics, nurses, doctors, midwives, community volunteers, drivers, and guards. This estimate could be higher due to the difficulties encountered in getting accurate data. The highest number of attacks are believed to have occurred in Afghanistan, the Central African Republic, Libya, the occupied Palestinian territory, Syria and Yemen.60 Attacks on health-care facilities are a form of physical violence or obstruction that interferes with the accessibility and delivery of health care, including all types of structures that provide health care and transport to medical facilities.58 During the conflict in Irag (between March 2003 and December 2011), about 12 health facilities were bombed, stormed, or attacked. While in Syria, between March 2011 to March 2017, about 465 attacks occurred in 315 different medical facilities.61 Over the same period, more than 700 health workers were believed to have been killed.62 In Cameroon, attacks on medical facilities and health workers are ongoing in the conflict in the northwest and southwest regions of the country. In a report by the non-governmental organization, Medicins Sans Frontieres (MSN),63 hospitals are deliberately attacked or occupied by fighting groups; ambulances are destroyed, patients or victims taken away, and summarily executed, health workers are being threatened, abducted, subjected to violence, or killed. So far, over 61 attacks on health-care facilities and 39 against medical professionals have been documented.63 Figure 3 shows the charred remains of the Muyuka District Hospital, Southwest region of the former British West Cameroon burnt on the 31st of March 2019 as a results of the ongoing conflict between the Ambazonian restoration fighters (Amba boys) and the Cameroon government forces.64 Figure 4 also, is an ambulance destroyed in Gaza in 2014 due to conflict.65
Figure 3.

Charred remains of the Muyuka District Hospital burnt in the Southwest region of Cameroon.64
Figure 4.

Destruction of ambulance in Gaza during the conflict.65
5.6.2. Forceful displacement and denial of access to health-care services
Globally and especially in the Middle East and the North African states, people are on the move as a result of conflicts. According to the UN High Commissioner for Refugees (UNHCR), by the end of 2014, there were over 59.5 million people that were forcibly displaced worldwide as a result of persecution, conflict, and generalized violence.66 The Middle East and the Mediterranean regions have the highest percentage of refugees in the world.67 Forceful displacement and denial of access to healthcare and humanitarian services are now the hallmark of conflict and remain a deeply troubling issue that worsens the direct impact of hostilities and has devastating aftermath on children, particularly in their formative stages.68 According to Save the Children Organization, the denial of humanitarian access during conflicts has increased by 1500% since 2010 including incidences whereby cities and governorates are no-go areas such as Aleppo and Raqqa in Syria, Mosul, and Fallujah in Iraq, and some parts of Somalia and Afghanistan. In 2016 alone, more than 1,014 incidents of denial of access to health care and humanitarian services were reported.47
In 2017, according to the United Nations Department of Economic and Social Affairs (UN DESA), more than 36 million children (less than 18 years were displaced from their homes and were living as refugees.69 The figures were similar to those that were internally displaced. In a 2018 report by the Internal Displacement Monitoring Center (IDMC),70 there were over 28 million new displacements caused by conflict and disasters across 148 countries and territories in 2018. In South Sudan, a state of about 13 million people, by 2017, almost 2 million people predominantly women and children were internally displaced, and more than 1.4 million more became refugees in neighboring countries (Uganda and Ethiopia).71 In Cameroon, according to the United Nations Office for the Coordination of Humanitarian Affairs (UN OCHA) as reported by Médecins Sans Frontières (MSF), in just about 3 years of fighting between the English-speaking restoration fighters (amba boys) and the government forces in the northwest and southwest regions of the country, more than 530,000 people have already been uprooted from their homes and are living predominantly in makeshift shelters in the forest where they live in extremely poor conditions. Schools have been shut down, and school premises are being used as military bases to launch attacks. Some families have been forced to relocate to other cities, where they live in overcrowded and unsanitary settings. Some areas are reported to be inaccessible due to severe insecurity and the restrictions on movement.63 Figure 5 shows children living in the forest without shelter as a result of the ongoing armed conflict in the former British West Cameroon.72
Figure 5.

Families with children living in the forest (Cameroon) following what is regarded as anglophone crises (conflict).72
5.7. Armed conflict, infectious disease outbreaks and the reemergence of VPDs
Several global initiatives aimed at eradication, and eliminating VPDs including the Global Polio Eradication Initiative (GPEI) and the Measles and Rubella Initiative (MRI) are ongoing. Eradication is the permanent reduction to zero of the worldwide incidence of an infection caused by a specific agent as a result of deliberate efforts while elimination is the reduction of the incidence of a specified disease to zero in a defined geographic area.66 A reemerging infectious disease is a disease that was once a major health problem globally or in a particular country but declined significantly and is again becoming a significant challenge to the population.73
Refugee camps remain one of the niduses for breeding communicable diseases. Factors promoting disease transmission interact synergistically in refugee camps, and these include, congestion, malnutrition, poor hygiene and sanitation, and lack of other essential social determinants of health, leading to high incidences of diarrhea, respiratory tract infections, malaria, measles, and other VPDs. Infectious diseases contribute to most of the morbidity and mortality in complex humanitarian emergencies such as armed conflicts.74 The reemergence of polio in Syria after 13 years was believed to have been imported from Pakistan. Within about 3 months, there were up to 35 cases of polio in Syria.75 Measles outbreaks also increased tremendously across Syria and spread into neighboring countries, including Turkey, Jordan, and Lebanon.76 In Africa, as a result of conflict, an outbreak of polio in the refugee camps along the Kenya-Somalia border in 2013 later spread into the surrounding communities.77 Similarly, in Somalia, low vaccination coverage caused by the conflict in 2010 and 2011 led to a massive measles outbreak, and the number of cases increased from 145 to 1562 cases per million children under 5 years.78 The arrival of refugees from Somalia into the Dadaab refugee camp in Kenya and the Dollo Ado refugee camp in Ethiopia in 2010 and 2011 led to a devastating measle outbreak.79,80
In the Eastern region of Europe, following a conflict that started in Ukraine (2014), the level of vaccination dropped, and VPDs reemerged, including polio. Two cases of polio were confirmed, raising a severe public health concern.81 Other diseases with records of severe outbreaks in countries that are affected by conflict, include cholera and measles. By the end of October 2018, over 1.2 million cholera cases were reported in Yemen, causing more than 2500 deaths (58% were children). This was regarded by the WHO as the worst humanitarian crisis in the world.82 When the current trend of globalization, migration, and refugee crises is taken into consideration, it is almost certain that VPDs are bound to cross borders. In Norway, for example, following a measles outbreak, 8 out of the 10 affected children were of Somali origin.83
6. Conclusion
Geographical location and population demographics are some of the well-established determinants of childhood immunization. However, the impact of armed conflict could undermine and reverse all the gains so far achieved in the control and eradication of VPDs. Even with the existing treaties and laws on the rules of engagement during conflicts, attacks on health workers and health-care facilities still go unabated with some countries experiencing a total collapse in their health-care system, including vaccination programs. In some places, access to health-care facilities by health-care workers is denied. Hospitals are attacked, and schools in some states are shut down, and the premises used as military bases. Repeated abuse of the vaccination process has tremendously raised public suspicion, especially during conflicts leading to increased vaccine hesitancy. Civilians, especially children, are the most affected.
Most existing vaccination strategies nowadays focus on those who manage to reach refugee camps during conflicts with less attention to those in the bushes, and those who escape into other cities or countries unrecorded. There is an urgent need for the expansion of vaccination coverage during conflicts to include non-camp populations. Armed conflict remains a direct war on children and an indirect weapon of mass destruction. Those affected are pushed into the poverty trap, which creates a spiral of deprivation that robs them of their health, education, and by extension, their future wellbeing. They are not only left behind in terms of vaccination but are also deprived of their overall cognitive and socioeconomic development that results from healthy living. Leaving some children behind is also a problem for those around them and the world at large. No country is immune to a communicable disease, likewise VPDs. With extensive globalization and migration, even regions and countries that seem to be a safe heaven are potential time bombs. Urgent attention is needed to nip the escalating challenges of childhood immunization during conflicts, including upholding and strengthening not just in theories but in principles international treaties that protect education and health-care facilities, health workers, essential and emergency services during conflict. There is a need for improved technology to reach those in need. It is time to tackle armed conflicts as a significant determinant of childhood immunization else global efforts toward the control, eradication, and elimination of VPDs will remain far-fetch.
The empirical discussion in this paper should be considered in the light of some limitations. Articles that were used in writing this literature review can not be considered to be extensive as only papers that were published in the English language between 1974 to August 2019 were considered. Both search terms and bibliographic data bases used are considered not to be exhaustive. Also, the SANRA guidelines for narrative review articles that was used in selecting quality articles was short of critical appraisal. We suggest the need for more in-depth qualitative studies in specific conflict regions on the contextual factors for the shortfalls in vaccination coverage so as to ensure the uptake of vaccination programs in these contexts.
Funding Statement
This research received no specific grant from any funding agency, commercial or not for profit sectors.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Ethical standard
The authors state that this article complies with ethical standard.
References
- 1.Nnadi C, Etsano A, Uba B, Ohuabunwo C, Melton M, Wa Nganda G, Esapa L, Bolu O, Mahoney F, Vertefeuille J, et al. Approaches to vaccination among populations in areas of conflict. J Infect Dis. 2017. July 1;216(1):S368–72. doi: 10.1093/infdis/jix175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Immunization programme [Internet]. Unicef.org; 2019. [accessed 2019 September2]. https://www.unicef.org/immunization. [Google Scholar]
- 3.Obradovic Z, Balta S, Obradovic A, Mesic S.. The impact of war on vaccine preventable diseases. Mater Socio-medica. 2014. December;26(6):382. doi: 10.5455/msm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnett-Vanes A. Armed conflict, medical training and health systems. Med Conflict Survival. 2016. January 2;32(1):30–39. [DOI] [PubMed] [Google Scholar]
- 5.Sadr-Azodi N, DeRoeck D, Senouci K. Breaking the inertia in coverage: mainstreaming under-utilized immunization strategies in the Middle East and North Africa region. Vaccine. 2018. July 16;36(30):4425–32. doi: 10.1016/j.vaccine.2018.05.088. [DOI] [PubMed] [Google Scholar]
- 6.UNICEF . Immunization: current status and progress. 2016. https://data.unicef.org/topic/child-health/immunization/#.
- 7.Arie S. Polio virus spreads from Syria to Iraq. BMJ. 2014;348:g2481. https://www.bmj.com/content/348/bmj.g2481.short. [DOI] [PubMed] [Google Scholar]
- 8.Ozaras R, Leblebicioglu H, Sunbul M, Tabak F, Balkan II, Yemisen M, Sencan I, Ozturk R. The Syrian conflict and infectious diseases. Expert Rev Anti Infect Ther. 2016. June 2;14(6):547–55. doi: 10.1080/14787210.2016.1177457. [DOI] [PubMed] [Google Scholar]
- 9.United Nations (UN) News. Two thirds of unimmunized children live in conflict-affected countries-UNICEP. 2016 April 22 [accessed 2019 November 11]. https://news.un.org/en/story/2016/04/527422-two-thirds-unimmunized-children-live-conflict-affected-countries-unicef. [Google Scholar]
- 10.Keja K, Chan C, Hayden G, Henderson RH. Expanded programme on immunization. World health statistics quarterly. Rapport Trimestriel De Statistiques Sanitaires Mondiales. 1988;41:59–63. [PubMed] [Google Scholar]
- 11.Muraskin W. The global alliance for vaccines and immunization: is it a new model for effective public–private cooperation in international public health? Am J Public Health. 2004. November;94(11):1922–25. doi: 10.2105/AJPH.94.11.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roush RW, Murphy TV, Are V, TV, Vaccine-Preventable Disease Table Working Group . Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007. [DOI] [PubMed] [Google Scholar]
- 13.Enserink M. What’s next for disease eradication? Science. 2010. December 24;330(6012):1736–39. doi: 10.1126/science.330.6012.1736. [DOI] [PubMed] [Google Scholar]
- 14.Zhou F, Shefer A, Wenger J, Messonnier M, Wang LY, Lopez A, Moore M, Murphy TV, Cortese M, Rodewald L. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014. April 1;133(4):577–85. doi: 10.1542/peds.2013-0698. [DOI] [PubMed] [Google Scholar]
- 15.The power of vaccines: still not fully utilized. World Health Organisation (WHO); 2017. [accessed 2019 September2]. https://www.who.int/publications/10-year-review/chapter-vaccines.pdf?ua=1 [Google Scholar]
- 16.Gavi annual progress report. Global Alliance for Vaccinatination and Imunisation (GAVI). 2017. [accessed 2019 August30]. https://www.gavi.org/progress-report/
- 17.Balding B Mandatory vaccination: why we still got to get folks to take their shots. https://dash.harvard.edu/handle/1/8852146.
- 18.Walkinshaw E. Mandatory vaccinations: the international landscape. CMAJ. 2011. November 08;183(16):E1167–E1168. doi: 10.1503/cmaj.109-3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lob-Levyt J. Contribution of the GAVI Alliance to improving health and reducing poverty. Philos Tran Royal Soc B. 2011. October 12;366(1579):2743–47. doi: 10.1098/rstb.2011.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global Immunization Factsheet. World Health Organisation . 2018. [accessed 2019 September2]. http://www.who.int/mediacentre/factsheets/fs378/en.
- 21.Mathew G, Johnson AR, Thimmaiah S, Kumari R, Varghese A. Barriers to childhood immunization among women in an urban underprivileged area of Bangalore city, Karnataka, India: a qualitative study. Int J Community Med Public Health. 2017. January 5;3(6):1525–30. [Google Scholar]
- 22.Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integrity Peer Rev. 2019. December;4(1):5. doi: 10.1186/s41073-019-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malone KM, Hinman AR. Vaccination mandates: the public health imperative and individual rights. Law Public Health Pract. 2003;262–84. https://www.cdc.gov/vaccines/imz-managers/guides-pubs/downloads/vacc_mandates_chptr13.pdf [Google Scholar]
- 24.Morabia A. Edward Jenner’s 1798 report of challenge experiments demonstrating the protective effects of cowpox against smallpox. J R Soc Med. 2018. July;111(7):255–57. doi: 10.1177/0141076818783658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eldred BE, Dean AJ, McGuire TM, Nash AL. Vaccine components and constituents: responding to consumer concerns. Med J Australia. 2006. February;184(4):170–75. doi: 10.5694/mja2.2006.184.issue-4. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention . Vaccine excipient & media summary-excipients included in US vaccines. Vaccine. [Acesso em. 2013. June;25]. Disponível em: http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/appendices/b/excipienttable-2.pdf. [Google Scholar]
- 27.Global Immunization Factsheet. World Health Organisation . 2016. [accessed 2019 August22]. http://www.who.int/mediacentre/factsheets/fs378/en/.
- 28.Bärnighausen T, Bloom DE, Cafiero ET, O’Brien JC. Economic evaluation of vaccination: capturing the full benefits, with an application to human papillomavirus. Clin Microbiol Infect. 2012. October;18:70–76. doi: 10.1111/j.1469-0691.2012.03977.x. [DOI] [PubMed] [Google Scholar]
- 29.Greenlee CJ, Newton SS. A review of traditional vaccine-preventable diseases and the potential impact on the otolaryngologist. Int Archiv Otorhinolaryngology. 2018. July;22(03):317–29. doi: 10.1055/s-0037-1604055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akil L, Ahmad HA. The recent outbreaks and reemergence of poliovirus in war and conflict-affected areas. Int J Infect Dis. 2016. August 1;49:40–46. doi: 10.1016/j.ijid.2016.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miguel E, Kremer M. Worms: identifying impacts on education and health in the presence of treatment externalities. Econometrica. 2004. January;72(1):159–217. doi: 10.1111/ecta.2004.72.issue-1. [DOI] [Google Scholar]
- 32.Global Alliance For Vaccine (GAVI). Economic benefits of vaccines. 2014. August 25 [accessed 2019 August27]. https://www.gavi.org/library/audio-visual/presentations/economic-benefits-of-vaccines/.
- 33.Mashal T, Nakamura K, Kizuki M, Seino K, Takano T. Impact of conflict on infant immunisation coverage in Afghanistan: a countrywide study 2000–2003. Int J Health Geogr. 2007. December;6(1):23. doi: 10.1186/1476-072X-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kelso JM, Li JT, Nicklas RA, Blessing-Moore J, Cox L, Lang DM, Oppenheimer J, Portnoy JM, Randolph C, Schuller DE, et al. Adverse reactions to vaccines. Annals Allergy Asthma Immunol 2009. October 1;103(4):S1–4. doi: 10.1016/S1081-1206(10)60350-X. [DOI] [PubMed] [Google Scholar]
- 35.Vines T, Faunce TA. Civil liberties and the critics of safe vaccination: australian vaccination network inc v. Health care complaints commission (2012) NSWSC 110. Health Care Complaints Commission. 2012. [PubMed]
- 36.UNICEF . Convention on the rights of the child: adopted and opened for signature, ratification and accession by general assembly resolution 44/25 of 20 November 1989: entry into force 2 September 1990, in accordance with article 49. Accordance with Article. 1989;49. https://www.ohchr.org/en/professionalinterest/pages/crc.aspx [Google Scholar]
- 37.McKee C, Bohannon K. Exploring the reasons behind parental refusal of vaccines. J Pediatr Pharmacol Ther. 2016. April;21(2):104–09. doi: 10.5863/1551-6776-21.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Serpell L, Green J. Parental decision-making in childhood vaccination. Vaccine. 2006. May 8;24(19):4041–46. doi: 10.1016/j.vaccine.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 39.Ozawa S, Stack ML. Public trust and vaccine acceptance-international perspectives. Hum Vaccin Immunother. 2013. August 8;9(8):1774–78. doi: 10.4161/hv.24961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Guadian . CIA organised fake vaccination drive to get Osama bin Laden’s family DNA. [accessed 2019. August 27]. https://www.theguardian.com/world/2011/jul/11/cia-fake-vaccinations-osama-bin-ladens-dna.
- 41.UNICEF . Two-thirds of unimmunized children live in conflict-affected countries—UNICEF. 2016. [accessed 2019 August22]. https://www.unicef.org/media/media_90987.html.
- 42.Vité S. Typology of armed conflicts in international humanitarian law: legal concepts and actual situations. Int Rev Red Cross. 2009. March;91(873):69–94. doi: 10.1017/S181638310999021X. [DOI] [Google Scholar]
- 43.Warbrick C, Rowe P. The international criminal tribunal for yugoslavia: the decision of the appeals chamber on the interlocutory appeal on jurisdiction in the tadic case. Int Comp Law Q. 1996. July;45(3):691–701. doi: 10.1017/S0020589300059431. [DOI] [Google Scholar]
- 44.List of countries with ongoing armed conflicts . Wikipedia the free Encyclopedia. [accessed 2019 September2]. https://en.wikipedia.org/wiki/List_of_ongoing_armed_conflicts.
- 45.Uppsala universitet . Department of peace and conflict research. 2000. [accessed 2019 August27]. https://www.pcr.uu.se/research/ucdp/definitions/.
- 46.Bull A, Mayhew E, Reavley P, Tai N, Taylor S. Paediatric blast injury: challenges and priorities. Lancet Child Adolesc Health. 2018. May 1;2(5):310–11. doi: 10.1016/S2352-4642(18)30073-7. [DOI] [PubMed] [Google Scholar]
- 47.Save the Children . The war on children: time to end grave violations against children in conflict. 2018. www.savethechildren.net/waronchildren.
- 48.Lee M. More than 350 million children living in conflict zones, says charity. Reuters. 2018. https://www.reuters.com/article/us-global-war-children/more-than-350-million-children-living-in-conflict-zones-says-charity-idUSKCN1FZ00M.
- 49.Wise PH. The epidemiologic challenge to the conduct of just war: confronting indirect civilian casualties of war. Daedalus. 2017;146(1):139–54. doi: 10.1162/DAED_a_00428. [DOI] [Google Scholar]
- 50.Wagner Z, Heft-Neal S, Bhutta ZA, Black RE, Burke M, Bendavid E. Armed conflict and child mortality in Africa: a geospatial analysis. The Lancet. 2018. September 8;392(10150):857–65. doi: 10.1016/S0140-6736(18)31437-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.WHO/UNICEF . Coverage estimates 2017 revision, for 195 countries, and “the world population prospects: revision” from the UN population division. 2018. https://data.unicef.org/wp-content/uploads/infograms/10054/index.html.
- 52.UNICEF . Two-thirds of unimmunized children live in conflict-affected countries—UNICEF. 2016. [accessed 2016 December1]. https://www.unicef.org/media/media_90987.html.
- 53.Grundy J, Biggs B-A. The impact of conflict on immunisation coverage in 16 countries. Int J Health Policy Manag. 2019. April;8(4):211. doi: 10.15171/ijhpm.2018.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organisation (WHO) . Country Profile Yemen. 2018. [accessed 2018 September8]. http://www.who.int/immunization/monitoring_surveillance/data/yem.pdf.
- 55.Bhutta ZA. Conflict and polio: winning the polio wars. JAMA. 2013. September 4;310(9):905–06. doi: 10.1001/jama.2013.276583. [DOI] [PubMed] [Google Scholar]
- 56.World Health Organisation (WHO) . Country profile Ukraine. 2018. [accessed 2018 8September]. http://www.who.int/immunization/monitoring_surveillance/data/ukr.pdf.
- 57.WHO . (2019). WHO vaccine-preventable diseases: monitoring system. 2019 global summary. https://apps.who.int/immunization_monitoring/globalsummary
- 58.Briody C, Rubenstein L, Roberts L, Penney E, Keenan W, Horbar J. Review of attacks on health care facilities in six conflicts of the past three decades. Confl Health. 2018. December;12(1):19. doi: 10.1186/s13031-018-0152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Heudtlass P, Speybroeck N, Guha-Sapir D. Excess mortality in refugees, internally displaced persons and resident populations in complex humanitarian emergencies (1998–2012)–insights from operational data. Confl Health. 2016. December;10(1):15. doi: 10.1186/s13031-016-0082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Safeguarding Health in Conflict Coalition . Impunity Remains: attacks on health care in 23 countries in conflict in 2018. 2019. https://www.safeguardinghealth.org
- 61.Physicians for Human Rights . Anatomy of a crisis, A map of attacks on health care in Syria, methodology. 2017. https://s3.amazonaws.com/PHR_syria_map/methodology.pdf
- 62.Devi S. Syria’s health crisis: 5 years on. Lancet (London, England). 2016. March 12;387(10023):1042. doi: 10.1016/S0140-6736(16)00690-5. [DOI] [PubMed] [Google Scholar]
- 63.Five things to know about the violence in North-West and South-West Cameroon. Medecins San Frontieres. 2019. May 23. https://www.msf.org/five-things-know-about-violence-cameroon
- 64.The National Times . http://natimesnews.com/muyukanational-times-the-health-sector-in-the-two-english-speaking-regions-of-cameroon-in-the-early-hours-of-sunday-march-31-2019-was-dealt-another-devastating-blow-when-the-muyuka-district-hosp.
- 65.The 2014 conflict left Gaza’s healthcare shattered. When will justice be done? https://www.theguardian.com/commentisfree/2015/jun/29/2014-conflict-gaza-healthcare-hospitals-war-crime-israel-hamas
- 66.Lam E, Diaz M, Maina AG, Brennan M. Displaced populations due to humanitarian emergencies and its impact on global eradication and elimination of vaccine-preventable diseases. Confl Health. 2016. December;10(1):27. doi: 10.1186/s13031-016-0094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baldwin-Edwards M. Migration in the middle east and mediterranean: a paper prepared for the policy analysis and research programme of the global commission on international migration. University Research Institute for Urban Environment and Human Resources, Mediterranean Migration Observatory; 2005. [Google Scholar]
- 68.UNICEF . 27 million children out of school in conflict zones. 2017. https://www.unicef.org/media/media_100857.html.
- 69.United Nations Department of Economic and Social Affairs (UN DESA) . International migrant stock. The 2017 Revision. https://www.un.org/en/development/desa/population/migration/data/estimates2/estimates17.asp.
- 70.Internal Displacement monitoring centre (IDMC) . The global displacement landscape. 2019. http://www.internal-displacement.org/global-report/grid2019/
- 71.UNHCR . South Sudan situation. Supplementary Apeal. 2017. https://www.unhcr.org/593e9e9b7.pdf.
- 72.Global Pearls . https://globalpearls.org/2018/04/19/cameroon-april-2018-sleeping-in-the-bushes-and-streets/.
- 73.National Institutes of Health . Biological sciences curriculum study NIH curriculum supplement series.understanding emerging and re-emerging infectious diseases. Bethesda (MD, USA): National Institutes of Health (US); 2007. [Google Scholar]
- 74.Connolly MA, Gayer M, Ryan MJ, Salama P, Spiegel P, Heymann DL. Communicable diseases in complex emergencies: impact and challenges. The Lancet. 2004. November 27;364(9449):1974–83. doi: 10.1016/S0140-6736(04)17481-3. [DOI] [PubMed] [Google Scholar]
- 75.Foot T. Foreign jihadists ‘responsible’for polio outbreak in Syria. The Independent. 2013.
- 76.Sharara SL, Kanj SS, Heitman J. War and infectious diseases: challenges of the Syrian civil war. PLoS Pathog. 2014. November 13;10(11):e1004438. doi: 10.1371/journal.ppat.1004438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.World Health Organization . Combined use of inactivated and oral poliovirus vaccines in a large-scale campaign in refugee camps and host communities—Kenya, December 2013. Weekly Epidemiological Record= Relevé Épidémiologique Hebdomadaire. 2014;89(12):127–32. [PubMed] [Google Scholar]
- 78.Kebede A, Ahmed H, Masresha BG, Perry RT, Burton A, Spiegel P, Blanton C, Husain F, Goodson JL, Alexander JP. Measles-Horn of Africa, 2010–2011. Morbidity and Mortality Weekly Rep. 2012. August 31;61(34):678–84. [PubMed] [Google Scholar]
- 79.Navarro-Colorado C, Mahamud A, Burton A, Haskew C, Maina GK, Wagacha JB, Ahmed JA, Shetty S, Cookson S, Goodson JL, et al. Measles outbreak response among adolescent and adult Somali refugees displaced by famine in Kenya and Ethiopia, 2011. J Infect Dis. 2014. August 12;210(12):1863–70. doi: 10.1093/infdis/jiu395. [DOI] [PubMed] [Google Scholar]
- 80.Polonsky JA, Ronsse A, Ciglenecki I, Rull M, Porten K. High levels of mortality, malnutrition, and measles, among recently-displaced Somali refugees in Dagahaley camp, Dadaab refugee camp complex, Kenya, 2011. Confl Health. 2013. December;7(1):1. doi: 10.1186/1752-1505-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.World Health Organisation . Humanitarian health action. Ukraine Humanitarian Response Plan 2016. 2016. https://www.who.int/hac/crises/ukr/appeals/en/.
- 82.Federspiel F, Ali M. The cholera outbreak in Yemen: lessons learned and way forward. BMC Public Health. 2018. December;18(1):1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mipatrini D, Stefanelli P, Severoni S, Rezza G. Vaccinations in migrants and refugees: a challenge for European health systems. A systematic review of current scientific evidence. Pathog Glob Health. 2017. February 17;111(2):59–68. doi: 10.1080/20477724.2017.1281374. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- UNICEF . Immunization: current status and progress. 2016. https://data.unicef.org/topic/child-health/immunization/#.


