ABSTRACT
In Japan, the governmental recommendation for HPV vaccination was suspended in June 2013 because of media reports of so-called adverse vaccine events. The HPV vaccination rate in Japan prior to this suspension was almost 70%, but fell afterward to almost zero. To explore ways to bolster HPV vaccination, between 2014 and 2019 we conducted three serial surveys of the opinions of obstetricians and gynecologists about HPV vaccination. This study aimed to discuss the changing attitudes found in this 5-year follow-up survey. In August 2014, January 2017, and June 2019, we posted questionnaires to about 570 obstetricians and gynecologists practicing in Osaka, Japan. All three surveys used the same structured and closed-ended questionnaire, including questions about their personal opinions regarding HPV vaccination. We compared our new results to those of the previous two surveys. The response rate for the latest survey was 51.1% (293/573), which was equivalent to the previous two surveys. Among the responders, 83.3% (244/293) now thought that the Japanese government should restart its HPV vaccine recommendation, and 84.6% (248/293) were already recommending HPV vaccines for teenagers in their daily care. Eleven of 30 doctors (36.7%) had their own teenage daughters vaccinated against HPV after the suspension of recommendation. The rate has maintained an increasing trend from the previous two surveys. This study indicated that the attitude of obstetricians and gynecologists in Japan toward HPV vaccination has changed positively over 5 years. The results should serve as an encouragement to resume the governmental recommendation of HPV vaccines.
KEYWORDS: HPV vaccine, Opinion, Obstetrician, Gynecologist, Japan, suspension of recommendation
Introduction
From numerous studies, the effectiveness of the human papillomavirus (HPV) vaccine for the prevention of HPV-associated precancerous lesions is now clear, and cervical cancer prevention programs with HPV vaccines have been implemented worldwide.1-3 In Japan, the HPV vaccine was approved for clinical use in October 2009, and a national promotional campaign for HPV vaccination was initiated by the Ministry of Health, Labour and Welfare (MHLW) in November 2010. This campaign, which included generous public subsidies for part of the cost of the vaccination, benefitted many women in Japan. By the spring of 2013, the HPV vaccination rate, the rate of at least one-dose vaccination among 12- to 16-year-old women eligible for public subsidies, was approaching 70–80%.4,5 The program was so successful that, in April 2013, the MHLW designated HPV vaccination as a national routine-immunization, making it possible for eligible girls, aged 12 to 16, to be vaccinated free-of-charge.6 However, especially around May of 2013, the Japanese media began repeatedly issuing reports of so-called adverse vaccine events, rare but serious symptoms that appeared to be occurring in young girls after their HPV vaccination. This media blitz almost immediately made the Japanese public deeply distrustful of the HPV vaccine. As a consequence of strong public pressure, in June 2013, the MHLW announced a ‘temporary suspension’ of its own recommendation for the HPV vaccine.7 As of this writing, that suspension remains in place, and as a result, the nationwide HPV vaccination rate in Japan has fallen substantially, currently holding at almost zero.
Several studies have examined the critical issue of how to recover back to international norms the national HPV vaccination rates in our young girls and adolescents. Some studies have indicated that the opinions of the girl’s mothers, and the recommendation of trusted health-care providers, were key to the girl’s HPV vaccination.8,9 Because obstetricians and gynecologists are the familiar health-care providers, and thus who can encourage HPV vaccination to the girls and their mothers, for the last 5 years – between 2014 and 2019 – we have been serially conducting surveys on the opinions of our Japanese obstetricians and gynecologists about HPV vaccination; these surveys have been done three times (Figure 1).
Figure 1.
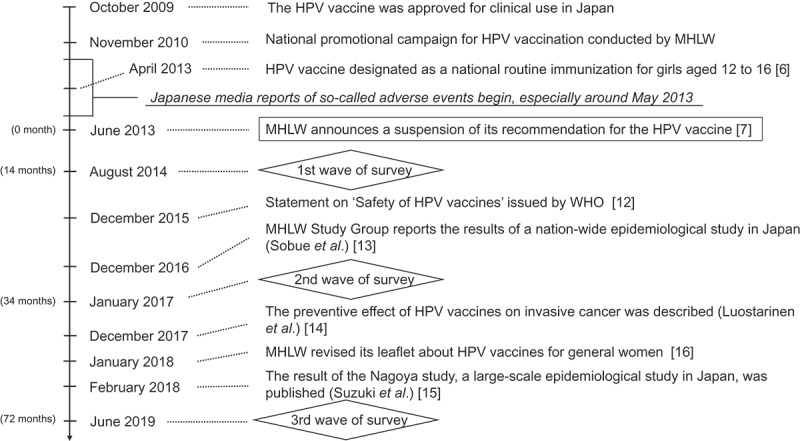
Changes in the social-political environment surrounding HPV vaccines in Japan.
Abbreviations: HPV, human papillomavirus; MHLW, the Ministry of Health, Labour and Welfare; WHO, World Health Organization
Our first wave of survey was conducted in August 2014, 14 months after the suspension of the governmental recommendation of the HPV vaccine. It demonstrated that obstetricians and gynecologists at that time were still affected negatively, by both the previous media reports of the so-called adverse events, and by the announcement of MHLW’s suspension of their recommendations for HPV vaccination.10
Our second wave of survey was conducted in January 2017, 43 months after the suspension.11 In the interim, the attitudes of the obstetricians and gynecologists in Japan had changed positively toward a recommendation of HPV vaccination, having been influenced by a statement from the World Health Organization (WHO) on the ‘Safety of HPV vaccines,’ issued in December 2015,12 and the report by Sobue et al., in December 2016, that the diverse adverse symptoms reportedly occurring after HPV vaccination were found at equal rates in non-vaccinated adolescents.13
We conducted our third wave of survey in this critical group of health-care providers in June 2019, 72 months after the suspension. Here, we compare the results of the three surveys and discuss the changes in attitudes of obstetricians and gynecologists that have occurred over the intervening 5 years.
Material and methods
Study design
We posted our standard questionnaire regarding the HPV vaccine in June 2019 to 573 targeted doctors working in and around the Osaka Prefecture, those who had been trained in the Department of Obstetrics and Gynecology of Osaka University Hospital, or one of its associated hospitals and clinics. The survey was the same as the previous two surveys; we used the same structured and closed-ended questionnaire, which included questions about the physician’s personal opinions regarding HPV vaccination, cervical cancer screening, and their own daughters’ HPV vaccination status. We compared the results of the three surveys regarding their intentions to recommend HPV vaccination to teenagers in their care, their opinions about whether the government should resume its HPV vaccination recommendation, and the number of the obstetricians and gynecologists who had their own daughters inoculated after the suspension of recommendation. The study was approved by the Osaka University Ethics Committee (approval #14361-8, approved on March 16, 2015).
Statistical analysis
We performed the chi-squared test or Fisher’s exact test using JMP Pro version 14.0.0 (SAS Institute, Cary, NC, USA). For our analysis of the three surveys, statistical significance is indicated by a p-value of <.05 in the comparison of respondent characteristics (Table 1), and <.017 (adjusted by the Bonferroni correction) in our analysis of the responders’ opinions on the HPV vaccine (Figure 2).
Table 1.
Characteristics of the responders of our three surveys.
| Third wave of survey (2019) (n = 293) |
Second wave of survey (2017) (n = 254) |
First wave of survey (2014) (n = 264) |
|||
|---|---|---|---|---|---|
| n (%) | n (%) | p value† | n (%) | p value‡ | |
| Gender | 0.044 | 0.083 | |||
| Male | 166 (56.7%) | 166 (65.4%) | 169 (64.0%) | ||
| Female | 127 (43.3%) | 88 (34.6%) | 95 (36.0%) | ||
| Age | 0.24 | 0.48 | |||
| Twenties | 17 (5.8%) | 6 (2.4%) | 7 (2.7%) | ||
| Thirties | 71 (24.2%) | 57 (22.4%) | 65 (24.6%) | ||
| Forties | 55 (18.8%) | 52 (20.5%) | 52 (19.7%) | ||
| Fifties | 63 (21.5%) | 58 (22.8%) | 67 (25.4%) | ||
| Sixties | 45 (15.4%) | 51 (20.1%) | 40 (15.2%) | ||
| Over seventy | 42 (14.3%) | 30 (11.8%) | 33 (12.5%) | ||
| Work status | 0.33 | 0.53 | |||
| Employed as a doctor | 189 (64.5%) | 148 (58.3%) | 160 (60.6%) | ||
| Owner of a clinic or hospital | 89 (30.4%) | 91 (35.8%) | 92 (34.8%) | ||
| Other | 15 (5.1%) | 15 (5.9%) | 11 (4.2%) | ||
| Medical specialty§ | 354 | 293 | 0.63 | 308 | 0.77 |
| General obstetrics and gynecology | 228 (64.4%) | 200 (68.3%) | 194 (73.5%) | ||
| Perinatal medicine | 45 (12.7%) | 29 (9.9%) | 36 (24.6%) | ||
| Gynecologic oncology | 40 (11.3%) | 37 (12.6%) | 45 (19.7%) | ||
| Reproductive and infertility medicine | 21 (5.9%) | 14 (4.8%) | 18 (6.8%) | ||
| Other | 20 (5.7%) | 13 (4.4%) | 15 (5.7%) | ||
| Experienced in examining a patient with cervical cancer | 0.42 | 1.00 | |||
| Yes | 291 (99.3%) | 250 (98.4%) | 263 (99.6%) | ||
| No | 2 (0.7%) | 4 (1.6%) | 1 (0.4%) | ||
| Experienced the death of a patient with cervical cancer | 0.58 | 0.37 | |||
| Yes | 264 (90.1%) | 225 (88.6%) | 244 (92.4%) | ||
| No | 29 (9.9%) | 29 (11.4%) | 20 (7.6%) | ||
| Have a child | 0.53 | 0.76 | |||
| Yes | 227 (77.5%) | 203 (79.9%) | 208 (78.8%) | ||
| No | 66 (22.5%) | 51 (20.1%) | 56 (21.2%) | ||
| Have a daughter aged 12 to 16 | 1.00 | 0.56 | |||
| Yes | 25 (8.5%) | 22 (8.7%) | 27 (10.2%) | ||
| No | 268 (91.5%) | 232 (91.3%) | 237 (89.8%) | ||
† p value from the chi-squared test or Fisher’s exact test – between our second and third wave of survey.
‡ p value from the chi-squared test or Fisher’s exact test – between our first and third wave of survey.
§ Multiple answers permitted.
Responders with no answer were excluded from our surveys.
Figure 2.
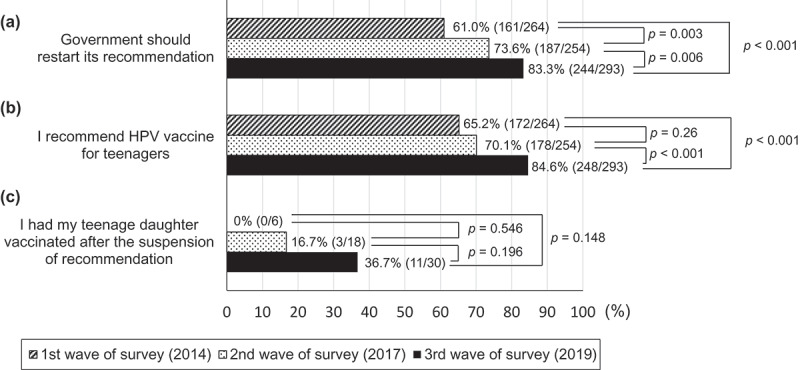
The results to questions in our three surveys about the responders’ opinion on the HPV vaccine. The rate of doctors who answered ‘yes’ to the question; (a) Whether the Japanese government should restart its HPV vaccine recommendation (b) Whether to recommend HPV vaccines for teenagers in their daily practice (c) Whether their own daughters had been inoculated after the suspension of recommendation. The bar with diagonal lines is the result of the first wave of survey in 2014, bar with dots is from the second wave of survey in 2017, and the black bar is from the third wave of survey. A p-value was calculated from the chi-squared test or Fisher’s exact test.
Results
Of the 573 obstetricians and gynecologists to whom our questionnaire was sent in June 2019, 293 replied by July 31, 2019. The response rate for about 2 months provided to the participants was 51.1%, which was not significantly different from the first and second waves of survey (45.9% [264/575], p = .087, and 45.7% [259/567], p = .067, respectively).
The characteristics of the responders are summarized in Table 1. There was no significant difference in the baseline characteristics of responders in each survey, except a higher proportion of females between the second and third wave of survey (p = .044). In all three surveys, approximately 99% of respondents were engaged in cervical cancer care, and almost 90% had experienced the death of one or more of their patients from cervical cancer.
The results of questions from our three surveys about the responders’ opinions on the HPV vaccine are shown in Figure 2. In this third wave of survey, 83.3% (244/293) of the obstetricians and gynecologists now have the opinion that the Japanese government should restart its recommendation for the HPV vaccine (Figure 2(a)). This was significantly higher compared with the first (61.0% [161/264], p < .001) and second wave of survey (73.6% [187/254], p = .006). In our third wave of survey, the proportion of doctors who recommended HPV vaccines for teenagers in their daily practice was 84.6% (248/293, Figure 2(b)), which was also significantly higher than in the first (65.2% [172/264], p < .001) and second wave of survey (70.1% [178/254], p < .001). Between the suspension of recommendation and the latest survey, 30 daughters of obstetricians and gynecologists had become the national recommended age for HPV vaccination, 12 to 16 years old. Our latest survey showed that eleven of the 30 daughters (36.7%) were vaccinated after the suspension of the HPV vaccination recommendation. The proportion of HPV vaccinations after the suspension has increased, compared to the first (0/6 [0%], p = .148) and second wave of survey (3/18 [16.7%], p = .196), and the trend has continued to increase over the course of 5 years (Figure 2(c)).
Discussion
Our most recent follow-up survey indicates that the attitudes of Japanese obstetricians and gynecologists, who have a critical role in the process of young girls and adolescents deciding to receive HPV vaccination, have changed significantly during the 5-year study period. They have become much more positive toward resuming the national recommendation for HPV vaccination.
After the suspension of the governmental recommendation for HPV vaccines in June 2013,7 various statements and reports were published, both within and outside of Japan, regarding the reported rare and diverse adverse symptoms arising in young girls following HPV vaccination. In December 2015, the WHO Global Advisory Committee on Vaccine Safety stated that: Policy decisions based on weak evidence, leading to lack of use of safe and effective vaccines, could result in real harm.12 In December 2016, Sobue et al. reported the results of a nation-wide epidemiological study regarding the reported HPV-vaccine-associated diverse symptoms in adolescents in Japan, which included pain and motor disability. From their survey, Sobue et al. concluded that the diverse symptoms reported after HPV vaccination were being found at similar rates in non-immunized adolescents, debunking, or at least weakening, the case for linkage of the symptoms to the vaccine.13 During that period, study sessions and lectures on HPV vaccines were held mainly by obstetricians and gynecologists in several regions such as Osaka Prefecture, but there was no official promotion campaign in municipalities. Collectively, the results of our first two surveys, the WHO statement, and the report by Sobue et al. have all improved our physician’s attitudes toward the HPV vaccine, which had been negative due to the adversarial media reports and MHLW’s suspension of their recommendation for HPV vaccination.
In the time since the release of our second wave of survey, several relevant studies regarding the HPV vaccine have been published. In December 2017, Luostarinen et al. provided evidence that vaccines have a preventive effect on HPV-associated invasive cancers, as well as precancerous lesions.14 In February 2018, the large-scale epidemiological study in Japan, Nagoya Study, suggested that there was no causal-link association between HPV vaccines and the previously reported adverse symptoms.15 In January 2018, the MHLW revised their own leaflet on HPV vaccines, geared for women in general, to describe the vaccine’s effectiveness – to counter fears of the potential for adverse events, that it also lists, and to encourage to judge the need for the vaccine.16 The results of these studies contribute to the reasons why our doctors’ attitudes toward HPV vaccines have changed, in a better direction, that we found in our third wave of survey. However, the national vaccination rate remains almost zero in 2019. The reason is presumed that attitudes of general physicians and pediatricians who were not included in our surveys toward HPV vaccines have not improved yet. Therefore, for the spread of HPV vaccination in Japan, it is the mission of us, obstetricians, and gynecologists, to provide correct understanding to all health-care providers who deliver HPV vaccines.
In a large cohort study, the age-adjusted incidence of cervical cancer in Japan has increased worrisomely since 2000.17 If HPV vaccination in Japan does not soon return to its pre-suspension rates of 70% or more, the risk of future cervical and other cancers in young Japanese women is expected to rise dramatically. We have already reported that these future cancer risks for girls and adolescents will differ in accordance with their birth year, whether they were lucky enough to have come of age during a period when HPV vaccination was still in vogue.18,19 Despite these epidemiological researches and scientific reports on HPV vaccines and cervical cancer, the MHLW has not yet restarted its recommendation for HPV vaccination. This is expected to be caused by complex factors. However, some municipalities have already started their own activities such as mailing HPV vaccine information to women aged 12 to 16 and describing the HPV vaccine information on their website although nationwide vaccination promotion activities have not been resumed. Increasing research and reports at the region level, including this study, that provide the correct understanding about the need and usefulness of HPV vaccines may change the current situation in Japan. If the governmental recommendation for HPV vaccines is restarted, the resurgence of HPV vaccinations might have some improved impetus now, as the results of our present study indicate that the attitudes of the obstetricians and gynecologists have become much more positive than 5 years ago.
A key strength of our study is that our surveys were conducted multiple times, for the same subject and over an extended period of time, and that these investigations focused on the attitudes of clearly critical personnel, the obstetricians, and gynecologists in Japan, and during a peculiar situation, where the governmental recommendations for the vaccine have been suspended. As far as we know, there is no other similar study, and it is a useful method for observing changes in the attitude of study-relevant doctors. All three surveys had a high response rate, in spite of the questionnaire survey being sent by postal mail.
We have two limitations of this study. First, this study was conducted only for Osaka Prefecture, not for all of Japan, and only for obstetricians and gynecologists, not including general physicians and pediatricians who usually deliver HPV vaccines. We thought that it would be ideal to conduct surveys in not only obstetricians and gynecologists but also doctors of multiple departments such as physicians and pediatricians. However, considering the importance of continuing a follow-up survey over a long period rather than conducting a large-scale study, we only targeted obstetricians and gynecologists in our surveys. Secondly, it was impossible to identify the participants who completed our three surveys. The list used to select the obstetricians and gynecologists who were mailed the questionnaire was updated each year, so it was different for each of the three surveys, and the questionnaire was anonymous, making it impossible to identify individuals. For these reasons, we were unable to perform sensitivity analysis on the participants who completed the three surveys.
In conclusion, the attitudes of obstetricians and gynecologists in Japan toward HPV vaccination have changed positively over the last 5 years. Unfortunately, despite various important reports regarding the efficacy and necessity of HPV vaccines, Japan’s MHLW has not yet restarted their recommendation for HPV vaccination. However, these reports and activities have had a great impact on the opinions of Japan’s ground-level obstetricians and gynecologists, so our continued efforts to give the correct understanding of vaccines will be a major force in causing the resumption of a national recommendation for HPV vaccination.
Acknowledgments
We would like to thank Dr. GS Buzard for his constructive critique and editing.
Funding Statement
This study was supported by a Health and Labour Sciences Research Grant [H29-024]; Ministry of Health, Labour and Welfare [H29-024].
Author contributions
YN, YU, AY, SN, KH, and TK contributed to the study conception and design, data collection, and drafting of the manuscript. All authors have read and approved the final version of this manuscript.
Disclosure of potential conflicts of interest
YU and AY have received a lecture fee, and YU received a research grant [J550703673] from Merck Sharp & Dohme (MSD). TK received a research fund [VT#55166] from MSD.
Abbreviations
- HPV
Human papillomavirus
- MHLW
The Ministry of Health, Labour and Welfare
- WHO
World Health Organization
References
- 1.Garland SM, Hernandez-Avila M, Wheeler CM, Perez G, Harper DM, Leodolter S, Tang GWK, Ferris DG, Steben M, Bryan J, et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N Engl J Med. 2007;356:1928–43. doi: 10.1056/NEJMoa061760. [DOI] [PubMed] [Google Scholar]
- 2.Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet. 2009;374:301–14. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- 3.Lu B, Kumar A, Castellsagué X, Giuliano AR.. Efficacy and safety of prophylactic vaccines against cervical HPV infection and diseases among women: a systematic review and meta-analysis. BMC Infect Dis. 2011;11:13. doi: 10.1186/1471-2334-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ueda Y, Enomoto T, Sekine M, Egawa-Takata T, Morimoto A, Kimura T.. Japan’s failure to vaccinate girls against human papillomavirus. Am J Obstet Gynecol. 2015;212:405–06. doi: 10.1016/j.ajog.2014.11.037. [DOI] [PubMed] [Google Scholar]
- 5.Hanley SJ, Yoshioka E, Ito Y, Kishi R. HPV vaccination crisis in Japan. Lancet. 2015;385:2571. doi: 10.1016/S0140-6736(15)61152-7. [DOI] [PubMed] [Google Scholar]
- 6.Japanese Immunization Act (Act No. 68 of June 30, 1948), Article 5 (1). [accessed 2019 November30]. https://www.mhlw.go.jp/web/t_doc?dataId=79015000&dataType=0&pageNo=1.
- 7.The Ministry of Health, Labour and Welfare . 2013. June 14. [accessed 2019 November30]. https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou28/pdf/kankoku_h25_6_01.pdf.
- 8.Bratic JS, Seyferth ER, Bocchini JA Jr.. Update on barriers to human papillomavirus vaccination and effective strategies to promote vaccine acceptance. Curr Opin Pediatr. 2016;28:407–12. doi: 10.1097/MOP.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 9.Egawa-Takata T, Ueda Y, Morimoto A, Yoshino K, Kimura T, Nishikawa N, Sekine M, Horikoshi Y, Takagi T, Enomoto T. Survey of Japanese mothers of daughters eligible for human papillomavirus vaccination on attitudes about media reports of adverse events and the suspension of governmental recommendation for vaccination. J Obstet Gynaecol Res. 2015;41:1965–71. doi: 10.1111/jog.12822. [DOI] [PubMed] [Google Scholar]
- 10.Egawa-Takata T, Ueda Y, Morimoto A, Tanaka Y, Matsuzaki S, Kobayashi E, Yoshino K, Sekine M, Enomoto T, Kimura T, et al. Human papillomavirus vaccination of the daughters of obstetricians and gynecologists in Japan. Int J Clin Oncol. 2016;21:53–58. doi: 10.1007/s10147-015-0869-5. [DOI] [PubMed] [Google Scholar]
- 11.Sawada M, Ueda Y, Yagi A, Morimoto A, Nakae R, Kakubari R, Abe H, Egawa-Takata T, Iwamiya T, Matsuzaki S, et al. HPV vaccination in Japan: results of a 3-year follow-up survey of obstetricians and gynecologists regarding their opinions toward the vaccine. Int J Clin Oncol. 2018;23:121–25. doi: 10.1007/s10147-017-1188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The statement of Global Advisory Committee on Vaccine Safety . 2015. December 2–3. [accessed 2019 August15]. https://www.who.int/vaccine_safety/committee/reports/wer9103.pdf.
- 13.The report of the Vaccine Adverse Reaction Review Committee (VARRC) . [accessed 2019 August15]. https://www.mhlw.go.jp/file/05-Shingikai-10601000-Daijinkanboukouseikagakuka-Kouseikagakuka/0000147016.pdf.
- 14.Luostarinen T, Apter D, Dillner J, Eriksson T, Harjula K, Natunen K, Paavonen J, Pukkala E, Lehtinen M. Vaccination protects against invasive HPV-associated cancers. Int J Cancer. 2018;142:2186–87. doi: 10.1002/ijc.31231. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki S, Hosono A. No association between HPV vaccine and reported post-vaccination symptoms in Japanese young women: results of the Nagoya study. Papillomavirus Res. 2018;5:96–103. doi: 10.1016/j.pvr.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The leaflet on HPV vaccines published by the Ministry of Health, Labour and Welfare . 2018. January [accessed 2019 August15]. https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou28/dl/hpv180118-info01.pdf.
- 17.Yagi A, Ueda Y, Kakuda M, Tanaka Y, Ikeda S, Matsuzaki S, Kobayashi E, Morishima T, Miyashiro I, Fukui K, et al. Epidemiologic and clinical analysis of cervical cancer using data from the population-based Osaka cancer registry. Cancer Res. 2019;79:1252–59. doi: 10.1158/0008-5472.CAN-18-3109. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka Y, Ueda Y, Egawa-Takata T, Yagi A, Yoshino K, Kimura T. Outcomes for girls without HPV vaccination in Japan. Lancet Oncol. 2016;17:868–69. doi: 10.1016/S1470-2045(16)00147-9. [DOI] [PubMed] [Google Scholar]
- 19.Yagi A, Ueda Y, Egawa-Takata T, Tanaka Y, Nakae R, Morimoto A, Terai Y, Ohmichi M, Ichimura T, Sumi T, et al. Realistic fear of cervical cancer risk in Japan depending on birth year. Hum Vaccin Immunother. 2017;13:1700–04. doi: 10.1080/21645515.2017.129219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Japanese Immunization Act (Act No. 68 of June 30, 1948), Article 5 (1). [accessed 2019 November30]. https://www.mhlw.go.jp/web/t_doc?dataId=79015000&dataType=0&pageNo=1.


