ABSTRACT
The impact of seasonal influenza has been under-appreciated in Asia and surveillance data lags in most other regions. The variety of influenza circulation patterns in Asia – largely due to the range of climates – has also only recently been recognized and its effect on the burden of disease is not fully understood. Recent reports that clinical protection wanes in the weeks after influenza vaccination emphasize the importance of optimally timing vaccination to local epidemiology. It also raises questions as to whether influenza vaccines should be administered more frequently than annually and what may be the benefits in Asia of access to new vaccines with enhanced immunogenicity and effectiveness. This review will summarize influenza surveillance data from Asian countries over 2011–2018, and consider the implications for vaccination strategies in different parts of Asia.
KEYWORDS: Adjuvant, Asia, high dose, influenza, older adults, recombinant, standard dose, vaccine, waning
Introduction
Pandemics and epidemics attributable to the influenza virus can be traced back through the historical record to the middle ages and perhaps antiquity.1 The first reliably documented pandemic occurred in 1580 and is generally accepted to have emerged in Asia.2 Two of the last three pandemics originated in Asia, as may have the 1918 ‘Spanish flu’3 Human infections with the highly pathogenic avian influenza viruses A/H5N1 and A/H7N9 over the past 20 years indicate Asia is also the most likely source for the next one.4
Understanding the burden from seasonal influenza in Asia and developing a regional vaccination policy needs to take into account its diversity. Asia is home to roughly 60% of the global population, including three of the world’s most populous countries in China, India, and Indonesia.5 Across Asia the rate of population growth has been slowing since 1990: families are having fewer children as infant mortality declines, but a larger proportion of the population is aged 65 years or older. However, economic development across the continent remains uneven, from wealthy globally connected cities to an estimated 400 million who still live in poverty.6 Similarly, while the majority of Asia is situated in the Northern hemisphere, seasonal influenza patterns vary widely across the continent. This reflects the range of climates, from the equatorial South to an almost polar North.7
Recent reports that clinical protection wanes in the weeks after influenza vaccination emphasize the importance of optimally timing vaccination to local epidemiology.8 It also raises questions as to whether influenza vaccines should be administered more frequently than annually and what may be the benefits in Asia of access to new vaccines with enhanced immunogenicity and effectiveness.
We will review FluNet influenza surveillance data from Asian countries over 2011–2018 and describe seasonal patterns; discuss recent evidence for waning protection following vaccination; and consider the implications for vaccination strategies in different parts of Asia.
Influenza epidemiology in asia
Since 1997 country-level influenza surveillance data submitted by National Influenza Centers (NICs) has been available at the World Health Organization (WHO) FluNet web portal.9 In response to the 2009 A/H1N1 pandemic, surveillance of seasonal influenza in Asia expanded considerably. By 2017–2018 data were available from 43 countries in Asia, covering 98% of the continent’s population (Table 1). Despite this broadening coverage, the amount of data available on a per capita basis in Asia continues to lag other continents except Africa. Coverage is also patchy, with proportionally less data available from South and South East Asia (0.46 and 0.86 influenza cases reported per 100,000 people, respectively).
Table 1.
Summary of influenza data by continent reported to FluNet, 2017–2018. Continent definition per WHO influenza transmission zones. Population data from the United Nations Population Division (2019).
| Africa | Asia | Europe | Latin America | North America | Oceania | Global | |
|---|---|---|---|---|---|---|---|
| No of countries reporting data | 30 | 43 | 40 | 39 | 3 | 5 | 160 |
| No of WHO transmission zones | 5 | 5 | 3 | 3 | 1 | 1 | 18 |
| Population in countries reporting data, ‘000s (2018) | 1 087 244 | 4 468 571 | 745 894 | 638 645 | 364 234 | 39 411 | 7 344 000 |
| Population of region, ‘000s (2018) | 1 275 921 | 4 560 667 | 746 419 | 642 217 | 364 296 | 41 571 | 7 631 091 |
| FluNet coverage (% of population) | 85.2% | 98.0% | 99.9% | 99.4% | 100.0% | 94.8% | 96.2% |
| Number of influenza cases per year reported to FluNet | 7 811 | 136 759 | 184 780 | 28 861 | 294 283 | 8 462 | 660 954 |
| Number people per reported influenza case | 139 203 | 32 675 | 4 037 | 22 128 | 1 238 | 4 657 | 11 111 |
| Number influenza cases reported per 100,000 people | 0.7 | 3.1 | 24.8 | 4.5 | 80.8 | 21.5 | 9.0 |
While it has limitations, the breadth and depth of influenza surveillance data now available offers a clearer perspective of the worldwide pattern of seasonal influenza epidemics. As a result of this the WHO has classified global influenza circulation into 18 ‘transmission zones’ – geographical groupings of countries with similar climates where seasonal influenza transmission patterns are expected to be similar. Asia covers five transmission zones, more than any other continent except Africa, which also has five.
The timing of epidemics varies between these transmission zones, as does the number of outbreaks per year and the extent of inter-epidemic transmission.10–12 Two key factors appear to determine the timing and intensity of an influenza epidemic: climate and population immunity to the circulating strain.
Climate and influenza in asia
Climate is largely a consequence of latitude, but is also influenced by terrain, altitude, and the presence of nearby large waterbodies.13 FluNet data is available for 27 countries across the five Asian influenza transmission zones from 2011 to 2018, and over this period 760,012 infections were reported, of which 28.3% were influenza A/H1N1, 39.2% A/H3N2 and 32.5% B (Figure 1(a, b)). Weekly reported influenza data for each country were analyzed using the EPIPOI program.14 This software estimates the seasonality of disease outbreaks by Fourier decomposition of the time-series data.
Figure 1.
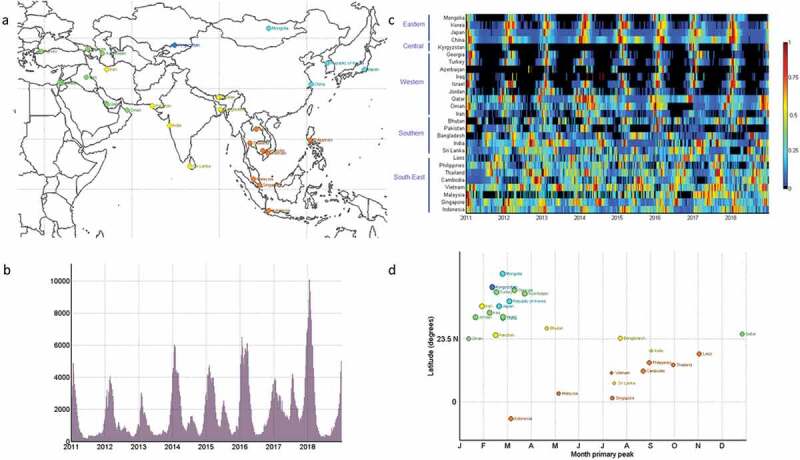
(a) Map of the 27 countries with weekly influenza data available from 2011 to 2018 on FluNet. Color groupings by WHO transmission zone [South-East (orange), Southern (yellow), Eastern (light blue), Central (dark blue), Western (green)]. (b) Number of influenza cases reported per week from 2011 to 2018 [Note for 1B and 1C labels indicate the beginning of the respective year]. (c) Heat map of weekly influenza cases (A/H1, A/H3 and B combined) reported to FluNet from 2011 to 2018 normalized to proportion per year (where 1 = week with highest proportion). Countries organized by WHO transmission zone and by the latitude of most populous city in that country from North to South. (d) Time-series analysis to infer the month of primary seasonal influenza peak from FluNet surveillance data, stratified by the latitude of countries most populous city and grouped by WHO influenza transmission zone [4-weekly smoothed and detrended by proportion of cases per year].
A heat-map of the weekly number of influenza cases (type A and B combined) illustrates the change in influenza patterns with the transmission zone (Figure 1(c)). For countries in tropical/sub-tropical Southern and South-East Asia, influenza infections were reported throughout the year, with generally two outbreaks per year. The primary peak was estimated as between May and October for most of these countries, but was not synchronized (Figure 1(d)).
For the Western, Central and Eastern transmission zones, influenza infections were largely confined to the winter season, with peaks between December and March. Outbreak timing within each zone was generally synchronized though there is some evidence of an East to West spread within the Western Asia transmission zone.
Analysis of the harmonic waves of influenza activity indicated there was a strong correlation between latitude and the amplitude of the primary influenza peak (r2 = 0.66, p < .0001). This indicates an increasingly sharp contrast in the amount of influenza circulating between epidemic and non-epidemic periods with rising latitude. Conversely, there was an inverse correlation between latitude and the secondary influenza peak – indicating larger secondary peaks of influenza activity at latitudes closer to the equator (r2 = 0.49, p = .0001).
The lack of important meta-data limits a more granular analysis of the data from FluNet. For example, there is wide variation both between countries in the amount of influenza surveillance data submitted – but within each country much is also unknown such as which patients are tested, how frequently testing occurs, in what parts of the country, and the source for data submitted to FluNet (e.g. clinical practice versus surveillance). The aggregation of surveillance data by country also obscures interpretation when countries have large population centers in different climates. This is most significant in Asia for China and India which have enormous populations, numerous mega-cities and cover diverse climates. Studies from within these countries support the overall trends described here – and highlights the importance of considering influenza circulation patterns on the basis of climate and local surveillance data rather than necessarily by country.15,16 Even in smaller countries, major population centers may occupy a different climate to the rest of the country, while seasonal labor migration routes also play a significant role in the timing of epidemics.
Differences in the epidemiology of influenza viruses are also evident, and outbreaks of different influenza types/subtypes are not always synchronous.7,17 For example, influenza A/H3N2 has been reported to cause shorter but more intense and more frequent epidemics than influenza A/H1N1 and B/Yamagata, perhaps reflecting differences in the rate of antigenic drift.18 The stability of the currently observed pattern may also be affected by climate change, and predictions that the climates across much of Asia will become warmer and wetter may have important implications for influenza virus activity.19
Burden of disease
As the epidemiology of influenza in different regions of the world becomes better understood, a number of studies have also investigated how the burden of disease (largely in terms of mortality) varies in different climates. A recent modeling study of influenza-associated mortality estimated there were ~290,000–645,000 deaths per year.20 The highest mortality estimates were in sub-Saharan Africa (2.8–16.5 per 100,000 individuals) and southeast Asia (3.5–9.2 per 100,000 individuals). Extremes of age (<5yrs, >65yrs) and residence in a lower-income country also predicted higher mortality.
Similar findings have been observed from individual studies comparing influenza attributable mortality between countries, and between different provinces in China.21,22 These studies suggest that differences in the burden of disease from influenza are a result of factors such as population density, the proportion of older adults, and access to healthcare rather than climate. However, a robust consideration of how the seasonal pattern of influenza activity affects morbidity and associated economic burden is lacking.
Population immunity
A diverse range of mechanisms have been proposed to explain how seasonal changes in weather might affect the timing of influenza outbreaks and extinction. These include changes in host behavior, susceptibility to infection (such as relative vitamin D deficiency), viral shedding and viral stability. While all are likely to contribute to seasonality to some extent, compelling evidence has emerged to place the effects of temperature and humidity on infectious aerosols as the most important factor.
The virus stability hypothesis proposes that environmental conditions affect the movement of water between virus and droplet. This affects the duration of virus infectivity in aerosols, by shifting the equilibrium between virus disruption, desiccation or stability.23 Physio-chemical modeling suggests water movement is closest to equilibrium and thus virus stability maintained in conditions where the air is either cold and dry, or warm and humid. Reflecting this, the timing of the onset of influenza outbreaks in temperate climates correlates most closely with the timing of the winter season decline in absolute humidity (AH).24 In warmer climates AH also predicts influenza season timing as part of the onset of monsoon or rainy seasons.25 More recently, the hypothesized U-shaped relationship between absolute humidity, temperature, and influenza transmission has been identified from a global analysis of surveillance and environmental data.26
In tropical climates, humidity, temperature, and rainfall vary little from month-to-month, so these effects seem unlikely to explain the timing of influenza outbreaks. Contact rates affect the scale of influenza epidemics, but while influenza transmission is reduced by school holidays and increases when people congregate, it is not known whether this might also have an effect on seasonality.27,28 Rather than changes in transmission frequency, it may be the importation of antigenically drifted strains by travelers during holiday periods which is more important. Longitudinal sero-epidemiological studies have correlated waves of seasonal influenza activity with population immunity in Singapore and Hong Kong.29,30 The balance between antigenic drift in circulating strains and waning immunity following infection and/or vaccination may be the main driver of outbreak timing in the tropics.
If population immunity changes at a similar rate in tropical regions and other climates, this suggests that the year-round influenza activity in tropical Asia is likely to play an important role in global influenza circulation. Initial genetic analysis of influenza A/H3N2 isolated from 2002 to 2007 suggested a source-sink model, in which new antigenic strains of influenza emerge in east and south-east Asia and then spread globally. This observation was attributed to intra-seasonal persistence of influenza virus in the tropics, with winter in temperate climates forming an ecological trap. Viral extinction at the end of the winter season reduces the probability of newly emerged temperate season strains would spread globally.31 Over the past two decades, strains of A/H3N2 isolated in East–Southeast Asia have been more ‘antigenically advanced’ than strains isolated elsewhere.32
Analysis of a wider selection of influenza viruses types and subtypes described a more heterogenous pattern of viral emergence. Rather than a single source, influenza can be construed as a series of populations, and travel between these populations ensures the long-term survival of influenza virus in humans. Despite this more nuanced view, new antigenic strains of A/H3N2 have typically emerged in East and Southeast Asia first, with the trunk present here in 87% of cases.33 In temperate regions, variants of A/H1N1 and B viruses persisted across multiple seasons and exhibited complex global dynamics with Asia playing a less prominent role in disseminating new variants.
Understanding the drivers behind the global evolution of influenza viruses is important both for detecting – and possibly predicting – the emergence of new pandemic strains, and for the biannual selection of influenza strains to be included in vaccines for the following Northern and Southern hemisphere winters.
Influenza vaccination strategies in asia
Influenza vaccine uptake within Asia is generally low, and a systematic review focused on Asian countries reported a median uptake of 14.9% among the general population and 37.3% among high-risk groups – far below the WHO target of 75%.34 The review uncovered few studies which investigated influenza vaccination knowledge, attitudes and behavior in the Asian context and further study is needed to understand the barriers which need to be overcome to improve uptake.
A specific issue for much of Asia is the duration of protection following vaccination. This has not been well studied in clinical trials, reflecting the relatively short duration of the influenza season in most countries with the resources to study this, and the standard recommendation for annual re-vaccination as strains within the vaccine are frequently updated.
Duration of immunity after vaccination
The hemagglutination-inhibition (HI) titer is an established immune correlate of protection against influenza infection, and has been adopted for licensure of inactivated influenza vaccines. A titer of ≥1:40 correlates with ~50% protection against infection, and this threshold is conventionally used to define ‘seroprotection’35 Several studies have documented a surprisingly rapid decline in HI titers following vaccination or infection, though results are mixed.
Investigators performing a trial of inactivated versus live-attenuated influenza in adults aged 18–49 years reported that a two-fold waning of HI titers took >600 days for all influenza strains.36 On the other hand, an observational study of HI titers following influenza vaccination in 1018 adults conducted in South Korea, reported a significant decline in HI GMTs for all age groups (18–49, 50–65, ≥65) and all influenza types/subtypes. In this study the HI titer 1 year after vaccination was not significantly different to pre-vaccination.37 Similar results to these were also reported from a sero-epidemiological study of HI persistence following infection with A/H1N1 during the 2009 pandemic: HI titers declined within a year after infection, with the fastest decline (to below a HI titer of 1:40) in adults aged ≥65.38
Intuitively, increasing age and health burden from co-morbidities are expected to reduce the duration of protection after vaccination. Limited data is available to corroborate this, and individual studies can be difficult to compare due to the complex effects of prior immunity – particularly variability in prior vaccination rates. A systematic review and meta-analysis of HI antibody titers up to 360 days after vaccination in adults aged ≥65 described a significant decline in titers 180 days after vaccination, such that by 1 year after vaccination GMTs and the proportion of study participants with a HI titer ≥1:40 was not significantly different to pre-vaccination.39 Conclusions from this systematic review were limited by the small number of studies which measured HI titers up to 360 days after vaccination, and potential bias from high loss-to-follow-up rates (up to 25%).
Duration of clinical protection
In parallel with these serological studies, observational studies of vaccine effectiveness (VE) have also reported a significantly increased risk of influenza with increasing time since vaccination. Most of these studies have used the test-negative design case-control study design (TND), which has become the standard method for assessing vaccine effectiveness over the past 15 years, and are conducted annually in many countries as part of influenza surveillance programs.40,41 In this study design, participants are enrolled when they present with an influenza-like-illness, and prior to virologic confirmation of influenza infection. The odds ratio for confirmed influenza is compared between participants with a history of influenza vaccination, and those without and adjusted for measured confounders such as age, co-morbidities, smoking history. This design is thought to largely overcome problems associated with the ‘healthy vaccinee effect’ – that is differences in health-seeking behavior and the risk of influenza infection between people who receive a vaccine and those who choose not to. Debate continues about analysis methodology and the appropriate selection of controls, however, these design yields estimates of vaccine effectiveness similar to clinical trials.42–44
A systematic review and meta-analysis of TND studies described higher vaccine effectiveness for all three influenza types/subtypes in the first 3 months after vaccination (days 15–90) compared with the subsequent 3 months (days 91–180).8 The majority of studies included in the systematic review were from Europe or the United States. In a ‘meta-regression’ of included studies, the proportion of older adults in each study did not predict the magnitude of VE decline though most studies were conducted in outpatient facilities, and enrolled relatively small numbers of older adults.
Following publication of this systematic review further studies have also documented intra-season waning of vaccine effectiveness. This includes a TND study of 49,272 individuals in California which enrolled only influenza vaccinated subjects. The odds ratio for influenza infection increased by 16% for each additional 28-days since vaccination, reaching an OR of 2.06 (95% CI 1.69–2.51) more than 154 days after vaccination.45 A TND study conducted in long-term care facilities in Singapore reported an adjusted VE of 59.3% (95% CI: 18.0–79.8%) against all influenza in the 15–180 days post-vaccination, but no significant VE for 181–365 days after vaccination.46
While no randomized clinical trials have directly addressed how protection changes with time following vaccination, waning efficacy was reported from a clinical trial of a live-attenuated influenza vaccination in children conducted in Asia, and of inactivated influenza vaccine and LAIV in healthy adults (aged 18–49 years).47,48
Taken together, the results of these studies suggest that to maximize VE influenza vaccination should be administered as close as possible to season onset. From a public health point of view, this has raised the concern that delaying vaccination may reduce population vaccine coverage and hence nullify any benefits.49 A clearer understanding of how VE changes with time since vaccination would help refine models and recommendations. For example, the rate of intra-season VE waning is inconsistent, perhaps reflecting differences in circulating strains or study methodologies. VE might wane linearly to zero effectiveness with time since vaccination; wane toward a threshold; or increase for the first month after vaccination, followed by a decline.
In parts of Asia where influenza seasons occur annually targeting vaccination to within 1–2 months before season onset may be optimal for the protection of vaccinated individuals (Figure 1). However, in tropical Asia where influenza is more unpredictable and occurs throughout the year the implications for vaccine practice are more complicated. The little data available indicates the current standard-dose inactivated influenza vaccine is unlikely to offer year-round protection, and alternative strategies to annual administration would be beneficial.
Vaccines with enhanced immunogenicity
Several alternative influenza vaccines, which aim to improve vaccine efficacy have been developed for older adults in recent years. This includes Fluzone® High-Dose vaccine, with four-times the regular amount of HA; adjuvanted vaccines such as FluAd®, which includes MF-59 to form an oil-in-water emulsion; and the cell-culture derived recombinant influenza vaccine Flublok®, which contains three times the regular amount of HA.
While these newer vaccines have been shown to reduce virologically confirmed infections in older adults, it is not known if they will extend the duration of clinical protection.50–52 All these vaccines are recommended for older adults by the US Advisory Committee on Immunization Practices (ACIP), but with only modest clinical benefits neither are recommended in preference to the standard inactivated vaccine.53 Further, despite significantly higher HI titers 21–28 days after vaccination with these new vaccines compared to the standard dose inactivated vaccine, evidence of improved year-round antibody persistence is lacking (Table 2).54 Access to these vaccines is also extremely limited, with none currently routinely available in an Asian country.55
Table 2.
Summary of HI persistence data following high-dose or MF59 adjuvanted influenza vaccination compared with the standard-dose vaccine in adults aged ≥65years. NS = not significant, *p ≤ 0.05.
| Day 21–42 (Seroconversion) |
Day 180 |
Day 360 |
||||||
|---|---|---|---|---|---|---|---|---|
| No | Study | Type | IIV3 | Comparator | IIV3 | Comparator | IIV3 | Comparator |
| High dose influenza vaccine (Fluzone HD) | ||||||||
| 1 | Nace, 2011–1246 | A/H1 | 27.4 | 78.2* | 28.3 | 59.7 | - | - |
| A/H3 | 10.2 | 26.2* | 9.4 | 22.3* | - | - | ||
| B | 14.3 | 25.6* | 15.4 | 22.9 | - | - | ||
| 2a | Nace, 2012-1346 | A/H1 | 50 | 45.6 | 51.8 | 46.8 | - | - |
| A/H3 | 14.2 | 23.4* | 13.4 | 24.7* | - | - | ||
| B | 17.4 | 26.0* | 18.9 | 25.3 | - | - | ||
| 3b | Kim47 | A/H1 | 35 | 71* | - | - | 22 | 28 |
| A/H3 | 29 | 81* | - | - | 18 | 24 | ||
| B | 41 | 80* | - | - | 27 | 34 | ||
| 4b | Merani48 | A/H1 | 61 | 97* | 50 | 54 | - | - |
| A/H3 | 91 | 141* | 67 | 83 | - | - | ||
| B | 102 | 107 | 84 | 63 | - | - | ||
| Adjuvanted influenza vaccine (Fluad) | ||||||||
| 5 | Minutello49 | A/H1 | 31 | 45 | - | - | 14 | 20 |
| A/H3 | 149 | 189 | - | - | 55 | 57 | ||
| B | 74 | 115* | - | - | 33 | 38 | ||
| 6c | Gasparini50 | A/H1 | 167 | 191 | NS | - | - | |
| A/H3 | 55 | 103* | NS | - | - | |||
| B | 70 | 102* | NS | - | - | |||
| 7 | Song29 | A/H1 | 81.2 | 78.8 | 35.6 | 40.7 | - | - |
| A/H3 | 92.4 | 157.7* | 28.8 | 48.4 | - | - | ||
| B | 24.1 | 34.5 | 11.0 | 16.0 | - | - | ||
| 8 | Seo51 | A/H1 | 68.1 | 92.7 | 25.4 | 32.5 | - | - |
| A/H3 | 54.7 | 102.3* | 48.3 | 63.2 | - | - | ||
| B | 12.2 | 16.5 | 10.7 | 12.0 | - | - | ||
| 9d | Frey42 | A/H1 | 141 | 198* | 68 | 71 | 52 | 49 |
| A/H3 | 337 | 544* | 91 | 123* | 54 | 70* | ||
| B | 48 | 55* | 22 | 25 | 20 | 21 | ||
| 10e | Schiefele52 | A/H1 | 79.7 | 113.4* | 39.0 | 47.4 | - | - |
| A/H3 | 70.1 | 101.4* | 37.6 | 44.3 | - | - | ||
| B | 221.2 | 239.8 | 158.0 | 158.7 | - | - | ||
aDifferent subjects included each year;
bGMT estimated from graph;
cGMT not provided;
dGMT data from day 180–360 from a persistence cohort (~6% subset);
eData at day 180 from personal communication with authors.
Six-monthly vaccination
An alternative strategy to overcoming waning year-round immunity and changes in influenza vaccine strain composition may be to simply vaccinate more regularly.
A few studies have been published over the past 40 years exploring the immune effects of a booster vaccination administered 1–3 months after the first dose in older adults. Overall, these studies found some evidence that the booster was able to ‘catch-up’ non-responders to the first vaccine administered, but offered limited increases in GMT or the proportion of subjects that were seroprotected.56–61
A systematic review in relatively immunocompromised individuals (dialysis and renal transplant) identified no significant improvement in GMTs with a booster vaccination.62 On the other hand, the TRANSGRIPE 1–2 studies conducted in ~500 solid-organ transplant recipients over the 2011–2012 northern hemisphere winter reported significant improvements in the seroprotection rate at 10 weeks for all three influenza subtypes/types in participants who received a booster vaccine.63 By 1 year after vaccination, GMT and seroprotection rates were not significantly different between the two groups. No difference in influenza infection rates were observed over the course of the study – though only five PCR-confirmed infections were identified.
Of note, this ‘prime-boost’ influenza vaccination strategy is standard practice for individuals who are (or at least are expected to be) immunologically naïve, for example, in young children (<9yrs) or in the event of an pandemic.53,64
Vaccinating older adults tropical Asia every 6-months with the standard-dose influenza vaccine is an attractive alternative strategy to those described above. This has the potential to synchronize vaccination with observed waning immunity/vaccine effectiveness and vaccine strain updates from the WHO. A clinical trial in Singapore randomized 200 older adults to annual versus six-monthly standard-dose influenza vaccination with follow up for 1 year.65 Participants who received repeat vaccination had significantly HI titers to A/H3N2 and A/H1N1 midway through the year, though titers waned and were not significantly different between groups six months later. Immune response to the vaccine after 6 months were significantly lower than the first dose for all three strains in the vaccine. Vaccine efficacy against confirmed influenza infection was not evaluated, though subjects receiving repeat influenza vaccination reported significantly fewer influenza-like-illness.
Findings were similar in an observational study of six-monthly vaccination was conducted over 2015 to 2016 in older adults in Hong Kong.66 This study indicated that individuals who received six-monthly vaccination are likely to have had significantly better protection to all three influenza types/subtypes in the influenza vaccine over the summer. However, HI responses to subsequent re-vaccination were lower in the group who had received a vaccine 6-months earlier. This apparent interference in vaccine response was also observed in measures of cell-mediated immunity, with lower influenza-specific CD4(+) responses in the repeated vaccine group.
The importance of the reduced immune response to repeated vaccination is of uncertain clinical significance. Reduced VE has been reported with sequential years vaccination in a number of observational studies. Over multiple seasons though, protection against influenza infection appears to be better with annual vaccination, rather than vaccinating less frequently and skipping years. If this interference from previous vaccination increases with six-monthly vaccination, particularly when vaccine strains have been updated, than the benefits from this strategy will be blunted. The cost-effectiveness of this strategy also needs to be clearly elucidated. An five-year study of six-monthly versus annual influenza vaccination in 400 older adults which began in 2016 in Hong Kong is expected to provide answers to some of these questions.67
Limitations
This is a narrative review of influenza in temperate and tropical Asia and attempts to address this topic more broadly than a systematic review with a focused question is able to. Some studies will have been overlooked or not included for lack of space. The limitations of the FluNet surveillance data are described in more detail above – but broadly important meta-data which documents how and where surveillance samples were collected is not available.
Conclusion
Seasonal influenza is a common infection in Asia, but an understanding of the epidemiology and burden of disease lags other regions. Alternative vaccination strategies to annual standard dose vaccination can reduce the impact of influenza, particularly in people at the highest risk for complications. The cost-effectiveness and practicality of this needs to be demonstrated in different Asian countries across a range of socio-economic conditions and climates. In addition to effectiveness the local barriers to vaccine uptake – from knowledge and attitude to financial and cultural – also need to be understood.
Funding Statement
This work was supported by the National Healthcare Group under Grant NTG/13007 and the National Medical Research Council under Grant NMRC/Fellowship/0042/2016.
Disclosure of potential conflicts of interest
BY has received honoraria from Sanofi Pasteur and Roche.
References
- 1.Cunha BA. Influenza: historical aspects of epidemics and pandemics. Infect Dis Clin North Am. 2004;18:141–55. doi: 10.1016/S0891-5520(03)00095-3. [DOI] [PubMed] [Google Scholar]
- 2.Potter CW. A history of influenza. J Appl Microbiol. 2001;91:572–79. doi: 10.1046/j.1365-2672.2001.01492.x. [DOI] [PubMed] [Google Scholar]
- 3.Nickol ME, Kindrachuk J. A year of terror and a century of reflection: perspectives on the great influenza pandemic of 1918–1919. BMC Infect Dis. 2019;19. doi: 10.1186/s12879-019-3750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lycett SJ, Duchatel F, Digard P. A brief history of bird flu. Philos Trans R Soc Lond B Biol Sci. 2019;374:20180257. doi: 10.1098/rstb.2018.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Nations Population Division | Department of Economic and Social Affairs . [accessed 2019 November 20]. https://www.un.org/en/development/desa/population/index.asp.
- 6.ESCAP Statistical Online Database. [accessed 2019 November 20] . http://www.data.unescap.org/escap_stat/#dataStories.
- 7.Kamigaki T, Chaw L, Tan AG, Tamaki R, Alday PP, Javier JB, Olveda RM, Oshitani H, Tallo VL, et al. Seasonality of influenza and respiratory syncytial viruses and the effect of climate factors in subtropical–tropical Asia using influenza-like illness surveillance data, 2010 –2012. PLoS One. 2016;11:e0167712. doi: 10.1371/journal.pone.0167712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young B, Sadarangani S, Jiang L, Wilder-Smith A, Chen MI-C. Duration of influenza vaccine effectiveness: a systematic review, meta-analysis, and meta-regression of test-negative design case-control studies. J Infect Dis. 2018;217:731–41. doi: 10.1093/infdis/jix632. [DOI] [PubMed] [Google Scholar]
- 9.WHO | FluNet . WHO. [accessed 2019 November 20]. http://www.who.int/influenza/gisrs_laboratory/flunet/en/.
- 10.Hirve S, Newman LP, Paget J, Azziz-Baumgartner E, Fitzner J, Bhat N, Vandemaele K, Zhang W. Influenza seasonality in the tropics and subtropics - when to vaccinate? PLoS One. 2016;11:e0153003. doi: 10.1371/journal.pone.0153003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman LP, Bhat N, Fleming JA, Neuzil KM. Global influenza seasonality to inform country-level vaccine programs: an analysis of WHO FluNet influenza surveillance data between 2011 and 2016. PLoS One. 2018;13:e0193263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caini S, Andrade W, Badur S, Balmaseda A, Barakat A, Bella A, Bimohuen A, Brammer L, Bresee J, Bruno A, et al. Temporal patterns of influenza A and B in tropical and temperate countries: what are the lessons for influenza vaccination?. PLoS One. 2016. Mar 31;11(3):e0152310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kottek M, Grieser J, Beck C, Rudolf B, Rubel F. World map of the köppen-geiger climate classification updated. Meteorol Z. 2006;15:259–63. doi: 10.1127/0941-2948/2006/0130. [DOI] [Google Scholar]
- 14.Alonso WJ, McCormick BJJ. EPIPOI: a user-friendly analytical tool for the extraction and visualization of temporal parameters from epidemiological time series. BMC Public Health. 2012;12:982. doi: 10.1186/1471-2458-12-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu H, Alonso WJ, Feng L, Tan Y, Shu Y, Yang W, Viboud C. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: spatio-temporal modeling of surveillance data. PLoS Med. 2013;10:e1001552. doi: 10.1371/journal.pmed.1001552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chadha MS, Potdar VA, Saha S, Koul PA, Broor S, Dar L, Chawla-Sarkar M, Biswas D, Gunasekaran P, Abraham AM, et al. Dynamics of influenza seasonality at sub-regional levels in India and implications for vaccination timing. PLoS One. 2015;10:e0124122. doi: 10.1371/journal.pone.0124122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saha S, Chadha M, Shu Y, Lijie W, Chittaganpitch M, Waicharoen S, KA L, Phengta V, Phonekeo D, Corwin A; ; . Divergent seasonal patterns of influenza types A and B across latitude gradient in Tropical Asia. Influenza Other Respir Viruses. 2016;10:176–84. doi: 10.1111/irv.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vijaykrishna D, Holmes EC, Joseph U, Fourment M, Su YC, Halpin R, Lee RT, Deng Y-M, Gunalan V, Lin X, et al. The contrasting phylodynamics of human influenza B viruses. eLife. 2015;4:e05055. doi: 10.7554/eLife.05055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck HE, Zimmermann NE, McVicar TR, Vergopolan N, Berg A, Wood EF. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data. 2018;5:180214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, JM G, Schanzer D, Cowling BJ, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet Lond Engl. 2018;391:1285–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang L, Ma S, Chen PY, He JF, Chan KP, Chow A, Ou CQ, Deng AP, Hedley AJ, Wong CM, et al. Influenza associated mortality in the subtropics and tropics: results from three Asian cities. Vaccine. 2011;29:8909–14. doi: 10.1016/j.vaccine.2011.09.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li L, Liu Y, Wu P, Peng Z, Wang X, Chen T, Wong JYT, Yang J, Bond HS, Wang L, et al. Influenza-associated excess respiratory mortality in China, 2010-15: a population-based study. Lancet Public Health. 2019;4:e473–e481. doi: 10.1016/S2468-2667(19)30163-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Minhaz Ud-Dean SM. Structural explanation for the effect of humidity on persistence of airborne virus: seasonality of influenza. J Theor Biol. 2010;264:822–29. doi: 10.1016/j.jtbi.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 2010;8. doi: 10.1371/annotation/35686514-b7a9-4f65-9663-7baefc0d63c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tamerius JD, Shaman J, WJ A, Bloom-Feshbach K, CK U, Comrie A, Viboud C. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9. doi: 10.1371/annotation/df689228-603f-4a40-bfbf-a38b13f88147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deyle ER, Maher MC, Hernandez RD, Basu S, Sugihara G. Global environmental drivers of influenza. Proc Natl Acad Sci U S A. 2016;113:13081–86. doi: 10.1073/pnas.1607747113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Litvinova M, Liu Q-H, Kulikov ES, Ajelli M. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc Natl Acad Sci U S A. 2019;116:13174–81. doi: 10.1073/pnas.1821298116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gautret P, Angelo KM, Asgeirsson H, Duvignaud A, van Genderen PJJ, Bottieau E, Chen LH, Parker S, Connor BA, Barnett ED, et al. International mass gatherings and travel-associated illness: A GeoSentinel cross-sectional, observational study. Travel Med Infect Dis. 2019;101504. doi: 10.1016/j.tmaid.2019.101504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao X, Ning Y, Chen MI-C, Cook AR. Individual and Population Trajectories of Influenza Antibody Titers Over Multiple Seasons in a Tropical Country. Am J Epidemiol. 2018;187:135–43. doi: 10.1093/aje/kwx201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wei VWI, Wong JYT, Perera RAPM, Kwok KO, Fang VJ, Barr IG, Peiris JSM, Riley S, Cowling BJ, et al. Incidence of influenza A(H3N2) virus infections in Hong Kong in a longitudinal sero-epidemiological study, 2009-2015. PLoS One. 2018;13:e0197504. doi: 10.1371/journal.pone.0197504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wen F, Bedford T, Cobey S. Explaining the geographical origins of seasonal influenza A (H3N2). Proc R Soc B Biol Sci. 2016;283. doi: 10.1098/rspb.2016.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russell CA, Jones TC, Barr IG, Cox NJ, Garten RJ, Gregory V, Gust ID, Hampson AW, Hay AJ, Hurt AC, et al. The global circulation of seasonal influenza A (H3N2) viruses. Science. 2008;320:340–46. doi: 10.1126/science.1154137. [DOI] [PubMed] [Google Scholar]
- 33.Bedford T, Riley S, Barr IG, Broor S, Chadha M, Cox NJ, Daniels RS, Gunasekaran CP, Hurt AC, Kelso A, et al. Global circulation patterns of seasonal influenza viruses vary with antigenic drift. Nature. 2015;523:217–20. doi: 10.1038/nature14460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheldenkar A, Lim F, Yung CF, Lwin MO. Acceptance and uptake of influenza vaccines in Asia: a systematic review. Vaccine. 2019;37:4896–905. doi: 10.1016/j.vaccine.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 35.Zhao X, Fang VJ, Ohmit SE, Monto AS, Cook AR, Cowling BJ. Quantifying protection against influenza virus infection measured by hemagglutination-inhibition assays in vaccine trials. Epidemiol Camb Mass. 2016;27:143–51. doi: 10.1097/EDE.0000000000000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petrie JG, Ohmit SE, Johnson E, Truscon R, Monto AS. Persistence of antibodies to influenza hemagglutinin and neuraminidase following one or two years of influenza vaccination. J Infect Dis. 2015;212:1914–22. doi: 10.1093/infdis/jiv313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Song JY, Cheong HJ, Hwang IS, Choi WS, Jo YM, Park DW, Cho GJ, Hwang TG, Kim WJ. Long-term immunogenicity of influenza vaccine among the elderly: risk factors for poor immune response and persistence. Vaccine. 2010;28:3929–35. doi: 10.1016/j.vaccine.2010.03.067. [DOI] [PubMed] [Google Scholar]
- 38.Hsu JP, Zhao X, Chen MIC, Cook AR, Lee V, Lim WY, Tan L, Barr IG, Jiang L, Tan CL, et al. Rate of decline of antibody titers to pandemic influenza A (H1N1-2009) by hemagglutination inhibition and virus microneutralization assays in a cohort of seroconverting adults in Singapore.. BMC Infect Dis. 2014;14. doi: 10.1186/1471-2334-14-414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Young B, Zhao X, Cook AR, Parry CM, Wilder-Smith A, Cheng I. Do antibody responses to the influenza vaccine persist year-round in the elderly? A systematic review and meta-analysis. Vaccine. 2017;35:212–21. [DOI] [PubMed] [Google Scholar]
- 40.Darvishian M, van den Heuvel ER, Bissielo A, Castilla J, Cohen C, Englund H, Gefenaite G, WT H, la Bastide-van Gemert S, Martinez-Baz I, et al. Effectiveness of seasonal influenza vaccination in community-dwelling elderly people: an individual participant data meta-analysis of test-negative design case-control studies. Lancet Respir Med. 2017;5:200–11. [DOI] [PubMed] [Google Scholar]
- 41.Foppa IM, Haber M, Ferdinands JM, Shay DK. The case test-negative design for studies of the effectiveness of influenza vaccine. Vaccine. 2013;31:3104–09. doi: 10.1016/j.vaccine.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 42.Feng S, Cowling BJ, Sullivan SG. Influenza vaccine effectiveness by test-negative design - Comparison of inpatient and outpatient settings. Vaccine. 2016;34:1672–79. doi: 10.1016/j.vaccine.2016.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Feng S, Cowling BJ, Kelly H, Sullivan SG. Estimating influenza vaccine effectiveness with the test-negative design using alternative control groups: a systematic review and meta-analysis. Am J Epidemiol. 2018;187:389–97. doi: 10.1093/aje/kwx251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sullivan SG, Tchetgen Tchetgen EJ, Cowling BJ. Theoretical basis of the test-negative study design for assessment of influenza vaccine effectiveness. Am J Epidemiol. 2016;184:345–53. doi: 10.1093/aje/kww064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ray GT, Lewis N, Klein NP, Daley MF, Wang SV, Kulldorff M, Fireman B. Intra-season Waning of Influenza Vaccine Effectiveness. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018. doi: 10.1093/cid/ciy770. [DOI] [Google Scholar]
- 46.Ng Y, Nandar K, Chua LAV, Mak TM, Foo K, Muhammad IR, Low CKK, Ma S, Ooi SPL, Lin RTP, et al. Evaluating the effectiveness of the influenza vaccine during respiratory outbreaks in Singapore’s long term care facilities, 2017. Vaccine. 2019;37:3925–31. doi: 10.1016/j.vaccine.2019.03.054. [DOI] [PubMed] [Google Scholar]
- 47.Tam JS, Capeding MRZ, Lum LCS, Chotpitayasunondh T, Jiang Z, Huang L-M, Lee BW, Qian Y, Samakoses R, Lolekha S, et al. Efficacy and safety of a live attenuated, cold-adapted influenza vaccine, trivalent against culture-confirmed influenza in young children in Asia. Pediatr Infect Dis J. 2007;26:619–28. doi: 10.1097/INF.0b013e31806166f8. [DOI] [PubMed] [Google Scholar]
- 48.Petrie JG, Ohmit SE, Truscon R, Johnson E, TM B, MZ L, Eichelberger MC, AS M. Modest waning of influenza vaccine efficacy and antibody titers during the 2007-2008 influenza season. J Infect Dis. 2016;214:1142–49. doi: 10.1093/infdis/jiw105. [DOI] [PubMed] [Google Scholar]
- 49.Ferdinands JM, Alyanak E, Reed C, Fry AM. Waning of influenza vaccine protection: exploring the trade-offs of changes in vaccination timing among older adults. Clin Infect Dis Off Publ Infect Dis Soc Am. 2019. doi: 10.1093/cid/ciz452. [DOI] [PubMed] [Google Scholar]
- 50.DiazGranados CA, Dunning AJ, Kimmel M, Kirby D, Treanor J, Collins A, Pollak R, Christoff J, Earl J, Landolfi V, et al. Efficacy of high-dose versus standard-dose influenza vaccine in older adults. N Engl J Med. 2014;371:635–45. doi: 10.1056/NEJMoa1315727. [DOI] [PubMed] [Google Scholar]
- 51.Dunkle LM, Izikson R, Patriarca P, Goldenthal KL, Muse D, Callahan J, MM C. Efficacy of recombinant influenza vaccine in adults 50 years of age or older. N Engl J Med. 2017;376:2427–36. doi: 10.1056/NEJMoa1608862. [DOI] [PubMed] [Google Scholar]
- 52.Frey SE, Aplasca-De Los Reyes MR, Reynales H, Bermal NN, Nicolay U, Narasimhan V, Forleo-Neto E, Arora AK. Comparison of the safety and immunogenicity of an MF59®-adjuvanted with a non-adjuvanted seasonal influenza vaccine in elderly subjects. Vaccine. 2014;32:5027–34. doi: 10.1016/j.vaccine.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Kim DK, Riley LE, Hunter P. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older — United States, 2018. Morb Mortal Wkly Rep. 2018;67:158–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ng TWY, Cowling BJ, Gao HZ, Thompson MG. Comparative immunogenicity of enhanced seasonal influenza vaccines in older adults: a systematic review and meta-analysis. J Infect Dis. 2019;219:1525–35. doi: 10.1093/infdis/jiy720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chang L-J, et al. Safety and immunogenicity of high-dose quadrivalent influenza vaccine in adults ≥65 years of age: a phase 3 randomized clinical trial. Vaccine. 2019;37:5825–34. doi: 10.1016/j.vaccine.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 56.Feery BJ, Cheyne IM, Hampson AW, Atkinson MI. Antibody response to one and two doses of influenza virus subunit vaccine. Med J Aust. 1976;1:188–89. [PubMed] [Google Scholar]
- 57.Gross PA, Weksler ME, Quinnan GV, Douglas RG, Gaerlan PF, Denning CR. Immunization of elderly people with two doses of influenza vaccine. J Clin Microbiol. 1987;25:1763–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keren G, Segev S, Morag A, Zakay‐Rones Z, Barzilai A, Rubinstein E. Failure of influenza vaccination in the aged. J Med Virol. 1988;25:85–89. doi: 10.1002/jmv.1890250112. [DOI] [PubMed] [Google Scholar]
- 59.Mancini G, Arangio-Ruiz G, Bianchi B, Diana L, Macchia T, Donatelli I, MR C, Campitelli L, Ruggieri A. Influenza vaccination in elderly residents in nursing homes: immune response to trivalent and monovalent inactivated influenza virus vaccine in the season 1986-87. Eur J Epidemiol. 1989;5:214–18. doi: 10.1007/BF00156833. [DOI] [PubMed] [Google Scholar]
- 60.Fagiolo U, Amadori A, Cozzi E, Bendo R, Lama M, Douglas A, Palu G. Humoral and cellular immune response to influenza virus vaccination in aged humans. Aging Milan Italy. 1993;5:451–58. [DOI] [PubMed] [Google Scholar]
- 61.Cools HJM, Gussekloo J, Remmerswaal JEM, Remarque EJ, Kroes ACM. Benefits of increasing the dose of influenza vaccine in residents of long-term care facilities: a randomized placebo-controlled trial. J Med Virol. 2009;81:908–14. doi: 10.1002/jmv.v81:5. [DOI] [PubMed] [Google Scholar]
- 62.Liao Z, Xu X, Liang Y, Xiong Y, Chen R, Ni J. Effect of a booster dose of influenza vaccine in patients with hemodialysis, peritoneal dialysis and renal transplant recipients: A systematic literature review and meta-analysis. Hum Vaccines Immunother. 2016;12:2909–15. doi: 10.1080/21645515.2016.1201623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cordero E, Roca-Oporto C, Bulnes-Ramos A, Aydillo T, Gavaldà J, Moreno A, Torre-Cisneros J, JM M, Fortun J, Muñoz P, et al. Two doses of inactivated influenza vaccine improve immune response in solid organ transplant recipients: results of TRANSGRIPE 1-2, a randomized controlled clinical trial. Clin Infect Dis Off Publ Infect Dis Soc Am. 2017;64:829–38. doi: 10.1093/cid/ciw855. [DOI] [PubMed] [Google Scholar]
- 64.Czako R, Subbarao K. Refining the approach to vaccines against influenza A viruses with pandemic potential. Future Virol. 2015;10:1033–47. doi: 10.2217/fvl.15.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Young B, Sadarangani S, Haur SY, Yung CF, Barr I, Connolly J, Chen M, Wilder-Smith A. Semiannual versus annual influenza vaccination in older adults in the tropics: an observer-blind, active-comparator-controlled, randomized superiority trial. Clin Infect Dis Off Publ Infect Dis Soc Am. 2019;69:121–29. doi: 10.1093/cid/ciy836. [DOI] [PubMed] [Google Scholar]
- 66.Tam YH, Valkenburg SA, Perera RA, Wong JH, Fang VJ, Ng TW, Kwong AS, Tsui WW, Ip DK, Poon LL, et al. Immune responses to twice-annual influenza vaccination in older adults in Hong Kong. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66:904–12. doi: 10.1093/cid/cix900. [DOI] [PubMed] [Google Scholar]
- 67.Immunogenicity of Twice-annual Influenza Vaccination in Older Adults in Hong Kong - Full Text View - ClinicalTrials.gov. [accessed 2019 November 20] . https://clinicaltrials.gov/ct2/show/NCT02957890.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- United Nations Population Division | Department of Economic and Social Affairs . [accessed 2019 November 20]. https://www.un.org/en/development/desa/population/index.asp.


