ABSTRACT
This study engaged health professionals in in-depth, semi-structured interviews to explore their opinions concerning the issues surrounding vaccine hesitancy in Malaysia and strategies to improve vaccination to stamp the rise of vaccine preventable diseases (VPDs). Opinions on how to address the resurgence of VPDs in the era of increasing vaccine hesitancy were obtained. Eight health professionals, including geriatricians, pediatricians, microbiologists, public health specialists, and family medicine specialists were interviewed. The influence of anti-vaccination propaganda, past-experience of adverse event following immunization (AEFI), perceived religious prohibition, a belief that traditional complementary and alternative medicine (TCAM) use is safer, pseudoscience beliefs, and anti-vaccine conspiracy theories were identified as reasons for refusing to vaccinate. The interplay of social, cultural and religious perspectives in influencing perceived religious prohibition, pseudoscience beliefs, and the use of TCAM contributing to vaccine refusal was found. Five broad themes emerged from the health professionals regarding strategies to address vaccine hesitancy, including establishing an electronic vaccination registry, increasing public awareness initiatives, providing feedback to the public on the findings of AEFI, training of front-line healthcare providers, and banning the dissemination of anti-vaccine information via social media. With regards to identifying strategies to address the resurgence of VPDs, mandatory vaccination received mixed opinions; many viewed supplementary immunization activity and the prevention of travel and migration of unvaccinated individuals as being necessary. In conclusion, the present study identified unique local cultural, traditional and religious beliefs that could contribute to vaccine hesitancy in addition to issues surrounding vaccination refusal similarly faced by other countries around the world. This information are important for the formulation of targeted intervention strategies to stamp vaccine hesitancy in Malaysia which are also a useful guide for other countries especially in the Southeast Asia region facing similar vaccine hesitancy issues.
KEYWORDS: Vaccine hesitancy, Asia
Introduction
The National Immunization Programme (NIP) in Malaysia which is integrated in the mother-and-child health services was introduced in the early 1950s. The NIP was designed based on the World Health Organization (WHO) Expanded Programme on Immunization (EPI). The EPI recommends that all countries immunize against 6 childhood diseases; however, Malaysia has expanded its NIP to 12 major childhood diseases. The 12 preventable diseases listed under the NIP include diphtheria, Haemophilus influenzae type B, hepatitis B, human papillomavirus, Japanese encephalitis, measles, mumps, pertussis, poliomyelitis, rubella, tetanus, and tuberculosis. Except for Japanese encephalitis vaccination, which is not obligatory in other parts of Malaysia except Sarawak, vaccination via the Immunization Schedule of the NIP in Malaysia is provided free-of-charge in all government clinics and hospitals across the country. Under this programme, the country has achieved more than 90% vaccination coverage among infants and young children.1 Data from the vaccination module in the National Health and Morbidity Survey (NHMS) 2016 showed that the following were among the reasons for incomplete or non-uptake of vaccination: 1) issues with healthcare facilities, such as a shortage of vaccine stocks; and 2) personal reasons such as time constraints, overlooked clinic/hospital appointments, geographical barriers, refusing vaccines, and concern that vaccines are non-halal (permissible under Islamic law), as well as previous experience of adverse effects.2
Based on the high percentage of vaccine coverage, Malaysia is expected to have achieved full immunity to all the vaccine-preventable childhood diseases (VPDs). The steady rise in the number of reported increase in cases of VPDs, especially measles, coupled with several deaths of toddlers from diphtheria have raised concern about the possible rise in vaccine hesitancy in Malaysia.3 Malaysia saw the rise of measles cases (892%) between 2013 and 2018. Among the non-immunized individuals, the number of measles cases rose from 125 cases (69%) in 2013 to 1467 cases (76%) in 2018, including six deaths.4 Other VPD-related deaths include four due to diphtheria and 19 due to pertussis in non-immunized individuals in Malaysia.5 While there have been a number of reports suggesting the possible factors contributing toward the rise, these factors on their own could be misleading as they do not explore the wider context involving local cultural, traditional and religious health believes, perceptions and misinformation.6 Hence, there is an urgent need to identify the various reasons behind vaccine hesitancy in the local Malaysia context to stamp the rise in VPDs.
The parental vaccine hesitancy spectrum that has been studied and reviewed extensively in western literatures;7–9 only a few studies, nevertheless, have been conducted in Asian countries, in particular in Southeast Asia, where social, cultural, traditional, and religious elements strongly influence health-seeking behaviors10 and this may include vaccination. Malaysia, a country in Southeast Asia, is a Muslim majority country with a mix of Malay, Chinese, Indian and European cultural influences. In Malaysia, there have been several but small-scale studies and reviews describing the demographics of vaccine-hesitant parents. The prevalence of vaccine hesitancy in the general Malaysian population is unknown. However, the prevalence of vaccine hesitancy in a small sample of urban parents was near 12%.11 A broad spectrum of universal reasons for vaccine hesitancy includes religion, safety concerns, personal beliefs, and preferences toward alternative medicine were highlighted.11-13 The immunization module record in the NHMS 20162 did not document detailed reasons for vaccine hesitancy among those with incomplete or non-uptake of vaccination. To date, there have been no thorough investigations on the specific reasons that underpin the refusal of individuals or groups to vaccinate among the Malaysian population. Exploring detailed reasons behind vaccine refusal is needed to provide information for the authorities to formulate targeted interventions to address vaccine hesitancy in Malaysia.
In order to address this gap, we conducted a qualitative in-depth interview investigating the opinions of health professionals with regards to issues surrounding vaccine hesitancy in Malaysia and strategies to overcome it. The second objective of this study was to gather opinions from health professionals on how to address the resurgence of VPDs in the climate of increasing vaccine hesitancy. Perspective from health professionals may be of advantage as vaccine hesitancy is a sensitive issue, and vaccine hesitant parents or caregivers may hesitate to provide true information or to be interviewed.
Method
We undertook a qualitative study in which we interviewed academics, researchers, and physicians in a teahing hospital located in Kuala Lumpur, Malaysia. In-depth, face-to-face semi-structured interviews were conducted. The study participants were recruited through convenient sampling method. Experts from diverse specialties were approached to enhance the representation of participants from diverse fields. Experts with interest, experience or research in subjects related to patients or parental behavior regarding vaccine acceptance were included in the study. Study information sheets detailing the purpose of the study, methodology, and voluntary and confidentiality aspects of the study were provided to the health professionals prior to commencing the interviews. Informed consent was documented by means of a written, signed and dated informed consent form. To facilitate the interview, a semi-structured interview protocol was developed that had three major questions: 1) what are the reasons behind vaccine hesitancy, 2) what strategies would you recommend for countering vaccine hesitancy, and 3) what is your opinion on how to address the resurgence of VPDs in the country?
Interviews were conducted in English and were audio-recorded and transcribed verbatim. Interviews were conducted as needed until saturation was reached. The data were analyzed using thematic analysis (NVivo software, version 11) to establish meaningful themes generated from the interviews. The transcripts were coded based on categories of themes in the study aims and interview guide. Emerging subthemes within those categories were identified and each was assigned a specific code. Two researchers worked together to identify the final themes, which were tested against the coded transcripts to ensure that they were representative of the data. A final review of emergent themes was conducted by the three project team researchers who agreed on the final list of themes. Illustrative quotes were selected to highlight central themes. Ethical approval was granted by the Medical Ethics Committee, University Malaya Medical Center, Kuala Lumpur, Malaysia (MEC Ref. No UM.TNC2/UMREC – 607).
Results
Between 24 April and 21 May 2019, interviews were conducted with a total of eight health professionals (3 females and 5 males); the group consisted of geriatricians (2 persons), pediatricians (2 persons), microbiologists (2 persons), a public health specialist (1 person), and a family medicine specialist (1 person). The age range of health professionals was 29- to 62-year-old.
Reasons surrounding vaccine hesitancy
Based on the collective opinions from the participating health professionals, six main themes surrounding the reasons for vaccine hesitate were identified. (Figure 1).
Figure 1.

Themes surrounding the reasons for vaccine hesitancy.
The participants viewed vaccine hesitation as being influenced by hearsay or anti-vaccination propaganda, which lead to negative perceptions about vaccines, both from social media and by word of mouth. They may not have experienced or witnessed adverse events following vaccination but have firm belief in information disseminated by friends and/or the media. A health professional regarded this group as having a lack of scientific knowledge on vaccination and thus, can be easily swayed by friends or social media.
All health professionals shared the opinion of vaccines are mostly safe, but acknowledged that there were instances of mild reactions in some cases. After an adverse event following immunization (AEFI) experienced by their child, the parents subsequently did not complete the vaccination schedule and did not consent their other children to have any subsequent vaccinations. There are also parents who deliberately create or exaggerate the symptoms or erroneously consider unrelated clinical events as that being vaccination-associated. There are also parents who claimed that their children received vaccines but developed the illness that the vaccine is supposed to protect against. These experiences raised doubts about the safety and efficacy of vaccination. Participants viewed that the individual’s actual experiences with AEFI and vaccine inefficacy exert a powerful influence on other parents.
There was also an opinion that vaccine hesitancy may have been derived from perceived religious prohibition to vaccination. Most of the concerns were regarding porcine content in vaccines, or their derivatives, being used to make vaccines. Health professionals believe that issues surrounding religion and vaccination are very prominent among the Muslim community in Southeast Asia, particularly in Malaysia and Indonesia.
They believe that vaccines are haram (prohibited because they contain aborted foetal DNA and lots of animal cells. They are not aware that not all vaccines contain porcine gelatine. All of the vaccines in our national immunisation schedule are free from porcine substances. They are not aware of the production process.
The health professionals noted that there are groups in the population with a general mistrust in science and scientists, and who instead hold high regards for TCAMs in disease prevention and treatment. This group believes that traditional medicine treatments and the use of natural remedies that have been used for generations are safer than modern medicine. Some also believe that taking high doses of vitamins is adequate and safer than receiving vaccines.
They claimed that measles can be cured with high doses of vitamin C. They can cure diphtheria with high doses of vitamin C and vitamin D.
The health professionals also identified a group who consider themselves as TCAM practitioners, but they are actually marketers of health products, which they claimed as alternatives to vaccination. This group may or may not be vaccine-hesitant individuals, but are opportunists who would help disseminate anti-vaccination ideas along with the promotion of sales of traditional and herbal remedies or vitamin supplements as alternatives to vaccines.
There are also alternative medicine practitioners; they are selling these vitamins for instance and said that these can cure vaccine-preventable diseases. They disseminate false information to convince other people not to vaccinate but to buy their products. They are very vocal, a lot in social media compared to real life.
Health professionals also noted that, among the TCAM believers, there are also people who believe in natural immunity and argue that the immunity gained via natural infection provides better protection than that provided by vaccinations. One health professional stated that while it is true that natural immunity lasts longer than vaccine-induced immunity in some cases, the risks of natural infection far outweigh the risks of vaccination.
The argument is that it is better to have the natural infection. But, natural infection, for instance polio, will cause lifelong paralysis. Some other infections may cause death. For instance, the recent death of a toddler due to diphtheria was because the child had never been immunised since birth.
Another group of vaccine-hesitant people is those labeled by health professionals as pseudoscience believers. These individuals claimed they favor “homeopathic vaccine” over the conventional vaccines. One health professional described people who hold onto this pseudoscientific belief are not necessarily against vaccination for prevention of diseases but favor the idea of protecting their child from diseases using “homeopathic vaccines” as the conventional vaccines consisted of toxic ingredients. Similar to TCAM practitioners, they view vaccines as containing harmful ingredients or chemicals that are dangerous for young children. The health professional further illustrated that they use homeopathic dilutions derived from plant substances as alternatives to commercially available vaccines. Many of these “homeopathic vaccines” are being promoted on social media platforms. The widespread use of social media in Malaysia facilitates the dissemination of support for “homeopathic vaccines” as an alternative to conventional vaccines among a small minority of the population. The health professionals also noted that there is an increasing number of pseudoscience practitioners among the supposedly highly educated people.
Several health professionals observed that vaccine skeptics include a minority group who holds firm irrational beliefs in conspiracy theories. The first is a conspiracy involving the profiteering motive of all parties along the vaccination supply chain, including pharmaceutical companies, authorities, and physicians. The second conspiracy theory is the belief that vaccination is a Western conspiracy against Muslims or a form of anti-Muslim plot.
Some believe that vaccine companies are controlled by the Jews, and that the Jews will try to destroy Muslim people in the world by giving them vaccines.
Countering vaccine hesitancy
Themes that emerged from the analysis related to strategies to counteract vaccine hesitancy in Malaysia are illustrated in Figure 2.
Figure 2.

Strategies to counteract vaccine hesitancy.
The majority of health professionals stated that there is a need to improve the current national vaccination registry. It is a challenge for medical professionals to track and contact those refusing vaccines as the population is large especially in urban areas. Population movement between rural and urban areas further compounded this problem.
In the klinik desa (rural clinics), that take care of 10,000 people, for instance, if the midwives and public health nurses are all from the same community and know each other, they will do home visits to convince them. Therefore, there is no problem in rural areas. The problem is with urban areas because the population is very large and mobile. It is difficult to catch them.
I think the system of vaccination is in place. But we don’t have a kind of more organised system to deal with vaccine refusals. We have a system which depends on parents bringing their children to hospitals or clinics. We don’t have a registry, and we don’t have a health system that has an outreach to make home visits to families where children are not brought in for vaccination.
In addressing vaccine-hesitancy groups who are influenced by hearsay or negative rumors, most of the health professionals suggested to aggressively conduct engagement activities to provide accurate facts on vaccination, the importance of protecting individuals against VPDs and to highlight to the public of their responsibilities to protect others from acquiring these diseases. It is imperative to address vaccine hesitancy associated with a lack of knowledge or ignorance as it could enlighten them and enable them to help support vaccination campaigns against the skeptics.
The public should be informed that it is their responsibility to get vaccinated because vaccination relies on a herd immunity percentage. If it drops down to certain percentage, the whole population is at risk.
When you receive a vaccine, you are not treating one person, but you are treating thousands of people, maybe hundreds of thousands of people. The public should be made aware.
In addressing the reluctance to vaccinate children following events where children suffer a reaction to vaccination, health professionals viewed parents reporting AEFIs should be provided with proper feedback on the outcome of AEFIs investigation to clear their misconceptions. Responding to parents’ concerns over vaccination-related adverse effects will also prevent the misunderstanding of erroneous adverse effects associated with vaccination and disseminating false information to others.
The current system is focused on collecting information of AEFIs, but there is no proper feedback to the parents. Therefore, this has caused parents some doubts in vaccination. Parents were wondering whether the report was done or not. This has also caused doubts in our system, and they think that the Ministry of Health is not reporting adverse events following immunisation. They claim that AEFIs are underreported by KKM (Ministry of Health Malaysia).
The health professionals were of the opinion that doctors as well as other medical professionals play an important role in counseling vaccine-hesitant parents and fostering vaccine acceptance, especially in clinical settings. In this regard, the health professionals’ view was that doctors should be equipped with in-depth knowledge and good communication skills when addressing the concerns of vaccine-hesitant parents, to encourage them toward vaccine acceptance.
We need to have our frontline staff and different levels of healthcare professionals equipped on how to communicate with patients about vaccination and answer the arguments brought up by patients, to effectively counsel and convince.
The WHO has guidelines on how to address vaccine refusal on both an individual and public basis. They can refer to these guidelines.
Health professionals in this study also noted that there is a minority group of doctors who are vaccine-hesitant themselves, and not only do not recommend vaccines to their patients but also promote anti-vaccine views to their patients. Health professionals also noted that some doctors may also play a role in falsely signing and endorsing the patient’s vaccination record. Health professionals suggest that it is best to impart a strong emphasis of the importance of vaccination at the medical school teaching level. The health professionals stated that all aspects, including knowledge on the process of vaccine development, understanding public refusal and vaccine hesitancy issues, should be incorporated into the medical curriculum in order to impart positive attitudes toward vaccination, enabling them to address patient vaccine hesitancy or refusal in their future practice.
According to the health professionals, currently those who are promoting views against vaccination or also known as anti-vaxxers in the country are still free to disseminate anti-vaccine contents via social media. They are urging for more stringent restrictions to curtail the spread of anti-vaccine information on social media in Malaysia. They stressed that it is important to stop these messages because anti-vaccine propaganda has a snowball effect and could garner a massive influence on the public. According to the health professionals it is crucial to ban social media from disseminating inaccurate and anti-vaccination information. They also viewed that responding to erroneous beliefs or vaccine misinformation on social media is important if banning these messages is not immediately possible. One health professional stated that there is a need for intensive responses, especially from doctors or medical professionals, over the anti-vaccine messages on social media. However, most health professionals acknowledged that there is a lack of medical professionals whom have been trained with effective communication skills to engage the public on the internet and social media.
We are also trying to approach Facebook to block the accounts of anti-vaxxers who are promoting anti-vaccine information.
On social media, you need to have the skills to entice people to read. We don’t have many experts in this. Furthermore, it is not easy for professionals to balance ethics and information dissemination on social media.
Addressing the resurgence of vaccine-preventable diseases
Some health professionals believe that vaccine enforcement or mandatory vaccination is an effective way to prevent the resurgence of VPDs. Nevertheless, views about mandatory vaccination received mixed responses. Some believe that vaccination should be made compulsory at best, but other health professionals are concerned that legislation to make vaccination mandatory may raise conflicts among the different societies in Malaysia. Some health professionals indicated that mandatory vaccination may be an issue for people living in geographically isolated or remote areas, such as the Aborigine population, locally known as Orang Asli, whereby many are still not vaccinated due to difficulty to access the population. In contrast, some health professionals indicated that it is crucial for the country to set up a computerized vaccination registry to track each child’s vaccination status, identify vaccine defaulters and subsequently carry out outreach vaccinations along with education to achieve full vaccination coverage. The current vaccination record is in the form of a printed checklist on the vaccination book (Figure 3). The health experts also stated that vaccination records, which are signed or endorsed by the physician administering the vaccines to children, can be easily falsified. Therefore, establishing a proper vaccination registry should be made a priority. The health professionals further stressed that should vaccination become mandatory, it is crucial for the country to first establish a computerized vaccination registry.
I don’t suggest mandatory vaccination; that is very cruel. You can go a bit of the nudge or pushing; for instance, “if you don’t vaccinate your child, your child cannot attend public school, and you may have to use home-schooling”. We don’t want to deprive the children from the right to be educated, but we also don’t want to harm other children. Perhaps … .my suggestion is if you don’t vaccinate your child you won’t get any subsidies for your healthcare. We can suggest stripping off some of the privileges of the parents, rather than pushing the act onto the child. They can be charged with the Negligence of the Child Act. The Ministry of Health is currently seeing these suggestions but the debate is ongoing.
The best way is to have a digital vaccination registry for every child, and information which goes to the server; it can be stored on their identity card, inside the chip. Once the system is there, we can push for mandatory vaccination because we have a way to recognise who has been truly vaccinated and who has not.
Figure 3.
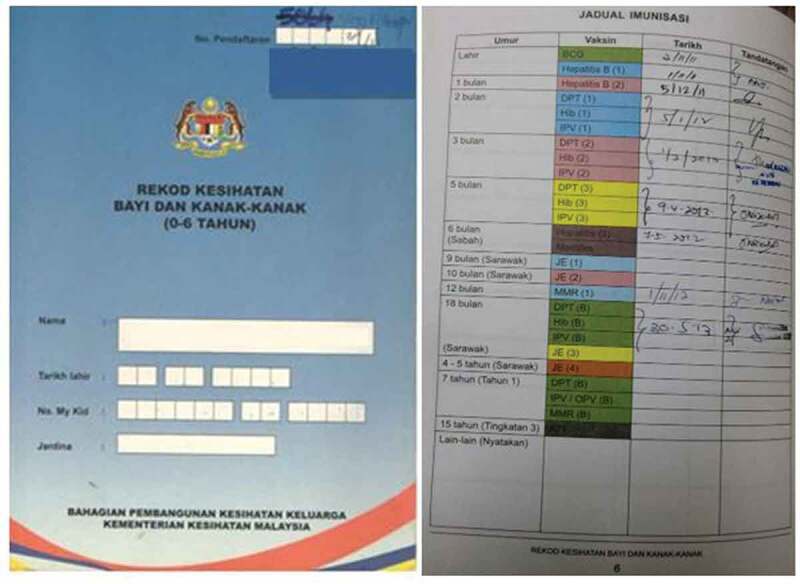
Immunization checklist in the immunization book.
All of the health professionals interviewed agreed that, despite high vaccination coverage in Malaysia, the high influx of legal and illegal foreign workers into the country in recent years, posed a risk of the resurgence of VPDs. Many consider it necessary for the NIP to also include children of the migrants. There is also a suggestion to check the vaccination history of migrants before they are allowed to enter the country.
Our statistics show that we have good vaccination coverage. So, I think as long as they are in Malaysia, the National Immunisation Program should also include foreign children. If we want to protect our citizens, we have to vaccinate them.
My suggestion is screening at the point of entry. It would be good if our Health Ministry could implement the screening of migrants, as well as looking at their childhood vaccination schedule received in their origin countries.
Secondly, the health professionals reported that there is a need to strengthen our routine vaccination through supplementary immunization activity (SIA). They noted that the country is doing well in this regard and is currently implementing health education and measles SIA in low coverage and outbreak areas to tackle the most susceptible groups. They also indicated that SIA should be intensified and should incorporate vaccines for other VPDs. The issue of revaccinating older adults for VPDs of children emerged in the midst of a discussion regarding the need for revaccination. It is understood that vaccination of the elderly may have waned over the years, possibly predisposing them to childhood VPDs. However, the health professionals in this study have mixed opinions regarding revaccinating older adults. Some noted that although there is no current directive from the WHO regarding vaccinating the elderly, and likewise in Malaysia, health professionals in geriatric medicine view the benefit of vaccinating the elderly far outweigh the potential risks of infection with the global resurgence of VPDs.
Our population is very mobile and we have a very large migrant population, so there is a need for revaccination. “In particular, if a person is going for Hajj, they need to vaccinate again. The Malaysian Ministry of Health encourages prospective Hajj pilgrims to take additional immunisations.
The elderly should be revaccinated, not only because of the resurgence, but actually as part of the vaccination schedule which is a continuation from childhood. For instance DTaP should be continued.
Vaccination is cost effective for the elderly; if you pay for vaccinations, you save the high hospitalisation costs. In some countries, vaccination of the elderly is funded by charities.
Although some view vaccination of the elderly as being beneficial in terms of preventing them from clogging up the health system, there were also some with the opinion that policies for vaccination of the elderly against VPDs of children warrant stronger evidence of the effectiveness, cost effectiveness of vaccination versus treatment. When probed about whether vaccines may pose a substantial safety risk in the elderly, all health professionals stated that vaccinations in the population aged 65 years and older are safe; nevertheless, they agreed that vaccines may be less immunogenic and effective in the elderly as their ability to mount immune responses may have decreased with aging. As such, one health professional stated that revaccinating the elderly should only be carried out if it is shown to be cost effective.
Discussion
Perspectives given by the health professionals from various fields in the present study provide a comprehensive overview of the issues surrounding vaccine hesitancy in Malaysia, some of which are unique to the context of the Asian culture and traditions. A highlight of utmost importance from this study is the urgent need to institute a mechanism to effectively respond to the proliferation of negative messages about vaccination in the country. It is clear that these negative messages play an important role in influencing many parents, leading to reduced vaccination coverage.14 Public awareness initiatives coupled with effective communication with the public is crucial to clarify misinformation about vaccines and vaccination. As social media is a powerful tool in propagating anti-vaccine sentiments, it is suggested that the government should enact a law to prevent anti-vaccine activists from disseminating misinformation via social media. The present study also showed that proper responses to AEFIs and feedback communication to the public are very much lacking in Malaysia. This is probably true as well in many developing countries and those in the Southeast Asia region. Building trust in vaccination program is important; therefore, if responses to reports of AEFIs are not handled appropriately, this may erode public confidence in vaccination.15
A large population of Southeast Asian countries practices Islam. Malaysia, being a Muslim-majority country, faces a number of issues related to vaccines being religiously not permissible or “haram”. While most are not against the idea of having their children vaccinated, there is a strong concern that the vaccines are not in compliance with the strict permissible standard outlined in Islam. The utmost major concern is the possible presence of animal products especially porcine or porcine-derived components. Currently, there are no vaccines that have been fully certified as Halal by the Malaysia Islamic Council (JAKIM), available for use in Malaysia. The Ministry of Health Malaysia has adopted a stand articulated by the edicts or fatwas implying that the currently available vaccines for VPDs in children are permissible to be administered to Muslims.16 As such, the role of religious leaders or “Ulama” is essential to address vaccine hesitancy associated with the vaccine being perceived as “Haram”. It is imperative that the “Ulama” and the Fatwa Council members are informed of the current state of technologies involved in vaccine manufacturing so that they could help allay the public fear.17,18
In addition to the sizable population of Muslims, the South-East Asia region also has a rich tradition in TCAM practices. TCAM is widely practiced in parallel to conventional Western medicine. Studies have shown that at least 70% of the Malaysian population will use traditional complementary medicine in their life.19 Unlike previous reports that show the common use of TCAM to remedy a wide range of illnesses, it is interesting to note that the present TCAM has also been extended as an alternative to vaccination. In the present study, health professionals interviewed raised an interesting concept that has not been discussed much before, the use of “homeopathic vaccines” in TCAM as an alternative to conventional vaccines. Centuries of reliance on traditional and natural remedies in the Asian culture coupled with a distrust of foreign vaccines have fueled the use of homeopathic “vaccines”. Furthermore, the mass circulation of anti-vaccine messages creates further mistrust in conventional Western medicine, and this, in turn, boosts beliefs in homeopathic vaccines. These so-called vaccines or referred as “nosodes” are said to contain pathological specimens diluted until very little or none of the original substances are present, yet sufficient to provide immunity.20 Homeopathic vaccines are hence argued much safer than conventional vaccines as “nosodes” do not contain adjuvants, preservatives, stabilizers and residual by-products found in conventional vaccines. In addition to homeopathic vaccines, there is also the belief that the administration of high doses of vitamins boosts immunity and could serve as vaccination alternatives. As most of these messages argued for safer vaccines and not against vaccination itself, it is important to emphasize to the public that the vaccines currently in used have gone through extensive safety assessment before it is declared safe for administration and continue to be monitored even years after the introduction. This is in contrast to the homeopathic vaccines where there are no scientific evidence to support its effectiveness and usage.
Among the identified factors possibly contributing to the rise in vaccine hesitancy in Malaysia, is the proliferation of anti-vaccination messages on social media platforms, which is quite similar to other Western countries.18 It is suggested in our study that; first, the public should be informed of the sources of information to trust on the internet.19 Secondly, it is important to have experts to respond to social media, posting in a professional manner, or medical professionals to engage and tackle the misconceptions about vaccine. Thirdly, the country should enforce the prevention of anti-vaccine propaganda or the spread of unverified information from vaccine skeptics via social media. The health professionals also strongly advocate for the prohibition of the promotion of herbal medicine or alternative medicine practices as an alternative to vaccination, which is currently very prominent via social media. The authorities should introduce restrictions on the promotion or sales of complementary and alternative medicines as alternatives to vaccination. The public should also be made aware of the lack of scientific evidence supporting the claims of “homeopathic vaccines”, herbal medicine or high doses of vitamins.
Conspiracy theories including the anti-Muslim plot, profiteering by greedy pharmaceutical companies, and the government and physicians earning profits from promoting and selling vaccines noted by the health professionals in the present study, warrant serious attention and emphatic dismissal. Public mistrust of health authorities and health workers was also found as an influencing factor of vaccine hesitancy in Europe countries.21 Community-based communication strategies including school and online discussion sessions overseen and managed by local health professionals are suggested as important strategies to maintain public trust.21
Likewise noted in other countries, the present study has identified the crucial role of medical professionals in combating vaccine hesitancy and increase vaccination in Malaysia.19 In particular, front-line vaccine providers are the influencer of vaccination decisions and must be equipped with accurate information about vaccines and vaccination in order to be able to respond and communicate with patients on the risk versus benefits of vaccination. Furthermore, the role of medical professionals in response to anti-vaccine propaganda online is crucial. Responses coming from medical professionals on social media platforms to eliminate doubts on vaccination and counter misconception held by the vaccine-hesitant group will be better received compared to those coming from nonprofessionals. Vaccine hesitancy among medical professionals has been reported in several studies,22,23 and this was also identified in the present study. It is of vital importance to identify health providers who are vaccine-hesitant and gain further understanding on the root cause of their hesitancies so that tailored strategies can be developed to address this.22 As a long-term measure, there is a need to incorporate specific teaching in the undergraduate medical curriculum to impart adequate knowledge on vaccine and favorable attitudes to vaccinations among the younger generation of healthcare providers. As many healthcare providers are ill-equipped to answer questions or engage in difficult conversations with those who are reluctant to be vaccinated, the curriculum of medical schools should also include soft skills training.24-26 In this regard, medical schools in Malaysia could intensify soft skill training and incorporate training on handling vaccine-hesitant group.
With regards to way forwards to reduce or eliminate VPDs, the present study highlighted the immediate need for Malaysia to establish an electronic vaccination registry system or record to track a child’s vaccination status in order to achieve full vaccination coverage.27 Such registry has been well-established in many developed countries but in most Southeast Asia countries, including Malaysia such system is still unavailable. This system is crucial for the identification of children who are for other than non-vaccine refusal reasons missing their vaccination. With the registry in place, it is still possible to do a catch-up vaccination or SIA, hence, ensuring that all children would have been vaccinated. This is especially beneficial for children living in extremely remote areas such as those of the Orang Asli where logistic issues and access to health services are the main barriers to effective vaccination program.28 Secondly, in countries with high vaccination rates, like Malaysia, vaccine-derived herd immunity may be short-lived due to high rate of human mobility, and the influx of international travelers and migrants.29,30 Presently, vaccination coverage of migrants is not monitored, exposing a gap in the NIP. There is recommendation from the study that children of migrants should also be included in the NIP as this would also contribute toward protection of the local children from being affected by VPDs. Efforts to strengthen routine vaccination through the establishment of SIAs targeting children in the communities of affected areas have been implemented in many countries in Southeast Asia, including Malaysia.31 Elderly adults are at an increased risk of disease morbidity, including VPDs. The burden of VPDs in older adults is evident in some disturbing trends of increasing measles and pertussis in older adults.32 Nonetheless, SIAs in the adult population, especially in the elderly, are relatively less common in Southeast Asia countries. Targeting older adults for SIAs has been recommended,32,33 as the burden of VPDs on the elderly may translate into significant social, public and economic costs to society.
Lastly, the opinion on mandatory vaccination is mixed. In particular, making vaccinations compulsory in response to falling vaccination rates in Malaysia may raise opposing attitudes based on religious grounds. To date, Malaysia’s highest Islamic body, the National Fatwa Council has yet to decide on an edict of mandatory vaccinations for Muslims. If vaccination is made compulsory in Malaysia, there is a crucial need for accompanying targeted communication and support, e.g. introducing vaccination counseling, particularly from Muslim religious leaders (Imams).
Some limitations of the present study were noted and these include the recruitment of participants from only one tertiary institution and the qualitative approach, both of which reduce the generalizability of results and limit our ability to draw firm conclusions. Due to these limitations, this study serves as a small snapshot that suggests areas for further investigation. Another potential limitation of this study is that viewpoints from the healthcare providers may not truly reflect the actual reasons for patient’s concern or beliefs about vaccination. As such, perspectives from vaccine refusal in the general population is warranted to confirm the findings of this study. It would also be useful for future studies to match the views of healthcare providers and vaccine refusals. The last limitation of this study is that the perspectives from health professionals in teaching hospital can be subjected to bias opinion as they do not routinely administer the vaccines to patients. It would be useful to gather perspectives from primary care physicians in the clinic or hospital that routinely administer vaccines to patients.
Conclusion
Vaccine hesitancy is a multi-layered phenomenon, related to various factors including the influence of anti-vaccination rumors, past-experience of AEFIs, perceived religious prohibition, a belief that traditional complementary and alternative medicine (TCAM) use is safer, pseudoscience beliefs, and anti-vaccine conspiracy theories. A counter-approach should embark on enhancing public awareness and changing their perceptions, while providing feedback to the reporting of AEFIs. Doctors and medical professionals play a vital role and should, therefore, be trained to have in-depth knowledge on vaccine and soft skills to communicate with anti-vaxxers and these trainings should be imparted early in their medical training. An electronic vaccination registry system is essential to document vaccination records of all individuals and to ensure the achievement of full vaccination coverage. Banning media dissemination of anti-vaccine information is also urgently required. While mandatory vaccination is still under debate, it is important to strengthen existing routine vaccination coverage and the prevention of travel and migration-associated VPDs. In conclusion, in addition to facing similar vaccine-hesitant issues comparable to that of other countries around the world, the present study identified specifically local culture, traditions and religion influence of vaccine hesitancy, which is useful as a guide for countries in Southeast Asia.
Funding Statement
This study was supported by the Ministry of Education, Malaysia for niche area research under the Higher Institution Centre of Excellence (HICoE) Program, Project No. MO002-2019.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Ministry of Health Malaysia . Health facts; 2018. [accessed 2019 October9]. https://www.dosm.gov.my/v1/index.php?r=column/ctwoByCat&parent_id=115&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09.
- 2.Ahmad NA, Jahis R, Kuay LK, Jamaluddin R, Aris T.. Primary immunization among children in Malaysia: reasons for incomplete vaccination. J Vaccines Vaccin. 2017;8(358):2. doi: 10.4172/2157-7560.1000358. [DOI] [Google Scholar]
- 3.Taib WRW, Yusoff NAM, Hussin TMAR, Ahmad A. Issues in vaccine hesitancy in Malaysia: a countering approach. JBCS. 2017;2:42–46. [Google Scholar]
- 4.World Health Organization . Measles-Rubella. Bulletin. 2019;13(1). [accessed 2019 September11]. https://apps.who.int/iris/bitstream/handle/10665/310883/Measles-Rubella-Bulletin-2019-Vol-13-No-01.pdf?sequence=1&isAllowed=y&ua=1. [Google Scholar]
- 5.Ministry of Health, Malaysia . Press release of the director general of health; 2019. January 22. [accessed 2019 September11]. https://kpkesihatan.com/2019/01/22/kenyataan-akhbar-kpk-22-januari-2019-penyebaran-maklumat-tidak-sahih-berkaitan-imunisasi/
- 6.World Health Organization . Vaccine-preventable diseases: monitoring system 2017 global summary; 2017. [accessed 2019 July1]. http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tsincidencediphtheria.html
- 7.Dubé E, Gagnon D, MacDonald N, Bocquier A, Peretti-Watel P, Verger P. Underlying factors impacting vaccine hesitancy in high income countries: a review of qualitative studies. Expert Rev Vaccines. 2018;17(11):989–1004. doi: 10.1080/14760584.2018.1541406. [DOI] [PubMed] [Google Scholar]
- 8.Hornsey MJ, Harris EA, Fielding KS. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018;37(4):307. doi: 10.1037/hea0000586. [DOI] [PubMed] [Google Scholar]
- 9.McClure CC, Cataldi JR, O’Leary ST. Vaccine hesitancy: where we are and where we are going. Clin Ther. 2017;39(8):1550–62. doi: 10.1016/j.clinthera.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Saint Arnault D, Woo S. Testing the influence of cultural determinants on help-seeking theory. Am J Orthopsychiatry. 2018;88(6):650–60. doi: 10.1037/ort0000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. doi: 10.1016/j.vaccine.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 12.AJ P, ZM Z, Jaafar N, Perialathan K, Ilman SS, Zakaria MR. Potential factors contributing to vaccine hesitancy among parents in malaysia: an overview. IJHSR. 2018;8(7):360–365. [Google Scholar]
- 13.Abidin ZZ, Juni MH, Ibrahim F. Adherence towards different vaccines of childhood immunization of under five year old children. Mal J Med Health Sci. 2017;13:43–50. [Google Scholar]
- 14.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccines Immunother. 2013;9(8):1763–73. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puliyel J, Naik P. Revised World Health Organization (WHO)’s causality assessment of adverse events following immunization—a critique; 2018. F1000Research. p. 7. [DOI] [PMC free article] [PubMed]
- 16.Ahmed A, Lee KS, Bukhsh A, Al-Worafi YM, Sarker MM, Ming LC, Khan TM. Outbreak of vaccine-preventable diseases in Muslim majority countries. J Infect Public Heal. 2018;11(2):153–55. doi: 10.1016/j.jiph.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 17.European Council of Fatwa and Research . Final statements. Eleventh ordinary session of the European council of fatwa and research. European council of fatwa and research, Stockholm, Sweden; 2017. [accessed 2019 July4]. https://www.e-cfr.org/eleventh-ordinary-session-european-council-fatwa-research/
- 18.Gezairy HA. WHO letter reports on Islamic legal scholars’ verdict on the medicinal use of gelatin derived from pork products. Cairo (Egypt): World Health Organization (WHO) for the Eastern Mediterranean; 2001. [Google Scholar]
- 19.Siti ZM, Tahir A, Farah AI, Fazlin SA, Sondi S, Azman AH, Maimunah AH, Haniza MA, Haslinda MS, Zulkarnain AK, et al. Use of traditional and complementary medicine in Malaysia: a baseline study. Complement Ther Med. 2009;17(5–6):292–99. doi: 10.1016/j.ctim.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Rieder MJ, Robinson JL. ‘Nosodes’ are no substitute for vaccines. Paediatr Child Health. 2015. May;20(4):219–20. doi: 10.1093/pch/20.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karafillakis E, Simas C, Jarrett C, Verger P, Peretti-Watel P, Dib F, De Angelis S, Takacs J, Ali KA, Pastore Celentano L, et al. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum Vaccines Immunother. 2019;15(7–8):1615–27. doi: 10.1080/21645515.2018.1564436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arede M, Bravo-Araya M, É B, Gill GS, Plajer V, Shehraj A, Shuaib YA. Combating vaccine hesitancy: teaching the next generation to navigate through the post truth era. Front Public Health. 2019;6:381. doi:10.3389/fpubh.2018.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One. 2014;9:e89177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubé E. Addressing vaccine hesitancy: the crucial role of healthcare providers. Clin Microbiol Infect. 2017;23(5):279–80. doi: 10.1016/j.cmi.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–06. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 26.Henrikson NB, Opel DJ, Grothaus L, Nelson J, Scrol A, Dunn J, Faubion T, Roberts M, Marcuse EK, Grossman DC. Physician communication training and parental vaccine hesitancy: a randomized trial. Pediatrics. 2015;136(1):70–79. doi: 10.1542/peds.2014-3199. [DOI] [PubMed] [Google Scholar]
- 27.Cutts FT, Izurieta HS, Rhoda DA. Measuring coverage in MNCH: design, implementation, and interpretation challenges associated with tracking vaccination coverage using household surveys. PLoS Med. 2013;10:e1001404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burghouts J, Del Nogal B, Uriepero A, PW H, de Waard JH, Verhagen LM. Childhood vaccine acceptance and refusal among warao amerindian caregivers in Venezuela; a qualitative approach. PLoS One. 2017;12:e0170227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tuite AR, Thomas-Bachli A, Acosta H, Bhatia D, Huber C, Petrasek K, Watts A, Yong JH, Bogoch II, Khan K. Infectious disease implications of large-scale migration of Venezuelan nationals. J Travel Med. 2018;25:tay077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peak CM, Reilly AL, Azman AS, Buckee CO. Prolonging herd immunity to cholera via vaccination: accounting for human mobility and waning vaccine effects. PLoS Negl Trop Dis. 2018;12:e0006257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biellik RJ, Orenstein WA. Strengthening routine immunization through measles-rubella elimination. Vaccine. 2018;36(37):5645–50. doi: 10.1016/j.vaccine.2018.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kandeil W, Atanasov P, Avramioti D, Fu J, Demarteau N, Li X. The burden of pertussis in older adults: what is the role of vaccination? A systematic literature review. Expert Rev Vaccines. 2019;18(5):439–55. doi: 10.1080/14760584.2019.1588727. [DOI] [PubMed] [Google Scholar]
- 33.Hayman DT. Measles vaccination in an increasingly immunized and developed world. Hum Vaccines Immunother. 2019;15(1):28–33. doi: 10.1080/21645515.2018.1517074. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Ministry of Health Malaysia . Health facts; 2018. [accessed 2019 October9]. https://www.dosm.gov.my/v1/index.php?r=column/ctwoByCat&parent_id=115&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09.


