Abstract
Coronavirus disease 2019 (COVID-19) is most frequently associated with a mild presentation of fever, cough, and shortness of breath. Typical radiographic findings of COVID-19 are bilateral ground-glass opacities on computed tomography (CT) scans. However, there have been instances of pneumothorax, giant bulla, and pneumomediastinum, mainly in elderly COVID-19 patients and predominately occurring at least one week after symptom onset. Here, we report a case where a healthy, young Hispanic man presented with three days of fever, cough, and dyspnea. On admission to the emergency department, he was found to have bilateral pneumothoraces, pneumomediastinum, and pneumopericardium requiring bilateral chest tubes. The patient had no predisposing risk factors for pneumothorax, such as a history of trauma, smoking, past intubations, asthma, high pressure oxygen delivery, or a history of prior pneumothorax. The only positive diagnostic test was a SARS-CoV-2 test by real-time reverse transcriptase–polymerase chain reaction assay. This case highlights the potential atypical presentation of a COVID-19 infection and is the first reported case, to our knowledge, that features bilateral spontaneous pneumothoraces, pneumomediastinum, and pneumopericardium as a probable rare presentation of COVID-19.
Keywords: COVID-19, Coronavirus, Pneumothorax, Pneumopericardium, Pneumomediastinum
Abbreviations list
- COVID-19
Coronavirus Disease 2019
- CT
Computed Tomography
- CXR
Chest radiograph
- ED
Emergency Department
- HD
Hospital Day
- HFNC
High-flow nasal cannula
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
1. Introduction
The novel coronavirus disease 2019 (COVID-19) has presented with a spectrum of symptoms and severity. Systematic reviews and meta-analyses demonstrate that the majority of presentations are mild with fever, cough, and dyspnea being the characteristic clinical features. Radiographically, the most frequently reported computed tomography (CT) findings are bilateral ground-glass opacities [1]. However, in this report, we describe a possible rare presentation of COVID-19 involving tension pneumothorax, pneumomediastinum, and pneumopericardium requiring emergent intervention in an otherwise healthy young adult.
2. Case report
In April 2020, a 31-year-old Hispanic man with an unremarkable past medical history presented to the emergency department (ED) with three days of fever, cough, and worsening dyspnea. He denied any chest pain and reported no recent trauma. Additionally, the patient had no history of cardiopulmonary disease, intubations, mechanical ventilation, or drug use.
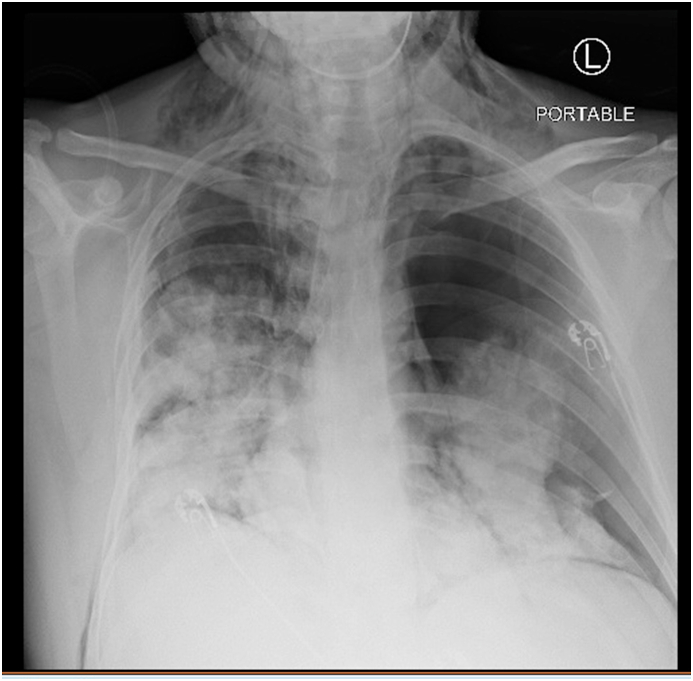
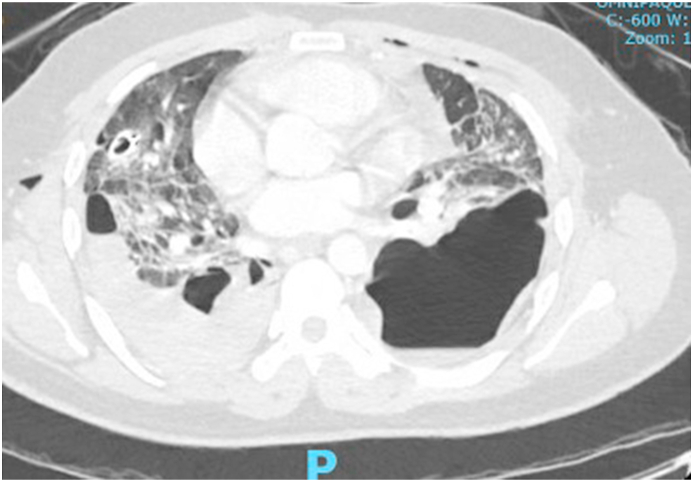
In the ED, he was found to be tachycardic (heart rate of 140 bpm) but normotensive (blood pressure of 130/88 mm Hg) and afebrile (37.2 °C). His peripheral oxygen saturation was 79% on room air which improved to 95% with the aid of a 15 L/min nonrebreather mask. Physical examination was significant for absent breath sounds on the left associated with crepitus extending bilaterally to the neck. A bedside ultrasound demonstrated pneumothorax and a portable anterior/posterior chest x-ray (CXR) confirmed a large left-sided tension pneumothorax as well as a small right-sided pneumothorax (Fig. 1). An emergent chest tube was placed on the left for the tension pneumothorax, and the patient was admitted to the medical intensive care unit.
Fig. 1.
CXR on Admission- Large left-sided tension pneumothorax and small right-sided pneumothorax.
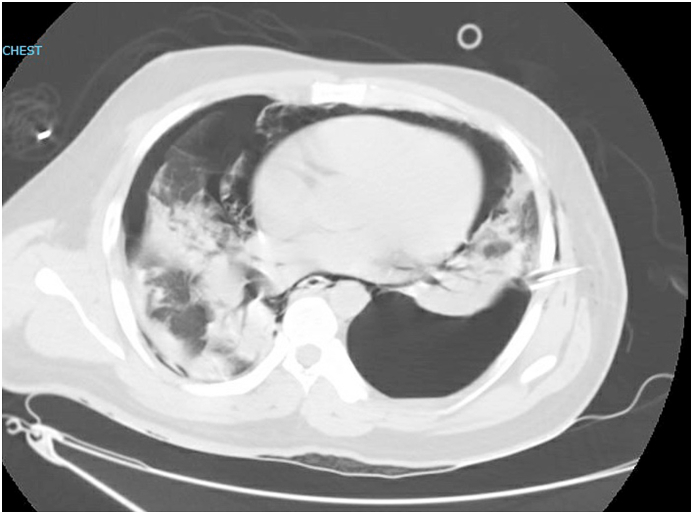
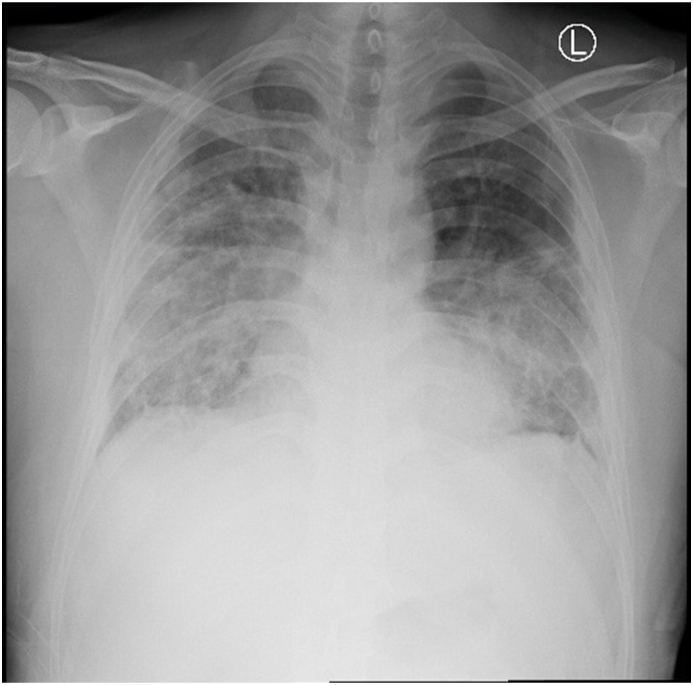
A nasopharyngeal swab was performed with a detected result for SARS-CoV-2 on real-time reverse transcriptase–polymerase chain reaction assay. Admission bloodwork demonstrated no leukocytosis, lymphopenia, anemia, or electrolyte abnormalities. Troponin T and serum creatinine levels were within normal limits. Serum samples were significant for an elevated d-dimer assay of 3,248 ng/mL DDU (normal: < 500 ng/mL), ferritin of 787 ng/mL (normal: 24–336 ng/mL), C-reactive protein of 2.90 mg/dL (normal: <0.8 mg/dL), and a procalcitonin of 0.09 ng/mL (normal: <0.1 ng/mL). Non-contrast chest CT was significant for extensive pneumomediastinum, pneumopericardium, and bilateral pneumothoraces, as well as bilateral confluent parenchymal consolidations, compatible with multilobar pneumonia (Fig. 2).
Fig. 2.
CT Chest on Admission- Extensive pneumomediastinum, pneumopericardium and bilateral pneumothoraces. Bilateral confluent parenchymal consolidations, compatible with multilobar pneumonia.
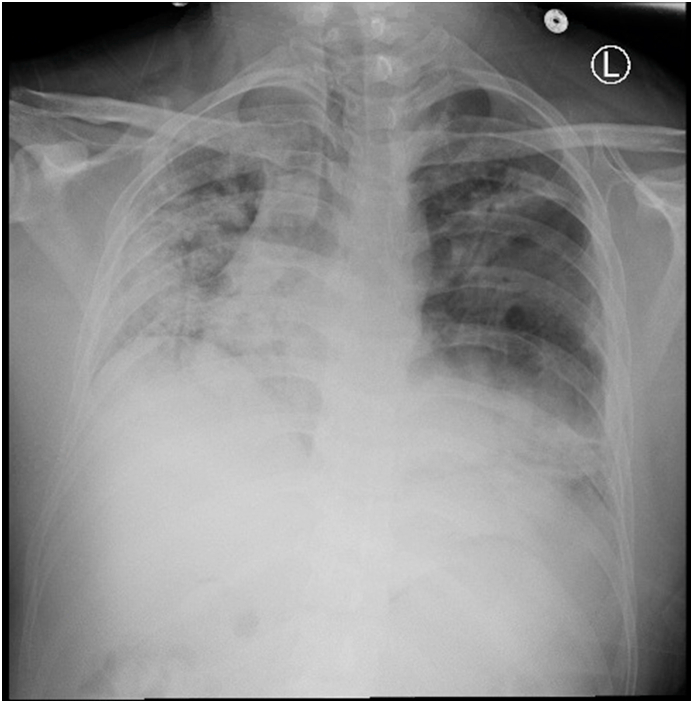
Over the following days, the patient's supplemental oxygen requirements decreased, and he was transferred to the medical floor on hospital day (HD) three with serial CXRs demonstrating gradual resolution of his pneumothoraces (Fig. 3). He received a dose of tocilizumab on HD three, and he completed a five-day course of hydroxychloroquine. On HD six, the chest tube was removed. He was stable on room air and was discharged home on HD nine.
Fig. 3.
CXR from HD six- Small residual left-sided pneumothorax. Stable bilateral opacities.
The following day, the patient returned to the ED with sudden-onset dyspnea. He was normotensive but tachycardic with a heart rate of 138 bpm, and his oxygen saturation was 84% on room air. CXR revealed recurrent new bilateral pneumothoraces with an approximate 7-cm airgap on the right and an approximate 4.5-cm airgap on the left (Fig. 4). Bilateral chest tubes were placed and remained for ten days. A CT chest with IV contrast was obtained and demonstrated worsening bilateral basilar loculated hydropneumothorax (Fig. 5). The patient underwent left-sided chemical pleurodesis on HD four and HD seven. Ultimately, the patient required CT-guided percutaneous placement of bilateral pigtail catheters which were placed on HD six and remained in place for seven days. By HD fifteen, all chest tubes were removed and repeat CXR noted resolved pneumothoraces (Fig. 6). The patient was subsequently confirmed to be stable on room air and was discharged home with close outpatient follow-up.
Fig. 4.
CXR from ten days after initial presentation to ED- New bilateral pneumothoraces with 7-cm airgap on right and 4.5-cm airgap on left. Airspace opacities consistent with viral pneumonia.
Fig. 5.
CT Chest on HD five- Right posterior basilar loculated hydropneumothorax.
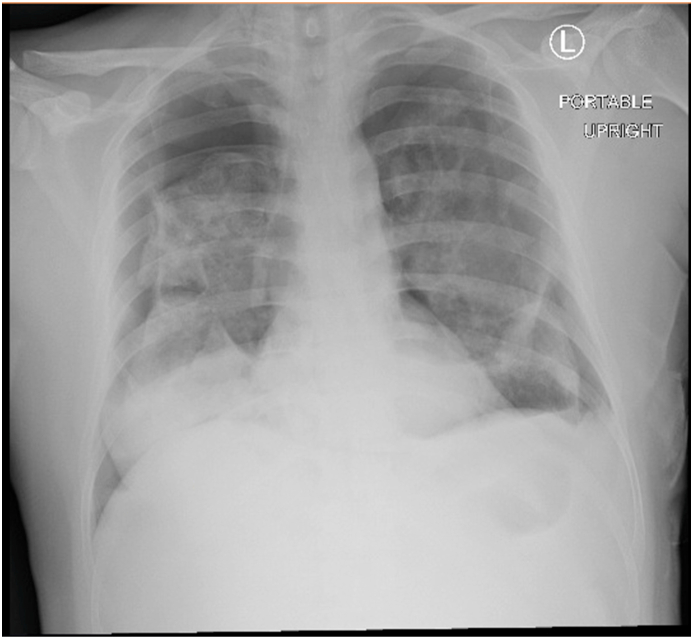
Fig. 6.
CXR from day of discharge (HD fifteen)- Stable mid/lower lung zone parenchymal opacities and pleural thickening. No pneumothorax.
3. Discussion
To the best of our knowledge, this is the first reported case that features bilateral spontaneous pneumothoraces, pneumomediastinum, and pneumopericardium as a probable rare presentation of COVID-19 as well as the first reported case which features pneumothoraces within a week of symptom onset. At the time of submission, only a handful of similar cases had been reported, and all cases had occurred after a reported symptom onset of over a week [[2], [3], [4], [5]]. The first reported case was a 38-year-old man from Wuhan diagnosed with COVID-19 pneumonia who, while on high-flow nasal cannula (HFNC), developed mediastinal emphysema, giant bulla, and pneumothorax with first appearance on HD eleven [2]. Another case involved a 38-year-old man from Wuhan admitted for COVID-19 pneumonia who developed exertional angina on HD eleven and imaging revealing spontaneous pneumomediastinum and subcutaneous emphysema [3]. Similarly, a 62-year-old man being treated for COVID-19 pneumonia had worsening dyspnea on HD twenty, and he was found to have right-sided pneumothorax in combination with pneumomediastinum and subcutaneous emphysema [4].
Well-known complications of invasive mechanical ventilation include pneumothorax and mediastinal emphysema; however, the subject of this report never required mechanical ventilation or HFNC oxygen therapy. Excessive cough, as reported by the patient, might be considered an inciting factor for pneumothorax as it has been reported in respiratory diseases such as acute respiratory distress syndrome and asthma [6,7]. Therefore, we suspect that the findings of pneumomediastinum, bilateral pneumothorax, and subcutaneous emphysema are related to COVID-19.
4. Conclusion
This case highlights the potential atypical presentation of COVID-19 requiring emergent intervention within a week of symptom onset in an otherwise healthy young adult. Individuals with as few as three days of symptoms may present with pneumomediastinum, bilateral pneumothorax, and subcutaneous emphysema related to COVID-19. The aim of this report is to educate physicians to consider this atypical and clinically severe presentation of COVID-19. Future case series and autopsy results are needed to elucidate a pathophysiological mechanism for how COVID-19 predisposes patients to pneumothoraces and whether there are any long-term sequelae of COVID-19-induced pneumothoraces.
Author contributions
All persons who meet authorship criteria are listed as authors. All authors certify that they have participated sufficiently in the work to take responsibility for the content. ASA and TQ made substantial contributions to conception and design of this case report. NN made substantial contributions acquisition of images. All authors made substantial contributions to the interpretation of date. ASA was involved in drafting the manuscript. TQ, NN, WS, and MNC revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript for publication.
Declaration of competing interest
No authors have any conflicts of interest related to this report. The authors have no competing interest to declare.
Contributor Information
Amrit S. Ahluwalia, Email: Amrit.Ahluwalia@downstate.edu.
Taha Qarni, Email: TQarni@northwell.edu.
Naureen Narula, Email: NNarula@northwell.edu.
Waleed Sadiq, Email: WSadiq@northwell.edu.
Michel N. Chalhoub, Email: MChalhoub1@northwell.edu.
References
- 1.Fu L., Wang B., Yuan T. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J. Infect. 2020;80(6):656‐665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun R., Liu H., Wang X. Mediastinal emphysema, giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J. Radiol. 2020;21(5):541‐544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou C., Gao C., Xie Y., Xu M. COVID-19 with spontaneous pneumomediastinum. Lancet Infect. Dis. 2020;20(4):510. doi: 10.1016/S1473-3099(20)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang W., Gao R., Zheng Y., Jiang L. COVID-19 with spontaneous pneumothorax,pneumomediastinum and subcutaneous emphysema [published online ahead of print, 2020 Apr 25] J. Trav. Med. 2020 doi: 10.1093/jtm/taaa062. taaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J., Su X., Zhang T., Zheng C. Spontaneous pneumomediastinum: a probable unusual complication of coronavirus disease 2019 (COVID-19) pneumonia. Korean J. Radiol. 2020;21(5):627‐628. doi: 10.3348/kjr.2020.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caceres M., Ali S.Z., Braud R., Weiman D., Garrett H.E., Jr. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann. Thorac. Surg. 2008;86(3):962‐966. doi: 10.1016/j.athoracsur.2008.04.067. [DOI] [PubMed] [Google Scholar]
- 7.Chu C.M., Leung Y.Y., Hui J.Y. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur. Respir. J. 2004;23(6):802‐804. doi: 10.1183/09031936.04.00096404. [DOI] [PubMed] [Google Scholar]