Abstract
Objectives. To review the trends in pregnancy outcomes after Hurricane Katrina and assess effects of the disaster on research and public health related to pregnant women.
Methods. We reexamined the 2004–2006 vital statistics data from Alabama, Louisiana, and Mississippi, assessing what the risk of adverse pregnancy outcomes in the population would have been under varying risk scenarios.
Results. We saw a reduction in number of births as well as in low birth weight and preterm birth. If the number of births had stayed constant and the relative higher risk in the “missing” births had been between 17% and 100%, the storm would have been associated with an increased risk instead of a decrease. Because the relative decline in births was larger in Black women, the higher risk in the “missing” births required to create a significant increase associated with the storm was generally not as great as for White women.
Conclusions. Higher exposure to Katrina may have produced a reduction in births among high-risk women in the region rather than increasing adverse outcomes among those who did give birth.
Birth outcomes are generally expected to worsen following natural disasters. Trauma may trigger labor.1 Mental illnesses, including posttraumatic stress disorder, anxiety, somatic complaints, alcohol addiction, and depression, rise after natural disasters and are associated with negative birth outcomes.2,3 Maternal psychological distress is also associated with an increased risk of preterm birth (PTB), low birth weight (LBW), and fetal growth restriction.4 Beyond psychosocial factors, other disaster-related exposures such as environmental contaminants can also have a negative impact on birth outcomes.5 Disaster research has generally shown small reductions in birth weight associated with exposure to disaster, while effects on gestational age are more mixed.6 Other complications, such as hypertensive disorders of pregnancy or gestational diabetes, are understudied—while a few studies have indicated increases in their occurrence after disaster,7–9 the literature is limited.
The March of Dimes predicted an increase in preterm births after Katrina.10 Instead, an unexpected improvement of birth outcomes occurred. Hamilton et al. and the National Center for Health Statistics compared affected areas 12 months before and after the disaster11 and found a decline in LBW in all affected areas, which included parts of Louisiana, Mississippi, and Alabama, and a decrease in PTB in Louisiana and Mississippi (however, there was an increase in PTB in Alabama). In Louisiana specifically, for instance, the incidence of very low birth weight (VLBW; < 1500 grams) before Hurricane Katrina was 2.3% and it decreased to 1.8% after Katrina, while the rate of very preterm birth (VPTB; < 32 weeks) also fell, from 3.2% to 2.4%.11 A more detailed analysis of Louisiana data for 2 years after Katrina similarly found declines in LBW and PTB in the New Orleans region and Orleans Parish specifically.12 In addition, the storm might have been expected to widen racial disparities, with African American women being more vulnerable and, therefore, more affected. However, racial disparities in LBW and PTB did not widen and may even have decreased somewhat; nor did the hurricane have a stronger impact on birth outcomes among African American women.12
Smaller studies with more detailed assessment of exposure did not necessarily reflect these population-level statistics, however. Xiong et al. found a graded association between exposure to the hurricane and adverse birth outcomes, with a greater number of severe exposures associated with higher risk of LBW and PTB.13 Similarly, Harville et al., examining birth outcomes in a cohort of Louisiana pregnant women 5 to 7 years after the storm, found that having experienced damage and injury during Katrina was associated with reduced birth weight and gestational age, although current experience of long-term recovery and other indicators of previous exposure were not.14 Other outcomes that might be expected to be associated with adverse birth outcomes, such as lack of prenatal care,11,12 cleft birth defects,15 and eclampsia,16 were reported to rise. In qualitative studies, women reported devastating complications, which they attributed to disaster exposure.17
Pre–post comparisons are complicated because of the decline in population and birth rate after Katrina. Katrina caused one of the largest internal migrations in US history, with a million people distributed across the United States in less than 2 weeks.18 There was a 19% decrease in the number of births in the 14 most-affected counties or parishes in the 12 months after Katrina compared with 12 months before.11 Moving can delay fertility until a more secure and permanent residence is established, employment is obtained, and lost assets are rebuilt, leading to a short-term fertility decline.19
The decline in fertility was not uniform: there was a sharper decrease in birth rates in non-Hispanic Black women than in non-Hispanic White women and Hispanic women. Return migration after Katrina was slower for Blacks compared with Whites.20 As measured by total fertility rate, Black fertility fell and remained 4% below expected values for at least 5 years after Katrina, whereas White fertility increased by 5%.19 Other demographic changes were also observed: women giving birth in the New Orleans region in the year after Katrina were more likely to be married, to be aged older than 20 years, and to have a college education than in the year before.12 However, no increase or a reduction in risk was found for both LBW and PTB in Orleans Parish and the New Orleans region after controlling for these factors and others (i.e., ethnicity, parity, smoking, interpregnancy interval).
The combination of these trends of lower complications but also lower fertility leads to concerns about live-birth bias in estimating the overall effect of Hurricane Katrina. Restricting a sample to include only live births can lead to an inaccurate estimate of overall exposure effect if the exposure affects both survival and the outcome under study; such a bias has been proposed as a possible explanation for the inverse association between neurodevelopmental outcomes and exposure to environmental pollutants.21 Similar questions arise with respect to natural disaster exposure when only live-birth data are used: many exposed women do not become pregnant, whether intentionally or unintentionally, and other pregnancies do not result in live births because of spontaneous and induced abortion, fetal death, and stillbirth. Zahran et al. reported a higher rate of fetal deaths to be correlated with living in an area with widespread destruction of housing stock after Katrina.22 We therefore explored the possible effects of the post-Katrina decline in fertility and whether differential reductions in fertility are possible explanations for the observed decline in adverse birth outcomes.
METHODS
We conducted an analysis of possible live birth bias following the principles of Liew et al.21 Data included in the 2009 report from the National Vital Statistics System11 provided the number of births and proportion of complications in areas affected by Hurricane Katrina 12 months before the storm and 12 months following the storm. We estimated what the effect of the storm on birth outcomes would have been if the number of births had stayed constant, varying the hypothetical proportions of each birth outcome. We first estimated the number of “missing” births as the difference between the number of births in the 12 months after compared with the 12 months before. We then calculated what the relative risk and confidence intervals (using standard Mantel–Haenszel formulas) would be if varying proportions of the “missing” births resulted in, for instance, LBW, comparing the probability of LBW occurring after disaster to the probability before the disaster under these hypothetical scenarios.
A schematic for this process is provided in Figure 1. For example, in the 14 most-affected counties or parishes, there were 34 520 births in the 12 months before Katrina and 27 848 in the 12 months after Katrina, for a reduction of 6672 births. Before Katrina, the incidence of PTB was 16.7%, or 5765 cases. After Katrina, the incidence of PTB was 16.7%, or 4651 cases. If 20% of the 6672 births had occurred and had been preterm (n = 1334), the overall incidence of PTB in the 12 months after the storm would have been (4651+1334)/34520 = 17.3%, with a relative risk of 1.04 (17.3/16.7; 95% confidence interval = 1.00, 1.07). By varying this percentage, the incidence of PTB under various conditions can be calculated (details in material available as a supplement to the online version of this article at http://www.ajph.org). We used Microsoft Excel’s What-If Analysis–Goal Seek (Microsoft, Redmond, WA) to calculate the point at which a statistically significant increase would have occurred.
FIGURE 1—
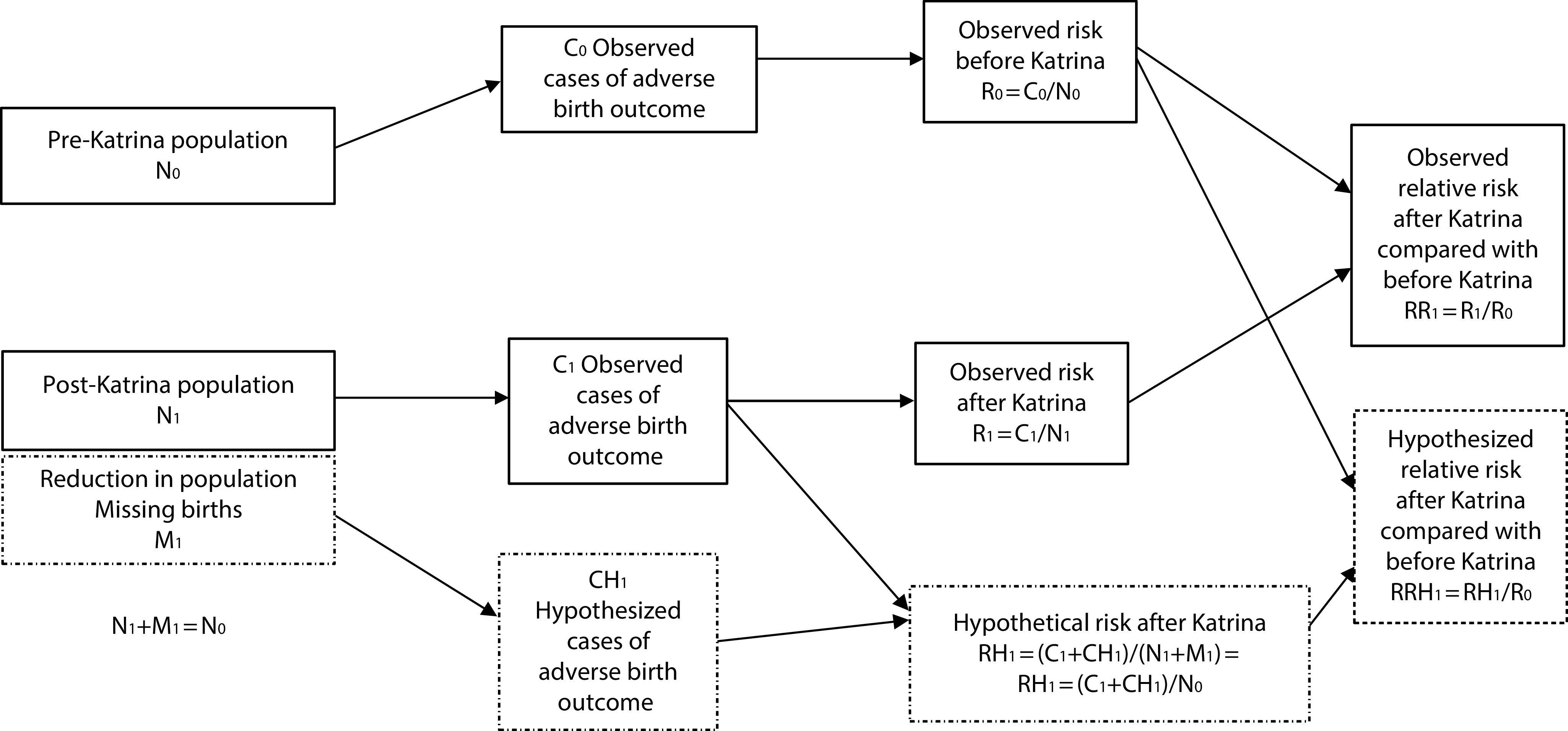
Schematic for Live-Birth Analysis
We repeated similar calculations for VLBW, PTB (< 37 weeks’ gestation), and VPTB and stratified by race/ethnicity (non-Hispanic White and non-Hispanic Black; the number of Hispanics and other groups was too small to analyze. Results for the overall population are not necessarily the average of the subgroups, both because of the lack of analysis of these smaller race/ethnicity groups and the fact that the baseline risk and the relative decline in births differed by race, creating a situation similar to confounding identifiable in stratified analysis.). We conducted the analysis for the 14 most-affected counties or parishes in the overall Katrina-affected region as well as Louisiana specifically. It should be noted that our analysis of live births is a thought experiment, to put bounds on the possible effects of differential changes in fertility and childbearing, rather than a true estimate of the hurricane’s effects, which would require a much more extensive consideration of uncertainty and variation and more detail on the relevant effect sizes.
RESULTS
If the missing births were to women at high risk, Hurricane Katrina might have been associated with worse outcomes rather than better (Table 1; detailed analysis in Tables A–F, available as supplements to the online version of this article at http://www.ajph.org). Whether the higher risk required to create that association is plausible varies by the association being analyzed. The risk in the missing births that led to a harmful effect of Katrina, rather than a protective one, varied by outcome. For the most affected counties across the region, it would be a 5.7% incidence of VPTB, 19.5% of PTB, 3.7% of VLBW, and 14.2% for LBW; somewhat higher incidences would be required in Louisiana specifically. This would be between a 17% increase and a doubling of risk in the missing group compared with the observed risk.
TABLE 1—
Live Birth Analysis, Complete Population, 14 Counties Most Affected by Hurricane Katrina: Alabama, Louisiana, and Mississippi, 2004–2006
| No. of Births |
Incidence (No. Cases) |
Required Risk in Missing Births to Indicate a Harmful Effect of the Storm | Ratio of Risk in Missing Births to Observed Risk | |||||
| Before Katrina | After Katrina | Difference (“Missing”) | Before Katrina | After Katrina | Observed Baseline RR (95% CI) | |||
| Overall region | 34 520 | 27 848 | 6 672 | |||||
| VPTB | 0.031 (1070) | 0.028 (780) | 0.90 (0.82, 0.99) | 0.057 | 2.02 | |||
| PTB | 0.167 (5765) | 0.167 (4651) | 1.00 (0.97, 1.04) | 0.195 | 1.17 | |||
| VLBW | 0.021 (725) | 0.020 (557) | 0.95 (0.85, 1.06) | 0.037 | 1.85 | |||
| LBW | 0.110 (3797) | 0.108 (3008) | 0.98 (0.94, 1.03) | 0.143 | 1.31 | |||
| Louisiana | 21 361 | 14 932 | 6 429 | |||||
| VPTB | 0.032 (684) | 0.024 (358) | 0.75 (0.66, 0.85) | 0.062 | 2.58 | |||
| PTB | 0.161 (3439) | 0.154 (2300) | 0.96 (0.91, 1.00) | 0.200 | 1.30 | |||
| VLBW | 0.023 (491) | 0.018 (269) | 0.78 (0.68, 0.91) | 0.044 | 2.43 | |||
| LBW | 0.110 (2350) | 0.105 (1568) | 0.95 (0.90, 1.01) | 0.142 | 1.35 | |||
Note. CI = confidence interval; LBW = low birth weight; PTB = preterm birth; RR = relative risk; VLBW = very low birth weight; VPTB = very preterm birth.
Source. Baseline numbers and risks taken from National Vital Statistics Reports.11
Because the decline in births was larger in Black women, the higher risk in the “missing” births required to create a significant increase associated with the storm was generally not as great as for White women (Table 2). The reduction of risk noted overall was also stronger in the Black population than the White population, where mostly there was no change or perhaps a small increase. For Black women, the increased risk in the missing births required to create a significant increase after the storm was less than 50% above baseline for the region, up to 80% for VPTB in Louisiana.
TABLE 2—
Live Birth Analysis—Stratified by Race (Non-Hispanic White and Non-Hispanic Black), 14 Counties Most Affected by Hurricane Katrina: Alabama, Louisiana, and Mississippi, 2004–2006
| No. of Births |
Incidence (No. Cases) |
Required Risk in Missing Births to Indicate a Harmful Effect of the Storm | Ratio of Risk in Missing Births to Observed Risk | |||||
| Before Katrina | After Katrina | Difference (“Missing”) | Before Katrina | After Katrina | Observed Baseline RR (95% CI) | |||
| Overall region | ||||||||
| Black | ||||||||
| VPTB | 13 170 | 8 478 | 4 692 | 0.050 (659) | 0.047 (398) | 0.94 (0.83, 1.06) | 0.071 | 1.51 |
| PTB | 0.215 (2 832) | 0.219 (1 857) | 1.02 (0.96, 1.07) | 0.236 | 1.08 | |||
| VLBW | 0.034 (448) | 0.034 (288) | 1.00 (0.86, 1.16) | 0.047 | 1.38 | |||
| LBW | 0.151 (1 989) | 0.160 (1 356) | 1.06 (0.99, 1.13) | 0.159 | 0.99 | |||
| White | ||||||||
| VPTB | 18 706 | 17 020 | 1 686 | 0.019 (355) | 0.020 (340) | 1.05 (0.91, 1.22) | 0.041 | 2.05 |
| PTB | 0.138 (2 581) | 0.144 (2 451) | 1.04 (0.99, 1.10) | 0.155 | 1.08 | |||
| VLBW | 0.014 (262) | 0.015 (255) | 1.07 (0.90, 1.27) | 0.031 | 2.07 | |||
| LBW | 0.086 (1 609) | 0.088 (1 498) | 1.02 (0.96, 1.10) | 0.129 | 1.47 | |||
| Louisiana | ||||||||
| Blacka | ||||||||
| VPTB | 9 296 | 4 575 | 4 721 | 0.050 (465) | 0.040 (183) | 0.80 (0.68, 0.95) | 0.072 | 1.79 |
| PTB | 0.208 (1 934) | 0.205 (938) | 0.99 (0.92, 1.06) | 0.284 | 1.39 | |||
| VLBW | 0.035 (325) | 0.030 (137) | 0.86 (0.70, 1.04) | 0.051 | 1.70 | |||
| LBW | 0.149 (1385) | 0.155 (709) | 1.04 (0.96, 1.13) | 0.164 | 1.06 | |||
| White | ||||||||
| VPTB | 10 203 | 8 808 | 1 395 | 0.017 (173) | 0.017 (150) | 1.00 (0.81, 1.24) | 0.044 | 2.59 |
| PTB | 0.125 (1 275) | 0.131 (1 154) | 1.05 (0.97, 1.13) | 0.154 | 1.18 | |||
| VLBW | 0.014 (143) | 0.013 (115) | 0.93 (0.73, 1.19) | 0.045 | 3.46 | |||
| LBW | 0.081 (826) | 0.084 (740) | 1.04 (0.94, 1.14) | 0.118 | 1.40 | |||
Note. CI = confidence interval; LBW = low birth weight; PTB = preterm birth; RR = relative risk; VLBW = very low birth weight; VPTB = very preterm birth.
Source. Baseline numbers and risks taken from National Vital Statistics Reports.11
The number of births in Alabama rose slightly, so the decline in numbers in Louisiana is larger than for the region as a whole.
DISCUSSION
After Hurricane Katrina, adverse birth outcomes did not rise as expected, and birth rates fell. Our analysis of the possible effects of these changes in population suggests the incidence of adverse outcomes in the “missing births” would have had to be high to create the reduction in adverse birth outcomes that was seen. For many outcomes, the increased risk is plausible: for instance, a 14.3% risk of LBW, 31% higher than baseline, is consistent with overall statistics for non-Hispanic Black women or for other populations worldwide. For others, it is unlikely to be realistic—few exposures cause a doubling or tripling of risk for PTB, so this bias is unlikely to have been the cause of the lack of increase in VPTB or VLBW in White women, for instance. For live-birth bias to be the cause of the lower incidence in the overall population, the women who delivered live births would have to have been, on the contrary, very low risk and apparently not particularly affected by the hurricane. Some of the post-Katrina research that found higher risk of adverse birth outcomes with more exposure to the hurricane also found a low baseline risk among less-exposed women in the study samples.13
It is also notable that the decline in births was larger and the required increase in risk lower for the Black population than for the White population. A reasonable conclusion might be that, on the whole, Black women were more affected by Katrina but that the consequences of exposure were primarily a reduction in births among vulnerable women rather than increased adverse outcomes among those who did give birth. This reduction in births could be attributable to one or more of the following: selective migration, choosing not to become pregnant or carry to term, biologically lower fertility, or increased pregnancy losses.
Katrina was a major cause of the internal migration.18 Beyond the short-term fertility decline attributable to the complications of moving,19 family size also directly affects the inclination to move after disaster: individuals with smaller families have a higher propensity to move away from the affected region than do larger families. Smaller families tend to have smaller homes, own fewer items, and are easier to house in a new area.23 Return migration after Katrina was slower for Blacks, generally at higher risk for adverse birth outcomes, compared with Whites,20 and this likely accounts for some of the lower overall population risk in the year that followed the storm.
Changes in fertility may be attributable to conscious decisions as well as the biological ability to conceive. Warnings or experiences of natural disasters can prompt families who are already planning on having a child to either conceive earlier or postpone and conceive later, known as the “harvesting effect.”24 After severe disasters, mothers or couples may desire to conceive children to replace lives lost, either in response to mortality levels in the broader community or to replace a child lost during the disaster.25 Several disaster-related factors affect reproductive decision-making. Reduced income and economic pressures may lead couples to delay childbearing. Unemployment rates and harsh economic conditions are tied to lower fertility rates via a decline in marriage rates and an increase in divorce rates.2 Marital conflict is also very common following natural disasters and during times of high stress.2 These types of conflicts can interfere with a couple’s desire to have children together or lead to decreased sexual activity: 1 study found that women’s satisfaction with their sexual life had markedly decreased following an earthquake, with 89.4% of them saying they did not want to become pregnant.26 Access to health care can be limited after disaster, and women may worry about receiving necessary prenatal and obstetrical care. Costs of contraception, abortion, and basic health care can also rise after a disaster, with potential effects in both directions on fertility rates: Kissinger et al. found an increase in unplanned pregnancy after Katrina.27 In addition, access to medically assisted fertility treatment is likely to be limited; however, this affects only a small portion of births.
Fertility may also be biologically affected by disaster, because of physical illnesses, mental health and stress, and environmental contaminants. After the 2017 Wenchuan earthquake, women had significantly higher rates of lower genital tract infection, pelvic inflammatory disease, and menstrual disorders than before the earthquake.26 Stress can contribute to infertility through neuroendocrine pathways; for instance, high levels of stress can reduce levels of estrogen and luteinizing hormone,28 leading to a delay in ovulation and follicle maturation.25 A study of men’s health after Katrina found significant changes in sperm parameters associated with decreased fertility potential.29 Environmental contaminants that have been associated with disaster include lead after Katrina,16 fecal bacteria after Superstorm Sandy,25,30 and radiation after the Fukushima earthquake and tsunami.25 In addition, lack of electricity after a disaster can expose individuals to dangerous heat or cold.
Similar pressures operate on other outcomes that reduce live births. An increase in spontaneous abortion was reported after flooding in New York State31 and in fetal death associated with proportion of the housing stock destroyed after Katrina.32 In addition, a reduction in the sex ratio in Katrina-affected areas was seen in November 2005 (though not in months before or following); such declines in male births are often hypothesized to indicate a relative vulnerability of male fetuses to external stressors,32 producing differential pregnancy loss. Miscarriage, fetal death, and stillbirth are all associated with chemical and nonchemical stressors, and disaster can lead to increased exposures of both types—for instance, raising the risk of stillbirth attributable to carbon monoxide poisoning from improperly ventilated generators.33
Katrina could also have genuinely improved birth outcomes. The postdisaster period can be a time of communities pulling together, and pregnant women and infants are a concrete sign of renewal. Many people report posttraumatic growth and “silver linings” related to disaster. Even in wartime, increased support to women and children has been associated with improved birth outcomes.34
PUBLIC HEALTH IMPLICATIONS
Several clinical and public health groups provided descriptions of their experience during Hurricane Katrina relevant to pregnant women (see list of references in Appendix A, available as a supplement to the online version of this article at http://www.ajph.org). Hospitals that sheltered pregnant women reported deliveries by flashlight or generator light. Infants were evacuated by air, often separated from their mothers, and Woman’s Hospital in Baton Rouge, Louisiana, received patients from the neonatal intensive care units of several New Orleans hospitals. Those experiencing the disaster stressed the need for flexibility and adaptability as well as infrastructure that can stand up to multiple days without power, and those receiving patients stressed the importance of communication. Both sides expressed the importance of disaster planning and qualified coordination. The obstetrics/gynecology residency program at Louisiana State University suffered short-term loss of trainees and less opportunity for skills training in some areas. However, the disaster and subsequent reaccreditation process allowed for shifts in the program, including a greater use of private-practice sites and obstetric simulators, and ultimately higher numbers of medical students entered obstetrics/gynecology.
Analysis of vital statistics data made it clear that some women were not able to access prenatal care after Katrina, with the proportion of women receiving inadequate prenatal care significantly higher in the New Orleans region after Katrina and almost doubling in Orleans Parish.12 This increasing trend was stronger in White than Black women, both in relative and absolute terms, although Black women were still more likely overall to receive inadequate care.11,12 Not only in the Gulf region, Katrina encouraged clinicians to work with patients to develop disaster preparedness plans and be aware of particular postdisaster needs of pregnant women.
The Centers for Disease Control and Prevention (CDC) assessed a number of public health actions taken for reproductive health after Katrina, concluding that future programs need to encourage breastfeeding and provide contraception, and pregnancy-related considerations need to be incorporated into general public health disaster response programs; for instance, some vaccines and antibiotics are contraindicated in pregnant women. Newborn screening was disrupted and a large proportion of neonates did not have valid samples provided to the state laboratory. Health educators at the CDC worked to develop public service announcements and fact sheets targeting pregnant women affected by the hurricane, specifically encouraging seeking care, eating healthily, and taking hygiene precautions. The Organization for Teratology Information Specialists fielded a number of Katrina-related calls to their hotline and provided additional information on topics of special concern, such as mold, Vibrio, and pesticides. In the recovery phase, Healthy Start New Orleans served women who were particularly exposed to the disaster, and those women reported receiving more mental health counseling and prenatal education than women enrolled in traditional prenatal care.
Hurricane Katrina also led to the development of tools to assist with understanding postdisaster reproductive health care needs. Based on the Reproductive Health Assessment for Conflict-Affected Women Toolkit, the Reproductive Health After Disaster toolkit was developed to assess the needs of pregnant, postpartum, and reproductive-aged women35 and includes modules assessing exposure to disaster and service needs for pregnancy, family planning, and social services, with guidance on data entry and analysis. The toolkit was piloted after flooding and tornado disasters, along with sampling strategies to specifically reach the reproductive-aged population. It was also successfully implemented along the Gulf Coast after Hurricane Isaac, including training community health workers and patient navigators to administer it.
Hurricane Katrina’s effects on pregnant women provide a number of lessons for disaster planning and response. To begin with, pregnant women and infants must be considered not only by programs that address their needs specifically but also as an important and vulnerable subpopulation for any disaster planning and response group. Second, disasters will almost certainly lead to a reduction in access to prenatal care. For low-risk women, this is likely to be a minor inconvenience, while for high-risk women, this can be a major danger. Third, in the long term, major disasters lead to complicated effects on the birth rate, fertility, and adverse birth outcomes, which cannot necessarily be predicted.
CONFLICTS OF INTEREST
None of the authors have a conflict of interest.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed as no human participants were involved.
Footnotes
REFERENCES
- 1.Hernández-Díaz S, Boeke CE, Romans AT et al. Triggers of spontaneous preterm delivery—why today? Paediatr Perinat Epidemiol. 2014;28(2):79–87. doi: 10.1111/ppe.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohan CL, Cole SW. Life course transitions and natural disaster: marriage, birth, and divorce following Hurricane Hugo. J Fam Psychol. 2002;16(1):14–25. doi: 10.1037//0893-3200.16.1.14. [DOI] [PubMed] [Google Scholar]
- 3.Giarratano GP, Barcelona V, Savage J, Harville E. Mental health and worries of pregnant women living through disaster recovery. Health Care Women Int. 2019;40(3):259–277. doi: 10.1080/07399332.2018.1535600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lobel M, Dunkel Schetter C. Pregnancy and prenatal stress. In: Friedman HS, editor. Encyclopedia of Mental Health. Waltham, MA: Academic Press; 2016. pp. 318–329. [Google Scholar]
- 5.Ferguson KK, O’Neill MS, Meeker JD. Environmental contaminant exposures and preterm birth: a comprehensive review. J Toxicol Environ Health B Crit Rev. 2013;16(2):69–113. doi: 10.1080/10937404.2013.775048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harville EW, Xiong X, Buekens P. Hurricane Katrina and perinatal health. Birth. 2009;36(4):325–331. doi: 10.1111/j.1523-536X.2009.00360.x. [DOI] [PubMed] [Google Scholar]
- 7.Tong VT, Zotti ME, Hsia J. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern Child Health J. 2011;15(3):281–288. doi: 10.1007/s10995-010-0576-9. [DOI] [PubMed] [Google Scholar]
- 8.Oyarzo C, Bertoglia P, Avendano R et al. Adverse perinatal outcomes after the February 27th 2010 Chilean earthquake. J Matern Fetal Neonatal Med. 2012;25(10):1868–1873. doi: 10.3109/14767058.2012.678437. [DOI] [PubMed] [Google Scholar]
- 9.Xiao J, Huang M, Zhang W et al. The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Sci Total Environ. 2019;678:755–760. doi: 10.1016/j.scitotenv.2019.04.436. [DOI] [PubMed] [Google Scholar]
- 10. March of Dimes helping babies and pregnant women imperiled by Hurricane Katrina. Arlington, VA: March of Dimes Birth Defects Foundation; 2005.
- 11.Hamilton BE, Sutton PD, Mathews TJ, Martin JA, Ventura SJ. The effect of Hurricane Katrina: births in the US Gulf Coast Region, before and after the storm. Natl Vital Stat Rep. 2009;58(2):1–28,32. [PubMed] [Google Scholar]
- 12.Harville EW, Tran T, Xiong X, Buekens P. Population changes, racial/ethnic disparities, and birth outcomes in Louisiana after Hurricane Katrina. Disaster Med Public Health Prep. 2010;4(suppl 1):S39–S45. doi: 10.1001/dmp.2010.15. [DOI] [PubMed] [Google Scholar]
- 13.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med. 2010;5(3):181–187. doi: 10.5055/ajdm.2010.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harville EW, Giarratano G, Savage J, Barcelona de Mendoza V, Zotkiewicz T. Birth outcomes in a disaster recovery environment: New Orleans women after Katrina. Matern Child Health J. 2015;19(11):2512–2522. doi: 10.1007/s10995-015-1772-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goenjian AK, Pynoos RS, Steinberg AM et al. Psychiatric comorbidity in children after the 1988 earthquake in Armenia. J Am Acad Child Adolesc Psychiatry. 1995;34(9):1174–1184. doi: 10.1097/00004583-199509000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Zahran S, Magzamen S, Breunig IM, Mielke HW. Maternal exposure to neighborhood soil Pb and eclampsia risk in New Orleans, Louisiana (USA): evidence from a natural experiment in flooding. Environ Res. 2014;133:274–281. doi: 10.1016/j.envres.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Badakhsh R, Harville E, Banerjee B. The childbearing experience during a natural disaster. J Obstet Gynecol Neonatal Nurs. 2010;39(4):489–497. doi: 10.1111/j.1552-6909.2010.01160.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grier P. The great Katrina migration. Christian Science Monitor. September 12, 2005. Available at: https://www.csmonitor.com/2005/0912/p01s01-ussc.html. Accessed April 20, 2020.
- 19.Seltzer N, Nobles J. Post-disaster fertility: Hurricane Katrina and the changing racial composition of New Orleans. Popul Environ. 2017;38:465–490. doi: 10.1007/s11111-017-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fussell E, Sastry N, Vanlandingham M. Race, socioeconomic status, and return migration to New Orleans after Hurricane Katrina. Popul Environ. 2010;31(1-3):20–42. doi: 10.1007/s11111-009-0092-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liew Z, Olsen J, Cui X, Ritz B, Arah OA. Bias from conditioning on live birth in pregnancy cohorts: an illustration based on neurodevelopment in children after prenatal exposure to organic pollutants. Int J Epidemiol. 2015;44(1):345–354. doi: 10.1093/ije/dyu249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zahran S, Breunig IM, Link BG, Snodgrass JG, Weiler S, Mielke HW. Maternal exposure to hurricane destruction and fetal mortality. J Epidemiol Community Health. 2014;68(8):760–766. doi: 10.1136/jech-2014-203807. [DOI] [PubMed] [Google Scholar]
- 23.Finlay J. Fertility response to natural disasters: the case of three high mortality earthquakes. Report No. 4338.Washington, DC: The World Bank; 2009. [Google Scholar]
- 24.Evans RW, Hu Y, Zhao Z. The fertility effect of catastrophe: US hurricane births. J Popul Econ. 2008;23(1):1–36. [Google Scholar]
- 25.Davis J. Fertility after natural disaster: Hurricane Mitch in Nicaragua. Popul Environ. 2017;38(4):448–464. doi: 10.1007/s11111-017-0271-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu S, Han J, Xiao D, Ma C, Chen B. A report on the reproductive health of women after the massive 2008 Wenchuan earthquake. Int J Gynaecol Obstet. 2010;108(2):161–164. doi: 10.1016/j.ijgo.2009.08.030. [DOI] [PubMed] [Google Scholar]
- 27.Kissinger P, Schmidt N, Sanders C, Liddon N. The effect of the Hurricane Katrina disaster on sexual behavior and access to reproductive care for young women in New Orleans. Sex Transm Dis. 2007;34(11):883–886. doi: 10.1097/OLQ.0b013e318074c5f8. [DOI] [PubMed] [Google Scholar]
- 28.Schliep KC, Mumford SL, Vladutiu CJ et al. Perceived stress, reproductive hormones, and ovulatory function: a prospective cohort study. Epidemiology. 2015;26(2):177–184. doi: 10.1097/EDE.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baran C, Hellstrom WJ, Sikka SC. A comparative evaluation of semen parameters in pre- and post-Hurricane Katrina human population. Asian J Androl. 2015;17(4):676–680. doi: 10.4103/1008-682X.143738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guilford G. Hurricane Sandy turned a New York subway station into a petri dish of Antarctic bacteria. Quartz. 2015 Available at: https://qz.com/340259/hurricane-sandy-turned-a-new-york-subway-station-into-a-petri-dish-of-antarctic-bacteria. Accessed April 20, 2020. [Google Scholar]
- 31.Janerich DT, Stark AD, Greenwald P, Burnett WS, Jacobson HI, McCusker J. Increased leukemia, lymphoma, and spontaneous abortion in Western New York following a flood disaster. Public Health Rep. 1981;96(4):350–356. [PMC free article] [PubMed] [Google Scholar]
- 32.Grech V, Zammit D. A review of terrorism and its reduction of the gender ratio at birth after seasonal adjustment. Early Hum Dev. 2017;115:2–8. doi: 10.1016/j.earlhumdev.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Henretig FM, Calello DP, Burns MM, O’Donnell KA, Osterhoudt KC. Predictable, preventable, and deadly: epidemic carbon monoxide poisoning after storms. Am J Public Health. 2018;108(10):1320–1321. doi: 10.2105/AJPH.2018.304619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buekens P, Miller CA. Pre-natal care in occupied Belgium during the Second World War. Eur J Public Health. 1996;6(2):105–108. [Google Scholar]
- 35.Zotti ME, Williams AM. Reproductive Health Assessment After Disaster: introduction to the RHAD toolkit. J Womens Health (Larchmt) 2011;20(8):1123–1127. doi: 10.1089/jwh.2011.3021. [DOI] [PubMed] [Google Scholar]


