Abstract
Objectives:
Serious infectious complications of opioid use disorder (OUD), and specifically endocarditis, are becoming more common in the U.S. Individuals with OUD-associated endocarditis require long periods of complex medical care, often face recurrent addiction- and infection-related complications, and have dismal clinical outcomes. The objective of this study was to perform journey mapping analysis to capture common trajectories and patterns of care for people with OUD-associated endocarditis.
Methods:
This was an analysis of qualitative semi-structured interviews of individuals who received care for OUD-associated endocarditis. Interviews were conducted among individuals receiving care at a single academic healthcare system in Boston, Massachusetts. Ten participants meeting DSM-5 criteria for at least mild OUD and a culture-positive diagnosis of endocarditis who had previously completed care for OUD-associated endocarditis were recruited from inpatient and ambulatory settings. Details of participant’s care episodes were extracted and visualized in an iterative journey mapping process. A grounded theory approach was then used to identify shared themes and care patterns among participants’ journey maps.
Results:
Common patterns of care included early addiction treatment and intensive outpatient care preceding periods without rehospitalization, while leaving outpatient care and return to drug use often directly preceded rehospitalization. Participants frequently left care by choice and proactively reengaged with care.
Conclusions:
Journey mapping is a novel, patient-centered approach to capturing the care experiences and trajectories of a patient population experiencing significant stigma, who engage with the healthcare system in unexpected and fragmented ways. For individuals with OUD-associated endocarditis, we identified critical moments to support and engage patients to prevent return to drug use and rehospitalization.
Keywords: Opioid use disorder, endocarditis, journey mapping, stigma, qualitative research
Introduction:
Rising non-medical use of prescription opioids, heroin, and illicitly manufactured fentanyl are a national public health crisis (Compton et al, 2016) (Rudd, 2016) (Frank and Pollack, 2017) (Martin et al, 2017) and have contributed to a decreasing life expectancy among Americans over the past three years (Murphy et al, 2018). Beyond deaths from opioid and polysubstance overdoses, there has been at least a doubling of serious bacterial infections resulting from drug use, including endocarditis, osteomyelitis, septic arthritis and epidural abscesses (Ronan and Herzig, 2016).
Care for patients with opioid use disorder (OUD)-associated endocarditis is particularly complex and costly to the healthcare system (Wurcel et al 2016) (Fleischauer et al, 2017) (Schranz et al, 2019), and optimal care for individuals with comorbid addiction and addiction-associated infectious conditions is not well understood (Libertin, 2017). A single episode of care may include a long hospitalization followed by prolonged post-acute hospital care at skilled nursing facilities and linkage to longitudinal addiction, primary, psychiatric, infectious disease and cardiac care.
Outcomes among individuals with OUD-associated endocarditis without appropriate treatment of underlying addiction are dismal (Rosenthal, 2016), and discrimination towards individuals with OUD and internalized shame also negatively impact care for patients with OUD-associated endocarditis (Van Boekel et al 2013) (Kelly et al, 2015) (Botticelli and Koh, 2016) (Wakeman and Rich, 2017).
In order to better understand the experiences of care for patients with addiction-associated infections, we conducted qualitative semi-structured interviews of individuals with OUD-associated endocarditis and healthcare providers who deliver care to these individuals at a single healthcare system between 2017 and 2018. In our initial published analysis (Bearnot et al, 2019), we identified five major themes that may explain poor clinical outcomes experienced by individuals with OUD-associated endocarditis. These themes included: stigma-related inequities and delays in care, social and medical comorbidities experienced by patients, return to substance use as an anticipated outcome of participants’ addiction, differing perspectives on and challenges of long hospitalizations for OUD-associated endocarditis, and a lack of care integration within a single institution in addition to discontinuities of longitudinal care across multiple institutions.
Importantly, we noted that none of the patient participants’ clinical courses followed the theoretical episode of care framework that informed our semi-structured interview guides, but rather described more complicated and fragmented care. Given the complexities of the individual participants’ narratives, we were unable to accurately represent their unique episodes of care in our prior manuscript or allow for direct comparisons between their journeys.
To address this issue directly, we used journey mapping (Følstad and Kevale, 2018), a well-developed technique for creating compelling and easy-to-understand diagrams of individuals’ movement through a complex system. This approach was developed for use in business and marketing settings to understand and improve on customer experiences (Rawson et al, 2013), starting with initial contact and continuing through long-term engagement. It has been used in a limited, but growing, number of healthcare applications as a way to better capture the patient experience in an increasingly complicated healthcare system (Murray et al, 2005) (British Columbia Patient Safety and Quality Council, 2018). The objective of this analysis was to perform journey mapping to capture common trajectories and analyze patterns of care among individuals with OUD-associated endocarditis.
Methods:
Context:
This qualitative study was conducted at Massachusetts General Hospital (MGH), a large academic healthcare system in Boston, Massachusetts. Since 2012, MGH has developed a comprehensive and integrated outpatient and inpatient substance use disorders initiative (Wakeman et al, 2017) (Jack et al 2017) (Snow et al, 2019).
Data Collection:
Data were drawn from semi-structured interviews of both patients with OUD-associated endocarditis and their multidisciplinary healthcare providers, described more fully elsewhere (Bearnot et al, 2019). Interviews from 10 patients who met inclusion criteria of having a culture-positive diagnosis of infective endocarditis at MGH and at least mild OUD per DSM-5 criteria, were extracted and analyzed in this subgroup analysis. One participant was excluded from this analysis because they were not diagnosed with OUD until many years after receiving care for endocarditis.
Participants were asked to retrospectively recall and comment on the particular details and experiences of their care from their first hospitalization for OUD-associated endocarditis through the time of interview. The semi-structured interview questions and subsequent probes prompted participants to recall the details, approximate dates and locations of each hospitalization, post-acute care and outpatient care plan at MGH and non-MGH sites. Patients were also asked to recall their drug use and addiction treatment history. All interviews were conducted between 2017 and 2018 by the study investigators, with participants asked to recall details of their substance use and OUD-associated endocarditis care leading up to the time of the interview. The interviews were recorded, deidentified and transcribed verbatim. Demographic survey data were linked to each deidentified transcript by a unique participant code before being uploaded to a secure database for analysis.
The study was approved by the Partners Healthcare Institutional Review Board, and verbal consent was obtained from all study participants.
Recruitment:
Patients were recruited from both the inpatient and outpatient settings. Outpatient participants were identified and recruited through their primary care provider (PCP) while inpatients were identified and recruited by a research coordinator. Inclusion criteria was confirmed by study staff and a purposeful effort was made to recruit a diverse cohort of patients, including participants who experienced a range of care settings and trajectories. Recruitment and interviews were continued until thematic saturation was achieved per grounded theory methodology.
Inclusion Criteria:
Inclusion criteria included a completed prior episode of care for a culture-positive diagnosis of infective endocarditis and a concurrent diagnosis of at least a mild OUD per the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria (American Psychiatric Association, 2013).
Data Analysis:
Interview transcripts and survey data were reviewed independently by study investigators. Details of patients’ care experiences, dates of presentations, care settings, diagnoses, care plans and substance use histories were extracted for this analysis. An interim review of these data helped inform a preliminary assessment of various journey mapping modalities representing the trajectories, episodes and settings of care and substance use. One narrative and two graphical modalities were considered. These modalities were modified in an iterative process, and compared with other published examples, to produce a single accurate and mutually agreed upon journey mapping structure. The care details for each patient were subsequently transposed on to this same journey mapping structure and reviewed by the study investigators for accuracy and consistency. The maps, which did not include any personal health information, were created using Google Slides graphic tools.
Using a grounded theory approach (Ando et al, 2014), each map was subsequently reviewed and emerging visual patterns and themes were discussed in detail by study staff. Each map was then cross-referenced against the other journey maps and compared with a theorized episode of care. Significant thematic agreement was appreciated between the study investigators and a finalized visual codebook was agreed upon in an iterative, constant-comparative process (Glaser and Strauss, 1967).
Results:
Participant Characteristics:
We reviewed the care experiences and episodes of care for 10 individuals, 5 outpatients and 5 inpatients. Table 1 provides a summary of participant characteristics. Their median age was 37 [IQR 29–42], with 5 participants identified as female and 8 as non-Hispanic white. Six of the patients were homeless at the time of interview. All patients reported a history of using intravenous heroin or a synthetic opioid such as fentanyl, and 8 reported receiving treatment with a medication for opioid use disorder (MOUD).
Table 1:
Participant Characteristics
| Participant Characteristics | N=10 |
|---|---|
| Age, median [IQR] | 37 [29–42] |
| Female | 5 |
| Non-Hispanic White | 8 |
| Unemployed/Disability | 8 |
| Unstable Housing | 6 |
| Public Insurance/Medicaid | 10 |
| History of Buprenorphine Treatment | 7 |
| History of Methadone Treatment | 1 |
The median number of hospital presentations during the study period per participant, including emergency department presentations and hospital admissions, was 3 [IQR 2–5]. Three individuals received surgical heart valve replacement, with two requiring a prosthetic valve repair or repeat surgery due to reinfection. All ten participants received intravenous antibiotics for their infective endocarditis and were seen by an inpatient infectious disease consultant. At least four received a peripherally inserted central catheter (PICC) in the hospital and only one was discharged home with a PICC to complete their antibiotic course. Eight individuals transitioned from inpatient care at MGH to a post-acute hospital care setting, such as a skilled-nursing facility or rehabilitation hospital. Eight individuals left a care setting by choice. All ten participants reported receiving some outpatient care, particularly specialty addiction services, from a non-MGH affiliated community resource. Four of the five outpatient participants who continued care at MGH after their hospitalization were cared for by a primary care physician waivered to prescribe buprenorphine. All patients reported returning to substance use sometime after their initial hospitalization.
Journey Map Design:
A simple two-dimensional graphing method was used with color blocking and labeling to add additional detail. These journey maps illustrate the trajectories, settings, and time course of each participant’s episode of care for OUD-associated endocarditis and concurrent substance use. We labeled the vertical axis as care needs, establishing a gradient of increasingly intensive health care resources offered in different care settings. Routine outpatient care represents typical and less frequent primary and addiction care visits, while intensive outpatient care designates more frequent and coordinated interdisciplinary care with specialists and primary care providers. The horizontal axis was labelled as time, with months or years used depending on the time scale of the participant’s care episode. Within an individual journey map, a single line represents a participant’s trajectory of care; it connects horizontal time periods in care settings and highlights transitions from one setting to another with sloped or vertical jumps. There is no inherent value in a line’s slope. A solid line was used to represent periods when the participant reported not using substances, while a dotted line was used to represent periods of reported substance use. Periods of engagement or no engagement in addiction treatment were illustrated using purple and orange color blocking, respectively. A red ‘L’ on the graph was used to indicate any time when the participant reported leaving care by choice. Finally, red boxes were used to draw readers’ attention to the specific features of the journey map illustrative of each theme.
Theme 1: Two common patterns of care emerge, with early addiction treatment and intensive outpatient care observed to precede periods without re-hospitalization.
Two divergent patterns of care were observed when reviewing the mapped trajectories and episodes of care. The first pattern starts with hospitalization for OUD-associated endocarditis characterized by early addiction treatment, followed by a measured stepwise transition from the hospital to post-acute hospital care before several months of intensive outpatient care. Intensive outpatient care, while unique for each patient, typically included regular interdisciplinary care with specialists, addiction medicine and primary care providers, often with additional patient navigation support. This pattern was observed to precede periods of no re-hospitalization. The second pattern was characterized by a lack of addiction treatment during hospitalization and no period of intensive outpatient care after discharge from the hospital. This second pattern was observed to precede frequent re-hospitalization.
The first pattern was best illustrated by the journey map of participant 003, a 35 year old non-Hispanic white woman (Figure 1, Insert A). This individual had a relatively brief hospitalization requiring intensive care. She received early addiction treatment and was seen by both an inpatient infectious disease and addiction medicine consult team. This hospital stay lasted three weeks and was followed by several months in a post-acute care setting where the participant completed her antibiotic course, continued addiction treatment and was engaged in rehabilitation care. This was followed by a transition to intensive outpatient care for nearly ten months. During this time period, the participant continued to see specialty providers and was engaged in an intensive outpatient addiction treatment program. The participant did not return to substance use during this time and remained out of the hospital.
Figure 1: Journey Maps Illustrative of Theme 1:
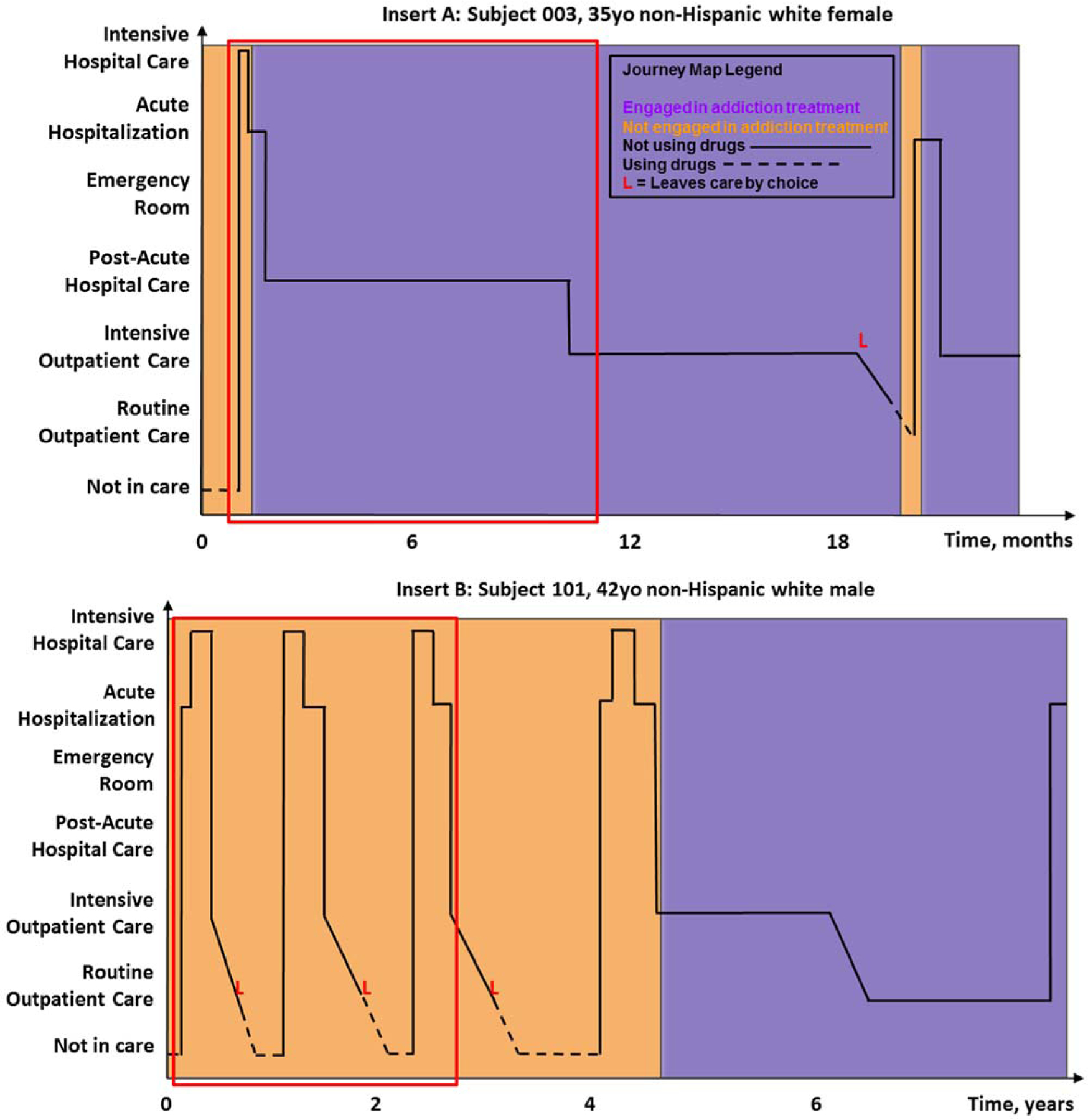
Two common patterns of care emerge, with early addiction treatment and intensive outpatient care observed to precede periods without re-hospitalization.
The second pattern was best illustrated by the journey map of participant 101, a 42 year old non-Hispanic white man (Figure 1, Insert B). This individual was initially hospitalized at a community hospital in intensive care and remained there for several weeks before transfer to MGH for consideration of surgical heart valve replacement. He did not receive any addiction treatment during this hospitalization and an addiction consult service was not available at either the referring community hospital or MGH at the time of his initial care. The participant was eventually discharged directly home with a limited plan for outpatient follow-up. There was no plan for outpatient addiction care and the participant reported not seeking out any community resources. Upon return home, he remained disengaged from care and eventually left care by choice. The participant returned to substance use shortly thereafter. He required three intensive and lengthy re-hospitalizations, observed to exhibit a similar care pattern, over the next three to four years.
Theme 2: Participants proactively leave and re-engage in care.
Multiple participants described making intentional and proactive choices to leave or re-enter care following diagnosis of OUD-associated endocarditis, highlighting the importance of an individual’s autonomy in making decisions about their care. Patients who left care by choice commonly reported undertreatment of their withdrawal or pain symptoms, discriminatory behaviors by healthcare providers, or prolonged periods in care triggering underlying post-traumatic stress, which led to patient directed discharges from the hospital or choosing not to follow up in outpatient care settings. Conversely, several participants who were without care for a period of time reported seeking out and re-engaging in care, often after returning to substance use and looking for additional resources to assist with recovery from opioids or other substances.
Participant 105, a 41 year old non-Hispanic white woman experiencing homelessness, provided illustrative examples of individuals leaving care by choice (Figure 2, Insert A). This participant left care by choice prior to hospital admission three times in rapid succession at the outset of her OUD-associated endocarditis symptoms due to undertreatment of opioid withdrawal by healthcare providers. After this initial delay, she was then admitted for emergent valve replacement surgery within days of her hospitalization. Post-operatively, this participant had a long hospitalization followed by post-acute hospital care and then intensive outpatient follow-up where she engaged in intensive addiction treatment as well as cardiac and infectious disease specialty care.
Figure 2: Journey Maps Illustrative of Theme 2:

Participants purposefully leave and re-engage in care.
Alternatively, several patients sought out outpatient addiction care during times of recurrent substance use. This was demonstrated most clearly by participant 001, a 29 year old white non-Hispanic woman (Figure 2, Insert B), who returned to addiction care on three separate occasions. This participant experienced several long periods of remission from OUD, and sought out addiction care promptly following her return to substance use on multiple occasions. In one particularly poignant moment, she described going out to meet her dealer to continue to use drugs but instead goes to the emergency department for care, explicitly attempting to reconnect to addiction treatment.
Theme 3: Leaving intensive outpatient care and returning to substance use often directly precede re-hospitalization.
Among participants re-hospitalized following their initial diagnosis of OUD-associated endocarditis, there were common patterns of outpatient care utilization and substance use observed in the time immediately preceding re-hospitalization. Individuals often disengaged from intensive outpatient care prior to returning to opioid use, and this recurrent drug use commonly directly preceded re-hospitalization related to addiction and infection-related morbidity.
This first step in this process, a departure from intensive outpatient care, was best demonstrated in the journey map of participant 102, a 27 year old non-Hispanic biracial man (Figure 3, Insert A). Following his first prolonged episode of care for OUD-associated endocarditis, this participant described being homeless, dividing his time between two different family member’s homes. This housing instability made it difficult for him to attend his outpatient follow up appointments, resulting in care lapses. This, in turn, led to several seizures from running out of antiepileptic medication and a return to alcohol and cocaine use related to spending time among the people, places and things that triggered his substance use in the past. This period of return to use directly preceded re-hospitalization.
Figure 3: Journey Maps Illustrative of Theme 3:

Leaving intensive outpatient care and returning to substance use often directly precede re-hospitalization.
This trajectory of care was not isolated. Multiple participants returned to substance use after leaving intensive outpatient care, and this disengagement commonly resulted in re-hospitalizations for worsening addiction or infection symptoms. This is best illustrated in the journey map of participant 104, a 28 year old non-Hispanic man (Figure 3, Insert B). This individual was receiving addiction care in New Hampshire for approximately one year following his initial episode of OUD-associated endocarditis care, but continued to misuse opioid pain medications while on buprenorphine treatment. The patient reported being “kicked out” of his treatment program rather than being offered increased intensity of addiction treatment. This in turn led to an escalation of substance use including a return to injection heroin use, and, shortly thereafter, recurrent mitral valve endocarditis, requiring another lengthy hospitalization.
Conclusions:
While journey mapping approaches are commonly used in the corporate world, we believe this to be a novel approach to capture the care experiences and trajectories of a stigmatized patient population, who commonly engage with the healthcare system in unexpected and fragmented ways. The journey mapping approach was particularly helpful for putting the individuals’ experiences at the center of this analysis, highlighting the importance of patients’ experiences in understanding why clinical outcomes among individuals with OUD-associated endocarditis are often so poor.
We identified the potential importance of engagement in early inpatient and outpatient addiction care to prevent recurrent hospitalizations for OUD-associated endocarditis. Some of the notable strategies to engage individuals in early addiction treatment included prompt treatment of pain and withdrawal symptoms, the availability of addiction consultation in the hospital, and low-threshold addiction treatment, including bridge clinics, emergency rooms, and healthcare for the homeless programs with integrated addiction treatment.
Multiple participants returned to substance use after leaving intensive outpatient care, and this disengagement commonly resulted in re-hospitalizations for worsening addiction or infection symptoms. This recurrent pattern of care attrition represents an opportunity to prevent re-hospitalization by identifying critical moments where individuals need additional support after a return to using drugs, but prior to re-hospitalization. As one participant incisively told us, “You’re always jumping through hoops. Something’s always going on. It’s never straight forward, get your prescription, go to the pharmacy, pick it up, and have it on time. It just really doesn’t work that way.” Participants identified family members, social workers, patient navigators and recovery coaches as providing much needed support in these highly vulnerable periods. Healthcare providers should be encouraged and trained to partner with these complementary sources of longitudinal support in order to keep patients engaged in care, provide continuity, and help prevent a return to drug use and rehospitalization.
Participants described multiple instances of making intentional, proactive decisions about their care, including leaving care by choice and re-engaging in addiction care during periods of drug use. These decisions were often made in reaction to feelings of isolation. One participant shared a particularly poignant and illustrative memory of turning for help at a critical moment after returning to drug use: “So I left and was going to meet my [drug] dealer but I got on the train and went to the [hospital] instead and I walked into the emergency room and told them I needed help, that I didn’t want to do this anymore.” While the journey maps illustrate this pattern of proactive decision-making, they regrettably do not clearly capture the role that stigma towards individuals with OUD plays in their care. We highlight this important issue here, and note that nearly all participants reported feeling discriminated against during their care and perceived being treated differently than patients without substance use disorders. One participant shared their experience with stigma in the hospital: “As soon as it became known that I was [in the hospital for] IV drug use that resulted in endocarditis, I noticed a difference in care from everyone really, […] and some of the staff would antagonize me, like take hours and hours to give me my meds knowing that I’m a drug addict and I need my opioids.” We cannot emphasize enough the importance of using medically accurate, person-first, non-judgmental language in conducting this work, with the goal of framing addiction as a chronic treatable illness, and recognize individuals with OUD as valued and valuable members of the community (Van Boekel et al 2013) (Kelly et al, 2015) (Botticelli and Koh, 2016) (Wakeman and Rich, 2017). This includes avoiding the description of patients being ‘discharged against medical advice,’ instead using more descriptive and less pejorative terms such as ‘patient directed discharge’ or ‘leaving care by choice’. Additionally, patient reports of discrimination, undertreatment of pain, and trauma from being cared for in confined environments during hospitalizations highlight opportunities for care innovation and improvement.
There are several limitations to this journey mapping study: we anticipate recall bias when asking participants to remember past experiences and remote care details; interviews were conducted in a Medicaid expansion state within a single hospital system with a comprehensive substance use disorders initiative; we are unable to examine the association between experiences of care and the clinical outcomes using these qualitative methods. However, we found journey mapping to be a valuable tool for deepening our understanding of the care experiences and trajectories of individuals with OUD-associated endocarditis, and was relatively straightforward to perform with semi-structured interview transcripts. We strongly recommend that future work in this area incorporate patient perspectives towards addiction treatment and harm reduction strategies in order to hasten the implementation of all acceptable interventions. There is no time to waste.
Acknowledgements:
The authors would like to thank Dr. Elyse Park and Dr. Nancy Rigotti for reading earlier versions of this manuscript.
Support: Dr. Bearnot’s work is supported by NIH and NIDA under award number K12DA043490.
References:
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Arlington, VA: APA; 2013. [Google Scholar]
- Ando H, Cousins R, Young C. Achieving saturation in thematic analysis: Development and refinement of a codebook. Comp Psychol. 2014;3:4. [Google Scholar]
- Bearnot B, Mitton JA, Hayden M, Park ER. Experiences of care among individuals with opioid use disorder-associated endocarditis and their healthcare providers: Results from a qualitative study. J Substance Abuse Treat. 2019;102: 16–22. [DOI] [PubMed] [Google Scholar]
- Botticelli M, Koh H. Changing the language of addiction. JAMA. 2016; 316(13): 1361–2. [DOI] [PubMed] [Google Scholar]
- British Columbia Patient Safety and Quality Council. Journey Mapping Substance Use Treatment. https://bcpsqc.ca/wp-content/uploads/2018/03/Journey-Mapping-Substance-Use-Treatment-Report-1.pdf Accessed August 21, 2019. [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. Longo DL, ed. N Engl J Med. 2016; 374(2): 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for Endocarditis and Associated Health Care Costs Among Persons with Diagnosed Drug Dependence — North Carolina, 2010–2015. Morb Mortal Wkly Rep. 2017;66(22):569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Følstad A, Kvale K. Customer journeys: a systematic literature review. J Service Theory Pract. 2018. March 12;28(2):196–227. [Google Scholar]
- Frank RG, Pollack HA. Addressing the fentanyl threat to public health. New Engl J Med. 2017; 376(7): 605–7. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The constant comparative method of qualitative analysis. The discovery of grounded theory: Strat Qual Res. 1967;101:158. [Google Scholar]
- Jack HE, Oller D, Kelly J, Magidson JF, Wakeman SE. Addressing substance use disorder in primary care: The role, integration, and impact of recovery coaches. Subst Abuse. 2017; 13:1–8. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Wakeman SE, Saitz R. Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. Am J Med. 2015;128(1):8–9. [DOI] [PubMed] [Google Scholar]
- Libertin CR, Camsari UM, Hellinger WC, Schneekloth TD, Rummans TA. The cost of a recalcitrant intravenous drug user with serial cases of endocarditis: Need for guidelines to improve the continuum of care. IDCases. 2017;8:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in US lifetime heroin use and heroin use disorder: prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psych. 2017;74(5):445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Xu JQ, Kochanek KD, Arias E. Mortality in the United States, 2017 NCHS Data Brief, no 328. Hyattsville, MD: National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005; 330 (7498): 1007–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson A, Duncan E, Jones C. The truth about customer experience. Harvard Bus Rev. 2013; 91(9): 90–8. [Google Scholar]
- Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002–12. Health Aff (Millwood). 2016;35(5):832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal ES, Karchmer AW, Theisen-Toupal J, Castillo RA, Rowley CF. Suboptimal addiction interventions for patients hospitalized with injection drug use-associated infective endocarditis. Am J Med. 2016;129(5):481–485. [DOI] [PubMed] [Google Scholar]
- Rudd RA. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morb Mortal Wkly Rep. 2016; 65 (50–51);1445–1452. [DOI] [PubMed] [Google Scholar]
- Schranz AJ, Fleischauer A, Chu VH, Wu LT, Rosen DL. Trends in drug use–associated infective endocarditis and heart valve surgery, 2007 to 2017: a study of statewide discharge data. Ann Int Med. 2019. January 1;170(1):31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snow RL, Simon RE, Jack HE, Oller D, Kehoe L, Wakeman SE. Patient experiences with a transitional, low-threshold clinic for the treatment of substance use disorder: A qualitative study of a bridge clinic. J Substance Abuse Treat. 2019; 107: 1–7. [DOI] [PubMed] [Google Scholar]
- Van Boekel LC, Brouwers EP, Van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1):23–35. [DOI] [PubMed] [Google Scholar]
- Wakeman SE, Rich JD. Barriers to Post-Acute Care for Patients on Opioid Agonist Therapy; An Example of Systematic Stigmatization of Addiction. J Gen Intern Med. 2017;32(1):17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Int Med. 2017;32(8):909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurcel AG, Anderson JE, Chui KKH, et al. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open Forum Infect Dis. 2016;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]


