Abstract
BACKGROUND:
The purpose was to explore whether baseline sociodemographic and physical characteristics moderated effects of an intervention on moderate-to-vigorous physical activity (MVPA), percent body fat, body mass index z-score, and cardiorespiratory fitness (CRF) at post-intervention, relative to the control condition.
METHODS:
A secondary analysis of data from a group randomized trial including 24 schools (12 intervention and 12 control; N=1519 girls) was conducted. Age, ethnicity, race, socioeconomic status, and pubertal stage were assessed via survey. Height, weight, MVPA (min/hr), percent body fat, and CRF were measured. Mixed-effects linear models were performed.
RESULTS:
Compared to the control, the intervention increased overweight and obese girls’ CRF (F=4.36, p=.037; F=6.56, p=.011, respectively), but not healthy weight girls’ CRF (F=0.01, p=.925). Pre- to mid-puberty girls in the intervention group had slightly lower post-intervention MVPA than those in the control (3.04 vs. 3.31, p=.055), while late to post-puberty intervention and control girls’ post-intervention MVPA was similar (3.12 vs. 3.04, p=.542).
CONCLUSIONS:
A PA intervention can improve overweight and obese girls’ CRF, possibly attenuating their cardiovascular risk. Effective strategies are needed to assist adolescent girls, especially those in pre- to mid-puberty, in maintaining their MVPA after an intervention ends.
INTRODUCTION
Regular participation in moderate-to-vigorous physical activity (MVPA) is associated with improvements in body weight status, percent body fat, and cardiorespiratory fitness (CRF) among adolescents (1). To reap these health benefits, the World Health Organization recommends that adolescents attain 60 minutes or more of MVPA daily (2). Yet, globally, data from 2016 indicated 84.7% of adolescent girls, compared to 77.6% of boys, reported insufficient PA. Similarly, in the U.S., a higher percentage of adolescent girls (80.5%) than boys (64.0%) reported insufficient PA. In addition, from 2011 to 2016, both the global and U.S. prevalence of insufficient PA decreased for boys, but remained the same for girls (3). These dismal findings highlight the need for effective interventions to increase PA, particularly among adolescent girls (4).
Although no definitive explanation exists for the findings concerning adolescent girls, sociodemographic and physical characteristics have been suggested as playing a role (5). For example, girls’ PA participation has been found to decline with increasing age across adolescence (6–7). According to the 2017 U.S. Youth Risk Behavior Survey (8) involving high school students, the prevalence of attaining PA for at least 60 minutes on every day of the week was higher among girls who were Non-Hispanic White (18.4%) than those who were Non-Hispanic African American (15.5%) or of Hispanic ethnicity (18.1%). In a recent U.S. study (9), the odds ratio for eligible to receive free and reduced-price lunches at school (a widely used proxy for socioeconomic status [SES] based on U.S. Income Eligibility and Poverty Guidelines [10]), compared to not eligible, predicting failure to meet aerobic fitness standards approached statistical significance for 4th and 5th grade girls, but not boys (9). In another U.S. study, receipt of free and reduced-price lunches at school was significantly associated with higher odds of obesity among adolescent girls (11). However, findings from a systematic review examining the effects of SES on adolescents’ PA were not uniform across the included studies (12). In addition, a global investigation involving 146 countries showed no consistent pattern in adolescent girls’ PA based on country income (3). These discrepancies underscore a need for continued research to increase understanding of these relationships.
Pubertal development during adolescence may also influence PA due to various sexually dimorphic changes occurring during this period, but rigorously conducted studies investigating this association are sparse. In a recently conducted longitudinal study, pubertal stage measured by the Peterson et al. Pubertal Development Scale (13) was not significantly associated with MVPA in Finnish adolescent girls at baseline in 5th grade or at follow-up in 7th grade (14). Interestingly, in a study with South African adolescent girls, pubertal stage was significantly associated with an increase in sedentary time but not PA (15). Unfortunately, one major limitation of the two studies focusing on pubertal stage was that PA was assessed via self-report, possibly resulting in inaccurate measurement due to social desirability and recall bias (16).
Excessive weight gain among adolescents has been associated with reduced levels of MVPA. A 2018 systematic review showed that the mean minutes per day that adolescents engaged in MVPA, measured via accelerometers, did not reach 60 minutes in 18 of 20 included studies. Moreover, in 10 of 16 studies that compared accelerometer-measured MVPA in obese versus non-obese groups, mean daily time spent attaining MVPA was significantly lower in obese than non-obese adolescents. The findings from the review provide strong evidence that the vast majority of obese adolescents are not achieving the U.S. or international PA recommendations (17).
Collectively, the information suggests that adolescents’ responses to an intervention to increase their PA may vary based on these sociodemographic and physical characteristics. However, it is important to note that although these characteristics are associated with or can predict variation in the behavior itself, they may not have the same direction or magnitude of effect on variation in response to a PA intervention (18). To advance the science focusing on adolescent girls, who are at high risk for health problems related to inadequate PA, this study focuses on exploring the effect of these potential moderators on adolescent girls’ responses to a PA intervention.
To address the low levels of PA noted among adolescent girls, interventions to promote PA have been tested in community settings. To examine intervention effectiveness in increasing adolescent girls’ PA, systematic reviews and meta-analyses (5–7) were recently conducted. Voskuil and colleagues’ (6) systematic review included PA intervention studies in which PA was objectively measured in 6- to 18-year-old girls. Voskuil et al. (6) found that only one study resulted in significant MVPA differences between intervention and control groups, but the mean MVPA differences were only 1.6 minutes/day. One major explanation provided by the researchers for the modest effects of the interventions included in the review was that the dose received by the participating girls might not have been intense enough to produce the anticipated effects. Owen et al. (5) and Pearson et al. (7) each conducted a meta-analysis including studies involving adolescent girls who had their PA assessed either via self-report or an objective measure. Findings from the two meta-analyses showed significant, but small, intervention effects on PA (g=0.09, 0.35). Pearson et al. (7) found that the intervention effect was even smaller (g=0.29) in studies that used an objective measure instead of self-report (g=0.38), suggesting that self-report’s weak validity due to recall bias may have inflated the effect. Only the Pearson et al. (7) study included moderation analyses, which showed stronger effects for interventions designed for younger than older girls (g=0.42) and those that used multicomponent strategies (g=0.62), were theory-based (g=0.42), had moderate (g=0.42) or high (g=0.52) study quality. Although these results regarding the girls’ age are important to note, no additional findings based on other participant characteristics were reported.
The limited effectiveness of PA interventions for adolescent girls to date and the complexity of PA behavior necessitate examination of potential moderators of intervention effects (19). Moderation analyses can be useful for determining the type of intervention that may be successful in a subgroup (20) and for tailoring an intervention to optimally meet each participant’s needs. Yet, little research has been conducted to explore moderators in PA interventions, and baseline physical and sociodemographic characteristics that may moderate responses of adolescent girls to interventions remain relatively unknown (21). The current study was designed to address the gap in information concerning moderators of PA interventions among adolescent girls. Specifically, this study’s purpose was to explore whether certain baseline participant sociodemographic (age, ethnicity, race, socioeconomic status determined by free and reduced-price school lunch eligibility) and physical (pubertal stage, weight status) characteristics moderated the effects of an intervention on moderate-to-vigorous physical activity (MVPA), percent body fat, body mass index (BMI) z-score, and cardiorespiratory fitness (CRF) at post-intervention, relative to the control condition. The research question was: What baseline participant sociodemographic (age, ethnicity, race, free and reduced-price school lunch eligibility) and physical (pubertal stage, weight status) characteristics moderate the effects of a PA intervention on MVPA (primary outcome), percent body fat, BMI z-score, and CRF (secondary outcomes) at post-intervention, relative to the control condition?
METHODS
Design
A secondary analysis of data from a 5-year (2011–2016) school-based group randomized controlled (RCT) trial that included adolescent girls was conducted. The primary aim of the trial’s intervention was to increase post-intervention MVPA. Secondary aims were to improve post-intervention BMI z-score, percent body fat, and CRF. Although no differences between intervention and control groups occurred in MVPA or BMI z-score, percent body fat increased less and CRF decreased less among intervention than control girls (4,22). The intervention effects on MVPA, percent body fat, BMI z-core, and CRF have been published (4,22).
The Michigan State University Biomedical Institutional Review Board provided ethical approval to conduct the trial that involved 24 public schools located in low-income urban areas in the Midwestern U.S. School administrators gave permission to conduct the trial in their respective school districts.
Participants, setting, and procedures
During assemblies in each school, researchers presented the trial to 4192 5th–8th grade girls and invited them to participate. A total of 4146 girls received packets including a consent and assent form and screening tool designed to determine eligibility based on the following inclusion criteria: 1) not attaining 60 minutes per day of MVPA; 2) not engaging in MVPA ≥3 days per week during sports, lessons, or other forms of organized PAs; 3) available and interested in participating in a PA club after school 3 days per week for 17 weeks; 4) able to read, speak, and understand English; and 5) having no health issue preventing safe involvement in MVPA. A total of 2024 girls agreed to participate and returned packets with signed informed consent and assent forms and completed screening tools. After excluding 505 girls (e.g, did not meet inclusion criteria, withdrew before baseline data collection), 1519 girls remained in the trial.
Schools were paired based on having similar school characteristics (e.g., school size, demographics). During the beginning of each academic school year over a 3-year period, trained research assistants collected baseline data on the girls’ sociodemographic and physical characteristics (8 different schools per year). A statistician then randomly assigned the schools in each pair to receive either a 17-week PA intervention (n=12 [4 schools per year]; n=753 girls) or control condition including usual school offerings only (n=12 [4 schools per year]; n=766 girls). Data were collected at baseline before the intervention had started and again at post-intervention immediately after the intervention had ended. Details about procedures, along with a flow diagram depicting girls’ participation in the trial, have been published (22–23). The trial was registered: ClinicalTrials.gov Identifier NCT01503333.
Intervention
The 17-week PA intervention included three components. One component involved two face-to-face motivational interviews conducted by a health professional/counselor with each girl at her school at the beginning and end of the intervention period. Motivational interviewing, which is a collaborative communication style used to strengthen an individual’s own motivation to positively change behavior (24), has been used with adolescent girls in a prior PA intervention that resulted in a decrease in their sedentary behavior (25). The second component was an Internet-based session that delivered motivational feedback messages based on each girls’ responses to survey questions at the intervention midpoint; and the third component included a 90-minute after-school PA club offered three days per week at each school. Details about the intervention can be found elsewhere (23).
Measurements
Baseline data on four potential moderators, including age, race, ethnicity, and enrollment in the free or reduced-price lunch program at school were obtained from responses to single items on the consent form or screening tool. Baseline data on two potential moderators (e.g., pubertal stage and weight status) and post-intervention data on the four outcomes of interest (e.g., MVPA, BMI z-score, percent body fat, and CRF) were obtained from girls at each school.
Pubertal Stage.
The reliable and valid (26) 5-item Pubertal Development Scale was used (13) to assess each girl’s pubertal stage. Girls rated themselves, as compared to other girls of similar age, on body hair, breast development, and menstruation. For body hair and breast development, they selected one of four choices: 1) no, not yet started; 2) yes, barely; 3) yes, definitely; and 4) development complete. For menstruation, they chose: 1) no or 4) yes (menstrual period started). Girls who noted no menstruation and had a summed score for body hair and breast development of 2, 3, or >3 were in the pre-pubertal, early, or mid-pubertal stage, respectively. Girls who reported menstruation and had a summed hair and breast development score of ≤7 or 8 were in the late or post-pubertal stage, respectively (26). The scale has a McDonald’s omega of 0.65 in the study.
Weight Status, BMI z-score, and percent body fat.
Each girls’ height was measured twice to the nearest 0.1 cm with a Shorr Board (Shorr Productions, Olney, MD). Weight and percent body fat were assessed with a portable digital foot-to-foot bioelectric impedance analysis scale (Model Number BC-534; Tanita Corporation, Tokyo, Japan). Body weight was assessed twice to the nearest 0.1 kg. The two measures of height and weight were averaged. BMI was estimated by calculating kg/meters2. To determine BMI z-scores and BMI percentiles (BMI-P) for age, a SAS program for the Centers for Disease Control and Prevention Growth Charts (available online) was used (27). Based on the charts, girls were classified as underweight, healthy weight, overweight, or obese if their BMI-P was <5th, 5th to <85th, 85th to <95th, or ≥95th, respectively (28). Percent body fat was estimated to the nearest 0.1% via the same scale, which was found to be reliable and valid with adolescents.
Minutes per hour of MVPA were measured with ActiGraph GT3X+ accelerometers, which are reliable and valid for assessing PA intensity. The accelerometer was attached to a belt that each girl wrapped around her waist. At baseline and post-intervention, each girl wore the accelerometer on her right hip from the time getting out of bed in the morning to the time going to sleep at night for 7 consecutive days (e.g., 5 weekdays; 2 weekend days). Data were reintegrated to 15-second epochs and processed using PA intensity cut-points validated with adolescent girls: 547–1002 counts per 15 seconds for moderate and ≥1003 counts per 15 seconds for vigorous PA (29). In the trial, close to 92% of the girls provided ≥ 8 hours of data on three weekdays and one weekend day, which is adequate data (30) for aggregating to represent a week (7 days). To avoid bias (31), imputation based on all available data in hour blocks on all 7 days was used. Time of accelerometer wear was standardized to 14 hours per weekday, including one hour before the actual start time at each school, 7 hours during the school day, and 6 hours after school. For each weekend day, the time was standardized to 10 hours due to later awake times on no-school days. If any hour block of the 90 hours/week included incomplete data, the entire hour was identified as missing (22). ActiLife (ActiGraph Corporation, Pensacola, FL) and R statistical software [version 3.2.4] using the MICE package (32) were employed for data reduction and imputation. Additional details have been published (22).
CRF.
The Progressive Aerobic Cardiovascular Endurance Run (PACER) test, an endurance shuttle run that is reliable and valid for estimating adolescents’ maximal oxygen consumption (VO2max), was used (33). The shuttle run distance, 15-meter or 20-meters, was determined by space in each school and marked by two cones. Each girl ran between the cones, trying to reach each cone before hearing an audio cue. As the test progressed, the time between audio cues decreased. A girl’s test was finished when she failed to complete two laps before the audio cues. To estimate VO2max, number of completed laps was converted into the mile equivalency (34); then, the following equation was used: VO2max = [−8.41*(mile-equivalent)] + [0.34*(mile-equivalent*mile-equivalent)] + [0.21*(age*gender)] − (0.84*body mass index) + 108.94 (35). A higher VO2max indicates greater CRF.
Data analysis
To reduce missing data biases and maximize statistical power, multiple imputation (R, version 3.2.4.) was employed to produce 20 datasets (21, 36–37). We used absolute numbers and percentages to describe categorical variables and included means and standard deviations for continuous variables. Independent t-test or chi-square test was used to examine group differences (intervention vs. control) in study variables. Intent-to-treat principle was followed for all data analyses. Mixed effect models were applied to examine the potential moderators including race, ethnicity, free/reduced-price lunch enrollment, pubertal stage, and baseline weight status. To reduce potential multicollinearity and increase interpretability, the continuous moderator age was centered for the moderation analyses (38). For each of the six potential moderators, an interaction term was created as the product of group (intervention vs. control) multiplied by the moderator. A series of mixed effect models were performed for each outcome of interest (MVPA, BMI z-score, percent body fat, and CRF) while controlling for age, race, ethnicity, pubertal stage, weight status, free/reduced-price lunch enrollment, and baseline dependent variable of interest. All moderation analyses accounted for clustering of girls within schools. If the interaction effect was significant, then post hoc tests were performed using the LSMESTIMATE statement (39). The LSMESTIMATE statement is a combination of the LSMEANS and ESTIMATE statements and is used to obtain custom hypothesis tests among LS-means (39). Results from the 20 imputed datasets were combined to obtain a single F-statistic and a p-value (40). All analyses were performed in SAS 9.4 with a significance level of 0.05.
RESULTS
Preliminary analyses
As shown in Table 1, the intervention and control groups did not differ on age, ethnicity, free/reduced-price lunch enrollment, pubertal stage, MVPA, percent body fat, BMI z-score, and CRF at baseline. The control group included a higher percentage of African American girls than the intervention group (64.23% vs. 56.18%, p=.001). The control group had a higher proportion of obese girls (34.33% vs. 28.55%), and a lower proportion of healthy weight girls (45.23% vs. 48.61%, p=.046) than the intervention group.
Table 1.
Participants’ sociodemographic and physical characteristics at baseline (N=1519)
| Characteristics | Total | Intervention (n=753) | Control (n=766) |
|---|---|---|---|
| Mean (SD) or n (%) | Mean (SD) or n (%) | Mean (SD) or n (%) | |
| Age (years) | 12.05 (1.01) | 12.05 (0.99) | 12.05 (1.02) |
| Race* | |||
| Black | 915 (60.24%) | 423 (56.18%) | 492 (64.23%) |
| Non-black | 604 (39.76%) | 330 (43.82%) | 274 (35.77%) |
| Ethnicity | |||
| Hispanic | 201 (13.23%) | 111 (14.74%) | 90 (11.75%) |
| Non-Hispanic | 1232 (81.11%) | 603 (80.08%) | 629 (82.11%) |
| Missing | 86 (5.66%) | 39 (5.18%) | 47 (6.14%) |
| Free/reduced price lunch | |||
| Yes | 1182 (77.81%) | 577 (76.63%) | 605 (78.98%) |
| No | 234 (15.40%) | 113 (15.01%) | 121 (15.80%) |
| N/A | 103 (6.79%) | 63 (8.36%) | 40 (5.22%) |
| Pubertal stage | |||
| Pre-puberty | 59 (3.88%) | 34 (4.52%) | 25 (3.26%) |
| Early puberty | 143 (9.41%) | 64 (8.50%) | 79 (10.31%) |
| Mid-puberty | 601 (39.57%) | 298 (39.58%) | 303 (39.56%) |
| Late puberty | 708 (46.61%) | 353 (46.88%) | 355 (46.35%) |
| Post-puberty | 2 (0.13%) | 1 (0.13%) | 1 (0.13%) |
| Missing | (0.39%) | 3 (0.39%) | 3 (0.39%) |
| Weight status* | |||
| Underweight | 18 (1.18%) | 8 (1.06%) | 10 (1.31%) |
| Healthy weight | 687 (45.23%) | 366 (48.61%) | 321 (41.91%) |
| Overweight | 305 (20.08%) | 154 (20.45%) | 151 (19.71%) |
| Obese | 478 (31.47%) | 215 (28.55%) | 263 (34.33%) |
| Missing | 31 (2.04%) | 10 (1.33%) | 21 (2.74%) |
| MVPA (min/hour) | 2.96 (1.32) | 3.02 (1.33) | 2.89 (1.30) |
| Percent body fat | 29.96% (9.71%) | 29.47% (9.56%) | 30.44% (9.84%) |
| BMI z-score | 0.97 (1.06) | 0.92 (1.03) | 1.02 (1.08) |
| Cardiovascular fitness | 37.89 (5.19) | 38.15 (5.17) | 37.64 (5.19) |
Note. Table includes non-imputed data;
p<.05, calculated with chi-square test.
Table 2 shows the bivariate correlations among all study variables. Age and pubertal stage were positively correlated with weight status (r=0.07, p=0.014; r=0.19, p<0.001), percent body fat (r=0.19, p<0.001; r=0.28, p<0.001), BMI z-score (r=0.10, p<0.001; r=0.26, p<0.001), but negatively correlated with MVPA (r=−0.07, p=0.012; r=−0.12, p<0.001) and CRF (r=−0.25, p<0.001; r=−0.29, p<0.001). African American girls tended to have higher percent body fat and BMI z-score, but lower CRF. Weight status was positively correlated with percent body fat (r=0.87, p<0.001) and BMI z-score (r=0.85, p<0.001), while negatively correlated with MVPA (r=−0.09, p<0.001) and CRF (r=−0.84, p<0.001).
Table 2.
Bivariate correlations among study variables (N=1519)
| Number | Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | −.11** | −.06* | 19** | .46** | .07* | −.07* | .19** | .10** | −.25** |
| 2 | Race | 2 | .29** | −.05 | −.12** | −.06* | −.04 | −.07** | −.06* | .07** |
| 3 | Ethnicity (Hispanic) | 3 | .06* | −.02 | .002 | −.01 | −.01 | −.01 | .03 | |
| 4 | Free/reduced price lunch | 4 | .10** | −.01 | .06* | .05 | .03 | −.06* | ||
| 5 | Pubertal stage | 5 | .19** | −.12** | .28** | .26** | −.29** | |||
| 6 | Weight status | 6 | −.09** | .87** | .85** | −.84** | ||||
| 7 | MVPA (min/hour) | 7 | −.10** | −.08** | .09** | |||||
| 8 | Percent body fat | 8 | .95** | −.96** | ||||||
| 9 | BMI z-score | 9 | −.90** | |||||||
| 10 | Cardiovascular fitness | 10 |
Note. SD=standard deviation. Statistical significance:
p<.05,
p<.01.
Race: 1=African American, 2=White, 3=Mixed-racial or other; Ethnicity (Hispanic): 1=yes, 0=no; Free/reduced price lunch: 1=yes, 0=no; Pubertal stage: 1=pre-mid puberty, 2=late-post puberty; Weight status: 1=underweight and healthy weight, 2=overweight, 3=obese.
Moderation analysis
Table 3 demonstrates the results of moderation effects on MVPA, BMI z-score, percent body fat, and CRF at post-intervention. Weight status significantly moderated the intervention effects on CRF (F3.98, 1277.06=3.39, p<0.01). Results from the post hoc tests showed that overweight or obese girls in the intervention group had significantly higher CRF at post-intervention than those in the control group (overweight girls: mean difference b=0.28, t=1.97, p=0.049; obese girls: b=0.31, t=2.60, p<0.01). However, among under/healthy weight girls, post-intervention CRF did not differ significantly between intervention and control groups (b=0.04, t=0.38, p=0.706). Figure 1 shows the post-intervention CRF between intervention and control group by baseline weight status. Age, race, ethnicity, free/reduced-price lunch enrollment, and pubertal stage were not significant moderators for CRF.
Table 3.
Moderators of intervention effects on post-intervention MVPA, BMI z-score, percent body fat, and cardiovascular fitness (N=1519)
| Moderator | MVPA | BMI z-score | Percent body fat | CRF | ||||
|---|---|---|---|---|---|---|---|---|
| Moderator × Treatment | Moderator × Treatment | Moderator × Treatment | Moderator × Treatment | |||||
| F-statistic | p-value | F-statistic | p-value | F-statistic | p-value | F-statistic | p-value | |
| Age | 0.00 | 0.27 | 2.84 | 0.10 | 0.06 | 0.74 | 0.00 | 0.19 |
| Race | 2.07 | 0.13 | 0.28 | 0.73 | 0.66 | 0.52 | 0.89 | 0.41 |
| Ethnicity | 0.00 | 0.27 | 0.00 | 0.25 | 0.03 | 0.32 | 0.01 | 0.13 |
| Free/reduced price lunch | 1.71 | 0.19 | 0.02 | 0.33 | 0.05 | 0.19 | 1.00 | 0.27 |
| Pubertal stage | 3.03 | 0.08 | 0.01 | 0.29 | 1.53 | 0.22 | 0.11 | 0.68 |
| Weight status | 1.14 | 0.27 | 2.04 | 0.11 | 0.94 | 0.42 | 3.39 | <0.01 |
Note. MVPA=moderate to vigorous physical activity, BMI=body mass index, CRF=cardiorespiratory fitness
Figure 1.
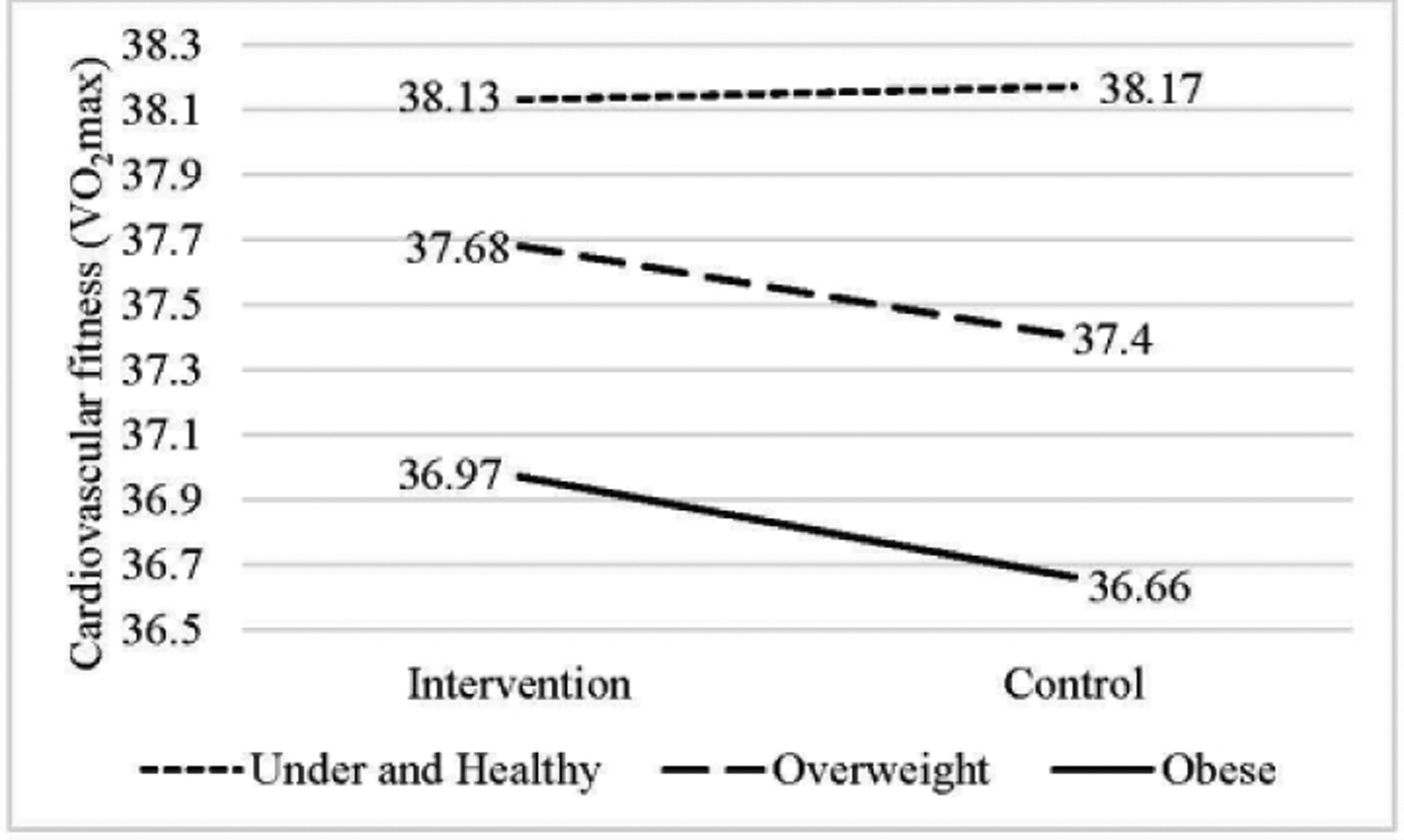
Post-intervention cardiovascular fitness between intervention and control group by baseline weight status
There was no statistically significant moderator for the intervention effects on MVPA, BMI z-score, or percent body fat. Only pubertal stage was identified as a marginally significant moderator for MVPA (F0.94, 1056.42=3.03, p=0.08). At post-intervention, girls in the pre- to mid-pubertal stage in the intervention group had lower MVPA than those in the control group (b=0.263, t=1.92, p=0.055); while girls in the late to post-pubertal stage had similar MVPA between the intervention and control groups (b=0.07, t=0.61, p=0.542). As demonstrated in Figure 2, in the control group, girls in the late to post-pubertal stage were significantly less active than those in the pre- to mid-pubertal stage (b= 0.26, t=2.47, p=0.014); while in the intervention group, girls in the late to post-pubertal stage were slightly more active than those in the pre- to mid-pubertal stage (b=0.07, t=0.70, p=0.484).
Figure 2.
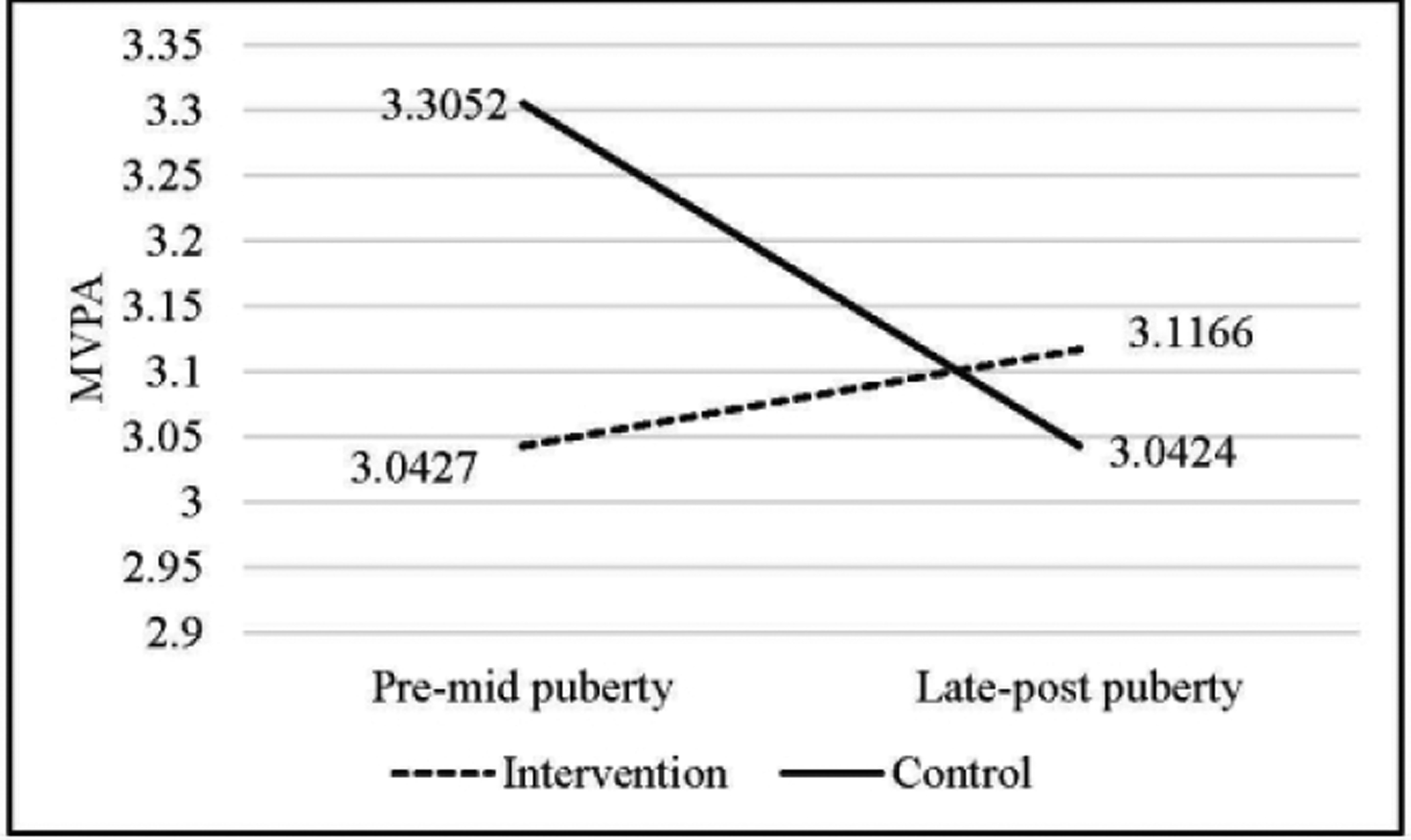
Post-intervention MVPA between intervention and control group by pubertal stage
DISCUSSION
The current study identified whether the effects of a PA intervention on adolescent girls’ MVPA, percent body fat, BMI z-score, and CRF at post-intervention were greater for some subgroups than others, relative to the control condition. Findings showed that the intervention was more effective in improving CRF in overweight or obese girls than among girls having a healthy weight and in increasing MVPA among late to post-pubertal girls, as compared to pre- to mid-pubertal girls.
The obesity epidemic has been associated with obesogenic factors, such as low levels of PA, that then result in impaired CRF. Overall, the CRF of adolescent girls having a healthy weight has been found to be better than the CRF of girls with overweight or obesity (41). The current study’s findings that no between-group differences in CRF occurred for under/healthy weight girls, but overweight or obese girls in the intervention group had higher CRF than their control group counterparts may have resulted because baseline CRF fitness was lower among overweight and obese girls than under/healthy weight girls, resulting in an opportunity for greater gains in CRF across time for the former than the latter group. Of importance is that overweight or obese girls may have reaped health benefits from their participation in the PA intervention. The findings imply that a targeted PA intervention that increases CRF among overweight or obese girls, many of whom probably have low levels of CRF, may provide a greater return on investment than a more diffuse program implemented with the general population of adolescent girls.
In a group RCT involving adolescent girls in low-income communities, no differences between the intervention and control groups occurred in minutes of MVPA measured immediately following a PA intervention (22); but, CRF was significantly higher among intervention than control group girls (4). The researchers who conducted the group RCT explained that after the PA intervention had ended, the girls in the low-income communities lost the opportunity to be physically active, and this occurrence may have reduced their ability to attain MVPA post-intervention when their PA was measured (22). Perhaps, CRF is a better outcome than MVPA to measure in PA interventions, given that CRF is somewhat stable over a short time period, as compared to MVPA, the latter of which may be influenced by contextual factors. However, research is needed to support these contentions.
The finding that late to post-pubertal girls in the control group were significantly less active than the pre- to mid-pubertal girls in the same group aligns with evidence supporting that girls’ PA declines during adolescence (42). In contrast, however, in the intervention group, late to post-pubertal girls were slightly more active at post-intervention than the pre- to mid-pubertal girls, although the finding did not reach statistical significance. The findings suggest that the intervention may have had a better effect on the MVPA of late to post-pubertal girls relative to the pre- to mid-pubertal girls. Two plausible explanations are that: 1) pre- to mid-pubertal girls in the intervention group no longer had the after-school club to engage in MVPA and the related support for the behavior after the intervention had ended and when post-intervention measures were conducted, possibly resulting in a reduction in their MVPA; and 2) late to post-pubertal girls in the intervention group, given their relatively matured cognition, might have been able to continue to attain MVPA even though the intervention had ended (19).
Girls’ responses to the intervention, as indicated by its effects on the outcome variables, did not differ based on age, race, ethnicity, or participation in free or reduced-price lunch program at school. Similarly, ethnicity did not emerge as a significant moderator in a cluster RCT to evaluate the impact of an obesity prevention intervention on BMI z-score, adiposity, and PA (43). The lack of significant differences in intervention effects based on age and SES in the current study conflicted with results of other studies. For example, Cook et al. (19) reported that an Internet-based computer-tailored intervention program was more effective for commuting by bicycle and leisure-time walking among older than younger adolescents (16–18 years old vs. 13–15 years old, respectively). The findings by Cook et al. (19) suggest that the young age, ranging from 10–15 years, of the girls in the current study may have contributed to the non-significant results. In addition, following a health-promoting school initiative with 4- to 12-year olds, Bartelink and colleagues (44) noted that the effects on BMI z-score and PA were more favorable among higher than lower SES groups. Perhaps, in the current study, the ability to detect significant differences in the girls’ responses to the intervention based on their SES was limited because the vast majority of girls (78%) were of low SES. Regardless, the inconsistent results indicate a need for continued research involving moderation analyses.
Also, in the current study, weight status did not significantly moderate the intervention effects on BMI z-score or percent body fat, inconsistent with Annesi’s (45) study showing that reductions in BMI were more pronounced after an obesity prevention intervention in African-American pre-adolescents who were overweight and obese than among those with a healthy weight. One plausible explanation for the inconsistent findings is that Annesi’s (45) intervention addressed nutrition as well as PA, whereas the current intervention focused only on PA.
Limitations and strengths
The study had strengths and limitations. One strength is that many participants were low-income African American adolescent girls, representing a group having high obesity rates (46). Other strengths include the presence of a control group, the longitudinal design, and measurement of PA via accelerometers. One limitation is that data were collected from adolescent girls in urban areas so results may not be generalizable to other groups. Another limitation is that SES was determined based solely on enrollment in the free and reduced-price lunch program; unfortunately, parent education and income were not assessed.
Conclusions
A PA intervention can improve overweight and obese girls’ CRF, possibly attenuating their cardiovascular risk. Moreover, girls in late-to-post-puberty, who typically attain lower levels of MVPA than those in earlier pubertal stages, can increase their MVPA beyond levels demonstrated by girls in pre-to mid-puberty as a result of their participation in a PA intervention. This information indicates that both overweight and obese girls and girls in late-to-post-puberty should be included in a PA intervention because both groups respond well to and benefit from it. Also, many adolescent girls, especially those in pre-to mid-puberty, may need assistance to maintain their MVPA after an intervention ends; therefore, effective strategies for accomplishing this task warrant consideration when designing PA interventions for this population.
Moderation analyses need to become common practice in PA and obesity prevention research to identify subgroups of adolescent girls that respond differently to interventions. Then, in future PA interventions, special attention can be directed toward less responsive subgroups of girls, and interventions can be optimized to enhance effectiveness. Continued research is needed to increase understanding regarding why PA interventions do not work for certain subgroups and how this problem can be resolved.
Moderators of physical activity intervention effects among adolescent girls are important to identify because the effectiveness of these interventions to date in this population has been limited.
This article contributes to the notable gap in knowledge regarding moderators in physical activity interventions involving adolescent girls, particularly baseline characteristics that may moderate their responses to physical activity interventions. Awareness of the moderators can be useful for determining the type of intervention that may be successful in subgroups of adolescent girls and for tailoring a physical activity intervention to optimally meet each girl’s needs to achieve maximal effects.
Findings show that weight status moderated the intervention effects on cardiorespiratory fitness. Compared to the control condition, the intervention increased overweight and obese, but not healthy weight, girls’ cardiorespiratory fitness.
A physical activity intervention can improve overweight and obese girls’ cardiorespiratory fitness, possibly attenuating their cardiovascular risk. Therefore, it is essential to include overweight and obese girls in PA interventions to help them reap this important benefit.
ACKNOWLEDGEMENTS
The study was funded by a grant from the National Heart, Lung, and Blood Institute at the National Institutes of Health (R01HL109101); PI: L. B. Robbins. The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH. The authors thank the school administrators, teachers, nurses, and other staff members for their support. We acknowledge former Project Managers Stacey Wesolek and Kelly Bourne and former Intervention Coordinators Ann Kostin-McGill and Patrice Patrick-Banks for their assistance with managing the project. We are grateful to the undergraduate and graduate nursing and kinesiology students for helping us during various phases of the study. We appreciate the assistance received from Maria Cotts, an undergraduate nursing student, who reviewed and edited the references included in the manuscript. Finally, we thank the adolescent girls for their participation.
Footnotes
Consent and Assent: Parents/guardians gave written consent for their adolescent child to participate in the study, and adolescents provided written assent.
Trial Registration: ClinicalTrials.gov Identifier NCT01503333
Competing interests: The authors declare no competing interests.
REFERENCES
- 1.Isensee B, Suchert V, Hansen J, Weisser B, Hanewinkel R. Effects of a school-based pedometer intervention in adolescents: 1-year follow-up of a cluster-randomized controlled trial. J Sch Health 2018;88: 717–724. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland: WHO; 2010. [PubMed] [Google Scholar]
- 3.Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health 2020;4:23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfeiffer KA, et al. Effects of the Girls on the Move randomized trial on adiposity and aerobic performance (secondary outcomes) in low-income adolescent girls. Pediatr Obes 2019;14:e12559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Owen MB, Curry WB, Kerner C, Newson L, Fairclough SJ. The effectiveness of school-based physical activity interventions for adolescent girls: A systematic review and meta-analysis. Prev Med 2017;105:237–249. [DOI] [PubMed] [Google Scholar]
- 6.Voskuil VR, Frambes DA, Robbins LB. Effect of physical activity interventions for girls on objectively measured outcomes: a systematic review of randomized controlled trials. J. Pediatr Health Care 2017;31:75–87. [DOI] [PubMed] [Google Scholar]
- 7.Pearson N, Braithwaite R, Biddle SJ. The effectiveness of interventions to increase physical activity among adolescent girls: a meta-analysis. Acad Pediatr 2015;15:9–18. [DOI] [PubMed] [Google Scholar]
- 8.Kann L, et al. Youth Risk Behavior Surveillance - United States, 2017. MMWR Surveillance Summ 2018;67:1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark BR, et al. Failure to meet aerobic fitness standards among urban elementary students. Prev Med Rep 2018;12:330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Office Of The Assistant Secretary For Planning And Evaulation. HHS Federal Poverty Guidelines For 2019. [Internet]. 2019. Available from: https://aspe.hhs.gov/poverty-guidelines
- 11.Rundel A, et al. Individual- and school-level sociodemographic predictors of obesity among New York City public school children. Am J Epidemiol 2012;176:986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stalsberg R, Pedersen AV. Effects of socioeconomic status on the physical activity in adolescents: a systematic review of the evidence. Scand J Med Sci Sports 2010;20:368–383. [DOI] [PubMed] [Google Scholar]
- 13.Peterson AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J. Youth Adolesc 1998;17:117–133. [DOI] [PubMed] [Google Scholar]
- 14.Haapala EA, et al. Longitudinal associations of physical activity and pubertal development with academic achievement in adolescents. Journal of Sport and Health Science 2019:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michlesfield LK, et al. Physical activity and sedentary behavior amoung adolescents in rural South Africa: levles, patterns, and correlates. BMC Public Health 2014;14:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dollman J, et al. A hitchhiker’s guide to assessing young people’s physical activity: Deciding what method to use. J Sci Med Sport 2009;12:518–525. [DOI] [PubMed] [Google Scholar]
- 17.Elmesmari R, Martin A, Reilly JJ, Paton JY. Comparison of accelerometer measured levels of physical activity and sedentary time between obese and non-obese children and adolescents: a systematic review. BMC Pediatr 2018;18:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang RAH, et al. Moderators of wellbeing interventions: Why do some people respond more positively than others? PLoS One 2017;12:e0187601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook TL, et al. Moderators of the effectiveness of a web-based tailored intervention promoting physical activity in adolescents: the HELENA Activ-O-Meter. J Sch Health 2014;84:256–266. [DOI] [PubMed] [Google Scholar]
- 20.Lubans DR, Morgan PJ, Callister R. Potential moderators and mediators of intervention effects in an obesity prevention program for adolescent boys from disadvantaged schools. J Sci Med Sport 2012;15:519–525. [DOI] [PubMed] [Google Scholar]
- 21.Kremers SP, de Bruijn GJ, Droomers M, van Lenthe F, Brug J. Moderators of environmental intervention effects on diet and activity in youth. Am J Prev Med 2007;32:163–172. [DOI] [PubMed] [Google Scholar]
- 22.Robbins LB, et al. Intervention effects of “Girls on the Move” on increasing physical activity: a group randomized trial. Ann Behav Med 2019;53:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robbins LB, et al. “Girls on the Move” intervention protocol for increasing physical activity among low-active underserved urban girls: a group randomized trial. BMC Public Health 2013;13:474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller WR, Rollnick S. Motivational Interviewing. 3rd ed. New York, NY: The Guilford Press, 2013. [Google Scholar]
- 25.Neumark-Sztainer DR, et al. New moves-preventing weight-related problems in adolescent girls a group-randomized study. Am J Prev Med 2010;39:421–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carskadon MA, Acebo C. A self-administered rating scale for pubertal development. J Adolesc Health 1993;14:190–195. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC growth charts (ages 0 to <20 years). [Internet]. 2016. Available from: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
- 28.Centers for Disease Control and Prevention. About child & teen BMI. [Internet]. 2018. Avaiable from: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html
- 29.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–1565. [DOI] [PubMed] [Google Scholar]
- 30.Fitzgibbon ML, et al. Family-based hip-hop to health: outcome results. Obesity (Silver Spring) 2013;21:274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Catellier DJ, et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc 2005;37 Suppl 11:S555–S562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software 2011;45:1–67. [Google Scholar]
- 33.The Cooper Institute, Meredith MD, Welk JG. Fitnessgram & Activitygram Test Administration Manual. 4th ed. Champaign, IL: Human Kinetics, 2010. [Google Scholar]
- 34.Zhu W, Plowman SA, Park Y. A primer-test centered equating method for setting cut-off scores. Res Q Exerc Sport 2010;81:400–409. [DOI] [PubMed] [Google Scholar]
- 35.Cureton KJ, Sloniger MA, O’Bannon JP, Black DM, McCormack WP. A generalized equation for prediction of VO2peak from 1-mile run/walk performance. Med Sci Sports Exerc 1995;27:445–451. [PubMed] [Google Scholar]
- 36.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons, 1987. [Google Scholar]
- 37.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377–399. [DOI] [PubMed] [Google Scholar]
- 38.Aiken LS, West SG, Reno RR. Multiple regression: testing and interpreting interactions. Newbury Park, CA: Sage Publications, 1991. [Google Scholar]
- 39.Kiernan K, Tobias R, Gibbs P, Tao J, SAS Institute. CONTRAST and ESTIMATE statements made easy: the LSMESTIMATE statement (Paper 351–2011). [Internet]. Cary, NC: SAS Global Forum; 2011. Available from: https://support.sas.com/resources/papers/proceedings11/351-2011.pdf [Google Scholar]
- 40.Wang B, Fang Y, Jin M. Combining type-III analyses from multiple imputations (Paper 1543–2014). [Internet]. 2014. Available from: http://support.sas.com/resources/papers/proceedings14/1543-2014.pdf
- 41.Bonney E, Ferguson G, Smits-Engelsman B. Relationship between body mass index, cardiorespiratory and musculoskeletal fitness among South African adolescent girls. Int J Environ Res Public Health 2018;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bacil ED, Mazzardo Junior O, Rech CR, Legnani RF, de Campos W. [Physical activity and biological maturation: a systematic review]. Rev Paul Pediatr 2015;33:114–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Nassau F, et al. The Dutch Obesity Intervention in Teenagers (DOiT) cluster controlled implementation trial: intervention effects and mediators and moderators of adiposity and energy balance-related behaviours. Int J Behav Nutr Phys Act 2014;11:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bartelink N, van Assema P, Jansen M, Savelberg H, Kremers S. The moderating role of the school context on the effects of the healthy primary school of the future. Int. J. Environ. Res. Public Health 2019;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Annesi JJ. Initial body mass index and free-time physical activity moderate effects of the Youth Fit for Life treatment in African-American pre-adolescents. Percept Mot Skills 2010;110:789–800. [DOI] [PubMed] [Google Scholar]
- 46.Ogden CL, et al. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA 2018;319:2410–2418. [DOI] [PMC free article] [PubMed] [Google Scholar]


