Abstract
This study examined the effects of food insecurity and housing instability experiences during early childhood on adolescent anxiety and depressive symptoms through maternal depression and parenting stress. This longitudinal study included four waves of data from the Fragile Families and Child Well-Being Study (n=2,626). Food insecurity was measured when the child was five years of age using the United States Department of Agriculture’s 18-item Food Security Scale. Housing instability was also measured when the child was five years of age based on an affirmative response to six housing adversity items. Maternal depression and parenting stress were measured when the child was nine years of age. Anxiety and depressive symptoms were assessed when the child (now adolescent) was 15 years of age using 6-items of the BSI-18 anxiety subscale and 5-items of the Centers for Epidemiologic Studies Depression Scale respectively. Two structural equation models assessed the associations between food insecurity and housing instability on adolescent anxiety (model 1) and depressive symptoms (model 2) through maternal depression and parenting stress simultaneously, controlling for sociodemographic characteristics. Results suggest that experiencing both food insecurity and housing instability during early childhood increases the risk of long-term adolescent depressive (indirect: B=0.008, CI: 0.002, 0.016) and anxiety (indirect: B=0.012, CI: 0.002, 0.026) symptoms through maternal depression to parenting stress. Screening for food insecurity and housing instability during early childhood could potentially identify both mothers who are at risk for depression and parenting stress and children who are at increased risk for anxiety or depressive symptoms during adolescence.
Keywords: economic hardship, Fragile Families and Child Wellbeing study, mental health, residential hardship, structural equation models
INTRODUCTION
The association between economic hardship and long-term adverse physical and psychological health outcomes have been well documented (Hernandez & Pressler, 2014; Kahn & Pearlin, 2006; Lillard, Burkhauser, Hahn, & Wilkins, 2015). Food insecurity and housing instability characterize specific types of economic hardships and are associated with one another (Huang & King, 2018; King, 2018). Food security is defined as the state of access to enough food for an active and healthy life, while food insecurity is the lack of access to an adequate amount of healthy and nutritious food (Coleman-Jensen, Rabbitt, Gregory, & Singh, 2018). The association between food insecurity and negative short-term and long-term child health outcomes is well documented in the literature (Council on Community Pediatrics, 2015; Gundersen & Ziliak, 2015). Food insecurity during childhood influences children’s physical health (Holben, 2010) and contributes to internalizing and externalizing problems (Slopen, Fitzmaurice, Williams, & Gilman, 2010). Several studies have linked food insecurity during childhood with adolescent anxiety and depression (McIntyre, Williams, Lavorato, & Patten, 2013; McIntyre, Wu, Kwok, & Patten, 2017; McLaughlin et al., 2012; Poole-Di Salvo, Silver, & Stein, 2016).
Housing instability refers to a continuum of experiences that include: frequent residential relocation, inability to consistently pay rent or mortgage, living in an overcrowded household, doubling up with family or friends, or staying in a car or abandoned building due to economic hardship (Geller & Curtis, 2011; Ma, Gee, & Kushel, 2008). The available body of literature on residential instability suggests poor emotional development and experiences with depression for adolescents (Coley, Leventhal, Lynch, & Kull, 2013; Fowler, Henry, & Marcal, 2015).
Food insecurity and housing instability are correlated and highly prevalent among low-income families and families that access public and private assistance. For instance, over half of clients that access food banks through the Feeding America network have described the daunting task of choosing between paying for housing or food (Weinfield et al., 2014). Consistent food supply and stable housing are basic needs that influence access and utilization of health care (Kushel, Gupta, Gee, & Haas, 2006). The literature on how both food insecurity and housing instability are related to child behavior problems (Fernandez, Yomogida, Aratani, & Hernandez, 2018) and to chronic diseases among adults is growing (Charkhchi, Fazeli Dehkordy, & Carlos, 2018; Stupplebeen, 2019). However, there is a lack of longitudinal research focusing on how early childhood exposure to both food insecurity and housing instability can influence adolescent mental health.
The Life Course Health Development (LCHD) framework can be used to describe how food insecurity and housing instability during early childhood could possibly influence anxiety and depressive symptoms during adolescence (Halfon & Hochstein, 2002). The LCHD theory attempts to explain how early experiences affect future health patterns and how these experiences can increase the development of diseases in future stages of a life course. Adolescent anxiety and depressive symptoms can be influenced by the programming or latency model within the LCHD framework. Depression and anxiety are highly prevalent comorbid mental health disorders that often manifest during childhood and adolescence (Axelson & Birmaher, 2001). The programming model suggests that early exposure to risk factors during critical periods can have long-term health consequences (Ben-Shlomo & Kuh, 2002; Hertzman, Power, Matthews, & Manor, 2001). Adverse experiences during early childhood, specifically before the age of five, have been found to be predictive of anxiety disorders during adolescence, specifically at age 15 (Phillips, Hammen, Brennan, Najman, & Bor, 2005). Further, early childhood adversity prior to age five has been related to adolescent depression (Hazel, Hammen, Brennan, & Najman, 2008). The negative experiences associated with food insecurity and housing instability during early childhood could contribute to depressive and anxious symptomology in adolescence. Thus, early exposure to food insecurity and housing instability could contribute to mental health disparities in adolescence which then places adolescents at risk for dropping out of school (Quiroga, Janosz, Bisset, & Morin, 2013), substance use (Valentiner, Mounts, & Deacon, 2004), and adult unemployment (Egan, Daly, & Delaney, 2016).
Within the family environment there could be mechanisms that could influence the relationship between early childhood experiences with food insecurity and housing instability. The accumulation of stress associated with food insecurity and housing instability could influence maternal depression (Bronte-Tinkew, Zaslow, Capps, Horowitz, & McNamara, 2007; Davey-Rothwell, German, & Latkin, 2008; Suglia, Duarte, & Sandel, 2011; Whitaker, Phillips, & Orzol, 2006), and maternal depression has been associated with adolescent anxiety and depressive symptoms (Spence, Najman, Bor, O’Callaghan, & Williams, 2002). In addition, the depletion of resources associated with experiencing food insecurity and housing instability could contribute to greater parenting stress (Gershoff, Aber, Raver, & Lennon, 2007; Rodriguez-JenKins & Marcenko, 2014). Increase levels of parenting stress have been associated with placing adolescents at risk for depression and anxiety (Tan & Rey, 2005). Last, prior research has suggested that maternal depression influences parenting stress (Gerdes et al., 2007). Thus, mechanisms of the relationship between early childhood experiences with food insecurity and housing instability with adolescent depressive and anxiety symptoms could be through maternal depression, parenting stress, or maternal depression to parenting stress. Pinpointing some of the underlying mechanisms that predict the development of adolescent depressive and anxiety symptoms can help in the development of prevention programs.
Drawing from the LCHD framework (Halfon & Hochstein, 2002), the current study examines how food insecurity and housing instability experiences during early childhood influence anxiety and depressive symptoms during adolescence while accounting for maternal depression and parenting stress as mediators. Based on the programming model, experiencing food insecurity or housing instability during early childhood could be a critical period for later experiencing mental health problems during adolescence. The effect of experiencing both food insecurity and housing instability during a critical period on anxiety and depressive symptoms has not been reported in the adolescent literature.
METHODS
Data and sample
This paper used secondary data from the Fragile Families and Child Well-Being Study which follows 4,898 U.S. children born between 1998 and 2000. The data was collected from 20 large U.S. cities. The main survey, which consists of interviews with mothers and fathers, were initially conducted at birth, and then by telephone when the child was at one, three, five, nine, and 15 years old. At age 15, the children, now adolescents, reported on their own anxiety and depression symptomology. In addition to the main survey, a subsample of mothers participated in an in-home assessment when the child was three and five years old. The in-home assessment included questions regarding household food insecurity that are not available in the main survey. Sampling and study design have been previously reported (Reichman, Teitler, Garfinkel, & McLanahan, 2001).
The sample for the current study excluded adolescents who did not participate in year 15 youth interview (1,454 excluded), mothers who did not participate in year 9 mother interview (314 excluded), families who were missing both year three and five in-home assessments (46 excluded), and mothers who were not interviewed at year three (151 excluded). The sample was further reduced based on missing data on adolescents’ measures of anxiety and depressive symptoms (6 excluded) and covariates (301 excluded). Families that had complete data on the variables of interest but were missing data on year five food insecurity or housing instability, were kept in the data set if there was available data for these measurements at year three. Keeping with the LCHD framework, the focus of the independent variable was on experiences that occurred during early childhood. Based on additional analyses (not reported), families who experienced food insecurity at year three were more likely to experience food insecurity at year five. In addition, families who experienced housing instability at year three were more likely to experience housing instability at year five. Data available at year three was used when data from year five was missing because of the correlational relationship and the data fit the stage of development that coincided with our LCHD framework (n = 808 food insecurity; n=390 housing instability). The final sample for this study was 2,626 families.
Attrition analyses were done to compare analytic sample to the excluded sample due to missing data using one-way analysis of variance tests for continuous variables and chi-square tests for categorical variables. The excluded families in this study were more likely to be at or below 1.99 of the poverty ratio. Excluded mothers were more likely to be employed and have less than high school education. Excluded children were more likely to be male and uninsured. The study was approved by the authors’ Institutional Review Board #13394-EX (Fragile Families Study).
Measures
Adolescent Depressive and Anxiety Symptoms
Depressive symptoms.
Adolescents’ self-reported depressive symptoms were assessed using five-items of the Centers for Epidemiologic Studies Depression Scale (CES-D) (Perreira, Deeb-Sossa, Harris, & Bollen, 2005) at year fifteen. Adolescents reported the difficulty for overcoming depressive feeling, sadness, happiness, being depressed, and as though life was not worth living in the past week using a four-point scale ranging from 0 = strongly agree to 3 = strongly disagree. The response about “feeling happiness” was reversely coded. Responses were summed to create a total score ranging from 0 to 15 with higher scores indicating greater depressive symptoms (Perreira et al., 2005). Internal consistency (Cronbach’s alpha) of the five items for depression measure in this sample was 0.76.
Anxiety symptoms.
Adolescents’ self-reported anxiety symptoms were assessed using six-items of the Brief Symptom Inventory 18 (BSI-18) item anxiety subscale (Derogatis & Fitzpatrick, 2004) at year fifteen. Adolescents responded to the six questions “During the past seven days, how much were you distressed by: spells of terror or panic, feeling tense or keyed up, suddenly scared for no reason, nervousness or shakiness inside, feeling fearful, feeling so restless you couldn’t sit still.” A four-point scale ranging from 0 = not at all to 3 = extremely was used. Responses were summed to create a total score ranging from 0 to 18 with higher scores indicating greater anxiety symptoms. Internal consistency (Cronbach’s alpha) of the six items for anxiety measure in this sample was 0.76.
Potential mediators: Maternal Depression and Parenting Stress
Maternal Depression.
Maternal depression was self-assessed using the 15-item Composite International Diagnostic Interview-Short Form (CIDI-SF) at year 9 (Kessler, Andrews, Mroczek, Ustun, & Wittchen, 1998). The CIDI-SF is a screener that is used to evaluate the probability an individual would be diagnosed with depression if the full CIDI questions were provided. The items are consistent with the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). Mothers were asked items such as low energy, feeling sad or blue, and weight changes in the past year that lasted for two weeks or more during the past 12 months. Mothers were classified as depressed based on CIDI-SF scoring criteria as outlined by Kessler et al. (1998). Further information on the scoring criteria can be found on the Fragile Families and Child Wellbeing Study website (Bendheim-Thoman Center for Research on Child Wellbeing, 2018).
Parenting stress.
Parenting stress was assessed by mothers responding using the Parenting Stress Inventory at year 9 (Abidin, 1995). Mothers were asked the following four-items, “Being a parent is harder than I thought it would be.”, “I feel trapped by my responsibilities as a parent.”, “I find that taking care of my child(ren) is much more work than pleasure.”, and “I often feel tired, worn out, or exhausted from raising a family.” A four-point scale ranging from 1=strongly disagree to 4=strongly agree was used. An average score ranging from 1 to 4 was used, and higher scores indicate greater parenting stress (Bendheim-Thoman Center for Research on Child Wellbeing, 2018). Internal consistency (Cronbach’s alpha) of the four items for parenting stress measure in this sample was 0.66.
Early Childhood Experiences with Food Insecurity & Housing Instability
Food Insecurity.
Household food insecurity was reported by mothers at year five using the 18-item United States Department of Agriculture’s Food Security Survey Module questionnaire (Bickel, Nord, Price, Hamilton, & Cook, 2000). Examples of survey questions which assessed food access and availability in the past 12 months included: how often participants “worried about running out of food before having more money to buy food again” and how often “meals were skipped or cut size to last longer”. Families were categorized into two categories: 1) food secure if mothers gave 0–2 affirmative responses or 2) food insecure if families answered three or more affirmative responses (Coleman-Jensen et al., 2018).
Housing instability.
Housing instability was determined based on whether the family experienced a housing adversity at any point in the 12 months preceding the interview. At year five, the mothers answered six questions that capture housing hardships caused by financial constraints (Geller & Curtis, 2011). These questions included: “not being able to pay rent or mortgage”, “getting evicted”, “being delinquent on housing-related bills”, “borrowing money from friends or family to pay for bills”, “moving in with others”, and “staying at a shelter, abandoned building, or in a car due to financial problems”. In this study, participants were classified into two categories: 1) housing stability if the mothers did not give any affirmative answers and 2) housing instability if the mothers gave one or more affirmative answers (Geller & Franklin, 2014).
Experiences with food insecurity and housing instability. Four dichotomous variables were created to classify the independent variables in this study: 1) both food security and housing stability, 2) food insecurity only, 3) housing instability only, and 4) both food insecurity and housing instability. Both food and housing secure included all families who did not experience any instances of food insecurity nor housing instability (reference group). Food insecurity included all families who experienced food insecurity while being housing stable. Housing instability included all families who experienced housing instability while being food secure. Both food insecurity and housing instability included all families who experienced both food insecurity and housing instability.
Covariates
Socio-demographic characteristics were used to control for factors that are known to influence food insecurity, housing instability, maternal depression, parenting stress, and adolescent’s anxiety and depressive symptoms. Adolescent characteristics included adolescent’s sex (male or female [reference]) at baseline, health insurance (uninsured [reference], private insurance, or public insurance) at year 3, (Kushel et al., 2006), and race/ethnicity (white, Hispanic, or black [reference]) at year fifteen. Maternal and household characteristics at year three included: mother’s age (years), marital status (married/cohabitating or single/widowed/divorced [reference]), education (less than a high school degree [reference], high school degree or equivalent, or some college or more), employment (employed or unemployed [reference]), income (based on the family income to the federal poverty line (FPL) FPL≤1.99 [reference], FPL 2.00–2.99, or FPL≥ 3.00) (Slopen et al., 2010), and history of paternal incarceration (no [reference] or yes) (Geller & Franklin, 2014; Turney, 2015). Because the intergenerational transmission of mental illness has been observed in previous studies (Garber & Cole, 2010), maternal depression and anxiety based on the Composite International Diagnostic Interview-Short Form (CIDI-SF) at year three were also included in the respective models (no [reference] or yes) (Kessler et al., 1998; Walters, Kessler, Nelson, & Mroczek, 2002). Food insecurity and housing instability at year fifteen was also included as covariate (none [reference], housing instability only, food insecurity only, and both food insecurity and housing instability).
Statistical Analysis
Descriptive statistics were conducted for the full sample and by food insecurity and housing instability groups. Bivariate analyses were conducted to compare variables of interest among those that experienced food security and housing stability with 1) those that experienced food insecurity only, 2) those that experienced housing instability only, and 3) those that experienced both food insecurity and housing instability. One-way analysis of variance tests were used for continuous variables; chi-squared tests were used for categorical variables. Covariate-adjusted structural equation models were used to test the association of the categorical food insecurity and housing instability experiences during early childhood with anxiety and depressive symptoms occurring during adolescence through mediators, maternal depression and parenting stress. Models predicting adolescent anxiety symptoms included maternal anxiety. Models predicting adolescent depressive symptoms included maternal depression. Descriptive statistics, one-way analysis of variance tests, and chi-squared tests were performed using STATA SE version 15.1 statistical software (StataCorp LP, College Station, Texas), and structural equation models were performed using Mplus (Muthen & Muthen, Los Angeles, CA). We report the unstandardized betas and 95% confidence intervals of 5,000 bootstrap sample below unless where noted.
RESULTS
Descriptive Results
Table 1 presents descriptive statistics for the entire analytic sample and by food insecurity and housing instability subgroups. In the full sample, average scores of adolescent’s depressive and anxiety symptoms at year 15 are 5.12 (SD=2.29) (out of 15) and 4.82 (SD=3.90) (out of 18), respectively. During early childhood, 52% of families experienced both food security and housing stability, and 4% of families experienced food insecurity only while being housing stable. Thirty-three percent of families experienced housing instability while being food secure, and 11% of families were both food insecure and housing unstable. Fifty-one percent of adolescents were males, 49% were black, and 52% had public health insurance. On average, mothers were 28 years old, 37% were single, 39% had some college or more, 60% were employed, 65% were 1.99 or less of the FPL, and 45% of the adolescent’s fathers had experienced incarceration. Five percent of mothers had met anxiety criteria and 21% of mothers met depression criteria at year three. During adolescence (year 15), 55% of families were both food secure and housing stable, and 3% of families experienced food insecurity only while being housing stable. Thirty percent of families experienced housing instability while being food secure, and 12% of families experienced both food insecurity and housing instability.
Table 1.
Descriptive statistics of the total analytic sample and by food and housing insecurity status [M (SD) or %]
| Total Analytic Sample N = 2,626 | Food and Housing Secure n = 1,370 | Housing Instability Only n = 883 | Food Insecurity Only n = 92 | Food Insecurity and Housing Instability n = 281 | |
|---|---|---|---|---|---|
| Adolescent Mental Health | |||||
| Depressive symptoms | 5.12 (2.29) | 5.01 (2.24) b, c | 5.09 (2.27) | 5.93 (2.85) | 5.50 (2.37) |
| Anxiety symptoms | 4.82 (3.90) | 4.58 (3.82) b, c | 4.85 (3.97) | 5.77 (4.06) | 5.59 (3.87) |
| Early Childhood Economic Hardship Experiences | |||||
| Food and housing secure | 52% | 100% | -- | -- | -- |
| Housing instability only | 33% | -- | 100% | -- | -- |
| Food insecurity only | 4% | -- | -- | 100% | -- |
| Food insecurity and housing instability | 11% | -- | -- | -- | 100% |
| Potential Maternal Mediators | |||||
| Mother Depression | |||||
| No | 83% | 89% | 78% | 77% | 70% |
| Yes | 17% | 11% a, b, c | 22% | 23% | 30% |
| Parent Stress | 2.71(1.07) | 2.64(1.07) a, c | 2.72(1.05) | 2.77(1.13) | 3.00(1.03) |
| Adolescent Characteristics | |||||
| Sex | |||||
| Female | 49% | 47% | 55% | 46% | 43% |
| Male | 51% | 53% a | 45% | 54% | 57% |
| Race | |||||
| White | 27% | 31% a, b, c | 23% | 9% | 18% |
| Hispanic | 24% | 27% a | 19% | 28% | 27% |
| Black | 49% | 42% a, b, c | 58% | 63% | 55% |
| Health insurance | |||||
| Uninsured | 6% | 5% c | 5% | 9% | 9% |
| Private | 42% | 50% a, b, c | 37% | 15% | 29% |
| Public | 52% | 45% a, b, c | 57% | 76% | 62% |
| Maternal and Household Characteristics | |||||
| Age | 28.16 (6.01) | 28.99 (6.30) a, b, c | 27.18 (5.45) | 27.59 (6.71) | 27.38 (5.38) |
| Marital status | |||||
| Married/cohabiting | 63% | 70% | 59% | 54% | 54% |
| Single/widowed/divorced | 37% | 30% a, b | 41% | 46% | 46% |
| Education | |||||
| Less than high school | 30% | 27% b, c | 31% | 47% | 36% |
| High school diploma | 31% | 30% b | 31% | 41% | 34% |
| Some college or more | 39% | 43% a, b, c | 38% | 13% | 30% |
| Employment | |||||
| Employed | 60% | 61% | 61% | 42% | 53% |
| Unemployed | 40% | 39% b, c | 39% | 58% | 47% |
| Income (based on Federal Poverty Line, FPL) | |||||
| ≤1.99 FPL | 65% | 56% a, c | 71% | 82% | 86% |
| 2.00–2.99 FPL | 14% | 15%c | 15% | 9% | 10% |
| ≥3.00 FPL | 21% | 29% a, b, c | 14% | 9% | 4% |
| History of paternal incarceration | |||||
| No | 55% | 64% | 52% | 36% | 40% |
| Yes | 45% | 36% a, b, c | 48% | 64% | 60% |
| Maternal depression | |||||
| No | 79% | 86% | 75% | 71% | 61% |
| Yes | 21% | 14% a, b, c | 25% | 29% | 39% |
| Maternal anxiety | |||||
| No | 95% | 98% | 94% | 91% | 85% |
| Yes | 5% | 2% a, b, c | 6% | 9% | 15% |
| Adolescent Economic Hardship Experiences | |||||
| Food and housing secure | 55% | 63% | 43% | 48% | 29% |
| Housing instability only | 30% | 29% a, c | 39% | 24% | 35% |
| Food insecurity only | 3% | 3% b | 3% | 11% | 5% |
| Food insecurity and housing instability | 12% | 5% a, b, c | 15% | 17% | 31% |
p<.05 Food and housing secure vs Housing instability only
p<.05 Food and housing secure vs Food insecurity only
p<.05 Food and housing secure vs Food and housing insecure
On average, adolescents who were food secure and housing stable showed different characteristics compared to adolescents who had experienced both/either food insecurity and/or housing instability during early childhood. Adolescents who were food secure and housing stable reported significantly lower scores of depressive and anxiety symptoms, were more likely to be white and less likely to be black, and have private health insurance. Their mothers were older and more likely to live with their spouse and partner, have some college or more education, employed, and be at or above 3.00 of the poverty ratio. Also, the percentage of paternal incarceration and maternal anxiety and depression were lower than those who had experienced both/either food insecurity and/or housing instability during early childhood.
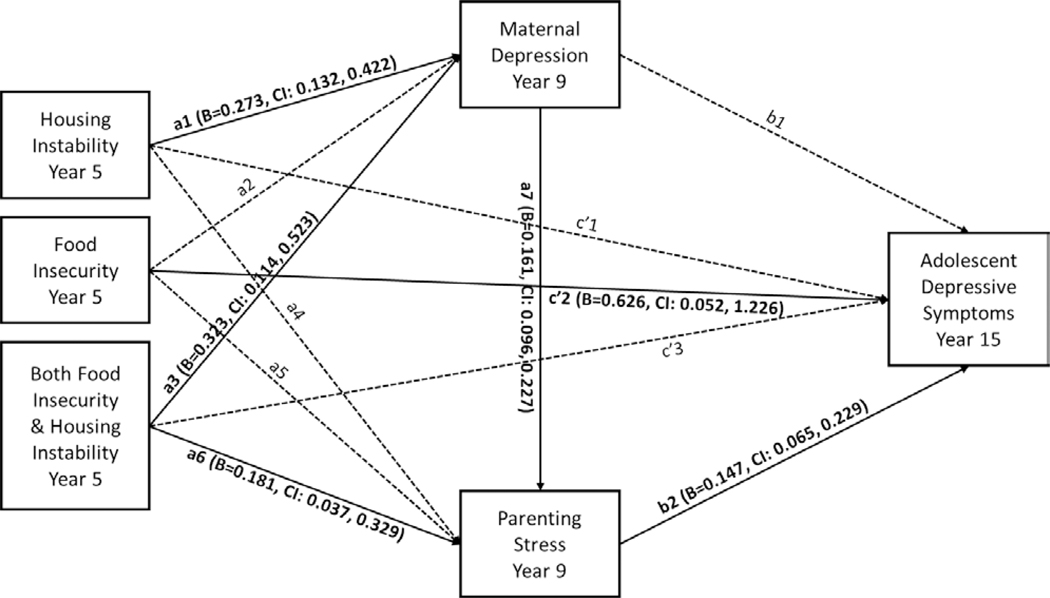
Adolescent depressive symptom model
Only the significant paths of the covariate-adjusted structural equation model for each outcome are described below. In the context of the overall model (Figure 1), adolescents who experienced food insecurity only during early childhood significantly showed greater adolescent depressive symptoms at (B=0.626, CI: 0.052, 1.226). Early childhood experiences of housing instability only (B=0.273, CI: 0.132, 0.422) and experiencing both food insecurity and housing instability (B=0.323, CI: 0.114, 0.523) significantly predicted maternal depression at year 9. Experiences of both food insecurity and housing instability at year 5 predicted greater parenting stress at year 9 (B=0.181, CI: 0.037, 0.329), and greater parenting stress at year 9 predicted greater adolescent depressive symptoms at year 15 (B=0.147, CI: 0.065, 0.229). Maternal depression at year 9 significantly predicted higher parenting stress at year 9 (B=0.161, CI: 0.096, 0.227).
Figure 1.
Covariate-adjusted structural equation model for adolescent depressive symptoms
The paths without the unstandardized beta and 95% confidence interval were tested but not observed significance. The root mean square error of approximation (RMSEA)=0.645, comparative fit index (CFI)=0.883, Tucker-Lewis index (TLI)=−0.230, and Chi-square test of model fit <.001 are reported as the model fit.
Taken together, the relationship of both food insecurity and housing instability at year 5 predicting adolescent depressive symptom at year 15 through both maternal depression and parenting stress at year 9 were statistically significant (total indirect: B=0.055, CI: 0.007, 0.110). Mediation through both mediators explained 4.4% of the relationship between housing instability only (total effect: B=−0.037, CI: −0.233, 0.169), food insecurity only (total effect: B=0.647, CI: 0.071, 1.236), and both food insecurity and housing instability (total effect: B=0.265, CI: −0.062, 0.588) during early childhood and of adolescent depressive symptoms at year 15.
Parenting stress at year 9 partially mediated experiencing both food insecurity and housing instability during early childhood and adolescent depressive symptom at year 15, controlling for maternal depression at year 9 (specific indirect: B=0.026, CI: 0.004, 0.058). Parenting stress at year 9 accounted for 4.2% of the total effects from food insecurity and housing instability at year 5 to adolescent depressive symptom at year 15. Last, there was significant indirect effect from housing instability only (specific indirect: B=0.006, CI: 0.002, 0.013) and both food insecurity and housing instability (specific indirect: B=0.008, CI: 0.002, 0.016) at year 5 to adolescent depressive symptom at year 15 through maternal depression to parenting stress.
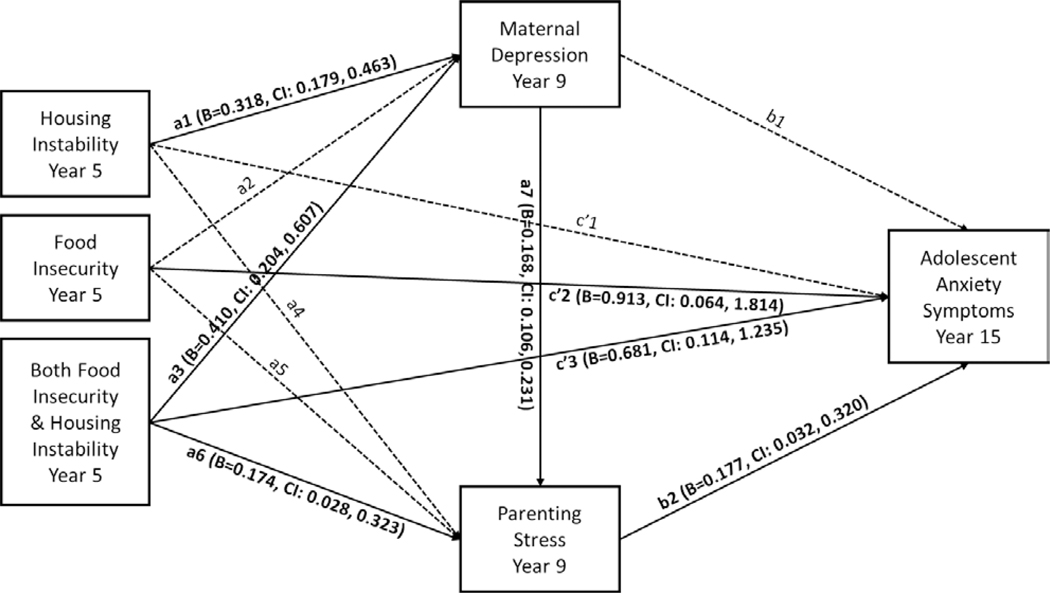
Adolescent anxiety symptom model
In the context of the overall model (Figure 2), adolescents who experienced food insecurity only (B=0.913, CI: 0.064, 1.814) and both food insecurity and housing instability (B=0.681, CI: 0.114, 1.235) at year 5 significantly showed greater adolescent anxiety symptoms at year 15. Experiencing housing instability only (B=0.318, CI: 0.179, 0.463) and both food insecurity and housing instability (B=0.410, CI: 0.204, 0.607) significantly predicted maternal depression at year 9. Experiencing both food insecurity and housing instability at year 5 (B=0.174, CI: 0.028, 0.323) significantly predicted parenting stress at year 9, and greater parenting stress at year 9 significantly predicted greater adolescent anxiety symptom at year 15 (B=0.177, CI: 0.032, 0.320). Maternal depression at year 9 significantly predicted higher parenting stress at year 9 (B=0.168, CI: 0.106, 0.231).
Figure 2.
Covariate-adjusted structural equation model for adolescent anxiety symptoms
The paths without the unstandardized beta and 95% confidence interval were tested but not observed significance. The root mean square error of approximation (RMSEA)=0.469, comparative fit index (CFI)=0.803, Tucker-Lewis index (TLI)=−1.066, and Chi-square test of model fit <.001 are reported as the model fit.
Taken together, the relationship of housing instability only (total indirect: B=0.042, CI: 0.032, 0.124), food insecurity only (total indirect: B=0.041, CI: −0.038, 0.134), and both food insecurity and housing instability (total indirect: B=0.091, CI: −0.003, 0.196) at year 5 predicting adolescent anxiety symptoms through both maternal depression and parenting stress at year 9 were not statistically significant. Mediation through both mediators explained 3.2% of the relationship between housing instability only (total effect: B=0.117, CI: −0.220, 0.473), food insecurity only (total effect: B=0.954, CI: 0.118, 1.839), and both food insecurity and housing instability (total effect: B=0.772, CI: 0.211, 1.308) at year 5 and of adolescent anxiety symptoms at year 15.
Parenting stress at year 9 partially mediated experiencing both food insecurity and housing instability during early childhood and adolescent anxiety symptom at year 15, controlling for maternal depression at year 9 (specific indirect: B=0.031, CI: 0.001, 0.075). Parenting stress at year 9 accounted for 4.2% of the total effects from food insecurity and housing instability at year 5 to adolescent anxiety symptom at year 15. Last, there was significant indirect effect from housing instability only (specific indirect: B=0.009, CI: 0.001, 0.021) and both food insecurity and housing instability (specific indirect: B=0.012, CI: 0.002, 0.026) at year 5 to adolescent anxiety symptom at year 15 through maternal depression to parenting stress at year 9.
DISCUSSION
The current study drew on the LCHD framework to examine how food insecurity and housing instability experiences during early childhood influence the development of adolescent mental health symptoms through maternal depression and parenting stress (Halfon & Hochstein, 2002). Results indicate the majority of the families did not experience any economic hardship in the form of food insecurity and housing instability. While few families only experienced food insecurity (while being housing secure) a greater percentage of families experienced only housing instability (while being food secure). This discrepancy could be related to numerous anti-poverty programs available to families with young children that are directly (i.e. Women, Infants and Children (WIC) program) or indirectly (i.e. Early Head Start and Head Start) targeted at preventing food insecurity. Further, findings suggest that food insecurity and housing instability co-exist with 11% of the sample experiencing both forms of economic hardship during early childhood. Although few families only experienced food insecurity (while being housing secure), several more families that experienced food insecurity appear to be experiencing other forms of hardship, in this case housing-related.
Similar to previous research food insecurity during early childhood directly influences adolescent depressive symptoms (standardized B = 0.273, CI = 0.023, 0.533) and anxiety symptoms (standardized B = 0.234, CI = 0.016, 0.466) (McIntyre et al., 2013; McIntyre et al., 2017; McLaughlin et al., 2012). Contrary to previous research the findings from the current study does not indicate a direct relationship between housing instability and adolescent depressive symptoms (Coley et al., 2013; Fowler et al., 2015), nor was a direct relationship between housing instability and adolescent anxiety symptoms found. Interestingly, the cumulative effect of experiencing both food insecurity and housing instability influences adolescent anxiety symptoms directly (standardized B = 0.175, CI = 0.029, 0.316). When comparing the standardized betas of the significant direct paths, the path from food insecurity to adolescent anxiety symptoms is larger than the path from the cumulative effect of experiencing both food insecurity and housing instability on adolescent anxiety symptoms. Thus, the risk of experiencing adolescent anxiety symptoms does not increase as a result of experiencing both food insecurity and housing instability compared to solely experiencing food insecurity. Overall, 1) experiencing food insecurity without any other economic hardship or 2) experiencing food insecurity, in addition to another form of economic hardship places children at greater risk of experiencing depressive and anxiety symptoms during adolescence. While the independent and dependent measures are 10 years apart, there seems to be a direct correlation between the household-level anxiety of not having food available nor stable housing and adolescents experiencing poor mental health symptoms.
The mechanisms that help to partially explain the relationship between economic hardship during early childhood and adolescent mental health symptoms does differ depending on the independent variable. While the current findings are similar to previous research that has found housing instability to be predictive of maternal depression (Davey-Rothwell et al., 2008; Suglia et al., 2011), maternal depression was not directly influenced by food insecurity. Despite prior research finding food insecurity to directly influence maternal depression (Bronte-Tinkew et al., 2007; Whitaker et al., 2006), the models in prior research did not include housing instability, which may be why current findings differ. In addition, there could be other parenting and family environmental mechanisms that were not assessed that could be more influential in explaining the relationships between early childhood experiences with food insecurity and adolescent mental health. Further, comparable to earlier work that has found maternal depression to be predictive of parenting stress (Gerdes et al., 2007), and parenting stress to be predictive of child and adolescent depressive and anxiety symptoms (Tan & Rey, 2005), the current findings replicated such work. The behaviors associated with housing instability (e.g., frequent moves, the inability to pay rent, and borrowing money) may contribute to social isolation and a lack of social support, which could then lead to maternal depression, and ultimately increase the stress associated with parenting. The progression of these risk factors are then internalized by adolescents and manifested as depressive and anxiety symptoms.
In addition, the cumulative effect of experiencing both food insecurity and housing instability influences adolescent depressive and anxiety symptoms indirectly: 1) through maternal depression to parenting stress and 2) through parenting stress. The underlying behaviors associated with the first indirect path (i.e. maternal depression to parenting stress) could be similar to what was previously described in the above paragraph. It is important to point out, that our models found a significant association between maternal depression and parenting stress; however, prior research has found parenting stress to be predictive of maternal depression (Farmer & Lee, 2011). Further, the current findings suggest that the behaviors associated with experiencing both insufficient access to food and the inability to pay rent or frequently moving directly influences parenting stress, which increases the risk of adolescents experiencing poor mental health symptoms. Thus, maternal depression and parenting stress are significant consequences to experiencing both food insecurity and housing instability and precursors to adolescents withstanding depressive and anxiety symptoms.
These findings suggest the need for interventions that integrate broad mental health and coping strategies for families that experience economic hardship. WIC and similar public food assistance programs, such as the Supplemental Nutrition Assistance Program, present a promising opportunity to screen for housing instability. Another notable opportunity for housing instability screening is at pediatricians’ offices where food insecurity screening is already recommended by the American Academy of Pediatrics (Council on Community Pediatrics, 2015). Additional opportunities for screening could be available through private programs, such as food pantries and farmers’ market program. Screening for housing instability within the food assistance programs, or screening for both during a child well visit, can clear a path for identifying those who are in need of both food and housing assistance. Such screening will also identify mothers who are at risk for maternal depression and increased parenting stress, and children who are at increased risk for anxiety or depressive symptoms during adolescence. The collaborating nature of organizations working together to address multiple components of economic adversity could possibly lead to reducing mental health disparities among mothers and adolescents.
While this study highlights the risk factors that may lead up to adverse mental symptoms during adolescence, the results should be interpreted within the context of its limitations. Food insecurity and housing instability were self-reported by the mothers and mental health outcome measures were self-reported by the adolescents. This raises the possibility of reporting bias which may lead to under- or over-estimating the variables of interest. However, having the independent and dependent variables measured by different reporters decreases the findings to be attributed to shared method variance. Another limitation is that our study used dichotomous variables to measure food insecurity and housing instability. This resulted in our analysis not accounting for the variability in these measures and the severity of experiences during early childhood. Despite this limitation, our measures make an important contribution because they are consistent with how previous studies have used these items. This consistency allows for the comparison of findings across literature. Related, the current study does not take into account additional economic hardships that can co-occur with food insecurity and housing instability; thus the measure of hardship is conservative in this study. Yet, the narrow focus does provide the opportunity to pinpoint services (as described above) that could reduce the type of hardship experienced along with the negative mental health consequences by collaborating together. Last, the first data collection time point in this study was 1998, followed by subsequent years. Consequently, the data may be not be perceived as current. For a longitudinal study, however, to examine the influence of early childhood experiences on adolescent mental health outcomes, it is necessary to use data that spans over a least 15 years. Therefore, using this data is appropriate for the aims of the study.
This is the first study to the authors’ knowledge to demonstrate that experiencing food insecurity and housing instability during early childhood does place children at risk for depressive and anxiety symptoms in subsequent adolescent years. The current findings could possibly inform interventions geared at mothers who are most at risk for experiencing depression and increased parenting stress and children who are most at risk for experiencing depressive and anxiety symptoms during adolescence based on food insecurity and housing instability experiences during early childhood. Future studies are encouraged to examine how experiences with food insecurity and housing instability at different stages of development – early childhood vs. middle childhood – influence adult and adolescent mental health. Additionally, research studies are needed to understand the temporal order of food insecurity and housing instability experiences. That is, it is important to know which form of economic hardship precedes the other or whether a bidirectional relationship exists. The findings, in addition to previous literature (Geller & Franklin, 2014; Turney, 2015), also suggest that there are other correlating family environmental factors (e.g., parental incarceration) that may place added economic and mental pressure for some families more than others. In other words, examining the moderating factors, in addition to the mechanisms, is needed to progress the literature. Understanding how experiencing different forms of economic hardship at various stages of development, the temporal order of economic hardship experiences, and how the family environmental factors moderate the relationship between early childhood economic hardship experiences and adolescent mental health can inform family-based prevention strategies.
Acknowledgments
Funding: Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD36916, R01HD39135, and R01HD40421, as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The last authors’ time was partial supported by the William T. Grant Foundation, grant # 187656.
References
- Abidin R. (1995). Parent Stress Inventory, 3rd Edition Psychological Assessment Resources; Odessa, FL. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition American Psychiatric Association; Washington, DC. [Google Scholar]
- Axelson DA, & Birmaher B. (2001). Relation between anxiety and depressive disorders in childhood and adolescence. Depression and Anxiety, 14(2), 67–78. [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y, & Kuh D. (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31(2), 285–293. [PubMed] [Google Scholar]
- Bendheim-Thoman Center for Research on Child Wellbeing. (2018). User’s Guide for Fragile Families and Child Wellbeing Study Public Data, Year 9. Retrieved from https://fragilefamilies.princeton.edu/sites/fragilefamilies/files/year_9_guide.pdf
- Bickel G, Nord M, Price C, Hamilton W, & Cook J. (2000). Guide to measuring household food security, revised 2000: U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. [Google Scholar]
- Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, & McNamara M. (2007). Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. The Journal of Nutrition, 137(9), 2160–2165. doi: 10.1093/jn/137.9.2160 [DOI] [PubMed] [Google Scholar]
- Charkhchi P, Fazeli Dehkordy S, & Carlos RC. (2018). Housing and food insecurity, care access, and health status among the chronically ill: An analysis of the Behavioral Risk Factor Surveillance System. Journal of General Internal Medicine, 33(5), 644–650. doi: 10.1007/s11606-017-4255-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman-Jensen A, Rabbitt MP, Gregory CA, & Singh A. (2018). Household food security in the United States in 2017. United States Department of Agriculture, Economic Research Service. [Google Scholar]
- Coley RL, Leventhal T, Lynch AD, & Kull M. (2013). Relations between housing characteristics and the well-being of low-income children and adolescents. Developmental Psychology, 49(9), 1775–1789. doi: 10.1037/a0031033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council on Community Pediatrics. (2015). Promoting food security for all children. Pediatrics, 136(5), e1431–1438. doi: 10.1542/peds.2015-3301 [DOI] [PubMed] [Google Scholar]
- Davey-Rothwell MA, German D, & Latkin CA. (2008). Residential transience and depression: does the relationship exist for men and women? Journal of Urban Health, 85(5), 707–716. doi: 10.1007/s11524-008-9294-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, & Fitzpatrick M. (2004). The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18 In Maruish ME. (Ed.), The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults (pp. 1–41). Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Egan M, Daly M, & Delaney L. (2016). Adolescent psychological distress, unemployment, and the Great Recession: Evidence from the National Longitudinal Study of Youth 1997 . Social Science & Medicine, 156, 98–105. doi: 10.1016/j.socscimed.2016.03.013 [DOI] [PubMed] [Google Scholar]
- Farmer AY, & Lee SK. (2011). The effects of parenting stress, perceived mastery, and maternal depression on parent–child interaction. Journal of Social Service Research, 37(5), 516–525. doi: 10.1080/01488376.2011.607367 [DOI] [Google Scholar]
- Fernandez CR, Yomogida M, Aratani Y, & Hernandez D. (2018). Dual food and energy hardship and associated child behavior problems. Academic Pediatrics, 18(8), 889–896. doi: 10.1016/j.acap.2018.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler PJ, Henry DB, & Marcal KE. (2015). Family and housing instability: Longitudinal impact on adolescent emotional and behavioral well-being. Social Science Research, 53, 364–374. doi: 10.1016/j.ssresearch.2015.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, & Cole DA. (2010). Intergenerational transmission of depression: A launch and grow model of change across adolescence. Development and Psychopathology, 22(4), 819–830. doi: 10.1017/s0954579410000489 [DOI] [PubMed] [Google Scholar]
- Geller A, & Curtis MA. (2011). A sort of homecoming: Incarceration and the housing security of urban men. Social Science Research, 40(4), 1196–1213. doi: 10.1016/j.ssresearch.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller A, & Franklin AW. (2014). Paternal incarceration and the housing security of urban mothers. Journal of Marriage and the Family, 76(2), 411–427. doi: 10.1111/jomf.12098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, & Jensen PS. (2007). Maternal depressive symptomatology and parenting behavior: exploration of possible mediators. Journal of Abnormal Child Psychology, 35(5), 705–714. doi: 10.1007/s10802-007-9134-3 [DOI] [PubMed] [Google Scholar]
- Gershoff ET, Aber JL, Raver CC, & Lennon MC. (2007). Income is not enough: incorporating material hardship into models of income associations with parenting and child development. Child Development, 78(1), 70–95. doi: 10.1111/j.1467-8624.2007.00986.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen C, & Ziliak JP. (2015). Food insecurity and health outcomes. Health Affairs, 34(11), 1830–1839. doi: 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- Halfon N, & Hochstein M. (2002). Life course health development: An integrated framework for developing health, policy, and research. The Milbank Quarterly, 80(3), 433–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, & Najman J. (2008). Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychological Medicine, 38(4), 581–589. doi: 10.1017/s0033291708002857 [DOI] [PubMed] [Google Scholar]
- Hernandez DC, & Pressler E. (2014). Accumulation of childhood poverty on young adult overweight or obese status: Race/ethnicity and gender disparities. Journal of Epidemiology and Community Health, 68(5), 478–484. doi: 10.1136/jech-2013-203062 [DOI] [PubMed] [Google Scholar]
- Hertzman C, Power C, Matthews S, & Manor O. (2001). Using an interactive framework of society and lifecourse to explain self-rated health in early adulthood . Social Science & Medicine, 53(12), 1575–1585. doi: 10.1016/S0277-9536(00)00437-8 [DOI] [PubMed] [Google Scholar]
- Holben DH. (2010). Position of the American Dietetic Association: Food insecurity in the United States. Journal of the American Dietetic Association, 110(9), 1368–1377. doi: 10.1016/j.jada.2006.01.016 [DOI] [PubMed] [Google Scholar]
- Huang X, & King C. (2018). Food insecurity transitions and housing hardships: Are immigrant families more vulnerable? Journal of Urban Affairs, 40(8), 1146–1160. doi: 10.1080/07352166.2018.1468222 [DOI] [Google Scholar]
- Kahn JR, & Pearlin LI. (2006). Financial strain over the life course and health among older adults. Journal of Health and Social Behavior, 47(1), 17–31. doi: 10.1177/002214650604700102 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, & Wittchen HU. (1998). The World Health Organization composite international diagnostic interview short‐form (CIDI‐SF). International Journal of Methods in Psychiatric Research, 7(4), 171–185. [Google Scholar]
- King C. (2018). Food insecurity and housing instability in vulnerable families. Review of Economics of the Household, 16(2), 255–273. doi: 10.1007/s11150-016-9335-z [DOI] [Google Scholar]
- Kushel MB, Gupta R, Gee L, & Haas JS. (2006). Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine, 21(1), 71–77. doi: 10.1111/j.1525-1497.2005.00278.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillard DR, Burkhauser RV, Hahn MH, & Wilkins R. (2015). Does early-life income inequality predict self-reported health in later life? Evidence from the United States. Social Science & Medicine, 128, 347–355. doi: 10.1016/j.socscimed.2014.12.026 [DOI] [PubMed] [Google Scholar]
- Ma CT, Gee L, & Kushel MB. (2008). Associations between housing instability and food insecurity with health care access in low-income children. Ambulatory Pediatrics, 8(1), 50–57. doi: 10.1016/j.ambp.2007.08.004 [DOI] [PubMed] [Google Scholar]
- McIntyre L, Williams JV, Lavorato DH, & Patten S. (2013). Depression and suicide ideation in late adolescence and early adulthood are an outcome of child hunger. Journal of Affective Disorders, 150(1), 123–129. doi: 10.1016/j.jad.2012.11.029 [DOI] [PubMed] [Google Scholar]
- McIntyre L, Wu X, Kwok C, & Patten SB. (2017). The pervasive effect of youth self-report of hunger on depression over 6 years of follow up. Social Psychiatry and Psychiatric Epidemiology, 52(5), 537–547. doi: 10.1007/s00127-017-1361-5 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Alegria M, Jane Costello E, Gruber MJ, Sampson NA, & Kessler RC. (2012). Food insecurity and mental disorders in a national sample of U.S. adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 51(12), 1293–1303. doi: 10.1016/j.jaac.2012.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira KM, Deeb-Sossa N, Harris KM, & Bollen K. (2005). What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Social Forces, 83(4), 1567–1601. doi: 10.1353/sof.2005.0077 [DOI] [Google Scholar]
- Phillips NK, Hammen CL, Brennan PA, Najman JM, & Bor W. (2005). Early adversity and the prospective prediction of depressive and anxiety disorders in adolescents. Journal of Abnormal Child Psychology, 33(1), 13–24. doi: 10.1037/a0016123 [DOI] [PubMed] [Google Scholar]
- Poole-Di Salvo E, Silver EJ, & Stein RE. (2016). Household food insecurity and mental health problems among adolescents: What do parents report? Academic Pediatrics, 16(1), 90–96. doi: 10.1016/j.acap.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Quiroga CV, Janosz M, Bisset S, & Morin AJ. (2013). Early adolescent depression symptoms and school dropout: Mediating processes involving self-reported academic competence and achievement. Journal of Educational Psychology, 105(2), 552–560. [Google Scholar]
- Reichman NE, Teitler JO, Garfinkel I, & McLanahan SS. (2001). Fragile families: Sample and design. Children and Youth Services Review, 23(4/5), 303–326. doi: 10.1016/S0190-7409(01)00141-4 [DOI] [Google Scholar]
- Rodriguez-JenKins J, & Marcenko MO. (2014). Parenting stress among child welfare involved families: Differences by child placement. Children and Youth Services Review, 46, 19–27. doi: 10.1016/j.childyouth.2014.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Fitzmaurice G, Williams DR, & Gilman SE. (2010). Poverty, food insecurity, and the behavior for childhood internalizing and externalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 49(5), 444–452. doi: 10.1016/j.jaac.2010.01.018 [DOI] [PubMed] [Google Scholar]
- Spence SH, Najman JM, Bor W, O’Callaghan MJ, & Williams GM. (2002). Maternal anxiety and depression, poverty and marital relationship factors during early childhood as predictors of anxiety and depressive symptoms in adolescence. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 43(4), 457–469. doi: 10.1111/14697610.00037 [DOI] [PubMed] [Google Scholar]
- Stupplebeen DA. (2019). Housing and food insecurity and chronic disease among three racial groups in Hawai’i. Preventing Chronic Disease, 16, E13. doi: 10.5888/pcd16.180311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Duarte CS, & Sandel MT. (2011). Housing quality, housing instability, and maternal mental health. Journal of Urban Health, 88(6), 1105–1116. doi: 10.1007/s11524011-9587-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan S, & Rey J. (2005). Depression in the young, parental depression and parenting stress. Australas Psychiatry, 13(1), 76–79. doi: 10.1080/j.1440-1665.2004.02155.x [DOI] [PubMed] [Google Scholar]
- Turney K. (2015). Paternal incarceration and children’s food insecurity: A consideration of variation and mechanisms. Social Service Review, 89(2), 335–367. doi: 10.1086/681704 [DOI] [Google Scholar]
- Valentiner DP, Mounts NS, & Deacon BJ. (2004). Panic attacks, depression and anxiety symptoms, and substance use behaviors during late adolescence. Journal of Anxiety Disorders, 18(5), 573–585. doi: 10.1016/j.janxdis.2003.04.001 [DOI] [PubMed] [Google Scholar]
- Walters EE, Kessler RC, Nelson CB, & Mroczek D. (2002). Scoring the World Health Organization’s Composite International Diagnostic Interview Short Form (CIDI-SF). World Health Organization; Geneva. [Google Scholar]
- Weinfield NS, Mills G, Borger C, Gearing M, Macaluso T, Montaquila J, & Zedlewski S. (2014). Hunger in America 2014. Westat and the Urban Institute: National report prepared for Feeding America. [Google Scholar]
- Whitaker RC, Phillips SM, & Orzol SM. (2006). Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics, 118(3), e859–868. doi: 10.1542/peds.2006-0239 [DOI] [PubMed] [Google Scholar]