Abstract
Anxiety is the most prevalent psychological disorder among youth, and even following treatment, confers risk for anxiety relapse and the development of depression. Anxiety disorders are associated with heightened response to negative affective stimuli in brain networks underlying emotion processing. One factor that can attenuate symptoms of anxiety and depression in high-risk youth is parental warmth. The current study investigates whether parental warmth helps to protect against future anxiety and depressive symptoms in adolescents with histories of anxiety, and whether neural functioning in brain regions implicated in emotion processing and regulation can account for this link. Following anxiety disorder treatment (Time 1), thirty adolescents (M age=11.58, SD=1.26) reported on maternal warmth and, two years later (Time 2), participated in functional neuroimaging task where they listened to pre-recorded criticism and neutral statements from a parent. Higher maternal warmth predicted lower neural activation during criticism, compared with neutral statements, in the left amygdala, bilateral insula, subgenual anterior cingulate, right ventrolateral prefrontal cortex, and anterior cingulate cortex. Maternal warmth was associated with adolescents’ anxiety and depressive symptoms due to the indirect effects of sgACC activation, suggesting that parenting may attenuate risk for internalizing through its effects on brain function.
Keywords: adolescence, parental warmth, anxiety, depression, fMRI
Anxiety is the most prevalent psychiatric disorder among children and adolescents, affecting up to one in five youth (Beesdo, Knappe, & Pine, 2009). These youth are known to have more difficulty coping with challenging events and negative or potentially threatening information, such as negative social evaluation, leading to poorer psychosocial functioning and distressing levels of emotional reactivity (see reviews by Asselmann & Beesdo-Baum, 2015; Beesdo et al., 2009). Furthermore, studies have shown that the excessive emotional reactivity found in anxiety may be a consequence of neural hypersensitivity to a variety of negative stimuli, including social evaluation and negative facial expressions (see reviews by Beesdo et al., 2009; Strawn et al., 2014). Unfortunately, homotypic and heterotypic continuity of psychiatric disorders is common throughout the lifespan for youth with anxiety (Costello, Copeland, & Angold, 2011), even following anxiety treatment (Kendall, Safford, Flannery-Schroeder, & Webb, 2004). Specifically, the occurrence of childhood clinical anxiety is highly predictive of the re-occurrence of anxiety and onset of depression during adolescence (Bittner et al., 2007; Costello et al., 2011).
This is a major concern for the continued development of youth with a history of anxiety because adolescence is already known to be a risk period for depression and anxiety (Birmaher et al., 1996; Hankin, 2006; Hofmann, Sawyer, Fang, & Asnaani, 2012; Yap, Allen, & Sheeber, 2007), and youth experience increases in emotional lability as they begin facing many new social challenges, such as navigating more complex peer and romantic relationships and more conflictual relationships with parents (Laursen & Collins, 2009; Parker, Rubin, Erath, Wojslawowicz, & Buskirk, 2006; Rudolph & Hammen, 1999). Adolescents also experience an increased awareness of social evaluation and heightened self-consciousness (Rankin, Lane, Gibbons, & Gerrard, 2004). Therefore, it remains important to better understand how positive environmental factors, such as parental warmth, may help bolster resilience against this heightened risk for future disorder in youth with histories of anxiety.
Despite an emphasis on peer influence during adolescence, parents remain an integral part of adolescents’ social environments and play an important role in youths’ emotional development (see reviews by Baumrind, 1991; Yap, Pilkington, Ryan, & Jorm, 2014). Gottman, Katz, and Hooven (1996) theorized that beginning in childhood, youth learn how to effectively regulate their emotions in response to stressful events through warm, responsive, and communicative parenting behavior. Accordingly, warm, positive parenting has been associated with lower levels of child anxiety and depressive symptoms (Bayer, Sanson, & Hemphill, 2006; Schwartz et al., 2014; Schwartz et al., 2017; Yap & Jorm, 2015), and, further, adolescents’ affective response to stress or negative situations have been found to mediate this relationship (Schwartz et al., 2017; Valiente, Lemery‐Chalfant, & Swanson, 2009; Yap, Allen, & Ladouceur, 2008; Yap, Schwartz, Byrne, Simmons, & Allen, 2010). Given that youth with a history of childhood anxiety have a propensity towards emotional overreactivity in response to challenging situations and socially evaluative contexts (Silk, Davis, McMakin, Dahl, & Forbes, 2012), the effects of parental warmth are likely of particular importance to whether these youth will develop anxiety and/or depressive symptoms during the adolescent years. However, the relationship between parenting and clinical child anxiety is not straight-forward, as parents of youth with clinical anxiety can become overprotective and overinvolved which inhibit opportunities for these youth to gain autonomy coping with challenging situations (Ollendick & Grills, 2016).
To this end, previous research on childhood clinical anxiety has found that parenting behaviors are important factors to consider when investigating the maintenance of anxiety in youth (see review by Fisak & Grills-Taquechel, 2007). For example, it is suggested that parents may play a role in transmitting their own cognitions and expectations onto their youth, which consequently either support or discourage threat interpretation biases, anxious behavior, such as avoidance, and fear reactivity in their children (Barrett, Rapee, Dadds, & Ryan, 1996; Dadds, Barrett, Rapee, & Ryan, 1996; Fliek, Roelofs, van Breukelen, & Muris, 2019; Silk et al., 2013). In contrast, supportive and positive parenting behaviors that encourage youth to face fearful or challenging situations have been found to associated with better cognitive behavioral therapy treatment response in youth with anxiety (Silk et al., 2013). Much of the research on the effects of parenting on anxiety and depressive symptoms in youth following anxiety treatment has been completed in studies that assess the enhancing effects of parental involvement in child anxiety therapy treatment protocols (see review by Breinholst, Esbjørn, Reinholdt-Dunne, & Stallard, 2012). Although results of these have been mixed, there are several studies showing that bolstering parenting behaviors that increase parental warmth, increase child autonomy, and enhance parent-child communication during treatment helps to mitigate youths’ risk for the re-occurrence of anxiety and depressive symptoms at long-term follow-up (Barrett, Dadds, & Rapee, 1996; Cobham, Dadds, Spence, & McDermott, 2010).
According to the parental acceptance–rejection theory, individuals who experience low levels of parental warmth are more emotionally labile when faced with stressful events and are more likely to perceive threat within interpersonal contexts (i.e., social threat), compared to those who experience high levels of warmth and acceptance (Rohner, 2004). This suggests that high levels of warmth and acceptance from parents may help buffer or protect adolescents with histories of anxiety after treatment from maintaining a trajectory of increased sensitivity to social evaluative threat, including critical or rejection feedback from parents and peers. The perception that one’s parents are approachable, safe, and helpful during times of need may also help these youth continue to develop their own capacity and self-efficacy to regulate negative emotion when facing stressful situations. Given that depression, similar to and highly co-morbid with anxiety, is also characterized by problems with high negative emotionality, dysregulation, and interpersonal sensitivity (Hankin, 2006), parental warmth following treatment may also be a protective factor against the development of depressive symptoms in these at-risk adolescents.
Developmental models posit that parents continue to influence the development of emotion processing and regulation and associated neural circuitry throughout adolescence because this neural circuitry is still developing and is therefore sensitive to environmental input (A. S. Morris, Silk, Steinberg, Myers, & Robinson, 2007). This suggests that altered activation in such neural circuitry may an important role in linking between parenting and internalizing problems later. Specifically, two key neural networks (i.e., the affective salience network and emotion regulatory network) are found to play a key role in emotion processing and regulation (Casey, Jones, & Hare, 2008; Phillips, Drevets, Rauch, & Lane, 2003; Phillips, Ladouceur, & Drevets, 2008). Within the affective salience network, regions including the amygdala, anterior insula, and subgenual cingulate (sgACC), have been implicated in identifying, appraising, and experiencing emotion in response to negative events (Baird et al., 1999; Casey et al., 2008; Guyer, Lau, McClure-Tone, & et al., 2008; Masten et al., 2011; Mayberg et al., 1999; J. Morris et al., 1996; Phan, Wager, Taylor, & Liberzon, 2002; Phillips et al., 2003; Rudolph, Miernicki, Troop-Gordon, Davis, & Telzer, 2016; Silk et al., 2014). Within the emotion regulatory network, regions including the anterior and posterior dorsolateral and ventrolateral regions (DLPFC; VLPFC), as well as dorsal and rostral regions of the anterior cingulate (ACC) are thought to support cognitive processes involved in down-regulating negative emotion (Casey et al., 2008; Goldin, McRae, Ramel, & Gross, 2008; Nelson & Guyer, 2011; Ochsner & Gross, 2005, 2008; Phan et al., 2002; Phillips et al., 2003; Phillips et al., 2008). For example, when asked to actively reappraise sadness or ignore negatively salient stimuli, both adults and adolescents typically exhibit greater activation in these regulatory regions (Fales et al., 2008; Goldin et al., 2008; Lévesque et al., 2003; Lévesque et al., 2004; Price, Paul, Schneider, & Siegle, 2013; Silvers et al., 2016), supporting this network’s engagement in regulation processes. Therefore, it may be that the effects of parenting on adolescent emotion processing and regulation found in behavioral research may be at least partially attributed to the parental influence on adolescents’ brain function within these two important neural networks.
The current study aims to examine the extent to which adolescents’ perceptions of parenting behavior, specifically warmth, predicts the function of brain regions within the affective-salience and emotion regulation neural networks two-years later, in a sample of adolescents with a history of clinical anxiety. We further test whether the neural function in these brain regions mediates the links between parental warmth and adolescents’ levels of anxiety and depressive symptoms two years later. Importantly, all assessments included in this study were measured after adolescents underwent psychotherapy treatment for their anxiety. Adolescents reported on their perceptions of parental warmth within several weeks of completing a 16-week psychotherapy protocol and adolescents’ neural function and internalizing symptomatology were measured two years later. Therefore, this study is unique in that the results may shed light on the importance of parental warmth for the re-occurrence of internalizing symptoms in a group of adolescents who have an increased risk for future internalizing disorders. Moreover, our longitudinal assessment of adolescents’ neural functioning and internalizing symptoms occurs when adolescents are approximately 13 years old, and subsequently entering a highly transitional period marked by high risk for development of depression.
The current study also specifically assesses adolescents’ neural functioning while they are listening to and processing salient, negative feedback from their parent (i.e., criticism). We chose to utilize real-world parental criticism as a highly salient task stimulus, given that one of the most salient contexts for adolescents is the social domain and adolescents have shown a heightened neural sensitivity to social evaluation (Nelson, Leibenluft, McClure, & Pine, 2005; Silk et al., 2012; Sontag, Graber, & Clemans, 2011). Further, higher levels of neural response to social threat stimuli (e.g., peer rejection and maternal criticism) have been related to the occurrence of anxiety and depression in adolescents (Guyer et al., 2008; Masten et al., 2011; Rudolph et al., 2016; Silk et al., 2017; Silk et al., 2014). Specifically, parental criticism has been shown to effectively elicit activation in the affective-salience (e.g., insula and amygdala) and emotion regulation (e.g., DLPFC and caudal ACC) networks (Aupperle et al., 2016; Hooley et al., 2009; Lee, Siegle, Dahl, Hooley, & Silk, 2014), while higher levels of amygdala activation to criticism has been found in adults and adolescents with depression, relative to healthy individuals (Aupperle et al., 2016; Hooley et al., 2009; Hooley, Gruber, Scott, Hiller, & Yurgelun-Todd, 2005; Silk et al., 2017).
Few studies have reported links between parenting and adolescent neural response to negative or socially threatening stimuli in regions of the affective-salience and/or emotion regulation networks (Butterfield et al., 2019; Guyer et al., 2015; Romund et al., 2016). Existing results show that warm and supportive parenting behaviors are associated with lower levels of adolescent neural response in the amygdala, anterior insula, and perigenual cingulate in response to negatively valenced facial expressions, simulated peer rejection, and threat words (Butterfield et al., 2019; Guyer et al., 2015; Romund et al., 2016), whereas adolescents with mothers reporting higher levels of harsh and punitive parenting behaviors showed reduced VLPFC response to peer rejection (Guyer et al., 2015). Results of one study showed that positive parenting behaviors were inversely related to neural activation in the insula and cingulate (i.e., greater activation) in clinically anxious youth compared to healthy controls, and that these mediated associations with lower levels of avoidant coping in the real world (Butterfield et al., 2019). These studies suggest that warmer and more positive parenting is associated with lower activation in affective salience regions in response to negatively valenced stimuli in healthy youth, while harsher parenting may be associated with lower activation in emotion regulation regions. In addition, one study that investigated the association between parental warmth and concurrent brain activation in healthy adolescents using parental criticism stimuli (as in the current study) found that more warmth was related to less activation in response to criticism within regions involved in social-cognitive processing (e.g., temporal parietal junction and precuneus) but no significant findings within the affective salience or regulatory neural regions (Lee et al., 2014).
Based on the theory that individuals with low levels of parental warmth are more likely to perceive threat within interpersonal contexts (i.e., social threat) (Rohner, 2004), it follows that adolescents who perceive greater levels of warmth from their parent, indexed by perceptions of parenting behaviors that convey acceptance, love, approachability, and attention, will perceive parental critical feedback as less salient and/or threatening and perhaps be more equipped to regulate subsequent negative affect. As such, these youth would likely exhibit lower levels of depressive and anxiety symptoms, compared to those who perceive less warmth from their parents. The present study aims to test this neurodevelopmental model of resilience in which warm parenting may be an important protective factor against continued problems with internalizing disorders in at-risk adolescents. To do this, we investigate how parental warmth may help to buffer the occurrence of future symptoms of anxiety and depression, through the indirect effects of brain function in response to critical parental feedback, in high-risk youth as they age into mid-adolescence. Accordingly, we hypothesized that in response to parental criticism, adolescents who perceived their parent as being warm would exhibit, two years later: 1) less activation in affective salience regions (i.e., amygdala, insula, and sgACC); and 2) more activation in emotion regulatory regions (i.e., VLPFC, DLPFC, and ACC). We next explored to what extent levels of anxiety and depression at the time of the scan could be explained by the association between maternal warmth and neural activation. We hypothesized that lower neural activation in affective salience regions and greater activation in emotion regulation regions would mediate the relationship between higher levels of parental warmth and lower levels of internalizing symptoms two years later.
Method
Participants
Participants were 30 adolescents with a history of anxiety disorder along with their primary caregivers, including 29 birth mothers and one father. Data were collected as part of the Child Anxiety Treatment Study (CATS) and the subsequent longitudinal Child Anxiety Treatment Study-Depression Follow-up (CATS-D) study. CATS was a randomized treatment study assessing predictors and correlates of treatment response to cognitive behavioral therapy (CBT) and child centered therapy (CCT) in anxious youth (see Silk et al., 2016 for treatment descriptions). Participants were recruited from the community through local media advertisements, referrals from pediatricians, school counselors, University mental health clinics, and other University research studies ( Silk et al., 2016). At the original CATS assessment, 9-to-14-year-old anxious youth were required to meet DSM-IV criteria (American Psychiatric Association, 1994) for current generalized anxiety disorder (GAD), separation anxiety disorder (SAD), and/or social anxiety disorder (SocAD). Youth were excluded if they received a primary diagnosis of major depressive disorder, obsessive–compulsive disorder, post-traumatic stress disorder, conduct disorder, substance abuse or dependence, or ADHD combined type or predominantly hyperactive-impulsive type. Exclusion criteria also included an IQ below 70 as assessed by the Wechsler Abbreviated Scale of Intelligence (Psychological Corporation, 1999), or lifetime diagnoses of autism spectrum disorder, bipolar disorder, psychotic depression, schizophrenia, or schizoaffective disorder. Additionally, adolescents with metal braces or other metal objects in their body were excluded due to functional magnetic resonance imaging (fMRI) contraindications. The study was approved by the University Institutional Review Board and written informed consent and assent were obtained from participating primary caregivers and youth, respectively.
A subset of participants from the CATS study was enrolled in the CATS-D follow-up study, which is the focus of the present investigation. The CATS-D study involved annual psychiatric assessments following the conclusion of treatment and an fMRI assessment two years after treatment. The present study includes the youth who provided questionnaire data on parental warmth at post-treatment and completed the 2-year post-treatment fMRI scan as part of the CATS-D follow-up study (N=32). Two participants were removed from analyses due to excessive movement during the fMRI scan. The final sample of 30 participants (56.7% female) were predominantly European American (93.2%). Prior to anxiety treatment, all participants met DSM-IV criteria for at least one primary anxiety diagnosis. Following treatment (i.e., at post-treatment visit/Time 1) participants were an average of 11.58 years old (SD=1.26 years), and 76.7% (n=23) no longer met diagnostic criteria for any clinical diagnosis, 16.7% (n=5) continued to meet for at least one anxiety disorder, and 3.3% (n=1) met for ADHD (non-attentive subtype), and 3.3% (n=1) met for Enuresis. At 2-year, follow-up (i.e., Time 2), participants were on average 13.58 years old (SD=1.27 years), and 70.0% (n=21) of the adolescents no longer met diagnostic criteria for any clinical diagnosis. The remaining participants (n=9) had at least one anxiety diagnosis (n=8) or Tourette syndrome (n=1). None of the participants met criteria for a comorbid diagnosis of depression. Only one participant reported taking a psychotropic medication at 2-year follow-up. See Table 1 for complete demographics and clinical characteristics.
Table 1.
Participant characteristics at pre-treatment, post-treatment, and 2-year follow-up (n=30)
| Pre-treatment | Post-treatment | 2-year follow-up | |
|---|---|---|---|
| Child Age [M (SD)] | 11.10 (1.27) | 11.58 (1.26) | 13.57 (1.27) |
| Sex [N (%) female] | 17 (56.7) | 17 (56.7) | 17 (56.7) |
| Head of Household Education a | 6.06 (.91) | N/A | 6.03 (.82) |
| Race [N (%)] | |||
| White, non-Hispanic | 27 (90.0) | 27 (90.0) | 27 (90.0) |
| Black | 1 (3.3) | 1 (3.3) | 1 (3.3) |
| Biracial | 1 (3.3) | 1 (3.3) | 1 (3.3) |
| Treatment History [N (%)] | |||
| CBT 1 | 19 (62.5) | 19 (62.5) | 19 (62.5) |
| CCT 2 | 11 (37.5) | 11 (37.5) | 11 (37.5) |
| Current DSM IV Diagnosis [N (%)] | |||
| None | 0 | 23 (76.7) | 21 (70.0) |
| Anxiety disorder (1 or more) | 30 (100) | 5 (16.7) | 8 (26.7) |
| GAD 3 | 23 (76.7) | 5 (16.7) | 6 (20.0) |
| Social phobia | 7 (23.3) | 2 (6.6) | 3 (9.9) |
| Specific phobia | 4 (13.3) | 1 (3.3) | 3 (9.9) |
| Separation anxiety | 5 (16.7) | 1 (3.3) | 0 |
| Panic | 1 (3.3) | 0 | 0 |
| ADHD 4 | 1 (3.3) | 1 (3.3) | 0 |
| Tourette syndrome | 1 (3.3) | 0 | 1 (3.3) |
| Enuresis | 2 (6.6) | 1 (3.3) | 0 |
Education levels (4=High School Graduate, 5=some college, 6=college degree, 7=graduate degree; range=4–7), N/A=not assessed
CBT=cognitive behavioral therapy
CCT=child-centered therapy
GAD=Generalized anxiety disorder
ADHD=attention-deficit/hyperactivity disorder.
Procedure
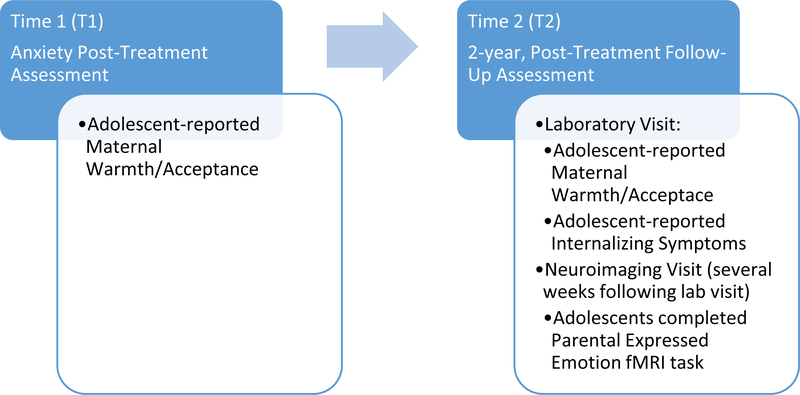
After qualifying for the CATS study, participants were randomized to participate in either a 16-week cognitive behavioral therapy (CBT; n=19) or child centered therapy (CCT; n=11) treatment. Participants randomized to the CBT treatment protocol engaged in anxiety-management skill training, progressive muscle relaxation training, and anxiety-exposure sessions (Kendall & Hedtke, 2006). Participants randomized to the CCT treatment protocol engaged in a non-directive therapy in which the therapist engaged in active listening, reflection, empathy, and encouragement to talk about feelings (CCT; Cohen, Deblinger, Mannarino, & Steer, 2004; Cohen, Mannarino, & Knudsen, 2005). Both treatment types included two parent sessions and parental consultation throughout the treatment period. Full details on treatment protocol and outcomes can be found in Silk et al. (2016). The current study used data collected during post-treatment (Time 1) and 2-year follow-up (Time 2) assessments (collected through the CATS-D follow-up study). At the post-treatment visit, primary caregivers and adolescents completed questionnaires on internalizing symptoms and on caregiver’s parenting behaviors. Two years later, youth repeated the same protocol of clinical interviews and questionnaire assessments during a laboratory visit, and completed an fMRI assessment during a second visit approximately two to three weeks later (see Figure 1 for flow chart of assessments).
Figure 1.
Flow of data collection for variables of interest used in the current study.
Measures
Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (KSADS-PL).
The KSADS-PL (Kaufman et al., 1997) was completed at intake to confirm diagnosis for CATS study eligibility and was repeated at follow-up assessments. Trained Master’s-degree level independent evaluators (IE’s) interviewed parents and youth separately. Based on 20% of interviews, inter-rater reliability was high (κ=.89) for anxiety diagnoses.
Screen for Child Anxiety-Related Emotional Disorders (SCARED-C).
Adolescents reported on their level of anxiety symptoms using the SCARED-C (Birmaher et al., 1997) at post-treatment and at 2-year follow-up. This is a 41-item questionnaire for use in 8- to 18-year-olds. Using the two-year follow-up assessment, high internal consistency (α=.92) was established in the current sample.
Mood and Feelings Questionnaire (MFQ-C), Child-Report.
The Mood and Feelings Questionnaire (MFQ; (Costello & Angold, 1988) is a 33-item self-report questionnaire assessing depressive symptoms in youth 8 to 18 years of age. Participants are asked to rate how true each item is of their mood and behavior within the past two-weeks on a three-point Likert scale (0 = “not true,” 1 = “sometimes,” 2 = “true”). Sample items include “I felt miserable or unhappy,” “I cried a lot,” “I slept a lot more than usual.” Higher total scores reflect greater symptomatology.
The MFQ was administered at various points throughout the larger study. Adolescent-reported, total scores at post-treatment follow-up (T1) were used as a covariate in analyses. Total scores from the two-year follow-up assessment (T2) were used as an outcome measure. Using the two-year follow-up assessment, high internal consistency (α=.96) has been established in the current sample.
Child Report on Parental Behavior Inventory (CRPBI).
Adolescents completed the short version of the CRPBI (Schaefer, 1965; Schludermann & Schludermann, 1970), which includes 30-items that measured perceptions of their mother’s behaviors on three constructs: acceptance, psychological control, and behavioral control. The present study focused on the 10-item parental warmth/acceptance subscale scores. For the current study, subscale scores collected at post-treatment were used as the primary predictor and scores collected at two-year follow-up were used as a covariate. This subscale indicates adolescent’s perceptions of parenting behaviors that convey acceptance, love, approachability, and attention. Items include “my parent…”: “makes me feel better after talking over my worries with her”; “gives me a lot of care and attention”; “believes in showing her love for me”; “smiles at me very often”; “is able to make me feel better when I am upset”; “enjoys doing things with me”; “cheers me up when I am sad”; “makes me feel like the most important person in their life”; “often praises me;” “is easy to talk to”. Statements are rated as “not like”, “somewhat like”, or “a lot like” on a three-point Likert scale (scale range=10.00 – 30.00). The scale evidenced high internal consistency (α=.78) for the current sample.
Functional Magnetic Resonance Imaging (fMRI) Assessment
Parental Expressed Emotion task.
Functional images were collected using an adaptation of the Parental Expressed Emotion neuroimaging paradigm (Hooley et al., 2009; Hooley et al., 2005; Lee et al., 2014). On the first visit of the two-year follow-up assessment, parents were asked to create and record two 30-second clips describing aspects of their adolescents’ behavior that bothered them (i.e., criticism), two 30-second clips describing aspects of their adolescents’ behavior that they especially liked (i.e., praise), and two 30-second neutral clips (i.e., neutral). The current study focused on the criticism condition and uses the neutral condition for comparison. Each criticism statement began with a scripted introduction (i.e.; “[Child’s Name], one thing that bothers me about you is...”). The neutral condition included parents’ statements about the weather, or a trivial event that they felt the child would not be very interested in.
At the second visit of the two-year follow-up assessment, youth underwent an fMRI assessment at a University brain imaging center. Participants were oriented to the scanner noises, trained to minimize head movement, and given time to practice the paradigms and become familiar with the scanner environment in an MRI simulator. During the fMRI scan, participants completed a 7-minute structural scan, followed by the Parental Expressed Emotion fMRI paradigm. During the fMRI assessment, the parent recorded clips were played over scanner-safe headphones in a block design. There was a run for each statement condition (praise, criticism, and neutral). Each run began with a 30.06 second rest period, followed by one 30.06 second statement presentation (30 s audio clip with 0.06 s additional duration to match with our 1.67-second TR), a second rest period, the second statement presentation (same-condition), and a third rest period. Each run of the task followed this procedure and were each 150.3 seconds long. The neutral run began the task for all participants, followed by either the praise and criticism runs, which were counterbalanced across the sample. Following the fMRI assessment, participants were asked to rate their subjective emotions regarding the recorded comments outside of the scanner. Using a post-assessment valence and arousal form, they rated on a scale of 1 (not at all) to 10 (very) how positive and negative each comment was and how good and upset each comment made them feel.
fMRI Data Acquisition
Data were collected on a 3T Siemens Trio scanner. Each volume consisted of 32 interleaved slices (3.2mm). Volumes were acquired parallel to the posterior-anterior commissure line using a T2*-weighted echo planar imaging pulse sequence with 1670ms repetition time (TR), 29ms echo time (TE), 75° flip angle, 3.2 × 3.2 × 3.2mm voxels, 205 × 205 field of view (FOV), 64 × 64 matrix size. Scanning began at the first rest-period onset, and 18 scans were acquired per 30.06 second trial including both rest and stimulus types. Three conditions (criticism, praise, and neutral) were acquired during individual scan runs, lasting 2.5 minutes each. A total of 270 volumes were acquired for the complete task (90 volumes per run). 176 high-resolution, T1-weighted MPRAGE images were also acquired (TR=2100ms, TE=3.31ms, FOV=256 × 256, voxel size=1.0 × 1.0 × 1.0mm, flip angle=8°, slice thickness=1mm) for co-registration pre-processing procedures.
fMRI Data Analysis
Images were pre-processed using SPM12 (http://www.fil.ion.ucl.ac.uk/spm). Volumes were re-oriented to the AC and corrected for slice timing. Images were next realigned to correct for head motion, segmented, and co-registered to a mean functional image. Realigned images were spatially normalized to a standard MNI template (Montreal Neurological Institute template) using a 12-parameter affine model. Normalized images were smoothed with a 6mm full-width at half-maximum Gaussian filter. Voxels were resampled during preprocessing to be 2mm3. If participants exhibited absolute motion greater than 2mm/2º and global intensities more than 3 SD from the mean for more than 25% of volumes per run (i.e., either during the criticism or neutral runs), they were excluded (n=2) from analyses. For all included participants, voxel-wise despiking was completed with interpolation using the ArtRepair toolbox. Repaired volumes were used for 1st level analysis. Six motion parameters were included as regressors in the 1st level GLM design to correct for slow-drift motion.
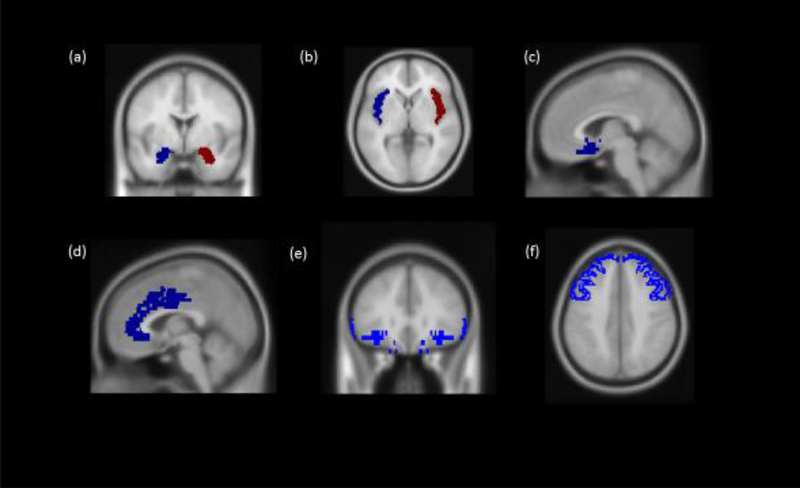
Conditions from each run, including criticism, praise, neutral, and rest, along with six motion parameters, were included as regressors in the 1st level GLM design. Contrasts were created in the 1st level SPM designs. The current analyses included data using the Criticism>Neutral contrast of interest. A priori regions-of-interest (ROI) were anatomically predefined by either Brodmann areas or the Automated Anatomical Labelling (AAL) atlas using the WFU PickAtlas Tool (v3.0.5). ROIs included the bilateral amygdala (AAL), bilateral anterior insula (AAL), sgACC (BA25), ACC (BA24/BA32), bilateral VLPFC (BA45/47), and bilateral DLPFC (BA8/BA9/BA46). Using individual masks of each a priori ROI (see Figure 2), parameter estimates (beta weights) for Criticism>Neutral contrast were extracted using Marsbar. Given the current study’s focus on threat circuitry, we focus on neural response to criticism because adding ROIs implicated in neural response to reward would have increased the number of analyses inflating Type 1 error. Results of neural response to parental praise are provided elsewhere (see Sequeira, Butterfield, Silk, Forbes, & Ladouceur, 2019).
Figure 2.
Masks of anatomically defined regions-of-interest:(a) amygdala and (b) insula, (c) subgenual cingulate, (d) anterior cingulate, (e) ventrolateral prefrontal cortex and (f) dorsolateral prefrontal cortex. All ROIs were bilateral.
Statistical Analysis
SPSS was used for all study analyses. Preliminary analyses assessed bivariate correlations between sample characteristics and variables of interest. Hypothesis testing was conducted using multiple regression models for each individual, a priori ROI (ntests=12). Benjamini-Hochberg procedures (Benjamini & Hochberg, 1995) were used to account for multiple comparisons with a false discovery rate (FDR) of 0.05. To adjust for changes in parental warmth between assessments, we covaried for parental warmth at Time 2. We next tested whether adolescents’ neural activation to criticism mediated associations found between parental warmth and adolescents’ anxiety and depressive symptoms at Time 2 (in separate models). The PROCESS macro for SPSS was used to test for indirect effects through Bootstrapping methods (5,000 iterations), controlling for parental warmth reported at Time 2 and adolescents’ symptom levels reported at Time 1. Due to 1–2 outlying data points for the independent variable of interest and several of the ROI variables, sensitivity analyses were completed with extreme values winsorized to their respective thresholds (i.e., 1st/3rd quartiles +/− 1.5*IQR). Results of the main analyses and of sensitivity analyses were maintained using winsorized data, suggesting that the effects are not due to outlier values. Therefore, we present results of the original data.
Results
Preliminary Results
Bivariate correlations between variables of interest are shown in Table 2. Of note, girls were more likely to report higher levels of depressive and anxiety symptoms at Time 2 (t=2.426, p=.02; t=2.035, p=.05, respectively). Older youth also reported higher depressive and anxiety symptom levels (r=.374, p=04; r=.347, p=06, respectively). Levels of anxiety symptoms were highly correlated across the two time points (r=.797, p=.001), whereas depressive symptoms across time were only modestly correlated (r=.239, p=.204). Anxiety level at post-treatment was highly predictive of depressive symptoms at two-year follow-up (r=.573, p=.001). Levels of anxiety and depressive symptoms at Time 2 were highly correlated (r=.743, p<.001). Adolescents’ reports of anxiety symptom levels at Time 1 (range=0–50; M=16.05, SD=13.48) were not significantly associated with concurrent reports of parental warmth (i.e., Time 1) (r=.072, p=.704) and were therefore not covaried in analyses assessing the relations between parenting and neural response to criticism.
Table 2.
Correlation matrix of all variables of interest (n=30).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | 1 | ||||||||||||||
| 2. Age | .038 | 1 | |||||||||||||
| 3. Parental warmth (post-tx) | −.197 | −.187 | 1 | ||||||||||||
| 4. Depressive Sx (2-years post-tx) | .417* | .374* | .112 | 1 | |||||||||||
| 5. Anxiety Sx (2-years post-tx) | .344 | .347 | .187 | .743*** | 1 | ||||||||||
| 6. L Amygdala | .225 | .046 | −.546*** | −.040 | −.203 | 1 | |||||||||
| 7. R Amygdala | .269 | .141 | −.264 | .100 | −.059 | .708*** | 1 | ||||||||
| 8. L Anterior Insula | .133 | .029 | −.498*** | −.061 | −.166 | .523*** | .468** | 1 | |||||||
| 9. R Anterior Insula | .165 | .058 | −.481*** | −.024 | −.189 | .630*** | .664*** | .896*** | 1 | ||||||
| 10. sgACC | .421* | .055 | −.528*** | .240 | .141 | .667*** | .545*** | .588*** | .549*** | 1 | |||||
| 11. ACC | .275 | −.111 | −.522*** | −.008 | −.254 | .713*** | .580*** | .768*** | .826*** | .715*** | 1 | ||||
| 12. L VLPFC | .149 | .075 | −.309 | .136 | −.035 | .397** | .344 | .813*** | .679*** | .534*** | .683*** | 1 | |||
| 13. R VLPFC | .204 | −.002 | −.474*** | .024 | −.180 | .486** | .437* | .752*** | .817*** | .564*** | .815*** | .751*** | 1 | ||
| 14. L DLPFC | −.014 | −.105 | −.168 | −.055 | −.355 | .495** | .263 | .310 | .356 | .303 | .541*** | .501*** | .457* | 1 | |
| 15. R DLPFC | .337 | .068 | −.302 | .241 | −.071 | .426** | .252 | .286 | .366* | .434* | .628*** | .492** | .629*** | .599*** | 1 |
p<.05,
p<.01
p<.005;
Note:Sx=symptoms, Tx=treatment, L=left, R=right; sgACC=subgenual cingulate cortex; ACC=anterior cingulate; VLPFC=ventrolateral prefrontal cortex; DLPFC=dorsolateral prefrontal cortex.
A paired samples t-test showed that levels of maternal warmth reported by adolescents at post-treatment (M=25.87, SD=4.42) and at 2-year follow-up (M=24.63, SD=4.16) did not differ significantly (t(29)=1.11, p=.290). However, levels of warmth were not significantly correlated (r=−0.067, p=.727) across time points. In order to probe the low correlation, outliers in change scores of maternal warmth from Time 1 to Time 2 were identified using the +/− 1.5 x IQR method, which showed that this low correlation may be driven by two participants who reported extreme change. Although these change scores are technically outliers, we believe that for some adolescents, such major changes in perceptions of parenting are possible. Thus, the low correlation seems to suggest that perceptions of parental warmth in our sample were not stable for a small portion of adolescents. Therefore, we included parental warmth at Time 2 as a covariate to control for changes in adolescents’ perceptions of parental warmth in our final analyses. Similar to reports across the full sample (Silk et al., 2019) levels of anxiety and depressive symptoms at Time 2 were significantly higher in adolescents who received child-centered therapy (anxiety: M=24.82, SD=12.02; depression: M=14.36, SD=9.28), compared to those who received cognitive behavioral therapy (anxiety: M=13.68, SD=9.25; depression: M=7.42, SD=8.22; t=2.847, p=.008; t=2.128, p=.04, respectively). No differences were found in other study variables between treatment type groups. Therefore, treatment type was added as a covariate in the final models assessing indirect effects of parenting on adolescents’ internalizing symptoms at Time 2 through brain functioning involved in emotion processing.
Adolescents’ Ratings of Parents’ Comments
One participant did not complete post-scan ratings after their scan, and one additional participant did not complete ratings for neutral statements; behavioral results are based on participants with full data available. A paired samples t-test of adolescents’ post-scan ratings showed that parents’ critical statements were both more negative and upsetting (M=5.21, SD=1.33; M=4.60, SD=1.97, respectively) to participants than parents’ neutral statements (M=2.30, SD=1.47; M=2.07, SD=1.68, respectively; t(27)=5.786, p<.001). Neither adolescent-reported parental warmth at Time 1 or Time 2 was correlated with their ratings of perceived negativity or upset feelings in response to hearing their parents’ critical statements (r’s= .119-.142, ps>.40). Higher post-scan ratings of perceived negativity were significantly positively associated with neural response to criticism in the sgACC (r=.385, p=.04).
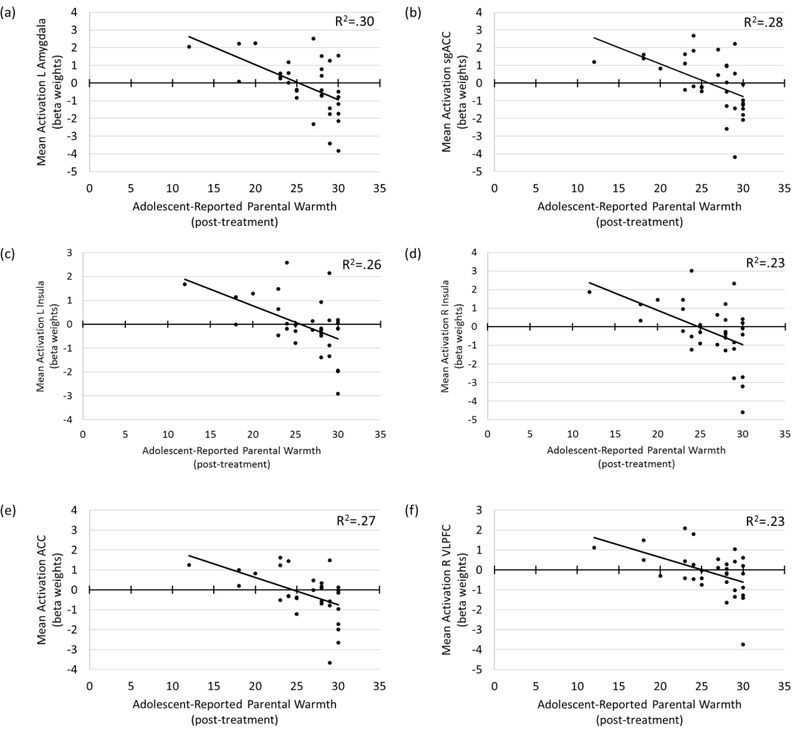
Parenting and Adolescents’ Neural Response to Parental Criticism Two Years Later
Adolescent-reported parental warmth at Time 1 predicted neural activation to parental criticism in several affective salience network regions at Time 2, controlling for levels of parental warmth at Time 2. Specifically, greater levels of parental warmth predicted lower activation in the left amygdala (β = −0.545, puncorr=.002), bilateral insula (Left: β = −0.504, puncorr=.005; Right: β = −0.480, puncorr=.008), and sgACC (β = −0.527, puncorr=.003) (see Fig. 3). Parental warmth did not predict activation in the right amygdala (β = −0.264, puncorr=.167). All significant results survived correction for multiple comparisons (ps-FDR<.05; Table 3). No significant Warmth X Sex interaction effects were found in the models and were therefore not considered further. Sensitivity analyses showed that after accounting for main effects of adolescent sex and age at the time of the scan in the models, parental warmth at Time 1 continued to predict neural response to criticism within the left amygdala (β = −0.527, puncorr=.005), bilateral insula (L: β = −0.518, puncorr=.008; R: β = −0.468, puncorr=.017), and sgACC (β = −0.428, puncorr=.010) (ps-FDR<.05).
Figure 3.
Associations between parental warmth at post-treatment (i.e., Time 1) and neural response to parental criticism (versus neutral) two years later in the: (a) left amygdala, (b) subgenual cingulate (sgACC), (c) left insula, (d) right insula, (e) ACC (incl. dorsal and perigenual regions), and (f) right ventrolateral prefrontal cortex (VLPFC). Note: R-square controls for parental warmth reported at Time 2.
Table 3.
Associations between adolescent-reported parental warmth and neural response to criticism at 2-year follow-up, controlling for concurrent (T2) levels of parental warmth (n=30)1
| Outcome Variable (T2) | F | R2 | B (SE) | β | t | p-uncorr | p-FDR-adjusted |
|---|---|---|---|---|---|---|---|
| L Amygdala | 5.746** | .299 | |||||
| Parental warmth T1 | −.180 (.053) | −.545*** | −3.373** | .002 | .0125 | ||
| R Amygdala | 1.010 | .070 | |||||
| Parental warmth T1 | −.131 (.093) | −.264 | −1.420 | .167 | .186 | ||
| L Anterior Insula | 4.643* | .256 | |||||
| Parental warmth T1 | −.135 (.045) | −.504*** | −3.027*** | .005 | .0125 | ||
| R Anterior Insula | 4.070* | .232 | |||||
| Parental warmth T1 | −.172 (.061) | −.480** | −2.839** | .008 | .016 | ||
| sgACC | 5.217* | .279 | |||||
| Parental warmth T1 | −.166 (.052) | −.527*** | −3.219*** | .003 | .0125 | ||
| ACC | 5.096* | .274 | |||||
| Parental warmth T1 | −.122 (.038) | −.525*** | −3.192*** | .004 | .0125 | ||
| L VLPFC | 2.921t | .178 | |||||
| Parental warmth T1 | −.095 (.050) | −.328t | −1.874t | .072 | .103 | ||
| R VLPFC | 3.924* | .225 | |||||
| Parental warmth T1 | −.121 (.043) | −.472** | −2.782** | .010 | .017 | ||
| L DLPFC | .669 | .049 | |||||
| Parental warmth T1 | −.058 (.069) | −.159 | −.844 | .406 | .406 | ||
| R DLPFC | 1.496 | .100 | |||||
| Parental warmth T1 | −.099 (.059) | −.308t | −1.685t | .104 | .130 | ||
p-uncorr≤.10,
p-uncorr≤.05,
p-uncorr≤.01,
p-uncorr≤.005;
Note: L=left, R=right, sgACC=subgenual cingulate, ACC=anterior cingulate; VLPFC=ventrolateral prefrontal cortex; DLPFC=dorsolateral prefrontal cortex. All analyses were conducted with extracted mean BOLD response across each anatomically defined ROI.
Because puberty is an important developmental consideration during adolescence and to brain function (Nelson et al., 2005), analyses were re-run replacing the covariate of adolescent age with adolescent-reported pubertal status at time of the scan, measured by the Pubertal Development Scale (PDS; Petersen, Crockett, Richards, & Boxer, 1988; Shirtcliff, Dahl, & Pollak, 2009). Adolescent age and pubertal status were significantly correlated (r=.559, p=.001). Results were replicated, showing that parental warmth at Time 1 continued to predict neural response in the left amygdala, bilateral insula, and sgACC (ps-FDR<.05).
Adolescent-reported parental warmth at Time 1 also significantly predicted neural activation in response to parental criticism in several emotion regulatory network regions at Time 2, controlling for levels of parental warmth at Time 2. Specifically, higher levels of parental warmth predicted lower activation in the ACC (β = −0.525, puncorr=.004) and right VLPFC (β = −0.472, puncorr=.010) (see Fig. 3). Parental warmth did not predict activation in the left VLPFC (β = −0.328, puncorr=.072) or bilateral DLPFC (Left: β = −0.159, puncorr=.406; Right: β = −0.308, puncorr=.104). Significant results survived correction for multiple comparisons (ps-FDR<.05; Table 3). No significant Warmth X Sex interaction effects were found in the models and therefore were not considered furthered. Sensitivity analyses showed that after accounting for main effects of sex and age at the time of the scan , parental warmth at Time 1 continued to predict neural response to criticism within the ACC (β = −0.532, puncorr=.004) and right VLPFC (β = −0.463, puncorr=.018) (ps-FDR<.05). Results were replicated when pubertal status rather than age, was used as a covariate (ps-FDR<.05).
Indirect Effects on Adolescent Internalizing Symptoms.
Anxiety Symptoms.
Controlling for adolescent anxiety symptoms at Time 1, parental warmth at Time 2, and treatment type, indirect effects of adolescents’ neural response in the sgACC to parental criticism at Time 2 were found to account for the link between parental warmth at Time 1 and adolescents’ anxiety symptoms at Time 2. Greater parental warmth at Time 1 predicted lower anxiety symptoms at Time 2 as a function of lower sgACC activation in response to criticism (Indirect Effect = −.553, SE=.24, β = −.212 [CI 95%: −1.106, −.117]). No further evidence of indirect effects were found in models using other ROIs as mediators. Sensitivity analyses showed that results were maintained after accounting for age and sex in the model [B = −448, SE=.27, β = −.172 [CI 95%: −.1.079, −.036]). Results were replicated using pubertal status as a covariate in place of age and also remained significant using winsorized data.
Depressive Symptoms.
Controlling for adolescent depressive symptoms at Time 1,parental warmth at Time 2, and treatment type, indirect effects were again found only through neural activation in the sgACC. Greater parental warmth at Time 1 predicted lower depressive symptoms at Time 2 as a function of lower sgACC activation in response to criticism (Indirect Effect = −.413, SE=.23, β = −.200; [CI 95%: −.927, −.009]). However, sensitivity analyses showed that after accounting for age (or pubertal status) and sex in the model, the indirect effect decreased [i.e., B = −293, SE=.21, β = −.142; [CI 95%: −.717, .124]), and was no longer significant. This was primarily due to the effects of sex in the model. Again, results were replicated using winsorized data.
Discussion
The aim of the current study was to examine whether adolescent perceived maternal warmth following anxiety treatment was associated with adolescents’ neural response to personalized parental criticism two years later. Another aim was to explore the extent to which these associations accounted for adolescents’ anxiety and depressive symptoms at the time of their scan. Findings from the present study show that adolescents who perceived their mothers to be higher in warmth, including acceptance, love, approachability, and attention, tend to show lower levels of neural activation in the left amygdala, bilateral insula, sgACC, ACC, and right VLPFC to personally relevant criticism from their parents two years later. In addition, results show that higher maternal warmth was related to adolescents’ lower internalizing symptoms two years later through the indirect effects of lower neural activation in the sgACC. These findings provide evidence that parenting may continue to play an important role in shaping neural processes supporting emotion processing and regulation during adolescence, and that these neural processes may be indirectly associated with how parenting relates to internalizing psychopathology in their adolescent children (see reviews by A. S. Morris et al., 2007; Tan, Oppenheimer, Ladouceur, Butterfield, & Silk, In Press), even following treatment for anxiety. Notably, the behavioral results showed that levels of maternal warmth were not associated with how negatively adolescents perceived the critical statements. This suggests that adolescents’ neural response to criticism was not necessarily due to differences between the harshness of statements, at least from participants’ perspectives.
As hypothesized, we found that higher adolescent-reported parental warmth is associated with reduced left amygdala, bilateral insula, and sgACC activation to parental criticism two years later. These brain regions are considered part of an affective salience network that has been shown to underlie processes involved in identifying, appraising, and perceiving cues as salient (Phillips et al., 2003). Our findings are consistent with previous results showing that heathy adolescents with warmer and more supportive parents exhibit reduced hemodynamic response in the amygdala and insula to challenging stimuli such as negative facial affect, threat words, and peer social rejection cues (Butterfield et al., 2019; Guyer et al., 2015; Romund et al., 2016). However, it should be acknowledged that adolescents’ neurobiological response and associated emotional arousal to negative stimuli may be influenced by genetic factors transmitted from parents. Therefore, genetic factors may be accounting for the observed association—for example, parents who are higher in positive affect, and subsequently display more warmth, may have passed along a different biological proclivity in emotional responses to their children in ways that contributed to emotional arousal response patterns.
We also hypothesized that higher parental warmth would be related to greater recruitment of regulatory brain regions, which are posited to dampen affective salience network reactivity (Casey et al., 2008; Phillips et al., 2003). Instead, findings showed that adolescents reporting higher levels of parental warmth and acceptance exhibited reduced activation in the ACC and right VLPFC to parental criticism. Because projections between the affective salience and emotion regulation networks are bi-directional (Casey et al., 2008), it is possible that the lower activation of regulatory regions in adolescents with warmer parents indicates a reduced need to regulate or dampen affective salience region activation, as these were the adolescents who did not show engagement of the affective salience network. Another possible interpretation may be drawn from literature on the neural substrates of social pain (i.e. painful feelings of rejection or experience of “hurt” feelings following negative social interactions or feedback) (Eisenberger, 2012). For example, Eisenberger et al. (2012) showed that greater dACC activation (in addition to insula and sgACC activation) is associated with the experience of pain, distress, and disconnectedness following social exclusion experiences (Eisenberger, 2012). Therefore, the lower ACC activation (inclusive of the dACC) in response to parental criticism may indicate that adolescents with greater parental warmth may be experiencing lower levels of distress following instances of social threat.
Notably, results of a previous study reported a different association between positive parenting and neural response to negative stimuli in the same sample of clinically anxious adolescents as in the current study (Butterfield et al., 2019). That study found that prior to anxiety treatment adolescents exhibited greater insula and pgACC activation to negatively valenced stimuli (i.e., physical threat words) if their parent tended to promote positive coping strategies, which in turn was associated with lower avoidant coping use in adolescents (Butterfield et al., 2019). However, we now find that following a 16-session psychotherapy anxiety treatment protocol, parental warmth (assessed at post-treatment) is related to lower neural activation in overlapping brain regions two years later. The contrasting results of these two studies within the same sample may be due to differences in adolescents’ development (i.e., the sample was older in the current study). Other considerations include differences in study methodology, such as major differences in parenting constructs (observed coping socialization practices versus adolescent-reported warmth), fMRI processing streams and task stimuli (physical threat words versus recorded, personalized parental criticism), study designs (correlational versus longitudinal) and analytical strategies, and possible effects of treatment on neural functioning. Therefore, it is difficult to attribute the differences in findings to one specific cause and future research is warranted—particularly with larger samples to assess changes in adolescent neural function as it relates to parenting using longitudinal, repeated assessments of the same parenting constructs and fMRI tasks. Nevertheless, the results of the current study offers an important addition to the field of developmental psychopathology by providing support that parenting has important and lasting effects on adolescents’ neural substrates of emotion processing. Furthermore, our findings also suggest that adolescents’ neural function in emotion processing regions mediate the longitudinal influence of parenting on adolescents’ internalizing symptoms following anxiety treatment in a sample of youth at high risk for anxiety remission and future depression.
Overall, the patterns of results in the current study support the theory posited by Rohner (2004) suggesting that those adolescents who perceive their parents as warmer may be less emotionally labile when processing critical feedback. Consistent with this theory, it may be that adolescents who perceive their parents as warmer and more accepting would also feel safer within the context of the relationship and have less neural reactivity in response to critical feedback from their parents. Of note, we found these effects in a sample of youth whose perceptions of maternal warmth were generally quite high. Therefore, our results may be somewhat conservative estimates of the effects of maternal warmth on neural response to criticism. Our findings further show that greater parental warmth predicts lower depressive and anxiety symptoms in adolescents two years later as a function of parental influence on sgACC activation. This suggests that adolescents who perceive their parents to be warmer may not only be less reactive to critical feedback, but also that this dampened neural reactivity has important clinical implications. Prior studies have shown that greater sgACC activation during cognitive and affective neuroimaging tasks is associated with elevated depressive and anxiety symptoms in adults and adolescents (Campbell-Sills et al., 2011; Hamilton, Farmer, Fogelman, & Gotlib, 2015; Masten et al., 2011; Simpson, Drevets, Snyder, Gusnard, & Raichle, 2001; Yang et al., 2009). Therefore, the sgACC has been a target of deep brain stimulation treatment for depression and is considered to play a critical role in depression (Holtzheimer et al., 2012; Mayberg et al., 2005). Our findings indicate that parents’ effects on the adolescents’ neural processing of critical evaluation from parents, particularly within the sgACC, may play a role in helping to minimize the risk for depression and anxiety in their adolescent children. These are exciting findings given that the population of adolescents represented in our sample is at increased risk for future psychopathology in adolescents and young adults (Costello et al., 2011). However, these findings should be interpreted with caution, as internalizing symptoms were reported several weeks prior to the fMRI scan, our sample size was limited, and the indirect effect predicting depressive symptoms was no longer statistically significant after covarying for age and sex.
The current study has many strengths, including its prospective longitudinal design, use of a personalized, ecologically valid neuroimaging task, and the investigation of parental influences on the neural substrates of emotion processing in a clinical sample of adolescents at high-risk for lifetime anxiety and depression. Despite these strengths, there were some limitations. Although the study focused on the neural systems supporting emotion processing and regulation, we recognize that the task does not include explicit emotion regulation (e.g., reappraisal of parental criticism), which potentially limits the interpretation of findings within the regulatory neural network. In addition, the sample size was relatively small, which hindered our ability to capture small to moderate effects in this study. For example, although we were not able to detect significant interactions between sex and parenting in the current study, there are recent findings showing that negative parenting may be associated with higher depressive symptoms in adolescent girls, but not boys, as a function of neural activation in the anterior insula and ACC (Chaplin et al., 2019). Therefore, more studies with larger samples are needed to more effectively examine the effects of this potentially important moderator. Also, the effects of race and socioeconomic status (SES) were also not explored in the study due to the ethnically homogeneous and mostly college-educated sample, which should be addressed in future research. In addition, several adolescents reported extreme changes in maternal warmth across the two study time points. Although we controlled for maternal warmth at Time 2 in the analyses, we acknowledge that the predictive value of parenting may be limited for youth whose perceptions shift dramatically across time. Future work should also consider the potential impact of paternal warmth and/or differences in adolescents’ neural response to hearing criticism from their fathers, as the current study assessed maternal warmth and neural response to mothers’ recordings of criticism, with the exception of one participant who heard their father’s criticism. Finally, future research should include a comparison group of untreated anxious youth to investigate the possible effects of therapy on the association between parental warmth and adolescent neural processing of social threat.
Despite these limitations, our results support theories that youth may learn how to adaptively process negative interpersonal feedback as a function of warm and responsive parenting behavior (Gottman, Katz, & Hooven, 1996; A. S. Morris et al., 2007; Rohner, 2004). These findings may have implications that could inform early intervention approaches. For example, social learning shaped by parents’ feedback could interact with how adolescents process negative evaluative feedback from by peers—which becomes more salient across child and early adolescent development. Although speculative, these could have important implications for adolescent trajectories, given the increase of novel peer-related social challenges occurring − an important direction for future research. Furthermore, the present study expands a limited yet growing area of research investigating how parental factors continue to affect the functioning of neural networks that support emotion processing and regulation throughout adolescence—and their relevance to inform intervention strategies for youth at high risk for lifetime anxiety and depression. Our results support the ongoing importance of parental factors, such as warmth, as remaining important to the psychological well-being of their adolescent children even following treatment for anxiety. Therefore, despite mixed results on the benefits of integrating parents into child and adolescent anxiety treatment (Breinholst et al., 2012), child anxiety interventions that include a focus of increasing parental warmth, acceptance, and approachability seems to be a promising approach to protecting adolescents against the risk of future anxiety relapse and depression onset. However, it is important to note that for youth with clinical anxiety, such parental warmth and acceptance may be most beneficial to adolescent development when provided in conjunction with enhanced parent-child communication and increased child autonomy granting behaviors, which should be addressed in future research.
Acknowledgments
Funding:
This work was supported by National Institutes of Health [P50 MH080215 and MH091327].
Footnotes
Sensitivity analyses were completed excluding the participant whose father recorded the statements for the fMRI task. Regression coefficients remained significant when associating warmth with the left amygdala, bilateral insula, subgenual cingulate, anterior cingulate, and right ventrolateral prefrontal cortex. Maternal warmth at time 1 continued to predict anxiety and depressive symptoms at time 2, with an indirect effect through activation of the subgenual cingulate in response to criticism (controlling for therapy type, symptoms at time 1, and warmth at time 2).
REFERENCES
- Asselmann E, & Beesdo-Baum K (2015). Predictors of the Course of Anxiety Disorders in Adolescents and Young Adults. Current Psychiatry Reports, 17(2), 1–8. doi: 10.1007/s11920-014-0543-z [DOI] [PubMed] [Google Scholar]
- Aupperle RL, Morris AS, Silk JS, Criss MM, Judah MR, Eagleton SG, … Alvarez RP (2016). Neural responses to maternal praise and criticism: Relationship to depression and anxiety symptoms in high-risk adolescent girls. NeuroImage: Clinical, 11, 548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird AA, Gruber SA, Fein DA, Maas LC, Steingard RJ, Renshaw PF, … Yurgelun-Todd DA (1999). Functional magnetic resonance imaging of facial affect recognition in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 38(2), 195–199. doi: 10.1097/00004583-199902000-00019 [DOI] [PubMed] [Google Scholar]
- Barrett PM, Dadds MR, & Rapee RM (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Rapee RM, Dadds MM, & Ryan SM (1996). Family enhancement of cognitive style in anxious and aggressive children. Journal of Abnormal Child Psychology, 24(2), 187–203. doi: 10.1007/BF01441484 [DOI] [PubMed] [Google Scholar]
- Baumrind D (1991). Effective parenting during the early adolescent transition. Family transitions, 2(1), 1. [Google Scholar]
- Bayer JK, Sanson AV, & Hemphill SA (2006). Parent influences on early childhood internalizing difficulties. Journal of Applied Developmental Psychology, 27(6), 542–559. [Google Scholar]
- Beesdo K, Knappe S, & Pine DS (2009). Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatric Clinics of North America, 32(3), 483–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale Construction and Psychometric Characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. doi: 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, … Nelson B (1996). Childhood and Adolescent Depression: A Review of the Past 10 Years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry, 35(11), 1427–1439. doi: 10.1097/00004583-199611000-00011 [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, & Angold A (2007). What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry, 48(12), 1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x [DOI] [PubMed] [Google Scholar]
- Breinholst S, Esbjørn BH, Reinholdt-Dunne ML, & Stallard P (2012). CBT for the treatment of child anxiety disorders: A review of why parental involvement has not enhanced outcomes. Journal of anxiety disorders, 26(3), 416–424. [DOI] [PubMed] [Google Scholar]
- Butterfield R, Siegle G, Lee K, Ladouceur C, Forbes E, Dahl R, … Silk J (2019). Parental Coping Socialization is Associated with Healthy and Anxious Early-Adolescents’ Neural and Real-World Response to Threat. Developmental Science, e12812. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Simmons AN, Lovero KL, Rochlin AA, Paulus MP, & Stein MB (2011). Functioning of neural systems supporting emotion regulation in anxiety-prone individuals. NeuroImage, 54(1), 689–696. doi: 10.1016/j.neuroimage.2010.07.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey B, Jones RM, & Hare TA (2008). The adolescent brain. Annals of the New York Academy of Sciences, 1124(1), 111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM, Poon JA, Thompson JC, Hansen A, Dziura SL, Turpyn CC, … Ansell EB (2019). Sex‐differentiated associations among negative parenting, emotion‐related brain function, and adolescent substance use and psychopathology symptoms. Social Development. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH, & McDermott B (2010). Parental anxiety in the treatment of childhood anxiety: A different story three years later. Journal of Clinical Child & Adolescent Psychology, 39(3), 410–420. [DOI] [PubMed] [Google Scholar]
- Costello EJ, & Angold A (1988). Scales to assess child and adolescent depression: checklists, screens, and nets. Journal of the American Academy of Child & Adolescent Psychiatry, 27(6), 726–737. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Copeland W, & Angold A (2011). Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadds MR, Barrett PM, Rapee RM, & Ryan S (1996). Family process and child anxiety and aggression: An observational analysis. Journal of Abnormal Child Psychology, 24(6), 715–734. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI (2012). The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nat Rev Neurosci, 13(6), 421–434. [DOI] [PubMed] [Google Scholar]
- Fales CL, Barch DM, Rundle MM, Mintun MA, Snyder AZ, Cohen JD, … Sheline YI (2008). Altered Emotional Interference Processing in Affective and Cognitive-Control Brain Circuitry in Major Depression. Biological Psychiatry, 63(4), 377–384. doi: 10.1016/j.biopsych.2007.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisak B, & Grills-Taquechel AE (2007). Parental modeling, reinforcement, and information transfer: Risk factors in the development of child anxiety? Clinical child and family psychology review, 10(3), 213–231. [DOI] [PubMed] [Google Scholar]
- Fliek L, Roelofs J, van Breukelen G, & Muris P (2019). A Longitudinal Study on the Relations Among Fear-Enhancing Parenting, Cognitive Biases, and Anxiety Symptoms in Non-clinical Children. Child Psychiatry & Human Development, 50(4), 631–646. doi: 10.1007/s10578-019-00868-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, McRae K, Ramel W, & Gross JJ (2008). The Neural Bases of Emotion Regulation: Reappraisal and Suppression of Negative Emotion. Biological Psychiatry, 63(6), 577–586. doi: 10.1016/j.biopsych.2007.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, & Hooven C (1996). Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology, 10(3), 243–268. doi: 10.1037/0893-3200.10.3.243 [DOI] [Google Scholar]
- Guyer AE, Jarcho JM, Pérez-Edgar K, Degnan KA, Pine DS, Fox NA, & Nelson EE (2015). Temperament and Parenting Styles in Early Childhood Differentially Influence Neural Response to Peer Evaluation in Adolescence. Journal of Abnormal Child Psychology, 43(5), 863–874. doi: 10.1007/s10802-015-9973-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer AE, Lau JF, McClure-Tone EB, & et al. (2008). Amygdala and ventrolateral prefrontal cortex function during anticipated peer evaluation in pediatric social anxiety. Archives of General Psychiatry, 65(11), 1303–1312. doi: 10.1001/archpsyc.65.11.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JP, Farmer M, Fogelman P, & Gotlib IH (2015). Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biological Psychiatry, 78(4), 224–230. doi: 10.1016/j.biopsych.2015.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2006). Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior, 8(1), 102–114. doi: 10.1016/j.yebeh.2005.10.012 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, & Asnaani A (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and anxiety, 29(5), 409–416. [DOI] [PubMed] [Google Scholar]
- Holtzheimer PE, Kelley ME, Gross RE, Filkowski MM, Garlow SJ, Barrocas A, … Chismar R (2012). Subcallosal cingulate deep brain stimulation for treatment-resistant unipolar and bipolar depression. Archives of General Psychiatry, 69(2), 150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM, Gruber SA, Parker HA, Guillaumot J, Rogowska J, & Yurgelun-Todd DA (2009). Cortico-limbic response to personally challenging emotional stimuli after complete recovery from depression. Psychiatry Research: Neuroimaging, 171(2), 106–119. doi: 10.1016/j.pscychresns.2008.04.001 [DOI] [PubMed] [Google Scholar]
- Hooley JM, Gruber SA, Scott LA, Hiller JB, & Yurgelun-Todd DA (2005). Activation in dorsolateral prefrontal cortex in response to maternal criticism and praise in recovered depressed and healthy control participants. Biological Psychiatry, 57(7), 809–812. doi: 10.1016/j.biopsych.2005.01.012 [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao UMA, Flynn C, Moreci P, … Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 980–988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, & Webb A (2004). Child Anxiety Treatment: Outcomes in Adolescence and Impact on Substance Use and Depression at 7.4-Year Follow-Up. Journal of Consulting and Clinical Psychology, 72(2), 276–287. doi: 10.1037/0022-006X.72.2.276 [DOI] [PubMed] [Google Scholar]
- Laursen B, & Collins A (2009). Parent-Child Relationships During Adolescence Handbook of Adolescent Psychology. [Google Scholar]
- Lee KH, Siegle GJ, Dahl RE, Hooley JM, & Silk JS (2014). Neural responses to maternal criticism in healthy youth. Social Cognitive and Affective Neuroscience. doi: 10.1093/scan/nsu133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lévesque J, Eugène F, Joanette Y, Paquette V, Mensour B, Beaudoin G, … Beauregard M (2003). Neural circuitry underlying voluntary suppression of sadness. Biological Psychiatry, 53(6), 502–510. doi: 10.1016/S0006-3223(02)01817-6 [DOI] [PubMed] [Google Scholar]
- Lévesque J, Joanette Y, Mensour B, Beaudoin G, Leroux JM, Bourgouin P, & Beauregard M (2004). Neural basis of emotional self-regulation in childhood. Neuroscience, 129(2), 361–369. doi: 10.1016/j.neuroscience.2004.07.032 [DOI] [PubMed] [Google Scholar]
- Masten CL, Eisenberger NI, Borofsky LA, McNealy K, Pfeifer JH, & Dapretto M (2011). Subgenual anterior cingulate responses to peer rejection: A marker of adolescents’ risk for depression. Development and Psychopathology, 23(1), 283–292. doi: 10.1017/S0954579410000799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, Jerabek PA, … Fox PT (1999). Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. The American Journal of Psychiatry, 156(5), 675–682. [DOI] [PubMed] [Google Scholar]
- Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, … Kennedy SH (2005). Deep brain stimulation for treatment-resistant depression. Neuron, 45(5), 651–660. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The Role of the Family Context in the Development of Emotion Regulation. Social Development, 16(2), 361–388. doi: 10.1111/j.1467-9507.2007.00389.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J, Frith CD, Perrett DI, Rowland D, Young AW, Calder AJ, & Dolan RJ (1996). A differential neural response in the human amygdala to fearful and happy facial expressions. Nature, 383(6603), 812–815. doi: 10.1038/383812a0 [DOI] [PubMed] [Google Scholar]
- Nelson EE, & Guyer AE (2011). The development of the ventral prefrontal cortex and social flexibility. Developmental Cognitive Neuroscience, 1(3), 233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EE, Leibenluft E, McClure E, & Pine DS (2005). The social re-orientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychological Medicine, 35(02), 163–174. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, & Gross JJ (2005). The cognitive control of emotion. Trends in cognitive sciences, 9(5), 242–249. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, & Gross JJ (2008). Cognitive emotion regulation insights from social cognitive and affective neuroscience. Current Directions in Psychological Science, 17(2), 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, & Grills AE (2016). Perceived control, family environment, and the etiology of child anxiety—revisited. Behavior Therapy, 47(5), 633–642. [DOI] [PubMed] [Google Scholar]
- Parker JG, Rubin KH, Erath SA, Wojslawowicz JC, & Buskirk AA (2006). Peer relationships, child development, and adjustment: A developmental psychopathology perspective Developmental psychopathology: Theory and methods (Cicchetti D and Cohen DJ, eds) Wiley, 1, 96–161. [Google Scholar]
- Phan KL, Wager T, Taylor SF, & Liberzon I (2002). Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI (Vol. 16, pp. 331–331). United States: Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- Phillips ML, Drevets WC, Rauch SL, & Lane R (2003). Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biological Psychiatry, 54(5), 504–514. doi: 10.1016/S0006-3223(03)00168-9 [DOI] [PubMed] [Google Scholar]
- Phillips ML, Ladouceur CD, & Drevets WC (2008). A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Molecular Psychiatry, 13(9), 833–857. doi: 10.1038/mp.2008.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Paul B, Schneider W, & Siegle GJ (2013). Neural Correlates of Three Neurocognitive Intervention Strategies: A Preliminary Step Towards Personalized Treatment for Psychological Disorders. Cognitive Therapy and Research, 37(4), 657–672. doi: 10.1007/s10608-012-9508-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin JL, Lane DJ, Gibbons FX, & Gerrard M (2004). Adolescent Self‐Consciousness: Longitudinal Age Changes and Gender Differences in Two Cohorts. Journal of Research on Adolescence, 14(1), 1–21. doi: 10.1111/j.1532-7795.2004.01401001.x [DOI] [Google Scholar]
- Rohner RP (2004). The Parental “Acceptance-Rejection Syndrome”: Universal Correlates of Perceived Rejection. American Psychologist, 59(8), 830–840. doi: 10.1037/0003-066X.59.8.830 [DOI] [PubMed] [Google Scholar]
- Romund L, Raufelder D, Flemming E, Lorenz RC, Pelz P, Gleich T, … Beck A (2016). Maternal parenting behavior and emotion processing in adolescents—An fMRI study. Biological psychology, 120, 120–125. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, & Hammen C (1999). Age and Gender as Determinants of Stress Exposure, Generation, and Reactions in Youngsters: A Transactional Perspective. Child Development, 70(3), 660–677. doi: 10.1111/1467-8624.00048 [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Miernicki ME, Troop-Gordon W, Davis MM, & Telzer EH (2016). Adding insult to injury: neural sensitivity to social exclusion is associated with internalizing symptoms in chronically peer-victimized girls. Social Cognitive and Affective Neuroscience, 11(5), 829–842. doi: 10.1093/scan/nsw021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer ES (1965). Children’s Reports of Parental Behavior: An Inventory. Child Development, 36(2), 413–424. doi: 10.2307/1126465 [DOI] [PubMed] [Google Scholar]
- Schludermann E, & Schludermann S (1970). Replicability of factors in children’s report of parent behavior (CRPBI). The Journal of Psychology, 76(2), 239–249. [Google Scholar]
- Schwartz OS, Byrne ML, Simmons JG, Whittle S, Dudgeon P, Yap MB, … Allen NB (2014). Parenting during early adolescence and adolescent-onset major depression: A 6-year prospective longitudinal study. Clinical Psychological Science, 2(3), 272–286. [Google Scholar]
- Schwartz OS, Simmons JG, Whittle S, Byrne ML, Yap MB, Sheeber LB, & Allen NB (2017). Affective parenting behaviors, adolescent depression, and brain development: A review of findings from the Orygen Adolescent Development Study. Child Development Perspectives, 11(2), 90–96. [Google Scholar]
- Sequeira SL, Butterfield RD, Silk JS, Forbes EE, & Ladouceur CD (2019). Neural Activation to Parental Praise Interacts with Social Context to Predict Adolescent Depressive Symptoms. Frontiers in Behavioral Neuroscience, 13, 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Davis S, McMakin DL, Dahl RE, & Forbes EE (2012). Why do anxious children become depressed teenagers? The role of social evaluative threat and reward processing. Psychological Medicine, 42(10), 2095–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Lee KH, Elliott RD, Hooley JM, Dahl RE, Barber A, & Siegle GJ (2017). ‘Mom—I don’t want to hear it’: Brain response to maternal praise and criticism in adolescents with major depressive disorder. Social Cognitive and Affective Neuroscience, 12(5), 729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Price RB, Rosen D, Ryan ND, Forbes EE, Siegle GJ, … Ladouceur CD (2019). A longitudinal follow-up study examining adolescent depressive symptoms as a function of prior anxiety treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 58(3), 359–367. [DOI] [PubMed] [Google Scholar]
- Silk JS, Sheeber L, Tan PZ, Ladouceur CD, Forbes EE, McMakin DL, … Ryan ND (2013). “You can do it!”: The role of parental encouragement of bravery in child anxiety treatment. Journal of anxiety disorders, 27(5), 439–446. doi: 10.1016/j.janxdis.2013.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Siegle GJ, Lee KH, Nelson EE, Stroud LR, & Dahl RE (2014). Increased neural response to peer rejection associated with adolescent depression and pubertal development. Social Cognitive and Affective Neuroscience, nst175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Tan PZ, Ladouceur CD, Meller S, Siegle GJ, McMakin DL, … Mannarino A (2016). A randomized clinical trial comparing individual cognitive behavioral therapy and child-centered therapy for child anxiety disorders. Journal of Clinical Child & Adolescent Psychology, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, Insel C, Powers A, Franz P, Helion C, Martin RE, … Ochsner KN (2016). vlPFC–vmPFC–amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cerebral Cortex, 27(7), 3502–3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson JR, Drevets WC, Snyder AZ, Gusnard DA, & Raichle ME (2001). Emotion-induced changes in human medial prefrontal cortex: II. During anticipatory anxiety. Proceedings of the National Academy of Sciences, 98(2), 688–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sontag LM, Graber JA, & Clemans KH (2011). The Role of Peer Stress and Pubertal Timing on Symptoms of Psychopathology During Early Adolescence. Journal of youth and adolescence, 40(10), 1371–1382. doi: 10.1007/s10964-010-9620-8 [DOI] [PubMed] [Google Scholar]
- Strawn JR, Dominick KC, Patino LR, Doyle CD, Picard LS, & Phan KL (2014). Neurobiology of Pediatric Anxiety Disorders. Current behavioral neuroscience reports, 1(3), 154–160. doi: 10.1007/s40473-014-0014-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan PZ, Oppenheimer CW, Ladouceur CD, Butterfield R, & Silk JS (In Press). A Review of Associations between Parental Emotion Socialization and Brain Correlates of Emotional Reactivity and Regulation in Youth. Developmental Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valiente C, Lemery‐Chalfant K, & Swanson J (2009). Children’s responses to daily social stressors: Relations with parenting, children’s effortful control, and adjustment. Journal of Child Psychology and Psychiatry, 50(6), 707–717. [DOI] [PubMed] [Google Scholar]
- Yang TT, Simmons AN, Matthews SC, Tapert SF, Frank GK, Bischoff-Grethe A, … Paulus MP (2009). Depressed adolescents demonstrate greater subgenual anterior cingulate activity. Neuroreport, 20(4), 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap MBH, Allen NB, & Ladouceur CD (2008). Maternal Socialization of Positive Affect: The Impact of Invalidation on Adolescent Emotion Regulation and Depressive Symptomatology. Child Development, 79(5), 1415–1431. doi: 10.1111/j.1467-8624.2008.01196.x [DOI] [PubMed] [Google Scholar]
- Yap MBH, Allen NB, & Sheeber L (2007). Using an Emotion Regulation Framework to Understand the Role of Temperament and Family Processes in Risk for Adolescent Depressive Disorders. Clinical child and family psychology review, 10(2), 180–196. doi: 10.1007/s10567-006-0014-0 [DOI] [PubMed] [Google Scholar]
- Yap MBH, & Jorm AF (2015). Parental factors associated with childhood anxiety, depression, and internalizing problems: A systematic review and meta-analysis. Journal of affective disorders, 175(0), 424–440. doi: 10.1016/j.jad.2015.01.050 [DOI] [PubMed] [Google Scholar]
- Yap MBH, Pilkington PD, Ryan SM, & Jorm AF (2014). Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of affective disorders, 156, 8–23. doi: 10.1016/j.jad.2013.11.007 [DOI] [PubMed] [Google Scholar]
- Yap MBH, Schwartz OS, Byrne ML, Simmons JG, & Allen NB (2010). Maternal Positive and Negative Interaction Behaviors and Early Adolescents’ Depressive Symptoms: Adolescent Emotion Regulation as a Mediator. Journal of Research on Adolescence, 20(4), 1014–1043. doi: 10.1111/j.1532-7795.2010.00665.x [DOI] [Google Scholar]