Abstract
The Cigarette Purchase Task (CPT), in which participants estimate the number of cigarettes they would smoke across increasing cigarette prices, measures the relative reinforcing value of cigarettes. Although opioid-dependent individuals are particularly vulnerable to tobacco addiction, more research is needed to elucidate whether and to what extent their motivation to smoke differs from not-opioid-dependent smokers controlling for potential sociodemographic differences. Participants were 173 women (65 opioid-dependent) in an ongoing clinical trial for smoking cessation. Baseline CPT responses were compared between opioid-dependent and not-opioid-dependent women using five demand indices: Demand Intensity; Omax; Pmax; Breakpoint (BP); and α, and two latent factors: Amplitude and Persistence. Final regression models adjusted for sociodemographic characteristics differing between the two groups. Opioid-dependent women had greater Demand Intensity (i.e. number of cigarettes they would smoke if they were free) than not-opioid dependent women in the adjusted model (F (1, 156) = 6.93, p = .016). No other demand indices differed significantly. Regarding latent factors, demand Amplitude (i.e., volumetric consumption), but not Persistence (i.e., price insensitivity), was greater for opioid-dependent women in the adjusted model (F (1, 146) = 4.04, p = .046). These results further demonstrate that the CPT is a highly sensitive task that can illuminate potentially important individual and population differences in the relative reinforcing value of smoking. Greater Demand Intensity and Amplitude differentiated smokers with comorbid opioid dependence; thus, decreasing smoking prevalence among opioid-dependent populations may require policies and interventions that can decrease cigarette Demand Intensity and Amplitude.
Keywords: Cigarette Purchase Task, Smoking, Opioid dependence, Women of Reproductive Age
Introduction
Behavioral economics integrates the principles of psychology and micro-economics and has been applied effectively in studying substance abuse including cigarette smoking (Bickel et al., 2014; Vuchinich & Heather, 2003). The Cigarette Purchase Task (CPT) is a behavioral economic simulation model in which participants estimate the number of cigarettes that they would smoke across an increasing range of hypothetical monetary prices (Jacobs & Bickel, 1999). The CPT is an alternative to time- and labor-intensive laboratory drug self-administration studies (Bickel & Madden, 1999a, 1999b), and a valid method of studying cigarette demand (Farris et al., 2017; Madden & Kalman, 2010). The CPT produces demand curves that correspond closely to those involving actual drug consumption (Amlung, Stojek, Murphy, & MacKillop, 2012; Wilson, Franck, Koffarnus, & Bickel, 2016). CPT demand is typically characterized by five indices: Demand Intensity (i.e., number of cigarettes participants estimate smoking per day if cigarettes were free or very low cost); Omax (i.e., peak expenditure, or the total amount of money participants would spend daily on smoking); Pmax (i.e., the financial price associated with Omax); Breakpoint (BP; i.e., the price at which participants indicate they would quit smoking rather than incur the cost); and α (i.e., overall sensitivity to changes in price, which is calculated as rate of change in elasticity across the demand curve).
The CPT has been useful in discerning individual differences in demand for cigarettes among various subpopulations (see Zvorsky et al., 2019, for a review), including those particularly vulnerable to tobacco addiction and its adverse health impacts, including those with serious mental illness (MacKillop & Tidey, 2009) and pregnant women (Higgins et al., 2017a; Nighbor et al., 2019). One population particularly vulnerable to cigarette smoking is those with comorbid opioid dependence. Prevalence of smoking among adults with opioid dependence is six-fold greater than the U.S. adult population (84-94% vs. 15%, respectively; Jamal et al., 2016) and in the context of the current opioid epidemic, these individuals constitute a larger proportion of the smoking population.
In an experimental examination of the effects of a national US regulatory policy to reduce the nicotine content in cigarettes and its effects on the relative reinforcing value of cigarettes among vulnerable populations, Higgins et al. (2017b) reported that Demand Intensity for research cigarettes was significantly higher among those with opioid dependence compared to two other vulnerable populations studied (i.e., smokers with affective disorders and women of low socioeconomic status). To our knowledge, Higgins et al. (2017b) is the only report documenting the ability of the CPT to reveal differences between opioid-dependent compared to not-opioid-dependent smokers, and, to our knowledge, no comparison exists between opioid-dependent and not-opioid-dependent smokers with respect to their usual-brand cigarettes. Thus, it is unclear if there are differences in the relative reinforcing efficacy of usual-brand cigarettes among these populations, the baseline upon which a reduced-nicotine policy would be implemented. Furthermore, several potential differences in sociodemographics (e.g., education, income) and smoking characteristics (e.g., cigarettes per day, nicotine dependence) not controlled for in Higgins et al (2017b) may have contributed to the differences observed between those with versus without opioid dependence, which is the primary rationale for the present study. An additional aim is to compare CPT latent factors among opioid-dependent versus not-opioid-dependent smokers. Correlations among the CPT demand metrics suggest the five indices can be more parsimoniously represented by a smaller number of factors (Jacobs & Bickel, 1999b; MacKillop et al., 2008; Murphy & MacKillop, 2006; Murphy et al., 2011). Indeed, recent CPT research shows that nicotine reinforcement may be better characterized by a bifactorial latent structure: Amplitude, or volumetric consumption, consisting of Demand Intensity and often Omax; and Persistence, or insensitivity of demand to increasing cigarette prices, often consisting of Omax, Pmax, BP, and α (Bidwell et al., 2012; Gonzalez-Roz et al., 2018; O’Connor et al., 2016).
Methods
Participants
Study participants were 173 women who were biochemically confirmed to be smoking upon intake and enrolled in an ongoing randomized controlled clinical trial on smoking cessation among mothers of young children. Of these women, 65 were deemed as opioid-dependent and 108 as not-opioid dependent. Trial inclusion criteria included: (a) mother was at least 18 years of age, (b) mother had a child < 12 years of age residing with her full time, (c) self-reported smoking ≥10 CPD in the past week that was biochemically verified, (d) interest in quitting and willingness to initiate but not currently using Nicotine Replacement Therapy (NRT), (e) plans to remain in the geographical area for the next 12 months, and (f) English-speaking. Exclusion criteria were: (a) current incarceration, (b) meeting DSM-IV criteria for alcohol or drug dependence other than nicotine or opioids in the past 12 months, (c) current/past psychotic disorder, or being suicidal, and (d) currently pregnant, breastfeeding, or planning to become pregnant in the next 12 months. Those in the opioid-dependent group also needed to report enrollment in medication-assisted treatment and test positive for an opioid-maintenance medication (e.g., Buprenorphine, Methadone), but not illicit opioids. Participants were recruited from Federal Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) offices and pediatric clinics located in the Burlington, Vermont area. The University of Vermont Institutional Review Board approved all study procedures and all participants provided written informed consent.
Assessments
All participants completed questionnaires examining sociodemographics, smoking history, smoking environment and motivations (e.g., the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991), Minnesota Tobacco Withdrawal Scale (MTWS; Hughes & Hatsukami, 1986), and intentions to quit smoking. Participants also completed the CPT assessment (described below). Abbreviated versions of the intake assessment were repeated at subsequent follow-up assessments, but the present study is focused exclusively on information collected at the study intake assessment.
Cigarette Purchase Task
As noted above, the CPT assesses the number of cigarettes that participants estimate they would smoke across an increasing range of hypothetical monetary prices. The version of CPT used in the current study was adapted from MacKillop et al. (2008). Participants were provided with the following oral instructions about how to complete the task: “Think about how you are feeling right now. The following questions ask how many cigarettes you would smoke if they cost various amounts of money. Assume that: (1) The available cigarettes are your usual brand. (2) You have the same income/savings that you have now and no access to any cigarettes or nicotine products other than those offered at these prices. (3) You would smoke the cigarettes that you request within 24 hours. You cannot save or stockpile cigarettes for a later date. (4) You can smoke without any restrictions and without factoring in what might occur in the next 24 hours related to your participation in the study.” The task included 19 prices/cigarette: $0.00 (free), $0.02, $0.05, $0.10, $0.20, $0.30, $0.40, $0.50, $0.60, $0.70, $0.80, $0.90, $1.00, $2.00, $3.00, $4.00, $5.00, $10.00, and $20.00, with associated prices per pack presented to the right of the individual cigarette prices. Prices were presented in ascending order. All participants completed a computerized version of CPT on an iPad device.
Demand curves were fit to mean reported CPT consumption at each price across participants separated by opioid-dependence status. In order to derive values for Elasticity (α), individual demand curves were fitted using the Hursh and Silberberg (2008) exponential demand equation, using a freely available GraphPad Prism® template (GraphPad Software, La Jolla California, USA, www.graphpad.com) provided by the Institutes for Behavior Resources (http://www.ibrinc.org):
| (1) |
where Q is consumption at each price (i.e., C), Q0 is consumption when cost is zero (converted to $.01 for curve fitting in log-log space), k is the range of consumption in logarithmic units (calculated as the difference of the logarithms of the maximum and minimum consumption values plus 0.5; k was 2.0 for the current experiment), and α is the rate of change in elasticity across the demand curve. Demand Intensity (Q0) was constrained to the participants’ reported consumption at $0.00 to leave elasticity as the only fitted parameter. All other demand indices were empirically quantified from observed values. Omax, Pmax, BP, and α were log10 transformed to correct for skewness. We examined degree of systematic responding for all CPT datasets using the procedure described by Stein, Koffarnus, Snider, Quisenberry, and Bickel (2015) with the following detection limits for trend (ΔQ), bounce (B), and reversals from zero, respectively: 0.025, 0.10, and 0. Systematic patterns were observed for 99% of demand curves; 2 were excluded from analyses. Values of each index which were above or below 3.29 standard deviations from the mean were considered outliers and were converted to missing. This was done for Elasticity for 11 of 171 cases, for Pmax for 7 of 171 cases, for Omax for 3 of 171 cases, and for Intensity for 3 of 171 cases. Factor analyses were conducted using a principal component analysis (PCA) method of estimation with oblique (oblimin) rotation to permit multifactorial solutions with correlated factors. As some indices typically have negligible associations, principal components analysis was selected to examine the factor structure of the overall correlation matrix, rather just shared variance. A factor loading of ≥ .40 on the pattern matrix was used as the criterion for determining if an item significantly loaded on a given factor (Stevens, 2002; Tabachnick & Fidell, 2001). Because the objective of the study was exploration of the latent structure of the variables, not identifying mutually exclusive factors (e.g., scale construction), facets of demand were permitted to load on multiple factors. Factor scores for each factor were created by summing the standardized scores for individual items, with the standardized scores computed as the factor loading applied to the standardized value of each index. Factors are scored such that the mean = 0.0 and standard deviation = 1.0.
Differences between opioid-dependent and not-opioid-dependent women in CPT indices and factors were examined using an analysis of covariance. The independent variable of interest was the opioid dependence status of the women, with those variables that differed significantly between the two groups included as covariates in all models. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC) and the Non-Systematic Purchase Task Data Identification Tool (Stein et al., 2015). Across all tests, statistical significance was defined as p < .05 (2-tailed).
Results
Participant Characteristics
Table 1 shows participant sociodemographic and smoking characteristics. Opioid-dependent women had less education, lower household incomes, were less likely to be employed outside of the home, less likely to have private health insurance, and had higher overall FTND scores than those not-opioid dependent.
Table 1.
Participant Sociodemographic and Smoking Characteristics
| Opioid-dependent (n=65) | Not-opioid dependent (n=108) | p value | |
|---|---|---|---|
| Sociodemographics | |||
| Age (years) | 33.1 (5.2) | 31.9 (6.8) | .22 |
| Education | .008 | ||
| % < 12 years | 24 (36.9%) | 20 (18.5%) | |
| % 12 years | 21(32.3%) | 32 (29.6%) | |
| % > 12 years | 20(30.8%) | 56 (51.9%) | |
| % Caucasian | 61 (93.9%) | 101 (93.5%) | 0.93 |
| % Married | 9 (13.9%) | 27 (25.0%) | .08 |
| % Employed outside of the home | 20 (30.8%) | 54 (50.5%) | .01 |
| % With private health insurance | 2 (3.1% | 29 (27.1%) | <.001 |
| Income | 22,504 (17,549) | 33,887 (31,522) | .003 |
| Smoking Characteristics | |||
| Cigs/day at intake | 17.4 (5.8) | 16.0 (5.7) | .12 |
| FTND Score | 5.3 (2.0) | 4.6 (2.3) | .04 |
| MNWS Craving | 4.0 (1.1) | 4.1 (.9) | .64 |
| MNWS Total Score | 2.2 (.9) | 2.4 (.9) | .26 |
| Age started smoking (years) | 14.8 (3.5) | 15.7 (3.0) | .08 |
| % Living with other smoker(s) | 35 (53.9%) | 44 (42.7%) | .16 |
| % With no smoking allowed in home | 88 (81.5%) | 48 (73.9%) | .24 |
| % With some or most friends/family who smoke | 24 (36.9%) | 41 (38.0%) | .89 |
| % Attempted to quit prior to intake | 55 (84.6%) | 99 (91.7%) | .15 |
Note: Tabled values represent means and standard deviations, or percents.
Overall Demand Curves and Individual Demand Indices
Opioid-dependent women had greater overall demand for cigarettes than those not-opioid dependent (Z = 2.78, p = .006; Figure 1). With respect to the individual demand indices, opioid-dependent women had greater Demand Intensity than not-opioid-dependent women (F (1, 169) = 9.90, p = .002; Figure 2), even after controlling for differing sociodemographic and smoking characteristics in the final regression model (F (1, 151) = 6.93, p = .016) (Table 2). Although a similar trend was observed for other demand indices, none differed significantly (ps > .05; see Supplemental Tables 5–8).
Figure 1.
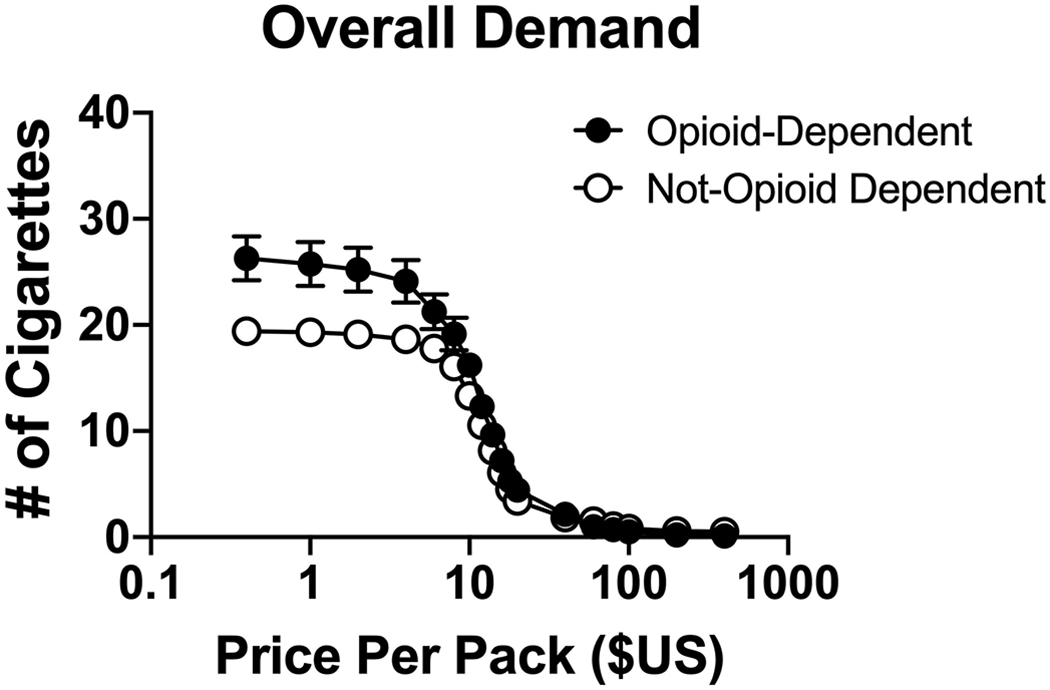
Overall demand curves, seperated by opioid-dependence, from the Cigarette Purchase Task simulating demand for cigarette smoking at escalating prices per pack. Bars represent standard error (Note: Error bars for the not-opioid dependent group are smaller than the symbols).
Figure 2.
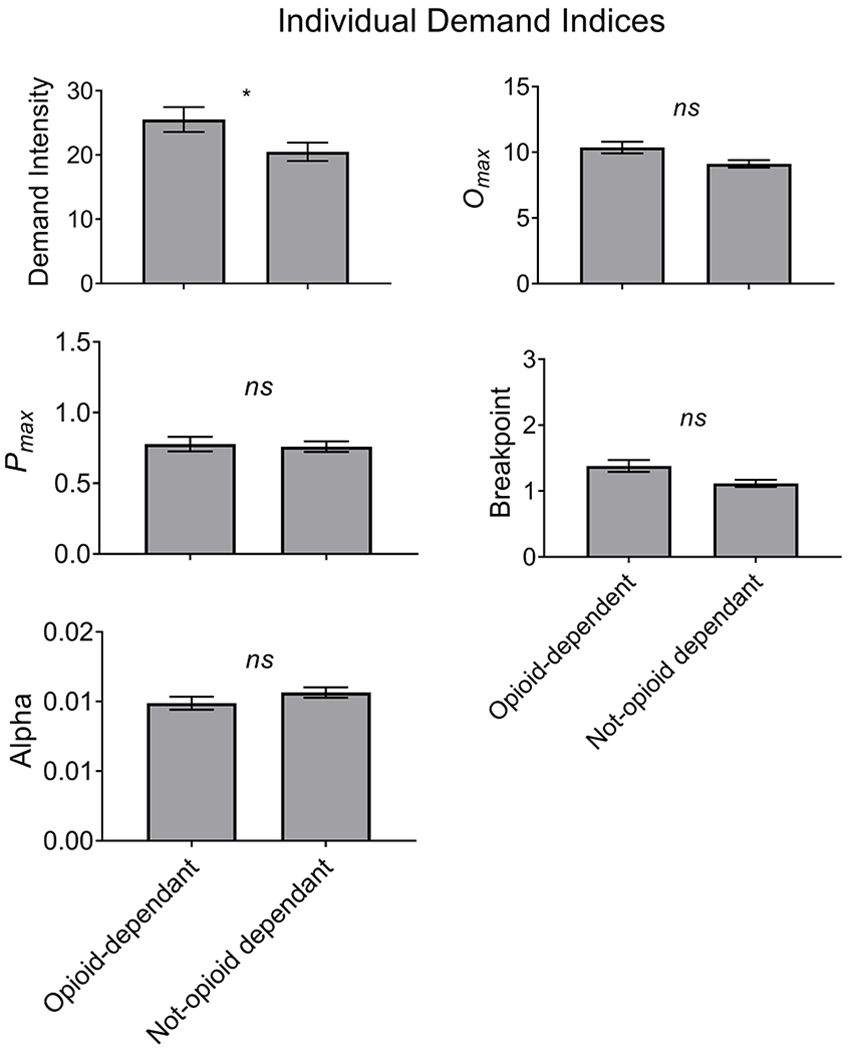
Individual demand indices, seperated by opioid-dependence, from the Cigarette Purchase Task simulating demand for cigarette smoking. Bars represent standard error.
Table 2.
Simple and multiple linear regressions predicting Demand Intensity based on opioid status, and sociodemographic and smoking characteristics that differed based on opioid status.
| Simple Linear Regression | Multiple Linear Regression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | F | df | p | β | SE | F | df | p | |
| Opioid Status | 9.90 | 1, 169 | .002 | 6.93 | 1, 156 | .016 | ||||
| Yes | 6.265 | 1.991 | 5.025 | 2.063 | ||||||
| No | REF | REF | ||||||||
| Education | 0.20 | 2, 168 | .822 | 2.55 | 2, 156 | .081 | ||||
| < 12 years | −1.500 | 2.492 | −5.723 | 2.551 | ||||||
| 12 years | −0.915 | 2.338 | −1.920 | 2.318 | ||||||
| > 12 years | REF | REF | ||||||||
| Work for Pay Outside the Home | 8.69 | 1, 168 | .004 | 2.40 | 1, 156 | .124 | ||||
| Yes | −5.808 | 1.970 | −3.155 | 2.038 | ||||||
| No | REF | REF | ||||||||
| Has Private Health Insurance | 3.07 | 1, 168 | .082 | .02 | 1, 156 | .879 | ||||
| Yes | −4.497 | 2.567 | 0.433 | 2.831 | ||||||
| No | REF | REF | ||||||||
| Income | −0.054 | 0.037 | 2.14 | 1, 163 | .146 | −0.036 | 0.042 | 0.75 | 1, 156 | .387 |
| FTND | 2.354 | 0.419 | 31.51 | 1, 169 | <.001 | 2.138 | 0.439 | 23.76 | 1, 156 | <.001 |
Latent Factor Analysis
Results of the factor analysis supported the two-factor solution, with Demand Intensity and Omax loading onto the demand Amplitude factor and Omax, Pmax, BP, and α loading onto the Persistence factor (Table 3). Opioid-dependent women had greater demand Amplitude (i.e., volumetric consumption) than not-opioid-dependent women (F (1,159) = 6.26, p =0.013), even after controlling for sociodemographic and smoking characteristics that differed at baseline in the final regression model (F (1,155) = 4.04, p = 0.046; Table 4). The two groups did not differ with respect to Persistence (F (1,159) = 0.02, p = 0.880; see Supplemental Table 9).
Table 3.
Factor Loadings
| Factor 1 Amplitude | Factor 2 Persistence | |
|---|---|---|
| Demand Intensity | .94 | −.04 |
| Omax | .42 | .84 |
| Pmax | −.27 | .94 |
| BP | −.21 | .92 |
| α | .33 | .75 |
Note: Loadings of .400 and greater are bolded.
Table 4.
Simple and multiple linear regressions predicting demand Amplitude based on opioid status and sociodemographic and smoking characteristics that differed based on opioid status.
| Simple Linear Regression | Multiple Linear Regression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | F | df | p | β | SE | F | df | p | |
| Opioid Status | 6.26 | 1, 159 | .013 | 4.04 | 1, 146 | .046 | ||||
| Yes | 0.397 | 0.159 | 0.323 | 0.160 | ||||||
| No | REF | REF | ||||||||
| Education | 0.23 | 2, 158 | .797 | 2.67 | 2, 146 | .073 | ||||
| < 12 years | −0.133 | 0.197 | −0.438 | 0.197 | ||||||
| 12 years | −0.056 | 0.187 | −0.083 | 0.180 | ||||||
| > 12 years | REF | REF | ||||||||
| Work for Pay Outside the Home | 7.56 | 1, 158 | .007 | 1.79 | 1, 146 | .183 | ||||
| Yes | −0.431 | 0.157 | −0.211 | 0.158 | ||||||
| No | REF | REF | ||||||||
| Has Private Health Insurance | 2.26 | 1, 158 | .135 | 0.01 | 1, 146 | .908 | ||||
| Yes | −0.308 | 0.205 | 0.025 | 0.220 | ||||||
| No | REF | REF | ||||||||
| Income | −0.004 | 0.003 | 1.73 | 1, 153 | .191 | −0.002 | 0.003 | 0.43 | 1, 146 | .511 |
| FTND | 0.206 | 0.033 | 38.89 | 1, 159 | <.001 | 0.195 | 0.035 | 31.93 | 1, 146 | < .001 |
Discussion
To our knowledge, this is first report on using the CPT to characterize demand for usual-brand cigarettes among an opioid-dependent population. Given the strikingly high prevalence of smoking and related adverse health impacts in the opioid-dependent population, a great deal more needs to be learned about the variables that control their smoking. The current results further demonstrate the utility of CPT in such efforts. The CPT is highly sensitive to detecting differences in the relative reinforcing efficacy of cigarettes (Zvorsky et al., 2019). In particular, Demand Intensity, which reflects cigarette consumption at zero or very low price, and Amplitude, a latent factor that encompasses Demand Intensity and Omax and reflects maximum overall cigarette consumption, appear to be especially sensitive to these differences. In the present study demand Amplitude was higher among opioid-dependent women, and those differences remained significant even after controlling for baseline sociodemographics (e.g., education; income) and smoking characteristics (i.e., the FTND). The current results systematically replicate those previously reported by Higgins et al. (2017b) that opioid-dependent smokers have greater Demand Intensity for cigarettes and are novel in that they extend this previous observation to participant usual-brand cigarettes and to the demand Amplitude latent factor.
In a recent meta-analysis, Zvorsky et al. (2019) reported that Demand Intensity and Omax exhibited the greatest sensitivity to discerning individual differences in demand for various substances (e.g., cigarettes, alcohol, marijuana), which included differences in substance-related correlates (e.g., dependence severity), population differences (e.g., heavy versus light users, those with and without comorbid mental illness) and outcomes (e.g., drunk driving). The use of latent factors is still relatively new in the CPT literature and thus there were too few articles to examine their sensitivity in that meta-analysis. Consistent with the findings of Zvorsky et al. on CPT indices, the current results further underscore the ability of demand Intensity to differentiate between populations with respect to the relative reinforcing value of cigarettes. Additionally, the current results extend the Zvorsky et al findings by demonstrating that demand Amplitude is also quite sensitive to population differences in the relative reinforcing effects of cigarettes in this case differentiating between women with versus without opioid dependence. As described above, demand Intensity is a primary component of Amplitude, and although the Omax index also loaded onto the latent factor of Amplitude in the present study, the current results indicate that differences in Amplitude were primarily driven by demand Intensity.
An important finding of the current study is that the observed differences in demand Intensity and Amplitude remained significant after controlling for nicotine dependence. In line with previous research (e.g., Breslau &Johnson, 2000; Parker, Streck, & Sigmon, 2018), the current study demonstrated that opioid-dependent smokers had greater FTND scores than those not-opioid-dependent smokers. As these CPT differences remained significant in the final models after accounting for FTND scores, this finding contributes to the emerging evidence that the CPT provides information unique to the reinforcing effects of cigarettes that is not captured by other conventional behavioral measures of reinforcer value or dependence (see Higgins et al., 2017b; Higgins et al., 2018; Zvorsky et al., 2019). Relatedly, cigarettes per day did not differ significantly between the two groups, thus highlighting the importance of financial constraint (or in the case of Demand Intensity, the lack thereof) in contributing to these between population differences.
Given that smoking rates among women have decreased at a slower rate than among men, and have even increased among socioeconomically disadvantaged women where smoking prevalence can be as high as 40% (Cepeda-Benito et al., 2018; Chilcoat, 2009; Higgins & Chilcoat, 2009), the current results highlight the importance of reducing demand Intensity and Amplitude among socioeconomically disadvantaged women who are smokers. The current results highlight that this is especially important among women with comorbid opioid dependence. With respect to tobacco control, there is accumulating evidence demand Intensity is significantly related to clinically relevant outcomes (e.g., nicotine dependence; quitting smoking; see González-Roz et al., 2019; Zvorsky et al., 2019, for review), although more research is surely needed on this topic. With respect to regulatory science, the Consortium on Methods Evaluating Tobacco explicitly recommends the use of behavioral economic demand approaches, including purchase tasks, to inform US FDA regulations (Berman et al., 2018), and the Tobacco Centers of Regulatory Science use these approaches to guide their policy-informing research (Perry et al., 2019). In light of the current results, it appears reducing the strikingly high smoking prevalence among the opioid-dependent population, which is six-fold that of the U.S. adult population (Jamal et al., 2016), may require policies that aim to decrease Demand Intensity and Amplitude more generally. Experimental evidence indicates that reducing the nicotine content of cigarettes reduces Demand Intensity among populations especially vulnerable to smoking and dependence, including individuals with comorbid opioid dependence (Higgins et al., 2017b). Still, further research is needed in this area.
Several limitations to the current investigation merit mention. First, the study sample was a convenience sample selected from an ongoing clinical trial made up of economically disadvantaged individuals, all of whom were women and most of whom were Caucasian. Thus, this sample was not nationally representative and therefore results may not generalize to other participants with differing sociodemographic or smoking characteristics. Second, results were based on self-reported demand, which may vary from actual consumption., although hypothetical demand has been found to correspond closely to demand involving actual consumption (Amlung et al., 2012; Wilson et al., 2016). These limitations non-withstanding, the current results further demonstrate the utility of the CPT for uncovering detailed differences in the relative reinforcing effects of cigarette smoking among opioid-dependent individuals, and the important role that demand Intensity or Amplitude play in such differences. Greater understanding of CPT Demand Intensity and Amplitude and associated underpinning processes has the potential to improve tobacco control and regulatory efforts to help reduce cigarette smoking.
Supplementary Material
Figure 3.
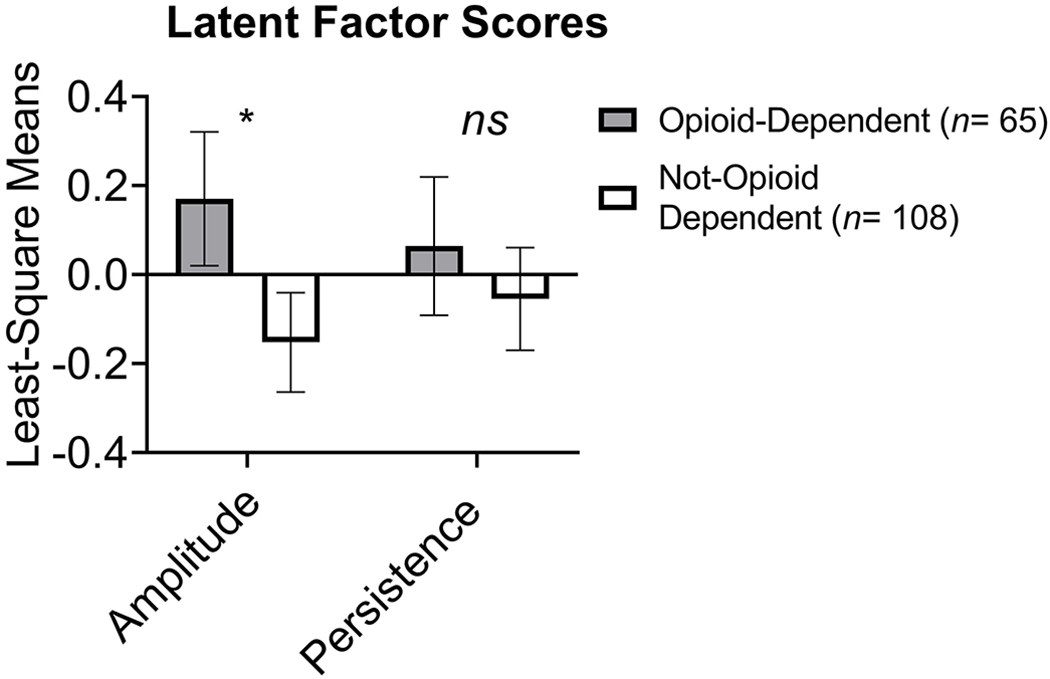
Latent factors scores, seperated by opioid-dependence, from the Cigarette Purchase Task simulating demand for cigarette smoking. Bars represent standard error.
Statement of Public Significance:
The current study demonstrates the independent utility of the Cigarette Purchase Task for uncovering underlying differences in the rewarding effects of cigarettes among opioid-dependent populations from those without comorbid opioid dependence. These findings have the potential to better inform tobacco control and regulatory strategies to help reduce the strikingly high smoking prevalence among the opioid-dependent population.
Acknowledgments
Funding: This project was supported in part by Research award R01HD075669 from the National Institute of Child Health and Human Development (NICHD), Tobacco Centers of Regulatory Science (TCORS) award U54DA036114 from the National Institute on Drug Abuse (NIDA) and Food and Drug Administration (FDA), Institutional Training Grant award T32DA07242 from NIDA, Centers of Biomedical Research Excellence P20GM103644 award from the National Institute on General Medical Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration. The funding sources had no other involvement other than financial support.
Footnotes
Author Note: Portions of this manuscript have been presented at the 2019 Tobacco Regulatory Science Conference in Bethesda, MD and the 2019 Vermont Center on Behavior & Health Annual Conference in Burlington, VT.
Conflicts of interest: None to declare.
References
- Amlung MT, Acker J, Stojek MK, Murphy JG, & MacKillop J (2012). Is talk “cheap”? An initial investigation of the equivalence of the alcohol purchase task performance for hypothetical and actual rewards. Alcoholism, Clinical and Experimental Research, 36, 716–724. 10.1111/j.1530-0277.2011.01656.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677. 10.1146/annurev-clinpsy-032813-153724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman ML, Bickel WK, Harris AC, LeSage MG, O’Connor RJ, Stepanov I, …Hatsukami DK (2018). Consortium on Methods Evaluating Tobacco: Research tools to inform US Food and Drug Administration regulation of snus. Nicotine & Tobacco Research, 20, 1292–1300. doi: 10.1093/ntr/ntx228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, & Madden GJ (1999a). Similar consumption and responding across single and multiple sources of a drug. Journal of the Experimental Analysis of Behavior, 72, 299–316. 10.1901/jeab.1999.72-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, & Madden GJ (1999b). A comparison of measures of relative reinforcing efficacy and behavioral economics: Cigarettes and money in smokers. Behavioural Pharmacology, 10(6–7), 627–637. 10.1097/00008877-199911000-00009 [DOI] [PubMed] [Google Scholar]
- Bidwell LC, MacKillop J, Murphy JG, Tidey JW, & Colby SM (2012). Latent factor structure of a behavioral economic cigarette demand curve in adolescent smokers. Addictive Behaviors, 37(11), 1257–1263. doi: 10.1016/j.addbeh.2012.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda-Benito A, Doogan N, Redner R, Roberts M, Kurti A, Villanti A, … Higgins S (2018). Trend differences in men and women in rural and urban U.S. settings. Preventive Medicine, 117, 69–75. doi: 10.1016/j.ypmed.2018.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat H (2009). An overview of the emergence of disparities in smoking prevalence, cessation, and adverse consequences among women. Drug and Alcohol Dependence, 104(1), S17–S23. doi: 10.1016/j.drugalcdep.2009.06.002 [DOI] [PubMed] [Google Scholar]
- Farris SG, Aston ER, Abrantes AM, & Zvolensky MJ (2017). Tobacco demand, delay discounting, and smoking topography among smokers with and without psychopathology. Drug and Alcohol Dependence, 179, 247–253. 10.1016/j.drugalcdep.2017.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Roz A, Jackson J, Murphy C, Rohsenow DJ, & MacKillop J (2019). Behavioral economic tobacco demand in relation to cigarette consumption and nicotine dependence: A meta-analysis of cross-sectional relationships. Addiction, doi: 10.1111/add.14736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Roz A, Secades-Villa R, Weidberg S, Garcia-Perez A, & Reed DD (2018). Latent structure of the CPT among treatment-seeking smokers with depression and its predictive validity on smoking abstinence. Nicotine Tob Res. doi: 10.1093/ntr/nty236 [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, & Fagerstrom KO (1991). The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict, 86(9), 1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- Higgins ST, & Chilcoat HD (2009). Women and smoking: an interdisciplinary examination of socioeconomic influences. Drug and Alcohol Dependence, 104 Suppl 1(Suppl 1), S1–S5. doi: 10.1016/j.drugalcdep.2009.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Reed DD, Redner R, Skelly JM, Zvorsky IA, & Kurti AN (2017b). Simulating demand for cigarettes among pregnant women: A Low-Risk method for studying vulnerable populations. Journal of the Experimental Analysis of Behavior, 107(1), 176–190. doi: 10.1002/jeab.232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Sigmon SC, Tidey JW, Gaalema DE, Hughes JR, Stizer ML, Durand H, Bunn JY, Priest JS, Arger CA, Miller ME, Bergeria CL, Davis DR, Streck JM, Reed DD, Skelly JM, & Tursi L (2017b). Addiction potential of cigarettes with reduced nicotine content in populations with psychiatric disorders and other vulnerabilities to tobacco addiction JAMA Psychiatry, 74(10), 1056–1064. doi: 10.1001/jamapsychiatry.2017.2355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Bergeria CL, Davis DR, Streck JM, Villanti AC, Hughes JR, Sigmon SC, Tidey JW, Heil SH, Gaalema DE, Stitzer ML, Priest JS, Skelly JM, Reed DD, Bunn JY, Tromblee MA, Arger CA, & Miller ME (2018). Response to reduced nicotine content cigarettes among smokers differing in tobacco dependence severity. Preventive Medicine, 117, 15–23. doi: 10.1016/j.ypmed.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, & Hatsukami D (1986). Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry, 43(3), 289. doi: 10.1001/archpsyc.1986.01800030107013 [DOI] [PubMed] [Google Scholar]
- Jacobs E, & Bickel W (1999). Modeling drug consumption in the clinic using simulation procedures: Demand for heroin and cigarettes in opioid-dependent outpatients. Experimental and Clinical Psychopharmacology, 7, 412–426. 10.1037//1064-1297.7.4.412 [DOI] [PubMed] [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, & Graffunder CM (2016). Current Cigarette Smoking Among Adults — United States, 2005–2015. Morbidity and Mortality Weekly Report, 65(44), 1205–1211. doi: 10.15585/mmwr.mm6544a2 [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DT, Lisman SA, Lum JK, & Wilson DS (2008). Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol, 16(1), 57–65. doi: 10.1037/1064-1297.16.1.57 [DOI] [PubMed] [Google Scholar]
- MacKillop J, & Tidey JW (2011). Cigarette demand and delayed reward discounting in nicotine-dependent individuals with schizophrenia and controls: An initial study. Psychopharmacology, 216, 91–99. 10.1007/s00213-011-2185-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, & Kalman D (2010). Effects of bupropion on simulated demand for cigarettes and the subjective effects of smoking. Nicotine & Tobacco Research, 12, 416–422. 10.1093/ntr/ntq018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, & MacKillop J (2006). Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol, 14(2), 219–227. doi: 10.1037/1064-1297.14.2.219 [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J, Tidey JW, Brazil LA, & Colby SM (2011). Validity of a demand curve measure of nicotine reinforcement with adolescent smokers. Drug Alcohol Depend, 113(2-3), 207–214. doi: 10.1016/j.drugalcdep.2010.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nighbor TD, Zvorsky I, Kurti AN, Skelly JM, Bickel WK, Reed DD, … Higgins ST (2019). Examining interrelationships between the Cigarette Purchase Task and delay discounting among pregnant women. Journal of the Experimental Analysis of Behavior, 111(3), 405–415. doi: 10.1002/jeab.499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Creamer MR, Chaffee BW, Unger JB, Sutfin EL, Kong G, … Pentz M (2019). Research on Youth and Young Adult Tobacco Use, 2013-2018, from the FDA-NIH Tobacco Centers of Regulatory Science. Nicotine & Tobacco Research. doi: 10.1093/ntr/ntz059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RJ, Heckman BW, Adkison SE, Rees VW, Hatsukami DK, Bickel WK, & Cummings KM (2016). Persistence and amplitude of cigarette demand in relation to quit intentions and attempts. Psychopharmacology (Berl), 233(12), 2365–2371. doi : 10.1007/s00213-016-4286-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker MA, Streck JM, & Sigmon SC (2018). Associations between opioid and nicotine dependence in nationally representative samples of United States adult daily smokers. Drug and Alcohol Dependence, 186, 167–170. doi: 10.1016/j.drugalcdep.2018.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roma PG, Reed DD, DiGennaro Reed FD, & Hursh SR (2017). Progress of and Prospects for Hypothetical Purchase Task Questionnaires in Consumer Behavior Analysis and Public Policy. The Behavior Analyst, 40(2), 329–342. doi: 10.1007/s40614-017-0100-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, & Bickel WK (2015). Identification and management of nonsystematic purchase task data: Toward best practice. Experimental and Clinical Psychopharmacology, 23(5), 377–386. doi: 10.1037/pha0000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JP (2002). Applied multivariate statistics for the social sciences. Mahwah, NJ: Lawrence Erblaum. [Google Scholar]
- Tabachnick BG, & Fidell LS (2001). Using multivariate statistics (4th edition). : Allyn & Bacon. [Google Scholar]
- Wilson AG, Franck CT, Koffarnus MN, & Bickel WK (2016). Behavioral economics of cigarette purchase tasks: Within-subject comparison of real, potentially real, and hypothetical cigarettes. Nicotine & Tobacco Research, 18, 524–530. 10.1093/ntr/ntv154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuchinich RE, & Heather N (2003). Choice, behavioural economics and addiction. Amsterdam: Pergamon/ Elsevier Science. [Google Scholar]
- Zvorsky I, Nighbor TD, Kurti AN, DeSarno M, Naudé G, Reed DD, & Higgins ST (2019). Sensitivity of hypothetical purchase task indices when studying substance use: A systematic literature review. Preventive Medicine, 105789. doi: 10.1016/j.ypmed.2019.105789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


