Abstract
Latino emerging adults in the United States are at a high risk of HIV and have a low prevalence of HIV testing. This study examined the association between self-efficacy for HIV testing, distress tolerance and lifetime history of HIV testing, and tested the moderating effect of distress tolerance and sexual risk behaviors on the association between self-efficacy for HIV testing and lifetime history of HIV testing. Data were collected from a cross-sectional sample of 157 sexually active Latino emerging adults aged 18–25 using an online survey and were analyzed using hierarchical logistic regression and moderation analyses. We found that 62.8% of those engaging in sexual risk behaviors had ever been tested for HIV. Participants that were female (aOR=3.14, 95% CI: 1.41–7.02) and those that reported higher levels of self-efficacy for HIV testing (aOR=3.49, 95% CI: 1.78–6.83) were more likely to have ever been tested for HIV in their lifetime. There was a statistically significant three-way interaction among self-efficacy for HIV testing, distress tolerance and sexual risk behaviors (b=2.76, 95% CI: .52, 5.00, p=.016). This interaction suggests that among those that reported any sexual risk behaviors, higher levels of self-efficacy were associated with lifetime history of HIV testing only at higher levels of distress tolerance. More research is warranted to determine how self-efficacy for HIV testing and distress tolerance work together among high-risk groups to promote HIV testing.
Keywords: Latino/a, HIV testing, self-efficacy, distress tolerance, sexual risk behavior
Introduction
Latino emerging adults aged 18–24 in the United States (U.S.) are disproportionately impacted by the HIV epidemic. Latinos accounted for 23.3% of all new HIV diagnoses among emerging adults and had the second highest rate of new HIV diagnoses after non-Latino Blacks in 2016 (CDC, 2018a). In addition, young Latinos in the U.S. are more likely to engage in unprotected sex compared to non-Latino Blacks (Copen, 2017). Despite this elevated HIV risk, both female and male Latino emerging adults have a low prevalence of HIV testing relative to non-Latino Black emerging adults (Latino males: 26.8%, Latino females: 46.5%; non-Latino Black males: 45.3%, non-Latino Black females: 59.9%) (Van Handel, Kann, O’Malley Olsen, & Dietz, 2016). This is concerning as Latinos and young people under the age of 24 are the groups most likely to be unaware of their HIV status (16.5% and 44% respectively) (CDC, 2018b, 2019b). In addition, Latinos are more likely to be diagnosed with AIDS one year after receiving an HIV diagnosis when compared to non-Latino Blacks and Whites (CDC, 2009). Therefore, increasing HIV testing among Latino emerging adults is important to increase the number of people aware of their HIV status, and to link this group to treatment promptly. Early treatment with antiretroviral drugs is critical as it significantly decreases the risk of HIV transmission, reduces HIV-related morbidity, and improves survival (Antiretroviral Therapy Cohort Collaboration, 2017; Rodger et al., 2019).
Self-Efficacy for HIV Testing
Understanding modifiable psychological factors that facilitate HIV testing, particularly among individuals at high risk, is crucial to promote and increase HIV testing (de Wit and Adam, 2008). One psychological factor that may play a role in facilitating testing for HIV is self-efficacy (SE) for HIV testing - defined as a person’s confidence in their ability to test for HIV (Evangeli, Pady, & Wroe, 2016; Pham et al., 2019; Prati et al., 2014; Zhao et al., 2018). It is suggested that individuals with high levels of SE are more likely to take the necessary actions to engage in HIV prevention behaviors (Bandura, 1990). However, to date, no studies have examined the association between SE and HIV testing among Latino emerging adults or in any other stage of development.
Distress Tolerance
Another psychological factor that may influence HIV testing behaviors is distress tolerance (DT). DT is defined as the capacity to withstand and experience negative psychological distress (Simons and Gaher, 2005). Those individuals that have low DT tend to perceive distress as unbearable, cannot handle being distressed and tend to avoid or delay potentially distressing situations (Simons and Gaher, 2005). HIV testing may involve several stressors that can cause psychological distress including the uncertainty of an unknown HIV status or the potential negative consequences of getting a positive test or others finding out about being tested or test results (e.g. stigma, discrimination, rejection) (Adebayo and Gonzalez-Guarda, 2017; de Wit and Adam, 2008; Evangeli, et al., 2016). In fact, evidence from a recent study shows that psychological distress (e.g. worry) is common among people seeking HIV testing (Kagee, Saal, & Bantjes, 2017). As such, differential capacity for tolerating the psychological distress related to HIV testing may distinguish people who seek testing for HIV. However, DT has not been examined in relation to HIV testing.
Sexual Risk Behaviors
Individuals that engage in sexual risk behaviors are of particular importance for HIV testing interventions because they are more likely to contract HIV and if they are unaware of their HIV status, they will continue to unknowingly transmit HIV to others. In fact, 40% of ongoing HIV transmissions are from people unaware of their HIV status (Gopalappa, Farnham, Chen, & Sansom, 2017). In addition, individuals that become aware of their HIV infection reduce their engagement in unprotected sex (Marks, Crepaz, & Janssen, 2006). Emerging adults reporting higher frequency of sexual risk behaviors are more likely to get tested for HIV compared to those reporting lower frequency of sexual risk behaviors (Caldeira, Singer, O’Grady, Vincent, & Arria, 2012). However, the prevalence of HIV testing is low among emerging adults engaging in high-risk HIV behaviors (Trepka and Kim, 2010). Therefore, understanding factors that facilitate HIV testing decisions among individuals engaging in sexual risk behaviors are vital to effectively scale up HIV testing among those at a higher risk for HIV.
Accordingly, the aims of this study were to examine (1) the associations of SE and DT with lifetime history of HIV testing among Latino emerging adults and (2) test the moderating effect of DT and sexual risk behaviors on the association between SE and lifetime history of HIV testing. We hypothesized that (a) higher SE for HIV testing would be associated with a higher likelihood of lifetime history of HIV testing (Hypothesis 1), (b) higher DT would be associated with a higher likelihood of lifetime history of HIV testing (Hypothesis 2), and (c) higher DT would strengthen the association between SE and lifetime history of HIV testing (Hypothesis 3). In addition, a three-way interaction among SE, DT and sexual risk behaviors in relation to lifetime history of HIV testing were explored.
Methods
Participants and Procedures
Data for this study was obtained from the cross-sectional study Project on Health among Emerging Adult Latinos (Project HEAL). The sample included 200 Latino emerging adults; however, forty-one participants were excluded because they had not initiated sexual debut and two had a missing value on questions about having had sexual intercourse or lifetime history of HIV testing. Therefore, the sample for the present study included 157 participants. Eligible participants had to be (1) Latino/Hispanic, (2) between 18 to 25 years of age, (3) currently living in Maricopa County, Arizona or Miami Dade County, Florida, and (4) able to read English. Participants were recruited through social media, listservs, flyers, and word-of-mouth. All participants were enrolled from August 2018 to February 2019 using a quota sampling. Individuals interested in the study contacted the research staff via email and were screened for eligibility, and those eligible were emailed an Internet link to complete the confidential survey and informed consent. The survey completion time was approximately 50 minutes and participants received a $30 Amazon e-gift card as compensation. The study was approved by the Institutional Review Board of Florida International University.
Measures
Lifetime History of HIV Testing was assessed using the following question “Have you ever been tested for HIV, the virus that causes AIDS? (Do not count tests done if you donated blood) (CDC, 2017).
Self-Efficacy for HIV testing was measured using two items “I feel confident that I could get tested for HIV” and “I feel confident that I could locate a place where I can get tested for HIV” (Pham et al., 2017). Items were rated on a 4-point Likert scale ranging from strongly disagree (1) to strongly agree (4). Mean scores ranged from 1 to 4 and higher scores indicated higher SE for HIV testing. Cronbach’s reliability coefficient for this measure was α= .69.
Distress Tolerance was measured using the three-item tolerance sub-scale from the Distress Tolerance Scale (i.e. “feeling distressed or upset is unbearable to me”, “I can’t handle feeling distressed or upset”, “there’s nothing worse than feeling distressed or upset”) (Simons and Gaher, 2005). Items were rated on a 5-point Likert scale strongly disagree (1) to strongly agree (5) and reverse scored. Mean scores ranged from 1 to 5 and higher scores represented higher tolerance for psychological distress. Cronbach’s reliability coefficient for this measure was α= .83. The DT scale has been used in previous studies with emerging adult samples and has demonstrated good to excellent reliability (Beck, Ali, & Daughters, 2014; Iverson, Follette, Pistorello, & Fruzzetti, 2012).
Sexual Risk Behaviors
Participants were classified as reporting any sexual risk behaviors in the past 3 months if they self-reported having >1 sexual partners in the past 3 months (based on response to the question: “In the past 3 months, with how many people did you have sexual intercourse (this includes vaginal and/or anal sex)?”), OR sex under the influence of alcohol or drugs in the past 3 months (based on response to the question: “In the past 3 months, did you drink alcohol or use drugs before you had sexual intercourse (this includes vaginal and/or anal sex)?”), OR unprotected sex with primary and casual partner in the past 3 months (based on response to questions: a) “In the past 3 months, did you use a condom every time you had vaginal and/or anal sex with your primary partner (someone with whom you feel the most committed such as boyfriend/girlfriend, spouse, significant other, or life partner)?” and b) “In the past 3 months, did you use a condom every time you had vaginal and/or anal sex with a casual partner (someone with whom you do not feel committed to or know very well)?”).
Sociodemographic Variables included were age, gender (0=male, 1=female), partner status (0=single, 1=has a partner), sexual minority status (0=heterosexual, 1=sexual minority), nativity (0=immigrant, 1=U.S. born), college student status (0=not a current college student, 1=current college student), education level (0=no bachelor’s degree, 1=has bachelor’s degree or higher), employment status (0=unemployed, 1=employed), health insurance (0=not insured, 1=insured), study site (0=Maricopa County (Arizona), 1=Miami-Dade County (Florida)), and financial strain (1=has more money than needed, 2=just enough money for needs, 3=not enough money to meet needs).
Statistical Analysis
All data analyses were conducted using SPSS V.25. Frequencies and proportions for categorical variables and means and standard deviations for continuous variables were reported. Lifetime history of HIV testing was compared across all independent variables using independent sample t-tests and chi-square tests of association. Using a hierarchical logistic regression (HLR), variables were entered into the model in a specific order to determine the contribution of each group of predictors to the explained variance of the dependent variable (Block 1: sociodemographic variables, Block 2: sexual risk behaviors, and Block 3: SE for HIV testing and DT scores). Only those sociodemographic variables with a p-value <0.10 were included in the model along with sexual risk behaviors, SE and DT scores. The statistical significance level was <0.05 and adjusted odds ratios (aOR) and 95% confidence intervals (CI) were reported.
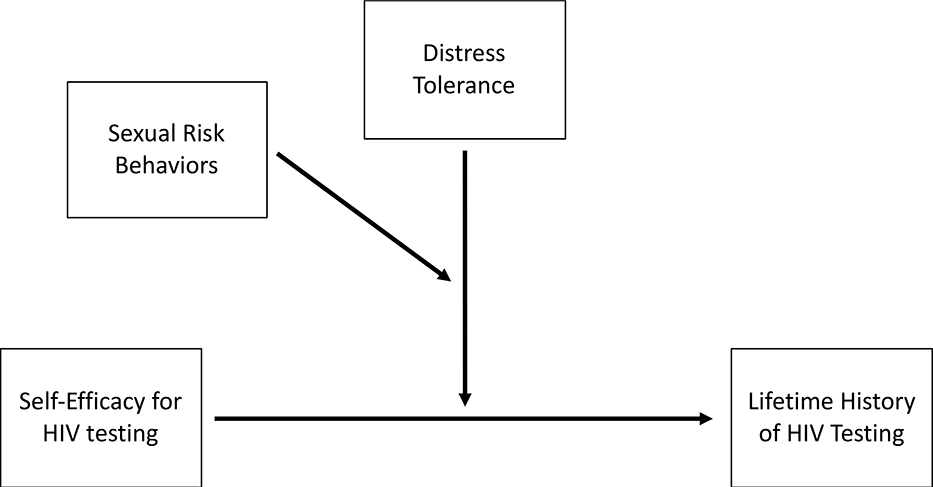
Using PROCESS v3.3 for SPSS (Hayes, 2017), two moderation tests were conducted with 10,000 bootstraps to examine if DT and sexual risk behaviors moderated the association between SE and lifetime history of HIV testing. Bootstrapping was used to calculate confidence intervals of conditional effects. The first moderation test examined the following two-way interaction in relation to lifetime history of HIV testing: SE for HIV testing x DT. The second moderation test examined the following three-way interaction in relation to lifetime history of HIV testing: sexual risk behaviors x DT x SE for HIV testing (Figure 1). All moderation analyses were conducted controlling for sociodemographic variables included in the HLR model. Unstandardized regression coefficients and CIs were reported.
Figure 1.
Three-way interaction modeling between self-efficacy for HIV testing, distress tolerance and sexual risk behaviors on lifetime history of HIV testing.
Results
The sample was comprised of 81 (51.6%) females and 76 males (48.4%) with an average age of 21.5 years (SD=2.04) (Table 1). Most participants were college students (n=104, 66.2%) and born in the U.S. (n=108, 68.8%). The majority identified as Mexican (n=75, 47.8%), Cuban (n=22, 14.0%), Colombian (n=19, 12.1%), non-Colombian South American (n=17, 10.8%), and Central American (n=13, 8.3%). Participants were living in Miami Dade County, Florida (n=74, 47.1%) and Maricopa County, Arizona (n=83, 52.9%). Of those participants living in Florida 97.3% (n=72) were of non-Mexican heritage and of those living in Arizona 88.0% (n=73) were of Mexican heritage.
Table 1.
Characteristics of sexually active Latino emerging adults by lifetime history of HIV testing (n=157).
| Lifetime History of HIV Testing | |||||
|---|---|---|---|---|---|
| Characteristic | Total | Yes | No | ||
| n (%) | n (%) | χ2a | p-value | ||
| Total | 157 | 94 (59.9%) | 63 (40.1%) | ||
| Gender | 4.49 | .034 | |||
| Male | 76 (48.4) | 39 (51.3) | 37 (48.7) | ||
| Female | 81 (51.6) | 55 (67.9) | 26 (32.1) | ||
| Partner Status | 4.29 | .038 | |||
| Single | 102 (65.0) | 55 (53.9) | 47 (46.1) | ||
| Has partner | 55 (35.0) | 39 (70.9) | 16 (29.1) | ||
| Sexual Minority Status | 3.22 | .073 | |||
| Heterosexual | 132 (84.1) | 75 (56.8) | 57 (43.2) | ||
| Sexual minority | 25 (15.9) | 19 (76.0) | 6 (24.0) | ||
| Nativity | 2.32 | .127 | |||
| Immigrant | 49 (31.2) | 25 (51.0) | 24 (49.0) | ||
| U.S. born | 108 (68.8) | 69 (63.9) | 39 (36.1) | ||
| Current College Student | .89 | .347 | |||
| Yes | 104 (66.2) | 65 (62.5) | 39 (37.5) | ||
| No | 53 (33.8) | 29 (54.7) | 24 (45.3) | ||
| Education Level | 9.82 | .002 | |||
| No bachelor’s degree | 116 (73.9) | 61 (52.6) | 55 (47.4) | ||
| Completed bachelor’s degree or higher |
41 (26.1) | 33 (80.5) | 8 (19.5) | ||
| Employment Status | .06 | .804 | |||
| Employed | 131 (83.4) | 79 (60.3) | 52 (39.7) | ||
| Unemployed | 26 (16.6) | 15 (57.7) | 11 (42.3) | ||
| Health Insurance | .16 | .690 | |||
| Yes | 127 (80.9) | 77 (60.6) | 50 (39.4) | ||
| No | 30 (19.1) | 17 (56.7) | 13 (43.3) | ||
| Study Site | 4.23 | .040 | |||
| Miami-Dade County | 74 (47.1) | 38 (51.4) | 36 (48.6) | ||
| Maricopa County | 83 (52.9) | 56 (67.5) | 27 (32.5) | ||
| Sexual Risk Behaviors (Past 3 months) | 1.90 | .169 | |||
| Yes | 121 (77.1) | 76 (62.8) | 45 (37.2) | ||
| No | 36 (22.9) | 18 (50.0) | 18 (50.0) | ||
| >1 sexual partners in the past 3 months | |||||
| Yes | 46 (29.3)b | 24 (52.2) | 22 (47.8) | ||
| No | 108 (68.8) | 70 (64.8) | 38 (35.2) | ||
| Sex under the influence of alcohol or drugs | |||||
| Yes | 58 (36.9) | 42 (72.4) | 16 (27.6) | ||
| No | 99 (63.1) | 52 (52.5) | 47 (47.5) | ||
| Unprotected sex | |||||
| Yes | 77 (49.0)b | 54 (70.1) | 23 (29.9) | ||
| No | 76 (48.4) | 38 (50.0) | 38 (50.0) | ||
| M(SD) | M(SD) | M(SD) | t-valuec | p-value | |
| Age | 21.5 (2.04) | 21.9 (1.92) | 21.0 (2.13) | −2.66 | .009 |
| Financial Strain | 2.31 (.59) | 2.37 (.59) | 2.22 (.58) | −1.58 | .116 |
| Self-Efficacy for HIV testing | 3.28 (.64) | 3.47 (0.57) | 3.01 (0.65) | −4.62d | < .0005 |
| I feel confident that I could get tested for HIV. | 3.25 (.75) | 3.47 (.65) | 2.93 (.79) | ||
| I feel confident that I could locate a place where I can get tested for HIV. | 3.32 (.73) | 3.48 (.67) | 3.09 (.77) | ||
| Distress Tolerance | 2.75 (1.06) | 2.85 (1.04) | 2.60 (1.09) | −1.47 | .143 |
All expected cell frequencies were greater than five for chi-square tests.
Numbers may not sum up to n=157 due to missing data.
The assumption of homogeneity of variances was met based on p-value >.05 on Levene’s tests of equality of variance.
Welch t-test was used due to the assumption of homogeneity of variances being violated, as assessed by Levene’s test for equality of variances (p= .047).
Most participants identified as heterosexual (n=132, 84.1%). In terms of sexual risk behaviors in the past 3 months, 49.0% (n=77) reported having had unprotected sex, 36.9% (n=58) reported sex under the influence of alcohol or drugs, and 29.3% (n=46) reported >1 sexual partners. Only 59.9% (n=94) of participants reported having ever been tested for HIV and 62.8% (n=76) of those that reported engaging in any sexual risk behaviors in the past 3 months had ever been tested for HIV.
Descriptive characteristics and results of t-tests and chi-square tests are found in Table 1.
Predictors of Lifetime History of HIV Testing
Results of the HLR indicated that 34.2% of the variance of lifetime history of HIV testing was explained by all predictor variables included in the model (Table 2). The first block included the sociodemographic variables and explained 20.3% of the variance of lifetime history of HIV testing [Nagelkerke R2=20.3, χ2(6)=25.5, p=<.0005]. The second block included the sexual risk behaviors variable which explained an additional 1% of the variance of lifetime history of HIV testing [Nagelkerke R2=21.3, χ2(7)=26.9, p=<.0005]. The third block included the SE for HIV testing score and DT score which explained an additional 12.9% of the variance in lifetime history of HIV testing (Nagelkerke R2=34.2, χ2(9)=45.8, p=<.0005). Of the nine predictor variables, only two were statistically significant in the final HLR model: gender and SE for HIV testing. The adjusted odds of having ever been tested for HIV was 3.14 times higher for females compared to males (aOR=3.14, 95%CI: 1.41–7.02). Also, a one-unit increase in SE score was associated with being 3.49 times more likely to have ever been tested for HIV (aOR=3.49, 95%CI: 1.78–6.83). Although not statistically significant (p=0.06), a one-unit increase in DT score was associated with being 1.43 times more likely to have ever been tested for HIV (aOR=1.43, 95%CI: .98–2.08).
Table 2.
Hierarchical Logistic Regression Model Predicting Lifetime History of HIV Testing among sexually active Latino emerging adults (n=157).
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Variable | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
| Block 1 | ||||||
| Age | 1.21 | .99, 1.47 | 1.20 | .99, 1.46 | 1.23 | .99, 1.52 |
| Gender (Ref: Male) Female |
2.30 | 1.12, 4.69* | 2.39 | 1.16, 4.93* | 3.14 | 1.41, 7.02* |
| Education Level (Ref: No Bachelor Degree) | ||||||
| Completed Bachelor Degree or Higher | 2.27 | .89, 5.78 | 2.27 | .89, 5.77 | 1.83 | .67, 4.98 |
| Partner Status (Ref:
Single) Has a Partner |
1.33 | .61, 2.91 | 1.28 | .58, 2.82 | 1.26 | .53, 3.02 |
| Sexual Minority (Ref: Heterosexual)
Sexual Minority |
3.27 | 1.10, 9.76* | 3.48 | 1.14, 10.65* | 2.92 | .82, 10.38 |
| Study Site (Ref:
Arizona) Florida |
.64 | .32, 1.31 | .68 | .33, 1.38 | .77 | .36, 1.66 |
| Block 2 | ||||||
| Sexual Risk Behaviors (Ref: No) | ||||||
| Yes | - | - | 1.66 | .71, 3.84 | 1.21 | .48, 3.02 |
| Block3 | ||||||
| Self-Efficacy for HIV testing | - | - | - | - | 3.49 | 1.78, 6.83* |
| Distress Tolerance | - | - | - | - | 1.43 | .98, 2.08 |
Note:
p < .05; Nagelkerke R2=.203 for Block 1, Nagelkerke R2 for Block 2=.213; Nagelkerke R2 for Block 3=.342; Ref: Reference Group.
Moderation Analyses
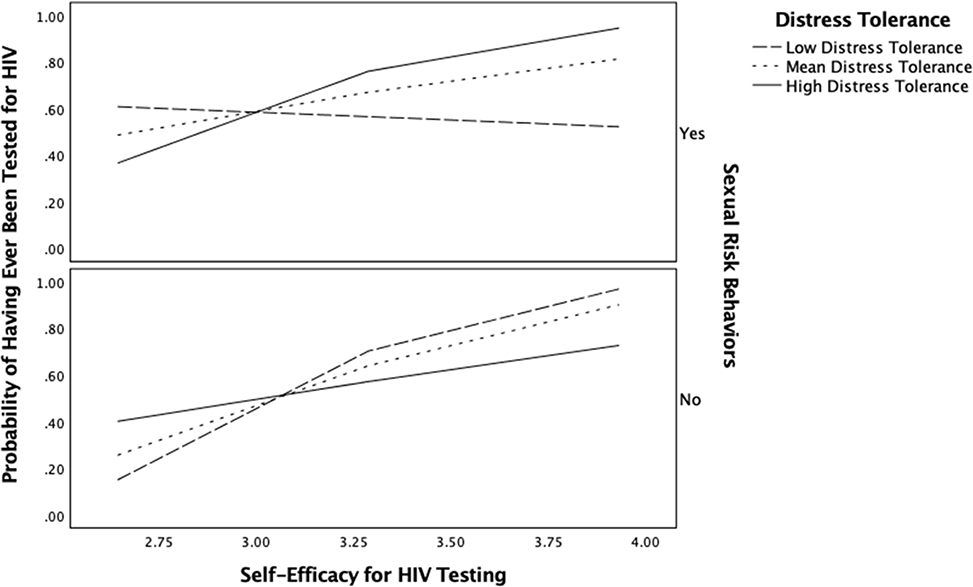
The two-way interaction between SE and DT was not significant (b=0.63, 95%CI: −.11–1.37, p=.094), indicating that DT did not moderate the association between SE and lifetime history of HIV testing. However, the three-way interaction term was significant (b=2.76, 95%CI: .52–5.00, p=.016), adding 7.51% to the explained variance above and beyond the HLR model. Results indicated that among participants who did not report any sexual risk behaviors, the interaction between SE and DT, did not have an effect on lifetime history of HIV testing (b =−1.39, p=.165). However, if participants reported any sexual risk behaviors, higher SE was associated with a higher likelihood of lifetime history of HIV testing (b=1.37, p=.012) at mean (mean=2.75; b=1.19, 95%CI: 0.31–2.07, p=.008) and high levels of DT (1 SD above the mean=3.82; b=2.65, 95%CI: 1.00–4.29, p=.002) but not at low levels of DT (1 SD below the mean=1.69; b=−.27, 95%CI: −1.46-.92, p=.654) (Figure 2). Therefore, DT only functioned as a moderator when participants engaging in sexual risk behaviors reported mean and high levels of DT.
Figure 2.
Three-way interaction with sexual risk behaviors and distress tolerance moderating the association between self-efficacy for HIV testing and lifetime history of HIV testing. Low distress tolerance=1 SD below the mean and high distress tolerance=1 SD above the mean.
Discussion
This study extends the literature on HIV testing by examining the association of lifetime history of HIV testing in relation to SE for HIV testing and DT. Our first hypothesis of the positive association between SE for HIV testing and lifetime history of HIV testing was supported and is consistent with previous studies among other population groups that have shown that increasing SE may help to promote HIV testing (Pham, et al., 2019; Prati, et al., 2014; Zhao, et al., 2018). However, this finding should be interpreted with caution as we could not assess the temporality of this association. It is also likely that higher levels of SE increased as a consequence of having received HIV testing. According to (Bandura, 1977), learning from personal experiences of mastery arising from successful performances can increase a person’s SE. Therefore, it is also possible that participants may have strengthened their SE for HIV testing as a result of having received HIV testing. Nonetheless, this finding shows a potential causal association between SE and lifetime history of HIV testing, and the potential value of incorporating SE in prevention strategies to facilitate HIV testing.
Our second hypothesis that DT would be positively associated with lifetime history of HIV testing was not supported among our study sample. Although DT was not a significant predictor of lifetime history of HIV testing, it approached statistical significance in the direction of higher levels of DT associated with being more likely to have ever been tested for HIV. Further research is needed to elucidate whether this association is stronger when measuring DT in the context of HIV testing and whether it exists among other Latino and emerging adult populations.
Our third hypothesis that DT would strengthen the association between SE and lifetime history of HIV testing was partially supported as this was only found among those that reported any sexual risk behaviors. Specifically, we found that the association between SE and lifetime history of HIV testing was stronger for participants that reported any sexual risk behaviors and have high and mean levels of DT. This finding suggests that DT and SE can work together to promote HIV testing among those engaging in sexual risk behaviors. It appears that although having confidence in one’s ability to getting tested for HIV and finding a testing place may motivate a person to get tested for HIV, higher DT levels may further facilitate HIV testing among those that engage in sexual risk behaviors. Being able to tolerate and not avoid the psychological distress related to HIV testing may enhance one’s confidence in their ability to take the preventive action of getting tested for HIV by regulating emotional responses to the uncertainty and negative expectations associated with HIV testing (Simons and Gaher, 2005). It is important to note that this finding should be interpreted with caution as the direction of this association is unknown. It is also possible that those participants that engaged in sexual risk behaviors were more likely to utilize HIV prevention services, and as a result, they had higher levels of SE for HIV testing and DT. Further research should explore the direction of this three-way interaction.
If this finding is replicated, both SE for HIV testing and DT may be incorporated as targets in HIV testing interventions to effectively increase and promote HIV testing among individuals engaging in sexual risk behaviors, and to further strengthen the effect of current HIV prevention interventions. For example, strategies to increase SE such as individualized risk-reduction counseling and motivational interviewing may incorporate strategies to develop DT (e.g. emotional acceptance skills) to encourage individuals engaging in sexual risk behaviors to seek HIV testing even in the face of psychological distress related to HIV testing (Chapman, 2006; Herbst et al., 2007).
Furthermore, consistent with previous studies among emerging adults, females were more likely to have ever been tested for HIV than males (Caldeira, et al., 2012). This could be the result of females utilizing health services more than males and having more opportunities to be tested for HIV through routine gynecological and prenatal screenings (Anderson and Sansom, 2006; Caldeira, et al., 2012). This finding emphasizes the importance of continued outreach efforts to reach Latino males and increase the uptake of HIV testing in this population. This is particularly important as Latino males account for 22% of new HIV diagnoses in the U.S. (CDC, 2019a).
The prevalence of HIV testing among Latino emerging adults in this study was sub-optimal (59.9%), despite CDC guidelines recommending that adults aged 13–64 should test at least once in their lifetime (Branson et al., 2006). However, HIV testing prevalence for females (67.9%) and males (51.3%) in this sample were higher than national estimates of HIV testing for female (46.5%) and male (26.8%) Latino emerging adults (Van Handel, et al., 2016); this may be due to the higher proportion of college students in our sample (66.2%) whom may be more likely to access sexual health services which could lead to HIV testing. Nonetheless, both Latino females and males face barriers to accessing and receiving HIV testing including limited access to health care and HIV prevention services (Rao, 2016; Taveras et al., 2017).
Forty percent (n=63) of participants reported never having been tested for HIV. Among these, the most frequently reported reasons for not testing included “weren’t offered an HIV test” (47.6%) and “haven’t done anything to get HIV” (47.6%) (data not shown). Both having a low HIV risk perception and never having been offered an HIV test have been consistently found to be significant barriers for HIV testing among young people in the U.S. (Cheong, Tucker, & Chandler, 2018; Peralta, Deeds, Hipszer, & Ghalib, 2007; Schnall, Rojas, & Travers, 2015). Therefore, these findings underscore the importance of changing HIV risk perceptions and improving self-efficacy to encourage Latino emerging adults to proactively seek and/or request HIV testing.
The present study has several limitations. The use of a non-probability sampling and only offering the online survey in English may limit the generalizability of these findings. Thus, this study should be replicated with other Latino and emerging adult populations. The reliance on self-reported measures may have introduced recall and social desirability biases, however, to minimize these biases some measures used a 3-month recall period and confidentiality was assured. The cross-sectional design of this study limited the analysis of temporal relationships. Also, this study didn’t use standardized, validated scales to measure SE and DT in the context of HIV testing, as none exist specifically for HIV testing. Therefore, developing and validating SE and DT for HIV testing scales is important to allow comparisons across studies and better synthesize evidence to guide prevention programs. Lastly, the scales used to measure SE for HIV testing and DT may reflect a limited understanding of these constructs as they do not consider the sociocultural context that influence how these constructs work to change health behaviors in Latino populations.
Despite these limitations, the findings of this study may have implications for the development of tailored HIV testing interventions for Latino emerging adults. Since HIV testing is suboptimal in this population, prevention interventions should focus on increasing SE and DT to promote HIV testing among Latino emerging adults with the goal of reducing undiagnosed infections and HIV transmission. Future studies using prospective designs should examine the association between HIV testing in relation to SE and DT to determine temporality and how SE and DT work together to promote HIV testing.
Acknowledgements
The authors would like to acknowledge Carlos Estrada, Diana Gutierrez, and Irma Beatriz Vega de Luna for their work in recruiting participants for the project and all the study participants. Preparation of this article was supported by FIU University Graduate School Dissertation Year Fellowship, the National Institute on Alcohol Abuse and Alcoholism [K01 AA025992] and the National Institute on Minority Health and Health Disparities [K01 MD013770, 5S21MD010683, U54MD012393]. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health.
Footnotes
Disclosure Statement
All authors declare that they have no conflicts of interest and do not have any financial disclosures to report.
References
- Adebayo OW, & Gonzalez-Guarda RM (2017). Factors associated with HIV testing in youth in the United States: an integrative review. Journal of the Association of Nurses in AIDS Care, 28(3), 342–362. [DOI] [PubMed] [Google Scholar]
- Anderson JE, & Sansom S (2006). HIV testing among US women during prenatal care: findings from the 2002 National Survey of Family Growth. Maternal and Child Health Journal, 10(5), 413–417. [DOI] [PubMed] [Google Scholar]
- Antiretroviral Therapy Cohort Collaboration. (2017). Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV, 4(8), e349–e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1977). Self-efficacy: toward a unifying theory of behavioral change. Psychological Review, 84(2), 191. [DOI] [PubMed] [Google Scholar]
- Bandura A (1990). Perceived self-efficacy in the exercise of control over AIDS infection. Evaluation and Program Planning 13(1), 9–17. [Google Scholar]
- Beck KH, Ali B, & Daughters SB (2014). Distress tolerance as a predictor of risky and aggressive driving. Traffic Injury Prevention, 15(4), 349–354. [DOI] [PubMed] [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, & Clark JE (2006). Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report: Recommendations and Reports, 55(RR14), 1–17. [PubMed] [Google Scholar]
- Caldeira KM, Singer BJ, O’Grady KE, Vincent KB, & Arria AM (2012). HIV testing in recent college students: prevalence and correlates. AIDS Education and Prevention, 24(4), 363–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2009). Late HIV testing - 34 states, 1996–2005. Morbidity and Mortality Weekly Report, 58(24), 661–665. [PubMed] [Google Scholar]
- CDC. (2017). 2017 National Youth Risk Behavior Survey. Retrieved Date Accessed, 2018 from https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/2017_yrbs_national_hs_questionnaire.pdf.
- CDC. (2018a). Diagnoses of HIV infection among adolescents and young adults in the United States and 6 dependent areas, 2011–2016. HIV Surveillance Supplemental Report, 23(23(No.3)), pp. 1–45. Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. [Google Scholar]
- CDC. (2018b). Estimated HIV incidence and prevalence in the United States 2010–2015. HIV Surveillance Supplemental Report 2018, 23(No.1)Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-23-1.pdf [Google Scholar]
- CDC. (2019a). HIV and Hispanics/Latinos. Retrieved Date Accessed, 2019 from https://www.cdc.gov/hiv/pdf/group/racialethnic/hispaniclatinos/cdc-hiv-latinos.pdf.
- CDC. (2019b). HIV and Youth. Retrieved Date Accessed, 2019 from https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf.
- Chapman AL (2006). Acceptance and mindfulness in behavior therapy: A comparison of Dialectical Behavior Therapy and Acceptance and Commitment Therapy. International Journal of Behavioral Consultation and Therapy, 2(3), 308. [Google Scholar]
- Cheong J, Tucker JA, & Chandler SD (2018). Reasons for Accepting and Declining Free HIV Testing and Counseling Among Young African American Women Living in Disadvantaged Southern Urban Communities. AIDS Patient Care and STDs, 33(1), 25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copen CE (2017). Condom Use During Sexual Intercourse Among Women and Men Aged 15–44 in the United States: 2011–2015 National Survey of Family Growth. National Health Statistics Reports(105), 1–18. [PubMed] [Google Scholar]
- de Wit JB, & Adam PC (2008). To test or not to test: psychosocial barriers to HIV testing in high-income countries. HIV Medicine, 9 Suppl 2, 20–22. [DOI] [PubMed] [Google Scholar]
- Evangeli M, Pady K, & Wroe AL (2016). Which Psychological Factors are Related to HIV Testing? A Quantitative Systematic Review of Global Studies. AIDS and Behavior, 20(4), 880–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopalappa C, Farnham PG, Chen YH, & Sansom SL (2017). Progression and Transmission of HIV/AIDS (PATH 2.0). Medical Decision Making, 37(2), 224–233. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach: Guilford Publications. [Google Scholar]
- Herbst JH, Beeker C, Mathew A, McNally T, Passin WF, Kay LS, Crepaz N, Lyles CM, Briss P, Chattopadhyay S, Johnson RL, Task Force on Community Preventive Services. (2007). The effectiveness of individual-, group-, and community-level HIV behavioral risk-reduction interventions for adult men who have sex with men: a systematic review. American Journal of Preventive Medicine, 32(4), 38–67. [DOI] [PubMed] [Google Scholar]
- Iverson KM, Follette VM, Pistorello J, & Fruzzetti AE (2012). An investigation of experiential avoidance, emotion dysregulation, and distress tolerance in young adult outpatients with borderline personality disorder symptoms. Personality Disorders: Theory, Research, and Treatment, 3(4), 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagee A, Saal W, & Bantjes J (2017). Distress, depression and anxiety among persons seeking HIV testing. AIDS Care, 29(3), 280–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks G, Crepaz N, & Janssen RS (2006). Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS, 20(10), 1447–1450. [DOI] [PubMed] [Google Scholar]
- Peralta L, Deeds BG, Hipszer S, & Ghalib K (2007). Barriers and facilitators to adolescent HIV testing. AIDS Patient Care and STDS, 21(6), 400–408. [DOI] [PubMed] [Google Scholar]
- Pham MD, Aung PP, Agius PA, Pasricha N, Oo SM, Tun W, Bajracharya A, Luchters S (2019). Relationship between self-efficacy and HIV testing uptake among young men who have sex with men in Myanmar: a cross-sectional analysis. International Journal of STD & AIDS, 30(1), 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham MD, Aung PP, Paing AK, Pasricha N, Agius PA, Tun W, Bajracharya A, Luchters S (2017). Factors associated with HIV testing among young men who have sex with men in Myanmar: a cross-sectional study. Journal of the International AIDS Society, 20(3), e25026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G, Breveglieri M, Lelleri R, Furegato M, Gios L, & Pietrantoni L (2014). Psychosocial correlates of HIV testing among men who have sex with men in Italy: a cross-sectional study. International journal of STD & AIDS, 25(7), 496–503. [DOI] [PubMed] [Google Scholar]
- Rao S (2016). HIV testing and outcomes among hispanics/latinos—United States, Puerto Rico, and US Virgin Islands, 2014. MMWR. Mrbidity and Mortality Weekly Report, 65 [DOI] [PubMed] [Google Scholar]
- Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. (2019). Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet, 393(10189), 2428–2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall R, Rojas M, & Travers J (2015). Understanding HIV testing behaviors of minority adolescents: a health behavior model analysis. Journal of the Association of Nurses in AIDS Care, 26(3), 246–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102. [Google Scholar]
- Taveras J, Trepka MJ, Madhivanan P, Gollub EL, Devieux J, & Ibrahimou B (2017). HIV Testing Behaviors Among Latina Women Tested for HIV in Florida, 2012. Hispanic Health Care International, 15(1), 27–34. [DOI] [PubMed] [Google Scholar]
- Trepka MJ, & Kim S (2010). Prevalence of human immunodeficiency virus testing and high-risk human immunodeficiency virus behavior among 18 to 22 year-old students and nonstudents: Results of the National Survey of Family Growth. Sexually Transmitted Diseases, 37(10), 653–659. [DOI] [PubMed] [Google Scholar]
- Van Handel M, Kann L, O’Malley Olsen E, & Dietz P (2016). HIV testing among US high school students and young adults. Pediatrics, 137(2), e20152700. [DOI] [PubMed] [Google Scholar]
- Zhao P, Liu L, Zhang Y, Cheng H, Cao B, Liu C, Wang C, Yang B, Wei C, Tucker JD, Tang W (2018). The interaction between HIV testing social norms and self-efficacy on HIV testing among Chinese men who have sex with men: results from an online cross-sectional study. BMC Infectious Diseases, 18(1), 541. [DOI] [PMC free article] [PubMed] [Google Scholar]