Abstract
Background
Attention deficit/hyperactivity disorder (ADHD) is associated with emotional problems and their co-occurrence often leads to worse outcomes. We investigated the developmental associations between ADHD and emotional problems from childhood to early adolescence and examined the genetic and environmental contributions to their developmental link. We further tested whether this developmental association remained across the transition to young adulthood.
Methods
We used data from the Environmental Risk (E-Risk) Longitudinal Twin Study, a cohort of 2,232 British twins. In childhood, ADHD and emotional problems were assessed at ages 5, 7, 10 and 12 with mothers’ and teachers’ reports. At age 18, we used self-reported symptoms according to DSM-5 criteria for ADHD, and DSM-IV for anxiety and depression.
Results
Longitudinal analyses showed that earlier ADHD was associated with later emotional problems consistently across childhood. However, earlier emotional problems were not associated with later ADHD symptoms. The developmental association between ADHD and later emotional problems in childhood was entirely explained by common genetic factors. Consistent with results in childhood, earlier symptoms of ADHD were associated with later emotional problems during the transition to young adulthood.
Conclusions
Our findings demonstrate that ADHD symptoms are predictors of the development of emotional problems, from childhood up to young adulthood, through shared genetic influences. Interventions targeting ADHD symptoms might prevent the development of emotional problems. Clinicians treating youth with ADHD must be aware of their risk for developing emotional problems, and ought to assess, monitor, and treat emotional problems alongside ADHD symptoms from childhood to adulthood.
Keywords: ADHD, depression, anxiety, development, genetics
Introduction
Attention deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental disorder characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning and development (American Psychiatric Association, 2013). ADHD typically presents with comorbid psychiatric disorders including a range of emotional problems (Erskine et al., 2016; Thapar & Cooper, 2016). Both ADHD and emotional problems are influenced by a combination of genetic and environmental factors (American Psychiatric Association, 2013; Thapar & Cooper, 2016). Studies have reported that ADHD and emotional problems co-occur in childhood (Chen et al., 2015; Cole, Ball, Martin, Scourfield, & McGuffin, 2009; Rydell, Taylor, & Larsson, 2017; Spatola et al., 2007) throughout adolescence and up to early adulthood (Chen et al., 2015; Cole et al., 2009; Michelini, Eley, Gregory, & McAdams, 2015; Spatola et al., 2007). Compared to ADHD alone, its co-occurrence with emotional problems is associated with greater social impairment, poorer academic functioning, greater risk of psychiatric disorders, substance misuse, and suicide attempts (Biederman et al., 2008; Blackman, Ostrander, & Herman, 2005; Daviss, 2008; Rydell et al., 2017).
The reasons for the co-occurrence of ADHD and emotional problems remain, however, unclear. The link between ADHD and emotional problems could be limited to concurrent associations, with symptoms of both disorders influencing each other as they occur, or representing overlapping neurobiological constructs. People with ADHD may experience emotional problems because of psychosocial stressors associated with ADHD, including harsh parenting, academic failure and problems with peers (Meinzer, Pettit, & Viswesvaran, 2014). In addition, symptoms of emotional problems such as lack of motivation or perception of threat could influence concentration difficulties, irritability and restlessness (Daviss, 2008; Fraser, et al., 2018; Michielsen et al., 2013; Shaw, Stringaris, Nigg, & Leibenluft, 2014). It could also be that rather than the link between ADHD and emotional problems acting only cross-sectionally, this association is developmental, with ADHD symptoms leading to emotional problems later in life. Previous studies have shown that children and adolescents with ADHD are at increased risk for later depression and anxiety (Eyre et al., 2019; Fergusson, Boden, & Horwood, 2010; Meinzer et al., 2013; 2016). Aspects of ADHD, such as problems with emotional regulation, could be an early manifestation of later emotional problems (Shaw, Stringaris, Nigg, & Liebenluft, 2014). However, prior longitudinal studies did not test the hypothesis that emotional problems could predict the development of subsequent ADHD, as untreated symptoms of emotional problems in early years could develop into inattention and impulsivity symptoms of ADHD later on.
The purpose of our longitudinal study was to extend understanding of the developmental associations between ADHD symptoms and emotional problems across childhood and up to young adulthood. We focused on ADHD symptoms as genome-wide association studies (GWAS) found strong concordance between population measures of ADHD symptoms and clinical diagnoses of ADHD indicating that diagnoses are an extreme expression of variation of symptoms in the population (Demontis et al., 2019). Firstly, we investigated the developmental associations between ADHD and emotional problems between ages 5 and 12 using prospectively-collected measures from a longitudinal nationally-representative cohort study. We tested whether ADHD symptoms predicted later emotional problems across childhood and whether emotional problems predicted later ADHD symptoms. We further tested the specificity of the association by examining symptoms of inattention and hyperactivity-impulsivity separately.
Secondly, we examined common genetic and environmental influences on the developmental associations between ADHD and emotional problems in childhood. Previous research explored the co-occurrence of ADHD and emotional problems. They provided mixed findings regarding the proportion of the phenotypic overlap explained by common genetic influence, varying between 27% and 84% (Chen et al., 2015; Cole et al., 2009; Michelini et al., 2015; Rydell et al., 2017). Conclusions based on these findings are tentative. The wide age range of participants in these studies - between 5 to 19 years - might explain the inconsistent findings as this association may vary across different developmental periods (Rydell et al., 2017). However, results indicating 27% of genetic co-morbidity were found in a sample of twins aged 6 to 18 years (Chen et al., 2015), whereas estimates of 84% were obtained with a sample of girls aged 5 to 17 years (Cole et al., 2009). No study so far has examined the genetic and environmental contributions to the developmental link between ADHD and emotional problems in childhood.
Thirdly, we investigated the developmental association between ADHD and emotional problems from childhood to young adulthood. There is little evidence that the association between ADHD and emotional problems persists into the adult years. Both ADHD and emotional problems develop in early childhood, show some continuity into adulthood and can even emerge in adulthood (Asherson & Agnew-Blais, 2019; Nivard et al., 2015). Adults with ADHD also experience comorbid anxiety and depression (Erskine et al., 2016; Kessler et al., 2006). However, the developmental nature of the association between ADHD and emotional problems into adulthood remains unclear. We tested whether the association across age periods was specific to childhood symptoms of inattention or hyperactivity-impulsivity, as well as to symptoms of anxiety or depression in young adulthood.
Methods
Sample
Participants were members of the Environmental Risk (E-Risk) Longitudinal Twin Study, which tracks the development of a birth cohort of 2,232 British children. The sample was drawn from a larger birth register of twins born in England and Wales in 1994–1995 (Trouton, Spinath, & Plomin, 2002). Full details about the sample are reported elsewhere (Moffitt & E-Risk Study Team, 2002). Briefly, the E-Risk sample was constructed in 1999– 2000, when 1,116 families (93% of those eligible) with same-sex 5-year-old twins participated in home-visit assessments. This sample comprised 56% monozygotic (MZ) and 44% dizygotic (DZ) twin pairs; sex was evenly distributed within zygosity (49% male). Families were recruited to represent the UK population with newborns in the 1990s, on the basis of residential location throughout England and Wales and mother’s age. Teenaged mothers with twins were over-selected to replace high-risk families who were selectively lost to the register through non-response. Older mothers having twins via assisted reproduction were under-selected to avoid an excess of well-educated older mothers.
Follow-up home visits were conducted when children were aged 7 (98% participation), 10 (96%), 12 (96%), and 18 years (93%). Home visits at ages 5, 7, 10, and 12 included assessments with participants and their mother (or primary caretaker). With parents’ permission, questionnaires were mailed to the children’s teachers, who returned questionnaires for 94% of children at age 5 years, 93% of those followed up at age 7 years, 90% at age 10 years, and 83% at age 12 years. Home visits at age 18 included interviews only with participants (n=2,066). Each twin was assessed by a different interviewer. There were no significant differences between those who did and did not take part at age 18 years in socioeconomic status when the cohort was initially defined (χ2=0.86; p=0.65), age-5 IQ scores (t=0.98; p=0.33), age-5 behavioural or emotional problems (t=0.40; p=0.69 and t=0.41; p=0.68, respectively), or rates of childhood ADHD (χ2=2.08; p=0.72). At follow up, the study sample represented the full range and prevalence rates of socioeconomic levels in the UK (Odgers et al., 2012). The Joint South London and Maudsley and the Institute of Psychiatry Research Ethics Committee approved each phase of the study. Parents gave written informed consent and twins gave assent between ages 5 and 12 and then written informed consent at age 18.
Measures
Childhood
We assessed ADHD and emotional problems when participants were aged 5, 7, 10 and 12 using mothers’ and teachers’ reports. Mothers were interviewed face-to-face and teachers responded by mail. Both informants rated each item as being ‘not true’ (0), ‘somewhat or sometimes true’ (1), or ‘very true or often true’ (2). Symptoms were reported for the preceding 6 months. We combined mothers’ and teachers’ reports into total symptom scales for both ADHD and emotional problems; information was included if at least the mother or teacher responded.
ADHD symptoms were assessed using 18 items concerning inattention (e.g., ‘inattentive, easily distracted’) and hyperactivity-impulsivity (e.g. ‘very restless, has difficulty staying seated for long’, ‘impulsive, acts without thinking’) according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV, American Psychiatric Association, 1994). Cronbach’s alpha for the combined mothers’ and teachers’ reports were 0.92 at age 5 and 0.94 at age 12.
Emotional problems were assessed using the Child Behavior Checklist for mothers (Achenbach, 1991a) and the Teacher’s Report Form (Achenbach, 1991b). The emotional problems scale is the sum of the Withdrawn and Anxious/depressed subscales, including items such as ‘cries a lot,’ ‘withdrawn,’ ‘does not get involved with others,’ and ‘worries’. Cronbach’s alpha for the combined mothers’ and teachers’ reports were 0.85 at age 5 and 0.89 at age 12.
Participants’ family socio-economic status (SES) was measured via a composite of parental income (total household), education (highest mother/father), and occupation (highest mother/father) when they were aged 5, and was categorized into tertiles (i.e., low-, medium-, and high-SES).
Young adulthood
We assessed symptoms at age 18 based on face-to-face private structured interviews with participants. Symptoms were reported for the preceding 12 months. ADHD symptoms were queried based on 18 symptoms of inattention and hyperactivity-impulsivity according to DSM-5 criteria (American Psychiatric Association, 2013). Co-informant also rated participants on 8 ADHD symptoms at age 18 years. Prior work in this cohort showed co-informant reports of ADHD symptoms at age 18 corroborated self-reports, as those with self-reported ADHD in young adulthood have significantly more co-informant-rated ADHD symptoms than those without ADHD (Agnew-Blais, Polanczyk, Danese, Wertz, Moffitt, & Arseneault, 2016). Additionally, heritability estimates were similar co-informant reports, indicating that these estimates were not artefacts of twins’ self-reports. We assessed symptoms of depression and generalized anxiety according to DSM-IV criteria (American Psychiatric Association, 1994), using the Diagnostic Interview Schedule (Robins, Cottler, Bucholz, & Compton, 1995). We combined the reports of depression symptoms and generalized anxiety symptoms to obtain comprehensive measure of emotional problems comparable to the one in childhood.
Statistical analyses
Descriptive statistics were conducted in Stata 15.0 (StataCorp, 2017). To examine the concurrent and longitudinal associations between ADHD symptoms and emotional problems throughout childhood (ages 5, 7, 10 and 12), we used structural equation modelling (SEM) in Mplus 7.11 (Muthén & Muthén, 2012).
We tested a full cross-lagged model with the autoregressive effects and both ADHD symptoms and emotional problems predicting each other at a later time point. This model accounted simultaneously for the cross-sectional overlap and stability of symptoms across years. Each individual path in the model deleted cases listwise, and the overall N reported for the whole model is the N of the path with the highest number of observations. Analyses were controlled for sex and family SES and we accounted for non-independence of twin observations and non-normality of the data by using robust standard errors (Muthén & Muthén, 2012).
To test twin correlations and the infiuence of genetic and environmental factors on the longitudinal associations between ADHD symptoms and emotional problems in childhood, we used twin modelling. We used a bivariate Cholesky decomposition to partition the variance in ADHD symptoms and emotional problems, and the covariance between them, into latent factors reflecting additive genetic (A), shared environmental (C) and non-shared environmental (E) effects. Behavioural genetic modelling was conducted using the OpenMx software for R (Boker et al., 2011).
To examine the concurrent and longitudinal associations between ADHD symptoms and emotional problems from childhood (averaged across ages 5, 7, 10 and 12) to young adulthood (age 18), we used SEM procedures. Analyses controlled for sex and family SES.
Results
In childhood, ADHD symptoms and emotional problems decreased from ages 5 to 12, for both boys and girls (Table 1). While emotional problems did not vary across gender, boys showed higher ADHD symptoms at all ages compared to girls. At age 18, we found no gender differences in ADHD, but emotional problems were higher among young women compared to men. Despite those gender differences, patterns of results throughout the analyses were not significantly different between genders. We presented findings for the total sample.
Table 1.
ADHD symptoms and emotional problems across childhood and in young adulthood.
| Total sample | Males | Females | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | Range of scores | M (SD) | N | M (SD) | N | M (SD) | N | t | p | |
| ADHD symptoms | ||||||||||
| 5 | 0–36 | 4.27 (5.19) | 2232 | 5.06 (5.64) | 1092 | 3.52 (4.60) | 1140 | −5.99 | <0.001 | |
| 7 | 0–34 | 3.46 (4.98) | 2177 | 4.33 (5.69) | 1067 | 2.62 (4.02) | 1110 | −6.93 | <0.001 | |
| 10 | 0–31 | 2.83 (4.46) | 2138 | 3.79 (5.09) | 1036 | 1.92 (3.54) | 1102 | −8.23 | <0.001 | |
| 12 | 0–28 | 2.54 (4.40) | 2145 | 3.37 (5.11) | 1044 | 1.76 (3.41) | 1101 | −7.23 | <0.001 | |
| 18 | 0–18 | 5.79 (4.29) | 2061 | 5.79 (4.27) | 976 | 5.78 (4.31) | 1085 | −0.03 | 0.979 | |
| Emotional problems | ||||||||||
| 5 | 0–58 | 12.13 (8.35) | 2232 | 12.19 (8.68) | 1092 | 12.08 (8.02) | 1140 | −0.25 | 0.802 | |
| 7 | 0–66 | 11.60 (8.56) | 2177 | 11.96 (9.02) | 1068 | 11.25 (8.08) | 1109 | −1.63 | 0.102 | |
| 10 | 0–67 | 11.57 (8.90) | 2138 | 11.88 (9.41) | 1036 | 11.28 (8.38) | 1102 | −1.32 | 0.186 | |
| 12 | 0–72 | 10.98 (8.30) | 2141 | 11.14 (8.78) | 1043 | 10.82 (7.81) | 1098 | −0.75 | 0.454 | |
| 18 | 0–15 | 2.75 (4.13) | 2057 | 2.10 (3.66) | 977 | 3.34 (4.43) | 1080 | 6.18 | <0.001 | |
Note. ADHD, attention deficit hyperactivity disorder. M, mean. N, number of participants. SD, standard deviation.
Assessment of ADHD symptoms and emotional problems at ages 5, 7, 10 and 12 was made using informants’ (mother and teacher) reports, and at age 18 using twins’ self-reports.
Longitudinal associations between ADHD and emotional problems across childhood
Results from cross-lagged models indicated four notable findings (Figure 1). First, ADHD symptoms and emotional problems were concurrently associated across childhood, at ages 5, 7, 10 and 12. Correlations ranged from 0.19 at age 7 to 0.27 at age 5. Second, ADHD was correlated over time across the childhood years. We found a similar pattern of correlations for emotional problems. Third, longitudinal analyses showed that ADHD at earlier ages was associated with emotional problems later on, controlling for prior emotional problems and concurrent ADHD symptoms. This indicates that early ADHD predicts later new, or increased levels of, emotional problems. Fourth, emotional problems at an earlier age were not associated with later ADHD, consistently across childhood. Furthermore, when examining symptoms of inattention and hyperactivity-impulsivity separately, we found a similar pattern of findings for both subscales in which different domains of ADHD symptoms led to emotional problems, but not the other way around (Figure S1).
Figure 1.
Longitudinal associations between symptoms of attention deficit hyperactivity disorder (ADHD) and emotional problems across childhood. Note: Analyses controlled for sex and family socio-economic status. All associations are expressed as standardized path coefficients. The 95% confidence intervals are reported in parentheses. Arrows in dashed lines represent non-significant associations. For individual paths, N ranges from 2,138 to 2,232. AIC = 97454.518.
***p<0.001
Genetic and environmental influences on the association between age-5 ADHD and age-12 emotional problems
Given the consistent pattern of associations across childhood, and in order to better characterise the longitudinal associations, we next focused on the association between age-5 ADHD symptoms and age-12 emotional problems.
The phenotypic correlation between age-5 ADHD and age-12 emotional problems was 0.29 (95%CI=0.25–0.33). Twin correlations were higher for MZ twins (r=0.28; 95%CI=0.23–0.33) than for DZ twins (r=0.17; 95%CI=0.10–0.23), suggesting genetic influence contributed to the longitudinal association in childhood. In addition, twin correlations within ADHD were higher for MZ twins (r=0.58; 95%CI=0.53–0.63) than for DZ twins (r=0.20; 95%CI=0.12–0.29), as the correlations within emotional problems (r=0.47; 95%CI=0.41–0.53 for MZ twin and r=0.23; 95%CI=0.15–0.32 for DZ twins). Estimates from the Cholesky model indicated that the covariance between age-5 ADHD and age-12 emotional problems was entirely explained by additive genetic factors common to both phenotypes (Figure 2)1. We found that shared environmental influences (C) on age-5 ADHD and age-12 emotional problems were negligible (0.00 and 0.01, respectively). We dropped the C paths from the full ACE model without significant loss of fit (Δ−2LL=0.02, Δdf=3, p=1.00). The non-shared environmental effects on both ADHD and emotional problems was also close to zero (0.01) and was dropped from the model without significant deterioration in fit (Δ−2LL=0.01, Δdf=1, p=0.91). Furthermore, shared genetic influences between age-5 ADHD and age-12 emotional problems accounted for 15% of the variance in age-12 emotional problems, with a further 32% of variance in age-12 emotional problems explained by genetic influences specific to emotional problems and the remaining 53% of variance by non-shared environmental effects specific to emotional problems.
Figure 2.
Bivariate Cholesky decomposition.
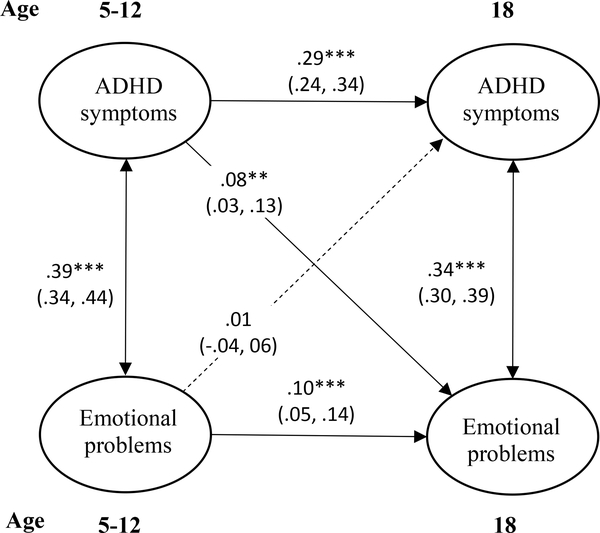
Longitudinal associations between ADHD symptoms and emotional problems from childhood to young adulthood
ADHD symptoms and emotional problems, averaged across ages 5–12, were concurrently correlated, as were ADHD symptoms and combined anxiety and depression symptoms in young adulthood (Figure 3). In addition, childhood ADHD symptoms were longitudinally associated with ADHD symptoms in young adulthood (r=0.29). The longitudinal correlation between childhood and young adulthood emotional problems was lower (r=0.10). Consistent with the cross-lagged model in childhood, longitudinal analyses showed that ADHD in childhood was associated with new, or increased levels of, emotional problems at age 18, even after controlling for prior emotional problems in childhood and concurrent ADHD symptoms in young adulthood. However, the phenotypic correlation between childhood ADHD and age-18 emotional problems was small (r=0.08). Furthermore, emotional problems in childhood were not associated with later ADHD symptoms in young adulthood. Additional analyses showed that the longitudinal association of ADHD symptoms in childhood with later emotional problems was specific to hyperactivity-impulsivity symptoms in childhood (Figure S3). Finally, we found that childhood ADHD symptoms were associated specifically with symptoms of depression at age 18, but not with symptoms of anxiety (Figure S4).
Figure 3.
Longitudinal associations between symptoms of attention deficit hyperactivity disorder (ADHD) and emotional problems from childhood (ages 5–12) to young adulthood (age 18). Note: Analyses controlled for sex and family socio-economic status. All associations are expressed as standardized path coefficients. The 95% confidence intervals are reported in parentheses. Arrows in dashed lines represent non-significant associations. For individual paths, N ranges from 2,057 to 2,218. AIC = 46810.885.
**p<0.01
***p<0.001
Discussion
Our findings from a prospective, longitudinal genetically-sensitive study provide three new pieces of evidence on the nature of the developmental associations between ADHD and emotional problems across childhood and up to young adulthood. First, earlier symptoms of ADHD predict subsequent emotional problems, but not the other way around, a finding that was consistent across the childhood years. Second, this pattern of developmental associations of ADHD and later emotional problems continued in the transition to young adulthood. Third, we found the developmental association between ADHD symptoms and later emotional problems in childhood to be explained by genetic factors. Overall, these findings highlight the risks associated with ADHD symptoms for the development of emotional problems, from childhood up to young adulthood.
Early ADHD symptoms as risk factors for later emotional problems
Our study showed that early symptoms of ADHD are associated with later emotional problems consistent with previous studies (Eyre et al., 2019; Fergusson et al., 2010; Meinzer et al., 2013; 2016). We found this developmental association from childhood to young adulthood, thus across two important developmental stages that involve biological, social and emotional changes. Given the increased likelihood of the new onset of mental health problems during these periods, it is important to consider risks for emotional problems among people with ADHD. Another longitudinal study focusing on older adults showed that those with higher ADHD symptoms reported increased levels of depression and anxiety both cross-sectionally and over six years (Michielsen et al., 2013). Taking together, these findings emphasize the strength of the association between ADHD and emotional problems cross-sectionally, its consistency across time, and its continuity over the life span.
Despite the continuity of the association, the correlation between ADHD and emotional problems throughout the transition to young adulthood was weak. We found this association to be specific to symptoms of depression at age 18, and not anxiety. This may indicate that emerging emotional problems post-puberty have a different developmental nature than early-onset. Moreover, this finding could be explained by lesser variance in our measure of anxiety as we have fewer young adults with high levels of anxiety in our sample.
Genetic and environmental influences on the association between ADHD and emotional problems in childhood
Our findings that genetic factors explained entirely the overlap between early ADHD symptoms and later emotional problems add to the existing knowledge on concurrent associations. Together, previous findings reported mixed evidence about the relative important of genetic factors. The developmental nature of the association in our study, along with the limited age range of the study participants which did not include adults, may contribute to the observation that genetics play a predominant role in the longitudinal overlap between ADHD and emotional problems across the childhood years. However, these findings do not rule out possible influences from environmental factors. Influence of the environment could operate via gene-environment correlation. The cumulative effects of ADHD-related impairments and the negative environmental circumstances triggered by these may lead some youths with ADHD to develop emotional problems (Daviss, 2008). There is a growing body of evidence suggesting that children’s cognition, temperament, and behaviour influence the response and reaction of others towards them (Pardini, 2008; Stern et al., 2018; Wertz et al., 2016). The challenging behaviour of children with ADHD, including restlessness and impulsiveness, could provoke negative reactions from others (e.g., abuse). These negative experiences, in turn, can lead to the development of emotional problems such as anxiety and depression (e.g., failure model). The environment can influence the association between ADHD and emotional problems via gene-environment interaction. Children with ADHD may have genetic propensity to over-react or be over-sensitive to negative aspects of the environment. They may experience difficulties with regulating feelings of stress and frustration and have limited resources to cope with challenging and stressful environments. This, in turn, can lead to the development of emotional problems such as anxiety and depression.
Specific associations between symptom domains of ADHD and emotional problems
Our findings show associations between emotional problems with both domains of ADHD symptoms in childhood. However, it appears that with the transition into young adulthood, these associations become more distinct: we found specific associations between hyperactivity-impulsivity in childhood and symptoms of depression in young adulthood. A possible explanation is that symptoms of hyperactivity-impulsivity in childhood might result in worse functional outcomes and lead to depression in young adulthood. Our findings are somewhat different from a recent study which found that attention problems in adolescence, rather than hyperactivity-impulsivity, appear to be driving the relationship between ADHD and anxiety (Michelini et al., 2015). Mixed findings could relate to the fact these studies focused on different age periods and the association between ADHD dimensions and emotional problems can change over time. Furthermore, ADHD was assessed differently across the two studies and one study focused on a broad definition of emotional problems while the other examined specific anxiety subtypes.
Limitations
Our findings should be considered in light of some limitations. First, we used different informants across ages. Yet, we used reports from the same informants within each age period. The use of different informants may explain the low phenotypic correlation between ADHD in childhood and emotional problems in adulthood. However, a strength of our study is the availability of reports from several informants, which were correlated with participants’ self-reports. The low correlation in our study could reflect the actual correlation between childhood ADHD and later emotional problems, free of shared methods variance.
Second, the time lag is not constant across all assessments. There is a gap of six years between the assessment in adolescence and in young adulthood, compared to the shorter age gap between the childhood assessments. This calls for further studies on the link between ADHD and emotional problems throughout adolescence. Third, although we identified a major role for genetic factors, we are unable to provide insight into the specific genetic factors that may be involved in the association between ADHD and emotional problems. Identifying a strong role for genetic factors in the longitudinal link between ADHD and emotional problems is an important first step towards a deeper understanding of the genetic influences on this developmental association. Fourth, the E-Risk sample is composed of twins and the results may not generalize to singletons. Reassuringly, the prevalence of childhood ADHD at each age in our sample is well within the range of 3.4%–11% estimated previously (Polanczyk et al., 2015) and our rate of ADHD persistence is similar to that found in a meta-analysis (Faraone, Biederman, & Mick, 2006).
Clinical implications
A better understanding of the developmental associations between ADHD and emotional problems has implications for clinical assessment and treatment. The NICE guidelines recommend monitoring ADHD among people with emotional problems (National Institute for Health and Care Excellence [NICE], 2018). Our findings complement these recommendations and suggest monitoring the development of emotional problems among people with ADHD over time in order to detect change and prevent worsening in symptoms (Fraser, et al., 2018). We must also be vigilant with assessing emotional problems and not mistaking them as ADHD symptoms as they may have a similar clinical presentation, for example with difficulties in concentration. Interventions for people with ADHD should focus on preventing the emergence of emotional problems in addition to targeting the symptoms and behavioural aspects of ADHD.
While our findings show that the developmental association between early ADHD and later emotional problems is genetically-mediated, clinical interventions remain meaningful for preventing the development of emotional problems in people with ADHD. Findings from a recent longitudinal study indicate that ADHD medication reduced the long-term risk of depression (Chang, D’Onofrio, Quinn, Lichtenstein, & Larsson, 2016). These findings are in line with previous reports from clinical studies of youths with ADHD (Biederman, Monuteaux, Spencer, Wilens, & Faraone, 2009; Daviss, 2008). Various treatment approaches targeting ADHD can improve academic and social functioning, and over time, may decrease the risk of depression and other disorders (Chang, et al., 2016).
Conclusions
Our findings shed new light on the developmental association between ADHD and emotional problems, and the mechanisms underlying this association. We found that earlier symptoms of ADHD lead to later emotional problems from childhood through adolescence, and to a lesser extend up to early adulthood. The developmental association between childhood ADHD symptoms and emotional problems in childhood was accounted for by genetic factors. The findings stress the importance of assessing and monitoring symptoms of emotional problems among children with ADHD. This study proposes new lines of research into the genetic and environmental factors involved in the development of emotional problems among people with ADHD.
Supplementary Material
Figure S1. Longitudinal associations between (a) inattention symptoms and emotional problems, and (b) hyperactivity-impulsivity symptoms and emotional problems across childhood.
Figure S2. Bivariate Cholesky decomposition using log-transformed variables.
Figure S3. Longitudinal associations between (a) inattention symptoms and emotional problems, and (b) hyperactivity-impulsivity symptoms and emotional problems from childhood (ages 5–12) to young adulthood (age 18).
Figure S4. Longitudinal associations between symptoms of attention deficit hyperactivity disorder (ADHD) and emotional problems in childhood (ages 5–12) and ADHD and (a) depression symptoms, and (b) anxiety symptoms in young adulthood (age 18).
Key points.
ADHD and emotional problems tend to co-occur, but little is known about their developmental association in childhood and up to young adulthood.
In a nationally-representative longitudinal twin study, we showed that symptoms of ADHD in childhood were associated with later emotional problems. Early emotional problems, however, did not lead to later ADHD symptoms.
This developmental association in childhood was entirely explained by common genetic factors.
ADHD symptoms in childhood were associated with emotional problems (symptoms of anxiety and depression) in young adulthood, but not the other way around.
Interventions targeting ADHD symptoms could contribute to preventing the development of emotional problems. Furthermore, emotional problems should be assessed, monitored and treated alongside ADHD symptoms from childhood to adulthood.
Acknowledgments
The E-Risk Study is funded by the Medical Research Council (UKMRC grant G1002190). Additional support was provided by National Institute of Child Health and Human Development (grant HD077482) and by the Jacobs Foundation. J.A-B. is an MRC Skills Development Fellow. T.M. is a British Academy Postdoctoral Fellow. H.L.F. is supported by an MQ Fellows Award (MQ14F40). L.A. is the Mental Health Leadership Fellow for the UK Economic and Social Research Council (ESRC). The authors are grateful to the Study members and their families and teachers for their participation. The authors would like to thank Terrie E. Moffitt and Avshalom Caspi, the founders of the E-Risk Study, CACI, Inc., and to members of the E-Risk team for their dedication, hard work, and insights. The authors have declared that they have no competing or potential conflicts of interest.
Footnotes
Conflict of interest statement: No conflicts declared.
Results from the Cholesky model using log transformed variables are presented in Figure S2.
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of the article:
References
- Achenbach TM (1991a). Manual for the child behaviour checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry. [Google Scholar]
- Achenbach TM (1991b). Manual for the teacher’s report form and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry. [Google Scholar]
- Agnew-Blais JC, Polanczyk G, Danese A, Wertz J, Moffitt TE, & Arseneault L (2016). Persistence, remission and emergence of ADHD in young adulthood: Results from a longitudinal, prospective population-based cohort. JAMA Psychiatry, 73(7), 713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) (1994). DSM-IV: Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: Author. [Google Scholar]
- American Psychiatric Association (APA) (2013). DSM-5: Diagnostic and statistical manual of mental disorders (5th ed). Washington DC: Author. [Google Scholar]
- Asherson P, & Agnew-Blais J (2019). Annual Research Review: Does late-onset attention-deficit/hyperactivity disorder exist? Journal of Child Psychology and Psychiatry, 60, 333–352. [DOI] [PubMed] [Google Scholar]
- Biederman J, Ball SW, Monuteaux MC, Mick E, Spencer TJ, McCreary M, … Faraone SV (2008). New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 426–434. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Spencer T, Wilens TE, & Faraone SV (2009). Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics, 124, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackman GL, Ostrander R, & Herman KC (2005). Children with ADHD and depression: A multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders, 8, 195–207. [DOI] [PubMed] [Google Scholar]
- Boker S, Neale M, Maes H, Wilde M, Spiegel M, Brick T, … Fox J (2011) OpenMx: an open source extended structural equation modelling framework. Psychometrika, 76, 306–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Z, D’Onofrio BM, Quinn PD, Lichtenstein P, & Larsson H (2016). Medication for attention-deficit/hyperactivity disorder and risk for depression: A nationwide longitudinal cohort study. Biological Psychiatry, 80, 916–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen TJ, Ji CY, Wang SS, Lichtenstein P, Larsson H, & Chang Z (2015). Genetic and environmental infiuences on the relationship between ADHD symptoms and internalizing problems: A Chinese twin study. American Journal of Medical Genetics, Part B, 171B, 931–937. [DOI] [PubMed] [Google Scholar]
- Cole J, Ball HA, Martin NC, Scourfield J, & McGuffin P (2009). Genetic overlap between measures of hyperactivity/inattention and mood in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 1094–1101. [DOI] [PubMed] [Google Scholar]
- Daviss WB (2008). A review of co-morbid depression in pediatric ADHD: Etiologies, phenomenology, and treatment. Journal of Child and Adolescent Psychopharmacology, 18, 565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, … Neale BM (2019). Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nature Genetics, 51, 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erskine HE, Norman RE, Ferrari AJ, Chan GCK, Copeland WE, Whiteford HA, & Scott JG (2016). Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: A Systematic Review and Meta-Analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 841–850. [DOI] [PubMed] [Google Scholar]
- Eyre O, Hughes RA, Thapar AK, Leibenluft E, Stringaris A, Smith GD, … Thapar A (2019). Childhood neurodevelopmental difficulties and risk of adolescent depression: the role of irritability. Journal of Child Psychology and Psychiatry, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, & Mick E (2006). The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychological Medicine, 36, 159–165. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, & Horwood LJ (2010). Classification of behavior disorders in adolescence: Scaling methods, predictive validity, and gender differences. Journal of Abnormal Psychology, 119, 699–712. [DOI] [PubMed] [Google Scholar]
- Fraser A, Cooper M, Agha SS, Collishaw S, Rice F, Thapar A, & Eyre O (2018). The presentation of depression symptoms in attention‐deficit/hyperactivity disorder: comparing child and parent reports. Child and Adolescent Mental Health, 23, 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, … Zaslavsky AM (2006). The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. The American Journal of Psychiatry, 163, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Lewinsohn PM, Pettit JW, Seeley JR, Gau JM, Chronis-Tuscano A, & Waxmonsky JG (2013). Attention-deficit/hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depression and Anxiety, 30, 546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, & Viswesvaran C (2014). The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: A meta-analytic review. Clinical Psychology Review, 34, 595–607. [DOI] [PubMed] [Google Scholar]
- Meinzer MC, Pettit JW, Waxmonsky JG, Gnagy E, Molina BSG, & Pelham WE (2016). Does childhood attention-deficit/hyperactivity disorder (ADHD) predict levels of depressive symptoms during emerging adulthood? Journal of Abnormal Child Psychology, 44, 787–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelini G, Eley TC, Gregory AM, & McAdams TA (2015). Aetiological overlap between anxiety and attention deficit hyperactivity symptom dimensions in adolescence. Journal of Child Psychology and Psychiatry, 56, 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michielsen M, Comijs HC, Semeijn EJ, Beekman AT, Deeg DJ, & Sandra Kooij JJ (2013). The comorbidity of anxiety and depressive symptoms in older adults with attention-deficit/hyperactivity disorder: A longitudinal study. Journal of Affective Disorders, 148, 220–227. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, & E-risk Study team. (2002). Teen-aged mothers in contemporary Britain. Journal of Child Psychology and Psychiatry, 43, 727–742. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2012). Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Institute for Health and Care Excellence (2018). Attention deficit hyperactivity disorder: diagnosis and management. (NICE Guideline). nice.org.uk/guidance/ng87. [PubMed]
- Nivard M, Dolan C, Kendler K, Kan K, Willemsen G, van Beijsterveldt C, … Boomsma D (2015). Stability in symptoms of anxiety and depression as a function of genotype and environment: A longitudinal twin study from ages 3 to 63 years. Psychological Medicine, 45, 1039–1049. [DOI] [PubMed] [Google Scholar]
- Odgers C, Caspi A, Russell MA, Sampson RJ, Arseneault L, & Moffitt TE (2012). Supportive parenting mediates neighborhood socioeconomic disparities in children’s antisocial behavior from ages 5 to 12. Development and Psychopathology, 24, 705–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardini DA (2008). Novel insights into longstanding theories of bidirectional parent–child influences: Introduction to the special section. Journal of Abnormal Child Psychology, 36, 627–631. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Salum GA, Sugaya LS, Caye A, & Rohde LA (2015). Annual Research Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry, 56, 345–365. [DOI] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, & Compton W (1995). Diagnostic Interview Schedule for DSM-IV. Washington University School of Medicine, St. Louis. [Google Scholar]
- Rydell M, Taylor MJ, & Larsson H (2017). Genetic and environmental contribution to the association between ADHD and affective problems in early childhood – A Swedish population-based study. American Journal of Medical Genetics, 174B, 538–546. [DOI] [PubMed] [Google Scholar]
- Shaw P, Stringaris A, Nigg J, & Liebenluft E (2014). Emotional dysregulation and attention deficit/hyperactivity disorder. American Journal of Psychiatry,171, 276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatola CA, Fagnani C, Pesenti-Gritti P, Ogliari A, Stazi MA, & Battaglia M (2007). A general population twin study of the CBCL/6–18 DSM-oriented scales. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 619–627. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. College Station, TX: StataCorp LP. [Google Scholar]
- Stern A, Agnew-Blais JC, Danese A, Fisher HL, Jaffee SR, Matthews T, … Arseneault L (2018). Associations between abuse/neglect and ADHD from childhood to young adulthood: A prospective nationally-representative representative twin study. Child Abuse & Neglect, 81, 274–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, & Cooper M (2016). Attention deficit hyperactivity disorder. The Lancet, 387, 1240–1250. [DOI] [PubMed] [Google Scholar]
- Trouton A, Spinath FM, & Plomin R (2002). Twins Early Development Study (TEDS): A multivariate, longitudinal genetic investigation of language, cognition and behavior problems in childhood. Twin Research, 5, 444–448. [DOI] [PubMed] [Google Scholar]
- Wertz J, Wright K, Agnew-Blais JC, Matthews T, Pariante CM, Moffitt TE, & Arseneault L (2016). Parental monitoring and knowledge: A test of bidirectional associations of youths’ antisocial behaviour. Development & Psychopathology, 28, 623–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Longitudinal associations between (a) inattention symptoms and emotional problems, and (b) hyperactivity-impulsivity symptoms and emotional problems across childhood.
Figure S2. Bivariate Cholesky decomposition using log-transformed variables.
Figure S3. Longitudinal associations between (a) inattention symptoms and emotional problems, and (b) hyperactivity-impulsivity symptoms and emotional problems from childhood (ages 5–12) to young adulthood (age 18).
Figure S4. Longitudinal associations between symptoms of attention deficit hyperactivity disorder (ADHD) and emotional problems in childhood (ages 5–12) and ADHD and (a) depression symptoms, and (b) anxiety symptoms in young adulthood (age 18).