Abstract
The present study examined empathy deficits in toddlerhood (age 14 to 36 months) as predictors of antisocial personality disorder (ASPD) symptoms and psychopathy measured by the Levenson Self-Report Psychopathy scale (Levenson et al., 1995) in adulthood (age 23 years) in 956 individuals from the Colorado Longitudinal Twin Study. Consistent with the hypothesis that antisocial behavior is associated with “active” rather than “passive” empathy deficits, early disregard for others, not lack of concern for others, predicted later ASPD symptoms. Early disregard for others was also significantly associated with factor 1 of the Levenson Self-Report Psychopathy Scale, which includes items assessing interpersonal and affective deficits, but not with factor 2, which includes items assessing impulsivity and poor behavioral control. The association between early disregard for others and psychopathy factor 2 was near zero after controlling for the shared variance between psychopathy factors 1 and 2. These results suggest that there is a propensity toward adulthood ASPD symptoms and psychopathy factor 1 that can be assessed early in development, which may help identify individuals most at risk for stable antisocial outcomes.
Keywords: empathy deficits, psychopathy, antisocial personality disorder
Psychopathy is characterized by interpersonal features such as superficial charm and grandiosity, affective features such as callousness and lack of empathy, and behavioral features such as impulsivity and antisocial behavior (Hare, 2003). Antisocial personality disorder (ASPD), a diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) significantly associated with psychopathy (Crego & Widiger, 2015), is characterized by the pervasive pattern of disregard for and violation of the rights of others. Across different version of the DSM, ASPD has been characterized more by the behavioral features of psychopathy than its affective features (Crego & Widiger, 2015), although the DSM-5’s (American Psychiatric Association, 2013) “emerging measures and models” section includes a more dimensional approach for diagnosis that is more convergent with the construct of psychopathy (Few, Lynam, Maples, MacKillp, & Miller, 2015). Although much more research has been conducted on psychopathy than ASPD (Crego & Widiger, 2015), ASPD is also recognized as a disorder associated with substantial clinical, public health, and economic burden (Goldstein et al., 2017).
Low empathy is a hallmark trait of psychopathy (Hare, 2003). However, there is not research addressing whether empathy deficits assessed as early as toddlerhood predict adulthood psychopathy. To address this gap in the literature, the present study examined whether empathy deficits assessed in toddlerhood (14 to 36 months) predict psychopathy and ASPD symptoms in adulthood (age 23 years), with the goal of early identification of individuals most at risk for stable antisocial outcomes.
Early Empathy Deficits as a Predictor of Psychopathy
Empathy is an “emotional response that is congruent with and stems from the apprehension of another’s emotional state or condition” (p. 108, Zahn-Waxler & Radke-Yarrow, 1990). Empathy includes both affective (i.e., feelings of empathic or sympathetic concern for the other person in distress) and cognitive (i.e., apprehending or understanding the other person’s experience) components, and can lead to prosocial behaviors that alleviate the distress of others. Measuring empathy in toddlers is challenging. Assessments must address the emerging affective, cognitive, and behavioral components that develop in children’s empathic responses (Knafo, Zahn-Waxler, Van Hulle, Robinson, & Rhee, 2008). Despite the challenges, substantial progress has been made in constructing reliable and valid measures of empathy in young children (e.g. Davidov, Zahn-Waxler, Roth-Hanania, & Knafo, 2013; Eisenberg, Fabes, & Spinrad, 2006; Svetlova, Nichols, & Brownell, 2010; Vaish, Carpenter, & Tomasello, 2009). Researchers have shown that the capacity for empathy and prosocial behavior occurs as early as the second year of life (Zahn-Waxler, Schoen, & Decety, 2018). There are also significant individual differences in empathy and prosocial behavior in very young children (Knafo, et al., 2008).
Although there is a lack of longitudinal research examining whether very early observed empathic deficits are a propensity for psychopathy in adulthood, research examining callous-unemotional (CU) traits is informative. CU traits, a childhood construct primarily characterized by empathy deficits, lack of guilt, and shallow emotions, are significantly associated with later psychopathy (Frick & Dickens, 2006). Several studies show that CU traits can be assessed reliably in preschool children (Kimonis et al., 2006; Kimonis et al., 2016; Waller et al., 2016). A recent meta-analysis indicates that there is a cross-sectional association between CU traits and conduct problem severity assessed prior to age 5 years (r = .39, p < .001; Longman, Hawes, & Kohlhoff, 2016). Additionally, CU behavior1 assessed at age 3 years uniquely predicts CU behavior assessed at age 9.5 years (β = .33 to .38, p < .001), suggesting the stability of CU behavior (Waller et al., 2016). There is also evidence of association between interpersonal callousness in later childhood (age 7 to 12 years) and psychopathy in young adulthood (age 18 to 19 years) (β = .04 to .07, p < .01 to .001; Burke, Loeber, & Lahey, 2007), and between psychopathy assessed during adolescence (age 13 years) and adulthood (age 24 years) (r = .31, p < .001; Lynam et al., 2007). CU traits also characterize individuals with particularly severe, aggressive, and stable antisocial behavior (Frick, Stickle, Dandreaux, Farrell, & Kimonis, 2005; Frick & White, 2008). Research on CU traits led to the “limited prosocial emotions” specifier in the diagnostic criteria for conduct disorder in the DSM-5 (American Psychiatric Association, 2013), which may help identify individuals with serious antisocial behavior.
Recently, our group examined whether low “concern for others” and high “disregard for others”, two constructs negatively associated with empathy assessed very early in life (14 to 36 months), predict later conduct problems (4 to 17 years) (Rhee, Friedman, et al., 2013; Rhee et al., 2016). “Concern for others” encompasses the behavioral, affective, and cognitive factors associated with empathic and prosocial reactions to others’ distress, such as helping the victim or proximity to the victim, whereas “disregard for others” is characterized by responding to others’ distress with active, negative responses, such as anger and hostility. Low concern for others did not predict later conduct problems, and mother-reported disregard for others was only associated with later parent-reported conduct problems, suggesting method covariance. In contrast, observed disregard for others predicted later parent- (r = .26, p = .04), teacher- (r = .34, p = .01), and self-reported (r = .36, p < .01) conduct problems and a higher-order conduct problems factor (r = .51, p < .01).
These results were consistent with conclusions from previous studies suggesting that empathy deficits are not always associated with antisocial behavior. For example, although autism spectrum disorders are associated with significant empathy deficits, they are not always associated with antisocial behavior (Rogers, Viding, Blair, Frith, & Happé , 2006). Additionally, individuals with psychopathy and autism spectrum disorders may have different types of empathy deficits (e.g., deficits in resonating with others’ distress in psychopathy and deficits in cognitive perspective taking in autism spectrum disorders; Jones, Happé, Gilbert, Burnett, & Viding, 2010). The results also supported the hypothesis that conduct problems are associated with “active” empathy deficits (i.e., reactions charged by negative affect and aggressive responses to others’ distress marked by anger and amusement) rather than the “passive” empathy deficits (i.e., a lack of either interest or capacity for empathy and prosocial behavior) that characterize autism spectrum disorders (Decety & Meyer, 2008).
Distinction Between Psychopathy Factor 1 and Factor 2
Although psychopathy is often described as a taxonic construct, there is evidence suggesting that it is on a continuous dimension in both children and adults (e.g., Edens et al., 2006; Marcus et al., 2006; Murrie et al., 2007). Researchers examining several measures of psychopathy also suggest that there are two distinct factors with a weak to moderate positive correlation. Factor 1 has been called primary psychopathy (Levenson, Kiehl, & Fitzpatrick, 1995), the interpersonal affective factor (Hare, 2003), and the fearless dominance factor (Benning, Patrick, Blonigen, Hicks, & Iacono, 2005). Items loading on these factors include those assessing superficial charm, grandiosity, manipulation, shallow affect, and low empathy. Factor 2 has been called secondary psychopathy (Levenson, Kiehl, & Fitzpatrick, 1995), the antisocial deviance factor (Hare, 2003), and the impulsive antisocial factor (Benning et al., 2005). Items loading on these factors include those assessing impulsivity, aggression, and poor behavior control. Levenson et al. (1995), whose Levenson Self-Report Psychopathy scale (LSRP) is examined in the present study, used the terms primary and secondary psychopathy to describe dimensions associated with the primary and secondary psychopathy subtypes described by Karpman (1941). In the present study, the terms “psychopathy factor 1” and “psychopathy factor 2” are used to describe the LSRP primary and secondary psychopathy dimensions. Although some have found that a three-factor model of the LSRP fits the data better than a two-factor model (e.g., Brinkley, Diamond, Magaletta, & Heigel, 2008; Salekin, Chen, Sellbom, Lester, and MacDougall, 2014), evidence from analyses evaluating convergent and discriminant validity suggest that the 2-factor model may still be the best way to interpret the LSRP (Salekin et al., 2014).
The Present Study
The present study addressed whether early empathy deficits can be identified as a propensity for adulthood psychopathy, a question not yet addressed in the literature. It extends our recent work showing that early disregard for others rated by independent observers is a significant predictor of parent-, teacher-, and self-reported conduct problems (Rhee, Friedman, et al., 2013; Rhee et al., 2016) by examining mother-reported and observed concern and disregard for others assessed during toddlerhood as predictors of adulthood ASPD symptoms and psychopathy.
We predict more robust results for observed rather than mother-reported empathy deficits, given that there may be rater bias (e.g., tendencies toward social desirability) in the assessment of mother-reported empathy deficits used in the present study (Rhee, Boeldt, et al., 2013). Given previous results’ support of the suggestion that conduct problems are associated with “active” rather than “passive” empathy deficits (Decety & Meyer, 2008), we hypothesized that early observed disregard for others, rather than lack of concern for others, will be associated with later ASPD symptoms and psychopathy. Also, we hypothesized that observed disregard for others will have stronger associations with psychopathy factor 1 than psychopathy factor 2, given that empathy deficits are a hallmark trait of psychopathy factor 1 (Levenson, Kiehl, & Fitzpatrick, 1995).
Second, we examined whether the associations between toddlerhood empathy deficits and adulthood psychopathy/ASPD symptoms were significant after controlling for aggression observed during toddlerhood, to test the hypothesis that empathy deficits, not behavioral aggression alone, predict adulthood psychopathy/ASPD symptoms. We were also interested in addressing this question because the coding for disregard for others included aggressive responses to others’ distress (i.e., “hits” in mother report and “hits offending object” in the observations), and there was a moderate correlation between disregard for others and aggression (r = .41, p = .04).
Also, given significantly higher prevalence of disregard for others, ASPD symptoms, and psychopathy in boys/men than in girls/women, we explored potential sex differences in the associations, and whether they were significant after controlling for sex. Given results of previous studies, we hypothesized that the associations between disregard for others and ASPD/psychopathy would be present in both boys/men and girls/women, and that the associations would be significant after controlling for sex.
Finally, we explored whether childhood/adolescent conduct problems mediate the association between toddlerhood empathy deficits and adulthood psychopathy/ASPD symptoms, and whether toddlerhood empathy deficits have a direct influence on adulthood psychopathy/ASPD. We hypothesized that the association would be mediated by childhood/adolescent conduct problems given research demonstrating that interpersonal and affective deficits are associated with stable, severe antisocial behavior (e.g., Byrd, Loeber, & Pardini, 2012; Frick et al., 2005; Frick & White, 2008). We also conducted this analysis to examine whether the association between adult psychopathy and ASPD is explained by early empathy deficits and conduct problems.
Method
Participants
Participants were from the Colorado Longitudinal Twin Study, a sample of same-sex twin pairs who were born in Colorado between 1984 and 1990 and recruited through the Colorado Department of Health. Inclusion criteria included birth weight not lower than 1000 grams, gestational age of at least 34 weeks, and living within a two-hour drive of Boulder, CO. More than 50% of parents meeting these criteria enrolled in the study. The ethnicity distribution of the LTS is 86.6% Caucasian, 8.5% Hispanic, 0.7% African American, 1.2% Asian, and 2.9% other. Mothers of twins had a mean of 14.29 years of education, and fathers of twins had a mean of 14.42 years of education. Additional information regarding the LTS is reported in Rhea, Gross, Haberstick, and Corley (2006; 2013).
The present study examined data collected from age 14 months to 23 years. It examined a subset of the LTS (956 individuals; 484 girls/women and 472 boys/men) with data for at least one measure included in the study. There were 261 monozygotic (MZ) twin pairs, 215 dizygotic (DZ) twin pairs, and two pairs whose zygosity could not be confirmed. The sample size for each measure assessed from toddlerhood to adulthood is presented in Appendix 1 in the Supplemental Online Materials. Written informed consent was obtained from the participants (the parents of the twins when they were children or the twins themselves when they were adults) and written assent was obtained from children age 7 years old and older after complete description of the study. Research protocols and consent forms were approved by University of Colorado Boulder’s Institutional Review Board.
Zygosity Determination
Testers rated each twin pair’s similarity on 10 physical characteristics (Nichols & Bilbro, 1966) each time participants were seen in person across the ages. Twins were coded as MZ if they were rated highly similar, and coded as DZ if two or more features were rated only somewhat similar or not at all similar. Zygosity was considered unambiguous if 85% of the raters agreed, and blood testing was used to resolve ambiguity in nine twin pairs. Zygosity ratings were also confirmed for all participants using 11 polymorphic DNA microsatellite markers.
Measures
The descriptive statistics of the measures described below are presented in Appendices 2 and 3 in the Supplemental Online Materials.
Concern and disregard for others.
Observed concern and disregard for others were assessed at 14, 20, 24, and 36 months in the home and the laboratory. During separate episodes in both settings, the mother and the examiner pretended to hurt themselves for 30 seconds while vocalizing pain and simulating pained facial expressions, then gradually decreased expression of distress during the next 30 seconds. A 30-second recording of an infant crying broadcast from a speaker (in a laboratory observation room containing ten toys, including a baby doll) was also an empathy probe at 14, 20, and 24 months. Observers coded children’s responses, including “concern for victim”, “helps victim”, “proximity to victim”, “hypothesis testing” (i.e., nonverbal or verbal attempt to understand distress; e.g., looking at the injured body part), “anger”, “hits offending object”, and “hostility”. Inter-observer reliabilities ranged from .76 to .99. Different observers coded twins within a twin pair. Codes were averaged across empathy probes to maximize reliability, then the average scores were transformed into ordinal variables given high skewness2. The number of categories was chosen to maximize variability while avoiding small cell sizes, and choices regarding the number of categories were made before any analyses were conducted (three or four categories for the four observed concern for others items and two categories for the three observed disregard for others items).
At 14, 20, 24, and 36 months, mothers completed an interview assessing concern (α = .74) and disregard (α = .47) for others. They were asked, “Do you ever see ___ spontaneously help (prompt: pick up things, getting dressed, offering toy)?”, and asked whether their children show particular responses when either the co-twin or mother is distressed, including “approaches”, “comforts”, “hits”, “runs”, and “laughs”. Given high skewness, mother-reported concern and disregard for others were transformed into ordinal variables, with the number of categories chosen to maximize variability while avoiding small cell sizes; there were four to six categories for the four mother-rated concern for others items, and four categories for the three mother-rated disregard for others items.
In a previous study, exploratory and confirmatory factor analyses of items from each assessment method (observed and mother-reported) suggested two underlying factors at each age (Rhee, Boeldt, et al., 2013). At each age, the two-factor model fit the data well. In the mother interviews, “helps”, “approaches”, and “comforts” had significant loadings on the “concern for others” factor and “hits”, “runs”, and “laughs” had significant loadings on the “disregard for others” factor. The correlations between the mother-reported “concern for others” and “disregard for others” were significant and positive at each age except age 14 months (r = .13 to .28), raising concerns regarding rater bias. In the observed measures, “concern for victim”, “helps victim”, “proximity to victim”, and “hypothesis testing” had significant loadings on the “concern for others” factor and “anger”, “hits offending object”, and “hostility” had significantly loadings on the “disregard for others” factor. The correlations between the two factors were significant and negative at each age (r = −.14 to −.31) except 36 months. The correlations between observations and mother reports were modest and not consistently significant (.21 to .29 for concern for others and .03 to .20 for disregard for others); therefore, observed and mother-reported concern and disregard for others were examined separately.
There were several cases of bivariate missingness when examining longitudinal data from 14 to 36 months (e.g., no one who had non-zero score for both “hits offending object” at 14 months and “anger” at 24 months). Therefore, composite variables were created at each age by summing the items loading on each factor in individuals with data for all items. Given significant skewness of the composite variables, they were transformed into ordinal variables with four categories for mother-rated concern for others, observed concern for others, and mother-rated disregard for others, and three categories for observed disregard for others (% of individuals in each category in Appendix 2 of Supplemental Online Materials). Latent variables with loadings on each time point (14, 20, 24, and 36 months), which capture common variance across time points, were examined.
Observed aggression.
A free play session in the family’s living room, with toys set in a standardized array on the floor, was observed at 14, 20, and 24 months. Children played freely without interruption by the examiners or the mother for 15 minutes. The level of aggression (four categories from unaggressive to highly aggressive; % of individuals in each category in Appendix 2 of Supplemental Online Materials) of each twin’s interactions with the co-twin was rated by coders. Each twin within a twin pair was rated by two separate coders.
Conduct problems.
Conduct problems were assessed via parent and teacher report throughout childhood and self-report at age 17 years. Parent reports of conduct problems were assessed via the externalizing scale (α = .94) of the Child Behavior Checklist (CBCL/4–18; Achenbach, 1991a) at age 4, 5, 7, 9, 10, 11, and 12 years. Teacher reports of conduct problems were assessed via the externalizing scale (α = .95) of the Teacher’s Report Form (TRF; Achenbach, 1991b) yearly from age 7 to 12 years. Given significant skewness, the externalizing scale scores were binned into ordinal variables with 4 categories, with the number of categories chosen to avoid small cell sizes (% of individuals in each category in Appendix 2 of Supplemental Online Materials).
Conduct disorder symptoms were assessed via the Diagnostic Interview Schedule for Children-IV (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), a structured interview, at age 17 years. Past year conduct disorder symptoms (as defined by the DSM-IV; American Psychiatric Association, 2000) were not common in the LTS, so stem questions for lifetime conduct disorder symptoms were assessed. Two items, “stealing with confrontation” (0.8%) and “forced sex” (0.1%), were dropped from the analyses because of extremely low prevalence. Prevalence of the remaining items ranged from 1.5% for cruelty to animals to 38.1% for stealing without confrontation.
In Rhee et al. (2016), we examined a hierarchical model with latent variables underlying parent-reported conduct problems (with loadings on each age), teacher-reported conduct problems (with loadings on each age), and self-reported conduct problems (with loadings on each symptom), and a higher-order conduct problems factor (with loadings on the parent-, teacher-, and self-report latent variables) representing the common variance across the three informants. This model fit the data well (see Analyses section re: criteria for good data fit), X2 (296) = 420.54, p < .01, TLI = .98, RMSEA = .02.
Psychopathy.
The Levenson Self-Report Psychopathy (LSRP) Scale (Levenson, Kiehl, & Fitzpatrick, 1995) was used to assess psychopathy at age 23 years. Items loading on the two psychopathy factors determined by Levenson et al. were summed, after reverse-scoring the appropriate items3. Examples of factor 1 scale items (α = .82) include “I enjoy manipulating other people’s feelings” and “For me, what’s right is whatever I can get away with.” Examples of factor 2 scale items (α = .63) include “I have been in a lot of shouting matches with other people” and “I don’t plan anything very far in advance.” The factor 1 and factor 2 scale scores had skewness and kurtosis < 1 (see descriptive statistics in Appendix 3 of Supplemental Online Materials).
Antisocial Personality Disorder (ASPD) symptoms.
Lifetime endorsement of the seven ASPD criteria (e.g., deceitfulness, lack of remorse) were assessed at age 23 using the Diagnostic Interview Schedule – IV (DIS-IV; Robins et al., 2000), a structured clinical interview. Endorsement of the seven criteria ranged from 4.1% for deceitfulness to 34.3% for lack of remorse, and criteria for ASPD diagnosis was met by 4.5% of the sample. We examined a latent variable with loadings on the seven criteria. This model fit the data well (see Analyses section re: criteria for good data fit), X2 (34) = 65.92, p < .01, TLI = .98, RMSEA = .05, and all loadings were statistically significant.
Analyses
Analyses were conducted in Mplus, version 8 (Muthén & Muthén, 1998–2017). Most variables being ordinal necessitated the use of the weighted least squares, mean and variance adjusted (WLSMV) estimation method, which uses pairwise deletion to handle missing data. In the phenotypic analyses, nonindependence of twin pairs was taken into account when computing standard errors and model fit using the TYPE=COMPLEX option (Rebollo, De Moor, Dolan, & Boomsma, 2006). We had a specific, primary hypothesis that observed disregard for others would be significantly associated with psychopathy factor 1. Therefore, an alpha of .05 was used to determine statistical significance. The parameters’ significance was determined by p-values for the z-statistic, or the ratio of the parameter estimate to its standard error, but the X2 difference test was used if there was an inconsistency between the conclusions regarding the parameter significance reached from the p value and the X2 difference test. In addition to the X2, supplementary fit indices less sensitive to sample size were examined. Specifically, we used a Tucker-Lewis index (TLI; Bentler, 1990) > .95 and a root mean square error of approximation (RMSEA; Browne & Cudeck, 1993) < .06 as indicative of good model fit (Hu & Bentler, 1998).
A model examining whether the association between toddlerhood disregard for others and adulthood psychopathy factor 1/ASPD symptoms is mediated by childhood/adolescent conduct problems was tested. For the mediation model, bootstrapping with replacement on 1000 samples was used to estimate an empirical approximation of the sample distributions of the parameters, allowing asymmetrical confidence intervals, as recommended by Preacher and Hayes (2008).
The LTS is a genetically informative sample, and our previous study (Rhee et al., 2016) found that shared environmental influences promoting disregard for others also predisposed individuals to conduct problems in later childhood and adolescence. We explored whether these shared environmental influences also influenced adulthood psychopathy and ASPD symptoms. Specifically, we estimated the magnitude of genetic and environmental influences on the associations between toddlerhood empathy deficits and adulthood psychopathy and ASPD symptoms. We also examined the association between childhood/adolescent conduct problems and adulthood psychopathy/ASPD symptoms that are due to genetic and environmental influences shard in common with toddlerhood empathy deficits. Overall, there was not adequate power to distinguish between genetic and environmental influences. Additional details regarding these analyses and results are presented in the Supplemental Online Materials (Appendices 4 to 9).
Results
Associations Between Toddlerhood Concern and Disregard for Others and Adulthood ASPD Symptoms and Psychopathy
The correlation between psychopathy factor 1 and factor 2 scale scores was significant (r = .47, p < .01) and consistent with the correlation of .40 found by Levenson et al. (1995). The correlation between the latent ASPD variable and the psychopathy factor 2 scale score (r = .51, p < .01) was significantly higher than that between the latent ASPD variable and the psychopathy factor 1 scale score (r = .28, p < .01), ΔX2 (1) = 29.22, p < .01, which is also consistent with previous findings (e.g., Crego & Widiger, 2015).
Table 1 presents the correlations between the latent variables capturing the common variance for toddlerhood concern and disregard for others assessed from 14 to 36 months and adulthood ASPD symptoms and psychopathy. There was a modest negative correlation between mother-reported concern for others and psychopathy factor 1 and factor 2. Although these correlations are in the expected direction, they were not significant. As predicted, the only significant correlations were between observed disregard for others and ASPD symptoms (r = .32, p < .01) and between observed disregard for others and psychopathy factor 1 (r = .31, p < .01); higher disregard for others was associated with higher levels of ASPD symptoms and psychopathy. Also, as predicted, the correlation between observed disregard for others and psychopathy factor 2 was not statistically significant (r = .16, p =.10), although equating the correlations of observed disregard for others with psychopathy factor 1 and factor 2 did not lead to a significant decrement in the fit of the model, ΔX2 (1) = 1.96, p = .16. Observed disregard for others assessed during toddlerhood was not associated with later participation in the study during adulthood (r = .05, p = .73).
Table 1.
Correlations Between Toddlerhood Concern and Disregard for Others and Adulthood Antisocial Personality Disorder and Psychopathy
| Toddlerhood Measures |
Adulthood Measures | ||
|---|---|---|---|
| Antisocial Personality Disorder |
Psychopathy Factor 1 |
Psychopathy Factor 2 |
|
| Mother-Reported Concern for Others | .02 | −.12+ | −.10+ |
| Observed Concern for Others | .04 | −.01 | .02 |
| Mother-Reported Disregard for Others | −.13 | −.01 | .02 |
| Observed Disregard for Others | .32** | .31** | .16 |
Note. Latent variables with loadings on each time point were examined for the toddler measures and a latent variable with loadings on each criterion was examined for antisocial personality disorder. X2 (256) = 339.54, p < .01, TLI = .95, RMSEA = .02.
p < .10 * p < .05
p < .01
Given the correlation of .47 between psychopathy factor 1 and factor 2, we examined whether observed disregard for others was associated with each psychopathy scale after controlling for the other. The regression of psychopathy factor 1 on observed disregard for others remained significant after controlling for psychopathy factor 2 (β = .25, p = .02), but the regression of psychopathy factor 2 on observed disregard for others after controlling for psychopathy factor 1 was near zero (β = .02, p = .78). The regression of ASPD symptoms on observed disregard was significant after controlling for either factor 1 (β = .33, p = .03) or factor 2 (β = .32, p = .01) psychopathy or both (β = .32, p = .02), suggesting that the association between observed disregard for others and ASPD symptoms is not mediated by psychopathy.
Appendix 10 presents the correlations between observed disregard for others assessed at each age and ASPD and psychopathy assessed in adulthood. Observed disregard for others assessed at 14 and 20 months was significantly associated with psychopathy factor 1, and observed disregard for others at 24 months was significantly associated with ASPD. Observed disregard for others assessed at 36 months was not significantly associated with any outcome.
Toddlerhood observed aggression was significantly correlated with toddlerhood observed disregard for others (r = .41, p = .04) and adulthood ASPD symptoms (r = .22, p = .05), but not with psychopathy factor 1 (r = −.03, p = .69) or factor 2 (r = .07, p = .44) . In the analysis regressing psychopathy factor 1 on disregard for others and aggression, disregard for others was significantly associated with psychopathy factor 1 after controlling for aggression (β = .36, p = .01). Aggression was not associated with psychopathy factor 1 after controlling for disregard for others (β = −.15, p = .26). Similarly, disregard for others was significantly associated with ASPD after controlling for aggression (β = .36, p = .05) , but aggression was not associated with ASPD after controlling for disregard for others (β = .07, p = .66).
ASPD symptoms’ correlation with psychopathy factor 2 was greater than that with psychopathy factor 1, consistent with other findings in the literature (Credo & Widiger, 2015). This is not surprising, given that the ASPD criteria include mostly behavioral symptoms. For example, Patrick (2007) noted that only two of the seven ASPD criteria (i.e., deceitfulness and lack of remorse) intersect with the emotional and interpersonal features of Factor 1 (or interpersonal affective factor) of the Psychopathy Checklist Revised (Hare, 2003). It is somewhat surprising that disregard for others had a significant association with ASPD symptoms despite a higher correlation between ASPD symptoms with psychopathy factor 2 than psychopathy factor 1. Therefore, we conducted exploratory analyses examining the correlation between disregard for others and each ASPD criterion (see Appendix 11 in Supplemental Online Materials). Disregard for others was significantly correlated with three of the seven criteria, including deceitfulness and lack of remorse.
Sex Differences
Regressing observed disregard for others (β = .86, p < .01), ASPD symptoms (β = .48, p < .01), psychopathy factor 1 (β = .65, p < .01), and psychopathy factor 2 (β = .36, p < .01) on sex showed that all of these variables were significantly higher in boys/men than in girls/women. We examined whether the association between toddlerhood observed disregard for others and adult outcomes was significant after controlling for sex. The regression of psychopathy factor 1 on observed disregard for others remained significant after controlling for sex (β = .21, p = .03), and the regression of ASPD symptoms on observed disregard for others was marginally significant after controlling for sex (β = .21, p = .07). The association between observed disregard for others and psychopathy factor 2 (β = .05, p = .55) remained non-significant after controlling for sex. The sex effects on ASPD symptoms (β = .48, p < .01), psychopathy factor 1 (β = .65, p < .01), and psychopathy factor 2 (β = .36, p < .01) remained significant after controlling for observed disregard for others, suggesting that the sex differences in the adult outcomes are not explained by earlier observed disregard for others.
We also examined potential sex moderation. Specifically, we analyzed boys/men and girls/women in separate groups, then examined whether the correlations between toddlerhood observed disregard for others and adult outcomes could be constrained to be equal across boys/men and girls/women4. The correlations between observed disregard for others and psychopathy factor 1 (ΔX2 (1) = .05, p = .82) and between observed disregard for others and psychopathy factor 2 (ΔX2 (1) = .69, p = .41) could be constrained across sex. There was a statistical trend of a significant sex difference in the correlation between observed disregard for others and ASPD symptoms in boys/men and girls/women (ΔX2 (1) = 3.51, p = .06; r boys/men = .44, p < .01, r girls/women = −.04, p = .84).
Does Childhood/Adolescent Conduct Problems Mediate the Association Between Toddlerhood Observed Disregard for Others and Adulthood Psychopathy factor 1/ASPD Symptoms?
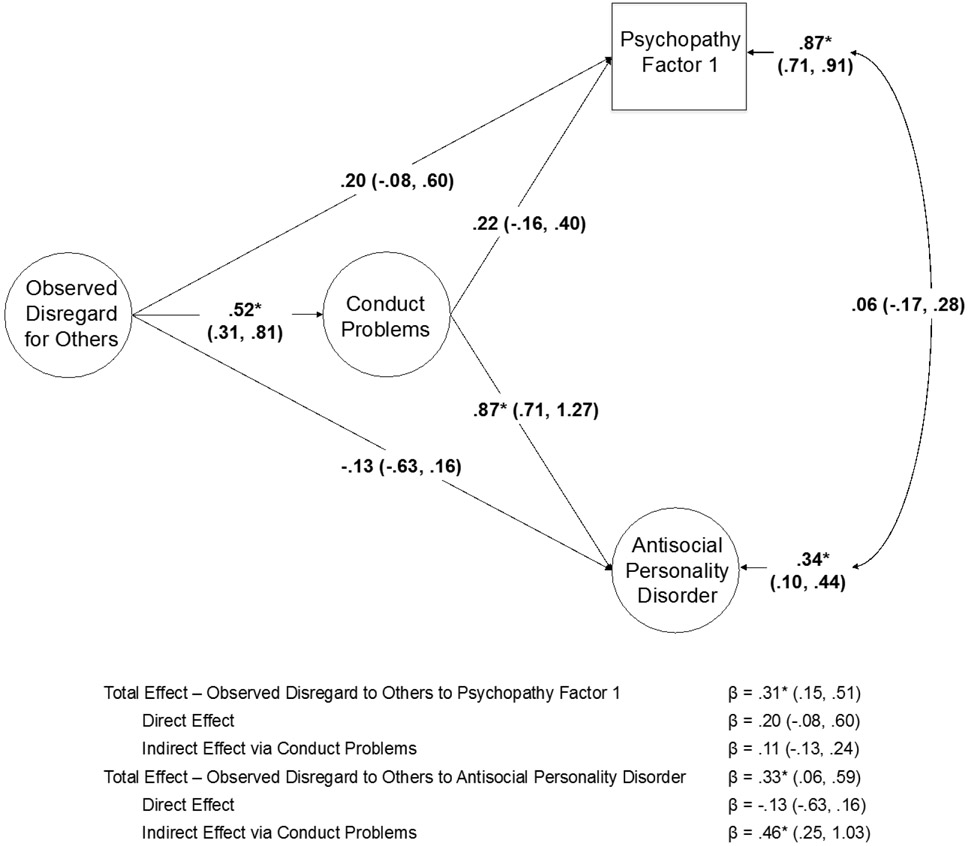
Figure 1 presents the results of a model testing whether the association between toddlerhood observed disregard for others and adulthood psychopathy factor 1/ASPD symptoms is mediated by childhood/adolescent conduct problems. Disregard for others did not have a direct influence on either psychopathy factor 1 or ASPD symptoms. The indirect effect via childhood/adolescent conduct problems was significant for ASPD symptoms, but not psychopathy factor 1. The residual correlation between psychopathy factor 1 and ASPD symptoms was not significant.
Figure 1.
Association between toddlerhood observed disregard for others and adulthood psychopathy factor 1/antisocial personality disorder mediated by childhood/adolescent conduct problems (higher-order factor with loadings on parent-, teacher-, and self-reported conduct problems). Standardized parameters and 95% confidence intervals are presented. * p < .05
Discussion
The primary goal of the present study was to examine whether empathy deficits assessed very early in life (age 14 to 36 months) predict symptoms of ASPD and psychopathy in adulthood (age 23 years). Consistent with our hypotheses, toddlerhood observed disregard for others, not low concern for others, was a modest but significant predictor of adulthood psychopathy factor 1, but not factor 2. Moreover, the associations between disregard for others and psychopathy factor 1 were similar in boys/men and girls/women and significant after controlling for sex.
These results bolster previous suggestions that conduct problems and antisocial behavior are associated with “active”, not “passive” empathy deficits (Decety & Meyer, 2008; Jones, Happé, Gilbert, Burneet, & Viding, 2010), and may help explain the lower than expected association between empathy deficits and aggression found in the literature (Vachon, Lynam, & Johnson, 2014). Moreover, our findings suggest that these deficits can be observed in the second year of life in the form of active disregard for others in distress. They also suggest that psychopathy factors 1 and 2 have differing correlates and predictors. This conclusion is further supported by results from recent studies suggesting that executive functioning deficits (Friedman et al., in press) and internalizing disorders (e.g., Eisenbarth et al., 2019) are associated with factor 2, not factor 1, psychopathy.
Responses to others’ distress are assessed more reliably in older than younger toddlers (Nichols, Svetlova, & Brownell, 2015), and the ability to view harming others as wrong increases across toddlerhood (Dahl & Freda, 2016). In contrast to results expected by these findings, the association between observed disregard for others and psychopathy factor 1 was significant for observed disregard for others assessed at 14 and 20 months, not 24 and 36 months. First, it is possible that these results may be spurious. Another possibility is that observed disregard for others at earlier ages is a better measure of the individual risk for antisocial propensity than that assessed at later ages, which may have more heterogeneous etiology. For example, one study reported that parental harshness was associated with increases in callous unemotional behavior from age 2 to 4, over and above earlier behavior problems (e.g., Waller et al., 2012). A third possibility is that the construct validity of observed disregard for others is lower at 36 months, when the empathy probes may not seem as genuine because the children have had several previous exposures to the empathy probes by then.
There was also a significant association between toddlerhood observed disregard for others and ASPD symptoms, although ASPD symptoms correlated more strongly with psychopathy factor 2 than it did with psychopathy factor 1. Interestingly, exploratory post-hoc analyses showed that disregard for others correlated significantly with the two ASPD criteria that intersect with the emotional and interpersonal features of psychopathy (Patrick, 2007), and only one of the other ASPD criteria intersecting with the behavioral features of psychopathy.
Toddlerhood observed disregard for others and aggression were significantly correlated, and aggression was significantly correlated with adulthood ASPD symptoms (although not with psychopathy). Observed disregard for others predicted both psychopathy factor 1 and ASPD symptoms even after controlling for toddlerhood observed aggression, where aggression predicted neither psychopathy factor 1 nor ASPD symptoms after controlling for disregard for others. These results suggest that the significant associations in the present study are not explained by the simple continuity of aggression or conduct problems from toddlerhood to adulthood or the inclusion of aggressive responses to others’ distress in the assessment of disregard for others.
Observed disregard for others’ association with adulthood ASPD symptoms was mediated by childhood/adolescent conduct problems, and the direct effect of observed disregard for others was not significant. The overall association between observed disregard for others and adulthood psychopathy factor 1 was significant, but neither the direct nor indirect effects were significant. The lack of direct effect of observed disregard for others suggests the possibility that addressing conduct problems in childhood or adolescence may mitigate the stable continuation of interpersonal and affective deficits into adulthood. Also interesting is the result that the residual correlation between adulthood psychopathy factor 1 and ASPD symptoms was small and not significant, suggesting that its association is explained largely by earlier disregard for others and conduct problems.
Implications for Early Identification and Prevention
The present study’s results suggest that the propensity toward adulthood ASPD symptoms and psychopathy, especially psychopathy factor 1, can be identified early in development. They also suggest that early assessment of disregard for others may help identify those most at risk for antisocial outcomes that persists into adulthood. These results are consistent with other findings suggesting stability of callous-unemotional and psychopathic traits from toddlerhood to childhood (e.g., Waller et al., 2016) and childhood to adulthood (e.g., Burke et al., 2007).
Researchers who conducted the first seminal studies on the development of empathy have suggested that assessment of empathy in young children may be improved by the use of objective measures, such as autonomic responses and facial expressions (e.g., Zahn-Waxler & Radke-Yarrow, 1990). There has been significant advancement in this area of research; recent studies have demonstrated distinctive neural responses to others’ harm (e.g., Decety & Cowell, 2018; Decety, Meidenbauer, & Cowell, 2017), prosocial and antisocial actions (e.g., Cowell & Decety, 2015), and fearful emotional body expressions (Rajhans, Missana, Krol, & Grossmann, 2015) in infants and young children. Also, children’s prosocial behavior is predicted by neural responses to others’ distress (Decety, Meidenbauer, & Cowell, 2017).
In a recent review, Waller and Hyde (2017) discussed the ethical implications of studying CU behaviors in early childhood. They cautioned against inadvertently conveying that “preschool psychopaths” can be identified, given that CU traits are only weakly to moderately related to psychopathy, or suggesting that CU behaviors are purely genetic or untreatable. Our results support their caution, given that toddlerhood disregard for others, which is largely influenced by shared environmental influences (Rhee et al., 2016), had a modest association with adulthood psychopathy.
There has been some disagreement in the literature regarding whether psychopathy and CU traits are resistant to treatment (Hawes & Dadds, 2005; Hawes & Dadds, 2007; Salekin, 2002). However, there is general consensus that it is important to identify individuals most at risk for psychopathy as early as possible in order to maximize the potential for prevention (Frick, 2016; Waller et al., 2017). Also, the development of potential prevention strategies of psychopathy in individuals most at risk for stable antisocial outcomes is an important future direction. The significance of shared environmental influences on observed disregard for others suggests that the family environment may be an important target for prevention, and several lines of research provide supportive evidence.
First, preventing childhood maltreatment may be an important prevention strategy. The influence of maltreatment on the interpersonal features of psychopathy begins early. Physically abused toddlers and young children exhibit more aggression toward peers in distress than those who were not abused (Klimes-Dougan & Kistner, 1990; Main & George, 1985). The influence of childhood maltreatment on adulthood psychopathy is persistent (Weiler & Widom, 1996), and the association between childhood maltreatment and adulthood psychopathy is strongest between physical abuse and the antisocial features of psychopathy (Dargis, Newman, and Koenigs, 2016).
Another important facet of early prevention is the enhancement of positive parenting. First, several researchers have noted the importance of early socializing interactions with parents in the development of empathy, such as parental directiveness or parents explaining how a victim feels (e.g., Janssens & Gerris, 1992; Zahn-Waxler et al, 1979). Second, the negative association between positive parenting and CU traits is significant even after controlling for the effects of maltreatment (Kimonis, Cross, Howard, & Donoghue, 2013), and there is a prospective association between both negative and positive parenting and CU traits (Waller, Gardner, & Hyde, 2013). Moreover, the protective effect of early positive parenting against the development of CU traits is environmentally mediated (i.e., not due to confounding with gene–environment correlation). For example, in a recent adoption study, Hyde et al. (2016) found that adoptive mother positive reinforcement assessed at 18 months protected against CU behaviors assessed at 27 months, and that high levels of positive reinforcement buffered against the heritable risk for CU behaviors. Similarly, a study examining monozygotic twin differences in parental harshness and warmth found that the twin who received less harsh parenting and more parental warmth had lower CU traits (Waller et al., 2018). Additional evidence comes from recent studies reporting that the influence of the Fast Track intervention5 on reductions of the level of CU traits was mediated by higher parental warmth (Pasalich et al., 2016), and that the positive effects of a parent training intervention on CU traits was mediated by positive parenting (Kjøbli et al., 2018). Also, a recent open trial pilot study reported that parent–child interaction therapy with a focus on positive parenting strategies led to significant decreases in conduct problems and CU traits and increases in empathy in preschoolers (Kimonis et al., 2019).
In regard to prevention and intervention strategies directed at children at risk of developing psychopathy, a review examining the neurocognitive vulnerabilities of children with CU traits suggests that consistent reward-based interventions may be more effective than those using punishment (Viding & McCrory, 2012). Children with CU traits are relatively insensitive to punishment (Frick & Viding, 2009), and aggressive children who experience greater parental warmth and lower physical punishment show greater decrease in CU traits (Pardini, Lochman, & Powell, 2007). Results from a pilot intervention study suggesting a lower emphasis on punishment (Miller et al., 2014) and a case study suggesting rewards delivered using specific and predictable treatment goals in children with CU traits (Waschbusch et al., 2016) support these ideas. More recently, a comparison between personalized behavioral treatment emphasizing rewards and de-emphasizing punishments and standard behavior therapy showed mixed results across outcome measures (Waschbusch et al., in press). Additional research regarding these reward-based interventions is needed.
Strengths and Limitations of the Present Study
There is a lack of literature on very early predictors of adult psychopathy, despite suggestions that the interpersonal affective deficits of psychopathy begin early in life (e.g., Dadds et al., 2011; Kimonis et al., 2016). The present study is the first to demonstrate that empathy deficits assessed in toddlerhood predict psychopathy and ASPD symptoms in adulthood. It built upon previous work by examining longitudinal data spanning toddlerhood, childhood, adolescence, and adulthood, allowing us to demonstrate that the association between toddlerhood empathy deficits and adulthood ASPD symptoms is mediated by childhood/adolescent conduct problems. Another strength is the multi-method assessment of concern and disregard for others, including observational data.
The results of the present study should be interpreted while considering the following limitations. First, several aspects of the sample may limit the generalizability of the results. The present study examined a twin sample, and we did not directly assess the potential influence of having a same-age, same-sex sibling. The sample examined was mostly Caucasian. Also, the present study examined a community sample with low levels of ASPD and psychopathy. However, a significant association between observed disregard for others and externalizing problems has been reported in a study that over-sampled children with subclinical and clinical levels of externalizing problems (Hastings, Zahn-Waxler, Robinson, Usher, & Bridges, 2000), suggesting that these results may replicate in clinical samples as well. Second, there were some limitations to the assessments used in the present study. The correlations between the mother-reported and observed empathy deficits were low, and the correlations between mother-reported concern and disregard for others were positive, raising concerns regarding rater bias. Additional assessments appropriate for preschool children, such as CU behaviors (e.g., Waller & Hyde, 2017), would have strengthened the study. The assessment of toddlerhood aggression was limited to observations, as parent or teacher ratings were not available. Also, the LSRP primary psychopathy scale does not capture fearlessness or boldness, unlike other measures of psychopathy (Drislane et al., 2014). Finally, although the present study’s sample was large, there was lack of power to distinguish between the effect sizes for the association between disregard for others and psychopathy factor 1 versus factor 2 and between the genetic and environmental influences on the association between disregard for others and psychopathy factor 1.
There are significant shared environmental, but not genetic, influences on disregard for others (Rhee et al., 2016). Although this result seems inconsistent with findings that antisocial behavior with CU traits, including those present in childhood, are particularly heritable (Viding et al., 2004), this discrepancy may be explained by differences in age of assessment and assessment method. Researchers have found greater evidence of shared environmental influences in studies using observational assessments in young children compared to those using parent report or self-report, which cannot be used in young children (e.g., Kendler & Baker, 2007; Roisman & Fraley, 2006). These differing results may be due to differing limitations of the two methods. Parent reports are influenced by the rater contrast effect, or exaggeration of differences between their DZ infants (Loehlin, 1992). In contrast, observations are based on ratings by unbiased, trained individuals. Parent reports provide a general perspective of behaviors across situations and time, whereas observations are usually based on short segments of behavior. In the present study, this time-specific limitation of observational measures was offset by examining a latent factor of observations of empathy deficits across four timepoints.
Conclusions
Toddlerhood disregard for others, rather than lack of concern for others, had a modest but significant association with ASPD symptoms and psychopathy assessed in adulthood, and early disregard for others was significantly associated with psychopathy factor 1, but not factor 2. These results are consistent with the hypotheses that antisocial behavior is associated with “active” rather than “passive” empathy deficits, and that empathy deficits are a hallmark trait of psychopathy factor 1. The assessment of early disregard for others may facilitate the identification of individuals with propensity toward adulthood ASPD symptoms and psychopathy factor 1 for early prevention.
Supplementary Material
Acknowledgments
This study was supported by the MacArthur Foundation, the Fetzer Foundation, and National Institutes of Health grants MH016880, HD007289, DA017637, HD010333, HD050346, DA011015, and AG046938. We thank Corinne Gunn, Sally Ann Rhea, and the participants. Preliminary results of this study were presented at the bi-annual meeting of the Society for Research on Child Development on April 6, 2017.
Footnotes
We use the term “CU behavior” when discussing studies examining young children by Waller and colleagues, who prefer the term “CU behavior” in early childhood and “CU traits” in later childhood. “CU behavior” has fewer stigmatizing connotations of stability or lack of amenability to treatment, and the assessment used in these studies relies on parents reports of observable behaviors (e.g., Waller et al., 2017).
Examining ordinal variables retains the statistical advantages conferred by normality assumptions, and using this approach leads to the estimation of unbiased parameter estimates (Derks, Dolan, & Boomsma, 2004).
We analyzed the LSRP data in two other ways: 1. the two latent factors determined by Levenson et al. (1995) and 2. the three latent factors determined by Brinkley et al. (2008). Overall results and parameter estimates were very similar across the three sets of analyses. Observed disregard for others was significantly associated with the primary psychopathy scale/factor from the two-factor solution and the egocentricity factor from the three-factor solution, even after controlling for the shared variance between psychopathy scales/factors. There was a trend of an association between observed disregard for others and the secondary psychopathy scale/factor from the two-factor solution and the callous and antisocial factors from the three-factor solution; moreover, the association between observed disregard for others and secondary psychopathy/antisocial factors was near zero after controlling for the shared variance between psychopathy scales/factors. Given these results and the large number of items in the LSRP, we present results for the LSRP primary and secondary psychopathy scales.
Models examining measurement invariance, assessed with a chi square difference test, indicated that factor loadings and thresholds could be constrained to be equal for boys/men and girls/women. Factor means were allowed to differ across boys/men and girls/women.
Fast Track is a randomized controlled trial of a multimodal prevention for conduct problems including parent management training, a social emotional skill curriculum, and individualized components.
Contributor Information
Soo Hyun Rhee, University of Colorado Boulder.
Kerri Woodward, University of Colorado Boulder.
Robin P. Corley, University of Colorado Boulder
Alta du Pont, University of Colorado Boulder.
Naomi P. Friedman, University of Colorado Boulder
John K. Hewitt, University of Colorado Boulder
Laura K. Hink, University of Colorado Boulder
JoAnn Robinson, University of Connecticut.
Carolyn Zahn-Waxler, University of Wisconsin–Madison.
References
- Achenbach TM (1991a). Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry. [Google Scholar]
- Achenbach TM (1991b). Manual for the Teacher’s Report Form and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry. [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed). Washington, DC: American Psychiatric Association. [Google Scholar]
- Benning SD, Patrick CJ, Blonigen DM, Hicks BM, & Iacono WG (2005). Estimating facets of psychopathy from normal personality traits: A step toward community epidemiological investigations. Assessment, 12, 3–18. doi: 10.1177/1073191104271223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. [DOI] [PubMed] [Google Scholar]
- Brinkley CA, Diamond PM, Magaletta PR, & Heigel CP (2008). Cross-validation of Levenson’s Psychopathy Scale in a sample of federal female inmates. Assessment, 15, 464–482. [DOI] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit In Bollen KA, & Long JS (Eds.), Testing structural equation models (pp. 136–162). Newbury Park, CA: Sage Publications, Inc. [Google Scholar]
- Burke JD, Loeber R, Lahey BB (2007). Adolescent conduct disorder and interpersonal callousness as predictors of psychopathy in young adults. Journal of Clinical Child and Adolescent Psychology, 36, 334–346. doi: 10.1080/15374410701444223 [DOI] [PubMed] [Google Scholar]
- Byrd AL, Loeber R, & Pardini DA (2012). Understanding desisting and persisting forms of delinquency: The unique contributions of disruptive behavior disorders and interpersonal callousness. Journal of Child Psychology and Psychiatry, 53, 371–380. doi: 10.1111/j.1469-7610.2011.02504.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowell JM, & Decety J (2015). Precursors to morality in development as a complex interplay between neural, socioenvironmental, and behavioral facets. Proceedings of the National Academy of Sciences, 112, 12657–12662. doi: 10.1073/pnas.1508832112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crego C, & Widiger TA (2015). Psychopathy and the DSM. Journal of Personality 83, 665–677. doi: 10.1111/jopy.12115 [DOI] [PubMed] [Google Scholar]
- Dadds MR, Jambrak J, Pasalich D, Hawes DJ, & Brennan J (2011). Impaired attention to the eyes of attachment figures and the developmental origins of psychopathy. Journal of Child Psychology and Psychiatry, 52, 238–245. doi: 10.1111/j.1469-7610.2010.02323.x [DOI] [PubMed] [Google Scholar]
- Dahl A, & Freda GF (2017). How young children come to view harming others as wrong: A developmental analysis In Sommerville JA & Decety J (Eds.), Frontiers of developmental science. Social cognition: Development across the life span (pp. 151–184). New York, NY, US: Routledge/Taylor & Francis Group. [Google Scholar]
- Dargis M, Newman J, & Koenigs M (2016). Clarifying the link between childhood abuse history and psychopathic traits in adult criminal offenders. Personality Disorders: Theory, Research, and Treatment, 7, 221–228. doi: 10.1037/per0000147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidov M, Zahn-Waxler C, Roth‐Hanania R, & Knafo A (2013). Concern for others in the first year of life: Theory, evidence, and avenues for research. Child Development Perspectives, 7, 126–131. doi: 10.1111/cdep.12028 [DOI] [Google Scholar]
- Decety J, & Cowell JM (2018). Interpersonal harm aversion as a necessary foundation for morality: A developmental neuroscience perspective. Development and Psychopathology, 30, 153–164. doi: 10.1017/S0954579417000530 [DOI] [PubMed] [Google Scholar]
- Decety J, Meidenbauer KL, & Cowell JM (2017). The development of cognitive empathy concern in preschool children: A behavioral neuroscience investigation. Developmental Science, 21, e12570. doi: 10.1111/desc.12570 [DOI] [PubMed] [Google Scholar]
- Decety J, & Meyer M (2008). From emotion resonance to empathic understanding: a social developmental neuroscience account. Development and Psychopathology, 20, 1053–1080. doi: 10.1017/S0954579408000503 [DOI] [PubMed] [Google Scholar]
- Derks EM, Dolan CV, & Boomsma DI (2004). Effects of censoring on parameter estimates and power in genetic modeling. Twin Research, 7, 659–669. [DOI] [PubMed] [Google Scholar]
- Drislane LE, Patrick CJ, Arsal G, 2014. Clarifying the content coverage of differing psychopathy inventories through reference to the triarchic psychopathy measure. Psychological Assessment, 26, 350–362. 10.1037/a0035152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edens JF, Marcus DK, Lilienfeld SO, & Poythress NG (2006). Psychopathic, not psychopath: Taxometric evidence for the dimensional structure of psychopathy. Journal of Abnormal Psychology, 115, 131–144. doi: 10.1037/0021-843X.115.1.131 [DOI] [PubMed] [Google Scholar]
- Eisenbarth H, Godinez D, du Pont A, Corley RP, Stallings MC, & Rhee SH (2019). The influence of stressful life events, psychopathy, and their interaction on internalizing and externalizing psychopathology. Psychiatry Research, 272, 438–446. doi: 10.1016/j.psychres.2018.12.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, & Spinrad TL (2006). Prosocial development In Damon W (Series Ed.) & Eisenberg N (Vol. Ed.), Handbook of child psychology, Vol. 3: Social, emotional and personality development (6th ed., pp. 646–718). New York: Wiley. [Google Scholar]
- Few LR, Lynam DR, Maples JL, MacKillop J, & Miller JD (2015). Comparing the utility of DSM-5 section II and III antisocial personality disorder diagnostic approaches for capturing psychopathic traits. Personality Disorders, 6, 64–74. doi: 10.1037/per0000096 [DOI] [PubMed] [Google Scholar]
- Frick PJ (2016). Early identification and treatment of antisocial behavior. Pediatric Clinics of North America, 63, 861–871. doi: 10.1016/j.pcl.2016.06.008 [DOI] [PubMed] [Google Scholar]
- Frick PJ, & Dickens C (2006). Current perspectives on conduct disorder. Current Psychiatry Reports, 8, 59–72. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Stickle TR, Dandreaux DM, Farrell JM, Kimonis ER (2005). Callous-unemotional traits in predicting the severity and stability of conduct problems and delinquency. Journal of Abnormal Child Psychology, 33, 471–487. doi: 10.1007/s10648-005-5728-9 [DOI] [PubMed] [Google Scholar]
- Frick PJ, & Viding E (2009). Antisocial behavior from a developmental psychopathology perspective. Development and Psychopathology, 21, 1111–1131. doi: 10.1017/S0954579409990071 [DOI] [PubMed] [Google Scholar]
- Frick PJ, & White SF (2008). Research review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry, 49, 359–375. doi: 10.1111/j.1469-7610.2007.01862.x [DOI] [PubMed] [Google Scholar]
- Friedman NP, Rhee SH, Ross J, Corley RP, & Hewitt JK (in press). Genetic and environmental relations of executive functions to antisocial personality disorder symptoms and psychopathy. International Journal of Psychophysiology. doi: 10.1016/j.ijpsycho.2018.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Chou SP, Saha TD, Smith SM, Jung J, Zhang H, Pickering RP, Ruan WJ, Huang B, & Grant BF (2017). The epidemiology of antisocial behavioral syndromes in adulthood: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Journal of Clinical Psychiatry, 78, 90–98. doi: 10.1037/0021-843X.115.1.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hare RD (2003). The Hare Psychopathy Checklist-Revised (2nd ed.). Toronto, Ontario, Canada: Multi-Health Systems. [Google Scholar]
- Hastings PD, Zahn-Waxler C, Robinson J, Usher B, & Bridges D (2000). The development of concern for others in children with behavior problems. Developmental Psychology, 36, 531–546. doi: 10.1037/0012-1649.36.5.531 [DOI] [PubMed] [Google Scholar]
- Hawes DJ, & Dadds MR (2005). The treatment of conduct problems in children with callous–unemotional traits. Journal of Consulting and Clinical Psychology, 73, 737–741. doi: 10.1037/0022-006X.73.4.737 [DOI] [PubMed] [Google Scholar]
- Hawes DJ, & Dadds MR (2007). Stability and malleability of callous–unemotional traits during treatment for childhood conduct problems. Journal of Clinical Child and Adolescent Psychology, 35, 347–355. doi: 10.1080/15374410701444298 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods, 3, 424–453. [Google Scholar]
- Hyde LW, Waller R, Tretacosta CJ, Shaw DS, Neiderhiser JM, Ganiban JM, Reiss D, & Leve LD (2016). Heritable and nonheritable pathways to early callous-unemotional behaviors. American Journal of Psychiatry, 173, 903–910. doi: 10.1176/appi.ajp.2016.15111381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssens JMAM, & Gerris JRM (1992). Childrearing, empathy and prosocial behavior In Janssens JMAM & Gerris JRM (Eds.), Child rearing: Influence on prosocial and moral development (pp. 57–75). Amsterdam, the Netherlands: Swets. [Google Scholar]
- Jones AP, Happé FG, Gilbert F, Burnett S, & Viding E (2010). Feeling, caring, knowing: different types of empathy deficit in boys with psychopathic tendencies and autism spectrum disorders. Journal of Child Psychology and Psychiatry, 51, 1188–1197. doi: 10.1111/j.1469-7610.2010.02280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpman B (1941). On the need of separating psychopathy into two distinct clinical types: The symptomatic and the idiopathic. Journal of Criminal Psychopathology, 3, 112–137. [Google Scholar]
- Kendler KS, & Baker JH (2007). Genetic influences on measures of the environment: A systematic review. Psychological Medicine, 37, 615–626. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Cross B, Howard A, & Donoghue K (2013). Maternal care, maltreatment and callous-unemotional traits among urban male juvenile offenders. Journal of Youth and Adolescence, 42, 165–177. doi: 10.1007/s10964-012-9820-5 [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Frick PJ, Boris NW, Smyke AT, Cornell AH, Farrell JM, & Zeanah CH (2006). Callous-unemotional features, behavioral inhibition, and parenting: Independent predictors of aggression in a high-risk preschool sample. Journal of Child and Family Studies, 15, 745–756. doi: 10.1007/s10826-006-9047-8 [DOI] [Google Scholar]
- Kimonis ER, Fleming G, Briggs N, Brouwer-French L, Frick PJ, Hawes DJ, Bagner DM, Thomas R, & Dadds M (2019). Parent–child interaction therapy adapted for preschoolers with callous-unemotional traits: An open trial pilot study. Journal of Clinical Child & Adolescent Psychology, 48, Supplement 1, S347–S361. doi: 10.1080/15374416.2018.1479966 [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Fanti KA, Anastassiou-Hadjicharalambous X, Mertan B, Goulter N, & Katsimicha E (2016). Can callous-unemotional traits be reliably measured in preschoolers? Journal of Abnormal Child Psychology, 44, 625–638. doi: 10.1007/s10802-015-0075-y [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, & Kistner J (1990). Physically abused preschoolers’ responses to peers’ distress. Developmental Psychology, 26, 599–602. [Google Scholar]
- Kjøbli J, Zachrisson HD, & Bjørnebekk G (2018). Three randomized effectiveness trials — one question: Can callous-unemotional traits in children be altered? Journal of Clinical Child & Adolescent Psychology, 47, 436–443. doi: 10.1080/15374416.2016.1178123 [DOI] [PubMed] [Google Scholar]
- Knafo A, Zahn-Waxler C, Van Hulle C, Robinson JL, & Rhee SH (2008). The developmental origins of a disposition toward empathy: genetic and environmental contributions. Emotion, 8, 737–752. doi: 10.1037/a0014179 [DOI] [PubMed] [Google Scholar]
- Levenson MR, Kiehl KA, & Fitzpatrick CM (1995). Assessing psychopathic attributes in a noninstitutionalized population. Journal of Personality and Social Psychology, 68, 151–158. [DOI] [PubMed] [Google Scholar]
- Loehlin JC (1992). Sage series on individual differences and development, Vol. 2. Genes and environment in personality development. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Longman T, Hawes DJ, & Kohlhoff J (2016). Callous-unemotional traits as markers for conduct problem severity in early childhood: A meta-analysis. Child Psychiatry and Human Development, 47, 326–334. doi: 10.1007/s10578-015-0564-9 [DOI] [PubMed] [Google Scholar]
- Lynam DR, Caspi A, Moffitt TE, Loeber R, & Stouthamer-Loeber M (2007). Longitudinal evidence that psychopathy scores in early adolescence predict adult psychopathy. Journal of Abnormal Psychology, 116, 155–165. doi: 10.1037/0021-843X.116.1.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main M, & George C (1985). Responses of abused and disadvantaged toddlers to distress in agemates: A study in the day care setting. Developmental Psychology, 21, 407–412. [Google Scholar]
- Marcus DK, Lilienfeld SO, Edens JF, & Poythress NG (2006). Is antisocial personality disorder continuous or categorical? A taxometric analysis. Psychological Medicine, 36, 1571–1581. doi: 10.1017/S0033291706008245 [DOI] [PubMed] [Google Scholar]
- Miller NV, Haas SM, Waschbusch DA, Willoughby MT, Helseth SA, Crum KI, Coles EK, & Pelham WE (2014). Behavior therapy and callous-unemotional traits: Effects of a pilot study examining modified behavioral contingencies on child behavior. Behavior Therapy, 45, 606–618. doi: 10.1016/j.beth.2013.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrie DC, Marcus DK, Douglas KS, Lee Z, Salekin RT, & Vincent G (2007). Youth with psychopathy features are not a discrete class: A taxometric analysis. Journal of Child Psychology and Psychiatry, 48, 714–723. doi: 10.1111/j.1469-7610.2007.01734.x [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nichols RC, & Bilbro WC (1966). The diagnosis of twin zygosity. Acta Geneticae Medicae et Gemellologiae, 16, 365–275. [DOI] [PubMed] [Google Scholar]
- Nichols SR, Svetlova M, & Brownell CA (2015). Toddlers’ responses to infants’ negative emotions. Infancy, 20, 70–97. doi: 10.1111/infa.12066 [DOI] [Google Scholar]
- Pardini DA, Lochman JE, & Powell N (2007). The development of callous-unemotional traits and antisocial behavior in children: Are there shared and/or unique predictors? Journal of Clinical Child and Adolescent Psychology, 36, 319–333. doi: 10.1080/15374410701444215 [DOI] [PubMed] [Google Scholar]
- Pasalich DS, Witkiewitz K, McMahon RJ, Pinderhughes EE, & The Conduct Problems Prevention Research Group. (2016). Indirect effects of the Fast Track intervention on conduct disorder symptoms and callous-unemotional traits: Distinct pathways involving discipline and warmth. Journal of Abnormal Child Psychology, 44, 587–597. doi: 10.1007/s10802-015-0059-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ (2007). Antisocial personality disorder and psychopathy In O’Donohue W, Fowler KA, & Lilienfeld SO (Eds.), Personality disorders: Toward the DSM-V (pp. 109–166). Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Rajhans P, Missana M, Krol KM, & Grossmann T (2015). The association between temperament and maternal empathy with individual differences in infants’ neural responses to emotional body expression. Development and Psychopathology, 27, 1205–1216. doi: 10.1017/S0954579415000772 [DOI] [PubMed] [Google Scholar]
- Rebollo I, de Moor MHM, Dolan CV, & Boomsma DI (2006). Phenotypic factor analysis of family data: Correction of the bias due to dependency. Twin Research and Human Genetics, 9, 367–376. doi: 10.1375/183242706777591326 [DOI] [PubMed] [Google Scholar]
- Rhea SA, Gross AA, Haberstick BC, & Corley RP (2006). Colorado Twin Registry. Twin Research and Human Genetics, 9, 941–949. [DOI] [PubMed] [Google Scholar]
- Rhea SA, Gross AA, Haberstick BC, & Corley RP (2013). Colorado Twin Registry: An update. Twin Research and Human Genetics, 16, 351–357. doi: 10.1017/thg.2012.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Boeldt DL, Friedman NP, Corley RP, Hewitt JK, Young SE, Knafo A, Robinson J, Waldman ID, Van Hulle CA, & Zahn-Waxler C (2013). The role of language in concern and disregard for others in the first years of life. Developmental Psychology, 49, 197–214. doi: 10.1037/a0028318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Friedman NP, Boeldt DL, Corley RP, Hewitt JK, Knafo A, Lahey BB, Robinson J, Van Hulle CA, Waldman ID, Young SE, & Zahn-Waxler C (2013). Early concern and disregard for others as predictors of antisocial behavior. Journal of Child Psychology and Psychiatry, 54, 157–166. doi: 10.1111/j.1469-7610.2012.02574.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Friedman NP, Corley RP, Hewitt JK, Hink LK, Johnson DP, Smith Watts AK, Young SE, Robinson J, Waldman ID, & Zahn-Waxler C (2016). An examination of the developmental propensity model of conduct problems. Journal of Abnormal Psychology, 125, 550–564. doi: 10.1037/abn0000128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, & Rourke KM (2000). Diagnostic Interview Schedule for the DSM-IV (DIS-IV).
- Rogers J, Viding E, Blair RJ, Frith U, & Happé F (2006). Autism spectrum disorder and psychopathy: Shared cognitive underpinnings or double hit? Psychological Medicine, 36, 1789–1798. doi: 10.1017/S0033291706008853 [DOI] [PubMed] [Google Scholar]
- Roisman GI, & Fraley C (2006). The limits of genetic influence: A behavior-genetic analysis of infant-caregiver relationship quality and temperament. Child Development, 77, 1656–1667. [DOI] [PubMed] [Google Scholar]
- Salekin RT (2002). Psychopathy and therapeutic pessimism: Clinical lore or clinical reality? Clinical Psychology Review, 22, 79–112. [DOI] [PubMed] [Google Scholar]
- Salekin RT, Chen DR, Sellbom M, Lester WS, & MacDougall E (2014). Examining the factor structure and convergent and discriminant validity of the Levenson Self-Report Psychopathy Scale: Is the two-factor model the best fitting model? Personality Disorders: Theory, Research, and Treatment, 5, 289–304. doi: 10.1037/per0000073 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Svetlova M, Nichols SR, & Brownell CA (2010). Toddlers’ prosocial behavior: From instrumental to empathic to altruistic helping. Child development, 81, 1814–1827. doi: 10.1111/j.1467-8624.2010.01512.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vachon DD, Lynam DR, & Johnson JA (2014). The (non)relation between empathy and aggression: Surprising results from a meta-analysis. Psychological Bulletin, 140, 751–773. doi: 10.1037/a0035236 [DOI] [PubMed] [Google Scholar]
- Vaish A, Carpenter M, & Tomasello M (2009). Sympathy through affective perspective taking and its relation to prosocial behavior in toddlers. Developmental Psychology, 45, 534–543. doi: 10.1037/a0014322 [DOI] [PubMed] [Google Scholar]
- Viding E (2004). Annotation: Understanding the development of psychopathy. Journal of Child Psychology and Psychiatry, 45, 1329–1337. doi: 10.1111/j.1469-7610.2004.00323.x [DOI] [PubMed] [Google Scholar]
- Viding E, & McCrory EJ (2012). Genetic and neurocognitive contributions to the development of psychopathy. Development and Psychopathology, 24, 969–983. doi: 10.1017/S095457941200048X [DOI] [PubMed] [Google Scholar]
- Waller R, Dishion TJ, Shaw DS, Gardner F, Wilson MN, & Hyde LW (2016). Does early childhood callous-unemotional behavior uniquely predict behavior problems or callous-unemotional behavior in late childhood? Developmental Psychology, 52, 1805–1819. doi: 10.1037/dev0000165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller R, Gardner F, & Hyde LW (2013). What are the associations between parenting, callous-unemotional traits, and antisocial behavior in youth? A systematic review of evidence. Clinical Psychology Review, 33, 593–608. doi: 10.1016/j.cpr.2013.03.001 [DOI] [PubMed] [Google Scholar]
- Waller R, Gardner F, Hyde LW, Shaw DS, Dishion TJ, & Wilson MN (2012). Do harsh and positive parenting predict parent reports of deceitful-callous behavior in early childhood? Journal of Child Psychology and Psychiatry, 53, 946–953. doi: 10.1111/j.1469-7610.2012.02550.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller R, & Hyde LW (2017). Callous-unemotional behaviors in early childhood: Measurement, meaning, and the influence of parenting. Child Development Perspectives, 11, 120–126. doi: 10.1111/cdep.12222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller R, Hyde LW, Klump KL, & Burt SA (2018). Parenting is an environmental predictor of callous-unemotional traits and aggression: A monozygotic twin differences study. Journal of the American Academy of Child and Adolescent Psychiatry, 57, 955–963. doi: 10.1016/j.jaac.2018.07.882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller R, Shaw DS, Neiderhiser JM, Ganiban JM, Natsuaki MN, Reiss D, Trentacosta CJ, Leve LD, & Hyde LW (2017). Toward an understanding of the role of the environment in the development of early callous behavior. Journal of Personality, 85, 90–103. doi: 10.1111/jopy.12221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Bernstein MD, Mazzant JR, Willoughby MT, Haas SM, Coles EK, & Pelham WE (2016). A case study examining fixed versus randomized criteria for treating a child with conduct problems and callous-unemotional traits. Evidence-based Practice in Child and Adolescent Mental Health, 1, 73–85. doi: 10.1080/23794925.2016.1227946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waschbusch DA, Willoughby MT, Haas SM, Ridenour T, Helseth S, Crum KI, Altszuler AR, Ross JM, Coles EK, & Pelham WE (in press). Effects of behavioral treatment modified to fit children with conduct problems and callous-unemotional (CU) traits. Journal of Clinical Child and Adolescent Psychology. doi: 10.1080/15374416.2019.1614000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiler BL, & Widom CS (1996). Psychopathy and violent behaviour in abused and neglected young adults. Criminal Behavior and Mental Health, 6, 253–271. [Google Scholar]
- Zahn-Waxler C, & Radke-Yarrow M (1990). The origins of empathic concern. Motivation and Emotion, 14, 107–130. [Google Scholar]
- Zahn-Waxler C, Radke-Yarrow M, & King RA (1979). Child rearing and children’s prosocial initiations toward victims of distress. Child Development, 50, 319–330. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Radke-Yarrow M, Wagner E, & Chapman M (1992). Development of concern for others. Developmental Psychology, 28, 126–136. [Google Scholar]
- Zahn-Waxler C, Robinson JL, & Emde RN (1992). The development of empathy in twins. Developmental Psychology, 28, 1038–1047. [Google Scholar]
- Zahn-Waxler C, Schoen A, & Decety J (2018). An interdisciplinary perspective on the origins of concern for others: Contributions from psychology, neuroscience, philosophy, and sociology In Roughly Neil and Schramme Thomas, (Eds.), Forms of fellow feeling: Empathy, sympathy, concern and moral agency, (pp. 184–215). Cambridge, UK: Cambridge University Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.