Abstract
Objective
The purpose of the current study was to investigate the unique effects of a commonly used skill incorporated into treatment packages for borderline personality disorder (BPD), countering emotion-driven behavioral urges.
Method
Individuals with BPD (N = 8) participated in a single-case experimental design (SCED), specifically a multiple baseline, in which they were randomly assigned to complete a baseline assessment-only phase of two or four weeks. Participants then received four sessions of the Countering Emotional Behaviors module from the Unified Protocol (UP), followed by a four-week follow-up phase. Throughout the duration of the study, daily data capture was employed to assess real-time changes in the frequency of emotionally-avoidant behaviors in response to emotional experiences. Symptoms of BPD, depression, and anxiety were also assessed.
Results
By follow-up, the majority of patients demonstrated a meaningful reduction (per SCED guidelines for evaluating improvements) in their use of avoidant behaviors. There was also preliminary evidence that encouraging participants to act counter to avoidant urges is associated with decreases in BPD, depression, and anxiety symptoms, as well as negative affectivity.
Conclusions
The Countering Emotional Behaviors skill from the UP indeed engages its putative target of emotionally-avoidant behavioral coping, indicating it is an active ingredient in multi-component treatment packages for BPD with implications for downstream clinical endpoints such as BPD, depressive, and anxiety symptoms.
Keywords: Borderline Personality Disorder, Daily Diary, Emotion avoidance, Unified Protocol, Single Case Experimental Design
Borderline personality disorder (BPD) is a severe psychological condition marked by impairment in several areas of functioning. Symptoms associated with BPD include a pervasive pattern of emotion dysfunction (i.e., labile affect, anger), interpersonal distress (i.e., frantic attempts to avoid abandonment, relationship instability), behavioral difficulties (i.e., self-injurious behaviors, suicidality, and impulsive self-destructive behaviors), identity disturbance (i.e., unstable sense of self, chronic emptiness), and cognitive vulnerabilities (i.e., dissociation, transient paranoia in response to stress; American Psychiatric Association, 2013).
Given the complexity of BPD, most extant treatments for this disorder are long-term and intensive (Neacsiu & Linehan, 2014). Psychodynamic approaches, largely targeting interpersonal dysfunction, include Transference-Focused Therapy (Clarkin et al., 2001) and Mentalization-Based Therapy (Bateman & Fonagy, 2004), as well as General Psychiatric Management (which, in addition to psychodynamic psychotherapy, involves pharmacological treatment and case management; McMain et al., 2009). Additionally, cognitive/cognitive-behavioral approaches such as Schema-Focused Therapy (SFT; Young, Klosko, & Weishaar, 2006) and Dialectical Behavioral Therapy (DBT; Linehan, 1993; Linehan, 2015) have also been employed. However, because BPD is a heterogenous disorder and patients often present with less severe symptoms (Trull, Useda, Conforti, & Doan, 1997), less intensive interventions have also been evaluated; these include distinct treatments such as the Unified Protocol (UP; Barlow et al., 2018; Sauer-Zavala, Bentley, & Wilner, 2016), Systems Training for Emotional Predictability and Problem Solving (STEPPS; Black, Blum, Pfohl, & St. John, 2004), and internet-based psychoeducation (Zanarini, Conkey, Temes, & Fitzmaurice, 2018), as well as abbreviated or alternative delivery schemes (i.e., stepped care) of existing treatments (e.g., Laporte, Paris, Bergevin, Fraser & Cardin, 2018). Of these interventions, DBT has amassed the most empirical support and is associated with reduced non-suicidal self-injury, hospitalization, and anger, along with increased client retention and overall functioning (see: Kliem, Kröger, & Kosfelder, 2010).
In general, empirically supported treatment approaches for BPD consist of multiple treatment elements. For example, in its standard outpatient form (Linehan, 1993), patients in DBT are encouraged to attend weekly individual therapy sessions (with between-session phone-based skill coaching) and group skills training for at least one year. Within this treatment structure, patients learn skills related to four content modules: mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. Although component analyses suggests that skills training may be the most important element of DBT (Linehan et al., 2015) and that skill use is an active mechanism for change over the course of treatment for BPD (Neacsiu, Rizvi, & Linehan, 2010), these studies have not investigated the effects of each sub-skill contained within the four modules (e.g., the distress tolerance module alone includes 11 distinct skills; Linehan, 2015). As a result, it is difficult to isolate the components that are active agents of change in the treatment of BPD.
Interventions comprised only of active ingredients may be more potent, resulting in increasingly efficient improvements; however, when treatment packages are large, it can be difficult to know where to begin when isolating the effects each component. Focus on skills that are theoretically linked to core mechanisms maintaining symptoms may represent a useful starting point (Sauer-Zavala et al., 2017). Research on the processes underlying BPD symptoms suggest that emotion dysfunction is a core mechanism of BPD from which the other diagnostic features may manifest (Sanislow et al., 2002). Specifically, Linehan’s construct of emotional vulnerability, included as a risk factor in her biosocial model of BPD, is defined as being highly sensitive to emotion-provoking stimuli (i.e., a lower threshold for emotional responding), experiencing strong emotional responses, and taking a long time to return to baseline levels of arousal following a trigger (Linehan, 1993). Indeed, empirical studies have demonstrated greater levels of negative emotions in BPD compared to nonclinical controls and other personality disorders (Henry et al., 2001; Koenigsberg et al., 2002) and have linked this emotional intensity to severity of BPD symptoms (Yen, Zlotnick, & Costello, 2002).
Given the important role of negative emotionality in BPD pathology, treatment components that address this vulnerability may be particularly useful for symptom improvement. There is evidence to suggest that how one regulates intense affective states has important implications for the frequency of these emotional experiences (Sauer & Baer, 2009; Selby, Anestis, Bender, & Joiner, 2009; Wegner, Schneider, Carter, & White, 1987), as well as for symptom severity (Abramowitz, Tolin, & Street, 2001; Purdon, 1999). Emotion regulation refers to “monitoring, evaluating, and modifying emotional reactions, especially their intensity and temporal features,” (Thompson, 1994, p. 27). Although individuals with BPD appear to have a heightened ability to modulate these emotional qualities (Putnam & Silk, 2005), it is often through maladaptive behavioral responses (i.e., actions that provide short-term relief, yet lead to a greater likelihood of negative emotional states; Carpenter & Trull, 2012). For example, non-suicidal self-injury (NSSI), a commonly endorsed behavior in patients with BPD, is frequently used (successfully) to reduce negative internal states (e.g., Chapman, Gratz, & Brown, 2006), but prospectively predicts a greater propensity for negative emotionality (Burke, Hamilton, Abramson, & Alloy, 2015).
Moreover, there is ample evidence to suggest that many of the behavioral indicators of BPD (e.g., NSSI, binge eating, substance use, reckless sex, attempts to avoid abandonment) can be conceptualized as attempts to avoid strong emotional experiences (see: Sauer-Zavala & Barlow, 2014). Though these behaviors result in short-term relief, they have been shown to backfire in the long-term by paradoxically increasing the frequency and intensity of negative emotional experiences (Selby et al., 2009; Selby, Anestis, & Joiner, 2008). Asking patients to behave in ways that are counter to their emotionally-avoidant urges is a treatment element that may be particularly useful for reducing emotional dysfunction in BPD. Techniques that address emotionally-avoidant behavioral responding have been incorporated in extant multicomponent treatments for this disorder, including DBT (the opposite action skill) and the UP (the Countering Emotional Behaviors module), likely drawn from more basic emotion science suggesting a fundamental way to change emotional experiences is to alter the action-tendencies associated with them (Amir, Kuckertz, & Najmi, 2013; Izard, 1971, 1977). However, this skill has generally not been presented in isolation, making it difficult to draw conclusions regarding its effect on the frequency of emotionally-avoidant behaviors, negative affectivity, and BPD symptoms; notable exceptions include a laboratory-based paradigm comparing approach and avoidant behaviors on affect intensity in BPD patients (Sauer-Zavala, Wilner, Cassiello-Robbins, Saraff, & Pagan, 2018) and a treatment study specifically examining the effect of DBT opposite action on shame (Rizvi & Linehan, 2005).
Single-case experimental design (SCED), based on repeated measurement of one individual’s behavior across experimental conditions, is a cost-effect method for evaluating the ability of a given intervention to engage its putative target (Barlow, Nock & Hersen, 2009). Indeed, SCEDs represent the cornerstone of treatment development for behavioral interventions and are accepted as equally valid to nomothetic group comparisons for assessing treatment outcomes (Task Force on Promotion and Dissemination of Psychological Procedures, 1995). Unlike naturalistic and non-experimental case studies, SCEDs are based on stringent manipulations in which each patient serves as their own control, leading to strong internal validity. Replication of effects across individuals begins to establish external validity or generalizability (Barlow et al., 2009). SCED methods are able to isolate relationships between important individual characteristics and responses. Nomothetic designs, on the other hand, mask individual responses by averaging possibly important and differential responses to treatment across patients (Barlow et al., 2009). Given that BPD is a notoriously heterogeneous condition (Trull, Useda, Conforti, & Doan, 1997; Zimmerman & Coryell, 1989) and that, across interventions, there are many distinct treatment elements (i.e., skills) that have been applied to this disorder, SCED studies that can provide information about whether (and for whom) a specific therapeutic strategy engages the core processes that maintain symptoms are warranted. Thus, SCED may be particularly adept at determine active ingredients in BPD research, especially in a time and cost-efficient manner (Rizvi & Nock, 2008).
Present study
The primary goal of the present study was to explore the unique effect of the Countering Emotional Behaviors module from the UP (Barlow et al., 2018). Although the UP has been associated with large reductions in BPD symptoms when presented in its entirety (Sauer-Zavala, Bentley, & Wilner, 2016), the discrete effect of encouraging participants to act opposite to emotion-drive behavioral urges remains unclear. SCED methodology was used; participants each completed a baseline, assessment only phase that was either two or four weeks in duration, followed by four sessions of treatment, and a four-week follow-up phase. Daily questionnaires were employed to assess the frequency of emotionally-avoidant behaviors in response to emotional experiences as a function of study phase. We hypothesized that the frequency of maladaptive emotionally-avoidant behaviors would decrease only after the introduction of the study intervention, which discretely focused on promoting approach-oriented behavioral responses to strong emotions. Symptoms of BPD, depression, and anxiety were also assessed; although we did not anticipate clinical meaningful changes on these variables given the brevity of the intervention, we were interested in whether early improvements on symptoms could be detected for individuals who demonstrated decreased engagement in emotional behaviors.
Method
Participants
Individuals with BPD (N = 8) participated in the present study. Inclusion criteria consisted of the following: (a) Diagnostic and Statistical Manual (5th edition, DSM-5; American Psychiatric Association, 2013) diagnosis of BPD assessed via the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997); (b) willingness to maintain a stable dose of prescribed psychotropic medication throughout the study duration; (c) willingness to refrain from obtaining additional psychosocial treatment for the duration of the study; (d) fluency in English; and (e) access to a personal smartphone. In order to maximize generalizability, exclusion criteria were based solely on the well-being of the participant and consisted primarily of conditions that would require prioritization for immediate treatment. Specifically, these conditions were assessed via the Anxiety Disorders Interview Schedule (ADIS-5; Brown & Barlow, 2014) and included: (a) Current DSM-5 manic episode, schizophrenia, schizoaffective disorder, or organic mental disorder; (b) clear and current suicidal risk (intent); and (c) current or recent (within three months) history of drug dependence. Each of these participants completed all study procedures and their demographic and other baseline data are reported in Table 1.
Table 1.
Participant Characteristics
| Participant | Age | Sex | Race | Ethnicity | Baseline ZAN-BPD Score | Psychotropic Medication |
|---|---|---|---|---|---|---|
| 001 | 21 | F | A | NH | 13 | Antidepressant |
| 002 | - | M | A | NH | 15 | None |
| 003 | 19 | T | A | H | 20 | None |
| 004 | 22 | F | W/C | NH | 6 | None |
| 005 | 19 | F | A | NH | 15 | None |
| 006 | 24 | F | A | NH | 15 | None |
| 007 | 27 | M | B | NH | 12 | None |
| 008 | 19 | F | W/C | NH | 19 | None |
Note: F = female; M = male; T = transgender; A = Asian; W/C = White/Caucasian; B = Black/African American; H = Hispanic; NH = non-Hispanic; - = missing.
Participants were recruited from local treatment sites using IRB-approved flyers, via online postings (e.g., Craigslist, university jobs board), and by emailing flyers to individuals with BPD that had participated in other (non-treatment) studies conducted by our group. If interested, potential participants completed a brief telephone screening that included the McLean Screening Instrument for BPD (MSI-BPD; Zanarini et al., 2003), along with supplemental questions to assess exclusion criteria, and eligible individuals were then scheduled for an in-person appointment to obtain informed consent and confirm inclusion/exclusion with an in-depth diagnostic assessment (described below). Of the 22 individuals who completed an initial phone screen, 12 were excluded; seven individuals did not meet the MSI-BPD threshold of endorsing 7 of 10 items, three were lost to contact following an eligible screen, one individual was unwilling to discontinue her current psychotherapy, and one participant endorsed a recent (past 12 months) manic episode. The remaining 10 were scheduled for an in-person diagnostic assessment and 10 attended this appointment. Following the in-person assessment and consent procedures, two participants were withdrawn by study staff because they did not meet study inclusion/exclusion criteria, leaving eight eligible individuals.
Study Design
Single case experimental design (SCED), specifically a multiple baseline study (Barlow, Nock, & Hersen, 2009), was used to conduct this investigation; methods and results are presented in accordance with single-case reporting guidelines in behavioral interventions (SCRIBE; Tate et al., 2016). Participants were randomly assigned to a baseline length of two or four weeks. Then, all participants received four sessions of a Countering Emotional Behaviors intervention, followed by a four-week, assessment-only follow-up phase. The initial baseline served as a control condition to establish levels of negative affect and engagement in emotionally avoidant behaviors in the absence of treatment, and to potentially demonstrate that changes in these variables occurred when and only when the intervention was applied (regardless of randomly-assigned baseline length). This design allows causal inferences to be made and controls for many threats to internal validity, including the passage of time and repeated assessments. Since each participant acts as their own control, fewer participants are needed to demonstrate change as a result of the intervention (Kazdin, 2011). Additionally, replication of effects across participants provides preliminary evidence of generalizability and external validity (Barlow, Nock, & Hersen, 2009). All procedures were approved by our University’s Institutional Review Board and the study was registered with clinicaltrials.gov.
Study Assessment
Diagnostic Measures
In order to confirm study inclusion/exclusion criteria, participants attended a clinician-rated assessment session prior to starting the baseline phase. Study assessors were advanced doctoral students (AC, BW) who underwent rigorous reliability training. All diagnostic interviews were audio recorded and four tapes were rated by an additional clinician; agreement regarding study eligibly (yes/no) was high (Kappa = 1).
First, the BPD module of the SCID-II (First, Gibbon, Spitzer, Williams, & Benjamin, 1997) was administered to ensure participants indeed met criteria for BPD. The SCID-II is a semi-structured diagnostic interview used to determine the presence of personality disorders. It has demonstrated good psychometric properties and adequate convergent, discriminant, and predictive validity (e.g., Ryder, Costa, & Bagby, 2007). Additionally, modules from the ADIS-5 (Brown & Barlow, 2014) were used to assess study exclusion criteria (e.g., substance dependence, manic episode). The ADIS has also demonstrated excellent interrater reliability (Brown, Di Nardo, Lehman, & Campbell, 2001).
Daily Assessment
Frequency of emotional experiences and engagement in emotionally-avoidant behaviors were monitored continuously throughout all study phases using daily diary methods; this frequent data collection reduces recall bias associated with traditional self-report measures, augments ecological validity, and is ideal for obtaining information about sensitive behaviors (e.g., Shiffman, Stone, & Hufford, 2008). Patients also had the option to complete event-contingent entries (i.e., a self-initiated entry during the experience of a strong emotion). A structured series of questions was administered via a Qualtrics link provided daily by email or text message. Qualtrics is a secure online platform designed for research data collection. Participants were first asked how many strong emotions they had experienced since their last entry; if one or more emotional experiences was reported, they were then asked follow-up questions about each occurrence (e.g., type of emotions [anger, sadness, etc..], intensity of the emotions). Particularly germane to the present study, participants were instructed to indicate if their behavioral response to each emotion fell into one of the following categories1: 1) Purposefully tried to push the feeling away (e.g., distracted, used substances, engaged in self-injury, sought reassurance); 2) “Dug in” to the feeling (e.g., listened to angry music, vented, paced); and 3) Engaged in impulsive behavior (e.g., shopped, ate, used substances, lashed out). Given that participants completed this assessment during the baseline phase (prior to treatment wherein psychoeducation about emotionally avoidant behaviors was provided), efforts were made include many examples of behaviors that typically represent maladaptive attempts to dampen emotions. Participants were instructed to complete this survey once per day and were instructed to report on any emotional events that occurred since their last assessment. Examples of precipitating events included “I just really miss my boyfriend tonight,” “my brother was being a jerk”, and “my final project is due to tomorrow and I’m still not finished,” following which participants endorsed sadness, anger, and anxiety, respectively; in response to these events and emotions, participants indicated that they engaged in frequent texting (pushing away), vented to their mom (“dug in”), and binge ate (impulsivity).
Weekly Assessment
Participants completed a number of self-report measures weekly throughout all study phases (i.e., baseline, treatment, follow-up). Questionnaires were completed via Qualtrics; participants indicated whether they preferred to be prompted to complete questionnaires via text messages or email.
BPD symptoms were assessed with the self-report version of the Zanarini Rating Scale for BPD (ZAN-BPD; Zanarini, Weingeroff, Frankenburg, & Fitzmaurice, 2015), a continuous measure designed to capture change in BPD symptom severity over time. Items prompt respondents to rate the degree to which each of the nine DSM criteria for BPD applied to them during the previous week, using a five-point scale. In the validation sample, the internal consistency of these nine items was good (Cronbach’s alpha = 0.84), as was convergent validity between the interview and self‐report versions of this measure. Additionally, though same‐day test–retest reliability was high, the ZAN-BPD also demonstrated sensitivity to change in symptoms across a 7 – 10 day period.
Depressive symptoms were assessed with the Overall Depression Severity and Interference Scale (ODSIS; Bentley, Gallagher, Carl, & Barlow, 2014) and anxiety symptoms were measured with the Overall Anxiety Severity and Interference Scale (OASIS; Norman, Hami Cissell, Means-Christensen, & Stein, 2006). Both measures consist of five items that have demonstrated strong psychometric properties (Bentley et al., 2014; Norman et al., 2006).
The negative affect subscale of the brief version of Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) was used to assess the tendency to experience negative emotions during the past week. Respondents are presented with a list of 10 emotion words (e.g., distressed, upset, guilty, scared) and are asked to indicate the extent to which each feeling applied to them on a 5-point Likert Scale with anchors ranging from “very slightly or not at all” to “extremely.” This measure has also demonstrated strong psychometric properties (Watson et al., 1988).
Study Intervention
All participants attended four sessions of treatment using the Countering Emotional Behaviors module from the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2018); each session was 50 minutes in duration. Generally, sessions were conducted weekly, however a six-week treatment window was provided to allow for missed sessions that might occur for various reasons (e.g., illness, travel). This module focuses on identifying and changing patterns of behavioral and cognitive avoidance that, while serving to decrease emotional intensity in the short-term, maintain the frequency/intensity of emotional experiences in the long-term. Session 1 introduced the paradoxical consequences of emotional avoidance and patients were encouraged to identify various avoidant behaviors; for homework, they were asked to read the Countering Emotional Behavior chapter from the UP workbook and add to their working list of avoidant coping strategies. In Session 2, patients were asked to identify alternative behaviors to replace emotionally-avoidant coping with particular emphasis on recognizing the short- and long-term consequences of these new, approach-oriented responses. Specifically, therapists highlighted that new behaviors may increase uncomfortable emotions in the moment, but would reduce the likelihood of experiencing interfering emotions in the future. Finally, sessions 3 and 4 focused on upcoming emotion-eliciting events in order to proactively identify avoidant behavioral urges and generate a plan for alternative actions.
Treatment was provided by a licensed clinical psychologist (SSZ) and advanced doctoral students (CCR, JGW) who are all certified experts in the delivery of the UP. Treatment sessions were audio recorded and a subset (20%, n = 7) were selected at random and rated for therapist competence using a 5-point Likert type rating that accounted for fidelity to the protocol, along other important therapeutic elements (e.g., rapport, time management). Additionally, given our goal of isolating the unique effects of this module on the frequency of emotionally-avoidant behaviors, raters ensured that no disallowed interventions were included during sessions. Overall, average competence ratings were high (4.89 on a 5-point scale), though there was a single instance in which a non-UP intervention strategy was mentioned.
Data analytic plan
Analyses were conducted in accordance with established guidelines for SCED research and thus used a combination of visual inspection and statistical methods (Tate et al., 2016). Visual inspection is considered a rigorous approach to data analysis in SCED (Kazdin, 2011). For these analyses, the primary outcome variables (frequency of emotional experiences and avoidant behaviors) were first plotted graphically for each participant. Frequency of emotional experience refers to the number of discrete emotions endorsed each day via daily entries and frequency of emotionally-avoidant behaviors were established by summing instances in which participants indicated that they responded to their emotion with one of the behavioral categories listed in the daily assessment section. The primary outcome was the degree to which patients responded to strong emotions with avoidant behavioral coping, as evidenced by overlap of these variables. Overall, patients were expected to continue experiencing strong emotions; the goal of treatment was not to eliminate emotions. Thus, visual inspection was used to assess whether patients showed a reduction in the use of emotionally-avoidant behaviors as the study progressed, despite continued endorsement of strong emotions. Reduced overlap of these data points over the course of the study was considered evidence of the treatment effect. Prior to conducting these analyses, the second author (CCR) completed an online training course and established reliability in visual inspection analyses compared with expert raters (http://singlecase.org; Homer & Hoselton, 2012). To supplement visual inspection analyses, paired sample t-tests were used to examine group-level differences in the proportion of emotions to which patients responded with avoidant coping engagement across phases.
Weekly scores on measures of secondary outcomes were also plotted graphically and the level, mean, and slope of data during intervention and follow-up phases were compared against baseline using visual inspection. Significance of within participant change (from the baseline to the end of the intervention and follow-up phases) was evaluated by calculating a 95% confidence interval (CI) around observed change scores to determine reliability of changes (see: Au et al., 2017); Jacobson and Truax’s (1991) method was used for calculating standard error of the difference (Sdiff)2. SDs and internal consistency coefficients from the following psychometrics studies were used: Zanarini et al., 2015 (SD = 5.00, Cronbach’s α = .84); Bentley et al., 2014 (SD = 5.04, Cronbach’s α = .94); Norman et al., 2006 (SD = 3.05, Cronbach’s α = .80); Watson et al., 1988 (SD = 5.90, internal consistency = .87). The Sdiff for each outcome variable are as follows: ZAN-BPD Sdiff = 2.82, ODSIS Sdiff = 1.74, OASIS Sdiff = 1.92, PANAS-NA Sdiff = 3.00. For each measure, Sdiff was then multiplied by 1.96 to create a 95% confidence interval (CI) around each change score. When this 95% CI did not include zero, change was considered statistically significant. Group standardized mean difference scores were also calculated to estimate magnitude of change on these outcomes from baseline to each subsequent phase using a d-statistic developed for SCED studies (Shadish et al., 2014) and corresponding 95% CIs.
Results
Primary Outcomes: Engagement in Emotionally-Avoidant Behaviors
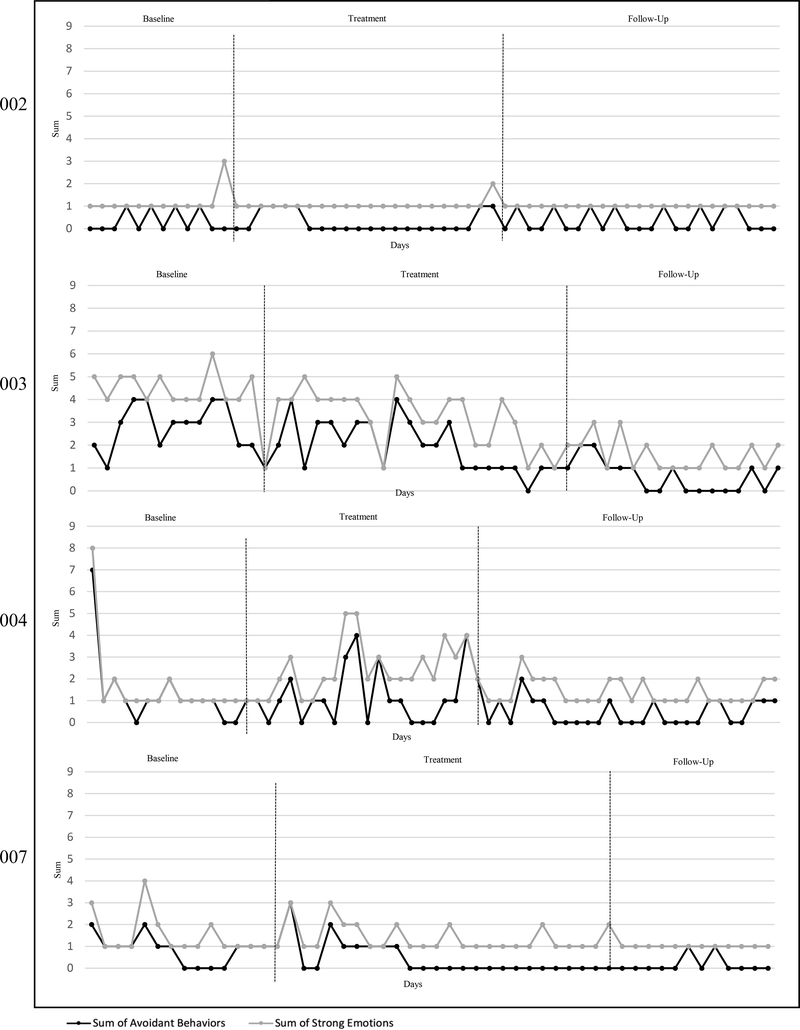
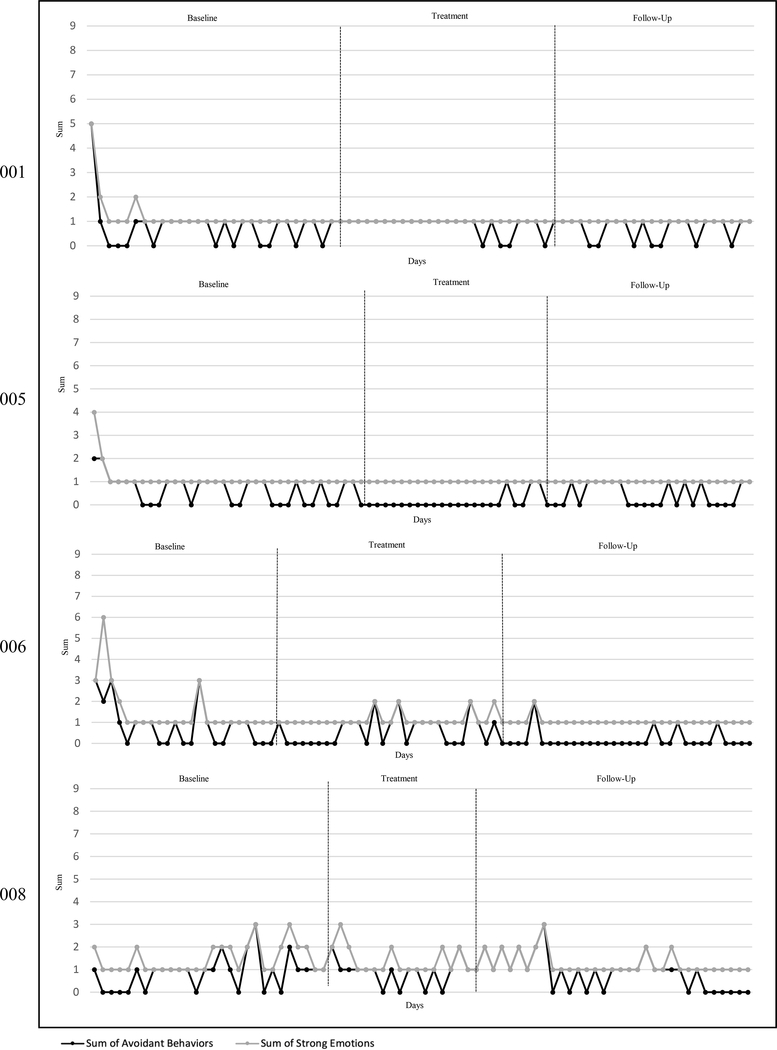
Overall, participants provided daily data on 86.1% of days in the study, resulting in 13.9% missing daily data overall. Across participants, the greatest amount of missing daily data occurred during the treatment phase (19.1%) and the least during baseline (4.3%). Between participants, missing daily data ranged from 1.6% (004) to 32.9% (003). Graphs of emotional experiences and avoidant behavioral responses are displayed in Figure 1.
Figure 1.
Proportion of daily emotional experiences to which patients responded with emotionally-avoidant behaviors. Gray lines indicate the number of strong emotions endorsed and black lines indicate the number of emotionally-avoidant behaviors the patient reported engaging in at each entry. Overlap of these lines suggests a patient responded to every emotion endorsed with an avoidant strategy. On the other hand, a black data point below a gray one, suggests the patient did not use attempt to behaviorally avoid the strong emotions reported at a given entry. The x axis for each graph refers to the absolute number of emotional experiences and avoidant behaviors, whereas the Y axis refers to days on which responses were recorded. Participants 002, 003, 004, and 007 were randomized to the two-week baseline condition. Participants 001, 005, 006, and 008 were randomized to the four-week baseline condition.
Six patients (001, 004, 005, 006, 007, and 008) showed a clear relationship between strong emotions and avoidant behavior use during the baseline phase. Of note, patient 002 indicated fairly low emotionally-avoidant coping throughout the study, making it difficult to observe meaningful improvement across phases.
During the treatment phase, four patients (004, 005, 006 and 007) showed a reduction in avoidant behavior use in response to strong emotions. During follow-up, one of these patients maintained their treatment gains (005), three patients (004, 006, 007) showed further improvement, and one additional patient demonstrated reductions compared to baseline (003). In contrast, one patient (001) evidenced increased engagement in emotional avoidance during the treatment phase, that returned to baseline levels during the follow-up period. The remaining patients (002, 008) did not show meaningful change in either direction. Given that the skills taught in treatment take time to learn and produce routine behavior change, it is likely that examining improvements during follow-up most accurately represents the effects of treatment. The fact that five (of eight) patients (62.5%) showed either improvement or maintenance of gains in follow-up suggests the intervention meaningfully reduced engagement in emotionally-avoidant behaviors in response to strong emotions. On average, patients engaged in emotionally-avoidant behaviors in response to 58.70% of the strong emotions they reported during the baseline phase. Consistent with the visual inspection analyses, there was a reduction in percent of the use of avoidant behaviors during the treatment phase (48.01%) and a further reduction during follow-up (40.32%). However, paired sample t-tests indicated the reductions in emotionally-avoidant behaviors from baseline to treatment (t(7) = 1.35, p = .22) and from baseline to follow-were not significant (t(7) = 2.03, p = .08).
Secondary Outcomes
Graphs of secondary outcomes can be viewed in Supplemental Figure 1. Change scores for baseline, treatment, and follow-up for each individual, along with their 95% confidence intervals, can be seen in Supplementary Table 1. With regard to BPD symptoms, visual inspection revealed that 5 of 8 participants displayed ZAN-BPD scores during the treatment phase that were largely non-overlapping (i.e., lower in level; 001, 005, 007) and/or steeper in (decreasing) slope (i.e., 002, 003, 007), in comparison with their baseline scores. By the follow-up phase, one additional patient (004) displayed scores that were non-overlapping with baseline levels of BPD symptoms, and 4 (of 5) patients (001, 002, 003, 007) maintained the gains they had made during the treatment phase. Of note, none of these improvements were large enough in magnitude to be considered statistically reliable. In contrast, non-responders (006, 008) displayed improvement during the baseline phase, along with statistically significant worsening during the treatment phase.
Depressive symptoms during the treatment phase were non-overlapping (002, 003, 004) and/or demonstrated a steeper negative slope (004, 007) for four patients and these improvements were all statistically reliable; these gains were largely maintained during the follow-up phase. One patient (006) improved significantly on depressive symptoms during baseline, but demonstrated significant worsening during treatment. With regard to anxiety symptoms, two patients’ graphs represented clinically-significant treatment effects (e.g., non-overlapping, steeper slope; 002, 007) that were statistically reliable and maintained during the follow-up phase. One additional patient (008) exhibited non-overlapping, statistically reliable reductions in anxiety symptoms during the follow-up phase.
Three patients (002, 005, 007) achieved clinical meaningful (i.e., differences in level and/or slope) and statistically reliable change on the tendency to experience negative emotions during the treatment phase; however, only one of these patients (007) maintained these improvements during the follow-up phase. One additional patient (008) demonstrated significant change during follow-up. Despite improvement on other outcomes during treatment, several patients showed statistically reliable increases in negative affect during treatment (003, 004) and/or follow-up (005, 006), compared to the baseline phase.
Finally, group descriptive statistics and effect sizes for secondary outcomes by study phase are presented in Table 2. Change was in the expected direction from the baseline phase to the treatment phase, with the most desirable scores on all self-report measures observed during the follow-up phase. Baseline to follow-up phase comparisons indicate small to moderate, significant effects on BPD symptoms, anxiety, depression, and negative affectivity in the sample as a whole.
Table 2.
Mean Summary Scores and Effect Sizes with 95% Confidence Intervals
| Baseline | Treatment | Follow-Up | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | M | SD | M | SD | dtx | 95% CI | M | SD | dfu | 95% CI |
| ZAN-BPD | 9.59 | 4.71 | 7.41 | 5.46 | 0.28* | (0.01, 0.57) | 7.12 | 5.78 | 0.35* | (0.07, 0.62) |
| ODSIS | 5.25 | 3.85 | 3.46 | 3.41 | 0.51* | (0.03, 0.98) | 3.29 | 4.12 | 0.49* | (0.05, 0.92) |
| OASIS | 6.94 | 4.23 | 6.59 | 4.15 | 0.14 | (−0.19, 0.46) | 5.10 | 3.67 | 0.49* | (0.10, 0.88) |
| PANAS-NA | 23.21 | 7.15 | 21.00 | 9.44 | 0.29 | (−0.07, 0.64) | 19.93 | 7.95 | 0.45* | (0.02, 0.89) |
Note: M = Mean of all observations within each phase; SD = Standard deviation; dtx = baseline vs treatment effect size; dfu = baseline vs follow-up effect size; CI = confidence interval
Discussion
The overarching goal of this study was to examine the effect of a discrete treatment skill, Countering Emotional Behaviors from the UP, on the frequency of emotionally-avoidant behaviors. During the baseline phase, six of the eight patients demonstrated a relationship between strong emotions and avoidant behavioral coping. During the treatment phase, four patients showed a clear reduction in the frequency of these behaviors, whereas one patient demonstrated increased use avoidant strategies and three patients did not evidence meaningful change. During the follow-up phase, one patient maintained treatment gains, three patients continued to reduce emotionally-avoidant behaviors, and one additional patient began to show improvements. Thus, by follow-up, the majority of patients (five out of eight) maintained gains or continued to improve; this suggests that it is possible for four sessions of treatment to produce meaningful change in use of avoidant behavioral coping among individuals with BPD.
Similar patterns emerged on secondary outcome variables. Five patients demonstrated improvements (per visual inspection) in BPD symptoms from baseline to the end of treatment, four of whom maintained these gains during follow-up. One additional patient improved only during follow-up. Statistically reliable changes between baseline and treatment and/or follow-up were seen for four patients on depressive symptoms and for two patients on anxiety symptoms. Finally, four patients demonstrated improvement on negative affect during either the treatment phase or follow-up phase; interestingly, several patients also demonstrated notable increases in negative affect despite improving on other outcome measures. This may be because countering behavioral avoidance involves abandoning strategies that have worked to reduce negative affect in the past in favor of strategies that may actually increase negative affect in the short-term; for some individuals, it may take more practice before alternative actions produce meaningful reductions in negative affect.
The present study utilized SCED and one advantage to this approach is the potential to provide idiographic explanations for treatment nonresponse. In the current study, several patients displayed outcome patterns that warrant explanation. For example, patient 001 actually engaged in a greater number of emotionally-avoidant behaviors during the treatment phase before making improvements during follow-up; sometimes, undergoing treatment makes patients more aware of their own behaviors, which can lead to an increase in reported instances of this phenomenon. This patient also started college classes during the treatment phase, which may have afforded more opportunities to engage in these behaviors given that much of their avoidant coping was related to schoolwork. Notably, although patient 006 showed a decrease in emotionally-avoidant behaviors use over the course of the study, many of their symptoms worsened. This could be due to additional stressors in their life, as they had broken up with a partner during the treatment phase. Finally, patient 008 showed only limited improvement on depression symptoms and negative affect during follow-up, but otherwise did not respond to treatment. Anecdotally, patient 008 was highly avoidant and expressed resistance to engage in the behavioral changes prescribed by the study treatment; for patients who are resistant, it may be helpful to provide other emotion regulation skills before introducing behavior change.
Overall, the results of the present study are well-situated within the larger literature supporting the tendency for individuals with BPD to attempt to avoid or suppress their frequently occurring negative affect (e.g., Selby, Anestis, & Joiner, 2008). Specifically, key features of BPD, including impulsivity and efforts to avoid abandonment, can be conceptualized as emotional avoidance (i.e., individuals are motivated to engage in these behaviors to decrease the intensity of an uncomfortable emotion). Empirically-supported treatments for emotional disorders, including the UP and DBT, include strategies aimed at facilitating behaviors that are counter to emotional urges; doing so is thought to be associated with decreased emotional avoidance and greater symptom reduction (see: Sauer-Zavala & Barlow, 2014; Sauer-Zavala et al., 2016, 2018).
These results lend empirical support to the idea that countering emotionally-avoidant behaviors may be a beneficial treatment skill for many individuals presenting with BPD. Extant treatments for this disorder, including DBT, are long-term and intensive to address the severe and sometimes life-threatening behavioral dysregulation that characterizes BPD. However, because BPD is a heterogeneous disorder and patients often present with less severe symptoms (Trull, Useda, Conforti, & Doan, 1997; Zimmerman & Coryell, 1989), less intensive interventions may be appropriate for individuals with lower-risk presentations of this disorder. Four sessions of a behavioral treatment focused on countering behavioral avoidance meaningfully reduced this phenomenon in the majority of patients in this study and produced a signal of early symptom change on BPD, depression, anxiety, and negative affectivity for some patients. Thus, this skill may be a promising component to include in potent, effective, and ultimately disseminable treatment packages for lower-risk BPD.
Additionally, it is worth noting that non-responders in the present study may have resulted from the fact that an intervention aimed at emotional avoidance/dysfunction may not be appropriate for all manifestations of BPD. For example, although some characteristic BPD behaviors may begin as emotional avoidance (i.e., substance use), other processes may maintain these behaviors over time (i.e., physiological addiction) and would render the present intervention less effective. Additionally, although BPD is strongly associated with negative affectivity, there is also evidence that this condition can also be accounted for, to a degree, by a higher-order externalizing factor (Eaton et al., 2011). Perhaps individuals who did not respond in the present study may be better served by interventions that also specifically address interpersonal dysfunction and impulsivity that is not accounted for by attempts to dampen emotion.
The present study should be considered in light of its limitations. First, our sample size was small, which may limit the generalizability of the findings. Of course, it must be noted that small samples are typical of SCEDs as the goal of these studies is to achieve strong internal validity and draw causal conclusions within individuals; moreover, a repeated pattern of results across participants suggests evidence of an effect that is likely generalizable. However, further replication is needed to confirm generalizability. Additionally, the treatment phase was relatively short and comprised of one module taken in isolation from a larger intervention. Despite having a follow-up phase, the ability to observe longer-term effects may have been impacted, and it is unclear whether additional therapeutic context preceding or following the module could have changed participants’ engagement or response to countering emotionally-avoidant behaviors; this is an area for further study. With regard to assessment, participants’ comorbid diagnoses were not formally measured, which may have limited abilities to draw conclusions related to overall psychopathological severity. Further, despite ensuring that participants were not in concurrent psychological treatments, we did not assess for previous therapeutic experiences that could have interacted with our observed outcomes. Similarly, we did not assess for the frequency of negative/stressful life events that could impact the frequency of negative emotions (i.e., a secondary outcome in the present study) regardless of the use of emotionally-avoidant coping. Additionally, our categories of emotionally-avoidant behaviors were developed to capture a wide range actions associated with several distinct emotions (e.g., anger, sadness, anxiety) that could be easily understood by patients across all phases of the study (including during baseline, prior to the receipt of psychoeducation around emotional avoidance); this approach may have oversimplified determinations of whether a behavior was maladaptive, as context was not considered. In terms of assessment procedures to characterize the use of emotional-avoidant behaviors, daily data capture increases the likelihood of respondent accuracy. However event-contingent responding (i.e., completing an entry during an emotional episode), as is done in ecological momentary assessment procedures, would have further enhanced our confidence in our data. While event-contingent responding was included in this study, no study patient completed an event-contingent entry. Finally, with regard to study design, lack of an active comparison condition makes it difficult to draw conclusions about the specificity of the UP’s Countering Emotional Behaviors module of the frequency of these action tendencies.
Overall, findings indicate that a single, four-session intervention of Countering Emotional Behaviors can be effective for reducing unhelpful behavioral avoidance, BPD symptoms, and, may be helpful for some individuals in reducing related symptoms of depression, anxiety and negative affect. It is promising that a brief, four-session intervention demonstrated reductions in symptoms and uptake of skill use amongst most participants particularly in light of the fact that extant treatments for BPD are long-term, and consist of multiple components. In order to continue to evaluate and isolate theoretically-informed “active” components of treatment to maximize cost-effectiveness and efficiency of intervention strategies, research should continue to isolate other skills in isolation, and results from the present study should be assessed in larger clinical trials.
Supplementary Material
Footnotes
These main categories for emotional behaviors were used across different types of emotions (e.g., anger, sadness, guilt); however, parenthetical examples of each category were tailored to correspond to the particular emotion experienced. For example, the examples for “dug into the feeling” for sadness were “isolated myself, cried, watched a sad movie,” whereas for anxiety they were “repeated checking, extra preparation for an event, sought reassurance.”
The resulting Sdiff represents the difference between scores (i.e., the change score) that would be expected by chance variation alone on a specific measure. For calculating Sdiff, it is possible to use the pre-treatment SD from the study sample, but given the small sample size of this study, using the SD and rxx from larger samples in published psychometrics studies yielded a more stringent and conservative Sdiff. For rxx, some studies have used the test-retest reliability coefficient, but using the internal consistency is especially recommended for clinical populations (Martinovich, Saunders, & Howard, 1996). We used internal consistency to calculate Sdiff in this study, since our change score intervals of interest do not match the test-retest intervals in most published studies, and test-retest reliability can be confounded with real change.
References
- Abramowitz JS, Tolin DF, & Street GP (2001). Paradoxical effects of thought suppression: A meta-analysis of controlled studies. Clinical Psychology Review, 21(5), 683–703. 10.1016/S0272-7358(00)00057-X [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (DSM-5) (5th edition). Arlington, VA: APA. [Google Scholar]
- American Psychiatric Association. (2013b). Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (5th ed.). Arlington, VA: APA. [Google Scholar]
- Amir N, Kuckertz JM, & Najmi S (2013). The effect of modifying automatic action tendencies on overt avoidance behaviors. Emotion, 13(3), 478–484. 10.1037/a0030443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au TM, Sauer-Zavala S, King MW, Petrocchi N, Barlow DH, & Litz BT (2017). Compassion-based therapy for trauma-related shame and posttraumatic stress: Initial evaluation using a multiple baseline design. Behavior Therapy, 48(2), 207–221. 10.1016/j.beth.2016.11.012 [DOI] [PubMed] [Google Scholar]
- Barlow DH, Nock MK, & Hersen M (2008). Single Case Experimental Designs: Strategies for Studying Behavior Change (3rd edition). Boston, MA: Pearson. [Google Scholar]
- Barlow DH, Sauer-Zavala S, Farchione TJ, Murray Latin H, Ellard KK, Bullis JR, … Cassiello-Robbins C (2018). Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders: Patient Workbook (2nd ed.). New York, NY: Oxford University Press. [Google Scholar]
- Bateman AW, & Fonagy P (2004). Mentalization-Based Treatment of Bpd. Journal of Personality Disorders; New York, 18(1), 36–51. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, & Barlow DH (2014). Development and validation of the Overall Depression Severity and Impairment Scale. Psychological Assessment, 26(3), 815–830. 10.1037/a0036216 [DOI] [PubMed] [Google Scholar]
- Black DW, Blum N, Pfohl B, & John DS (2004). The STEPPS group treatment program for outpatients with borderline personality disorder. Journal of Contemporary Psychotherapy, 34(3), 193–210. [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110(1), 49–58. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2014). Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5L): Client Interview Schedule (Lifetime version). New York, NY: Oxford University Press. [Google Scholar]
- Burke TA, Hamilton JL, Abramson LY, & Alloy LB (2015). Non-suicidal self-injury prospectively predicts interpersonal stressful life events and depressive symptoms among adolescent girls. Psychiatry Research, 228(3), 416–424. 10.1016/j.psychres.2015.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter RW, & Trull TJ (2012). Components of emotion dysregulation in borderline personality disorder: A Review. Current Psychiatry Reports, 15(1), 335 10.1007/s11920-012-0335-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy, 44(3), 371–394. 10.1016/j.brat.2005.03.005 [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Foelsch PA, Levy KN, Hull JW, Delaney JC, & Kernberg OF (2001). The Development of a Psychodynamic Treatment for Patients with Borderline Personality Disorder: A Preliminary Study of Behavioral Change. Journal of Personality Disorders, 15(6), 487–495. 10.1521/pedi.15.6.487.19190 [DOI] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, & Hasin DS (2011). Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine, 41(5), 1041–1050. 10.1017/S0033291710001662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB, & Benjamin LS (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Washington, D.C.: American Psychiatric Press. [Google Scholar]
- Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, & Siever LJ (2001). Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. Journal of Psychiatric Research, 35(6), 307–312. [DOI] [PubMed] [Google Scholar]
- Izard CE (1971). The Face of Emotion (1st ed.). New York, NY: Appleton-Century-Crofts. [Google Scholar]
- Izard CE (1977). Human Emotions (1st ed.). New York, NY: Springer. [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [DOI] [PubMed] [Google Scholar]
- Kazdin A (2011). Single-case research designs: Methods for clinical and applied settings (2nd ed.). New York, NY: Oxford University Press. [Google Scholar]
- Kliem S, Kröger C, & Kosfelder J (2010). Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling. Journal of Consulting and Clinical Psychology, 78(6), 936–951. 10.1037/a0021015 [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, … Siever LJ (2002). Characterizing affective instability in borderline personality disorder. The American Journal of Psychiatry, 159(5), 784–788. 10.1176/appi.ajp.159.5.784 [DOI] [PubMed] [Google Scholar]
- Laporte L, Paris J, Bergevin T, Fraser R, & Cardin JF (2018). Clinical outcomes of a stepped care program for borderline personality disorder. Personality and mental health, 12(3), 252–264. [DOI] [PubMed] [Google Scholar]
- Linehan M (1993). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: The Guildford Press. [Google Scholar]
- Linehan MM (2015). DBT Skills Training Manual, Second Edition (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, … Murray-Gregory AM (2015). Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiatry, 72(5), 475–482. 10.1001/jamapsychiatry.2014.3039 [DOI] [PubMed] [Google Scholar]
- Martinovich Z, Saunders S, & Howard K (1996). Some comments on “assessing clinical significance.” Psychotherapy Research, 6(2), 124–132. 10.1080/10503309612331331648 [DOI] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, & Streiner DL (2009). A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry, 166(12), 1365–1374. 10.1176/appi.ajp.2009.09010039 [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, & Linehan MM (2014). Borderline Personality Disorder. In Clinical handbook of psychological disorders: A step by step treatment manual (5th edition, pp. 394–400). New York, NY: Guildford Press. [Google Scholar]
- Neacsiu AD, Rizvi SL, & Linehan MM (2010). Dialectical behavior therapy skills use as a mediator and outcome of treatment for borderline personality disorder. Behaviour Research and Therapy, 48(9), 832–839. 10.1016/j.brat.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman SB, Hami Cissell S, Means-Christensen AJ, & Stein MB (2006). Development and validation of an Overall Anxiety Severity And Impairment Scale (OASIS). Depression and Anxiety, 23(4), 245–249. 10.1002/da.20182 [DOI] [PubMed] [Google Scholar]
- Purdon C (1999). Thought suppression and psychopathology. Behaviour Research and Therapy, 37(11), 1029–1054. [DOI] [PubMed] [Google Scholar]
- Putnam KM, & Silk KR (2005). Emotion dysregulation and the development of borderline personality disorder. Development and Psychopathology, 17(4), 899–925. 10.1017/S0954579405050431 [DOI] [PubMed] [Google Scholar]
- Rizvi SL, & Linehan MM (2005). The treatment of maladaptive shame in borderline personality disorder: A pilot study of “opposite action.” Cognitive and Behavioral Practice, 12(4), 437–447. 10.1016/S1077-7229(05)80071-9 [DOI] [Google Scholar]
- Rizvi SL, & Nock MK (2008). Single-case experimental designs for the evaluation of treatments for self-injurious and suicidal behaviors. Suicide and Life-Threatening Behavior, 38(5), 498–510. [DOI] [PubMed] [Google Scholar]
- Ryder AG, Costa PT, & Bagby RM (2007). Evaluation of the SCID-II personality disorder traits for DSM-IV: Coherence, discrimination, relations with general personality traits, and functional impairment. Journal of Personality Disorders, 21(6), 626–637. 10.1521/pedi.2007.21.6.626 [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, … McGlashan TH (2002). Confirmatory Factor Analysis of DSM-IV Criteria for Borderline Personality Disorder: Findings From the Collaborative Longitudinal Personality Disorders Study. American Journal of Psychiatry, 159(2), 284–290. 10.1176/appi.ajp.159.2.284 [DOI] [PubMed] [Google Scholar]
- Sauer SE, & Baer RA (2009). Responding to negative internal experience: Relationships between acceptance and change-based approaches and psychological adjustment. Journal of Psychopathology and Behavioral Assessment, 31(4), 378–386. 10.1007/s10862-009-9127-3 [DOI] [Google Scholar]
- Sauer-Zavala S, & Barlow DH (2014). The case for borderline personality disorder as an emotional Disorder: Implications for treatment. Clinical Psychology: Science and Practice, 21(2), 118–138. 10.1111/cpsp.12063 [DOI] [Google Scholar]
- Sauer-Zavala S, Bentley KH, & Wilner JG (2016). Transdiagnostic Treatment of Borderline Personality Disorder and Comorbid Disorders: A Clinical Replication Series. Journal of Personality Disorders; New York, 30(1), 35–51. http://dx.doi.org.ezproxy.bu.edu/101521pedi201529179 [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Gutner CA, Farchione TJ, Boettcher HT, Bullis JR, & Barlow DH (2017). Current definitions of “transdiagnostic” in treatment development: A search for consensus. Behavior Therapy, 48(1), 128–138. 10.1016/j.beth.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Wilner JG, Cassiello-Robbins C, Saraff P, & Pagan D (2018). Isolating the effect of opposite action in borderline personality disorder: A laboratory-based alternating treatment design. Behaviour Research and Therapy. 10.1016/j.brat.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, & Joiner TE Jr. (2009). An exploration of the emotional cascade model in borderline personality disorder. Journal of Abnormal Psychology, 118(2), 375–387. 10.1037/a0015711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, & Joiner TE (2008). Understanding the relationship between emotional and behavioral dysregulation: Emotional cascades. Behaviour Research and Therapy, 46(5), 593–611. 10.1016/j.brat.2008.02.002 [DOI] [PubMed] [Google Scholar]
- Shadish WR, Hedges LV, Pustejovsky JE, Boyajian JG, Sullivan KJ, Andrade A, & Barrientos JL (2014). A d-statistic for single-case designs that is equivalent to the usual between-groups d-statistic. Neuropsychological Rehabilitation, 24(3–4), 528–553. 10.1080/09602011.2013.819021 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Tate RL, Perdices M, Rosenkoetter U, Shadish W, Vohra S, Barlow DH, … Wilson B (2016). The Single-Case Reporting Guideline in BEhavioural Interventions (SCRIBE). Archives of Scientific Psychology, 46(1), 1–9. 10.1037/arc0000026 [DOI] [Google Scholar]
- Thompson RA (1994). Emotion Regulation: A Theme in Search of Definition. Monographs of the Society for Reesarch in Child Development, 59(2–3), 27–28. [PubMed] [Google Scholar]
- Trull TJ, Useda JD, Conforti K, & Doan B-T (1997). Borderline personality disorder features in nonclinical young ddults: Two-year outcome. Journal of Abnormal Psychology, 106(2), 307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, & White TL (1987). Paradoxical effects of thought suppression. Journal of Personality and Social Psychology, 53(1), 5–13. [DOI] [PubMed] [Google Scholar]
- Yen S, Zlotnick C, & Costello E (2002). Affect regulation in women with borderline personality disorder traits. The Journal of Nervous and Mental Disease, 190(10), 693–696. 10.1097/01.NMD.0000034744.11140.99 [DOI] [PubMed] [Google Scholar]
- Young JE, Klosko JS, & Weishaar ME (2006). Schema therapy: A practitioner’s guide. New York, NY. [Google Scholar]
- Zanarini MC, Conkey LC, Temes CM, & Fitzmaurice GM (2018). Randomized controlled trial of web-based psychoeducation for women with borderline personality disorder. The Journal of Clinical Psychiatry, 79(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Weingeroff JL, Frankenburg FR, & Fitzmaurice GM (2015). Development of the self-report version of the Zanarini Rating Scale for Borderline Personality Disorder. Personality and Mental Health, 9(4), 243–249. 10.1002/pmh.1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.