Abstract
Objectives:
To examine racial/ethnic differences in type of SSB most frequently consumed and in correlates of youth sugar-sweetened beverage (SSB) intake.
Methods:
Data were obtained from the National Health and Nutrition Examination Survey (NHANES), 2011–2016, for children and adolescents aged 5–17 years (n=6,507). The main outcome was SSB consumption (i.e., sodas, sweetened fruit drinks, nectars, sports and energy drinks, sweetened coffees and teas, enhanced waters). Mean and proportions of SSB intake were estimated accounting for complex sampling strategy and weighting. Multivariable regression models were developed for each race/ethnicity and age group.
Results:
Two-thirds of children and adolescents reported consuming SSB on a given day. Among consumers, mean SSB consumption was greatest for Black children and White adolescents and lowest for Asian American children and adolescents. The most popular type of SSB consumed was sweetened fruit drinks among children and soda among adolescents, except among White and Mexican American children for whom soda and Black adolescents for whom sweetened fruit drinks were most popular. Female sex and water intake were negatively associated with SSB consumption across most races/ethnicities. Screen time, dentist visits, nativity, and guardian education were associated with SSB intake among a subset of races/ethnicities.
Conclusions:
Associations between covariates and SSB intake as well as types of beverages preferred vary by race/ethnicity, as such chronic disease policies should not be ‘one size fits all’. Targeted interventions for specific groups of vulnerable youths hold promise for further reducing SSB consumption, including directing efforts towards reducing sweetened fruit drinks for Black children.
Keywords: dietary behaviors, racial disparities, children, adolescents
INTRODUCTION
Youth consumption of sugar-sweetened beverages (SSB) in the United States remains a major public health challenge, as SSB are among the leading sources of added sugars and calories in children’s diets.[1] Sugary drinks are associated with adverse health outcomes, including high blood pressure, increased waist-circumference, and overweight/obesity, [2–8] as well as long-term cardiometabolic and dental caries risk. [3, 9] Promisingly, SSB intake among adolescents and children has decreased over the past 2 decades, [10] likely due to the introduction of school-based policies[11–13] and intensified messaging around the health effects of SSB.[14–18] A systematic review of school food environment changes found that product-specific restrictions and standards on nutrients, calories, or portion sizes led to a 0.18 servings/day decrease in habitual intake.[13]
Previously, factors at multiple levels have been identified as determinants of consumption. Demographic characteristics, such as sex,[19] income,[20] and age,[21, 22] as well as parental factors, such as education,[20] have been studied. Health conditions and behaviors have also been associated with consumption, with higher consumption among those with poor oral health,[19, 23] higher BMIs,[24] and increased sedentary behavior.[25] Nativity has also been found to influence SSB consumption.[26, 27]
Despite overall reductions, racial/ethnic disparities persist in SSB consumption, with non-Hispanic Blacks consuming the most, and Asian Americans consuming the least,[20, 28, 29] though consumption patterns may differ in community-based or non-English-speaking samples. Yet, limited research has been conducted on the determinants of SSB consumption and preferred types of SSB within racial/ethnic minority groups, due to small sample sizes, lack of Asian American inclusion, or failure to stratify by race/ethnicity.[19, 28, 30–35] To our knowledge, only one paper has previously examined consumption patterns and associations by race/ethnicity among a sample of low-income youth from a single state.[19]
This study builds on prior research that has identified individual-level associations for children and adolescents of all racial/ethnic groups, and determine whether these associations exist within specific racial/ethnic groups.[19, 20] Further, it addresses gaps in the literature by using a US nationally representative sample to: 1) describe SSB consumption patterns by racial/ethnic subgroups among children and adolescents; and 2) determine the most popular types of SSB across race/ethnicities and 3) examine relationships between selected sociodemographic and behavioral characteristics and SSB intake by race/ethnicity subgroup.
PATIENTS AND METHODS
Study Design and Population
The National Health and Nutrition Examination Survey (NHANES) includes a series of 2-year health and nutrition surveys conducted by the National Center for Health Statistics (NCHS). NHANES is a stratified, multistage probability sample of the civilian noninstitutionalized population in the US. The technical details of the survey, including its content and operations, are publicly available (https://www.cdc.gov/nchs/nhanes/index.htm). All participants provided written informed consent and the data collection procedures were approved by the NCHS Institutional / Ethics Review Board to ensure human subject protection and confidentiality.
For the present study, data from 2011–2016 were used, as Asian Americans were oversampled during this time period. Participants were included in the analyses if they were 5–17 years of age and had one reliable, complete 24-hour recall dietary interview.
Measures
Sociodemographic Characteristics and Covariates of Interest
Covariates of interest were determined based on a review of the extant literature that identified factors associated with SSB consumption at the individual and parental levels.
Sociodemographic characteristics were self-reported and collected through in-home interviews, including age, race/ethnicity [(Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian American, and non-Hispanic other (hereafter White, Black, Asian American, and other)], sex, poverty index ratio (≤130%, 130–185%, ≥185%), health insurance, last dental visit (within the past year, more than a year ago, never) and nativity (US- or foreign-born). To determine screen-time, responses to the following questions were used: “Over the past 30 days, on average how many hours per day did you sit and watch TV or videos?” and “Over the past 30 days, on average how many hours per day did you use a computer or play computer games outside of school?” Consistent with previous research,[36–38] responses were categorized into more or less than 2 hours a day for television and videos, and more or less than 1 hour a day for computer use. The following information on the household reference person (hereafter, guardian) was also of interest: nativity and education level (less than high school education, high school graduate or GED, some college or associates degree, college graduate).
Body mass index (BMI) was calculated using height and weight measurements from the physical examination. BMI-for-age growth charts were used to categorize the participants as underweight (<5% percentile), normal weight (5th-84th percentile), overweight (85th-94th percentile), or obese (≥95th percentile).
As we combined three waves of NHANES data, we also assessed a variable to represent the years during which the data were collected, corresponding to 2011–2012, 2013–2014, and 2015–2016.
Dietary Intake
Water and SSB consumption were estimated using the first day of dietary recall, collected during an in person interview where all food/beverage items that each participant consumed during the prior 24-hour period were recorded. Individual food and beverage items were linked with What We Eat in America (WWEIA) categories, which are released every 2 years to coincide with the release of NHANES data, to classify beverages.[39] To account for changes in the classification scheme over time, the coding of categories in the 2011–2012 and 2013–2014 waves were aligned with the most recently available 2015–2016 wave. The United States Department of Agriculture (USDA) Food Patterns Equivalents Database (FPED), which translates food and beverage items into the 37 USDA Food Patterns components, was used to obtain the values of added sugars for reported beverages.[40]
Bottled and tap water were aggregated to represent total water consumption, and dichotomized into greater or less than one serving (250 grams) per day.[41] SSB was defined as regular soda, sweetened bottled waters, sweetened fruit drinks, sports and energy drinks, sweetened coffees and teas, smoothies and grain drinks, and nutritional beverages. When investigating most common type of SSB consumed, smoothies and grain drinks, nutritional beverages, and sweetened bottled waters were aggregated into other SSB. For estimation of mean intake and the linear regression analyses, total SSB consumed per day was reported in grams; amounts also presented in approximate ounces by dividing the gram amount by 28.35.
Statistical Analyses
All analyses were stratified by race/ethnicity and age (children = 5–11 years; adolescents = 12–17 years). Means (M) and standard error (SE) for SSB consumption per day were estimated. Population proportions of SSB consumed by type and race/ethnicity were calculated by summing the grams consumed within each type for all participants within each racial/ethnic group and dividing the sum by the total grams of SSB consumed for all persons within that racial/ethnic group, multiplied by 100%. Frequencies of sociodemographic, behavioral, and guardian characteristics of youths were calculated and compared across racial/ethnic subgroups using the design-based F statistic, which accounts for sample weighting. Factors of interest were examined for missing data and collinearity. Variables with 5% or more missing values were not included in the study, including language spoken at home and fast food consumption. A variance inflation factor (VIF) of 5 was used as the cutoff to determine collinearity, and all variables in the final model had a VIF<5.
A two-step analysis was conducted to examine the relationships between the dependent variable, SSB consumption, and the factors of interest. First, to measure factors associated with consumption on a given day, a binary variable of any vs. none was used in multivariable logistic regression models. Next, to measure factors associated with varying amounts of SSB consumption among consumers, a continuous variable was used in multivariable linear regression models. Place of birth for child and guardian were not included in the models for Whites, Blacks, and Other races/ethnicities, due to the high proportions of youths who were US-born (95–98%). Regression coefficients (βs) representing differences in intake and corresponding 95% confidence intervals (CIs) were obtained.
Separate linear regression models were used to determine whether there was a change in mean SSB consumption among consumers or in the proportion of SSB consumers across the three waves. The binary outcome of non-consumers vs. consumers was scaled to 0 and 100 when assessing the changes in percent of consumers. Annual absolute change and corresponding p-values are presented. The trend in mean consumption for the Other racial/ethnic group should be interpreted with caution due to small sample sizes when disaggregated by year.
All analyses accounted for the complex sampling design and weighting. Three cycles of data (2011–2012, 2013–2014, 2015–2016) were combined. A 6-year dietary weight was generated using one-third of the 1-day dietary weight for each 2-year cycle. Analyses were conducted using svy commands in Stata, version 15 (StataCorp LLC, College Station, TX) and SAS-callable SUDAAN version 11. Data are not presented for the Other racial/ethnic group
A sensitivity analysis was conducted using 2 alternative definitions of SSB consumption to estimate intake. One definition was broader (i.e., regular soda, sweetened bottled waters, sweetened fruit juices and nectars, sports and energy drinks, sweetened coffees and teas, and flavored milk) and the other was narrower (i.e., regular soda, sweetened fruit juices and nectars, sports and energy drinks)[42] than the SSB definition used in the main analyses.
RESULTS
The study population characteristics for children and adolescents, respectively, are presented in Table 1.
Table 1.
Demographic characteristics of children ages 5–11 years, NHANES 2011–2016
| Mexican American | Other Hispanic | White | Black | Asian American | Other | p-value | Total | |
|---|---|---|---|---|---|---|---|---|
| % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | SE | % (SE) | |
| CHILDREN | N=802 | N=431 | N=977 | N=949 | N=293 | N=245 | N=3697 | |
| Male | 48.71 (2.71) | 56.92 (2.79) | 54.18 (2.41) | 51.44 (1.86) | 54.08 (3.92) | 45.94 (5.35) | 52.70 (1.51) | |
| ADOLESCENTS | N=598 | N=309 | N=721 | N=708 | N=323 | N=151 | N=2810 | |
| Male | 51.78 (2.41) | 49.68 (2.98) | 48.10 (2.16) | 51.39 (2.17) | 46.69 (4.96) | 51.72 (7.64) | 0.765 | 49.32 (1.38) |
In total, 6,507 individuals included in the sample: 3,697 children, ages 5–11 years, and 2,810 adolescents, ages 12–17 years. Overall, the vast majority of participants (96% children; 93% adolescents) and their guardians (78% children and adolescents) were US-born. Over one third of children (34%) and adolescents (37%) were overweight or obese, and most had health insurance (94% children, 92% adolescents). Asian American children were less likely to be US-born (77%) than Mexican American (94%), other Hispanic (92%), White (99%), Black (98%), and Other (96%). Among adolescents, Asian American (65%), Mexican American (81%), and other Hispanic (79%) participants were less likely to be US-born compared to White (99%), Black (97%), and Other (98%). Overweight and obesity were especially prevalent among Mexican Americans (47% children and adolescents), other Hispanics (42% children and adolescents), Blacks (35% children, 43% adolescents) and Others (37% children, 53% adolescents). Almost two-thirds of children (62%) and adolescents (61%) reported consuming any SSB on a given day.
SSB Intake among Consumers
Among children who reported consuming any SSB on a given day, mean consumption was 419.93 grams (approximately 15 ounces, SE=11.28). Results by racial/ethnic subgroup were that SSB intake was greatest among Black (M=444.63 grams [approximately 16 ounces], SE=19.03) and Other (M=455.95 grams [approximately 16 ounces], SE=45.53) children. Asian American youths consumed the least amount of SSB (M=297.17 grams [approximately 10 ounces]; SE=19.03) (Table 2).
Table 2.
Mean sugar-sweetened beverage consumption among children (ages 5–11) and adolescents (ages 12–17) NHANES 2011–2016
| Total SSB | Soft drinks | Fruit drinks | Sports and energy drinks | Nutritional beverages | Enhanced water | Sweetened teas and coffee | Smoothies and grain beverages | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Children | ||||||||||||||||
| Mexican American | 416.89 | 19.99 | 185.97 | 11.03 | 175.45 | 17.66 | 39.61 | 7.59 | 0.00 | . | 0.27 | 0.28 | 17.83 | 5.25 | 15.59 | 5.32 |
| Other Hispanic | 418.90 | 30.69 | 147.55 | 15.57 | 186.32 | 15.93 | 67.30 | 21.95 | 1.17 | 0.84 | 2.77 | 2.71 | 26.70 | 10.84 | 13.78 | 3.82 |
| White | 417.31 | 21.19 | 199.76 | 15.55 | 156.03 | 9.85 | 45.47 | 9.24 | 0.27 | 0.28 | 4.88 | 2.89 | 30.19 | 6.78 | 10.90 | 6.32 |
| Black | 444.63 | 14.62 | 133.10 | 11.61 | 278.42 | 15.85 | 29.16 | 6.75 | 0.41 | 0.31 | 0.74 | 0.61 | 22.28 | 5.45 | 2.80 | 1.38 |
| Asian American | 297.17 | 19.03 | 90.93 | 10.83 | 138.80 | 17.96 | 27.25 | 13.47 | 0.00 | . | 0.00 | . | 21.43 | 13.89 | 40.19 | 15.22 |
| Other | 455.95 | 45.53 | 137.17 | 25.10 | 243.25 | 36.81 | 55.76 | 23.05 | 0.00 | . | 3.90 | 2.96 | 14.94 | 6.58 | 15.86 | 4.44 |
| Total | 419.93 | 11.28 | 175.46 | 8.13 | 185.54 | 8.16 | 43.77 | 5.34 | 0.31 | 0.16 | 3.03 | 1.43 | 25.45 | 3.58 | 11.83 | 3.34 |
| Adolescent | ||||||||||||||||
| Mexican American | 522.21 | 25.89 | 310.68 | 20.92 | 121.41 | 14.66 | 59.63 | 10.79 | 1.45 | 1.19 | 12.48 | 11 | 45.45 | 14.05 | 16.55 | 4.78 |
| Other Hispanic | 565.19 | 29.9 | 326.14 | 30.23 | 164.21 | 29.21 | 39.58 | 9.99 | 0.34 | 0.34 | 11.04 | 8.45 | 42.38 | 12.19 | 23.88 | 6.85 |
| White | 647.31 | 33.75 | 359.96 | 30.88 | 132.9 | 20.65 | 126.12 | 23.84 | 4.23 | 3.59 | 11.84 | 3.35 | 72.61 | 14.67 | 12.25 | 4.85 |
| Black | 586.61 | 21.24 | 255.13 | 20.16 | 263 | 15.24 | 61.93 | 12.22 | 0.99 | 0.98 | 2.52 | 1.68 | 33.79 | 4.05 | 3.04 | 1.42 |
| Asian American | 381.67 | 26.46 | 243.25 | 31.97 | 102.75 | 19.51 | 9.99 | 4.46 | 0 | . | 0.8 | 0.61 | 57.13 | 21.44 | 24.89 | 7.91 |
| Other | 612.38 | 69.71 | 342.76 | 48.06 | 148.1 | 38.66 | 95.28 | 43.24 | 0 | . | 14.47 | 10.52 | 19.52 | 11.49 | 11.76 | 7.87 |
| Total | 600.73 | 18.82 | 327.86 | 17.25 | 154.42 | 10.97 | 92.88 | 13.65 | 2.64 | 1.94 | 10.08 | 2.66 | 57.07 | 8.46 | 12.85 | 2.71 |
Among adolescents, mean consumption was 600.73 grams [(approximately 21 ounces), SE=18.82]. White [M=647.31 (approximately 23 ounces); SE=33.75] and Other [M=612.38 (approximately 22 ounces); SE=69.71] adolescents consumed the greatest amount of SSB whereas Asian Americans consumed the least [M=381.67 (approximately 13 ounces), SE=26.46] (Table 2).
The greatest source of SSB intake for children of most races/ethnicities was sweetened fruit drinks, except for Mexican Americans and White youths, for whom soft drinks were the greatest source (Figure 1a). For Black children, sweetened fruit drinks comprised over half (58%) of total SSB consumption. Similarly, Black adolescents consumed more sweetened fruit drinks than any other type of SSB. In contrast, for adolescents of all other race/ethnicities, the greatest source of SSB intake was soft drinks (Figure 1b).
Figure 1.
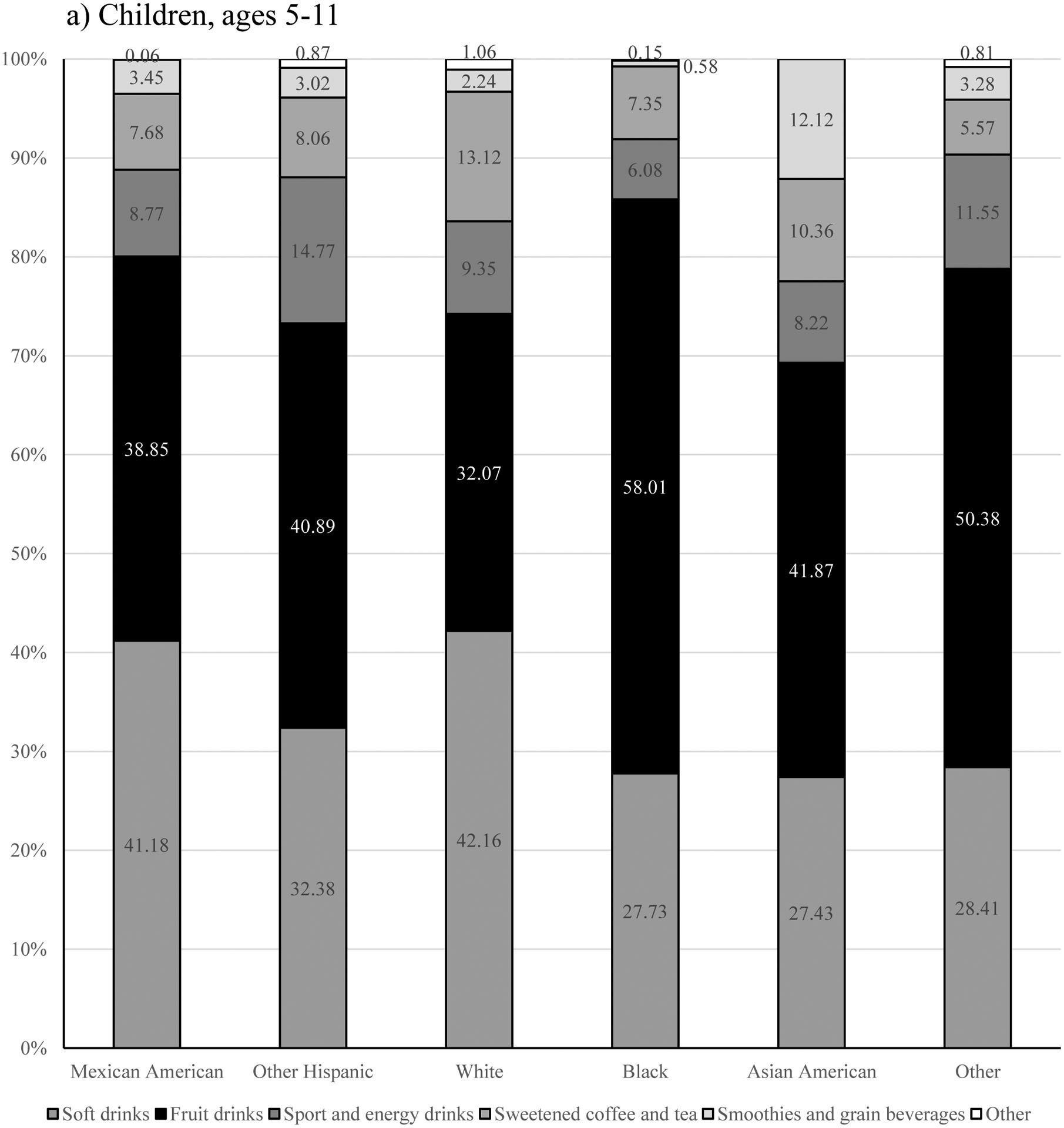
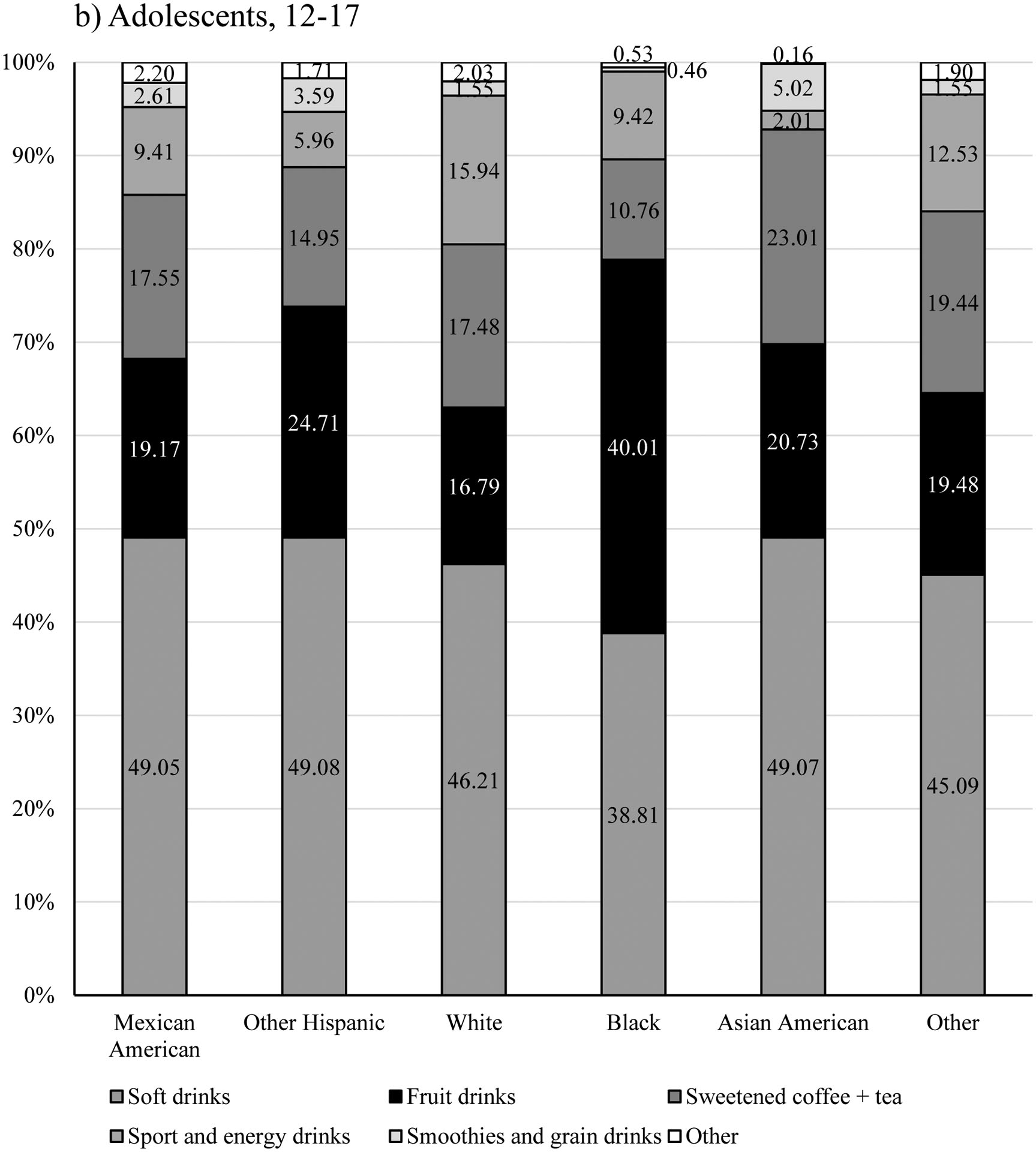
Proportion of SSB consumption by category and race/ethnicity, NHANES 2011–2016
a) Children, ages 5–11
b) Adolescents, ages 12–17
Factors Associated with Any SSB Consumption
Tables 3, 4, 5, and 6 present the multivariable logistic regression results of factors associated with SSB intake on a given day among children and adolescents by race/ethnicity.
Table 3.
Multivariable logistic regression models of factors associated with any sugar-sweetened beverage (SSB) intake among children, ages 5–11. by race/ethnicity, NHANES 2011–2016
| Asian American | Mexican-American | Other Hispanic | ||||
|---|---|---|---|---|---|---|
| aOR1 | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Age | 1.22 | [0.99,1.50] | 1.10* | [1.01,1.20] | 1.02 | [0.88,1.18] |
| Gender | 1.32 | [0.66,2.66] | 0.70* | [0.49,0.99] | 1.09 | [0.65,1.81] |
| Poverty ratio | ||||||
| ≤ 130% | REF | REF | REF | |||
| >130% and <185% | 2.96 | [0.73,11.99] | 0.57 | [0.32,1.04] | 0.89 | [0.31,2.51] |
| ≥185% | 4.05* | [1.01,16.21] | 0.57 | [0.28,1.19] | 1.29 | [0.59,2.80] |
| BMI category | ||||||
| Normal weight | REF | REF | REF | |||
| Overweight | 0.91 | [0.34,2.38] | 1.37 | [0.90,2.09] | 1.69 | [0.74,3.91] |
| Obese | 0.94 | [0.27,3.23] | 1.37 | [0.82,2.30] | 0.91 | [0.40,2.08] |
| Drink >1 cup of water/day | 0.93 | [0.53,1.61] | 0.47** | [0.30,0.73] | 0.54 | [0.27,1.07] |
| TV screen time >2 hours/day | 1.88 | [0.90,3.95] | 1.85* | [1.14,3.00] | 2.95** | [1.43,6.10] |
| Computer screen time >1 hour/day | 0.78 | [0.39,1.57] | 0.64 | [0.38,1.10] | 0.97 | [0.50,1.88] |
| Youth foreign-born | 0.87 | [0.29,2.56] | 0.41 | [0.14,1.16] | 0.97 | [0.35,2.67] |
| Health insurance | 1.80 | [0.23,14.08] | 0.66 | [0.30,1.46] | 2.02 | [0.66,6.22] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 1.13 | [0.32,3.93] | 0.85 | [0.45,1.59] | 1.96 | [0.77,5.00] |
| Never | 2.21 | [0.35,13.75] | 0.48 | [0.11,2.07] | 1.41 | [0.36,5.55] |
| Guardian education | ||||||
| Less than high school | REF | REF | REF | |||
| High school grad/GED or equivalent | 0.82 | [0.26,2.57] | 0.92 | [0.54,1.55] | 0.91 | [0.38,2.16] |
| Some college or AA degree | 0.67 | [0.11,4.14] | 0.97 | [0.55,1.74] | 0.82 | [0.37,1.85] |
| College graduate or above | 0.47 | [0.13,1.71] | 2.50 | [0.98,6.41] | 0.75 | [0.28,2.04] |
| Guardian foreign-born | 0.45 | [0.18,1.13] | 1.15 | [0.83,1.59] | 1.32 | [0.63,2.79] |
p < 0.05,
p < 0.01,
p < 0.001
Table 4.
Multivariable logistic regression models of factors associated with any sugar-sweetened beverage (SSB) intake among children, ages 5–11, by race/ethnicity, NHANES 2011–2016
| White | Black | Other | ||||
|---|---|---|---|---|---|---|
| aOR1 | 95% CI | aOR1 | 95% CI | aOR1 | 95% CI | |
| Age | 1.11* | [1.00,1.23] | 1.07 | [0.99,1.17] | 1.09 | [0.90,1.32] |
| Gender | 0.71* | [0.51,0.97] | 1.02 | [0.73,1.42] | 0.84 | [0.44,1.59] |
| Poverty ratio | ||||||
| ≤130% | REF | REF | REF | |||
| >130% and <185% | 0.73 | [0.39,1.36] | 0.81 | [0.39,1.67] | 2.35 | [0.78,7.08] |
| >=185% | 0.69 | [0.43,1.11] | 0.81 | [0.51,1.28] | 2.40* | [1.08,5.32] |
| BMI category | ||||||
| Normal weight | REF | REF | REF | |||
| Overweight | 1.42 | [0.78,2.57] | 0.68 | [0.43,1.07] | 0.41 | [0.13,1.27] |
| Obese | 1.14 | [0.66,1.98] | 0.99 | [0.59,1.67] | 1.30 | [0.39,4.30] |
| Drink >1 cup of water/day | 0.59* | [0.38,0.91] | 0.44*** | [0.32,0.62] | 0.37* | [0.17,0.80] |
| TV screen time >2 hours/day | 1.16 | [0.74,1.82] | 0.95 | [0.55,1.64] | 0.59 | [0.24,1.45] |
| Computer screen time >1 hour/day | 1.40 | [0.92,2.13] | 1.21 | [0.77,1.91] | 2.08 | [0.82,5.29] |
| Health insurance | 0.98 | [0.31,3.16] | 1.70 | [0.60,4.85] | 1.24 | [0.23,6.75] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 0.61 | [0.32,1.18] | 0.82 | [0.38,1.81] | 2.05 | [0.61,6.85] |
| Never | 0.65 | [0.30,1.42] | 1.15 | [0.30,4.39] | 0.53 | [0.05,5.04] |
| Guardian education | ||||||
| Less than high school | REF | REF | REF | |||
| High school grad/GED or equivalent | 1.02 | [0.58,1.79] | 1.05 | [0.53,2.08] | 0.48 | [0.06,3.88] |
| Some college or AA degree | 1.08 | [0.58,2.02] | 1.44 | [0.89,2.34] | 0.64 | [0.09,4.39] |
| College graduate or above | 0.97 | [0.47,1.98] | 0.94 | [0.53,1.67] | 0.30 | [0.04,2.12] |
p < 0.05,
p < 0.01,
p < 0.001
Table 5.
Multivariable logistic regression models of factors associated with any sugar-sweetened beverage (SSB) intake among adolescents, ages 12–17. by race/ethnicity, NHANES 2011–2016
| Asian American | Mexican-American | Other Hispanic | ||||
|---|---|---|---|---|---|---|
| aOR1 | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Age | 0.96 | [0.78,1.18] | 1.16 | [0.97,1.40] | 0.92 | [0.76,1.10] |
| Gender | 0.74 | [0.39,1.41] | 0.84 | [0.53,1.34] | 0.96 | [0.48,1.95] |
| Poverty ratio | ||||||
| ≤130% | REF | REF | REF | |||
| >130% and <185% | 2.96 | [0.73,11.99] | 0.57 | [0.32,1.04] | 0.89 | [0.31,2.51] |
| ≥185% | 4.05* | [1.01,16.21] | 0.57 | [0.28,1.19] | 1.29 | [0.59,2.80] |
| BMI category | ||||||
| Normal weight | REF | REF | REF | |||
| Overweight | 1.71 | [0.56,5.24] | 0.89 | [0.50,1.57] | 0.77 | [0.28,2.08] |
| Obese | 2.05 | [0.54,7.81] | 0.83 | [0.45,1.53] | 1.06 | [0.41,2.72] |
| Drink >1 cup of water/day | 0.43* | [0.20,0.93] | 0.39** | [0.22,0.69] | 0.38* | [0.17,0.82] |
| TV screen time >2 hours/day | 1.11 | [0.53,2.36] | 1.75* | [1.07,2.88] | 0.87 | [0.43,1.75] |
| Computer screen time >1 hour/day | 0.37 | [0.13,1.03] | 0.92 | [0.57,1.49] | 1.16 | [0.55,2.44] |
| Youth foreign-born | 0.58 | [0.24,1.42] | 0.99 | [0.38,2.54] | 1.04 | [0.37,2.88] |
| Health insurance | 0.45 | [0.11,1.85] | 0.75 | [0.42,1.32] | 0.79 | [0.30,2.07] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 0.84 | [0.26,2.76] | 0.83 | [0.43,1.59] | 1.75 | [0.84,3.64] |
| Never | 25.62* | [1.20,545.36] | 0.71 | [0.16,3.27] | 1.00 | [1.00,1.00] |
| Guardian education | ||||||
| Less than high school | REF | REF | REF | |||
| High school grad/GED or equivalent | 0.41 | [0.16,1.07] | 0.63 | [0.28,1.40] | 0.64 | [0.25,1.64] |
| Some college or AA degree | 0.62 | [0.20,1.92] | 0.36** | [0.18,0.72] | 0.61 | [0.24,1.55] |
| College graduate or above | 0.66 | [0.26,1.64] | 0.29* | [0.09,0.94] | 0.87 | [0.26,2.89] |
| Guardian foreign-born | 0.57 | [0.19,1.75] | 0.54 | [0.26,1.12] | 0.96 | [0.46,1.97] |
Table 6.
Multivariable logistic regression models of factors associated with any sugar-sweetened beverage (SSB) intake among adolescent, ages 12–17, by race/ethnicity, NHANES 2011–2016
| White | Black | Other | ||||
|---|---|---|---|---|---|---|
| aOR1 | 95% CI | aOR1 | 95% CI | aOR1 | 95% CI | |
| Age | 0.99 | [0.90,1.10] | 1.10 | [0.96,1.25] | 0.90 | [0.65,1.22] |
| Gender | 0.71 | [0.49,1.05] | 0.60** | [0.43,0.83] | 1.00 | [0.36,2.79] |
| Poverty ratio | ||||||
| ≤130% | REF | REF | REF | |||
| >130% and <185% | 1.60 | [0.84,3.05] | 0.54 | [0.25,1.17] | 52.66*** | [8.89,311.86] |
| ≥185% | 1.30 | [0.69,2.42] | 0.58 | [0.31,1.10] | 1.57 | [0.47,5.27] |
| BMI category | ||||||
| Normal weight | REF | REF | REF | |||
| Overweight | 0.92 | [0.50,1.68] | 1.03 | [0.53,2.01] | 0.37 | [0.08,1.78] |
| Obese | 1.86* | [1.03,3.38] | 1.00 | [0.50,2.01] | 1.11 | [0.25,4.99] |
| Drink >1 cup of water/day | 0.59* | [0.37,0.93] | 0.57** | [0.39,0.81] | 0.91 | [0.17,4.76] |
| TV screen time >2 hours/day | 1.17 | [0.75,1.82] | 1.21 | [0.71,2.04] | 0.38* | [0.15,0.93] |
| Computer screen time >1 hour/day | 0.98 | [0.63,1.52] | 0.93 | [0.56,1.55] | 3.40 | [0.53,21.68] |
| Health insurance | 2.07 | [0.73,5.89] | 0.31 | [0.10,1.02] | 23.67** | [3.77,148.57] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 0.64 | [0.37,1.09] | 1.09 | [0.58,2.07] | 0.55 | [0.09,3.20] |
| Never | 3.06 | [0.15,64.12] | 1.43 | [0.20,10.33] | 1.00 | [1.00,1.00] |
| Guardian education | ||||||
| Less than high school | REF | REF | REF | |||
| High schoolgrad/GED orequivalent | 0.76 | [0.37,1.57] | 0.74 | [0.39,1.41] | 9.80** | [1.88,51.03] |
| Some college or AA degree | 0.81 | [0.40,1.64] | 0.72 | [0.36,1.45] | 14.81*** | [3.18,69.02] |
| College graduate or Above | 0.68 | [0.30,1.57] | 0.72 | [0.30,1.72] | 3.87 | [0.54,27.78] |
Among children (Tables 3 and 4), water consumption was associated with lower odds of SSB consumption among Mexican American (aOR 0.47; 95% CI 0.30, 0.73), White (aOR 0.59; 95% CI 0.38, 0.91), and Black (aOR 0.44; 95% CI 0.32, 0.62) children. Asian American (aOR 4.05; 95% CI 1.01, 16.21) and Other (aOR 4.05; 95% CI 1.08, 5.32) children who lived in households above 185% of the poverty line had increased odds of consuming any SSB on a given day. For Mexican American and White children, older children (Mexican American - aOR 1.10; 95% CI 1.01, 1.20; White - aOR 0.71; 95% CI 0.51, 0.97) and males (Mexican American - aOR 0.70; 95% CI 0.49, 0.99; White - aOR 0.71; 95% CI 0.51, 0.97) had increased likelihood of SSB consumption. Increased screen time was associated with greater likelihood of SSB consumption among Mexican American (aOR 1.85; 95% CI 1.14, 3.00) and other Hispanic (aOR 2.95; 95% CI 1.43, 6.10) children.
Among adolescents (Tables 5 and 6), water consumption was associated with decreased odds of consuming SSB for most race/ethnicities: Asian American (aOR 0.43; 95% CI 0.20, 0.93), Mexican American (aOR 0.39; 95% CI 0.22, 0.69), other Hispanic (aOR 0.38; 95% CI 0.17, 0.82), White (aOR 0.59; 95% CI 0.37, 0.93), and Black (aOR 0.57; 95% CI 0.39, 0.81) adolescents. Asian American adolescents who lived in households above 185% of the poverty line (aOR 4.05; 95% CI 1.01, 16.21) and had never had a dental visit (aOR 25.62; 95% CI 1.20, 545.36) were more likely to consume SSB. Among Mexican American adolescents, the more education their guardian had the less likely adolescents were to consume SSB (some college: aOR 0.36; 95% CI 0.18, 0.72; college graduate: aOR 0.29; 95% CI 0.09, 0.94), whereas the more screen time they had, the more likely they were to consume SSB (aOR 1.75; 1.07, 2.99). Obesity was associated with increased odds of consuming SSB among White adolescents (aOR 1.86; 95% CI 1.03, 3.38), and females were less likely to consume SSB among Black adolescents (aOR 0.60; 95% CI 0.43, 0.83).
Sample Restricted to SSB Drinkers
Tables 7, 8, 9, and 10 present multivariable linear regression results of factors associated with SSB consumption among children and adolescents who consumed SSB on a given day.
Table 7.
Multilevel linear regression models among children, ages 5–11, who consumed sugar-sweetened beverages (SSB) by race/ethnicity, NHANES 2011–2016
| Asian American | Mexican-American | Other Hispanic | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Age | 4.33 | [−20.76,29.41] | 21.42** | [6.69,36.14] | 5.60 | [−19.54,30.74] |
| Gender | −84.77* | [−160.52,−9.03] | −103.15** | [−165.50,−40.79] | −101.53 | [−218.87,15.81] |
| Poverty ratio | ||||||
| ≤130% | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| >130% and <185% | −66.60 | [−264.31,131.11] | −24.81 | [−156.86,107.24] | 145.09 | [−90.86,381.04] |
| ≥185% | −65.01 | [−175.64,45.62] | 61.70 | [−59.15,182.55] | 14.93 | [−175.62,205.48] |
| BMI category | ||||||
| Normal weight | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| Overweight | −5.73 | [−108.70,97.25] | −23.99 | [−97.06,49.08] | −21.56 | [−131.23,88.11] |
| Obese | 40.82 | [−141.27,222.92] | −10.17 | [−95.79,75.46] | 42.64 | [−66.57,151.85] |
| Drink >1 cup water/day | −115.86** | [−182.24,−49.49] | −42.01 | [−137.58,53.55] | −112.54 | [−225.79,0.71] |
| TV screen time >2 hours/day | 46.29 | [−46.91,139.50] | 105.25** | [33.02,177.47] | 77.89 | [−2.80,158.58] |
| Computer screen time >1 hour/day | 18.80 | [−90.25,127.85] | 62.85 | [−5.82,131.51] | −58.23 | [−227.41,110.94] |
| Youth foreign-born | 93.83 | [−10.77,198.43] | 152.94* | [17.02,288.86] | 52.87 | [−64.56,170.30] |
| Health insurance | −70.06 | [−253.44,113.33] | −34.40 | [−204.59,135.78] | 101.49 | [−19.77,222.74] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 10.23 | [−181.69,202.14] | 61.94 | [−73.16,197.03] | −85.11 | [−233.52,63.29] |
| Never | 125.87 | [−64.99,316.74] | −145.51 | [−320.40,29.38] | −12.19 | [−174.84,150.46] |
| Guardian education | ||||||
| Less than high school | REF | REF | REF | |||
| High school grad/GED or equivalent | 110.75 | [−0.91,222.42] | −73.63 | [−151.89,4.62] | 32.66 | [−81.51,146.83] |
| Some college or AA degree | 75.58 | [−59.68,210.84] | −7.06 | [−91.30,77.17] | 61.81 | [−50.17,173.78] |
| College graduate or above | 13.25 | [−96.18,122.68] | 20.14 | [−203.93,244.21] | −94.63 | [−292.28,103.02] |
| Guardian foreign-born | 35.82 | [−63.54,135.18] | −110.19** | [−187.98,−32.41] | −160.46*** | [−244.92,−76.00] |
p < 0.05,
p < 0.01,
p < 0.001
Table 8.
Multilevel linear regression models among children, ages 5–11, who consumed sugar-sweetened beverages (SSB) by race/ethnicity, NHANES 2011–2016
| Non-Hispanic White | Non-Hispanic Black | Other Races/Ethnicities | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Age | 26.60*** | [16.53,36.68] | 28.20** | [11.57,44.83] | 46.99** | [18.33,75.65] |
| Gender | −61.30 | [−132.62,10.02] | 25.85 | [−30.29,81.98] | −109.76 | [−225.64,6.12] |
| Poverty ratio | ||||||
| ≤130% | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| >130% and <185% | −36.37 | [−125.30,52.56] | 42.24 | [−35.13,119.61] | 52.12 | [−79.04,183.29] |
| ≥185% | −28.02 | [−104.78,48.75] | 24.80 | [−43.37,92.97] | −78.33 | [−267.57,110.90] |
| BMI category | ||||||
| Normal weight | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| Overweight | −119.46*** | [−166.68,−72.23] | −40.28 | [−111.17,30.62] | 130.08* | [13.56,246.59] |
| Obese | 45.18 | [−26.75,117.10] | 91.14 | [−24.74,207.02] | 117.96 | [−67.93,303.85] |
| Drink >1 cup water/day | −115.04*** | [−174.56,−55.53] | −53.86 | [−126.27,18.56] | −219.11*** | [−329.95,−108.27] |
| TV screen time >2 hours/day | 6.21 | [−63.02,75.43] | 51.87 | [−10.32,114.06] | 112.71 | [−7.27,232.69] |
| Computer screen time >1 hour/day | −36.44 | [−97.29,24.42] | 80.63* | [18.72,142.53] | −115.45 | [−279.83,48.94] |
| Health insurance | −57.19 | [−212.98,98.61] | 31.83 | [−102.01,165.68] | 161.81 | [−64.43,388.04] |
| Last dental visit | ||||||
| Within past year | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| More than a year ago | 129.81 | [−35.66,295.27] | −87.77 | [−178.91,3.38] | 216.52* | [4.12,428.92] |
| Never | 97.53 | [−114.81,309.88] | 40.43 | [−66.05,146.92] | 35.12 | [−125.96,196.20] |
| Guardian education | ||||||
| Less than high school | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| High school grad/GED or equivalent | −47.35 | [−174.61,79.92] | 9.06 | [−39.93,58.05] | −71.42 | [−213.59,70.74] |
| Some college or AA degree | −21.90 | [−138.88,95.09] | 31.55 | [−47.81,110.92] | 86.79 | [−69.31,242.90] |
| College graduate or above | −36.25 | [−160.04,87.55] | 16.36 | [−107.32,140.04] | 186.12 | [−48.27,420.50] |
Table 9.
Multilevel linear regression models among adolescents, ages 12–17, who consumed sugar-sweetened beverages (SSB) by race/ethnicity, NHANES 2011–2016
| Asian American | Mexican-American | Other Hispanic | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Age | −1.20 | [−26.46,24.05] | 10.49 | [−12.46,33.44] | 42.96* | [9.33,76.60] |
| Gender | −118.27* | [−225.46,−11.08] | −71.06 | [−184.35,42.23] | −93.62 | [−239.20,51.96] |
| Poverty ratio | ||||||
| <130% | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| >130% and <185% | 61.27 | [−57.07,179.61] | 67.00 | [−121.64,255.64] | 193.33 | [−7.44,394.11] |
| >185% | 19.14 | [−91.85,130.14] | −30.47 | [−156.00,95.05] | 71.33 | [−97.60,240.25] |
| BMI category | ||||||
| Normal weight | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| Overweight | −48.25 | [−174.86,78.35] | −10.59 | [−92.94,71.76] | −143.09 | [−289.96,3.77] |
| Obese | 46.87 | [−38.98,132.73] | 21.31 | [−115.95,158.58] | −149.11 | [−309.78,11.56] |
| Drink >1 cup water/day | −55.12 | [−166.69,56.45] | −99.36* | [−192.45,−6.26] | −59.31 | [−211.69,93.06] |
| TV screen time >2 hours/day | 72.39* | [4.18,140.59] | 80.06 | [−7.83,167.94] | 188.20* | [36.56,339.84] |
| Computer screen time >1 hour/day | 47.06 | [−16.40,110.51] | 46.13 | [−56.77,149.02] | −100.68 | [−296.04,94.68] |
| Youth foreign−born | 49.84 | [−30.29,129.96] | −41.77 | [−232.01,148.47] | 88.28 | [−145.99,322.55] |
| Health insurance | 22.75 | [−144.93,190.42] | 10.82 | [−112.26,133.90] | −41.66 | [−290.56,207.24] |
| Last dental visit | ||||||
| Within past year | REF | REF | REF | |||
| More than a year ago | 119.05 | [−51.95,290.05] | 125.03 | [−8.13,258.18] | −35.33 | [−217.62,146.96] |
| Never | −151.54* | [−268.24,−34.85] | 365.22 | [−43.66,774.11] | −112.19 | [−324.12,99.75] |
| Guardian education | ||||||
| Less than high school |
REF | REF | REF | |||
| High school grad/GED or equivalent |
−4.26 | [−237.41,228.89] | −77.52 | [−185.73,30.70] | −116.95 | [−241.27,7.38] |
| Some college or AA degree |
−6.53 | [−123.50,110.43] | 70.25 | [−82.15,222.64] | 84.67 | [−103.92,273.25] |
| College graduate or above |
−12.52 | [−119.89,94.84] | 354.42 | [−73.57,782.40] | 26.60 | [−159.38,212.58] |
| Guardian foreign−born | 203.85*** | [132.25,275.45] | 94.59 | [−39.08,228.27] | −101.51 | [−240.16,37.14] |
p < 0.05,
p < 0.01,
p < 0.001
Table 10.
Multilevel linear regression models among adolescents, ages 12–17, who consumed sugar-sweetened beverages (SSB) by race/ethnicity, NHANES 2011–2016
| Non-Hispanic White | Non-Hispanic Black | Other Races/Ethnicities | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Age | 60.52** | [24.35,96.70] | 24.87 | [−4.67,54.41] | 61.23* | [5.90,116.56] |
| Gender | −194.73** | [−315.67,−73.79] | −5.63 | [−122.52,111.27] | −194.83* | [−362.95,-26.71] |
| Poverty ratio | ||||||
| <130% | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| >130% and <185% | −162.97 | [−359.09,33.16] | 108.47 | [−50.24,267.17] | −56.02 | [−321.78,209.75] |
| >185% | −84.63 | [−273.79,104.53] | −15.28 | [−109.73,79.18] | 126.47 | [−104.02,356.96] |
| BMI category | ||||||
| Normal weight | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| Overweight | −137.92* | [−255.99,−19.84] | −84.24 | [−221.63,53.16] | −112.96 | [−402.23,176.31] |
| Obese | −100.09 | [−243.16,42.97] | −65.87 | [−158.65,26.90] | −10.49 | [−188.41,167.43] |
| Drink >1 cup water/day | −96.28 | [−344.92,152.36] | −138.95** | [−221.80,−56.11] | −28.34 | [−239.37,182.70] |
| TV screen time >2 hours/day | 76.17 | [−25.41,177.75] | 32.91 | [−73.74,139.55] | −76.17 | [−255.85,103.51] |
| Computer screen time >1 hour/day | −145.07** | [−247.99,−42.16] | −10.19 | [−142.76,122.39] | −10.78 | [−182.73,161.16] |
| Health insurance | −318.01 | [−649.99,13.96] | 102.31 | [−23.36,227.98] | 221.41 | [−121.24,564.06] |
| Last dental visit | ||||||
| Within past year | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| More than a year ago | −75.74 | [−252.16,100.68] | 111.49 | [−45.00,267.98] | −294.04*** | [−422.45,−165.63] |
| Never | −194.51 | [−447.29,58.27] | 453.16 | [−393.23,1299.54] | ||
| Guardian education | ||||||
| Less than high school |
0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] | 0.00 | [0.00,0.00] |
| High school grad/GED or equivalent |
82.59 | [−117.66,282.85] | −27.72 | [−149.61,94.17] | 70.69 | [−437.22,578.59] |
| Some college or AA degree |
65.73 | [−143.88,275.35] | −19.60 | [−143.52,104.31] | −18.31 | [−395.85,359.23] |
| College graduate or above |
30.62 | [−229.92,291.16] | −16.59 | [−171.61,138.43] | −222.82 | [−572.20,126.56] |
p < 0.05,
p < 0.01,
p < 0.001
Among children (Tables 7 and 8), Asian American (−84.77 grams; 95% CI −160.52, −9.03) and Mexican American (−103.15 grams; 95% CI −165.50, −40.79) females consumed less SSB than males on a given day. Older Mexican American (21.42 grams; 95% CI 6.69, 36.14), White (26.60 grams; 95% CI 16.53, 36.68), Black (11.57 grams; 95% CI 44.83), and Other (46.99 grams; 95% CI 18.33, 75.65) children consumed more SSB. Children who consumed at least one serving of water consumed less SSB among Asian Americans (−115.86 grams; 95% CI −182.24, −49.49), Whites (−115.04; 95% CI −174.56, −55.53), and Other races/ethnicities (−219.11 grams; 95% CI −329.95, −108.27). Among Mexican Americans (105.25 grams; 95% CI 33.02, 177.47) and Blacks (80.63 grams; 95% CI 18.72, 142.53), children who reported higher screen times consumed more SSB. Mexican American foreign-born children (152.94 grams; 95% CI 17.02, 288.86) consumed more SSB. Children who had a guardian who was foreign-born consumed more SSB (−110.19 grams; 95% CI −187.98, −32.41) among Mexican Americans (110.19 grams; 95% CI −187.98, −32.41) and other Hispanics (−160.46 grams; 95% CI −244.92, −76.00). Overweight White (−119.46 grams; 95% CI −166.68, −72.23) and Other (130.08 grams; 95% CI 13.56, 246.59) children consumed more SSB than normal weight children. Visiting the dentist more than a year ago compared to within the past year was associated with consuming more SSB among Other children (216.52 grams; 95% CI 4.12, 428.92).
Among adolescents (Tables 9 and 10), females consumed less SSB on a given day among Asian American (−118.27 grams; 95% CI −225.46, −11.08), White (−194.73 grams; 95% CI −315.67, −73.79), and Other (−194.83 grams; 95% CI −362.95, −26.71) adolescents. Among Asian Americans, adolescents who reported never visiting the dentist compared within the past year consumed less SSB (−151.54 grams; 95% CI −268.24, −34.85), whereas those who had a guardian who was foreign-born consumed more SSB (203.85 grams; 95% CI 132.25, 275.45). Adolescents who reported higher screen times consumed more SSB among Asian Americans (72.39 grams; 95% CI 4.18, 140.59) and other Hispanics (72.39 grams; 95% CI 4.18, 140.59), but less among Whites (−145.07 grams; 95% CI −247.99, −42.19). Mexican American (−99.36; 95% CI −192.45, −6.26) and Black (−138.95; 95% CI −221.80, −56.11) adolescents who consumed at least one serving of water consumed less SSB. Among White (60.52 grams; 95% CI 24.35, 96.70), other Hispanic (42.96 grams; 95% CI 9.33, 76.60), and Other (61.23 grams; 95% CI 5.90, 116.56) adolescents, older adolescents consumed more SSB. Overweight adolescents consumed less SSB than normal weight adolescents among Whites only (−137.92 grams; 95% CI −255.99, −19.84).
Trend in SSB Consumption
Over the three two-year cycles, overall, there was a significant decrease in the percent of children (Annual Absolute Change [AAC] −0.04; p=0.021) and adolescents (AAC −0.05; p=0.003) consuming any SSB on a given day (Figures 2a–b). Among children, this decline appeared to be driven by decreases in consumption among Mexican American children (AAC −0.07; p=0.015), given that the percent of SSB consumers did not significantly change over time for children or adolescents of other racial/ethnic groups. Among adolescents, this decline appeared to be driven by decreases in the percentage of White (AAC −0.07; p=0.030) and Other (AAC −0.15; p=0.017) adolescents consuming SSB. (Supplemental Table 1) There was a significant decrease in mean consumption over time among adolescents (AAC −59.22; p=0.017) but not among children (Figures 2c–d). There were significant declines in mean SSB consumption for Other Hispanic (AAC −82.42; p=0.022) and White adolescents (AAC −96.53; p=0.001), and Black children (AAC −32.20; p=0.012), but no significant trends for any other racial/ethnic group. (Supplemental Table 2)
Figure 2.
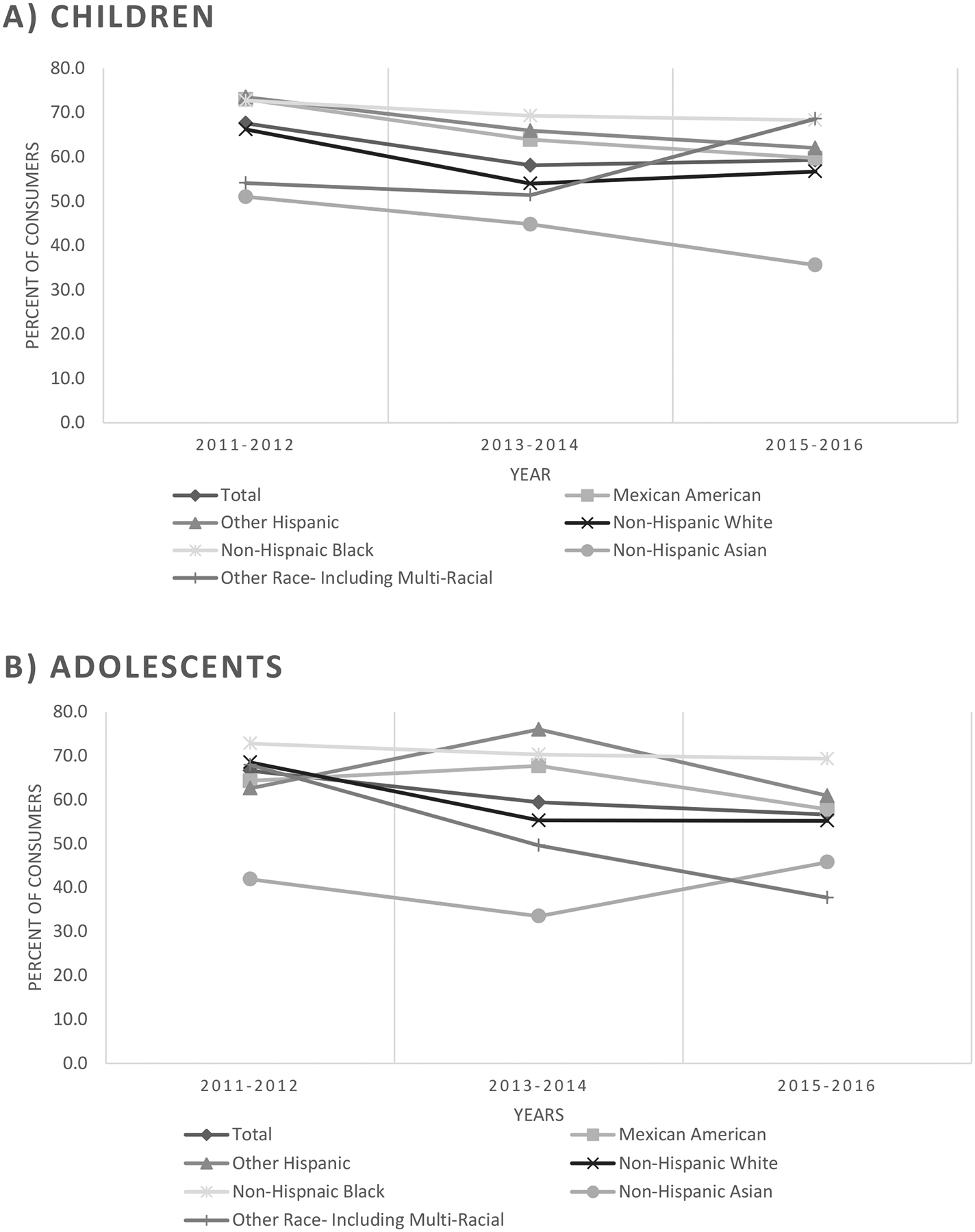
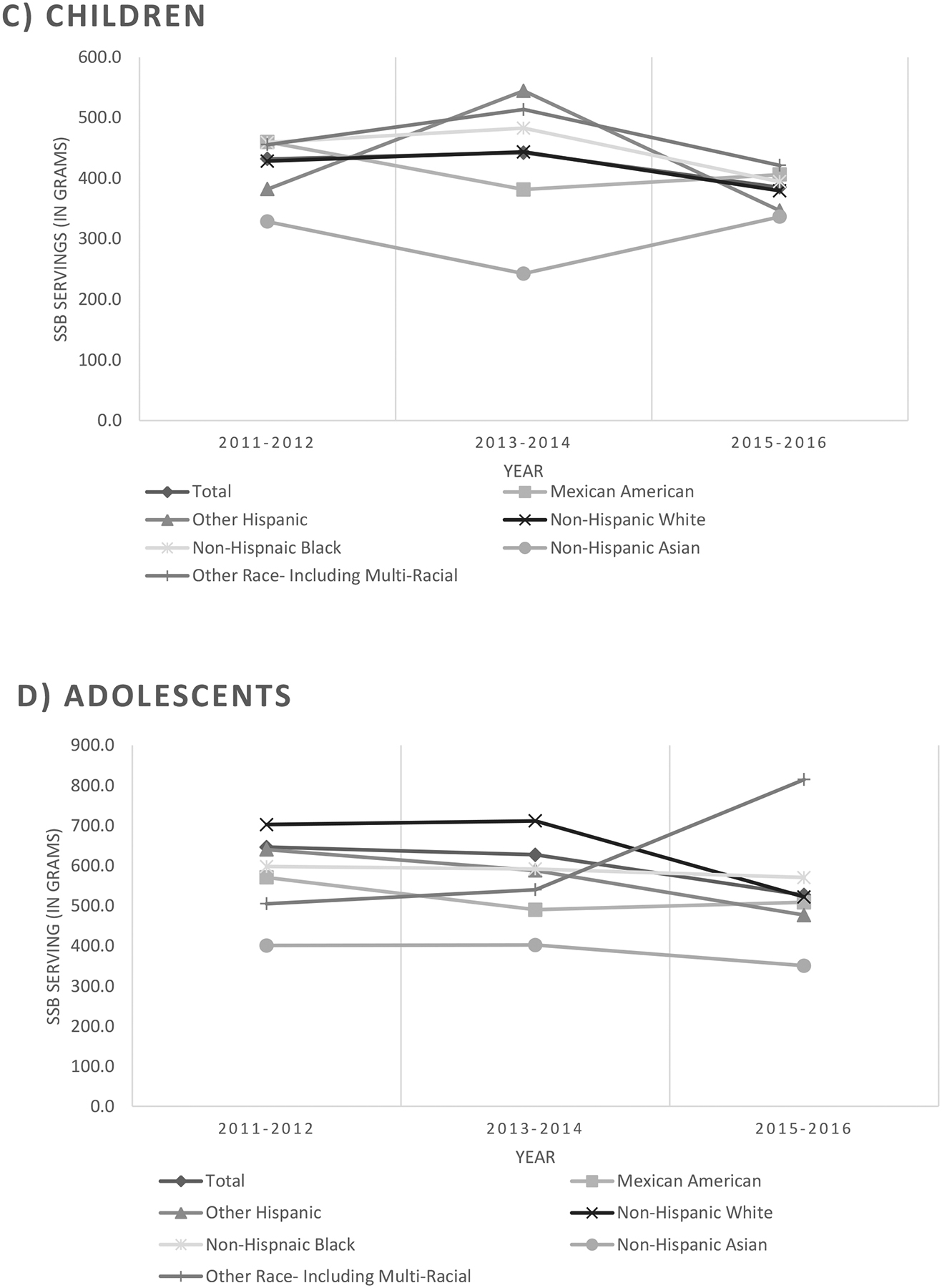
Trend in SSB consumption among children and adolescents from 2011–2016.
A) Percent of children, ages 5–11, consuming any SSB on a given day
B) Percent of adolescents, s 12–17, consuming any SSB on a given day
C) Mean SSB consumption on a given day among children, ages 5–11.
D) Mean SSB consumption on a given day among adolescents, ages 12–17
Sensitivity Analyses
Modifying the definition of SSB resulted in differences in estimated intakes. Among children, average SSB consumption increased from 419.93 grams (approximately 15 ounces; SE=11.28) to 517.17 grams (approximately 18 ounces; SE=13.87) using the broader definition; using the narrower definition, intake decreased to 404.76 grams (approximately 14 ounces; SD=11.13). Among adolescents, average SSB consumption increased from 600.73 grams (approximately 21 ounces; SE=18.82) to 691.01 grams (approximately 24 ounces; SE=21.32) using the broader definition; using the narrower definition, intake decreased to 575.15 grams (approximately 20 ounces; SE=18.04). Across all 3 definitions, SSB consumption remained highest for Black children and lowest for Asian American children; similarly, SSB consumption remained highest among White adolescents and lowest among Asian American adolescents (Supplemental Table 3).
DISCUSSION
This study investigated differences in factors associated with and types of youth SSB consumption by race/ethnicity in a US national sample of children and adolescents. Findings were that almost two-thirds of children and adolescents reported any SSB consumption on a given day. Among those reporting SSB consumption, children and adolescents consumed more than a serving of SSB per day and consumption was lowest among Asian Americans. Consumption of SSB was highest among Black and Other children and White and Other adolescents. Sweetened fruit drinks were the most popular source of SSB intake for most children, whereas soft drinks were the most common type of SSB consumed for most adolescents. Age was positively associated and female sex and water intake were negatively associated with SSB consumption across most races/ethnicities, whereas associations of other potential determinants and SSB consumption were only found in certain racial/ethnic subgroups.
The finding that Asian American youths had the lowest consumption of SSB, regardless of how SSB was defined, is consistent with previous studies.[20, 43] A limitation is that current dietary recall methods may not accurately capture SSB intake in Asian Americans, as they fail to explicitly record culturally relevant beverages, such as boba and aloe drinks.[44] Such beverages ought to be included in future nutritional surveys that include Asian Americans. More research is also needed to investigate how acculturation and dietary norms affect youth SSB consumption.
A systematic review of the literature on youth beverage consumption in the United States found that only 4% of published articles included Asian or Asian American children.[45] Even as recent NHANES surveys oversample Asian American participants, they tend to have higher education, English proficiency, and income levels than Asian Americans sampled at the community level.[46–48] Thus, the SSB consumption patterns reported here may only represent more acculturated and higher socioeconomic status Asian American youths. Moreover, Asian Americans are a heterogeneous population.[43, 48, 49] Future studies ought to examine differences within the Asian American population using innovative data collection methods to reach diverse communities and subgroups of Asian Americans (e.g., Asian Indian, Chinese, Filippino).
Previous studies have examined determinants of SSB consumption among youths and concluded that factors at multiple levels are important, including child, parent, and environmental characteristics.[28, 30–35] Only one previous study assessed such associations by race/ethnicity, for Hispanics, Whites, Blacks, and Other races/ethnicities.[19] Findings were that screen time had a moderate effect on SSB consumption among Hispanic children, and that youths of parents of Black and Hispanic children with at least a college education had less frequent youth SSB consumption than youths of parents with less education.
Screen time was associated with SSB intake among Hispanic children and adolescents and Asian American adolescents; guardian education level was statistically significantly associated with SSB intake among Mexican American adolescents. This is interesting, given the limited autonomy younger children, especially, have on their screen time and diets, and the considerable influence of their caretakers on these behaviors. Intergenerational influences, including caregivers’ attributes, attitudes, and knowledge, may be viewed as intermediary mechanisms through which societal and community influences affect children’s health behaviors.[49]
Other studies have investigated the types of SSB consumed among youths,[20, 22, 29, 31, 50] but only one previous study stratified results by race/ethnicity.[31] The present study assessed a wider variety of SSB types, including sweetened coffee and tea, fruit drinks, nutritional beverages, smoothies and grain drinks, and sweetened water, in addition to soda, sports and energy drinks, and included Asian Americans in the sample. Differences emerged by age group and race. While regular soda was the most commonly consumed SSB type among adolescents of most racial/ethnic subgroups, sweetened fruit drinks were the most commonly consumed SSB type among Black adolescents. Conversely, sweetened fruit drinks were the most commonly consumed SSB type among most children, whereas soft drinks were most popular among Mexican American and White children. Sweetened fruit drinks appear to be particularly relevant in the diets of Black youth, whereas soft drinks are more important for White and Hispanic youth. Future research should investigate sociocultural reasons for differences in SSB type preferences and how best to decrease fruit drink consumption while preventing its replacement with other types of SSB.
Prior studies have described promoting plain water to replace SSB thereby reducing energy intake, weight gain, and chronic disease risk.[51–53] A modeling study predicted that replacing SSB with water could significantly reduce the prevalence of obesity.[54] Yet, the relationship between promotion of water and replacement of SSB is unclear. Youths who were exposed to a combined school- and community-based social marketing campaign for water promotion had lower average SSB consumption.[55] Yet, youths attending a school in which environmental changes were made to support water consumption reduced SSB consumption, but did not replace SSB with water.[56] In the multivariable analyses, drinking at least one serving of water was associated with decreased SSB consumption for the majority of racial/ethnic subgroups in both age groups. Hence, encouraging water consumption may decrease SSB intake; more research is needed to determine the mechanism whereby this occurs.
Finally, the decreasing trend in percent of consumers among Mexican American children and White and Other adolescents has both positive and negative implications. While this finding points to the success of increased messaging, education and, therefore, awareness with regards to the harms of sugary drink consumption, it also provides support for the notion that health messaging or policies are not ‘one size fits all’[57] as has been demonstrated with other chronic disease related behaviors.[58] Bearing in mind the potential for these policies to widen disparities between population subgroups is also critical.[59]
This is the first US national study to assess determinants of SSB intake by racial/ethnic subgroup. A strength is the inclusion of Asian Americans and Other Hispanics as separate categories. Presenting data in their most disaggregated form can help in identifying disparities to target, thereby promoting health equity. Another strength is the continuous measure of SSB consumption used, as recorded through a reliable and complete 24-hour dietary recall. This facilitated the identification of factors that might influence SSB consumption, including factors with more modest effects. It also permitted the examination of various types of SSB and their contributions to overall consumption.
Important limitations also deserve mention beyond the need to include Asian American culturally relevant beverages, such as boba tea and aloe drinks, in future nutritional surveys that was previously discussed. Since NHANES is cross-sectional study, causality cannot be determined from the reported associations. Moreover, averaging 24-hour recalls may not represent usual consumption patterns, due to over-inflated zeros. Rather, the results here should be interpreted as intake on a given day. Dietary data may also be subject to under- or over-reporting. Finally, a parent, caregiver, or proxy of children reported food intake for children less than 6 years of age, and the accuracy of these reports is unknown.
Conclusion
SSB consumption among children and adolescents is a risk factor for general health conditions such as obesity and oral health conditions such as dental caries. While determinants of youth SSB intake vary by race/ethnicity, water consumption was associated with decreased SSB intake and screen time was associated with increased SSB intake for many groups, but the mechanisms through which this occurs remain unknown. Certain findings presented here may help target interventions to decrease SSB consumption among specific vulnerable groups. In particular, directing efforts towards reducing sweetened fruit juice consumption among children and Black adolescents may foster increased water intake and decreased SSB intake.
Supplementary Material
Funding:
Partial support for Drs Northridge and Yi was provided by the National Institute of Dental and Craniofacial Research (NIDCR), grant # U56DE027447. Additional support provided by NIH/National Institute on Minority Health and Health Disparities (U54MD000538) and National Heart, Lung, and Blood Institute (R01HL141427). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest: The authors have indicated they have no potential conflict of interest to disclose.
REFERENCES
- 1.Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association. 2010;110(10):1477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeBoer MD, Scharf RJ, Demmer RT. Sugar-sweetened beverages and weight gain in 2- to 5-year-old children. Pediatrics. 2013;132(3):413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ambrosini GL, Oddy WH, Huang RC, Mori TA, Beilin LJ, Jebb SA. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. The American journal of clinical nutrition. 2013;98(2):327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papandreou D, Andreou E, Heraclides A, Rousso I. Is beverage intake related to overweight and obesity in school children? Hippokratia. 2013;17(1):42–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. The American journal of clinical nutrition. 2013;98(4):1084–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frantsve-Hawley J, Bader JD, Welsh JA, Wright JT. A systematic review of the association between consumption of sugar-containing beverages and excess weight gain among children under age 12. Journal of public health dentistry. 2017;77 Suppl 1:S43–s66. [DOI] [PubMed] [Google Scholar]
- 7.Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obesity research. 2004;12(5):778–88. [DOI] [PubMed] [Google Scholar]
- 8.Dubois L, Farmer A, Girard M, Peterson K. Regular sugar-sweetened beverage consumption between meals increases risk of overweight among preschool-aged children. Journal of the American Dietetic Association. 2007;107(6):924–34; discussion 34–5. [DOI] [PubMed] [Google Scholar]
- 9.Chi DL, Scott JM. Added Sugar and Dental Caries in Children: A Scientific Update and Future Steps. Dental clinics of North America. 2019;63(1):17–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Association AH. Data Visualizations.: Centers for Health Metrics and Evaluation (CHME). [Available from: https://healthmetrics.heart.org/data-visualization/.
- 11.Taber DR, Stevens J, Evenson KR, Ward DS, Poole C, Maciejewski ML, et al. State policies targeting junk food in schools: racial/ethnic differences in the effect of policy change on soda consumption. American journal of public health. 2011;101(9):1769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cradock AL, McHugh A, Mont-Ferguson H, Grant L, Barrett JL, Wang YC, et al. Effect of school district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004–2006. Preventing chronic disease. 2011;8(4):A74. [PMC free article] [PubMed] [Google Scholar]
- 13.Micha R, Karageorgou D, Bakogianni I, Trichia E, Whitsel LP, Story M, et al. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PloS one. 2018;13(3):e0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kansagra SM, Kennelly MO, Nonas CA, Curtis CJ, Van Wye G, Goodman A, et al. Reducing sugary drink consumption: New York City’s approach. American journal of public health. 2015;105(4):e61–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farley TA, Halper HS, Carlin AM, Emmerson KM, Foster KN, Fertig AR. Mass Media Campaign to Reduce Consumption of Sugar-Sweetened Beverages in a Rural Area of the United States. American journal of public health. 2017;107(6):989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bleakley A, Jordan A, Mallya G, Hennessy M, Piotrowski JT. Do You Know What Your Kids Are Drinking? Evaluation of a Media Campaign to Reduce Consumption of Sugar-Sweetened Beverages. American journal of health promotion : AJHP. 2018;32(6):1409–16. [DOI] [PubMed] [Google Scholar]
- 17.Boles M, Adams A, Gredler A, Manhas S. Ability of a mass media campaign to influence knowledge, attitudes, and behaviors about sugary drinks and obesity. Preventive medicine. 2014;67 Suppl 1:S40–5. [DOI] [PubMed] [Google Scholar]
- 18.Jeong M, Gilmore JS, Bleakley A, Jordan A. Local news media framing of obesity in the context of a sugar-sweetened beverage reduction media campaign. Journal of nutrition education and behavior. 2014;46(6):583–8. [DOI] [PubMed] [Google Scholar]
- 19.Tasevska N, DeLia D, Lorts C, Yedidia M, Ohri-Vachaspati P. Determinants of Sugar-Sweetened Beverage Consumption among Low-Income Children: Are There Differences by Race/Ethnicity, Age, and Sex? Journal of the Academy of Nutrition and Dietetics. 2017;117(12):1900–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. Journal of the Academy of Nutrition and Dietetics. 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao G, Kirley K, Weiss-Coleman R, Inman JJ, Bauer V, Zhou Y, et al. Consumption patterns of sugar-sweetened carbonated beverages among children and adolescents. 2015;9(4):17. [Google Scholar]
- 22.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–14. [DOI] [PubMed] [Google Scholar]
- 23.Hardy LL, Bell J, Bauman A, Mihrshahi SJA, health NZjop. Association between adolescents’ consumption of total and different types of sugar‐sweetened beverages with oral health impacts and weight status. 2018;42(1):22–6. [DOI] [PubMed] [Google Scholar]
- 24.Marshall TA, Curtis AM, Cavanaugh JE, Warren JJ, Levy SM. Child and Adolescent Sugar-Sweetened Beverage Intakes Are Longitudinally Associated with Higher Body Mass Index z Scores in a Birth Cohort Followed 17 Years. Journal of the Academy of Nutrition and Dietetics. 2019;119(3):425–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bleich SN, Vercammen KAJBo. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. 2018;5(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lesser IA, Gasevic D, Lear SAJPo. The association between acculturation and dietary patterns of South Asian immigrants. 2014;9(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sofianou A, Fung TT, Tucker KL. Differences in diet pattern adherence by nativity and duration of US residence in the Mexican-American population. Journal of the American Dietetic Association. 2011;111(10):1563–9.e2. [DOI] [PubMed] [Google Scholar]
- 28.Elfassy T, Adjoian T, Lent M. Sugary Drink Consumption Among NYC Children, Youth, and Adults: Disparities Persist Over Time, 2007–2015. Journal of community health. 2019;44(2):297–306. [DOI] [PubMed] [Google Scholar]
- 29.Herrick KA, Terry AL, Afful J. Beverage consumption among youth in the United States, 2013–2016. 2018. [PubMed] [Google Scholar]
- 30.Ranjit N, Evans MH, Byrd-Williams C, Evans AE, Hoelscher DM. Dietary and activity correlates of sugar-sweetened beverage consumption among adolescents. Pediatrics. 2010;126(4):e754–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park S, Blanck HM, Sherry B, Brener N, O’Toole T. Factors associated with sugar-sweetened beverage intake among United States high school students. The Journal of nutrition. 2012;142(2):306–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erinosho TO, Berrigan D, Thompson FE, Moser RP, Nebeling LC, Yaroch AL. Dietary intakes of preschool-aged children in relation to caregivers’ race/ethnicity, acculturation, and demographic characteristics: results from the 2007 California Health Interview Survey. Maternal and child health journal. 2012;16(9):1844–53. [DOI] [PubMed] [Google Scholar]
- 33.Zahid A, Davey C, Reicks M. Beverage Intake among Children: Associations with Parent and Home-Related Factors. International journal of environmental research and public health. 2017;14(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Watts AW, Miller J, Larson NI, Eisenberg ME, Story MT, Neumark-Sztainer D. Multicontextual correlates of adolescent sugar-sweetened beverage intake. Eating behaviors. 2018;30:42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mazarello Paes V, Hesketh K, O’Malley C, Moore H, Summerbell C, Griffin S, et al. Determinants of sugar-sweetened beverage consumption in young children: a systematic review. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2015;16(11):903–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, et al. Trends in Sedentary Behavior Among the US Population, 2001–2016. Jama. 2019;321(16):1587–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. The international journal of behavioral nutrition and physical activity. 2011;8:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sisson SB, Church TS, Martin CK, Tudor-Locke C, Smith SR, Bouchard C, et al. Profiles of sedentary behavior in children and adolescents: the US National Health and Nutrition Examination Survey, 2001–2006. International journal of pediatric obesity : IJPO : an official journal of the International Association for the Study of Obesity. 2009;4(4):353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United States Department of Agriculture. What We Eat In America. 2018.
- 40.Agriculture USDo. Food Patterns Equivalents Database 2019. [Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/.
- 41.Rosinger A, Herrick KA, Gahche JJ, Park S. Sugar-sweetened beverage consumption among US youth, 2011–2014. 2017. [PubMed] [Google Scholar]
- 42.Services USDoAaUSDoHaH. USDA Dietary Guidelines 2010. Washingtion, DC: U.S. Printing Office; 2010. [Google Scholar]
- 43.Demmer E, Cifelli CJ, Houchins JA, Fulgoni VL, 3rd. Ethnic disparities of beverage consumption in infants and children 0–5 years of age; National Health and Nutrition Examination Survey 2011 to 2014. Nutrition journal. 2018;17(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Min JE, Green DB, Kim L. Calories and sugars in boba milk tea: implications for obesity risk in Asian Pacific Islanders. Food science & nutrition. 2017;5(1):38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grummon AH, Sokol RL, Hecht CA, Patel AI. Measuring beverage consumption in US children and adolescents: a systematic review. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2018;19(8):1017–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chong DKSYS. Comparing characteristics of Asian American populations represented in national vs. community level datasets. [Presentation]. In press 2018.
- 47.Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. Journal of health care for the poor and underserved. 2010;21(4):1354–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Northridge ME, Metcalf SS, Yi S, Zhang Q, Gu X, Trinh-Shevrin C. A Protocol for a Feasibility and Acceptability Study of a Participatory, Multi-Level, Dynamic Intervention in Urban Outreach Centers to Improve the Oral Health of Low-Income Chinese Americans. Frontiers in public health. 2018;6:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Northridge ME, Schrimshaw EW, Estrada I, Greenblatt AP, Metcalf SS, Kunzel C. Intergenerational and Social Interventions to Improve Children’s Oral Health. Dental clinics of North America. 2017;61(3):533–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.White AH, James SA, Paulson SW, Beebe LA. Sugar Sweetened Beverage Consumption Among Adults With Children in the Home. Frontiers in nutrition. 2018;5:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vargas-Garcia EJ, Evans CEL, Prestwich A, Sykes-Muskett BJ, Hooson J, Cade JE. Interventions to reduce consumption of sugar-sweetened beverages or increase water intake: evidence from a systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2017;18(11):1350–63. [DOI] [PubMed] [Google Scholar]
- 52.Bruce MA, Beech BM, Thorpe RJ Jr., Mincey K, Griffith DM . Racial and gender disparities in sugar consumption change efficacy among first-year college students. Appetite. 2017;109:33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shamah-Levy T, Garcia-Chavez CG, Rodriguez-Ramirez S. Association between Plain Water and Sugar-Sweetened Beverages and Total Energy Intake among Mexican School-Age Children. Nutrients. 2016;8(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duffey KJ, Poti J. Modeling the Effect of Replacing Sugar-Sweetened Beverage Consumption with Water on Energy Intake, HBI Score, and Obesity Prevalence. Nutrients. 2016;8(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van de Gaar VM, Jansen W, van Grieken A, Borsboom G, Kremers S, Raat H. Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: a controlled trial. The international journal of behavioral nutrition and physical activity. 2014;11:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Veitch J, Singh A, van Stralen MM, van Mechelen W, Brug J, Chinapaw MJ. Reduction in sugar-sweetened beverages is not associated with more water or diet drinks. Public health nutrition. 2011;14(8):1388–93. [DOI] [PubMed] [Google Scholar]
- 57.Hall M, Graffunder C, Metzler M. Policy Approaches to Advancing Health Equity. Journal of public health management and practice : JPHMP. 2016;22 Suppl 1:S50–9. [DOI] [PubMed] [Google Scholar]
- 58.Li S, Kwon SC, Weerasinghe I, Rey MJ, Trinh-Shevrin C. Smoking among Asian Americans: acculturation and gender in the context of tobacco control policies in New York City. Health promotion practice. 2013;14(5 Suppl):18s–28s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pearson-Stuttard J, Bandosz P, Rehm CD, Penalvo J, Whitsel L, Gaziano T, et al. Reducing US cardiovascular disease burden and disparities through national and targeted dietary policies: A modelling study. PLoS medicine. 2017;14(6):e1002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


