Abstract
The allostatic model of addiction suggests that negative affect, such as depressive symptoms, mediates the effect of stress on outcomes among individuals with substance use disorders. However, few longitudinal treatment studies have demonstrated this effect. We analyzed data from a 12-week randomized trial of galantamine and/or computerized cognitive-behavioral therapy (CBT4CBT) for individuals (N=120) with cocaine use disorder in methadone treatment for opioid use disorder. We evaluated baseline perceived stress as a predictor of end-of-treatment (EOT) substance use outcomes, and EOT perceived stress as a predictor of month 6 post-treatment outcomes. We conducted mediation models with intervening depressive symptoms as a mediator. We also explored whether CBT4CBT moderated the effects of perceived stress. Baseline perceived stress did not predict EOT outcomes (i.e., total effect). However, in mediation models, we found indirect effects of baseline perceived stress on EOT cocaine and illicit opioid use, via mid-treatment depressive symptoms. EOT perceived stress had significant total effects on month 6 cocaine and illicit opioid use, and an indirect effect on month 6 illicit opioid use (but not cocaine use), via month 3 depressive symptoms. Alternative models with depressive symptoms as the predictor and perceived stress as a mediator revealed no indirect effects. The addition of CBT4CBT to standard methadone treatment did not moderate total or indirect effects of perceived stress on substance use. Depressive symptoms may play a mediating role in the prospective indirect effect of perceived stress on substance use outcomes, particularly illicit opioid use. Further research is needed on therapies targeting stress.
Keywords: cocaine and opioid use disorder, perceived stress, depressive symptoms, mediation, methadone treatment
Stress is an important factor in the maintenance of substance use disorder (SUDs) (Koob et al., 2014; Sinha, 2007). Stress refers to the perception of circumstances as highly challenging and surpassing one’s ability to adapt (Lazarus & Folkman, 1984). The allostatic model posits that both the neural stress system and reward system are fundamentally altered during the progression to addiction (Koob & Schulkin, 2018). Specifically, the allostatic model includes three stages of addiction: the binge/intoxication stage, the withdrawal/negative affect stage, and the preoccupation/anticipation stage (Koob & Schulkin, 2018). The binge intoxication stage is characterized by excessive and compulsive drug use that over time induces a state of pathological “allostatic load,” in which the brain attempts to adapt by progressively upregulating the neural stress system and downregulating the neural reward system. The withdrawal/negative affect stage is characterized by repeated episodes of withdrawal during intermittent periods of abstinence, with each withdrawal episode further sensitizing the neural system and inducing increasingly worse negative affect (e.g., depressive symptoms), thereby heightening the negative reinforcing effects of drugs. Finally, the preoccupation/anticipation stage is characterized by abstinence, yet ongoing deficits in executive functioning, residual negative affect, and high vulnerability for life stressors to provoke negative affective states.
In support of the allostatic model, the literature among individuals with different types of SUDs generally demonstrates that stress is a reliable predictor of drug cravings and substance use (Back et al., 2010; MacLean, Armstrong, & Sofuoglu, 2019; Preston, Kowalczyk, et al., 2018; Preston, Schroeder, et al., 2018; Sinha, 2001; Sinha, Garcia, Paliwal, Kreek, & Rounsaville, 2006; Sinha & Li, 2007; Verplaetse et al., 2018). Studies have also found that individuals with SUDs have heightened affective reactivity to stressors as compared to individuals without SUDs (Chaplin et al., 2010; Fox, Hong, Siedlarz, & Sinha, 2008). Importantly, studies have specifically shown that subjective and physiological reactivity to lab-induced stress prospectively predicts relapse to alcohol and cocaine use following inpatient treatment (Sinha et al., 2011; Sinha et al., 2006).
Despite advances in understanding the role of stress in addiction, there remains a need to better understand the mechanisms by which stress leads to poor outcomes among treatment-engaged individuals with SUD. Based on the allostatic model, unresolved high levels of stress in an individual’s life would itself become a source of “allostatic load” that provokes a highly vulnerable neural system, inducing further neuroadaptations in both the stress and reward systems, which serve to maintain persistent depressive symptoms (i.e., the “dark side” of addiction) (Koob & Schulkin, 2018). The allostatic model emphasizes depressive symptoms because allostatic overload is posited to impair the functioning of the neural reward system (e.g., natural reward processing), in addition to the functioning of the neural stress system. The allostatic model also posits that ongoing depressive symptoms perpetuate the cycle of addiction by increasing the likelihood of returning to excessive drug use as means of relief from negative affective states. Critically, few clinical studies among individuals with SUDs have tested key tenets of this allostatic model. To our knowledge, no studies have evaluated whether depressive symptoms statistically mediate the effect of stress on poor substance use outcomes following treatment.
Perceived stress and depressive symptoms are similar, yet distinct constructs (Hammen, 2005). Of note, both constructs can be considered as indicators of a higher-order latent internalizing disposition, or a tendency to experience negative symptoms that are focused inwards (Krueger, McGue, & Iacono, 2001). Yet, there are also key differences. Perceived stress refers to one’s ongoing evaluations of life circumstances and one’s ability to adapt. Depressive symptoms, on the other hand, include a constellation of specific symptoms (i.e., depressed mood, anhedonia, guilt/worthlessness, concentration difficulties, psychomotor slowing, loss of energy, suicidal ideation, disruptions in appetite) that tend to co-occur. People vary in the degree to which perceived stress is associated with negative affective states and symptoms over time (McHugh, Kaufman, Frost, Fitzmaurice, & Weiss, 2013), and decoupling stress from these symptoms (i.e., building resilience to stress) is an important target of treatment for SUDs (McHugh & Kneeland, 2019). Distinguishing stress and depressive symptoms facilitates the investigation of the process over time in which life circumstances, specifically perceptions of these circumstances, and depressive symptomology influence one another.
Finally, there is a lack of research on how existing behavioral treatments for SUD, such as cognitive-behavioral therapy (CBT), may moderate the effect of stress on substance use. One study found that increases in coping skills following standard alcohol inpatient treatment mitigated the effect of severe stress on alcohol relapse (Brown, Vik, Patterson, Grant, & Schuckit, 1995). Hence, it is plausible that CBT, given its emphasis on coping skills training, may assist individuals in coping more adaptively with stress, thereby mitigating the effect of stress on subsequent affective symptoms and substance use.
The current study sought to address the abovementioned gaps in the literature by examining the role of perceived stress and intervening depressive symptoms in the prediction of substance use treatment outcomes. For the current study, we were particularly interested in evaluating whether stress may act as a source of “allostatic load” that provokes depressive symptoms (Koob & Schulkin, 2018). We conducted secondary analyses of data from a twelve-week, 2×2 factorial randomized trial of galantamine (a cognitive enhancer) and Computer Based Training for Cognitive Behavioral Therapy (CBT4CBT) (Carroll et al., 2008) among patients with current cocaine use disorder who were enrolled in methadone treatment for opioid use disorder (Carroll, Nich, DeVito, Shi, & Sofuoglu, 2018). Approximately half of patients with opioid use disorder receiving methadone treatment have co-occurring cocaine use disorder (Condelli, Fairbank, Dennis, & Rachal, 1991). Cocaine use among individuals with opioid use disorder is associated with poorer outcomes, including opioid use, HIV risk behaviors, criminal activity, and worse psychosocial functioning (Ball & Ross, 2012; Condelli et al., 1991; Kosten, Rounsaville, & Kleber, 1988; Schottenfeld et al., 2005). Hence, studying this particular subpopulation remains critically important. Moreover, examining this particular subpopulation in the current secondary analysis provided us the opportunity to evaluate whether stress and depressive symptoms might play differential roles with regard to opioid use and cocaine use.
First, we evaluated baseline perceived stress as a predictor of end-of-treatment (EOT) cocaine and illicit opioid use outcomes. Second, we evaluated EOT perceived stress as a predictor of cocaine and illicit opioid use outcomes at the most distal month 6 post-treatment follow-up. We then conducted a series of mediation models. For one set of models, we tested the indirect effect of baseline perceived stress on EOT substance use outcomes, via mid-treatment (week 6) depressive symptoms. For another set of models, we tested the indirect effect of EOT perceived stress on month 6 substance outcomes, via month 3 depressive symptoms. Drawing from the allostatic model of addiction (Koob & Schulkin, 2018), we hypothesized that perceived stress would exhibit a significant indirect effect on substance use outcomes via intervening depressive symptoms. Finally, we also conducted exploratory analyses of CBT4CBT as a moderator of the total and indirect effects of perceived stress on substance outcomes.
Method
Participants and Procedures
This is a secondary analysis using data from a twelve-week, 2×2 factorial randomized clinical trial of galantamine vs. placebo and CBT4CBT plus treatment-as-usual (TAU) vs. TAU for cocaine use disorder (Carroll et al., 2018). The sample consisted of 120 individuals with current (past 28 days) cocaine use disorder who were stabilized on methadone maintenance treatment for opioid use disorder. Table 1 provides a summary of descriptive analyses for demographic and substance-related variables for the sample. Inclusion criteria included: 1) 18 years of age or older, 2) DSM-IV (APA, 2000) criteria for current cocaine dependence, and 3) at least one cocaine-positive urine test during screening. Exclusion criteria included: 1) current dependence diagnosis for another illicit drug other than cocaine or opioids, 2) current medical condition contraindicating galantamine (asthma, chronic obstructive lung disease, history of or current gastrointestinal ulcer, hepatic or renal impairment, cardiac rhythm disturbance, or pregnancy), 3) screening liver function test greater than three times normal, 4) use of medications contraindicated with galantamine (e.g., beta blockers and nonsteroidal anti-inflammatory drugs), or 5) not psychiatrically stable for outpatient treatment (e.g., due to acute suicidality). Participants were assessed before treatment, during treatment, at 12-week EOT, and during a 6-month follow-up period after the end-of-treatment.
Table 1.
Descriptive statistics for demographics and substance-related variables
| N (%) or Mean (SD) | |
|---|---|
| Female gender | 40 (33.3%) |
| Race/Ethnicity | |
| White | 62 (51.7%) |
| Latin-x | 32 (26.7%) |
| Black | 25 (20.8%) |
| Other | 1 (0.8%) |
| Age | 38.35 (9.42) |
| Completed high school | 86 (71.7%) |
| Unemployed | 87 (72.5%) |
| Route of Administration for Cocaine | |
| Smoke | 80 (66.7%) |
| Nasal | 28. (23.3%) |
| IV | 11 (9.2%) |
| Speedball | 1 (0.8%) |
| Oral | 0 (0%) |
| Years of Regular Cocaine Use | 9.80 (8.56) |
| Years of Regular Opioid Use | 9.88 (7.83) |
| Number of prior outpatient episodes | 2.66 (3.14) |
| Number of prior inpatient treatment episodes | 3.07 (5.06) |
| Days of cocaine use during 28 days prior to treatment | 16.03 (8.48); Min = 0; Max = 28 |
| Days of illicit opioid use during 28 days prior to treatment | 2.96 (4.95); Min = 0; Max = 20 |
| Days of cocaine use at EOT (final 28 days of treatment period) | 8.19 (7.25); Min = 0; Max = 28 |
| Days of illicit opioid use at EOT (final 28 days of treatment period) | 3.08 (5.69); Min = 0; Max = 28 |
| Days of cocaine use at month 6 (28 days prior to month 6 post-treatment follow-up assessment) | 5.79 (8.44); Min = 0; Max = 28 |
| Days of illicit opioid use at month 6 (28 days prior to month 6 post-treatment follow-up assessment) | 2.62 (5.69); Min = 0; Max = 28 |
Note: SD = standard deviation.
Interventions
Treatment-as-usual (TAU).
All participants received TAU, which consisted of daily methadone treatment and weekly individual or group counseling at an outpatient program.
Galantamine.
Galantamine is a cognitive enhancer for treating mild to moderate cognitive deficits related to neuropsychological disorders. Participants assigned to galantamine received a maximum dose of 8 mg per day of galantamine extended release. In the parent trial (Carroll et al., 2018), galantamine was associated with significantly less cocaine use during treatment. Moreover, a recent secondary analysis of the parent trial demonstrated significant effects of galantamine on reduced illicit opioid use during and following treatment (Carroll, DeVito, Yip, Nich, & Sofuoglu, 2019).
CBT4CBT.
Previously described in greater detail (Carroll et al., 2008; Carroll et al., 2014), Computer Based Training for Cognitive Behavioral Therapy (CBT4CBT) is an interactive, multimedia web-based treatment program with seven modules that teach core CBT skills (e.g., functional analysis, coping with cravings, drug refusal skills) through video demonstrations, guided narration, graphic animations, quizzes, interactive games and exercises, and printable take-home practice worksheets. Participants completed the web modules at a private area in the clinic, typically at the time of weekly assessments. In the parent trial (Carroll et al. (2018), CBT4CBT was associated with significantly less cocaine use during treatment. As previously reported, levels of engagement in CBT4CBT in the parent trial were relatively high. Participants assigned to CBT4CBT completed an average of about 5 of the 7 modules (M = 4.73, SD = 2.55) (Carroll et al., 2018).
Measures
Substance use.
A calendar-based Timeline Follow-Back method (Sobell & Sobell, 1992) was used to measure the frequency (in days) of cocaine and illicit opioid use before, during, and following the twelve-week treatment period. For the current analyses, we focused on baseline substance use (during the 28-day period prior to the baseline assessment), end-of-treatment (EOT) substance use (during the final 28-days of the study treatment period), and month 6-follow-up substance use (during the 28-day period prior to the 6-month post-treatment follow-up assessment). Self-reported cocaine and illicit opioid use was corroborated with urine toxicology screens, which were administered at each assessment visit.
Perceived stress.
The 10-item Perceived Stress Scale (PSS) (Cohen, Kamarck, & Mermelstein, 1983) was used to measure perceived stress. Participants indicate how often they have felt or thought a certain way in the past month (e.g., “how often have you felt that you were unable to control the important things in your life?”) on a 5-point Likert-type scale ranging from 0 (never) to 4 (very often). PSS total scores can range from 0 to 40 (Cohen et al., 1983). In the current sample, the PSS demonstrated acceptable internal consistency. Cronbach’s alpha’s at baseline, EOT, and month 3 were .74, .85, and .83, respectively.
Depressive symptoms.
The 13-item short-form version of the Beck Depression Inventory (BDI) (Beck, Steer, & Carbin, 1988) was used to measure depressive symptoms. For each item, participants select one statement out of several statements that best describes how they have felt in the past two weeks (e.g., 0 = “I do not feel sad” to 3 = “I am so sad or unhappy that I can’t stand it”). In the current sample, the BDI demonstrated acceptable internal consistency. Cronbach’s alpha’s at baseline, EOT, and month 3 were .85, .94, and .91, respectively. Total scores on the short-form version of the BDI can range from 0 to 39 (Beck et al., 1988).
Statistical Analyses
Descriptive analyses were conducted in SPSS. All regression models and mediation models were conducted in Mplus Version 8. Using multiple regression models, we tested baseline perceived stress as a predictor of EOT cocaine and illicit opioid use days. We also tested models with EOT perceived stress as a predictor of cocaine and illicit opioid use days at the most distal month 6 post-treatment follow-up. For these regression models, we controlled for gender, age, racial/ethnic minority status (i.e., White vs. Non-White), baseline days of drug use (cocaine use days for models with cocaine use as the outcome and illicit opioid use days for models with illicit opioid use as the outcome), and treatment condition (whether participants were assigned to active galantamine vs. placebo and CBT4CBT vs. no CBT4CBT).
Next, we conducted a series of mediation models. The first set of models included baseline perceived stress as a predictor, mid-treatment (week 6) depressive symptoms as a mediator, and EOT substance use as the outcome. For these models we controlled for the same set of covariates in the multiple regression models noted above, as well as baseline depressive symptoms. The second set of models included EOT perceived stress as the predictor, month 3 depressive symptoms as the mediator, and month 6 substance use as the outcome. For these models we controlled for the same set of covariates in the multiple regression models noted above, as well as baseline perceived stress and baseline depressive symptoms.
We also conducted a series of moderated regression models to test whether CBT4CBT moderated the total effects of perceived stress on substance use outcomes. Finally, we conducted a series of moderated mediation models to test CBT4CBT as a moderator of the indirect effects of perceived stress on substance use outcomes via depressive symptoms. The moderated regression and moderated mediation models included the same sets of covariates in the regression and mediation models noted above, with the addition of a CBT4CBT by perceived stress interaction term.
As sensitivity analyses, we also conducted a series of alternative mediation models with depressive symptoms (rather than perceived stress) as the focal independent variable and perceived stress (rather than depressive symptoms) as the mediator.
For all mediation and moderated mediation models, we tested indirect effects with the distribution of products of coefficients approach with bias-corrected bootstrapped confidence intervals (Hayes & Rockwood, 2017). Effect sizes of indirect effects were calculated as kappa squared estimates (κ2), with 0.01, 0.09 and 0.25 considered small, medium and large effects (Preacher & Kelley, 2011). It is important to note that significant indirect effects are widely considered valid and meaningful in the context of nonsignificant total effects (Hayes & Rockwood, 2017). An indirect effect occurs when a variable X affects a mediator variable M, which transmits variable X’s effect to variable Y via the effect of variable M on variable Y. Overall, modern mediation approaches focus on the indirect effect itself by testing whether this indirect effect is different than zero. Moreover, as noted by Hayes and Rockwood (2017), there is less statistical power to detect total effects, relative to indirect effects.
Rates of missing data were low for key study variables. For perceived stress, 0, 19 (15.8%) and 12 (10%) participants were missing data at baseline, EOT, and month 3, respectively. For depressive symptoms, 2 (1.0%), 24 (20%), 22 (18.3%), and 12 (10%) participants were missing data at baseline, mid-treatment (week 6), EOT, and month 3, respectively. For substance use data, there was no missing data at baseline and only 2 (1.7%) and 4 (3%) participants were missing data for cocaine use and illicit opioid use days at EOT and month 6, respectively. Baseline demographics were not related to missing data. We employed full information maximum likelihood, a preferred method for utilizing all available data to estimate parameters when some data is missing (Witkiewitz et al., 2014).
Results
Descriptives and Preliminary Analyses
As shown in Table 1, the sample had relatively severe SUD, given the descriptive data for years of regular cocaine (M = 9.80) and opioid use (9.88), number of prior inpatient (M = 3.07) and outpatient treatment episodes (M =2.66), unemployment rates (72.5%), and baseline cocaine use days (M = 16.03) and illicit opioid use days (M = 2.96). As shown in Table 2, there were large concurrent and prospective correlations between perceived stress and depressive symptoms assessed before, during, and following treatment. The baseline mean score for perceived stress (M =18.15, possible range 0 to 40) was in a score range indicating moderate levels of perceived stress, on average, for the sample. The baseline mean score for depressive symptoms (M =8.11 possible range 0 to 39) was in a score range indicating moderate levels of depressive symptoms, on average, for the sample.
Table 2.
Descriptives and intercorrelations among perceived stress and depressive symptoms
| PSS Baseline | BDI Baseline | PSS Mid-Tx | BDI Mid-Tx | PSS EOT | BDI EOT | PSS Month 3 | BDI Month 3 | |
|---|---|---|---|---|---|---|---|---|
| PSS Baseline | -- | |||||||
| BDI Baseline | .53*** | -- | ||||||
| PSS Mid-Tx | --a | --a | -- | |||||
| BDI Mid-Tx | .48*** | 44*** | -- | -- | ||||
| PSS EOT | .54*** | .35*** | --a | -- | -- | |||
| BDI EOT | .47*** | .41*** | --a | .85*** | .45*** | -- | ||
| PSS Month 3 | .53*** | .37*** | --a | 45*** | .59*** | 44*** | -- | |
| BDI Month 3 | .41*** | .50*** | --a | .62*** | .47*** | .61*** | .54*** | -- |
| Mean | 18.15 | 8.11 | --a | 4.53 | 17.01 | 3.91 | 17.07 | 4.59 |
| SD | 6.01 | 5.4 | --a | 5.46 | 6.24 | 5.65 | 5.84 | 6.01 |
Note: PSS = Perceived Stress Scale score. BDI =Beck Depression Inventory score. EOT = End of treatment. SD = standard deviation.
p < .001;
p < .01;
p < .05.
parameter not available because PSS was not administered mid-treatment. Total scores on the short-form version of the BDI can range from 0 to 39. Total scores on the PSS can range from 0 to 40.
In regard to change over time in perceived stress and depressive symptoms among the full sample, paired samples t-tests revealed no significant change, on average, in perceived stress from baseline to EOT (18.15 to 17.01, p =.07) and baseline to month 3 (18.15 to 17.07, p =.15). Among those who received CBT4CBT, there was no significant change in perceived stress from baseline (M = 18.92) to EOT (M = 18.60) (p = .66). Among those who did not receive CBT4CBT, there was a small reduction in perceived stress from baseline (M = 17.14) to EOT (M = 15.27) (p = .05; within-person Cohen’s d = .28). Neither treatment condition showed significant changes in perceived stress from baseline to month 3 (p’s > .30). Among the full sample, there were significant reductions in depressive symptoms, on average, from baseline to EOT (8.11 to 3.91, p < .001) and baseline to month 3 (8.11 to 4.59, p < .001). The CBT4CBT group evinced significant reductions in depressive symptoms from baseline (M = 8.14) to EOT (M = 4.36) (p < .001; d = .57) and baseline (M = 8.14) to month 3 (M = 5.13) (p < .001; d = .52). Those who did not receive CBT4CBT also evinced significant reductions in depressive symptoms from baseline (M = 8.46) to EOT (M = 3.39) (p < .001; d = .94) and baseline (M = 8.46) to month 3 (M = 3.93) (p < .001; d = .94).
Baseline Perceived Stress as a Predictor of EOT Substance Use
In multiple regression models, baseline perceived stress did not significantly predict EOT cocaine use days (B(SE) = .17 (.10), β = .14, p = .07). Baseline perceived stress also did not significantly predict EOT illicit opioid use days (B(SE) = −.01 (.07), β = −.002, p = .86).
EOT Perceived Stress as a Predictor of Month 6 Substance Use
In multiple regression models, EOT perceived stress significantly predicted month 6 cocaine use days (B(SE) = .27 (.13), β = .20, p = .04), as well as month 6 illicit opioid use days (B(SE) = .18 (.09), β = .19, p = .04).
Mediation Models
Figures 1A and 1B provide a summary of the mediation models with baseline perceived stress as the independent variable, mid-treatment depressive symptoms as the mediator, and EOT substance use as the dependent variable. Baseline perceived stress had significant indirect effects on both EOT cocaine use days and illicit opioid use days via mid-treatment depressive symptoms, such that greater baseline perceived stress predicted greater mid-treatment depressive symptoms, which in turn predicted greater EOT cocaine use and illicit opioid use days. These indirect effect were medium-to-large in size (cocaine use days model: κ2 =.138, illicit opioid use days model: κ2=.113).
1A and 1B.
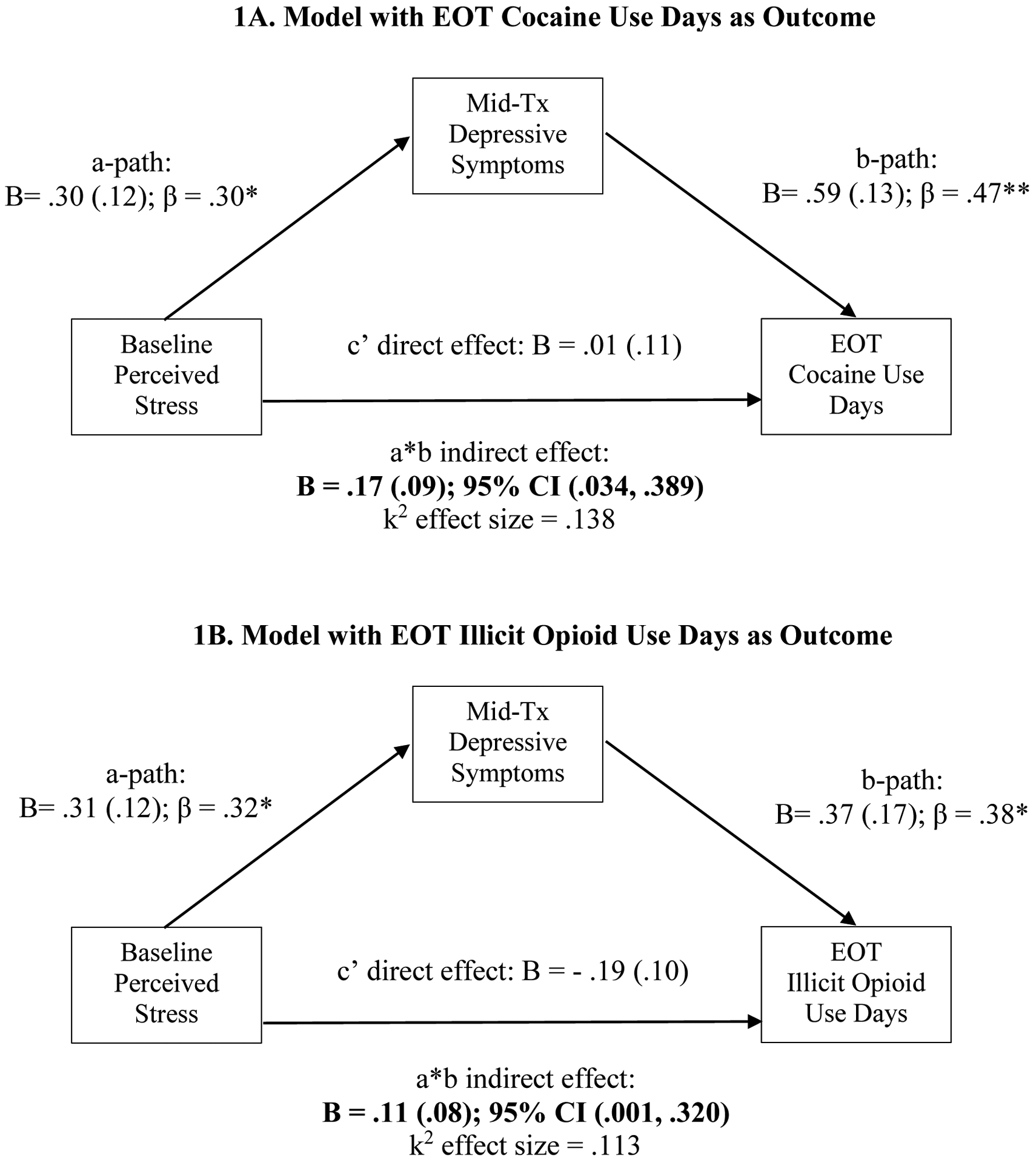
Mediation models with baseline perceived stress as the predictor, mid-treatment depressive symptoms as the mediator, and EOT substance use at the outcome. Confidence intervals for indirect effects not containing zero are bolded. B = unstandardized coefficient. β = standardized coefficient. *** = p < .001; ** = p < .01; * = p < .05.
Figures 2A and 2B provide a summary of the mediation models with EOT perceived stress as the independent variable, month 3 depressive symptoms as the mediator, and month 6 substance use as the dependent variable. EOT perceived stress had a significant indirect effect on month 6 illicit opioid use days via month 3 depressive symptoms, such that greater EOT perceived stress predicted greater month 3 depressive symptoms, which in turn predicted greater month 6 illicit opioid use days. This indirect effect was small-to-medium in size (κ2 = .046). EOT perceived stress also had a significant direct effect on illicit opioid use days at month 6. There were no significant indirect or direct effects of perceived stress on month 6 cocaine use days in the mediation models.
2A and 2B.
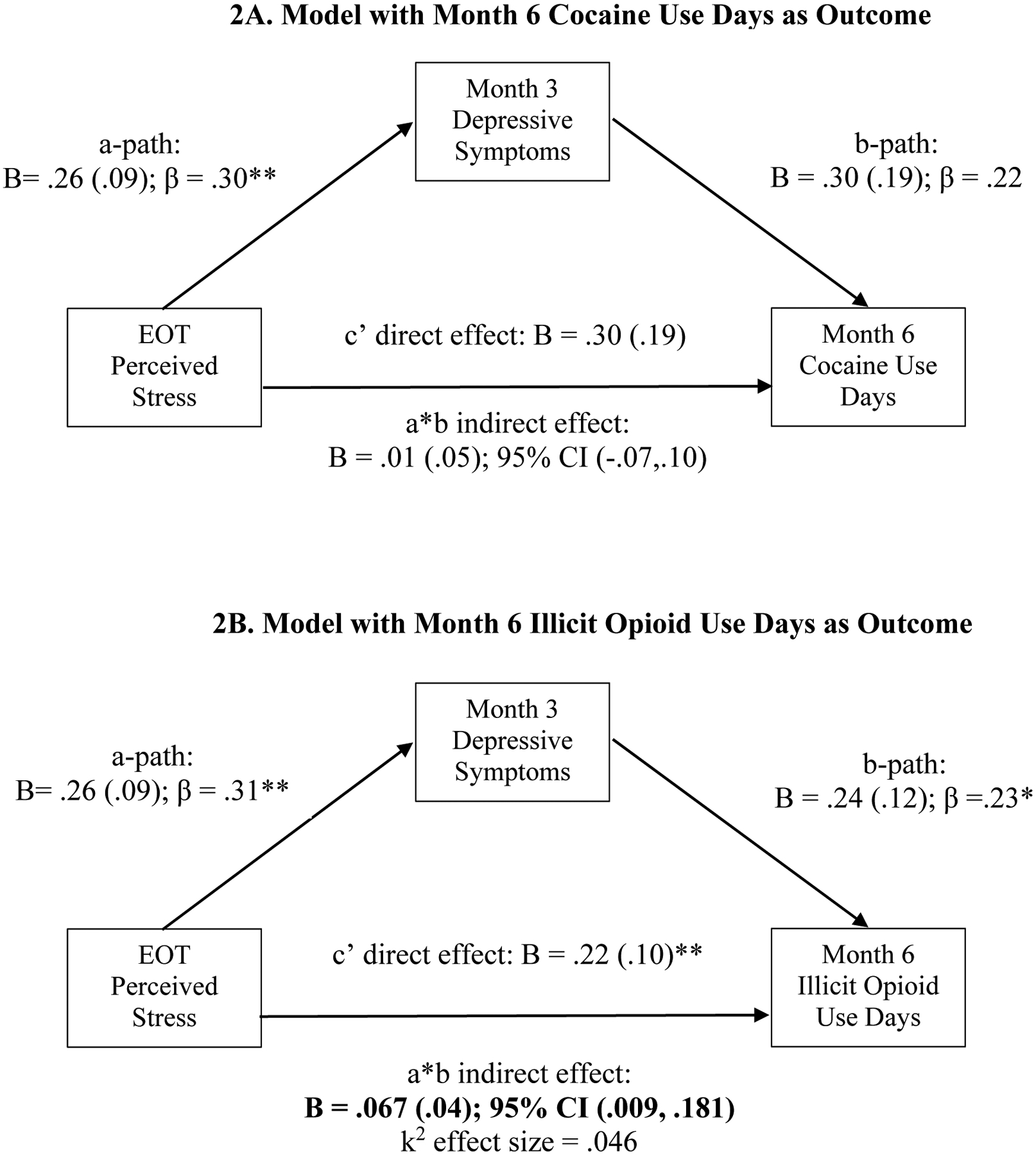
Mediation models with EOT perceived stress as the predictor, month 3 depressive symptoms as the mediator, and month 6 substance use at the outcome. Confidence intervals not containing zero are bolded. B = unstandardized coefficient. β = standardized coefficient. *** = p < .001; ** = p < .01; * = p < .05.
Sensitivity Analyses
We conducted sensitivity analyses to examine whether alternative mediation models with depressive symptoms as the focal independent variable and perceived stress as the mediator might also result in significant indirect effects. For the alternative mediation models with EOT substance use outcomes, we were not able to include mid-treatment perceived stress as a mediator because the parent trial did not assess perceived stress at mid-treatment. Hence, we opted to include EOT perceived stress as the mediator instead. Therefore, the alternative models included baseline depressive symptoms as the predictor, EOT perceived stress as the mediator, and EOT substance use as the outcome. For these models, there were no significant indirect effects of depressive symptoms via EOT perceived stress on EOT cocaine use (B (SE)= .06(.06); 95% CI (−.03, .20) or EOT illicit opioid use days (B (SE) = .03 (.03); 95% CI (−.01, .13). There were also no significant direct effects of depressive symptoms on EOT cocaine use (B (SE) = −.09 (.13), p = .47) or EOT illicit opioid use (B (SE) = .10 (.12); p = .41)
For alternative mediation models with month 6 substance use outcomes, there were no significant indirect effects of EOT depressive symptoms, via month 3 perceived stress, on month 6 cocaine use (B (SE)= .004 (.04); 95% CI (−.04, .07) or month 6 illicit opioid use days (B (SE) = .03 (.03); 95% CI (−.006, .117). There were also no significant direct effects of depressive symptoms on month 6 cocaine use (B (SE) = .27 (.24), p = .26) or month 6 illicit opioid use (B (SE) = .25 (.15); p = .10)
Exploratory Analyses
Moderated regression models showed that receiving CBT4CBT did not moderate the effect of baseline stress on EOT cocaine use days (B(SE) = −.37 (.20), p = .06) or EOT illicit opioid use days (B(SE) = .06 (.15), p = .66). CBT4CBT also did not moderate the total effect of EOT stress on month 6 cocaine use days (B(SE) = −.01 (.27), p = .94) and month 6 illicit opioid use days (B(SE) = .22 (.17), p = .19).
Moderated mediation models showed that there were no significant conditional indirect effects in which CBT4CBT moderated the indirect effect of baseline perceived stress, via mid-treatment depressive symptoms, on EOT cocaine use days (B (SE)= .03 (.03); 95% CI (−.02, .12) or illicit opioid use days (B (SE)= .04 (.04); 95% CI (−.01, .10). There were no significant conditional indirect effects in which CBT4CBT moderated the indirect effect of EOT perceived stress, via month 3 depressive symptoms, on month 6 cocaine use days (B (SE)= − .005 (.01); 95% CI (−.06, .02) or illicit opioid use days (B (SE)= .01 (.01); 95% CI (−.004, .07). Finally, among only individuals assigned to CBT4CBT, number of modules completed did not significantly moderate the stress to depressive symptoms to substance use outcome pathways (all p’s > .05).
Discussion
This secondary data analysis study evaluated the role of perceived stress and intervening depressive symptoms on substance use treatment outcomes among methadone-maintained individuals with cocaine use disorder who participated in a randomized trial of galantamine and computerized CBT (CBT4CBT). Key findings included the following: (1) although baseline perceived stress did not significantly predict end-of-treatment (EOT) substance use (i.e., total effects), there were significant indirect effects of baseline perceived stress on EOT cocaine and illicit opioid use, via mid-treatment depressive symptoms (medium-to-large effect sizes); (2) EOT perceived stress significantly predicted greater cocaine use days and illicit opioid use days 6-months following treatment (i.e., total effects), and had a significant indirect effect on month 6 illicit opioid use (but not cocaine use), via month 3 depressive symptoms (small-to-medium effect size); and (3) receiving CBT4CBT, in addition to standard methadone maintenance treatment, did not moderate any total or indirect effects of perceived stress on substance use outcomes.
Collectively, our findings indicate that depressive symptoms may play a mediating role in the prospective indirect effect of perceived stress on poor substance use outcomes. This mediation effect is consistent with the allostatic model of addiction (Koob & Schulkin, 2018), which posits that stress itself can become a source of “allostatic load” that disrupts vulnerable stress and reward neural systems, which in turn leads to increases in depressive symptoms, and drug use to relieve these symptoms (i.e., negative reinforcement). To our knowledge, our study is the first to show that depressive symptoms longitudinally mediate the effect of stress on substance use outcomes among individuals with substance use disorders.
For mediation models with opioid use as the outcome, we found an indirect effect, via depressive symptoms, for both baseline and EOT perceived stress. However, for mediation models with cocaine use as the outcome, we only found an indirect effect, via depressive symptoms, of baseline perceived stress and not EOT perceived stress. Hence, we found more consistent support for depressive symptoms playing a mediating role in the indirect effect of perceived stress on opioid use outcomes, as compared to cocaine use outcomes. Consistent with these findings, ecological momentary assessment studies suggest that opioid use may be more closely related to negative affective states (Epstein et al., 2009; Preston, Kowalczyk, et al., 2018), whereas cocaine use may be more closely related to environmental cues (Preston et al., 2009). Further work is needed to elucidate whether stress has a direct effect on cocaine use or whether its effect may be mediated by distinct mechanisms, such as executive functioning and inhibitory control in the presence of cues (Koob & Schulkin, 2018). Of note, in the current study EOT perceived stress also had a significant direct effect on opioid use outcomes, in addition to its indirect effect via depressive symptoms. Therefore, it is plausible that stress may directly influence opioid use or that its effect is mediated by additional mechanisms, such as executive functioning.
In this study, we found some differences in the findings based on timing of the assessments. For example, the indirect effect of perceived stress on opioid use via depressive symptoms was medium-to-large for the baseline to EOT model (a 3-month span), but was smallto-medium for the EOT to month 6 model (a 6-month span). Yet, on the other hand, it is interesting to note that in multiple regression models testing total effects, EOT perceived stress predicted month 6 substance use outcomes (a 6-month span), whereas baseline perceived stress did not predict EOT substance use outcomes (a 3-month). It is plausible that the time context (e.g., during treatment vs. after treatment) may influence the indirect or total effects of perceived stress on substance use outcomes. More research is needed to clarify when stress and depressive symptoms may be more or less of a risk factor for poor substance use outcomes in methadone-maintained individuals.
Receiving CBT4CBT did not moderate any total or indirect effects of perceived stress on substance use outcomes. These findings suggest that adding CBT4CBT to standard methadone maintenance treatment may not significantly influence the effects of stress on substance use outcomes among methadone-maintained individuals with cocaine use disorder. We also found that individuals who received CBT4CBT did not show significant change in perceived stress over time. The reasons behind these findings are unclear. It is possible that reduction in stress may not be a mechanism of change in CBT4CBT for this particular challenging subpopulation of methadone-maintained individuals with cocaine use disorder. For example, while one study found improvement in coping skills mediated the effect of CBT4CBT on substance use outcomes among a general outpatient sample of individuals with mixed substance use disorders (Kiluk, Nich, Babuscio, & Carroll, 2010), this effect was not replicated in a study among methadone-maintained individuals with cocaine use disorder (Kiluk et al., 2017). More research is needed on how improvement in targeted coping skills following CBT4CBT may influence stress and its effect on outcomes among various subpopulations of individuals with substance use disorders. Overall, there is limited research on how behavioral therapies, delivered in-person or via technology, may reduce stress and/or buffer the effect of stress on poor substance use outcomes. Future studies can examine how different behavioral therapies (e.g., CBT and mindfulness-based therapies) may affect stress and/or weaken the effects of stress on negative affect and substance use outcomes.
This study had several limitations. First, it is important to note that participants in this study were drawn from a sample of individuals with current cocaine use disorder who were stabilized on methadone treatment for opioid use disorder. The findings from this study may not generalize to other SUD populations, such as individuals actively using illicit opioids who are not receiving methadone or individuals receiving treatment for opioid use disorder in other settings like outpatient primary care. It is important to note that even though the sample was receiving methadone treatment for opioid use disorder, participants still reported illicit opioid use during the baseline period prior to the 12-week study treatment, as well as during and following the study treatment period. Second, this study was correlational in nature and causal conclusions about the role of stress cannot be drawn. Third, we examined stress and depressive symptoms with relatively infrequent and temporally spaced out assessments. Thus, conclusions cannot be drawn about the more proximal function of stress and its dynamic momentary or daily interrelationships with depressive symptoms and substance use. Yet, it is important to note that we did test alternative mediation models with depressive symptoms as the focal predictor and perceived stress as the mediator. There were no significant indirect effects from these models, lending support to our conceptualization of stress as the key factor that instigates the set of processes over time ultimately resulting in poor long-term substance use outcomes. Fourth, the parent trial did not measure mid-treatment perceived stress, so we were unable to conduct sensitivity analyses with alternative mediation models (with mid-treatment perceived stress as a mediator instead) that exactly matched the hypothesized within-treatment mediation models (with mid-treatment depressive symptoms as the mediator). Nevertheless, we did not find any significant indirect effects for alternative models with baseline depressive symptoms as the predictor, EOT perceived stress as a mediator, and EOT substance use as the outcome. Additionally, we did not find any indirect effects of EOT perceived stress on month 6 substance use via month 3 depressive symptoms. It is important to note that some view stress and depressive symptoms as indicators of the same higher-order internalizing construct (Krueger et al., 2001). Yet, the correlations between these constructs in our study (e.g., r = .53 at baseline) suggest that these are related, yet not redundant constructs. Finally, in this study we focused on depressive symptoms and did not examine other similar negative affective states (anger, anxiety, or irritability) or uncomfortable somatic states, which may also play important roles.
In sum, this study highlights that depressive symptoms play a mediating role in the prospective indirect effect of perceived stress on substance use outcomes, particularly illicit opioid use among those receiving methadone maintenance. Future work is warranted to better understand client characteristics, contextual factors, and treatment strategies that may buffer or potentiate the effects of stress on affective symptomology and substance use outcomes.
Acknowledgements
During the preparation of this manuscript, Dr. Roos was supported by the following training grant funded by the National Institute on Drug Abuse (NIDA): T32DA007238-27). NIDA had had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflicts of Interests
Dr. Carroll is a member in trust of CBT4CBT LLC, which makes CBT4CBT available to qualified clinical providers and organizations on a commercial basis. Dr. Carroll works with Yale University to manage any potential conflicts of interest. The other authors have no conflicts to disclose.
References
- APA. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association. [Google Scholar]
- Back SE, Hartwell K, DeSantis SM, Saladin M, McRae-Clark AL, Price KL, … Kreek MJ (2010). Reactivity to laboratory stress provocation predicts relapse to cocaine. Drug and alcohol dependence, 106(1), 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball JC, & Ross A (2012). The effectiveness of methadone maintenance treatment: patients, programs, services, and outcome: Springer Science & Business Media. [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical psychology review, 8(1), 77–100. [Google Scholar]
- Brown SA, Vik PW, Patterson TL, Grant I, & Schuckit MA (1995). Stress, vulnerability and adult alcohol relapse. Journal of studies on alcohol, 56(5), 538–545. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Nuro KF, … Rounsaville BJ (2008). Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. American Journal of Psychiatry, 165(7), 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, DeVito EE, Yip SW, Nich C, & Sofuoglu M (2019). Double Blind Placebo Controlled Trial of Galantamine for Methadone Maintained Individuals With Cocaine Use Disorder: Secondary Analysis of Effects on Illicit Opioid Use. The American journal on addictions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, Gordon MA, Portnoy GA, Marino DR, & Ball SA (2014). Computer-assisted delivery of cognitive-behavioral therapy: efficacy and durability of CBT4CBT among cocaine-dependent individuals maintained on methadone. American Journal of Psychiatry, 171(4), 436–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, DeVito EE, Shi JM, & Sofuoglu M (2018). Galantamine and Computerized Cognitive Behavioral Therapy for Cocaine Dependence: A Randomized Clinical Trial. The Journal of clinical psychiatry, 79(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM, Hong K, Fox HC, Siedlarz KM, Bergquist K, & Sinha R (2010). Behavioral arousal in response to stress and drug cue in alcohol and cocaine addicted individuals versus healthy controls. Human Psychopharmacology: Clinical and Experimental, 25(5), 368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of health and social behavior, 385–396. [PubMed] [Google Scholar]
- Condelli WS, Fairbank JA, Dennis ML, & Rachal JV (1991). Cocaine use by clients in methadone programs: significance, scope, and behavioral interventions. Journal of substance abuse treatment, 8(4), 203–212. [DOI] [PubMed] [Google Scholar]
- Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin J-L, & Preston KL (2009). Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Archives of general psychiatry, 66(1), 88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox HC, Hong K-IA, Siedlarz K, & Sinha R (2008). Enhanced sensitivity to stress and drug/alcohol craving in abstinent cocaine-dependent individuals compared to social drinkers. Neuropsychopharmacology, 33(4), 796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C (2005). Stress and depression. Annu. Rev. Clin. Psychol, 1, 293–319. [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour research and therapy, 98, 39–57. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, DeVito EE, Buck MB, Hunkele K, Nich C, & Carroll KM (2017). Effect of computerized cognitive behavioral therapy on acquisition of coping skills among cocaine-dependent individuals enrolled in methadone maintenance. Journal of substance abuse treatment, 82, 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, & Carroll KM (2010). Quality versus quantity: acquisition of coping skills following computerized cognitive–behavioral therapy for substance use disorders. Addiction, 105(12), 2120–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Buck CL, Cohen A, Edwards S, Park PE, Schlosburg JE, … Whitfield TW Jr (2014). Addiction as a stress surfeit disorder. Neuropharmacology, 76, 370–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Schulkin J (2018). Addiction and stress: an allostatic view. Neuroscience & Biobehavioral Reviews. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, & Kleber HD (1988). Antecedents and consequences of cocaine abuse among opioid addicts: A 2.5-year follow-up. Journal of Nervous and Mental Disease. [DOI] [PubMed] [Google Scholar]
- Krueger RF, McGue M, & Iacono WG (2001). The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Personality and Individual Differences, 30(7), 1245–1259. [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping: Springer publishing company. [Google Scholar]
- MacLean RR, Armstrong JL, & Sofuoglu M (2019). Stress and opioid use disorder: A systematic review. Addictive behaviors. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Kaufman JS, Frost KH, Fitzmaurice GM, & Weiss RD (2013). Positive affect and stress reactivity in alcohol-dependent outpatients. Journal of studies on alcohol and drugs, 74(1), 152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, & Kneeland ET (2019). Affective vulnerability in substance use disorders. Current opinion in psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Kelley K (2011). Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychological methods, 16(2), 93. [DOI] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin J-L, … Epstein DH (2018). Exacerbated craving in the presence of stress and drug cues in drug-dependent patients. Neuropsychopharmacology, 43(4), 859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Schroeder JR, Kowalczyk WJ, Phillips KA, Jobes ML, Dwyer M, … Epstein DH (2018). End-of-day reports of daily hassles and stress in men and women with opioid-use disorder: Relationship to momentary reports of opioid and cocaine use and stress. Drug and alcohol dependence, 193, 21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Vahabzadeh M, Schmittner J, Lin J-L, Gorelick DA, & Epstein DH (2009). Cocaine craving and use during daily life. Psychopharmacology, 207(2), 291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenfeld RS, Chawarski MC, Pakes JR, Pantalon MV, Carroll KM, & Kosten TR (2005). Methadone versus buprenorphine with contingency management or performance feedback for cocaine and opioid dependence. American Journal of Psychiatry, 162(2), 340–349. [DOI] [PubMed] [Google Scholar]
- Sinha R (2001). How does stress increase risk of drug abuse and relapse? Psychopharmacology, 158(4), 343–359. [DOI] [PubMed] [Google Scholar]
- Sinha R (2007). The role of stress in addiction relapse. Current psychiatry reports, 9(5), 388–395. [DOI] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong K.-i. A., Hansen J, Tuit K, & Kreek MJ (2011). Effects of adrenal sensitivity, stress-and cue-induced craving, and anxiety on subsequent alcohol relapse and treatment outcomes. Archives of general psychiatry, 68(9), 942–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, & Rounsaville BJ (2006). Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Archives of general psychiatry, 63(3), 324–331. [DOI] [PubMed] [Google Scholar]
- Sinha R, & Li C (2007). Imaging stress-and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug and alcohol review, 26(1), 25–31. [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back In Measuring alcohol consumption (pp. 41–72): Springer. [Google Scholar]
- Verplaetse TL, Moore KE, Pittman BP, Roberts W, Oberleitner LM, Smith PH, … McKee SA (2018). Intersection of stress and gender in association with transitions in past year DSM-5 substance use disorder diagnoses in the United States. Chronic Stress, 2, 2470547017752637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Falk DE, Kranzler HR, Litten RZ, Hallgren KA, O’Malley SS, … Workgroup, I. c. w. t. A. C. T. I. (2014). Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcoholism: clinical and experimental research, 38(11), 2826–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]


