Abstract
Background
Providing adequate psychiatry consultation capacity on a 24/7 basis is an intrinsic challenge throughout many multihospital health care systems. At present, implementation research has not adequately defined the effectiveness and feasibility of a centralized telepsychiatry consultation service within a multihospital health care system.
Objective
To demonstrate feasibility of a hub and spoke model for provision of inpatient consult telepsychiatry service from an academic medical center to 2 affiliated regional hospital sites, to reduce patient wait time, and to develop best practice guidelines for telepsychiatry consultations to the acutely medically ill.
Methods
The implementation, interprofessional workflow, process of triage, and provider satisfaction were described from the first 13 months of the service.
Results
This pilot study resulted in 557 completed telepsychiatry consults over the course of 13 months from 2018 to 2019. A range of psychiatric conditions commonly encountered by consultation-liaison services were diagnosed and treated through the teleconferencing modality. The most common barriers to successful use of telepsychiatry were defined for the 20% of consult requests that were retriaged to face-to-face evaluation. The average patient wait time from consult request to initial consultation was reduced from >24 hours to 92 minutes.
Conclusions
This study demonstrated the feasibility of a centralized telepsychiatry hub to improve delivery of psychiatry consultation within a multihospital system with an overall reduction in patient wait time. This work may serve as a model for further design innovation across many health care settings and new patient subpopulations.
Key words: telepsychiatry, consultation-liaison, digital health, implementation, centralization, technology
Introduction
Telepsychiatry is an evidence-based practice that has demonstrated feasibility and efficacy in many clinical settings and across diverse patient populations.1, 2, 3, 4 Studies in emergency telepsychiatry suggest its potential in reducing waiting times, length of stay, and hospital admissions rates.5 , 6 In addition to improving patient flow, emergency telepsychiatry has also demonstrated high rates of patient and provider satisfaction. At present, however, the literature has not adequately defined the effectiveness and feasibility of telepsychiatry in inpatient medical settings where the evaluation and treatment of patients may be challenged by the presence of acute medical conditions and complicated by the involvement of numerous stakeholders in care, including the patient, family, and medical providers. Although there are a few small studies demonstrating feasibility of consult telepsychiatry to medical/surgical inpatient units, none studied a multisite model using a hub-and-spoke design to address service shortage in a large health care system.7, 8, 9 Furthermore, there is limited understanding of the advantages and challenges of telepsychiatry for the acutely medically ill and few guidance on best practices for this specific population.
NewYork-Presbyterian Hospital/Weill Cornell Medicine (NYP) identified 4 of its regional affiliates that had inadequate staffing for psychiatry consultation to behavioral health patients, resulting in excess length of stay and long patient wait times of greater than 24 hours on average. To address the system-wide staffing shortage, NYP designed a centralized telepsychiatry hub to be equipped with staffing and technology to provide consultation-liaison (C-L) telemedicine services to NYP regional and affiliate hospitals on a 24/7 basis with the aim of reducing patient wait times and length of stay and increasing patient and provider satisfaction. This article describes the pilot C-L telepsychiatry program implemented at NYP and regional affiliates, Lower Manhattan Hospital (NYP-LMH) and Queens Hospital (NYP-Q). The first objective of this pilot study is to demonstrate feasibility of using a remote videoconferencing modality to evaluate and psychiatrically manage medically admitted patients across multiple hospital sites. The second objective is to identify clinical factors that guide triage of cases to in-person evaluation versus telepsychiatry. We further want to understand limitation of virtual presence and define potential compensatory strategies. A final objective is to test and optimize the necessary software and hardware requirements specific to interviewing patients who are acutely medically ill.
Methods
Setting
The NYP Telepsychiatry Service was developed with the goal of reaching 24/7 coverage of inpatient and emergency room psychiatry consults by the end of 2020 at 4 NYP regional sites that were identified to lack sufficient on-site psychiatry coverage. This pilot study took place from December 2, 2018, to December 31, 2019, in just 2 hospital sites: NYP-LMH and NYP-Q. The NYP Telepsychiatry Service was first implemented at NYP-LMH in December 2018 and followed by an expansion in August of 2019 to 3 inpatient medical units at NYP-Q that had a total of 150 staffed beds.
NYP-LMH is a 180-bed acute care hospital located in lower Manhattan of New York City. Psychiatry consults were requested from acute care settings that included emergency room, intensive care, general and orthopedic surgery, obstetrics, and general medicine. NYP-Q is a tertiary care facility and level 1 trauma center located in Queens County with a total of 535 beds.
Participants
Patients who require psychiatric evaluations in the emergency department or while admitted to inpatient services were prospectively enrolled in this study. The only exclusion is age below 5 years because of the concern that a complete evaluation cannot be achieved through videoconferencing modality only.
Implementation Design
The pilot C-L telepsychiatry program has a hub-and-spoke design delivering a hybrid of telemedicine and face-to-face intervention. It is organized with a telepsychiatrist at a remote central hub working in partnership with psychiatric nurse practitioners (NPs) on site. The telepsychiatry service was implemented in a 2-stage process. The first stage involved centralization of all inpatient psychiatric consultations from NYP-LMH to a telepsychiatry hub that exists within an office space inhabited by other NYP virtual services, called the Clinical Operations Center. A dedicated telepsychiatrist was available at the Clinical Operations Center Monday through Friday 9AM-5PM and worked in partnership with a psychiatric NP on site at NYP-LMH. The onsite NP assisted with in-person evaluations when clinically indicated or when there was a surge in consult volume that may compromise target consult completion times of 2 hours for urgent consults and 4 hours for routine consults.
In the second stage, the telepsychiatry service expanded to absorb all NYP-LMH emergency department consultations from August of 2019 onwards and simultaneously added on consulting responsibilities to 3 medical units at NYP-Q Hospital. Telepsychiatry staffing and hours increased as well in August to 2 telepsychiatrists on overlapping 8-hour shifts from 8AM to 8PM. This addition in staffing was in preparation for the goal of 24/7 coverage at all 4 affiliated regional sites mentioned previously once a complete service consisting of 6 full-time telepsychiatrists is achieved, and not in response to consult volume. At NYP-Q, the original psychiatry service consisting of 2 part-time psychiatrists making up 1.0 FTE remained available Monday–Friday 9AM–5PM, excluding vacations and holidays, to receive consults from the rest of the hospital. This service functioned as a bridge, pending the hiring of a psychiatric NP who will then act as the main on-site care provider. They also received and completed consults identified by the telepsychiatrists to require face-to-face intervention.
The 2-stage implementation process was necessary because of multiple rate-limiting factors as follows: timing of the telepsychiatry faculty expansion, telecart device availability, and need for large number of on-site staff training. Telepsychiatrists at the Clinical Operations Center performed telepsychiatry consultations exclusively without additional clinical duties; however, they were involved in all aspects of service expansion, including planning, implementation, education, and providing clinical perspective to technological barriers.
Consult Request and Workflow
Consults were centralized to the Clinical Operations Center using Avizia, an internet-based telemedicine software platform with videoconferencing capability. Consulting teams requested consults by using any hospital computer with Google Chrome, logging in to the Avizia platform, and submitting a request with patient name, medical record number, and reason for consult. Received consults were triaged by the on-shift telepsychiatrist in order of urgency and assigned to be seen by telepsychiatry or in-person evaluation. The triage of consults was based on volume of consults at each site and attention to limitations of videoconferencing for defined population, specifically those with sensory deficits, agitation, or altered sensorium. Initial consults assigned to the psychiatric NP were discussed and supervised by the telepsychiatrist.
The telepsychiatry consultations were performed using a desktop and installed webcam on the provider's side. On the patient side, evaluations took place using a mobile American Well C250 Telemedicine Cart, which is a registered FDA Class 1 medical device with a 20X zoom camera, integrated 5 GHz wireless connectivity, and 3-hour Lithium Iron battery. An external Phoenix MT202-EXE Duet Executive speaker/microphone was added to improve sound quality on both the provider and patient side. NYP provided American Well technical support. Each inpatient unit and the emergency room had one telemedicine cart dedicated to it, for a total of 6 devices at NYP-LMH and 3 devices at NYP-Q. Nursing was notified by the telepsychiatrist through Mobile Heartbeat, a unified communications application used by NYP system-wide, to transport the cart on the unit to the patient's bedside for evaluation.
The telepsychiatrists contacted the on-site consulting team by phone to communicate assessment, treatment plan, and disposition. The telepsychiatrist had access to and documented in the electronic health record at both sites. Diagnoses were made by board-certified psychiatrists who had fellowship training in either C-L or addiction psychiatry and used the Diagnostic and Statistical Manual of Mental Disorders (fifth edition; DSM-5) diagnoses.
Measures
Throughout the initial pilot phase of this study, we collected and structured clinical data manually by prospectively tracking cases and retrospectively reviewing descriptive and quality measures using NYP's electronic health record. Basic tracking measures of clinical care included consult volume, patient psychiatric diagnostic categories, and consult reason. Tableau analytics platform was used to interface with electronic health record and analyzed the average time to consult seen, defined as duration in minutes from time of consult request to start of consultation videoconferencing. All telehealth software and hardware used follow the privacy and security regulations and policies as specified by New York State Mental Hygiene Law and Health Insurance Portability and Accountability Act privacy and security regulations. The Weill Cornell Medicine Institutional Review Board approved a larger observational study that is continuously enrolling participants as the NYP telepsychiatry service expands to cover all 4 NYP regional sites and does include the data from this proof-of-concept study.
Provider Satisfaction Survey
A qualitative satisfaction survey was distributed to 2 telepsychiatrists who participated in this pilot study period. Questions to assess satisfaction included “What was your overall experience as first time telepsychiatrists?” “What about this pilot worked and did not work?”, “What could improve the service?” “What were the major service barriers?” “How confident did you feel overall with your evaluations, including diagnostic accuracy, ability to formulate treatment plan, and construct a safety plan?” “Did you feel able to form a connection with most patients?” “Did you feel able to form relationships with on-site staff and collaborate effectively on cases?”
Results
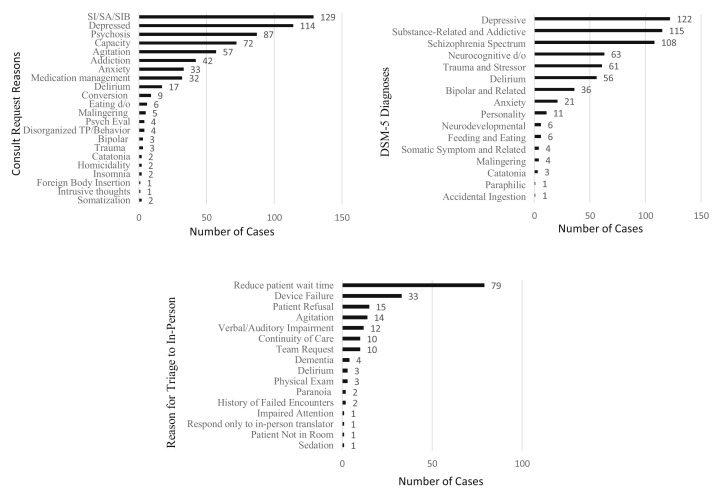
The pilot program implemented at NYP/Lower Manhattan and NYP/Queens resulted in 557 completed telepsychiatry consults (initial and follow-up evaluations) over the course of 13 months. There were 541 psychiatry consult requests, of which 191 requests (35%) were triaged to in-person evaluation and 350 requests (65%) were completed by telepsychiatry. The median age for the study participants was 60 years; 43% were female, and 57% were male. The consult questions were representative of those received commonly by C-L services, including suicidality, depression, psychosis, capacity, agitation, and addiction (Figure 1 ). Diagnosed psychiatric conditions were diverse and covered most DSM-5 classifications (Figure 1). Patient evaluation, diagnostic formulation, and treatment recommendations for these conditions were mostly able to be completed using videoconferencing modality.
Figure 1.
Depiction of Telepsychiatry Consult Service: Consult Reasons, Diagnoses, Reasons for Triage to In-Person for NYP/Queens and NYP/LMH. SA = suicide attempt; SI = suicidal ideation; SIB = self-injurious behaviors; TP = thought process.
The primary reason for triage of consults to in-person evaluation was to manage surge of consults that can occur unpredictably with the goal of completing all routine consults within 4 hours and all urgent consults within 2 hours. After removing triage to in-person to reduce patient wait time as a reason for in-person evaluation, the percentage of reassignment for other indications related to the videoconferencing modality itself was reduced to 20%. These included technology failure, patient and/or team request for in-person evaluation, agitation, and verbal or auditory impairment (Figure 1). The average time from consult request to start of video evaluation, or “time to consult seen”, was able to be obtained from May to December of 2019 and resulted in a mean time of 92 minutes, with a range between 4 and 358 minutes.
Provider Satisfaction
The qualitative free response survey was received from 2 psychiatrists who both had no previous experience in telepsychiatry. Both found this overall experience to be satisfying because of perceived gratitude of staff and patients, as well as reduction in commute time. The major source of dissatisfaction both psychiatrists mentioned was the videoconferencing technology used. The main barriers reported were poor internet connectivity, mic and speaker issues, and need for frequent telecart maintenance. Suggested improvements included real-time information technology assistance, choice of a more user friendly and stable telehealth device, and telepsychiatrists having access to device data, including battery percent and connectivity strength. Both telepsychiatry providers overall felt equally confident in their diagnostic accuracy and proposed treatment plans as compared to their past in-person evaluations. Both also felt able to form a therapeutic and trusting alliance with most patients. The providers had varying experience of ability to form relationships with on-site staff and collaborate effectively. One stated “effective collaboration was never an issue; however, relationship building with on-site staff leaves much to be desired”, citing the barrier as the limited nonvisual method of communication over text or phone calls. The other agreed that the relationship with physician assistants and physicians “felt a little impersonal compared to in-person consults” and commented that a better connection was made with nursing because they often appeared on video while transporting devices to patient rooms.
Discussion
Feasibility of a Hub-and-Spoke Tele-Consult Service
This pilot study demonstrated clinical feasibility of using a remote clinical hub to provide telepsychiatric consultations to 2 hospital sites while improving patient wait time from greater than 24 hours to a mean time of 92 minutes. While this proof-of-concept study was not designed to evaluate quantitative differences in the types of consultations completed between in-person and telepsychiatry, the preliminary data suggest that many of the common clinical questions and patient populations were well represented in completed telepsychiatry consultations and consistent with routine practice. Our pilot data demonstrated that a majority of C-L psychiatry consultations were completed using telepsychiatry; however, about 20% of the consult requests required in-person evaluation. The single most common reason for in-person evaluation outside of increasing efficiency and device failures was patient preference against the use of telemedicine. In some of these cases, primary teams who have concerns of telepsychiatry being subpar to in-person evaluations were offering patients an option between seeing an in-person provider or a telepsychiatrist, or directly advising against telepsychiatry. In other cases, patients expressed wariness of this new modality or have had poor experiences with telehealth in other contexts. This would be a useful area for further study to assess factors that may impact preference for in-person clinical encounters and strategies for improving engagement.
Technology Requirements in Acute Care Settings
The second most common reason for switching to in-person consultation was technology failure. A major technology problem was poor wireless connectivity strength resulting in significant audio and visual lags or disconnections. Another significant problem is a steep troubleshooting learning curve that is required in the use and upkeep of the Avizia 250 telecarts. Over time, the number of technology issues did diminish, starting with improved connectivity strength and staff's increasing familiarity with common troubleshooting techniques. As expected, a dedicated engineering and information technology team proved to be essential to the success of telepsychiatry implementation system wide. We recommend in Table 1 technology requirements that can optimize patient encounters in acute care settings. The most important specifications for service efficiency and high-quality video interviews include strong connectivity at patient's bedside in all hospital areas requiring consults, user-friendly software and hardware involving minimal steps to request consults and start video interview, 8 hours minimum battery life, and a dedicated information technology team that is accessible to user in real-time. In addition, a powerful noise-canceling microphone on the patient's end is uniquely important to the acute care setting because of the higher proportion of patients who are hypophonic, as well as the typically loud background noise of a busy emergency room or inpatient floor.
Table 1.
Technology Recommendations for Inpatient Telepsychiatry Consultation
| Stable and strong connectivity |
| Preferred wired ethernet, i.e., mounted smart TV in each patient room |
| Mobile Telecart with access to 5 GHz frequency band on wireless network |
| IT Surveillance of each patient unit before go-live |
| Ensure there is sufficient coverage through access points, to include windowed beds furthest away from access points |
| Structural interference or “dead zones” can occur, i.e., room with X-ray machine, thick concrete walls, and so on. |
| Hardware specifications and need for stability |
| Camera should have 10–20X resolution with pan and zoom capability |
| Motion-resistant camera, i.e., able to withstand telecart movement |
| High-quality stereo and microphone |
| Option for handset, headset, or earphone to preserve privacy |
| Long battery life (8 h minimum) |
| Long-duration consults can easily deplete battery life because of requirement of continuous audio and visual capability |
| Availability of a backup battery for mobile telecarts |
| User-friendly software and hardware |
| Minimal steps to request consult, and to complete consult |
| Easy troubleshooting when needed |
| Dedicated IT team, i.e., accessible 24/7, preferably by phone or chat in real-time |
| Dedicated transport and maintenance team on site for mobile telecarts |
| Allocate responsibilities to nonclinical staff, this includes transportation, charging of units, and troubleshooting. Recommend against adding this to nursing workflow. |
Clinical Factors that Guide Triage of Cases to In-Person Evaluation
The remaining reasons for assigning consults to in-person evaluation were all clinically based decisions by the telepsychiatrist. Patients with sensory impairments (auditory or visual) have significant difficulty interacting with a screen and can benefit from in-person visual (writing, mouthing) or tactile cues. Demented, acutely agitated, and/or delirious patients are unlikely to be able to maintain the attention and limited movement necessary for videoconferencing. The tele-device can also be used as a weapon or damaged during aggression. Consultations for assessment of suicidality or self-harm will require observation during evaluation so that on-site assistance can be recruited rapidly if the patient begins to self-harm. An in-person clinician can prove necessary in acute agitation and active suicidality to direct other clinical and security staff in emergent events where advanced protective measures, such as intramuscular injections or physical restraints, are needed for patient and/or staff safety. In dementia and delirium, in-person gestures to physically comfort the patient and having the ability to fully modulate tone and volume can be reassuring in common situations of disorientation, wandering, and picking at lines that require redirection. It is worth noting that a patient with delirium and/or neurocognitive impairments can be increasingly confused if language interpretation is embedded in the virtual program and shares the same speaker as the telepsychiatrist. Two voices coming from the same device can overwhelm the already tenuous task-switching executive function of these patients. Patients with persecutory or paranoid delusions involving being monitored electronically may have difficulty forming a trusting alliance through videoconferencing, although this has not always been the case when a thorough introduction and the reason for telepsychiatry use has been shared with the patient. Finally, there are clinical scenarios requiring daily physical examinations, including neuroleptic malignant syndrome, serotonin syndrome, catatonia, and opiate and alcohol withdrawal. Telepsychiatry can still be effective here if there is continuous collaboration with on-site staff to conduct examinations at specified intervals.
Limitations of Virtual Presence and Compensatory Strategies
A key and perhaps underappreciated aspect of C-L telepsychiatry is the broad and variable requirements of liaison work. C-L psychiatrists are often required to dexterously interface with the patient, primary teams, other consulting teams, and patient families in numerous different clinically complex or ethically ambiguous situations. Much of this work is effectively carried out through less formalized interaction channels and may be one of the more challenging domains for telepsychiatry to demonstrate effectiveness parity with in-person services. On the NYP telepsychiatry service, our first approach to this liaison gap is to fully train the telepsychiatrists in their recognition of the limitations of a virtual presence in interview and peripheral information gathering (Table 2 ) and importance in establishing working relationships with on-site staff.10 The on-site providers may experience a shift from in-person psychiatrist to a telepsychiatrist as a loss of presence and undervalue the telepsychiatrist's ability to maintain both liaison and consult functions. Thus, it is crucial for telepsychiatrists to understand that the evaluation does not end with the patient encounter and requires close phone contact with on-site providers, including hospitalists, physician assistants, nursing, social workers, patient care technicians performing safety observations, and other involved consultants. Information to obtain from the on-site staff should include the physical environment around the patient, for example, odors, room environment, hallway activity, and patient's appearance and behavior over time. By establishing phone contact, on-site providers will also have a direct way of communicating with the telepsychiatrist if there are changes in mental status, barriers encountered for medical intervention or disposition, among other concerns.
Table 2.
Inpatient Consultation Telepsychiatry Challenges and Solutions
| Challenge | Solutions |
|---|---|
| Loss of physical presence in interview | Take time to introduce videoconferencing modality to patient and reason for use |
| Always maintain visual connection with patient and simulate eye contact by looking at the webcam periodically | |
| Engage on-site staff to support with patient comfort and safety | |
| Request patient feedback on experience and adjust to improve satisfaction | |
| Lack of environmental context | Request for tele-device to be positioned 6 feet away from patient to allow for wide camera pan of the room and full-body view of patient |
| Loss of sensory cues (odor, room noises, hallway activity) | Be aware of this deficit and actively seek information from on-site staff |
| Loss of peripheral collateral (impromptu meetings with staff, family/friends) | Be active to communicate through phone with primary team, all on-site staff (RN, PCT, OT/PT, SW), and involved family or friends. |
| Use video communication with staff when possible. | |
| Providers should have a direct line to the telepsychiatrist for additional information or questions. | |
| Inability to perform physical examination | Request and educate primary teams to perform necessary examinations Routinely chart review for physical examinations performed by primary teams |
| Maintaining privacy in a cohorted room | Request for curtain to be drawn |
| Optional phone plug-in or headphone on patient end | |
| Volume of tele-device should be adjusted to patient's preference | |
| Ask patient to identify visitors and offer for interview to be held in private |
OT = occupational therapist; PCT = patient care technician; PT = physical therapist; RN = registered nurse; SW = social work.
Conclusion
The coming months and years will likely demonstrate a rapid expansion of the clinical literature dedicated to telepsychiatry in the setting of new institutional and governmental motivations during the COVID-19 response to increase access to numerous forms of telemedicine service. The NYP telepsychiatry hub demonstrates the value of using new technology and innovation in systems design to improve psychiatric health care delivery in this multihospital health care system. This work may serve as a proof-of-concept model for further design innovation across many health care settings. Further research is needed to assess equivalency in assessment, diagnoses, therapeutic alliance, and clinical outcomes of inpatient consultation telepsychiatry as compared to in-person evaluations.
Footnotes
Conflicts of Interest: The authors declare that they have no conflict of interest.
Funding: This was internally funded by NewYork-Presbyterian Hospital/Weill Cornell Medicine to meet the access to care needs of the hospital system. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Hubley S., Lynch S.B., Schneck C. Review of key telepsychiatry outcomes. World J Psychiatry. 2016;6:269–282. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hilty D.M., Ferrer D.C., Parish M.B. The effectiveness of telemental health: a 2013 review. Telemed J E Health. 2013;19:444–454. doi: 10.1089/tmj.2013.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hilty D., Yellowlees P.M., Parrish M.B. Telepsychiatry: effective, evidence-based, and at a tipping point in health care delivery? Psychiatr Clin North Am. 2015;38:559–592. doi: 10.1016/j.psc.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J Psychiatry. 2015;5:286–304. doi: 10.5498/wjp.v5.i3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Narasimhan M., Druss B.G., Hockenberry J.M. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatr Serv. 2015;66:1167–1172. doi: 10.1176/appi.ps.201400122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinhardt I., Gouzoulis-Mayfrank E., Zielasek J. Use of telepsychiatry in emergency and crisis intervention: current evidence. Curr Psychiatry Rep. 2019;21:63. doi: 10.1007/s11920-019-1054-8. [DOI] [PubMed] [Google Scholar]
- 7.DeVido J., Glezer A., Branagan L. Telepsychiatry for inpatient consultations at a separate campus of an academic medical center. Telemed J E Health. 2016;22:572–576. doi: 10.1089/tmj.2015.0125. [DOI] [PubMed] [Google Scholar]
- 8.Graziane J.A., Gopalan P., Cahalane J. Telepsychiatry consultation for medical and surgical inpatient units. Psychosomatics. 2018;59:62–66. doi: 10.1016/j.psym.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Kimmel R.J., Toor R. Telepsychiatry by a public, academic medical center for inpatient consults at an unaffiliated, community hospital. Psychosomatics. 2019;60:468–473. doi: 10.1016/j.psym.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Turner J.W. Telepsychiatry as a case study of presence: do you know what you are missing? J Comput Mediat Commun. 2001;6 [Google Scholar]