Abstract
Purpose:
In India, antenatal anxiety prevalence estimates range from 6% to 48%. Social support is strongly associated with mental wellbeing, yet most studies have examined the impact of support from partners and family members rather than peers, community members, or health care providers. This study explores the supportive role of Accredited Social Health Activists (ASHA) contacts for antenatal anxiety.
Methods:
Data were analyzed from the Saving Children, Improving Lives project, a quasi-experimental study conducted among rural, pregnant women in India. Regression models were used to estimate adjusted prevalence ratios (aPRs) and 95% confidence intervals for the relationship frequency of ASHA contacts and antenatal anxiety. Antenatal anxiety was measured using a subscale of the Edinburgh Postnatal Depression Scale.
Results:
The sample consisted of 480 pregnant women. Reported antenatal anxiety prevalence was 27% (95% CI: 23%, 31%). Participants who were more frequently visited by ASHAs at home (aPR: 0.90; 95% CI: 0.76, 0.98) and more frequently accompanied by ASHAs to their antenatal care visits (aPR: 0.86, 95% CI: 0.78, 0.95) were less likely to report antenatal anxiety. ASHA home visits were protective for the most vulnerable women (primigravida and those experiencing domestic violence) and ASHA accompaniment to antenatal care visits was equally protective for all women.
Conclusions:
ASHAs are valued for their contribution towards maternal health education and linking women of reproductive age to healthcare services. Our findings additionally suggest the important role ASHAs play in providing social support to pregnant women, particularly those who are most vulnerable to experiencing antenatal anxiety.
Keywords: antenatal anxiety, social support, community health workers
INTRODUCTION
Pregnancy is a time of immense physiological and psychosocial change for women, increasing their vulnerability for the onset or relapse of mental health issues.1 Some women may experience their first depressive or anxious episode during the antenatal period, while those with a history of depression or anxiety are at increased risk for recurrence, continuation, or intensification.2,3 Depression and anxiety during pregnancy have been linked with a number of adverse outcomes for both women and their children. Among women, antenatal depression and anxiety been associated with maternal malnutrition, increased substance abuse, and low uptake of antenatal care.4–7 Children of women with antenatal depression and anxiety are at a higher risk of premature birth, low birthweight, impaired cognitive growth, and development of depression in later life.8,9 Antenatal depression and anxiety have also been recognized as strong predictors of postnatal depression, one the causes of infant failure to thrive.1,10–12 Taken together, this evidence points to the importance of developing preventive and therapeutic mental health interventions for women during pregnancy.
The importance of antenatal mental health interventions may have even greater relevance in low- and middle-income countries (LMICs) compared to high-income countries (HICs) given the gap between the burden of mental health issues and available evidence-based services in LMICs.13–15 Recent systematic reviews and meta-analyses have found that the prevalence of antenatal depression and anxiety can range from 7% to 15% in HICs and from 19% to 25% in LMICs.13,14,16 While one out of five persons with depression receive care in HICs, only one out of 27 receive any care in LMICs, often due to a lack of funding, human resources, medication, and stigma relating to mental health care.15,17–21 This is particularly the case in India where antenatal depression and anxiety prevalence estimates range from 6% to 48% and a recent national mental health survey reported a treatment gap of 85% across the country for common mental disorders.22–29 Among studies from India, few have specifically focused on antenatal anxiety and its associated risk factors. Between the two existing studies, risk factors for antenatal anxiety include economic deprivation, low education, younger age, primigravida, male infant gender preference, intimate partner violence (IPV), domestic violence (DV).30,31
No studies in India have examined the association between antenatal anxiety and social support, despite considerable evidence in other contexts of its protective value.7,32–34 Social support is the provision of emotional, instrumental, or informational assistance leading one to believe that they are cared for, loved, esteemed, and a member of a network of mutual obligations.35 Social support may directly protect against anxiety or function by buffering the impact of stressful life circumstances that lead to anxiety.35–38 For example, experience of IPV is a risk factor for antenatal anxiety and its effect has shown to be buffered by social support.7,36,39 Studies examining antenatal anxiety have often only measured husband or husband’s family based social support rather than social support from peers, community members, or health care providers.7,32,33 In India, Accredited Social Health Activists (ASHA) are a cadre of community health volunteers who receive performance-based incentives for promoting universal immunization, referral and escort services for reproductive and child health and other healthcare programs in their villages.40 They have the potential to provide a unique source of social support given that they are often trusted women who are invested in improving the wellbeing of their fellow community members, and serve as a link to the local health system. Understanding the role of non-family member social support in this context, specifically from ASHAs, has the potential to inform the development of future evidence-based interventions for the prevention and treatment of antenatal anxiety.
The first aim of this analysis was to examine whether the frequency of contact with ASHAs, serving as a proxy for social support, was associated with antenatal anxiety among a sample of pregnant women in rural India. The second aim of this analysis was to assess the extent to which frequency of contact with ASHAs was protective for women most vulnerable to antenatal anxiety by investigating whether IPV, DV, and gravidity were moderators of the association between ASHA contact and antenatal anxiety.
METHODS
Parent Study Context and Design
Data for this analysis come from the Saving Children, Improving Lives (SCIL) project, a quasi-experimental study conducted among rural, pregnant women in Mysore district of Karnataka, India from 2011 to 2014. Mysore district has a mostly rural (58%) population of three million, half of whom are female.41 The SCIL project used a combination of community education efforts, mobile medical clinics, and social mobilization via self-help groups to increase uptake of antenatal care and HIV testing pregnant women. Additional details on the design and results of the SCIL project have been published previously.42,43
Parent Study Recruitment, Data Collection, and Ethics Approval
The SCIL project included 40 villages out of 209 total villages in Mysore district. Villiages were randomly selected using probability proportional to size sampling from a sampling frame defined by the following criteria: located 10 kilometers outside of Mysore city boundaries, a population size between 1,500–3000 individuals, and no existing public medical facility. Community education meetings were first conducted in each selected village to emphasize the importance of antenatal care and HIV testing and to inform members about the SCIL project. Mobile clinics then visited each village. Pregnant women who came to access health services at the mobile clinic were informed about the study, consented, and enrolled, if interested and eligible. Eligibility criteria included being currently pregnant, older than 18 years of age, and residing in a study village for more than six months.
Behavioral survey data and clinical data were collected from participants across three waves of the SCIL project. This analysis used behavioral survey data from the first wave of data collection, spanning April 2011 to March 2012. Surveys were administered by trained interviewers in Kannada, the local language, using structured questionnaires. The behavioral survey contained questions about demographics, socio-economic status, knowledge and attitudes about antenatal care, past and current care-seeking behaviors, interactions with healthcare workers, and psychosocial symptoms. Following the mobile clinic visit, survey data were entered into a Microsoft Access database by trained data entry staff (Microsoft Corporation, Redmond, WA).
The SCIL project received approval from the Institutional Review Board of the Public Health Research Institute of India (protocol number 2011–03-26–10) and Florida International University. Voluntary written informed consent was obtained from all participating women.
Measures
Outcome:
Antenatal anxiety symptoms were evaluated using a three-item sub-scale of the Edinburgh Postnatal Depression Scale (EPDS) known as EPDS-3A.44 The original EPDS is a 10-item instrument designed to identify symptoms of depression among women who are pregnant or postpartum.45–47 EPDS-10, which includes EPDS-3A items, has been previously translated, back-translated, and validated in Kannada among antenatal women in rural Karnataka.48 EPDS-3A has been found to be a valid tool for screening for anxiety in pregnant women and reliably able to distinguish between anxiety and depression symptoms. The three items in the EPDS-3A each included a choice of four answers that reflected how the participant was feeling over the past seven days. Individual item scores are recorded as zero, one, two, or three according to symptom severity. Total scores ranged from zero to nine and a cutoff score of six was utilized for detecting antenatal anxiety.49
Exposures:
Frequency of contact with ASHAs served as a proxy measure for social support in this analysis using two categorical items. Item one measured the frequency at which ASHAs visited the participant at home. Item two measured the frequency at which ASHAs accompanied the participant to antenatal care visits. Responses to both items included never, rarely (every three months), occasionally (every two months), and regularly (once a month).
Moderators:
Our moderators of interest were IPV, DV, and gravidity. Husband perpetrated IPV and husband’s family perpetrated DV were measured using the three-item Abuse Assessment Screen.50,51 Participants were asked whether they had ever been “kicked, hit, slapped, or otherwise physically hurt”, “forced into sexual activity against your wish”, or “humiliated or emotionally abused” by their husband or by their husband’s family. Ever experience of husband perpetrated IPV was recorded as positive if the participant answered yes to any of the three husband referent items and null if the participant answered no to all of the three husband referent items. Ever experience of husband’s family perpetrated DV was recorded as positive if the participant answered yes to any of the three husband’s family referent items and null if the participant answered no to all of the three husband’s family referent items. Gravidity was a dichotomous item measuring whether the participant was primigravida versus having been multigravida (previously pregnant).
Covariates:
Our covariates of interest included age (in continuous single years), primary school completion (standard 8), monthly income (in continuous Indian rupees), trimester, and number of living children. These variables have been shown to be associated with antenatal mental health among pregnant women in India.52
Data Analysis
We first calculated the number and proportion of participants who had each sociodemographic characteristic as well as the number and proportion who experienced pregnancy, childbirth, IPV, and DV. We then used chi-square tests to compare characteristics and experiences across participants with antenatal anxiety symptoms and participants without antenatal anxiety symptoms. Where cells were less than five, Fisher’s Exact tests were used (Table 1).
Table 1.
Participant Characteristics and Experiences by Antenatal Anxiety (N = 480)
| All Participants* (N = 480) | Anxious (N = 129) | Not Anxious (N = 351) | Chi-Square | ||||
|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | p-value | |
| Demographics | |||||||
| Age (years) | |||||||
| 18–22 | 336 | 70% | 81 | 63% | 255 | 73% | |
| 23–42 | 144 | 30% | 48 | 37% | 96 | 27% | 0.037 |
| Education Attained | |||||||
| Primary School Complete | 274 | 57% | 64 | 50% | 210 | 60% | |
| Primary School Incomplete | 206 | 43% | 65 | 50% | 141 | 40% | 0.045 |
| Monthly Income | |||||||
| < 5000 INR | 267 | 56% | 80 | 62% | 187 | 53% | |
| 5000–10,000 INR | 163 | 34% | 36 | 28% | 127 | 36% | |
| > 10,000 INR | 50 | 10% | 13 | 10% | 37 | 11% | 0.048 |
| Pregnancy and Children | |||||||
| Current Trimester | |||||||
| First (1–13 Weeks) | 58 | 12% | 8 | 6% | 50 | 14% | |
| Second (14–26 Weeks) | 248 | 52% | 74 | 57% | 174 | 50% | |
| Third (26–42+ Weeks) | 174 | 36% | 47 | 36% | 127 | 36% | 0.046 |
| Gravida | |||||||
| Primigravida | 311 | 65% | 94 | 73% | 217 | 62% | |
| Multigravida | 169 | 35% | 35 | 27% | 134 | 38% | 0.025 |
| Number of Living Children | |||||||
| 0 | 260 | 54% | 75 | 58% | 185 | 53% | |
| >1 | 220 | 46% | 54 | 42% | 166 | 47% | 0.290 |
| Violence Experience | |||||||
| Husband | |||||||
| Physical | 61 | 13% | 28 | 22% | 33 | 9% | p < 0.001 |
| Sexual | 54 | 11% | 30 | 23% | 24 | 7% | p < 0.001 |
| Emotional | 62 | 13% | 29 | 22% | 33 | 9% | p < 0.001 |
| Husband’s Family | |||||||
| Physical | 12 | 3% | 10 | 8% | 2 | 1% | p < 0.001 |
| Sexual | 1 | 0% | 1 | 1% | 0 | 0% | p < 0.001 |
| Emotional | 70 | 15% | 34 | 26% | 36 | 10% | p < 0.001 |
Columns do not add to total due to missing data
Second, we used a generalized linear model with a log link and binomial distribution to estimate prevalence ratios and corresponding 95% confidence intervals for the relationship between ASHA support and antenatal anxiety. We ran unadjusted and covariate adjusted models. The covariate adjusted models included age in years, primary school completion, monthly income, trimester, gravidity, and ever experience of IPV or DV (husband and husband’s family perpetrated). To explore our effect modification hypothesis, we refit our covariate adjusted model with interaction terms between the two types of ASHA support and gravida as well as the two types of ASHA support and having ever experienced IPV or DV (husband and husband’s family perpetrated). We then performed Wald-type F-tests to assess the joint statistical significance of the interaction terms. All analyses were conducted using StataSE, version 14.2 (College Station, TX).
RESULTS
Population Characteristics
The sample consisted of 480 pregnant women who were predominantly primigravida (65%) and were in their second trimester (52%). Median age was 21 years (interquartile range 18–23 years). The majority of participants had completed primary education (57%) and did not have living children (55%). Median monthly income 5000 INR (interquartile range 3000–8000 INR) and most participants had a monthly income less than 5000 INR per month (56%). Participants reported ever experiencing husband perpetrated physical (13%), sexual (11%), and emotional (13%) violence, as well as ever experiencing husband’s family perpetrated physical (3%), sexual (0.01%), and emotional (15%) violence (Table 1).
Population Characteristics and Antenatal Anxiety Prevalence
Prevalence of reported antenatal anxiety was 26.8% (95% CI: 0.23, 0.31). Participants with antenatal anxiety differed from participants without antenatal anxiety across most sociodemographic characteristics, experiences of pregnancy, and experiences of IPV. Compared to participants without anxiety, participants with anxiety were younger (median age 19 vs. 21, p = 0.032), a lower proportion had completed primary school (50% vs. 60%, p = 0.045), and higher proportion lived in households with monthly incomes less than 5000 INR (62% vs. 53%, p = 0.048).
ASHA Support and Antenatal Anxiety
Both types of ASHA support were negatively associated with prevalance of antenatal anxiety. Participants who were more frequently visited by ASHAs at home (adjusted prevalence ratio (aPR): 0.90; 95% CI: 0.76, 0.98) and participants who were more frequently accompanied by ASHAs to their ANC visits (aPR: 0.86, 95% CI: 0.78, 0.95) were less likely to have antenatal anxiety (Table 2 and Table 3).
Table 2.
Association Between ASHA Home Visits and Antenatal Anxiety (N = 480)
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| β | 95% Cl | aRR | 95% Cl | β | 95% Cl | aRR | 95% Cl | |
| Main Effects | ||||||||
| ASHA Home Visits | −0.16* | (−0.35,−0.02) | 0.90* | (0.76,0.99) | −0.17* | (−0.53,−0.02) | 0.90* | (0.73,0.99) |
| Age | 0.04 | (−0.03,0.11) | 1.03 | (0.97,1.10) | 0.04 | (−0.03,0.11) | 1.04 | (0.97,1.10) |
| Primary Education Complete | −0.02 | (−0.08,0.04) | 0.99 | (0.95,1.03) | −0.01 | (−0.07,0.05) | 0.99 | (0.95,1.03) |
| Monthly Income (INR) | −0.11 | (−0.44,0.22) | 0.93 | (0.74,1.16) | −0.12 | (−0.46,0.21) | 0.92 | (0.74,1.15) |
| Trimester | 0.19 | (−0.14,0.51) | 1.15 | (0.89,1.49) | 0.18 | (−0.15,0.51) | 1.14 | (0.88,1.46) |
| Primigravida | 0.25* | (0.02,0.99) | 1.19* | (1.03,1.67) | −0.05 | (−1.12,1.02) | 0.97 | (0.48,1.96) |
| Experienced Any DV (Husband) | 0.69* | (0.10,1.27) | 1.58* | (1.08,2.30) | 1.20 | (−0.34,2.75) | 2.13 | (0.92,4.90) |
| Experienced Any DV (Husband’s Family) | 0.73* | (0.10,1.36) | 1.62* | (1.09,2.40) | 2.07* | (0.35,3.81) | 3.05* | (1.70,5.49) |
| Interactions | ||||||||
| ASHA Home Visits X Primigravida | −0.13* | (−0.29,−0.06) | 0.91* | (0.74,0.98) | ||||
| ASHA Home Visits X DV (Husband) | −0.55* | (−1.20,−0.11) | 0.73* | (0.54,0.99) | ||||
| ASHA Home Visits X DV (Husband’s Family) | −0.19* | (−0.78,−0.04) | 0.89* | (0.62,0.99) | ||||
p-value < 0.05
Table 3.
Association Between ASHA ANC Visits and Antenatal Anxiety (N = 480)
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| β | 95% Cl | aRR | 95% Cl | β | 95% Cl | aRR | 95% Cl | |
| Main Effects | ||||||||
| ASHA ANC Visits | −0.23* | (−0.40,−0.06) | 0.86* | (0.78,0.95) | −0.24* | (−0.57,−0.09) | 0.89* | (0.70,0.99) |
| Age | 0.04 | (−0.03,0.11) | 1.04 | (0.97,1.11) | 0.04 | (−0.03,0.11) | 1.03 | (0.97,1.10) |
| Primary Education Complete | −0.02 | (−0.08,0.04) | 0.99 | (0.95,1.03) | −0.02 | (−0.08,0.04) | 0.99 | (0.95,1.02) |
| Monthly Income (INR) | −0.13 | (−0.46,0.20) | 0.92 | (0.73,1.15) | −0.12 | (−0.46,0.21) | 0.92 | (0.74,1.15) |
| Trimester | 0.15 | (−0.18,0.48) | 1.12 | (0.87,1.44) | 0.13 | (−0.20,0.47) | 1.10 | (0.86,1.40) |
| Primigravida | 0.23* | (−0.76,−0.07) | 1.17* | (1.08,1.93) | 0.79* | (0.08,1.51) | 1.72* | (1.04,2.83) |
| Experienced Any DV (Husband) | 0.77* | (0.17,1.37) | 1.6* | (1.14,2.41) | 1.25* | (0.27,2.23) | 2.15* | (1.28,3.6 |
| Experienced Any DV (Husband’s Family) | 0.74* | (0.09,1.38) | 1.61* | (1.09,2.39) | 0.73* | (0.18,1.76) | 1.59* | (1.01,2.94) |
| Interactions | ||||||||
| ASHA ANC Visits X Primigravida | 0.43 | −0.79,0.07) | 0.7 | (0.77,1.01) | ||||
| ASHA ANC Visits X DV (Husband) | −0.30 | −0.78,0.17) | 0.82 | (0.62,1.10) | ||||
| ASHA ANC Visits X DV (Husband’s Family) | −0.02 | (−0.48,0.52) | 0.96 | (0.73,1.41) | ||||
p-value < 0.05
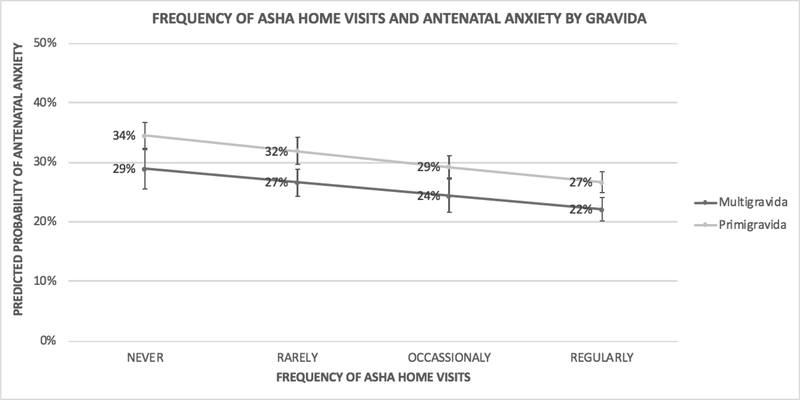
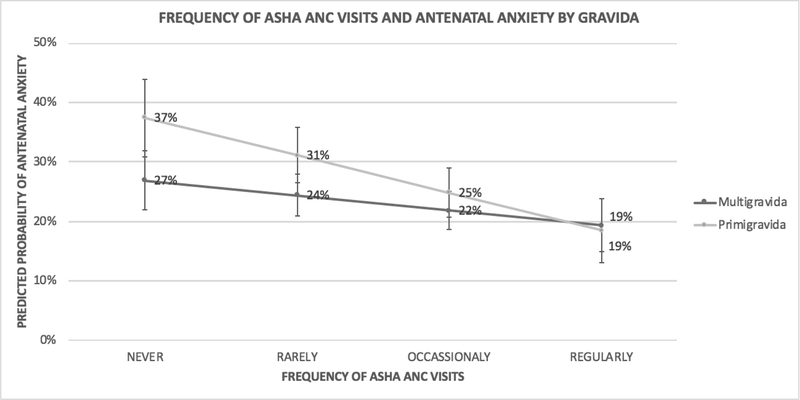
ASHA Support, Antenatal Anxiety, and Gravidity
Primigravida were more likely to have antenatal anxiety in the ASHA home visit adjusted model (aRR: 1.19, 95% CI: 1.03, 1.67) as well as the ASHA ANC visit adjusted model (aRR: 1.17, 95% CI: 1.08, 1.93). Gravidity was a modifier of ASHA home visits (Interaction Beta: −0.13, 95% CI: −0.29, −0.06) but not for ASHA ANC visits (Interaction Beta: −0.43, 95% CI: −0.79, 0.07) (Table 2 and Table 3). Our effect modification results suggest that ASHA home visits were only protective for primigravida and ASHA ANC visits were protective for all women, regardless of gravidity (Figure 1a-1b).
Figure 1a-1b.
ASHA Social Support and Antenatal Anxiety by Gravida
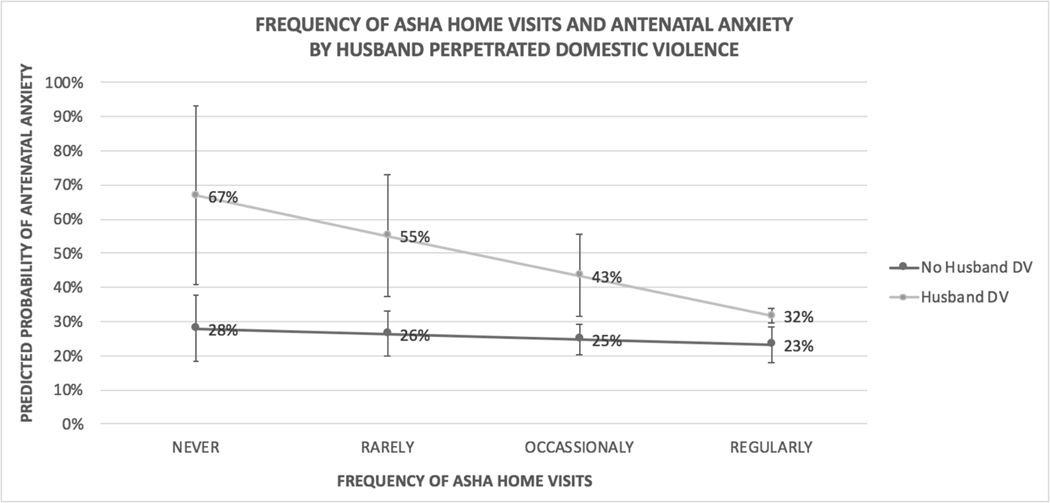
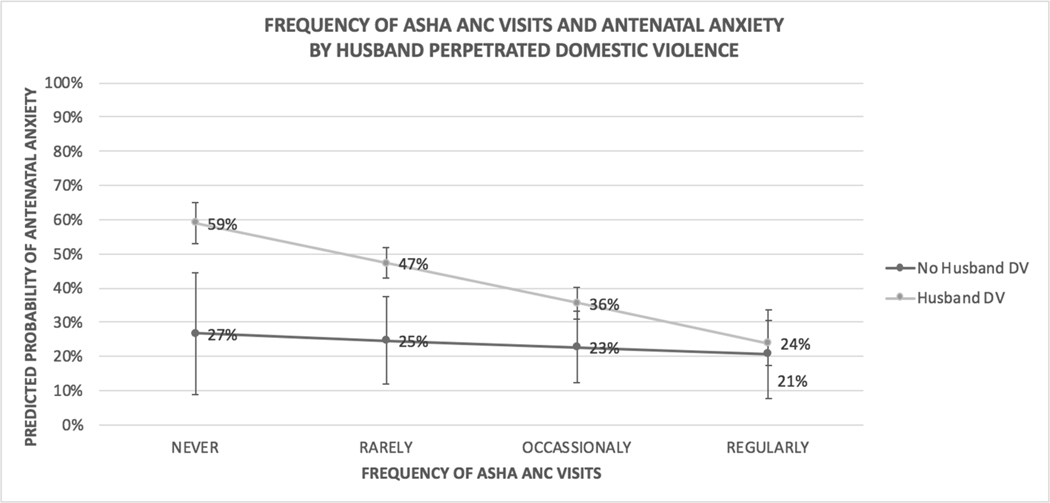
ASHA Support and Antenatal Anxiety Stratified by Husband Perpetrated IPV
Participants who had experienced any husband perpetrated IPV were more likely to have antenatal anxiety in our ASHA home visit adjusted model (aRR: 1.58, 95% CI: 1.08, 2.30) as well as our ASHA ANC visit adjusted model (aRR: 1.66, 95% CI: 1.14, 2.41). Husband perpetrated IPV was a modifier of ASHA home visits (Interaction Beta: −0.55, 95% CI: −1.20, −0.11) but not for ASHA ANC visits (Interaction Beta: −0.30, 95% CI: −0.78, 0.17) (Table 2 and Table 3). Our effect modification results suggest that ASHA home visits were only protective for participants who had experienced husband perpetrated IPV and ASHA ANC visits were protective for all women, regardless of husband perpetrated IPV experience (Figure 2a-2b).
Figure 2a-2b.
ASHA Social Support and Antenatal Anxiety by Husband Perpetrated Domestic Violence
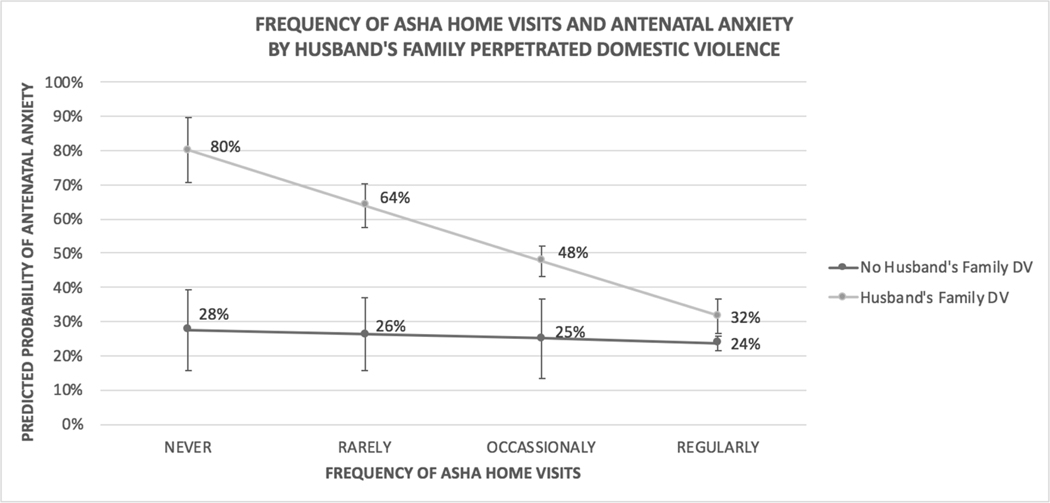
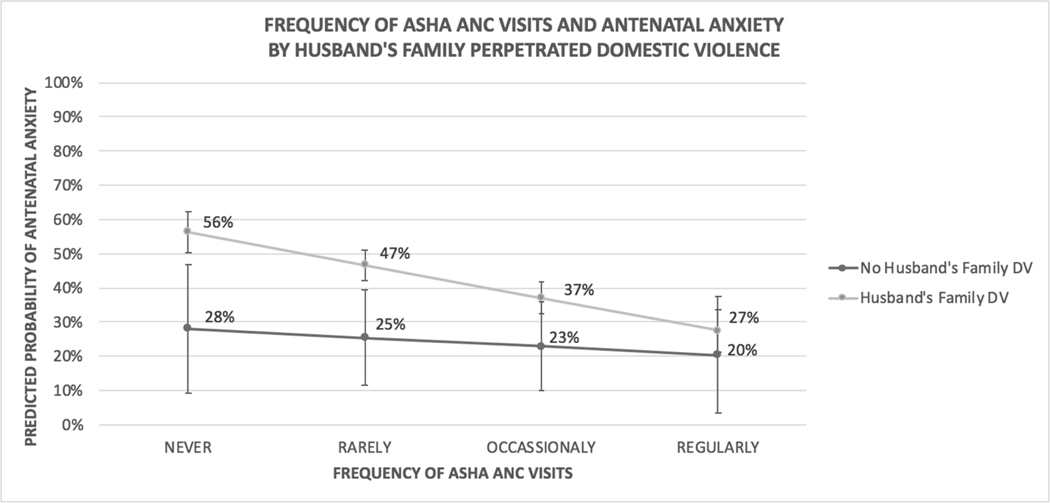
ASHA Support and Antenatal Anxiety Stratified by Husband’s Family Perpetrated DV
Participants who had experienced any husband’s family perpetrated DV were more likely to have antenatal anxiety in our ASHA home visit adjusted model (aRR: 1.62, 95% CI: 1.09, 2.40) as well as our ASHA ANC visit adjusted model (aRR: 1.61, 95% CI: 1.09, 2.39). Husband’s family perpetrated DV was a modifier of ASHA home visits (Interaction Beta: −0.19, 95% CI: −0.78, −0.04) but not for ASHA ANC visits (Interaction Beta: −0.02, 95% CI: −0.48, 0.52) (Table 2 and Table 3). Our effect modification results suggest that ASHA home visits were only protective for participants who have experienced husband’s family perpetrated DV and ASHA ANC visits were protective for all women, regardless of husband’s family perpetrated DV experience (Figure 3a-3b).
Figure 3a-3b.
ASHA Social Support and Antenatal Anxiety by Husband’s Family Perpetrated Domestic Violence
DISCUSSION
To our knowledge, this study is one of the first to examine the association between ASHA contacts and antenatal mental health outcomes in India. More than a quarter of all study participants reported antenatal anxiety. Participants who were more frequently visited by ASHAs at home and participants who were more frequently accompanied by ASHAs to their antenatal care visits were less likely to report antenatal anxiety. In addition, ASHA home visits were protective for the most vulnerable women (primigravida and those experiencing husband or husband’s family perpetrated intimate partner violence) and ASHA accompaniment to antenatal care visits was equally protective for all women. Taken together, our results suggest the potentially important role ASHAs play in providing contact-based social support to pregnant women, particularly those who are most vulnerable to experiencing antenatal anxiety.
The linkage between poor partner and family social support and antenatal depression has been well documented in India but non-family member social support is largely unexamined.23,54–57 Non-family member social support might be especially salient given the marital and household structure across many parts of the country. Women often leave their parental homes after marriage and join the multigenerational household of their spouse, exposing them to the norms and fertility preferences of their new family members. Pressure to conform to in-law expectations and to produce male children also has been found to be isolating and associated with antenatal anxiety and depression.23,58–61 Given this context, identifying non-family members who provide social support and facilitating their efforts could be equally as important as improving partner and family social support for pregnant women. Our findings add to the existing literature by examining ASHA social support and suggest its potential for protection against poor mental health outcomes.
Psychosocial interventions delivered by non-specialists have been found to be beneficial for common perinatal mental disorders in low and middle income countries.62,63 Many of these interventions have included a component of peer support provision by trained lay health workers or “mentor mothers”. 62,64,65 Lay peer support is built on the well documented effects of social support on health, as well as the recognition that people experiencing disease or other health challenges have a great deal to offer each other.38,66–69 In addition to knowledge and experience of a certain health concern or stressor, peer supporters often share a similar demographic background and community network with support recipients, enhancing their ability to provide socially relevant care and assistance.70 ASHAs are uniquely positioned to provide peer support given that they are trusted women who serve as a link between communities and health systems. Due to the observational nature of our study, we did not collect data on the characteristics of the ASHAs or the nature of their interactions with participants during home visits or accompaniment to ANC visits. Future research that documents shared characteristics and the type of support provided is essential for developing effective peer support components for antenatal anxiety and depression interventions.
Our antenatal anxiety prevalence results slightly differed from prior cross-sectional studies of antenatal anxiety in India. Beyond differences in population, all four studies used different tools to measure antenatal anxiety: the Pregnancy Related Thoughts Scale, the State Trait Anxiety Inventory, the Hospital Anxiety and Depression Scale, and the Pregnancy Related Anxiety Scale.26,31,71,72 These tools differ from the EPDS-3A as they include more than three items, physical symptoms, and suggest cut-points to scale the severity of antenatal anxiety. Although the EPDS-3A has been validated among pregnant women in southern India, future work that explores the differences among antenatal anxiety scales in this population is necessary.48
Our study has a few limitations. First, with our cross-sectional data, we report the prevalence of reported antenatal anxiety, but cannot make causal inferences about how any of the considered variables affect incidence and duration of reported antenatal anxiety. Our data do not show whether reported antenatal anxiety was incident during pregnancy or preceded the pregnancy. Second, we utilized contact with ASHAs as a proxy measure for social support which is a complex construct. Third, the EPDS, and the EPDS-3A subscale, are screening tools and do not diagnose antenatal anxiety or depression. While our cut-point of six was based on the validation study and demonstrated reasonable sensitivity and specificity, it is possible that some participants were falsely categorized as screening positive or negative for reported antenatal anxiety.44 The cross-sectional nature of the study imposed a fourth limitation. Anxiety symptoms may vary over time during a woman’s pregnancy but our assessment was restricted to a single point in time. Fifth, data were based on self-report which can be unreliable due to social desirability issues, perception, or memory challenges.Finally, our social support measures were derived from single items on the behavioral survey. Multidimensional scales may better capture these variables of interest more accurately.
CONCLUSION
ASHAs are valued for their contribution towards maternal health education and linking women of reproductive age, and their children, to healthcare services. Our findings additionally suggest the important role ASHAs play in providing social support to pregnant women, particularly those who are most vulnerable to experiencing antenatal anxiety.
Acknowledgments
Sources of Funding:
This study was funded by Positive Action for Children Fund and Elizabeth Glaser Pediatrics AIDS Foundation. NLB was supported by the National Institute of Allergy and Infectious Diseases (T32 AI007001–40), KK & PM were supported by the Fogarty International Center, National Heart Lung and Blood Institute, and National Institute of Neurological Disorders and Stroke (D43 TW010540). PM was also supported by National Institute of Allergy and Infectious Diseases (R15 AI128714–01).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- 1.Howard LM et al. Non-psychotic mental disorders in the perinatal period. The Lancet 384, 1775–1788 (2014). [DOI] [PubMed] [Google Scholar]
- 2.Nonacs R & Cohen LS Depression during pregnancy: diagnosis and treatment options. J. Clin. Psychiatry 63, 24–30 (2002). [PubMed] [Google Scholar]
- 3.Burt VK & Stein K. Epidemiology of depression throughout the female life cycle. J. Clin. Psychiatry 63, 9–15 (2002). [PubMed] [Google Scholar]
- 4.Marcus SM Depression during pregnancy: rates, risks and consequences. J. Popul. Ther. Clin. Pharmacol 16, (2009). [PubMed] [Google Scholar]
- 5.Rubertsson C, Hellström J, Cross M. & Sydsjö G. Anxiety in early pregnancy: prevalence and contributing factors. Arch. Womens Ment. Health 17, 221–228 (2014). [DOI] [PubMed] [Google Scholar]
- 6.Redshaw M. & Henderson J. From antenatal to postnatal depression: associated factors and mitigating influences. J. Womens Health 22, 518–525 (2013). [DOI] [PubMed] [Google Scholar]
- 7.Biaggi A, Conroy S, Pawlby S. & Pariante CM Identifying the women at risk of antenatal anxiety and depression: a systematic review. J. Affect. Disord 191, 62–77 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gelaye B, Rondon M, Araya R. & Williams MA Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 3, 973–982 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein A. et al. Effects of perinatal mental disorders on the fetus and child. The Lancet 384, 1800–1819 (2014). [DOI] [PubMed] [Google Scholar]
- 10.Leigh B. & Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8, 24 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson E, Grace S, Wallington T. & Stewart DE Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen. Hosp. Psychiatry 26, 289–295 (2004). [DOI] [PubMed] [Google Scholar]
- 12.Patel V, Rahman A, Jacob KS & Hughes M. Effect of maternal mental health on infant growth in low income countries: new evidence from South Asia. BMJ 328, 820 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA & Harris MG A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord 219, 86–92 (2017). [DOI] [PubMed] [Google Scholar]
- 14.Dennis C-L, Falah-Hassani K. & Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br. J. Psychiatry 210, 315–323 (2017). [DOI] [PubMed] [Google Scholar]
- 15.Thornicroft G. et al. Undertreatment of people with major depressive disorder in 21 countries. Br. J. Psychiatry 210, 119–124 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falah-Hassani K, Shiri R. & Dennis C-L The prevalence of antenatal and postnatal comorbid anxiety and depression: a meta-analysis. Psychol. Med 47, 2041–2053 (2017). [DOI] [PubMed] [Google Scholar]
- 17.Saxena S, Thornicroft G, Knapp M. & Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. The lancet 370, 878–889 (2007). [DOI] [PubMed] [Google Scholar]
- 18.Kakuma R. et al. Human resources for mental health care: current situation and strategies for action. The Lancet 378, 1654–1663 (2011). [DOI] [PubMed] [Google Scholar]
- 19.McBain R, Norton DJ, Morris J, Yasamy MT & Betancourt TS The role of health systems factors in facilitating access to psychotropic medicines: a cross-sectional analysis of the WHO-AIMS in 63 low-and middle-income countries. PLoS Med. 9, e1001166 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whitley R. Global mental health: concepts, conflicts and controversies. Epidemiol. Psychiatr. Sci 24, 285–291 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L. & Thornicroft G. Stigma and discrimination related to mental illness in low- and middle-income countries. Epidemiol. Psychiatr. Sci 24, 382–394 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubey C, Gupta N, Bhasin S, Muthal RA & Arora R. Prevalence and associated risk factors for postpartum depression in women attending a tertiary hospital, Delhi, India. Int. J. Soc. Psychiatry 58, 577–580 (2012). [DOI] [PubMed] [Google Scholar]
- 23.George C, Lalitha AR, Antony A, Kumar AV & Jacob KS Antenatal depression in coastal South India: prevalence and risk factors in the community. Int. J. Soc. Psychiatry 62, 141–147 (2016). [DOI] [PubMed] [Google Scholar]
- 24.Patel HL et al. Characteristics of postpartum depression in Anand district, Gujarat, India. J. Trop. Pediatr 61, 364–369 (2015). [DOI] [PubMed] [Google Scholar]
- 25.Shidhaye P, Shidhaye R. & Phalke V. Association of gender disadvantage factors and gender preference with antenatal depression in women: a cross-sectional study from rural Maharashtra. Soc. Psychiatry Psychiatr. Epidemiol 52, 737–748 (2017). [DOI] [PubMed] [Google Scholar]
- 26.Nath A, Metgud CS, Krishna M, Venkatesh S. & Murthy GVS Prenatal Depression and Its Associated Risk Factors Among Pregnant Women in Bangalore: A Hospital Based Prevalence Study. Front. Public Health 7, 108 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahendran R, Puthussery S. & Amalan M. Prevalence of antenatal depression in South Asia: a systematic review and meta-analysis. J Epidemiol Community Health 73, 768–777 (2019). [DOI] [PubMed] [Google Scholar]
- 28.Rathod SD, Honikman S, Hanlon C. & Shidhaye R. Characteristics of perinatal depression in rural central, India: a cross-sectional study. Int. J. Ment. Health Syst 12, 68 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gururaj G. & NMHS Collaborators Group. National Mental Health Survey of India, 2015–16: Prevalence, patterns and outcomes. (2016). [Google Scholar]
- 30.Supraja TA, Varghese M, Desai G. & Chandra PS The relationship of gender preference to anxiety, stress and family violence among pregnant women in urban India. Int. J. Cult. Ment. Health 9, 356–363 (2016). [Google Scholar]
- 31.Madhavan prabhakaran GK, D’Souza MS & Nairy KS Prevalence of pregnancy anxiety and associated factors. Int. J. Afr. Nurs. Sci 3, 1–7 (2015). [Google Scholar]
- 32.Gurung RA, Dunkel-Schetter C, Collins N, Rini C. & Hobel CJ Psychosocial predictors of prenatal anxiety. J. Soc. Clin. Psychol 24, 497–519 (2005). [Google Scholar]
- 33.Chan CY et al. Antenatal anxiety in the first trimester: Risk factors and effects on anxiety and depression in the third trimester and 6-week postpartum. Open J. Psychiatry (2013). [Google Scholar]
- 34.Haber MG, Cohen JL, Lucas T. & Baltes BB The relationship between self-reported received and perceived social support: A meta-analytic review. Am. J. Community Psychol 39, 133–144 (2007). [DOI] [PubMed] [Google Scholar]
- 35.Cobb S. Social support as a moderator of life stress. Psychosom. Med (1976). [DOI] [PubMed] [Google Scholar]
- 36.Coker AL, Watkins KW, Smith PH & Brandt HM Social support reduces the impact of partner violence on health: application of structural equation models. Prev. Med 37, 259–267 (2003). [DOI] [PubMed] [Google Scholar]
- 37.Ozbay F. et al. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry Edgmont 4, 35 (2007). [PMC free article] [PubMed] [Google Scholar]
- 38.Cohen S. & Wills TA Stress, social support, and the buffering hypothesis. Psychol. Bull 98, 310–357 (1985). [PubMed] [Google Scholar]
- 39.Coker AL et al. Social support protects against the negative effects of partner violence on mental health. J. Womens Health Gend. Based Med. 11, 465–476 (2002). [DOI] [PubMed] [Google Scholar]
- 40.Fathima FN et al. Assessment of ‘Accredited Social Health Activists’—A National Community Health Volunteer Scheme in Karnataka State, India. J. Health Popul. Nutr 33, 137–145 (2015). [PMC free article] [PubMed] [Google Scholar]
- 41.Census of India - 2011. (2011). [Google Scholar]
- 42.Madhivanan P. et al. Increasing antenatal care and HIV testing among rural pregnant women with conditional cash transfers to self-help groups: an evaluation study in rural Mysore, India. J. Sex. Transm. Dis. 2013, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kojima N. et al. Implementing and sustaining a mobile medical clinic for prenatal care and sexually transmitted infection prevention in rural Mysore, India. BMC Infect. Dis 17, 189 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matthey S. Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depression and Anxiety https://onlinelibrary.wiley.com/doi/abs/10.1002/da.20415 (2008) doi: 10.1002/da.20415. [DOI] [PubMed] [Google Scholar]
- 45.Gibson J, McKenzie-McHarg K, Shakespeare J, Price J. & Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr. Scand 119, 350–364 (2009). [DOI] [PubMed] [Google Scholar]
- 46.Cox JL, Holden JM & Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987). [DOI] [PubMed] [Google Scholar]
- 47.Kozinszky Z. & Dudas RB Validation studies of the Edinburgh Postnatal Depression Scale for the antenatal period. J. Affect. Disord 176, 95–105 (2015). [DOI] [PubMed] [Google Scholar]
- 48.Fernandes MC et al. Assessing prenatal depression in the rural developing world: a comparison of two screening measures. Arch. Womens Ment. Health 14, 209–216 (2011). [DOI] [PubMed] [Google Scholar]
- 49.Matthey S, Fisher J. & Rowe H. Using the Edinburgh postnatal depression scale to screen for anxiety disorders: Conceptual and methodological considerations. J. Affect. Disord 146, 224–230 (2013). [DOI] [PubMed] [Google Scholar]
- 50.McFarlane J, Parker B, Soeken K. & Bullock L. Assessing for Abuse During Pregnancy: Severity and Frequency of Injuries and Associated Entry Into Prenatal Care. JAMA 267, 3176–3178 (1992). [DOI] [PubMed] [Google Scholar]
- 51.Kalokhe A. et al. Domestic violence against women in India: A systematic review of a decade of quantitative studies. Glob. Public Health 12, 498–513 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arora P. & Aeri BT Burden of antenatal depression and its risk factors in Indian settings: A systematic review. Indian J. Med. Spec 10, 55 (2019). [Google Scholar]
- 53.Hayes AF Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. (Guilford Press, 2013). [Google Scholar]
- 54.Sheeba B. et al. Prenatal Depression and Its Associated Risk Factors Among Pregnant Women in Bangalore: A Hospital Based Prevalence Study. Front. Public Health 7, (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nongrum R, Thomas E, Lionel J. & Jacob KS Domestic Violence as a Risk Factor for Maternal Depression and Neonatal Outcomes: A Hospital-Based Cohort Study. Indian J. Psychol. Med 36, 179 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ajinkya S, Jadhav PR & Srivastava NN Depression during pregnancy: Prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind. Psychiatry J. 22, 37 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Srinivasan N. et al. Assessment of burden of depression during pregnancy among pregnant women residing in rural setting of Chennai. J. Clin. Diagn. Res. JCDR 9, LC08 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raman S, Srinivasan K, Kurpad A, Razee H. & Ritchie J. “Nothing Special, Everything Is Maamuli”: Socio-Cultural and Family Practices Influencing the Perinatal Period in Urban India. PLOS ONE 9, e111900 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rodrigues M, Patel V, Jaswal S. & De Souza N. Listening to mothers: qualitative studies on motherhood and depression from Goa, India. Soc. Sci. Med 57, 1797–1806 (2003). [DOI] [PubMed] [Google Scholar]
- 60.Roomruangwong C. & Epperson CN Perinatal depression in Asian women: prevalence, associated factors, and cultural aspects. Asian Biomed. 5, 179–193 (2011). [Google Scholar]
- 61.Takegata M, Ohashi Y, Lazarus A. & Kitamura T. Cross-national differences inpsychosocial factors of perinatal depression: A systematic review of India and Japan in Healthcare vol. 5 91 (Multidisciplinary Digital Publishing Institute, 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Clarke K, King M. & Prost A. Psychosocial Interventions for Perinatal Common Mental Disorders Delivered by Providers Who Are Not Mental Health Specialists in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. PLoS Med. 10, (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rahman A. et al. Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bull. World Health Organ. 91, 593–601I (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Singla DR et al. Psychological Treatments for the World: Lessons from Low- and Middle-Income Countries. Annu. Rev. Clin. Psychol 13, 149–181 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chowdhary N. et al. The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: A systematic review. Best Pract. Res. Clin. Obstet. Gynaecol 28, 113–133 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.House JS, Landis KR & Umberson D. Social relationships and health. Science 241, 540–545 (1988). [DOI] [PubMed] [Google Scholar]
- 67.Holt-Lunstad J, Smith TB & Layton JB Social relationships and mortality risk: a meta-analytic review. PLoS Med. 7, e1000316 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cohen S. Social relationships and health. Am. Psychol. 59, 676–684 (2004). [DOI] [PubMed] [Google Scholar]
- 69.Strine TW, Chapman DP, Balluz L. & Mokdad AH Health-related quality of life and health behaviors by social and emotional support. Their relevance to psychiatry and medicine. Soc. Psychiatry Psychiatr. Epidemiol. 43, 151–159 (2008). [DOI] [PubMed] [Google Scholar]
- 70.Dennis C-L Peer support within a health care context: a concept analysis. Int. J. Nurs. Stud 40, 321–332 (2003). [DOI] [PubMed] [Google Scholar]
- 71.Sahu P, Hansa J, Mohanty DP & Mishra SN Prevalence and pattern of anxiety and depressive disorders in pregnant women attending antenatal clinic. Indian J. Public Health Res. Dev 9, 52–58 (2018). [Google Scholar]
- 72.Aneja J. et al. Perceived stress and its psychological correlates in pregnant women: an Indian study. Int. J. Cult. Ment. Health 11, 268–279 (2018). [Google Scholar]