1. Introduction
Mechanical ventilation is a common life-saving protocol, but it has also been linked to ventilator-associated lung injury (VALI), a progressive injury caused by positive pressure ventilation [1]. Despite decades of research, lung-protective ventilation (LPV) with low tidal volume (VT) remains one of the few effective protocols for patients with acute respiratory distress syndrome (ARDS) [[2], [3], [4], [5]]. Growing evidence suggests that low VT may also benefit critically ill patients without pre-existing lung injury [[6], [7], [8], [9], [10], [11]]. In addition to low VT, adequate positive-end expiratory pressure (PEEP) and early titration of oxygen concentration (FiO2) are important components of LPV that minimize atelectasis [12,13] and oxygen toxicity [[14], [15], [16]], respectively.
The emergency department (ED) is a crucial setting for the prevention and treatment of VALI. ED overcrowding, boarding, and increased ICU admissions have tripled the amount of critical care and prolonged mechanical ventilation delivered in US EDs [17,18]. Of the estimated 240,000 patients mechanically ventilated in US EDs each year, one-quarter are ventilated for more than 5 h [19,20]. These initial hours of care are influential in the outcome of critically ill patients, as VALI has been shown to occur within minutes to hours of initiating mechanical ventilation [[21], [22], [23]] and progression to ARDS occurs early during ventilation of at-risk patients [7]. For these reasons, initial ventilator settings provided in the immediate post-intubation period can be critically important in determining patient outcomes. Observational data show large VT is commonly used in the ED, ED VT influences ventilation strategy in the ICU, and injurious early ventilation strategies are associated with worse clinical outcomes, implicating the ED as a vital link in the provision of LPV [24,25].
Standardization of mechanical ventilation through order sets and protocols provides an evidence-based and cost-effective opportunity to reduce variability in the care of ventilated ED patients [26]. Respiratory care protocols administered by non-physician staff have been shown to improve arterial blood gas sampling [27,28], early ventilator weaning, [29,30] and adoption of PEEP-FiO2 combination guidelines [31]. Successful adherence to a VT-focused ventilator order set further supports the feasibility of protocol-driven ventilation in the ED [32]. Implementation of a similar mechanical ventilation protocol in an academic ED increased ventilator-free days and hospital-free days while being associated with significantly decreased hospital mortality [33]. Based on the association between lung protective ventilation and improved clinical outcomes demonstrated in the LOV-ED study and the previously demonstrated prevalence of non-protective ventilation in multiple EDs, an RT-driven LPV protocol was implemented in the ED of a large, academic medical center to standardize care of mechanically ventilated ED patients. We hypothesized that implementation of this protocol would improve adherence to LPV ventilation parameters and improve clinical outcomes of patients intubated and mechanically ventilated in the ED.
2. Methods
2.1. Study design
This retrospective before-after observational cohort study was conducted at an academic 60,000-visit ED between March 2016 and July 2018, 15 months before through 13 months after the implementation of a lung-protective mechanical ventilation protocol. Inclusion criteria were adult patients (age ≥ 18 years) receiving mechanical ventilation following intubation while in the ED. Exclusion criteria included death or extubation while in the ED, missing height or ED VT in the electronic medical record (EMR), non-invasive ventilation only, and transfer from the ED to another facility. This study is reported in accordance with the Standards for Quality Improvement Reporting Excellence (SQUIRE) Statement: Guidelines for Reporting Observational Studies [34] and was approved by the local Institutional Review Board under a waiver of informed consent.
2.2. Protocol
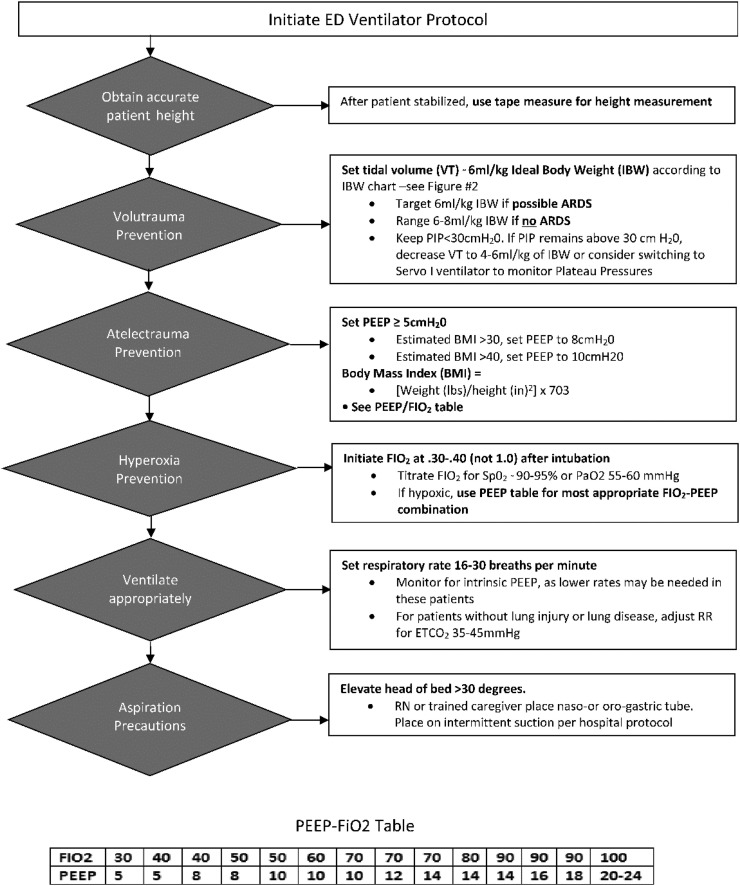
In June 2017, a new mechanical ventilation protocol was implemented in the ED to mimic the Lung Protective Ventilation Initiated in the Emergency Department (LOV-ED) study protocol [33]. The protocol was divided into five components, each intended to prevent a potential mechanism of VALI (Fig. 1 ). Mode selection of choice for this protocol was assist control-volume control (AC-VC).
Fig. 1.
Study protocol diagram.
Education for respiratory therapists included hands-on sessions with the mechanical ventilator, computer-based tutorial, and quiz. Tools were provided to respiratory therapists including laminated protocol sheets detailing ideal predicted body weight (PBW)-VT charts and tape measures to measure patient height. These tools were attached to the ED ventilators as part of standard protocol procedures. After implementation, weekly audits of all ventilated ED patients were performed to review adherence to the protocol, immediate feedback was provided, and adherence was reported at regular staff meetings.
2.3. Procedures
Baseline patient characteristics were abstracted from the EMR. Sequential organ failure assessment (SOFA) scores were calculated at the time of ED admission and 24 h after admission [35]. The first ventilator settings recorded in the ED and ICU were abstracted from the medical record. Names of the treating respiratory therapist, intubating physician (typically a resident), and attending physician were also recorded. Data were abstracted by trained data abstractors with regular meetings and monitoring of data collection. All variables were collected in a standardized format using a standard case report form.
2.4. Outcomes
The primary outcome of this study was mean difference in VT (mL/kg) administered in the ED between groups. Difference in VT was selected as the primary outcome because it is the most widely studied and supported mediator of VALI and would reflect a change in clinical practice induced by the protocol. Secondary outcomes included 24-h change in SOFA score, ventilator-free days, ICU VT, protocol adherence, mortality, ARDS, hospital-free days, and ventilator-associated pneumonia (VAP). We also tested adherence with individual protocol elements.
2.5. Definitions
Patient height and weight from the hospital encounter were used to calculate BMI and PBW as shown previously [36]. LPV was defined as the use of VT ≤ 8 mL/kg PBW.
SOFA scores were calculated as described previously [35]. Saturation by pulse oximetry (SpO2)/FiO2 ratios were used to calculate the SOFA score because of ED arterial blood gas infrequency. SpO2/FiO2 ratios approximated partial pressure of oxygen (PaO2)/FiO2 ratios using methods validated in a prior report [37]. Due to the shape of the oxyhemoglobin dissociation curve, any SpO2 values above 97% was assigned a zero for the respiratory component of the SOFA score because large PaO2 changes can occur with small changes in the SpO2 near 100% [38].
Adherence to each facet of the ventilator protocol was determined according to Fig. 1. If the patient received a tidal volume ≤ 8 mL/kg, they were considered adherent to the “Volutrauma Prevention” facet of the protocol. PEEP was to be ≥5 cm H20 to satisfy “Atelectrauma Prevention.” For “Hyperoxia Prevention,” FiO2 must have been set to between 0.3 and 0.4 immediately within 15 min of intubation. If a higher FiO2 was initially selected, the corresponding PEEP value must have been in accordance with the provided PEEP-FiO2 table (Fig. 1) to be considered adherent. Respiratory rate was to be set between 16 and 30 breaths per minute. Head-of-bed elevation was not included in adherence determinations due to lack of notation in the medical record (98.2% missing). For a patient to be considered adherent to the full protocol, each facet must have been satisfied. If any data value was not adherent, that patient was considered not adherent to the protocol.
ARDS was defined according to the Berlin definition through hospital day five [10,24,39,40]. A panel of three research team clinicians reviewed blinded chest radiographs independently and classified them as “consistent”, “inconsistent”, or “equivocal” for ARDS, and the diagnosis was made by consensus. Each member of the panel reviewed a set of training radiographs [41] prior to study participation and was blinded to protocol group and all other clinical data during the chest radiograph review. Patients were assumed to have clinical evidence of left atrial hypertension if respiratory failure was attributed to congestive heart failure or dialysis-dependent end-stage renal disease in the EMR, and thus were categorized as “not ARDS.”
VAP was defined as clinical suspicion for pneumonia by a board-certified intensivist with initiation of antibiotic treatment for a lower respiratory tract infection >48 h after initiation of mechanical ventilation, among patients not already being treated for pneumonia [42].
2.6. Sample size
A mean detectable difference for ED VT of 0.33 mL/kg (SD 1.28) for pre- versus post-protocol (power 0.8, alpha 0.05) required 476 patients (238 pre-protocol patients and 238 post-protocol patients). A mean difference of 0.33 mL/kg was chosen due to the low mean VT observed in a sample of pre-protocol patients performed prior to final data analysis. Given the already low pre-protocol tidal volume, the likelihood of demonstrating a smaller difference in tidal volume after protocol would require a greater number of patients than would be feasible for the study, but one could not expect a different that would bring the mean tidal volume to <6 mL/kg. We determined that a 0.33 mL/kg change was a compromise vale that would detect a meaningful change in clinical practice.
2.7. Analysis
Chi-square tests, Wilcoxon Mann-Whitney tests, and Fisher's exact tests compared distributions of baseline characteristics between the two groups. A scatterplot was used to visualize associations between ED and ICU VT.
Univariable and multivariable regression assessed the impact of the protocol on clinical and ventilator outcomes. For the primary outcome, a log-transformation of outcome was used, since the error terms on the continuous outcomes followed a right-skewed distribution. Linear, logistic, and negative binomial regression were used to estimate secondary outcomes as appropriate.
Covariate selection was guided by clinical knowledge and previous literature [33], and, stepwise backwards selection guided by Akaike Information Criterion (AIC) was used to select the final model. Respiratory therapist and intubator were also included as fixed effects to account for variance, observed and unobserved, associated with each fixed effect. A post hoc test for effect modification of protocol effect by subject height was conducted by testing an interaction term and then stratifying the analysis by protocol time (pre- vs. post-protocol).
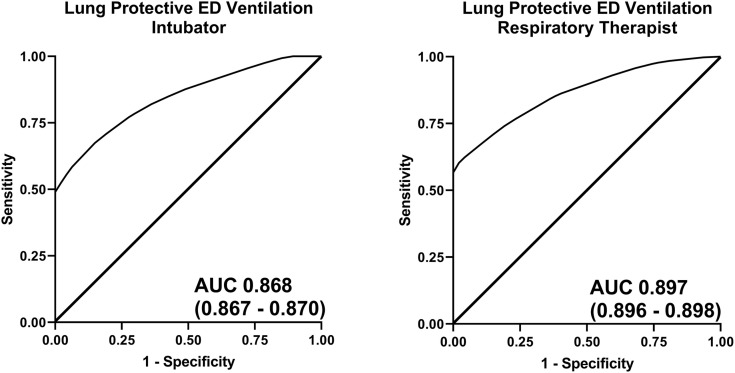
Differences in the time to ARDS and VAP (in days) between the protocol groups were assessed using log-rank tests and univariable Cox proportional hazards regression models. Finally, variation in ED LPV rates (VT ≤ 8 mL/kg) by intubator and respiratory therapist were estimated with risk-adjustment (adjusting for: sex, BMI, and initial SOFA score) and reliability-adjustment [43]. Predictive capability of attending physician, intubating physician, and respiratory therapist for ED LPV were separately estimated using univariable logistic regression models to estimate the area under the curve (AUC), using bootstrapping of 1000 independent data samples to estimate precision of the AUC confidence interval. Data analysis was completed in R (version 3.6; RStudio Inc., Vienna, Austria) and SAS (version 9.4; SAS Institute, Inc., Cary, NC), and figures were created in Prism (version 8.2, GraphPad, Inc., San Diego, CA).
2.8. Sensitivity analysis
A post hoc sensitivity analysis was conducted restricting the study population to resemble the eligibility criteria of a previous before-after study of LPV protocols in the ED [33]: excluding subjects that had ARDS at hospital admission or were extubated or died within 24 h.
3. Results
3.1. Characteristics of study subjects
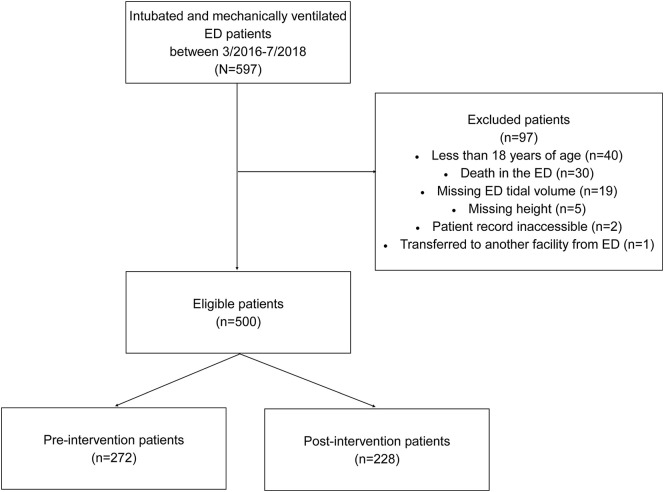
A total of 500 patients were enrolled in this study Supplemental Figure 1. Baseline characteristics of the study population are shown in Table 1. All measured baseline characteristics, including initial SOFA scores and ED length of ventilation, were similar between the two groups.
Supplemental Fig. 1.
Flow diagram.
Table 1.
Subject demographics and ventilator settings pre/post.
| Total |
Pre-intervention |
Post-intervention |
p-Value | ||||
|---|---|---|---|---|---|---|---|
| N | n | n | |||||
| Total | 500 | 272 | 54.4% | 228 | 45.6% | ||
| Age (yrs.) | |||||||
| Median (IQR) | 58.0 | (43.0–71.0) | 57.5 | (41.5–70.0) | 45.0 | (45.0–71.0) | 0.378 |
| Sex | 0.769 | ||||||
| Male | 293 | 58.6% | 161 | 59.2% | 132 | 57.9% | |
| Female | 207 | 41.4% | 111 | 40.8% | 96 | 42.1% | |
| Height (cm) | 172.7 | (165.1–180.3) | 172.7 | (165.1–180.3) | 172.7 | (165.1–180.2) | 0.664 |
| Weight (kg) | 82.3 | (68.0–97.1) | 84.9 | (69.9–97.9) | 80.6 | (66.4–95.2) | 0.271 |
| BMI | 27.4 | (23.7–32.6) | 28.0 | (23.7–33.1) | 27.1 | (23.7–32.2) | 0.242 |
| Reason for intubation | 0.295 | ||||||
| Asthma | 4 | 0.8% | 3 | 1.1% | 1 | 0.4% | |
| Chronic obstructive pulmonary disease | 5 | 1.0% | 5 | 1.8% | 0 | 0.0% | |
| Chronic heart failure/pulmonary edema | 20 | 4.0% | 9 | 3.3% | 11 | 4.8% | |
| Sepsis | 71 | 14.2% | 42 | 15.4% | 29 | 12.7% | |
| Trauma | 86 | 17.2% | 51 | 18.8% | 35 | 15.4% | |
| Cardiac arrest | 15 | 3.0% | 9 | 3.3% | 6 | 2.6% | |
| Alcohol/drug overdose | 76 | 15.2% | 41 | 15.1% | 35 | 15.4% | |
| Neurological | 119 | 23.8% | 49 | 18.0% | 55 | 24.1% | |
| Other | 104 | 20.8% | 63 | 23.2% | 56 | 24.6% | |
| SOFA score, median (IQR) | |||||||
| Initial SOFA | 2 | (0–4) | 0 | (0–4) | 2 | (0–4) | 0.419 |
| 24-hour SOFA | 4 | (2–7) | 4 | (2–6) | 4 | (2–7) | 0.185 |
| ED length of ventilation (min), median (IQR) | 106.0 | 66.0–161.5 | 101.5 | 66.5–159.5 | 107.5 | 65.5–163.0 | 0.317 |
| ED ventilator variables | |||||||
| Tidal volume (mL), median (IQR) | 425 | (380–450) | 440 | (400–462.5) | 405 | (370–450) | <0.001 |
| Tidal volume (ml/kg IBW), median (IQR) | 6.4 | (5.8–7.1) | 6.5 | (5.8–7.4) | 6.2 | (5.8–6.7) | <0.001 |
| PEEP, cmH2O, median (IQR) | 5 | (5–5) | 5 | (5–5) | 5 | (5–5) | 0.068 |
| Respiratory rate, median (IQR) | 18 | (16–20) | 18 | (15.5–20) | 18 | (16–20) | 0.006 |
| FiO2, median (IQR) | 50 | (40–75) | 60 | (40–80) | 50 | (40–70) | 0.029 |
| Lung-protective ventilation⁎⁎ (%) | 448 | 90.7 | 235 | 87.7 | 213 | 94.3 | 0.012 |
| Ventilator Mode | 0.068 | ||||||
| VC-AC | 454 | 90.8 | 238 | 87.5 | 216 | 94.7 | |
| PC-AC | 19 | 3.8 | 13 | 4.8 | 6 | 2.6 | |
| VC-SIMV | 14 | 2.8 | 10 | 3.7 | 4 | 1.8 | |
| PC-SIMV | 12 | 2.4 | 10 | 3.7 | 2 | 0.9 | |
| PS | 1 | 0.3 | 1 | 0.4 | 0 | 0.0 | |
| ED protocol adherence | 100 | 20.0 | 37 | 13.6 | 63 | 27.6 | <0.001 |
| ICU ventilator variables | |||||||
| Tidal volume (mL) | 430 | 380–475 | 439.5 | 381–480 | 420 | 380–460 | 0.161 |
| Tidal volume (ml/kg IBW) | 6.4 | 5.9–7.3 | 6.6 | 5.9–7.4 | 6.3 | 5.9–7.2 | 0.254 |
| PEEP, cmH2O | 5 | (5–5) | 5 | (5–5) | 5 | (5–5) | 0.322 |
| Respiratory rate | 18 | 15–22 | 18 | 15–22 | 18 | 16–21 | 0.340 |
| FiO2 (%) | 40 | 40–60 | 40 | 40–60 | 40 | 40–55 | 0.128 |
| Lung-protective ventilation⁎⁎ (%) | 407 | 82.2 | 219 | 82.0 | 188 | 84.7 | 0.433 |
| Ventilator mode | 0.002 | ||||||
| VC-AC | 238 | 48.2 | 135 | 50.0 | 103 | 46.0 | |
| PC-AC | 37 | 7.5 | 23 | 8.5 | 14 | 6.3 | |
| VC-SIMV | 4 | 0.8 | 2 | 0.7 | 2 | 0.9 | |
| PRVC-AC | 97 | 19.6 | 38 | 14.1 | 59 | 26.3 | |
| PS | 76 | 15.4 | 40 | 14.8 | 36 | 16.1 | |
| ICU protocol adherence | 132 | 33.8 | 55 | 20.2 | 77 | 33.8 | 0.001 |
Lung protective ventilation defined as tidal volume ≤ 8 mL/kg.
3.2. Main results
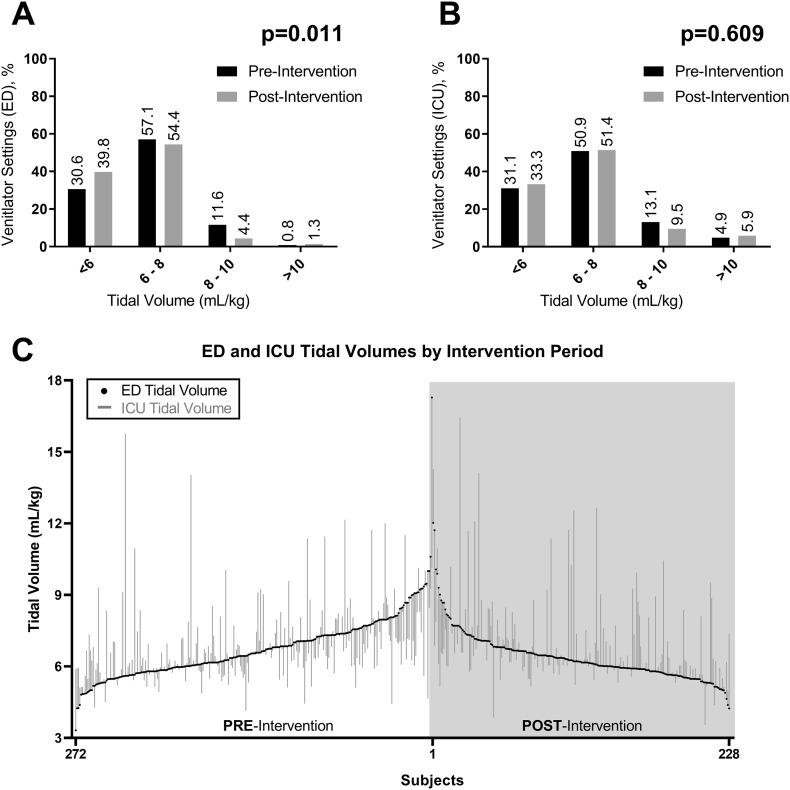
Of the study cohort, 272 subjects (54.4%) were in the pre-protocol group and 228 (45.6%) were in the post-protocol group (Table 1). Without adjustment, ED VTs were smaller in the post-protocol group (6.2 vs. 6.5 mL/kg IBW, p < 0.001), and more patients received LPV in the post-protocol group (94.3% vs. 87.7%, p = 0.012) (Table 1) than the pre-protocol group. Time to ARDS and time to VAP did not differ between the pre- and post-protocol groups (ARDS: HR 0.64 [0.34–1.20] and VAP: HR 1.12 [0.58–2.18]). Overall, ICU and ED VTs were moderately correlated (r2 = 0.484, p < 0.001) (Fig. 2 ).
Fig. 2.
(A) Upper left: differences in ED tidal volume by pre- and post-intervention; (B) upper right: differences in ICU tidal volume by pre- and post-intervention; (C) lower: plot of differences in individual subjects' ED (black dot) to ICU tidal volume in pre- and post-intervention groups. Differences between ED and ICU tidal volume are represented by the grey line. Subjects are rank-ordered by ED tidal volume.
After adjustment for sex, BMI, and initial SOFA score, ED VT remained lower in the post-protocol group when compared to the pre-protocol group (−0.76 mL/kg [95%CI −1.03 to −0.48]) (Table 2 ). There was no difference in proportion of patients who developed ARDS, VAP, or died between the protocol groups. There were differences in the change in SOFA scores after adjustment with the post-protocol group having greater increases in SOFA score from the ED to 24-hour score (1.40 [95%CI: 0.64 to 2.17]) (Table 2). When GCS was removed from the SOFA calculation, there was no longer a significant difference in the change in SOFA scores.
Table 2.
Regression models.
| n/mean | %/SE | Unadjusted OR/between group difference (95% CI) |
Adjusted⁎ OR/between group difference (95% CI) |
|
|---|---|---|---|---|
| Primary outcome | ||||
| ED tidal volume (mL/kg) | 6.6 | 0.1 |
−0.37 (−0.58 to −0.15) p = 0.001 |
−0.71 (−0.94 to −0.48) p < 0.001 |
| Log-transformed ED TV | – | – |
−0.05 (−0.08 to −0.02) p = 0.001 |
−0.10 (−0.13 to −0.06) p < 0.001 |
| Secondary outcomes | ||||
| ARDS, n (%) | 42 | 8.4% | 0.64 (0.33–1.23) p = 0.179 |
0.57 (0.08–4.11) p = 0.577 |
| VAP, n (%) | 35 | 7.0% | 1.14 (0.58–2.27) p = 0.703 |
0.76 (0.12–4.61) p = 0.762 |
| 28-day hospital free days, mean (SE) | 14.7 | 0.5 | −0.03 (−0.26 to 0.20) p = 0.798 |
−0.30 (−0.65 to 0.04) p = 0.085 |
| Change in SOFA, mean (SE) | −1.0 | 0.2 | 0.26 (−0.34 to 0.86) p = 0.392 |
1.42 (0.67 to 2.18) p < 0.001 |
| Change in SOFA (excluding GCS), mean (SE) | −0.79 | 0.1 | −0.01 (−0.47 to 0.46) p = 0.983 |
0.50 (−0.02 to 1.02) p = 0.061 |
| Change in SOFA components | ||||
| PaO2/FiO2 ratio | −1.0 | 0.1 | −0.19 (−0.51 to 0.14) P = 0.260 |
0.39 (0.12 to 0.67) p = 0.006 |
| Platelets | 0.2 | 0.0 | 0.06 (−0.05 to 0.16) p = 0.279 |
0.08 (−0.07 to 0.23) p = 0.304 |
| Glasgow Coma Score | −0.1 | 0.1 | 0.27 (−0.06 to 0.59) p = 0.107 |
0.90 (0.46 to 1.35) p < 0.001 |
| Creatinine | −0.1 | 0.0 | −0.04 (−0.16 to 0.07) p = 0.460 |
−0.14 (−0.30 to 0.01) p = 0.075 |
| Bilirubin | 0.0 | 0.1 | 0.17 (−0.09 to 0.43) p = 0.208 |
0.28 (−7.06 to 7.63) p = 0.940 |
| Mean arterial pressure | 0.2 | 0.1 | 0.24 (−0.00 to 0.49) p = 0.055 |
0.30 (−0.03 to 0.63) p = 0.073 |
| Mortality, n (%) | 120 | 24.0% | 1.03 (0.68–1.57) p = 0.873 |
1.22 (0.50–3.00) p = 0.666 |
| Total length of ventilation, (min) | 3831 | 272 | 0.06 (−0.13 to 0.25) p = 0.527 |
−0.12 (−0.40 to 0.17) p = 0.424 |
| ED volume settings | ||||
| TV cut-point of 8, n (%) | 448 | 90.6% |
2.29 (1.17–4.48) p = 0.015 |
3.92 (0.35–43.99) p = 0.268 |
| ICU volume settings | ||||
| Continuous TV, mean (SE) | 6.8 | 0.1 | −0.05 (−0.34 to 0.24) p = 0.739 |
−0.15 (−0.52 to 0.22) p = 0.416 |
| Log-transformed ICU TV | – | – | −0.01 (−0.05 to 0.03) p = 0.566 |
−0.03 (−0.08 to 0.01) p = 0.180 |
| TV cut-point of 8, n (%) | 407 | 83.2% | 1.29 (0.75–1.95) p = 0.435 |
1.97 (0.59–6.50) p = 0.268 |
Bold indicates p-value <0.05.
Adjusted for: sex, BMI (logarithmic transform), height (logarithmic transform), initial SOFA score, respiratory therapist, and intubator.
Subject height modified the relationship between the protocol and use of ED LPV (p = 0.044). Before the protocol, a 10% increase in subject height was associated with a 3.39 (95% CI 2.14–4.64) times higher odds of ED LPV. Whereas, after the protocol, the association between height and the protocol was no longer significant (95%CI 0.24–2.46).
3.3. Protocol adherence
Protocol adherence in the ED was greater in the post-protocol group (27.6% vs. 13.6%, p < 0.001) (Table 1) than the pre-protocol group. Adherence to all components in the protocol was modest in both the pre- and post-group (Table 3 ). Using the same methods, ICU protocol adherence increased from 20.2% before protocol to 33.8% after protocol (p = 0.001). When missing protocol components were assumed adherent for sensitivity analysis, neither relationship changed significantly.
Table 3.
Protocol adherence
| Total |
Pre |
Post |
||||
|---|---|---|---|---|---|---|
| Adherent n (%) |
Missing n (%) |
Adherent n (%) |
Missing n (%) |
Adherent n (%) |
Missing n (%) |
|
| ED protocol components | ||||||
| PEEP FiO2 or FiO2 (hyperoxia) | 174 (32.8) | 1 (0.2) | 75 (27.6) | 1 (0.4) | 99 (43.4) | 0 (0.0) |
| PEEP (atelectrauma) | 351 (70.2) | 15 (3.0) | 181 (66.5) | 7 (2.6) | 170 (74.6) | 8 (3.5) |
| Respiratory rate (ventilate) | 397 (79.4) | 2 (0.4) | 203 (74.6) | 0 (0.0) | 194 (85.1) | 2 (0.9) |
| Tidal volume (volutrauma) | 448 (89.6) | 6 (1.2) | 235 (86.4) | 4 (1.5) | 213 (93.4) | 2 (0.9) |
| ICU protocol components | ||||||
| PEEP FiO2 or FiO2 (hyperoxia) | 307 (61.4) | 6 (1.2) | 151 (55.5) | 2 (0.7) | 156 (68.4) | 4 (0.8) |
| PEEP (atelectrauma) | 368 (73.6) | 7 (1.4) | 195 (71.7) | 2 (0.7) | 173 (75.9) | 5 (2.2) |
| Respiratory rate (ventilate) | 342 (68.4) | 6 (1.2) | 182 (66.9) | 2 (0.7) | 160 (70.2) | 4 (1.8) |
| Tidal volume (volutrauma) | 407 (81.4) | 11 (2.2) | 219 (80.5) | 5 (1.8) | 188 (82.5) | 6 (2.6) |
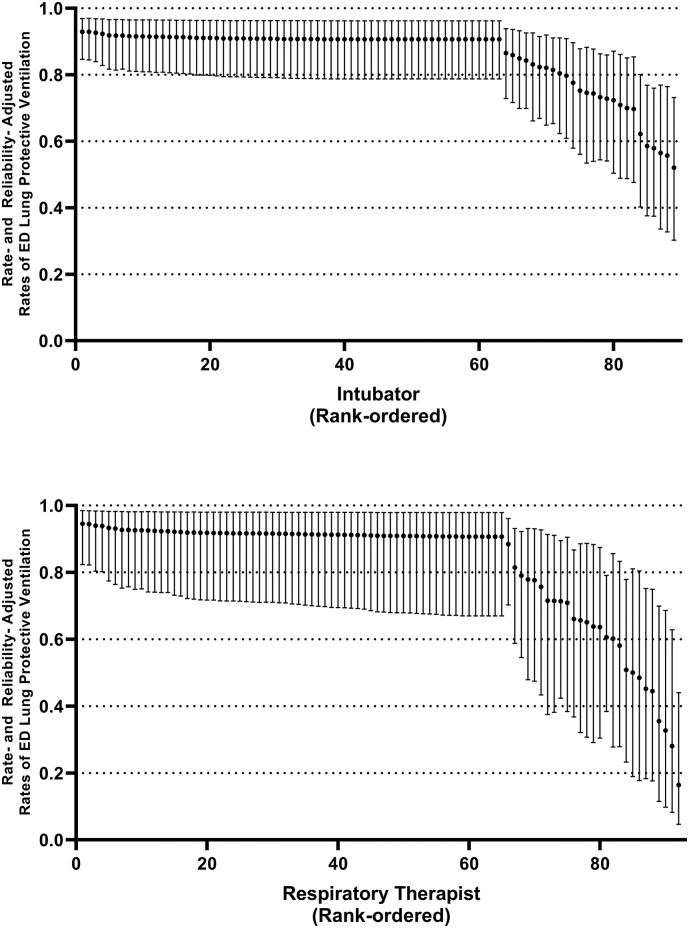
3.4. Variation by intubator and respiratory therapist
Adherence to use of LPV (VT ≤ 8 mL/kg IBW) varied by intubating physician and respiratory therapist (Fig. 3 ). More variation was observed by respiratory therapists than by intubator in adjusted proportion of ED LPV. Across intubators, the median adjusted rate of ED LPV was 90.7% (IQR 84.3–90.9). Whereas among respiratory therapists, the median adjusted proportion was similar, but more variation was observed (median 90.9% [IQR 77.8–91.7]). The impact of the care team in predicting adherence with the protocol was estimated with univariable models with respiratory therapist or intubator as the predictor and ED LPV as the outcome. Overall, the individual respiratory therapist affected ED LPV more than the intubating physician (Fig. 4 ), and respiratory therapists become even stronger predictors after the intervention (AUC 0.919 [95% CI 0.917–0.920]). There was no association between attending physician and use of ED LPV.
Fig. 3.
Variation in ED Lung Protective Ventilation Rates by Intubator and Respiratory Therapist.
Fig. 4.
Variation in ED Lung Protective Ventilation Rates by Intubator and Respiratory Therapist.
3.5. Sensitivity analysis
Of this study cohort, 5.2% had ARDS on arrival to the ED and 41.2% were extubated on the date of admission; no subjects died on the date of admission. In the sensitivity analysis including only patients who remained ventilated beyond 24 h, the adjusted associations between the protocol and ED VT (adj. β −0.16 [95% CI −0.21 to −0.12]) and between the protocol and mortality (aOR 0.28 [95% CI 0.02–3.41]) were similar to the primary analysis.
4. Discussion
This before-after observational cohort study was conducted to determine the impact of a bundled mechanical ventilator protocol on use of LPV in an academic ED. We found that such a protocol can be implemented and influence ventilation practices in the ED. After adjusting for multiple confounders, protocol administration was associated with a 0.76 mL/kg reduction in ED VT. Though LPV was widely used in the ED pre-protocol group, use of VT <8 mL/kg was significantly increased after implementation of the protocol. Adherence to PEEP, FiO2, and respiratory rate protocol parameters were improved in the ED post-protocol group, though full ED protocol adherence increased from 13.6% to only 27.6%. Despite the observed changes in ventilation practices, protocol implementation did not influence any of the measured clinical outcomes, including ARDS, VAP, hospital-free days, or mortality.
Our study is the third to analyze the effect of a bundled, lung-protective mechanical ventilation protocol administered in the ED. A previous before-after study, the LOV-ED trial, demonstrated a reduction in pulmonary complications and mortality following protocol implementation [33]. Our study did not find a significant difference in clinical outcomes between groups despite improvement in overall protocol adherence and reduction in ED VT. There are multiple potential explanations for a finding of a statistically significant decrease in ED VT without a change in clinical outcomes. First, our study was primarily quality improvement (QI) in nature, and thus was not adequately powered to detect a change in clinical outcomes. Second, our study included patients who underwent extubation or death at <24 h following ED admission and those meeting ARDS criteria while in the ED. This creates a broader range of illness severity across our patient population and makes direct comparison in clinical outcomes between the studies difficult. However, a sensitivity analysis using the same exclusion criteria as the LOV-ED study did not significantly change our primary outcome (change in VT) or mortality. Third, we detected a 0.76 mL/kg adjusted difference in VT between the pre and post protocol groups, which differs significantly from the 2 mL/kg difference detected in the LOV-ED trial [33]. Though reductions of 1 mL/kg have been shown to decrease mortality in patients with ARDS [44], 0.76 mL/kg may not be sufficient to elicit a change in secondary outcomes in a population that was receiving high rates of LPV even before protocol. The injurious effects of very high tidal volumes may be much more than modest tidal volumes, so the relatively protective settings in the pre-intervention group may not have led to high rates of clinical deterioration. Alternatively, the lack of clinical change could support the results of multiple studies challenging the clinical benefit of low VT ventilation in populations including patients without ARDS [20,45].
Consistent adherence to all parameters of a complex, bundled protocol can be difficult to attain. Despite improvement in adherence to each facet of the ventilation protocol between the pre- and post-protocol groups, full adherence was seen in only 27.6% of ED patients in the post-protocol group. This finding can be at least partially attributed to protocol dissemination and implementation. Similar before-after respiratory protocol studies were prospective in nature and involved run-in periods of up to 6 months [[31], [32], [33]]. Our study, on the other hand, was retrospective and did not utilize a run-in period. While compliance to the protocol was monitored in the post-protocol group, these differences may have contributed to the observed sub-optimal adherence. The protocol parameter with the lowest adherence involved the setting of FiO2 between 0.30 and 0.40 or in accordance with ARDSNet PEEP-FiO2 table for hyperoxia prevention (37.7% in the post-protocol group). This finding is consistent with previous studies demonstrating frequent use of FiO2 levels >90% with little oxygen titration in mechanically ventilated ED patients [24,25]. While use of low VTs had become standard practice in the ED, our results suggest that immediate titration of FiO2 (Fig. 1) remains poor. Future studies of bundled care protocols should involve active identification of barriers to implementation to ensure successful translation into clinical practice.
ED and ICU patients in both protocol groups received LPV at a much higher proportion than previous reports. We found that 87.7% of ED patients (median VT of 6.5 mL/kg) and 82.0% of ICU patients (median VT of 6.6 mL/kg) intubated at our site were ventilated with LPV in the ED prior to protocol implementation. This differs significantly from previous studies demonstrating use of LPV in 23–55.7% of ED patients and 20–46% of ICU patients [24,32,33]. Our data more closely resembles the recent Low Tidal Volume Universal Support (LOTUS) trial feasibility study, which showed an average VT of 7.1 mL/kg and LPV percentage of 78.2% in the ICUs of 49 hospitals [46]. In this context, our findings could reflect a shift in general practice to low VT ventilation in all patients undergoing respiratory failure, regardless of ARDS status.
Our study found that variation in VT administration was greater among RTs than intubating physicians, suggesting that the RTs were most directly influencing ventilator settings. Previous survey studies have identified discomfort of emergency medicine residents and physicians in the care of mechanically ventilated patients, causing them to frequently defer care to respiratory therapists [47,48]. Our findings indicate that respiratory therapists are influential in determining ventilator settings, which highlights the importance of tailoring protocols for mechanically ventilated patients to respiratory therapy staff.
This study has several important limitations. As a before-after study, the results may be reflective of temporal changes in care. Since there were no other institutional efforts aimed at prophylactic LPV during the period of this study, however, we think that it remains likely that the ED protocol influenced care. The retrospective design of this study limits data available, but the research team took steps to validate data when possible and selected measures are likely to be recorded accurately. This study was conducted at a single academic teaching facility, which limits generalizability, but since prior reports were also single-center studies, we feel that local factors may lead to heterogeneity in treatment effects. ED providers' and respiratory therapists' awareness of this study may have introduced a Hawthorne effect, in which providers performed differently knowing they were being monitored. However, as quality improvement monitoring is part of the implementation of this intervention, we considered it an important parameter to capture and part of the treatment effect. Data were collected through chart review and providers were never directly observed. Finally, we did not include plateau pressure in our definition of LPV [[49], [50], [51]], because it could not be measured with our standard ED transport ventilators.
5. Conclusion
Implementation of a bundled, ED-based mechanical ventilation protocol is associated with a significant decrease in ED VT and increase in use of LPV. The protocol was not associated with change in any measured clinical outcomes, including ventilator-free days, ARDS, VAP, or mortality. The results of our study support the use of protocols to standardize care of ventilated ED patients and emphasize the importance of tailoring these protocols to respiratory therapists, who were shown to have a more significant impact on LPV use than intubating physician. Further study to maximize adherence to protocol parameters, particularly the immediate titration of FiO2, and clarify the influence of ED VT on patient-centered outcomes is warranted.
The following are the supplementary data related to this article.
Financial support
This research was supported by the University of Iowa Carver College of Medicine and Department of Emergency Medicine.
CRediT authorship contribution statement
Tyler M. Foley: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Writing - review & editing. Brittany A. Philpot: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing. Alysa S. Davis: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing. Morgan B. Swanson: Formal analysis, Data curation, Writing - original draft, Writing - review & editing. Karisa K. Harland: Formal analysis, Data curation, Writing - original draft, Writing - review & editing. Justin D. Kuhn: Writing - original draft, Writing - review & editing. Brian M. Fuller: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Nicholas M. Mohr: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing.
Declaration of competing interest
None.
Footnotes
This research was presented at the Society of Academic Emergency Medicine Great Plains Regional Conference, September 21, 2018, in St. Louis, Missouri.
References
- 1.Slutsky A.S., Ranieri V.M. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 2.Brower R.G., Matthay M.A., Morris A., Schoenfeld D., Thompson B.T., Wheeler A., et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 3.Meade M.O., Cook D.J., Guyatt G.H., Slutsky A.S., Arabi Y.M., Cooper D.J., et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 4.Amato M.B., Barbas C.S., Medeiros D.M., Magaldi R.B., Schettino G.P., Lorenzi-Filho G., et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 5.Villar J., Kacmarek R.M., Pérez-Méndez L., Aguirre-Jaime A. A high positive end-expiratory pressure, low tidal volume ventilatory strategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial. Crit Care Med. 2006;34(5):1311–1318. doi: 10.1097/01.CCM.0000215598.84885.01. [DOI] [PubMed] [Google Scholar]
- 6.A. Serpa Neto, S.O. Cardoso, J.A. Manetta, V.G. Pereira, D.C. Espósito, M.e.O. Pasqualucci, M.C. Damasceno, M.J. Schultz, Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis, JAMA 308(16) (2012) 1651–9. [DOI] [PubMed]
- 7.Fuller B.M., Mohr N.M., Drewry A.M., Carpenter C.R. Lower tidal volume at initiation of mechanical ventilation may reduce progression to acute respiratory distress syndrome: a systematic review. Crit Care. 2013;17(1):R11. doi: 10.1186/cc11936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Determann R.M., Royakkers A., Wolthuis E.K., Vlaar A.P., Choi G., Paulus F., et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care. 2010;14(1):R1. doi: 10.1186/cc8230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Futier E., Constantin J.M., Paugam-Burtz C., Pascal J., Eurin M., Neuschwander A., et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–437. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 10.Gajic O., Dara S.I., Mendez J.L., Adesanya A.O., Festic E., Caples S.M., et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32(9):1817–1824. doi: 10.1097/01.ccm.0000133019.52531.30. [DOI] [PubMed] [Google Scholar]
- 11.Wolthuis E.K., Choi G., Dessing M.C., Bresser P., Lutter R., Dzoljic M., et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008;108(1):46–54. doi: 10.1097/01.anes.0000296068.80921.10. [DOI] [PubMed] [Google Scholar]
- 12.Halter J.M., Steinberg J.M., Gatto L.A., DiRocco J.D., Pavone L.A., Schiller H.J., et al. Effect of positive end-expiratory pressure and tidal volume on lung injury induced by alveolar instability. Crit Care. 2007;11(1):R20. doi: 10.1186/cc5695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCann U.G., Schiller H.J., Carney D.E., Gatto L.A., Steinberg J.M., Nieman G.F. Visual validation of the mechanical stabilizing effects of positive end-expiratory pressure at the alveolar level. J Surg Res. 2001;99(2):335–342. doi: 10.1006/jsre.2001.6179. [DOI] [PubMed] [Google Scholar]
- 14.Damiani E., Adrario E., Girardis M., Romano R., Pelaia P., Singer M., et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Crit Care. 2014;18(6):711. doi: 10.1186/s13054-014-0711-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helmerhorst H.J., Roos-Blom M.J., van Westerloo D.J., de Jonge E. Association between arterial hyperoxia and outcome in subsets of critical illness: a systematic review, meta-analysis, and meta-regression of cohort studies. Crit Care Med. 2015;43(7):1508–1519. doi: 10.1097/CCM.0000000000000998. [DOI] [PubMed] [Google Scholar]
- 16.Page D., Ablordeppey E., Wessman B.T., Mohr N.M., Trzeciak S., Kollef M.H., et al. Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study. Crit Care. 2018;22(1):9. doi: 10.1186/s13054-017-1926-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herring A.A., Ginde A.A., Fahimi J., Alter H.J., Maselli J.H., Espinola J.A., et al. Increasing critical care admissions from U.S. emergency departments, 2001–2009. Crit Care Med. 2013;41(5):1197–1204. doi: 10.1097/CCM.0b013e31827c086f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mullins P.M., Goyal M., Pines J.M. National growth in intensive care unit admissions from emergency departments in the United States from 2002 to 2009. Acad Emerg Med. 2013;20(5):479–486. doi: 10.1111/acem.12134. [DOI] [PubMed] [Google Scholar]
- 19.Easter B.D., Fischer C., Fisher J. The use of mechanical ventilation in the ED. Am J Emerg Med. 2012;30(7):1183–1188. doi: 10.1016/j.ajem.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Wilcox S.R., Richards J.B., Fisher D.F., Sankoff J., Seigel T.A. Initial mechanical ventilator settings and lung protective ventilation in the ED. Am J Emerg Med. 2016;34(8):1446–1451. doi: 10.1016/j.ajem.2016.04.027. [DOI] [PubMed] [Google Scholar]
- 21.Dreyfuss D., Soler P., Basset G., Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis. 1988;137(5):1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 22.Hoegl S., Boost K.A., Flondor M., Scheiermann P., Muhl H., Pfeilschifter J., et al. Short-term exposure to high-pressure ventilation leads to pulmonary biotrauma and systemic inflammation in the rat. Int J Mol Med. 2008;21(4):513–519. [PubMed] [Google Scholar]
- 23.Ramnath V.R., Hess D.R., Thompson B.T. Conventional mechanical ventilation in acute lung injury and acute respiratory distress syndrome. Clin Chest Med. 2006;27(4):601–613. doi: 10.1016/j.ccm.2006.06.009. [abstract viii] [DOI] [PubMed] [Google Scholar]
- 24.Fuller B.M., Mohr N.M., Miller C.N., Deitchman A.R., Levine B.J., Castagno N., et al. Mechanical ventilation and ARDS in the ED: a multicenter, observational, prospective, cross-sectional study. Chest. 2015;148(2):365–374. doi: 10.1378/chest.14-2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fuller B.M., Mohr N.M., Dettmer M., Kennedy S., Cullison K., Bavolek R., et al. Mechanical ventilation and acute lung injury in emergency department patients with severe sepsis and septic shock: an observational study. Acad Emerg Med. 2013;20(7):659–669. doi: 10.1111/acem.12167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Modrykamien A.M., Stoller J.K. The scientific basis for protocol-directed respiratory care. Respir Care. 2013;58(10):1662–1668. doi: 10.4187/respcare.02195. [DOI] [PubMed] [Google Scholar]
- 27.Beasley K.E., Darin J.M., Durbin C.G. The effect of respiratory care department management of a blood gas analyzer on the appropriateness of arterial blood gas utilization. Respir Care. 1992;37(4):343–347. [PubMed] [Google Scholar]
- 28.Pilon C.S., Leathley M., London R., McLean S., Phang P.T., Priestley R., et al. Practice guideline for arterial blood gas measurement in the intensive care unit decreases numbers and increases appropriateness of tests. Crit Care Med. 1997;25(8):1308–1313. doi: 10.1097/00003246-199708000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Dries D.J., McGonigal M.D., Malian M.S., Bor B.J., Sullivan C. Protocol-driven ventilator weaning reduces use of mechanical ventilation, rate of early reintubation, and ventilator-associated pneumonia. J Trauma. 2004;56(5):943–951. doi: 10.1097/01.ta.0000124462.61495.45. [discussion 951-2] [DOI] [PubMed] [Google Scholar]
- 30.Haas C.F., Loik P.S. Ventilator discontinuation protocols. Respir Care. 2012;57(10):1649–1662. doi: 10.4187/respcare.01895. [DOI] [PubMed] [Google Scholar]
- 31.Radosevich M.A., Wanta B.T., Meyer T.J., Weber V.W., Brown D.R., Smischney N.J., et al. Implementation of a goal-directed mechanical ventilation order set driven by respiratory therapists improves compliance with best practices for mechanical ventilation. J Intensive Care Med. 2019;34(7):550–556. doi: 10.1177/0885066617746089. 885066617746089. [DOI] [PubMed] [Google Scholar]
- 32.Prekker M.E., Donelan C., Ambur S., Driver B.E., O’Brien-Lambert A., Hottinger D.G., et al. Adoption of low tidal volume ventilation in the emergency department: a quality improvement intervention. Am J Emerg Med. 2019 doi: 10.1016/j.ajem.2019.06.026. In Press. [DOI] [PubMed] [Google Scholar]
- 33.Fuller B.M., Ferguson I.T., Mohr N.M., Drewry A.M., Palmer C., Wessman B.T., et al. Lung-protective ventilation initiated in the emergency department (LOV-ED): a quasi-experimental, before-after trial. Ann Emerg Med. 2017;70(3):406–418.e4. doi: 10.1016/j.annemergmed.2017.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davidoff F., Batalden P., Stevens D., Ogrinc G., Mooney S.E., S.D. Group Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152. doi: 10.1136/bmj.a3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vincent J.L., Moreno R., Takala J., Willatts S., De Mendonça A., Bruining H., et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 36.Pai M.P., Paloucek F.P. The origin of the “ideal” body weight equations. Ann Pharmacother. 2000;34(9):1066–1069. doi: 10.1345/aph.19381. [DOI] [PubMed] [Google Scholar]
- 37.Rice T.W., Wheeler A.P., Bernard G.R., Hayden D.L., Schoenfeld D.A., Ware L.B., et al. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;132(2):410–417. doi: 10.1378/chest.07-0617. [DOI] [PubMed] [Google Scholar]
- 38.Severinghaus J.W. Simple, accurate equations for human blood O2 dissociation computations. J Appl Physiol Respir Environ Exerc Physiol. 1979;46(3):599–602. doi: 10.1152/jappl.1979.46.3.599. [DOI] [PubMed] [Google Scholar]
- 39.Gajic O., Frutos-Vivar F., Esteban A., Hubmayr R.D., Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31(7):922–926. doi: 10.1007/s00134-005-2625-1. [DOI] [PubMed] [Google Scholar]
- 40.Ranieri V.M., Rubenfeld G.D., Thompson B.T., Ferguson N.D., Caldwell E., Fan E., et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 41.Ferguson N.D., Fan E., Camporota L., Antonelli M., Anzueto A., Beale R., et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–1582. doi: 10.1007/s00134-012-2682-1. [DOI] [PubMed] [Google Scholar]
- 42.Wong T., Schlichting A.B., Stoltze A.J., Fuller B.M., Peacock A., Harland K.K., et al. No decrease in early ventilator-associated pneumonia after early use of chlorhexidine. Am J Crit Care. 2016;25(2):173–177. doi: 10.4037/ajcc2016823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dimick J.B., Staiger D.O., Birkmeyer J.D. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45(6):1614–1629. doi: 10.1111/j.1475-6773.2010.01158.x. Pt 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Needham D.M., Yang T., Dinglas V.D., Mendez-Tellez P.A., Shanholtz C., Sevransky J.E., et al. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med. 2015;191(2):177–185. doi: 10.1164/rccm.201409-1598OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simonis F.D., Serpa Neto A., Binnekade J.M., Braber A., Bruin K.C.M., Determann R.M., et al. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial. JAMA. 2018;320(18):1872–1880. doi: 10.1001/jama.2018.14280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lanspa M.J., Gong M.N., Schoenfeld D.A., Lee K.T., Grissom C.K., Hou P.C., et al. Prospective assessment of the feasibility of a trial of low-tidal volume ventilation for patients with acute respiratory failure. Ann Am Thorac Soc. 2019;16(3):356–362. doi: 10.1513/AnnalsATS.201807-459OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilcox S.R., Seigel T.A., Strout T.D., Schneider J.I., Mitchell P.M., Marcolini E.G., et al. Emergency medicine residents’ knowledge of mechanical ventilation. J Emerg Med. 2015;48(4):481–491. doi: 10.1016/j.jemermed.2014.09.059. [DOI] [PubMed] [Google Scholar]
- 48.Wilcox S.R., Strout T.D., Schneider J.I., Mitchell P.M., Smith J., Lutfy-Clayton L., et al. Academic emergency medicine physicians’ knowledge of mechanical ventilation. West J Emerg Med. 2016;17(3):271–279. doi: 10.5811/westjem.2016.2.29517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Amato M.B., Meade M.O., Slutsky A.S., Brochard L., Costa E.L., Schoenfeld D.A., et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 50.Fuller B.M., Page D., Stephens R.J., Roberts B.W., Drewry A.M., Ablordeppey E., et al. Pulmonary mechanics and mortality in mechanically ventilated patients without acute respiratory distress syndrome: a cohort study. Shock. 2018;49(3):311–316. doi: 10.1097/SHK.0000000000000977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.C. Guérin, L. Papazian, J. Reignier, L. Ayzac, A. Loundou, J.M. Forel, I.o.t.A.a.P. trials, Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials, Crit Care 20(1) (2016) 384. [DOI] [PMC free article] [PubMed]