Spring in the Northeastern United States (US) usually represents a period of relatively high emergency department (ED) utilization for childhood asthma. Putative drivers of this phenomenon include seasonal allergens and the tail of winter respiratory viruses. The emergence and spread of the novel SARS-CoV2 virus in the US coincided with spring in the Northeastern US, and many national and international health organizations, including the Centers for Disease Control, were concerned that asthma would be a risk factor for worse outcomes.(1) The impact of the emergence of COVID-19 and institution of social distancing public health measures on health system utilization for childhood asthma has not been described.
With nearly 6000 asthma ED visits and over 2000 asthma hospitalizations every year, our hospital is a high-volume center with several on-going data collection efforts to monitor and respond to changes in asthma emergency care utilization. In this report, we describe the trends in ED utilization in the first four months of 2020 in comparison to prior years, allowing us to account for year-to-year differences in seasonal utilization.
We abstracted data on visits to the ED during the first four months of 2020 that included an asthma diagnosis entered by an ED provider into the electronic health record using a validated ICD code grouping system.(2) We compared these data to average daily visits for the corresponding four months of years 2016-2019 using longitudinal time series plots. We used a X and S statistical process control chart to depict mean daily ED utilization from 2016-2019, as well as 3 standard deviations (SD) from the mean.(3,4) We then compared the mean daily asthma ED visits in 2020 pre-COVID-19 (1/1/2020-3/18/2020) to the mean daily asthma ED visits for the month following the first positive case in our ED (3/19/2020-4/18/2020) using a paired t-test. We then stratified asthma visits by level of triage acuity for 2020 in a second time series plot and calculated the proportion of children subsequently hospitalized in the pre-COVID and COVID-era intervals. Finally, we compared ED utilization trends with the daily positivity for COVID-19 testing for all children, as well as children with asthma, within the same ED.
To assess contemporaneous trends in asthma ED utilization relative to other diagnoses, we calculated the percentage change in mean daily ED utilization for three other diagnosis groups between the same two time intervals: (1) non-asthma respiratory, (2) trauma, and (3) endocrine and metabolic.
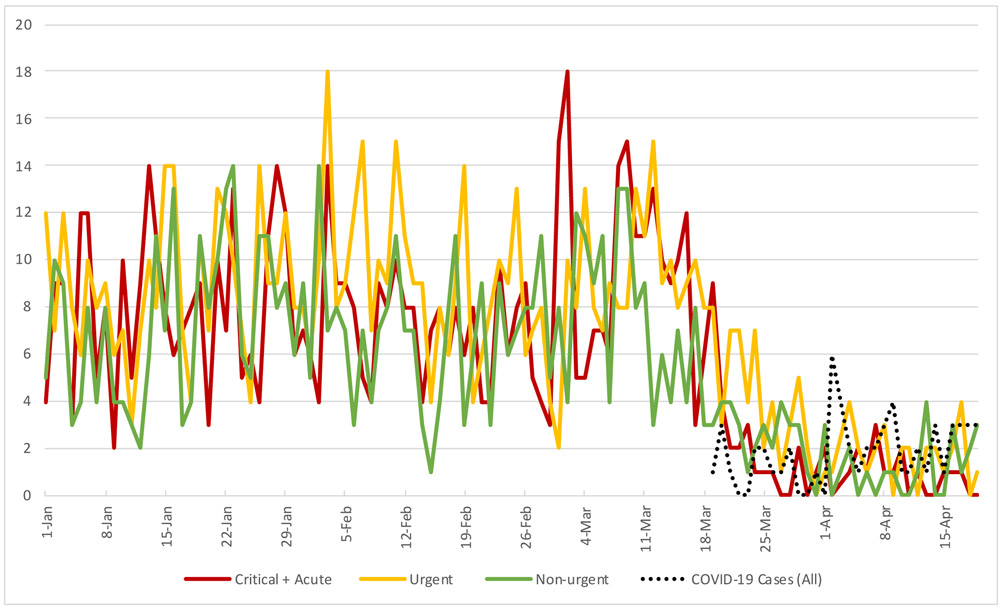
Prior to the first COVID-19 positive case in 2020 (March 19th), ED visits for asthma ranged between 11-39 visits per day (mean 24.3, SD 6.6), a utilization level that largely fell within 3 standard deviations of the daily average for the preceding four years. (Figure 1) The subsequent week, local authorities implemented a city-wide stay at home order that included home-based schooling. That same week, daily asthma ED visits dropped below 3 standard deviations of the daily mean from 2016-2019 for the remainder of the observation interval. In this second interval, mean daily asthma ED visit rate was 5.8 (SD 4.2), a decrease of 18.5 visits/day (95% CI [15.9, 21.0], p<0.0001) or 76% lower than pre-COVID utilization. Similar trends were observed for children of all levels of triage acuity (Figure 2) and the percentage of children subsequently admitted to the hospital decreased from 31% in the pre-COVID interval to 22% in the subsequent month. Between these same two time intervals, ED utilization for non-asthma respiratory diagnoses decreased by 75% (from 24.0 to 6.0 visits/day), 61% for trauma diagnoses (from 34.8 to 13.5 visits/day), and 48% for endocrine and metabolic diagnoses (from 3.3 to 1.7 visits/day). These graphical trends are provided in Figure E1.
Figure 1. Daily asthma ED visits during the first four months of the calendar year.
First four months of 2020 (blue) are compared to the daily average for the prior four years (grey; 3 standard deviations from the mean shown). COVID-19 cases (not asthma-specific) are shown (black-dotted).
Figure 2. Daily asthma ED visits in the first 4 months of 2020 by level of triage acuity.
Critical and acute represent the 2 highest triage levels (red), urgent represents the middle triage level (yellow), and non-urgent represents the 2 lowest levels of triage (green). COVID-19 cases (not asthma-specific) are shown (black-dotted).
In this report, we document initial data on asthma-related emergency care utilization during the local emergence of COVID-19 in a high-volume US children’s hospital. Our data demonstrate a dramatic decrease in asthma-related ED use that was well below historical seasonal variation. This pattern was observed for all levels of triage acuity and the proportion of asthma ED visits that resulted in hospitalization actually decreased in the month following the first COVID-19 positive case, suggesting that the decrease in utilization was not solely due to ED avoidance or delays in care-seeking behavior for lower acuity events. This is particularly striking given that the emergence of COVID-19 in the Northeastern US occurred during the spring, a season in which respiratory viruses and high-pollen counts can converge and exacerbate asthma symptoms.(5) These observations are balanced by sizeable contemporaneous decreases in other common diagnoses for ED visits (non-asthma respiratory conditions and trauma) and other chronic conditions of childhood (endocrine and metabolic disorders).
While these trends represent utilization patterns of a single, high-volume US children’s hospital, they highlight several important areas of future investigation. These include: (1) the relative contribution of person-to-person transmission of respiratory viruses, which have been shown to be a strong driver of asthma exacerbations(6), as a driver of severe pediatric asthma exacerbations, (2) the relative effects of reducing exposure to outdoor seasonal allergens (tree, grass, and flower pollens) and increasing exposure to indoor allergens (dust mites, animal dander, and cockroach antigen) on exacerbations, particularly in low-income, urban populations, and (3) the role of varying levels of traffic and industrial air pollution, including diesel exhaust particulates, in asthma exacerbations.
These data also raise additional questions about how the emergence of COVID-19 influenced caregiver and child behaviors around the care of asthma. For example, the extent to which better adherence to preventative medications or outreach to outpatient providers to access interventions by telemedicine earlier in the course of exacerbation influences asthma outcomes. If replicated, these results may offer new insights on where to best focus efforts to improve asthma outcomes outside of a pandemic scenario.
Supplementary Material
Figure E1: Daily ED utilization for the following 4 diagnosis groups in the first 4 months of 2020: Asthma (royal blue), non-Asthma Respiratory (light blue), Endocrine and Metabolic (purple), Trauma (orange)."
Clinical Implications:
Compared with historical trends, we describe a dramatic decrease in pediatric asthma-related emergency department utilization for all levels of acuity coincident with COVID-19 emergence. These findings have implications for clinicians and researchers seeking to understand the drivers of asthma exacerbations.
Acknowledgments
This work was supported by the following NIH awards: K23HL136842 (Kenyon), DK116668 (Hill), and K08AI135091 (Henrickson). Dr Henrickson’s effort was also supported by the Burroughs Wellcome Fund CAMS award. The authors have no other potential conflicts of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC COVID-19 Response Team. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020. April 3;69(13):382–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Gorelick MH. A new diagnosis grouping system for child emergency department visits. Acad Emerg Med. 2010. February;17(2):204–13. [DOI] [PubMed] [Google Scholar]
- 3.Carey R, Lloyd R. Measuring Quality Improvement in Healthcare: A Guide to Statistical Process Control Applications. American Society for Quality; 2001. [Google Scholar]
- 4.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003. December;12(6):458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ito K, Weinberger KR, Robinson GS, Sheffield PE, Lall R, Mathes R, et al. The associations between daily spring pollen counts, over-the-counter allergy medication sales, and asthma syndrome emergency department visits in New York City, 2002-2012. Environ Health. 2015. August 27;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papadopoulos NG, Christodoulou I, Rohde G, Agache I, Almqvist C, Bruno A, et al. Viruses and bacteria in acute asthma exacerbations--a GA2 LEN-DARE systematic review. Allergy. 2011. April;66(4):45 8–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure E1: Daily ED utilization for the following 4 diagnosis groups in the first 4 months of 2020: Asthma (royal blue), non-Asthma Respiratory (light blue), Endocrine and Metabolic (purple), Trauma (orange)."