Abstract
Objective: To evaluate the maternal and neonatal complications after frozen-thawed blastocyst transfer cycles utilizing different endometrial preparation regimens.
Design: This is a retrospective cohort study and a secondary analysis of a multicenter, randomized, controlled trial comparing live birth rate after fresh vs. frozen single blastocyst transfer (Frefro-blastocyst).
Setting: Reproductive medicine centers.
Patient(s): A total of 800 women with regular menstrual cycles undergoing their first cycle of in-vitro fertilization after frozen-thawed single blastocyst transfer.
Intervention(s): Endometrium preparation was performed with a natural cycle regimen or hormone replacement therapy (HRT) cycle regimen, at the discretion of local investigators. All pregnancies were followed up until delivery.
Main Outcome Measure(s): Maternal and neonatal complications.
Result(s): 513 infertile patients who underwent natural cycles regimen and 287 who underwent HRT cycles regimen were analyzed. The incidences of maternal and neonatal complications were comparable between the natural cycle and HRT cycle regimen. Regarding the risk of gestational diabetes, gestational hypertension, pre-eclampsia, preterm delivery, small for gestational age and large for gestational age, the HRT cycle was still not a significant risk factor after adjusting for potential confounders. The natural cycle regimen yielded an insignificant higher total live birth rate [59.45 vs. 50.17%, P = 0.001, adjusted odds ratio (AOR) 1.366, 95% confidence interval (CI) 0.975–1.913], clinical pregnancy rate (68.23 vs. 58.89%, P = 0.008, AOR 1.406, 95% CI 0.992–1.991) and ongoing pregnancy rate (62.18 vs. 52.61%, P = 0.008, AOR 1.387, 95% CI 0.988–1.948) than did the HRT cycle regimen. However, compared to natural cycles, HRT cycles were associated with a significantly higher risk of biochemical miscarriage (6.86 vs. 18.18%, P < 0.001, AOR 0.328, 95% CI, 0.176–0.611).
Conclusion(s): The incidence of maternal and neonatal complications in natural cycle and HRT cycle regimens after frozen single blastocyst transfer were comparable. Frozen-thawed single blastocyst transfer in a natural cycle was associated with lower biomedical miscarriage than the use of the HRT cycle.
Clinical Trial Registration Number: Frefro-blastocyst was registered at Chinese Clinical Trial Registry, ChiCTR-IOR-14005405.
Keywords: biomedical miscarriage, frozen embryo transfer, natural cycle, hormone replacement therapy cycle, single embryo transfer
Introduction
The goal of assisted reproductive technology (ART) is to achieve a live, healthy, full-term singleton baby. Single embryo transfer (SET) is the most efficient approach to reduce the risk of multiple pregnancies (1). With the development in cryopreservation technology, especially the introduction of vitrification, the application of frozen embryo transfer (FET) has become increasingly popular (2). Studies have shown that frozen embryo transfer by avoiding a supra-physiological environment for embryo implantation after ovarian stimulation increased pregnancy rate (3, 4). By prolonging the in vitro culture, only embryos of excellent quality with the highest potential for implantation will reach blastocyst stage selection. Blastocyst transfer has resulted in significantly higher rates of pregnancy and delivery than cleavage-stage embryo transfer (5).
Our previous trial suggested that frozen single blastocyst transfer was better for achieving singleton live birth than fresh single blastocyst transfer in women with good prognosis (6). However, frozen single blastocyst transfer was associated with a higher risk of pre-eclampsia (6). Further, higher rates of hypertensive disorders and placenta accreta in pregnancy were noted after frozen embryo transfer (7). FET singletons may be at an increased risk of being born large for gestation age (LGA) (7, 8). Whether these differences are due to the protocol used in frozen cycles remains unknown.
A crucial aspect of FET cycles is the preparation of the endometrium to receive the transferred embryo. The most commonly used endometrial preparation methods for FETs include hormone replacement therapy (HRT) cycle and natural cycle (NC). Many retrospective analyses were performed of frozen blastocyst transfers, and different conclusions were drawn about the implantation, pregnancy, and live birth rate (9–12). The results of meta-analysis and systematic review show that no sufficient evidence has been found to support the superiority of one method over the other (2, 13). While few studies have investigated the neonatal and maternal outcomes comparing these strategies, compared to natural cycle protocols, higher rates of hypertensive disorders in pregnancy (14, 15), postpartum hemorrhage (14, 16), post term birth (14), macrosomia (14), and cesarean section (15) were detected in the HRT cycle. It seemed that the HRT cycles of FET have a negative effect on obstetric outcome.
In this study, a secondary analysis was performed to see whether the method of endometrial preparation for transfer of vitrified blastocysts was associated with obstetric complications outcomes.
Materials and Methods
Study Population
The Frefro-blastocyst study was conducted during August 1, 2016, to June 3, 2017 in 21 academic fertility centers in China. The original study was approved by the ethics committees of all study sites and was registered at Chinese Clinical Trial Registry (number ChiCTR-IOR-14005405) (6). The design and main outcomes of this trial have been previously reported in detail (17). Briefly, 1,650 women with regular menstrual cycles undergoing their first cycle of in vitro fertilization were enrolled, and eligible women were randomly assigned to either fresh or frozen single blastocyst transfer. For those assigned to frozen blastocyst transfer, all blastocysts were cryopreserved, and a delayed frozen-thawed single blastocyst transfer was done. Considering the condition of switched groups in the randomized clinical trial (RCT), 724 patients adhered to frozen protocol and 87 women assigned to the fresh embryo transfer group who actually had single frozen blastocyst transfer were included. However, only natural cycle and HRT cycle regimens for endometrium preparation of FET were analyzed.
Study Procedure
After ovarian stimulation with a gonadotropin-releasing hormone antagonist protocol, women who obtain four or more than four embryos on day three of the embryo culture were randomized into two groups: fresh single blastocyst transfer group and frozen single blastocyst transfer group. The selection of the single blastocyst gave priority to the score of the inner cell mass, and the score of trophectoderm was also considered. The rank of blastocyst grade from top to good was AA, AB, BA, BB, AC, and BC. If two or more blastocysts were of equal grade, their early scores at cleavage stage were referred for the selection of the single blastocyst. Supernumerary embryos were frozen on day 5 or 6 according to embryo development. On day 5 or 6 of embryo culture, women who were assigned to the frozen blastocyst transfer group had their blastocysts vitrified and a deferred frozen blastocyst transfer. The selection of the frozen blastocyst for thawing was based on the blastocyst grade before freezing.
Endometrial Preparation Protocols
At least 4 weeks after blastocysts vitrified, endometrium preparation was performed with a natural cycle regimen or HRT cycle regimen. At the discretion of local investigators, this assignment was not randomized. For the natural cycle regimen, when it was detected that the dominant follicle and the endometrial thickness reached 7 mm or more, local investigators decided whether to use human chorionic gonadotropin (hCG) for ovulation triggering according to their clinical routine. Ovulation was determined by ultrasound monitoring and a single frozen-thawed blastocyst, either day 5 or day 6, was transferred on the 5th day after ovulation. Details of embryo transfer procedure were shown in a previous study (6). Luteal phase support was started after the ovulation day with oral dydrogesterone 10 mg three times daily. If the patient was pregnant, luteal phase support was continued until 10 weeks' gestation. For the HRT cycle regimen, the endometrium prepared with oral estradiol valerate (Progynova, Delpharm Lille, Lys-Lez-Lannoy, France) at a dose of 4–8 mg daily was started on days 1–3 of the menstrual cycle. Vaginal progesterone gel (Crinone, Merck Serono) 90 mg/day and oral dydrogesterone 10 mg twice daily were added when the endometrial thickness reached 7 mm or more. A single frozen-thawed blastocyst was transferred on the 5th day after progesterone initiation. Estradiol valerate at the dose for endometrium preparation was continued until the day of the serum hCG test, 2 weeks after embryo transfer. If pregnancy was achieved, estradiol valerate stopped gradually at 8–9 weeks of gestation; vaginal progesterone gel and oral dydrogesterone was continued until 10 weeks of gestation.
Outcome Measures
The study outcomes included clinical pregnancy, ongoing pregnancy, pregnancy loss, live birth, ectopic pregnancy, perinatal complications and neonatal complication gestational, e.g., gestational diabetes mellitus (GDM), pregnancy-induced hypertension (PIH), pre-eclampsia, gestational age at birth, preterm birth, small for gestational age (SGA), large for gestational age (LGA), and neonatal hospitalization for more than 3 days. Preterm birth was defined as delivery before 37 complete weeks of gestation. The outcomes SGA and LGA were, respectively, defined according to birth weight for the 10th and 90th percentile of gender-specific birth weight reference for Chinese (18).
Statistical Analysis
Continuous data were expressed as mean (SD) and compared by the Student's t-test. Categorical data were represented as frequency and percentage; differences in these variables between the treatment groups were assessed by χ2 analysis, with Fisher's exact test for expected frequencies less than five. A P < 0.05 was considered statistically significant. Crude odds ratios (OR) with 95% confidence intervals (CI) for each primary outcome were calculated. Logistic regression analysis was used to compare adjusted odds ratios (AOR) and 95% CI for the effect of natural cycle vs. HRT cycle regimen on obstetric and perinatal complications. Goodness of fit for logistic regression models were calculated by the Hosmer-Lemeshow (HL) test, if the P > 0.05, the model passed the test. All analyses were performed with the use of SPSS software 21.0.
Results
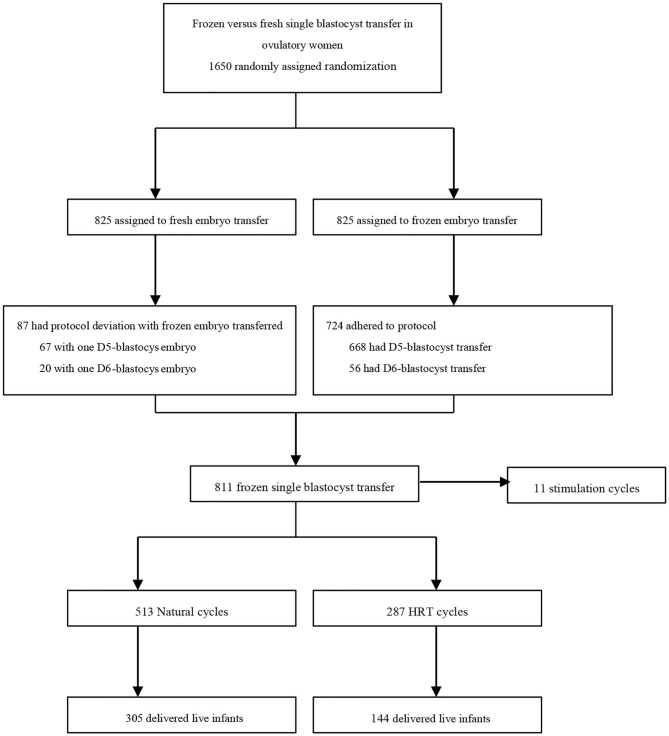
Seven hundred and twenty-four women who were assigned to the frozen embryo transfer group actually adhered to the protocol, while 87 women assigned to the fresh embryo transfer group actually had a frozen embryo transfer. Of these, 11 women were excluded due to a stimulation cycle regimen for endometrial preparation of FET. 513 infertile patients who underwent natural cycles regimen and 287 who underwent HRT cycles regimen were analyzed (Figure 1).
Figure 1.
Study flow diagram.
Baseline characteristics are listed in Table 1. Maternal age, body mass index, duration of infertility, proportion of previous conception, the proportion of IVF indications, antral follicle count (AFC), baseline follicle stimulating hormone (FSH), baseline luteinizing hormone (LH), oestradiol (E2), days of ovarian stimulation, endometrial thickness on day of trigger, number of oocytes, fertilization method and incidence of ovarian hyper-stimulation syndrome (OHSS) were comparable between the natural and HRT cycles. However, in the natural cycles compared to the HRT cycles, total testosterone level, total gonadotropin dose, E2 and progesterone level on the day of trigger were significantly lower (P < 0.001, P = 0.02, P = 0.006, respectively), the number of 2PN embryos, cleavage embryos and day-3 suitable for transferred embryos were less (P = 0.015, 0.032, 0.015, respectively), and the endometrial thickness was thinner (P < 0.001).
Table 1.
Baseline characteristics.
| Characteristics | Natural cycles (n = 513) | HRT cycles (n = 287) | P-value |
|---|---|---|---|
| Age (years) | 28.74 ± 2.89 | 29.08 ± 3.01 | 0.117 |
| Body-mass index (kg/m) | 22.32 ± 3.07 | 22.52 ± 3.30 | 0.379 |
| Duration of infertility (years) | 3.26 ± 2.11 | 3.29 ± 2.35 | 0.846 |
| Previous conception n (%) | 219/513 (42.69) | 133/287 (46.34) | 0.318 |
| Indications for IVF | 0.364 | ||
| Tubal factor | 276/513 (53.80) | 156/287 (54.36) | |
| Male factor | 113/513 (22.03) | 64/287 (22.30) | |
| Unexplained infertility | 20/513 (3.90) | 18/287 (6.27) | |
| Combined factors | 104/513 (20.27) | 49/287 (17.07) | |
| Antral follicle count in both ovaries | 16.46 ± 5.46 | 16.87 ± 5.99 | 0.339 |
| Baseline sex hormone | |||
| FSH (IU/L) | 6.34 ± 1.50 | 6.32 ± 1.46 | 0.812 |
| LH (IU/L) | 4.78 ± 1.93 | 4.83 ± 2.21 | 0.717 |
| Oestradiol (pg/mL) | 37.07 ± 14.60 | 37.94 ± 15.64 | 0.430 |
| Total testosterone (ng/dL) | 28.46 ± 14.03 | 35.96 ± 17.82 | <0.001 |
| Fresh cycle variables | |||
| Days of ovarian stimulation | 9.28 ± 1.40 | 9.49 ± 1.68 | 0.056 |
| Total gonadotropin dose (IU) | 1559.32 ± 479.52 | 1634.78 ± 500.26 | 0.036 |
| Oestradial level on HCG trigger day (pmol/L) | 3431.55 ± 1810.08 | 3758.37 ± 1801.59 | 0.020 |
| Progesterone level on HCG trigger day (nmol/L) | 1.14 ± 0.52 | 1.26 ± 0.58 | 0.006 |
| Endometrial thickness on HCG trigger day (cm) | 1.07 ± 0.20 | 1.06 ± 0.20 | 0.512 |
| No. of oocytes retrieved | 14.29 ± 5.74 | 14.69 ± 5.68 | 0.339 |
| No. of 2PN embryos | 9.43 ± 3.97 | 10.17 ± 4.53 | 0.015 |
| No. of cleavage embryos | 9.29 ± 3.96 | 9.94 ± 4.36 | 0.032 |
| Fertilization method | 0.333 | ||
| IVF n (%) | 359/513 (69.98) | 210/287 (73.17) | |
| ICSI n (%) | 127/513 (24.76) | 68/287 (23.69) | |
| IVF +ICSI n (%) | 27/513 (5.26) | 9/287 (3.14) | |
| No. of day-3 embryos suitable for transfer | 6.96 ± 2.99 | 7.59 ± 3.69 | 0.015 |
| OHSS n (%) | 3/513 (0.58) | 4/287 (1.39) | 0.258 |
| FET cycle variables | |||
| Endometrial thickness before transfer (cm) | 1.00 ± 0.17 | 0.94 ± 0.16 | <0.001 |
| Timing of embryo transfer—no./total no. (%) | 0.853 | ||
| Day 5 | 465/513 (90.64) | 259/287 (90.24) | |
| Day 6 | 48/513 (9.36) | 28/287 (9.76) | |
| No. of remaining frozen blastocysts | 4.19 ± 2.90 | 4.27 ± 3.00 | 0.720 |
The pregnancy outcomes after FET are shown in Table 2. The natural cycle regimen yielded a higher total live birth rate including singleton and twin than the HRT cycle regimen (59.45 vs. 50.17%, P = 0.011). Singleton live birth per woman was also higher in natural cycles (57.50 vs. 48.78%, P = 0.017), whereas twin live birth per woman was similar between the two protocols (P = 0.565). Clinical pregnancy (68.23 vs. 58.89%, P = 0.008) and ongoing pregnancy (62.18 vs. 52.61%, P = 0.008) were significantly higher in the natural cycles. Furthermore, the rate of biochemical miscarriage was significantly lower in the natural cycles (6.86 vs. 18.18%, P < 0.001). No significant differences were observed in terms of birth weight, gestational weeks, biochemical pregnancy and clinical pregnancy loss rate.
Table 2.
Livebirth, birthweight, pregnancy, and pregnancy loss.
| Natural cycles (n = 513) | HRT cycles (n = 287) | P-value | |
|---|---|---|---|
| Total live birth per woman | 305/513 (59.45) | 144/287 (50.17) | 0.011 |
| Singleton live birth per woman | 295/513 (57.50) | 140/287 (48.78) | 0.017 |
| Twin live birth per woman | 10/513 (1.95) | 4/287 (1.39) | 0.565 |
| Birth weight | |||
| Singleton (g) | 3395 ± 476.14 | 3417.39 ± 480.02 | 0.654 |
| Monozygotic Twin (g) | 2424.50 ± 501.58 | 2365.00 ± 525.03 | 0.782 |
| Gestational weeks (week) | 38.9 ± 1.66 | 39.04 ± 1.74 | 0.464 |
| Pregnancy | |||
| Biochemical pregnancy—no. (%) | 379/513 (73.88) | 209/287 (72.82) | 0.745 |
| Clinical pregnancy—no. (%) | 350/513 (68.23) | 169/287 (58.89) | 0.008 |
| Ongoing pregnancy—no. (%) | 319/513 (62.18) | 151/287 (52.61) | 0.008 |
| Pregnancy loss-no./total no. (%) | |||
| Total pregnancy loss among biochemical pregnancies | 67/379 (17.68) | 62/209 (29.67) | 0.001 |
| Biochemical miscarriage | 26/379 (6.86) | 38/209 (18.18) | <0.001 |
| Clinical pregnancy loss | 41/350 (11.71) | 24/169 (14.20) | 0.422 |
| First trimester pregnancy loss | 31/350 (8.86) | 18/169 (10.65) | 0.513 |
| Second trimester pregnancy loss | 10/350 (2.86) | 6/169 (3.55) | 0.669 |
Maternal and neonatal complications stratified by FET method are shown in Table 3. There were no significant differences in the incidence of ectopic pregnancy, GDM, PIH, pre-eclampsia, preterm rupture of membrane, preterm delivery and post-partum hemorrhage between the two groups. In addition, no significant between-group difference was found in the risks of small for SGA, LGA, neonatal hospitalization for more than 3 days, neonatal infection among live newborn, nor birth defect.
Table 3.
Maternal and neonatal complications.
| Natural cycles (n = 513) | HRT cycles (n = 287) | P-value | |
|---|---|---|---|
| Maternal complications | |||
| Ectopic pregnancy | 3/350 (0.79) | 2/169 (0.96) | 0.663 |
| Gestational diabetes | 40/350 (11.43) | 19/169 (11.24) | 0.950 |
| Gestational hypertension | 8/350 (2.29) | 5/169 (2.96) | 0.765 |
| Pre-eclampsia | 9/350 (2.57) | 6/169 (3.55) | 0.580 |
| Placenta previa | 6/350 (1.71) | 0 | 0.184 |
| Preterm rupture of membrane | 36/350 (10.29) | 18/169 (10.65) | 0.898 |
| Preterm delivery | 22/350 (6.29) | 10/169 (5.92) | 0.870 |
| Post-partum hemorrhage | 3/308 (0.97) | 5/144 (3.47) | 0.117 |
| Neonatal complications | |||
| Small for gestational age | 16/310 (5.16) | 10/144 (6.94) | 0.447 |
| Large for gestational age | 58/310 (18.71) | 27/144 (18.75) | 0.992 |
| Neonatal hospitalization >3 days | 39/303 (12.87) | 13/142 (9.15) | 0.255 |
| Neonatal jaundice among live newborns | 55/303 (18.15) | 26/142 (18.31) | 0.968 |
| Neonatal infection among live newborns | 11/303 (3.63) | 4/142 (2.82) | 0.783 |
| Birth defect | 10/318 (3.14) | 5/148 (3.38) | 1.000 |
Values are number (percentage).
Regarding the risk of gestational diabetes, gestational hypertension, pre-eclampsia, preterm delivery, SGA and LGA, the HRT cycle was still not a significant risk factor after adjusting the results for potential confounders. A multiple logistic regression analysis adjusted for potential confounders showed that natural cycle FET (vs. HRT cycle-FET) was a higher risk factor for live birth rate (AOR 1.411; 95% CI 1.011–1.970), clinical pregnancy rate (AOR 1.444, 95% CI 1.022–2.041), ongoing pregnancy rate (AOR 1.443, 95% CI 1.031–2.020) and a significant lower risk factor for biochemical miscarriage (AOR 0.323; 95% CI 0.174–0.599) in Model 1, which did not pass the HL test (Table 4). When adding age and FSH to adjust in Model 2, only the rate of biochemical miscarriage (AOR 0.328; 95% CI 0.176–0.611) was still significantly lower in natural cycles than in HRT cycles (Table 4).
Table 4.
Logistic regression for the effect of natural cycle vs. HRT cycle regimen on obstetric complication.
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | P-value | Adjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P-value | |
| Total live birth | 1.456 (1.089–1.948) | 0.011 | 1.411 (1.011–1.970) | 0.043 | 1.366 (0.975–1.913) | 0.070 |
| Clinical pregnancy | 1.499 (1.111–2.023) | 0.008 | 1.444 (1.022–2.041) | 0.037* | 1.406 (0.992–1.991) | 0.055 |
| Ongoing pregnancy | 1.481 (1.105–1.984) | 0.008 | 1.443 (1.031–2.020) | 0.033 | 1.387 (0.988–1.948) | 0.059 |
| Biochemical miscarriage | 0.331 (0.195–0.564) | <0.001 | 0.323 (0.174–0.599) | <0.001* | 0.328 (0.176–0.611) | <0.001 |
| Gestational diabetes | 1.019 (0.570–1.819) | 0.950 | 0.850 (0.428–1.688) | 0.642 | 0.886 (0.446–1.762) | 0.730 |
| Gestational hypertension | 0.767 (0.247–2.382) | 0.765 | 0.652 (0.186–2.289) | 0.505 | 0.662 (0.187–2.348) | 0.523 |
| Pre-eclampsia | 0.717 (0.251–2.048) | 0.580 | 0.732 (0.238–2.250) | 0.586 | 0.749 (0.244–2.300) | 0.613 |
| Preterm delivery | 1.066 (0.493–2.306) | 0.870 | 1.273 (0.518–3.130) | 0.599 | 1.274 (0.520–3.124) | 0.596 |
| Small for gestational age | 0.729 (0.322–1.649) | 0.447 | 0.712 (0.293–1.728) | 0.452 | 0.700 (0.285–1.715) | 0.435 |
| Large for gestational age | 0.997 (0.601–1.655) | 0.992 | 1.064 (0.602–1.881) | 0.832 | 1.084 (0.613–1.916) | 0.782 |
Modal 1 is adjusted for total testosterone, total gonadotropin dose (IU), oestradial level on HCG trigger day (pmol/L), progesterone level on HCG trigger day (nmol/L), No. of 2PN embryos, No. of cleavage embryos, No. of day-3 embryos suitable for transfer and endometrial thickness before transfer (cm). Modal 2 is adjusted for age, FSH, total testosterone, total gonadotropin dose (IU), oestradial level on HCG trigger day (pmol/L), progesterone level on HCG trigger day (nmol/L), No. of 2PN embryos, No. of cleavage embryos, No. of day-3 embryos suitable for transfer and endometrial thickness before transfer (cm). HRT cycle regimen was set to be the referent group.
Value of Hosmer-Lemeshow Test goodness-of-fit <0.05.
Discussion
In ovulatory women with a good prognosis, we found that the incidence of maternal and neonatal complications was similar in natural cycle and HRT cycle regimens after frozen single blastocyst transfer. HRT FET was associated with increased risks of biochemical miscarriage in comparison to the natural FET. However, the natural cycle regimen did not result in a higher rate of live birth, clinical pregnancy or ongoing pregnancy than in the HRT cycle regimen after adjusting for potential confounders.
HRT cycle is also called hormone replacement cycle (HRC), programmed cycle (PC) or artificial cycle (AC) in different literatures (10, 19–21). For anovulatory women, exogenous hormone preparation is often preferred. In ovulatory women, artificial endometrial preparation may benefit from minimal monitoring and ease of scheduling transfers. However, the universal application of HRT cycles may have potential disadvantages including an increased cost, inconvenience and the potential adverse events (e.g., increased thrombotic risk) associated with estrogen supplementation (22). Natural cycle of endometrium preparation can only be offered to patients with an ovulatory cycle. Developing follicle and urine or serum luteinizing hormone levels are needed to be monitored. Detection of an LH surge, thawing and transfer can be planned accordingly. While ovulation is triggered by hCG administration, the dominate follicular formation could reduce cancellation rates, shortening the duration of monitoring and improving corpus luteum function. No statistically significant difference for live birth rate was noted between spontaneous and induced ovulation (13, 23). Groenewoud et al. summarizes the differences between the two regimens, no optimal minimal monitoring regimen in NC–FET has been determined, routine use of luteal phase support in NC–FET has not been shown to be advantageous but to increase treatment burden. Furthermore, the costs of both protocols were comparable (2).
In this multicenter clinical trial, local investigators decide endometrium preparation protocols and whether to use hCG for ovulation triggering according to their clinical routine. The baseline characteristics of total gonadotropin dose, E2 and progesterone level on day of trigger, the number of 2PN embryos, cleavage embryos and day-3 suitable in the natural cycles were different from the HRT cycles. Thus, it can be hypothesized that more follicular developed during IVF procedure in the HRT cycle regimen. Although hyperandrogenism have a higher risk of maternal and neonatal pregnancy complications (24, 25), total testosterone in both regimens was within the normal range, regardless of its effect on obstetric outcomes. In multivariate analysis, the effects of these differences were adjusted. We observed that endometrial thickness before transfer was significantly thicker in natural cycles compared with HRT cycles, and it is consistent with previous reports (9, 26). Natural cycles yielding an optimal endometrial thickness may compromise the window of implantation (WOI) (9).
Thus, optimal endometrial preparation and identification of the receptive window are important factors in the process of embryo implantation (27). Recent data from both simple histologic endometrial dating and transcriptomic microarray had shown that the window of implantation in hormonally prepared cycles for FET be delayed in about 25% women (28). Cluster analysis demonstrated that natural cycles were associated with a better endometrial receptivity transcriptome than HRT cycles (29).
As only a few high quality RCTs on the optimal preparation for FET are available (22), no substantial difference in live birth was obtained from a recent meta-analysis (30). Many studies did not conduct subgroup analysis of cleavage stage embryo and blastocyst transfer; no statistically significant difference for both clinical pregnancy and live birth were noted between natural cycles and HRT cycles (15, 19). In the patients with frozen cleavage embryo transfer, natural cycle and HRT cycle protocols yielded a comparable clinical pregnancy rate and live birth rate (10), while in frozen blastocyst transfer HRT cycles were associated with higher live birth rate (10, 31). Nonetheless, our study suggests that the live birth rate of frozen blastocyst transfer was better with the natural cycle preparation protocol before adjustment, supporting previous findings (9, 12). The increase of live birth rate in natural cycles may potentially be due to the lower risk of biochemical miscarriage. A prospective and observational cohort study by Cerrillo et al. (20) was performed and a higher miscarriage rate was observed in the hormone replacement cycles when compared to the natural cycles.
Many factors influence the live birth and clinical pregnancy rate following FET: female age and basal FSH level, the number of top-quality embryos and maximal endometrial thickness were the significant factors (9, 32). Therefore, when model 1 did not pass the Hosmer-Lemeshow test after adjusting the potential confounding factors, we added age and FSH to adjust. In NC-FET, the serum level of progesterone elevation present for 2 or more days before the LH surge (33), HCG trigger or not, and luteal support type may affect live birth rate (34). In HRT-FET, duration of both estrogen and progesterone supplementation and various routes of estrogen and progesterone administration are necessary to be considered (2). In our study, the disproportionate number of NC and HRT cycle was due to the discretion of local investigators, and this can lead to an inherent bias.
Numerous studies have tried to identify the optimal regimen of FET to obtain better pregnancy outcomes and to avoid or reduce adverse obstetric and neonatal outcomes. A large-scale registry-based study (7) on maternal and neonatal outcome of pregnancy after single embryo transfer showed that FET was associated with improved outcomes of preterm birth (PTB), low birth weight (LBW), and SGA compared with fresh transfer. Moreover, FET was associated with a statistically significant higher rate of placenta accreta and PIH. Compared to natural frozen cycles, higher rates of hypertensive disorders and preeclampsia in pregnancy were detected in HRT cycles (14, 15, 21). Recent studies focused on the number of corpus luteum (CL) (14, 35), which can impact obstetric outcomes. Programmed frozen embryo transfer without ovulation is absent of CL, and natural cycle FET due to spontaneous ovulation has a CL. There is an increased rate of preeclampsia in programmed FET cycles where no CL is present. The study showed highly increased rates of preeclampsia in HRT FET cycles compared to other FET protocols (14). Vascular health in early pregnancy was altered in women with aberrant numbers of CL (0 or >3) and might represent insufficient cardiovascular adaptation contributing to an increased risk of preeclampsia (35).
The average birth weight from HRT was significantly greater compared with NC (36). A higher risk of post-term delivery and Cesarean section were noted in patients who conceived singletons after HRT cycle compared with those who conceived after NC-FET (21, 36). FET singletons had an increased risk of being born LGA (8), but the frequencies of macrosomia were comparable between patients after NC-FET and HRT-FET (21). Artificial hormone circumstances in frozen embryo transfer during the HRT cycle may change the placental basal plate and be causatively associated with the amount of bleeding in deliveries (16). The research indicated the association of the thinned decidual layer with pregnancies after the frozen-thawed embryo transfer (16).
Although our study had a relatively large sample, it was neither designed nor powered to show differences in obstetric and neonatal complications. The strengths of this study included the multicenter source of the data, which enhanced the generalizability of our results. In addition, data collection on maternal and neonatal outcomes was obtained in a consistent way and adjustment was made for several confounders. There are also limitations to this study. First, though it was a relatively large-sample study from a randomized clinical trial, the selection of endometrial preparation regimen for frozen single blastocyst is not random. Our results need to be confirmed by future randomized controlled trials. Second, there were differences in baseline characteristics between the two protocols, which reduced comparability. Although multivariate analysis was performed, the interaction between the confounders was not clear. Additionally, only young women with a good prognosis were included, thus we should also be cautious to extend the results to patients with older age, poor ovarian response, or repeatedly previous failed IVF cycles whose risks of obstetric complications may be higher than good prognosis patients. Finally, elements of the pragmatic design such as whether to use HCG trigger in natural cycles, duration of both estrogen and progesterone supplementation, or choice of luteal support could have affected results. Thus, whether endometrium preparation with hormone replacement acts as an unfavorable factor for the occurrence of biomedical miscarriage warrants further study. If so, what the mechanism is also needs to be investigated.
Conclusion
In summary, in women with ovulation there were no significant differences of maternal and neonatal complications in single frozen blastocyst transfer after natural cycle or HRT cycle regimens. Natural cycle was associated with a lower biomedical miscarriage rate.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Center for Reproductive Medicine of Shandong University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
YS was in charge of the trial conduct. JL, JZ, GH, JT, and YS designed the study. YS, JZ, GH, JT, ZW, and NX acquired the data. ZW, YP, and QJ performed the statistical analyses. YP, ZW, and QJ interpreted the data. JL wrote the first draft of the report with inputs from JZ, GH, and JT. YS provided comments, participated in additional discussions, and revised the paper. All authors approved the final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all participants in this study, all research staff in study sites.
Footnotes
Funding. This work was supported by National Key R&D Program of China (2018YFC1003202, 2017YFC1001004) and Taishan scholar project special funds (No. ts201712103).
References
- 1.Mancuso AC, Boulet SL, Duran E, Munch E, Kissin DM, Van Voorhis BJ. Elective single embryo transfer in women less than age 38 years reduces multiple birth rates, but not live birth rates, in United States fertility clinics. Fertil Steril. (2016) 106:1107–14. 10.1016/j.fertnstert.2016.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Groenewoud ER, Cohlen BJ, Macklon NS. Programming the endometrium for deferred transfer of cryopreserved embryos: hormone replacement versus modified natural cycles. Fertil Steril. (2018) 109:768–74. 10.1016/j.fertnstert.2018.02.135 [DOI] [PubMed] [Google Scholar]
- 3.Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y, et al. Fresh versus Frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med. (2016) 375:523–33. 10.1056/NEJMoa1513873 [DOI] [PubMed] [Google Scholar]
- 4.Wei D, Yu Y, Sun M, Shi Y, Sun Y, Deng X, et al. The effect of supraphysiological estradiol on pregnancy outcomes differs between women with PCOS and ovulatory women. J Clin Endocrinol Metab. (2018) 103:2735–42. 10.1210/jc.2018-00613 [DOI] [PubMed] [Google Scholar]
- 5.Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. (2016) CD002118 10.1002/14651858.CD002118.pub5 [DOI] [PubMed] [Google Scholar]
- 6.Wei D, Liu J-Y, Sun Y, Shi Y, Zhang B, Liu J-Q, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. (2019) 393:1310–8. 10.1016/S0140-6736(18)32843-5 [DOI] [PubMed] [Google Scholar]
- 7.Ishihara O, Araki R, Kuwahara A, Itakura A, Saito H, Adamson GD. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. (2014) 101:128–33. 10.1016/j.fertnstert.2013.09.025 [DOI] [PubMed] [Google Scholar]
- 8.Pinborg A, Henningsen AA, Loft A, Malchau SS, Forman J, Andersen AN. Large baby syndrome in singletons born after frozen embryo transfer (FET): is it due to maternal factors or the cryotechnique? Hum Reprod. (2014) 29:618–27. 10.1093/humrep/det440 [DOI] [PubMed] [Google Scholar]
- 9.Chang EM, Han JE, Kim YS, Lyu SW, Lee WS, Yoon TK. Use of the natural cycle and vitrification thawed blastocyst transfer results in better in-vitro fertilization outcomes. J Assist Reprod Genet. (2011) 28:369–74. 10.1007/s10815-010-9530-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng Y, Dong X, Huang B, Zhang H, Ai J. The artificial cycle method improves the pregnancy outcome in frozen–thawed embryo transfer: a retrospective cohort study. Gynecol Endocrinol. (2014) 31:70–4. 10.3109/09513590.2014.958988 [DOI] [PubMed] [Google Scholar]
- 11.Lathi RB, Chi YY, Liu J, Saravanabavanandhan B, Hegde A, Baker VL. Frozen blastocyst embryo transfer using a supplemented natural cycle protocol has a similar live birth rate compared to a programmed cycle protocol. J Assist Reprod Genet. (2015) 32:1057–62. 10.1007/s10815-015-0499-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alur-Gupta S, Hopeman M, Berger DS, Gracia C, Barnhart KT, Coutifaris C, et al. Impact of method of endometrial preparation for frozen blastocyst transfer on pregnancy outcome: a retrospective cohort study. Fertil Steril. (2018) 110:680–6. 10.1016/j.fertnstert.2018.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghobara T, Gelbaya TA, Ayeleke RO. Cycle regimens for frozen-thawed embryo transfer. Cochrane Database Syst Rev. (2017) 7:CD003414. 10.1002/14651858.CD003414.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ginstrom Ernstad E, Wennerholm UB, Khatibi A, Petzold M, Bergh C. Neonatal and maternal outcome after frozen embryo transfer: increased risks in programmed cycles. Am J Obstet Gynecol. (2019) 221:126.e1–18. 10.1016/j.ajog.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 15.Jing S, Li XF, Zhang S, Gong F, Lu G, Lin G. Increased pregnancy complications following frozen-thawed embryo transfer during an artificial cycle. J Assist Reprod Genet. (2019) 36:925–33. 10.1007/s10815-019-01420-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakamura Y, Yaguchi C, Itoh H, Sakamoto R, Kimura T, Furuta N, et al. Morphologic characteristics of the placental basal plate in in vitro fertilization pregnancies: a possible association with the amount of bleeding in delivery. Hum Pathol. (2015) 46:1171–9. 10.1016/j.humpath.2015.04.007 [DOI] [PubMed] [Google Scholar]
- 17.Wei D, Sun Y, Liu J, Liang X, Zhu Y, Shi Y, et al. Live birth after fresh versus frozen single blastocyst transfer (Frefro-blastocyst): study protocol for a randomized controlled trial. Trials. (2017) 18:253. 10.1186/s13063-017-1993-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, et al. Birth weight reference percentiles for Chinese. PLoS ONE. (2014) 9:e104779. 10.1371/journal.pone.0104779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Groenewoud ER, Cohlen BJ, Al-Oraiby A, Brinkhuis EA, Broekmans FJ, De Bruin JP, et al. A randomized controlled, non-inferiority trial of modified natural versus artificial cycle for cryo-thawed embryo transfer. Hum Reprod. (2016) 31:1483–92. 10.1093/humrep/dew120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerrillo M, Herrero L, Guillen A, Mayoral M, Garcia-Velasco JA. Impact of endometrial preparation protocols for Frozen embryo transfer on live birth rates. Rambam Maimonides Med J. (2017) 8:e0020. 10.5041/RMMJ.10297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saito K, Miyado K, Yamatoya K, Kuwahara A, Inoue E, Miyado M, et al. Increased incidence of post-term delivery and Cesarean section after frozen-thawed embryo transfer during a hormone replacement cycle. J Assist Reprod Genet. (2017) 34:465–70. 10.1007/s10815-017-0869-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackens S, Santos-Ribeiro S, Van De Vijver A, Racca A, Van Landuyt L, Tournaye H, et al. Frozen embryo transfer: a review on the optimal endometrial preparation and timing. Hum Reprod. (2017) 32:2234–42. 10.1093/humrep/dex285 [DOI] [PubMed] [Google Scholar]
- 23.Yarali H, Polat M, Mumusoglu S, Yarali I, Bozdag G. Preparation of endometrium for frozen embryo replacement cycles: a systematic review and meta-analysis. J Assist Reprod Genet. (2016) 33:1287–304. 10.1007/s10815-016-0787-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Wilde MA, Lamain-De Ruiter M, Veltman-Verhulst SM, Kwee A, Laven JS, Lambalk CB, et al. Increased rates of complications in singleton pregnancies of women previously diagnosed with polycystic ovary syndrome predominantly in the hyperandrogenic phenotype. Fertil Steril. (2017) 108:333–40. 10.1016/j.fertnstert.2017.06.015 [DOI] [PubMed] [Google Scholar]
- 25.Wei DM, Zhang ZZ, Wang Z, Li P, Wang JF, Liu YJ, et al. Effect of hyperandrogenism on obstetric complications of singleton pregnancy from in vitro fertilization in women with polycystic ovary syndrome. Zhonghua Fu Chan Ke Za Zhi. (2018) 53:18–22. 10.3760/cma.j.issn.0529-567X.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 26.Levron J, Yerushalmi GM, Brengauz M, Gat I, Katorza E. Comparison between two protocols for thawed embryo transfer: natural cycle versus exogenous hormone replacement. Gynecol Endocrinol. (2014) 30:494–7. 10.3109/09513590.2014.900032 [DOI] [PubMed] [Google Scholar]
- 27.Kang HJ. Programmed versus natural frozen embryo transfer: which is the best nest? Fertil Steril. (2018) 110:636–7. 10.1016/j.fertnstert.2018.06.020 [DOI] [PubMed] [Google Scholar]
- 28.Casper RF, Yanushpolsky EH. Optimal endometrial preparation for frozen embryo transfer cycles: window of implantation and progesterone support. Fertil Steril. (2016) 105:867–72. 10.1016/j.fertnstert.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 29.Altmae S, Tamm-Rosenstein K, Esteban FJ, Simm J, Kolberg L, Peterson H, et al. Endometrial transcriptome analysis indicates superiority of natural over artificial cycles in recurrent implantation failure patients undergoing frozen embryo transfer. Reprod Biomed Online. (2016) 32:597–613. 10.1016/j.rbmo.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 30.Groenewoud ER, Cantineau AEP, Kollen BJ, Macklon NS, Cohlen BJ. What is the optimal means of preparing the endometrium in frozen-thawed embryo transfer cycles? A systematic review and meta-analysis. Hum Reprod Update. (2017) 19:458–70. 10.1093/humupd/dmw046 [DOI] [PubMed] [Google Scholar]
- 31.Hill MJ, Miller KA, Frattarelli JL. A GnRH agonist and exogenous hormone stimulation protocol has a higher live-birth rate than a natural endogenous hormone protocol for frozen-thawed blastocyst-stage embryo transfer cycles: an analysis of 1391 cycles. Fertil Steril. (2010) 93:416–22. 10.1016/j.fertnstert.2008.11.027 [DOI] [PubMed] [Google Scholar]
- 32.Eftekhar M, Rahmani E, Pourmasumi S. Evaluation of clinical factors influencing pregnancy rate in frozen embryo transfer. Iran J Reprod Med. (2014) 12:513–8. [PMC free article] [PubMed] [Google Scholar]
- 33.Lee VCY, Li RHW, Chai J, Yeung TWY, Yeung WSB, Ho PC, et al. Effect of preovulatory progesterone elevation and duration of progesterone elevation on the pregnancy rate of frozen–thawed embryo transfer in natural cycles. Fertil Steril. (2014) 101:1288–93. 10.1016/j.fertnstert.2014.01.040 [DOI] [PubMed] [Google Scholar]
- 34.Montagut M, Santos-Ribeiro S, De Vos M, Polyzos NP, Drakopoulos P, Mackens S, et al. Frozen–thawed embryo transfers in natural cycles with spontaneous or induced ovulation: the search for the best protocol continues. Hum Reprod. (2016) 31:2803–10. 10.1093/humrep/dew263 [DOI] [PubMed] [Google Scholar]
- 35.Von Versen-Hoynck F, Narasimhan P, Selamet Tierney ES, Martinez N, Conrad KP, Baker VL, et al. Absent or excessive corpus luteum number is associated with altered maternal vascular health in early pregnancy. Hypertension. (2019) 73:680–90. 10.1161/HYPERTENSIONAHA.118.12046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ishii R, Shoda A, Kubo M, Okazaki S, Suzuki M, Okawa R, et al. Identifying a possible factor for the increased newborn size in singleton pregnancies after assisted reproductive technology using cryopreserved embryos, in comparison with fresh embryos. Reprod Med Biol. (2018) 17:307–14. 10.1002/rmb2.12206 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.