Abstract
Patient: Female, 25-year-old
Final Diagnosis: Wandering spleen
Symptoms: Abdominal pain
Medication:—
Clinical Procedure: —
Specialty: Surgery
Objective:
Rare disease
Background:
Wandering spleen is a rare condition in which the spleen lacks the usual peritoneal attachments, resulting in increased intra-abdominal mobility. Complications can occur due to the torsion of the splenic vascular pedicle, resulting in symptoms ranging from an incidental finding to an acute abdomen as a result of an ischemic necrosis of the spleen.
Case Report:
We present the case of a 25-year-old female patient who presented with a recurring abdominal pain associated with serum lipase and C-reactive protein elevation. The computed tomography scan revealed torsion of the splenic pedicle and hypoperfusion of the spleen. A surgical exploration was performed and a wandering spleen was diagnosed perioperatively. It was characterized by the lack of peritoneal ligaments, thus resulting in a splenic volvulus. A splenectomy was carried out due to the definite ischemic necrosis of the spleen.
Conclusions:
The diagnosis of this rare condition can be very challenging since it can be presented with a vast variety of symptoms, mimicking other abdominal pathologies. The intermittent nature of an ultimate splenic torsion can add to the diagnostic challenge. Medical literature concerning the wandering spleen and knowledge about this pathology originates mainly from individual case reports. Despite the evolving diagnostic modalities available, this rare and ambiguous disorder remains misdiagnosed, and a high index of suspicion is needed for the appropriate diagnosis to be established.
MeSH Keywords: Abdominal Pain, Splenectomy, Splenic Infarction, Wandering Spleen
Background
Wandering spleen is a rare condition in which the loss or weakening of one or more ligaments of the spleen leads to the organ’s increased mobility and instability [1]. An important sequela of this excessive mobilization is torsion of the splenic vascular pedicle, which ultimately causes necrosis of the parenchyma. The etiology of this uncommon disorder can be congenital or acquired. The rarity of this disease, as well as the non-specific nature of its clinical presentation, make the wandering spleen an elusive diagnosis. We present a case of a young woman, initially diagnosed with acute pancreatitis, who presented a torsion of the splenic vessels due to the absence of the splenocolic and splenophrenic ligaments.
Case Report
A 25-year-old female patient, with a medical history of depression under neuroleptic treatment, was investigated in the emergency department of our institution for an epigastric pain associated with several episodes of vomiting. The onset of symptoms was gradual, with a duration of several days and progressive worsening. Ultimately, abdominal pain exacerbation resulted in the patient’s consultation in the emergency department.
Initial physical examination revealed an epigastric pain without rebound tenderness, and laboratory evaluation showed normal laboratory inflammatory markers. As a result of the reassuring clinical examination and laboratory values, the patient was discharged.
The following day, a scheduled medical re-evaluation revealed an ongoing abdominal pain with elevated lipase and C-reactive protein on laboratory testing. At this point, a drug-induced pancreatitis was suspected due to the patient’s neuroleptic treatment, and she was hospitalized. Further investigations in the form of an abdominal ultrasound excluded a biliary cause of pancreatitis. However, the examination identified a splenomegaly as well as a small quantity of peritoneal effusion.
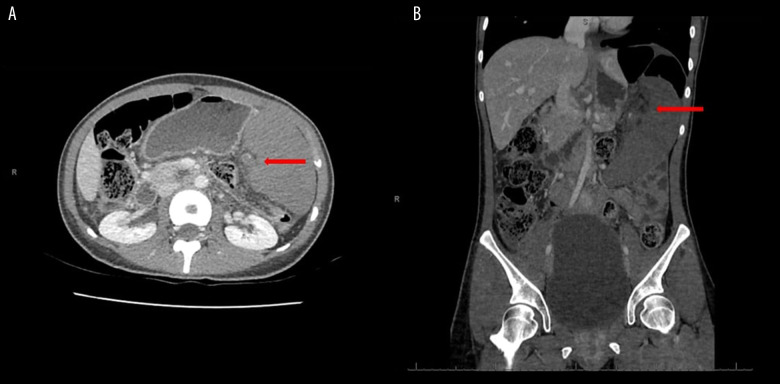
The findings of the abdominal ultrasound and the persistence of the patient’s symptoms dictated that we conduct of an abdominal/pelvic computed tomography scan. The examination confirmed the presence of a splenomegaly and demonstrated hypoperfusion of the enlarged spleen due to a volvulus of its vascular pedicle (Figure 1). At this point, a splenic volvulus was suspected, and the patient was transferred to our department of General Surgery. An exploratory laparotomy was conducted the following day. A torsion of the splenic vascular pedicle was discovered, secondary to the absence of the splenocolic and splenophrenic ligaments, therefore establishing the diagnosis of a wandering spleen.
Figure 1.
Computed tomography images with arrows demonstrating a splenomegaly associated with spleen hypoperfusion. Axial (A) and coronal (B) reconstruction planes.
After the detorsion of the vascular pedicle, the spleen remained necrotic, showing no signs of recuperation. A thrombosis of the splenic pedicle was suspected and a splenectomy was carried out (Figure 2). The operation was successful, without any perioperative complications.
Figure 2.
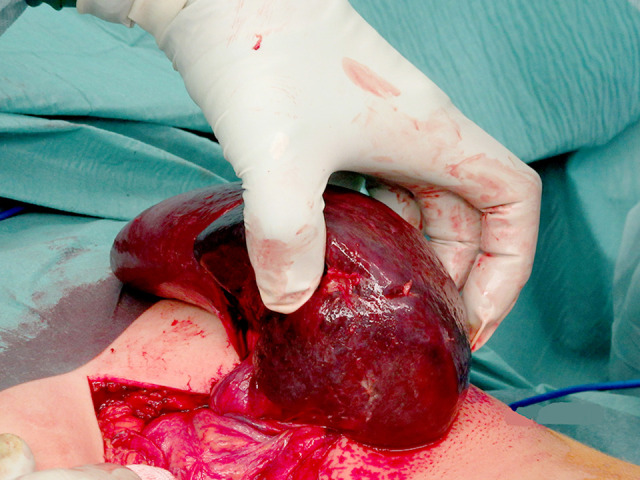
Torsion of the splenic vascular pedicle responsible for an ischemic necrosis of the spleen.
The final histopathology report documented a thrombosis of the splenic artery and vein associated with hemorrhagic necrosis of the splenic parenchyma. The patient had an uneventful recovery and was discharged 7 days after surgery.
Discussion
Wandering spleen is a condition characterized by the increased laxity or total absence of the splenic ligaments and subsequent failure of the spleen to maintain orthotopic position, predis-posing it to increased motility and even migration to unusual intra-abdominal or pelvic loci. Secondary to this phenomenon is the elongation of the spleen’s vascular pedicle, which acts as an axon and, prone to torsion, results in hypoperfusion of the splenic parenchyma, congestion, thrombosis, and ultimately infarction and necrosis of the spleen. A number of peritoneal attachments keep the spleen in its proper anatomic position, the most constant and clinically important being the splenogastric ligament, which contains the short gastric vessels. The others are the splenocolic ligament, splenophrenic ligament, splenoomental ligament, and splenorenal ligament, which envelops the hilar vessels [2]. In our patient’s case, we identified the complete absence of the splenocolic and splenophrenic ligaments.
The etiology of this disorder may be congenital or acquired. While the pathophysiologic mechanism of congenital wandering spleen remains unknown, most studies in the medical literature associate it with the faulty development of the mesogastrium dorsum during embryonic life. Related acquired conditions include splenomegaly, history of intra-abdominal trauma, and pregnancy [3].
Whether congenital or acquired, wandering spleen is a rare disorder with an unknown incidence rate, as fewer than 500 cases have been reported in the literature to date. Despite the lack of ample statistical data, a bimodal incidence may be suggested by the current evidence, further favoring both congenital and acquired etiologies. Up to one-third of all cases appear to be children, with 30% being under 10 years old. The male to female ratio is 1: 1 in this population. The second peak in incidence occurs between 20 and 40 years, with the male to female ratio changing to 1: 7, potentially further enhancing the association of wandering spleen with pregnancy [4].
The clinical presentation of wandering spleen may vary from chronic, mild abdominal discomfort caused by intermittent vascular torsion to acute abdomen caused by splenic infarction. An asymptomatic abdominal mass may also be the sole manifestation of the disease. Other infrequent conditions associated with a wandering spleen are gastric volvulus, variceal hemorrhage, and acute pancreatitis, due to affliction of the pancreatic tail confined to the lienorenal ligament [5,6]. Our patient presented with acute epigastric pain and elevated levels of lipase and C-reactive protein, findings compatible with the diagnosis of acute pancreatitis.
As clinical presentation and laboratory studies are nonspecific, imaging examinations form the basis of diagnosis. Ultrasonography and computed tomography are of use, offering the additional advantage of controlling blood flow [7]. Radio-isotopic study by Te99 can also be used to evaluate spleen function, although its availability is limited compared to conventional imaging techniques. Owing to the limited availability of data, there has been no conclusion drawn on the superiority of each imaging technique concerning sensitivity and specificity [7,8]. In our case, the abdominal ultrasound revealed an enlarged spleen and pathologic intra-abdominal effusion without other abnormalities, while the vascular torsion and hypoperfusion of the spleen were evident in the subsequent computed tomography scan.
Surgical treatment appears to be the optimal strategy in cases of a wandering spleen. When feasible, preservation of the spleen should be encouraged. The physiological importance of the spleen is well established since it is an important part of the reticulo-endothelial system and plays a vital role in antigen clearance, particularly in encapsulated organisms such as Pneumococcus, Meningococcus and Haemophilus influenza [9]. Splenopexy, either open or laparoscopic, is a spleen preserving technique that can be employed in the absence of infarction or abundant splenomegaly, precluding spleen mobilization. Multiple techniques have been described, with fixation of the spleen by absorbable sutures or by absorbable mesh placement [10,11]. No technique has shown superiority concerning long-term results.
In cases where spleen preservation is not an option because of lack of viable spleen parenchyma, splenectomy appears to be the only solution. Both open and laparoscopic approaches appear to be safe. Although reports of nonoperative treatment exist, it is not recommended, especially in the absence of important contraindications for surgery, because the risk of an impending abdominal catastrophe remains high.
Conclusions
Wandering spleen remains a rare condition with nonspecific presentation ranging from a mild, chronic discomfort to an acute abdomen. Despite the diagnostic modalities available, a high index of clinical suspicion is necessary for diagnosis. Surgical treatment is encouraged with spleen preservation techniques such as splenopexy, the preferable option if the spleen is viable and patient status allows such intervention. In our case, we opted for an open splenectomy owing to the extensive necrosis of the spleen parenchyma.
Footnotes
Conflict of interest
None.
References:
- 1.Reisner DC, Burgan CM. Wandering spleen: An overview. Curr Probl Diagn Radiol. 2018;47(1):68–70. doi: 10.1067/j.cpradiol.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Lefor AT, Phillips EH. Spleen. In: Norton JA, Barie PS, Bollinger RR, et al., editors. Surgery – basic science and clinical evidence. 2nd ed. Germany: Springer; 2008. p. 1112. [Google Scholar]
- 3.Allen KB, Gay BB, Skandalakis JE. Wandering spleen: Anatomic and radiologic considerations. South Med J. 1992;85:976–84. doi: 10.1097/00007611-199210000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Desai DC, Hebra A, Davidoff AM, Schnaufer L. Wandering spleen: A challenging diagnosis. Douth Med J. 1997;90:439–43. doi: 10.1097/00007611-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Qazi SA, Mirya SM, Muhammad AA, et al. Wandering spleen. Saudi J Gastroenterol. 2004;10:1–7. [PubMed] [Google Scholar]
- 6.Rosen A, Nathan H, Luciansky E, Sayfan J. The lienorenal ligament and the tail of the pancreas: A surgical anatomical study. Pancreas. 1988;3(1):104–7. doi: 10.1097/00006676-198802000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Taori K, Ghonge N, Prakash A. Wandering spleen with torsion of vascular pedicle: Early diagnosis with multiplaner reformation technique of multislice spiral CT. Abdom Imaging. 2004;29(4):479–81. doi: 10.1007/s00261-003-0142-7. [DOI] [PubMed] [Google Scholar]
- 8.Kanthan R, Radhi JM. The ‘true’ splenic wanderer. Can J Gastroenterol. 1999;13(2):169–71. doi: 10.1155/1999/828742. [DOI] [PubMed] [Google Scholar]
- 9.Dawson JH, Roberts NG. Management of the wandering spleen. Aust NZJ Surg. 1994;64(6):441–44. doi: 10.1111/j.1445-2197.1994.tb02249.x. [DOI] [PubMed] [Google Scholar]
- 10.Seashore JH, McIntosh S. Elective splenopexy for wandering spleen. J Pediatr Surg. 1990;25(2):270–72. doi: 10.1016/0022-3468(90)90438-f. [DOI] [PubMed] [Google Scholar]
- 11.Hirose R, Kitano S, Bando T, et al. Laparoscopic splenopexy for pediatric wandering spleen. J Pediatr Surg. 1998;33(10):1571–73. doi: 10.1016/s0022-3468(98)90503-6. [DOI] [PubMed] [Google Scholar]