Abstract
Background.
The relation between psychopathic traits and suicide ideation (SI) is frequently discussed but little research has examined potential mechanisms underlying this association. The interpersonal theory of suicide (ITS) proposes two mechanisms in the pathogenesis of suicidal desire: thwarted belongingness (TB) and perceived burdensomeness (PB). This study cross-sectionally tested TB and PB as possible explanatory links in the relation between psychopathic traits and SI.
Method.
Archival data from 784 male United Kingdom prisoners (Mage = 37.21, SD = 9.97) were analyzed using structural equation modeling.
Results.
Psychopathic traits were indirectly associated with SI through more specific suicide-promoting processes—namely, TB and PB. More specifically, results indicated that Egocentricity and Stimulus Seeking were indirectly associated with SI through PB and TB in combination. However, results indicated specific indirect effects of TB in the relations between the Antisocial Behavior, Egocentricity, and Stimulus Seeking facets, and SI; whereas, specific indirect effects for PB were only significant in the relations between Egocentricity and Stimulus Seeking facets and SI.
Conclusion.
Preliminary results are consistent with the ITS and suggest that psychopathic traits may be distal risk markers for SI and provide direction for future research that could inform suicide prevention efforts among male prisoners high in such traits.
Keywords: Psychopathic, thwarted belonging, perceived burden, interpersonal theory of suicide, prisoners, suicide ideation
Suicide is a leading cause of death in custodial settings across the globe (Konrad et al., 2007; Rabe, 2012). Data from 24 high-income countries indicate suicide rates among prisoners are three to nine times higher than those found in the general population (Fazel et al., 2017). In addition, international studies have documented that, during their lifetime, 15% to 21% of prisoners have attempted suicide and 34% to 44% have experienced suicide ideation (SI; Larney et al., 2012; Sarchiapone et al., 2009). These data indicate a need to examine risk factors for suicide among prisoners to inform prevention, assessment, and intervention efforts. The purpose of the current study was to further examine the association between specific psychopathic traits (Egocentricity, Stimulus Seeking, and Antisocial Behaviors), and SI through the lens of the interpersonal theory of suicide (ITS; Joiner, 2007; Van Orden et al., 2010).
Psychopathy
Psychopathy is a personality syndrome characterized by a diminished capacity for remorse, impulsive behavior, and superficial charm (Cleckley, 1976). Although several factor models have been validated using various psychopathy measures (e.g., Brinkley et al., 2008; Hare et al., 2018; Patrick et al., 2009), a two-factor solution has largely dominated the literature. Within this model, Factor 1 captures the callous and unemotional personality style indicative of psychopathy; whereas, Factor 2 is comprised of impulsivity, a deviant lifestyle, and, in some measures, antisociality (Hare & Neumann, 2010). These two factors have divergent relations with a number of psychological and social variables in incarcerated samples and across assessment methods. For example, Factor 1 has been associated with low anxiety, positive adjustment, social dominance, and emotional detachment1 (e.g., Benning et al., 2003; Patrick et al., 1993; Schmitt & Newman, 1999); whereas, Factor 2 has a unique association with more general externalizing tendencies, recidivism, and neuroticism (e.g., Benning et al., 2003; Hemphill et al., 1998).
Another way of conceptualizing the psychopathy construct (and thus the relations between psychopathy and SI) involves the triarchic model (Patrick et al., 2009). The triarchic model represents three distinct but intersecting phenotypic dispositions: Boldness, Meanness, and Disinhibition. Boldness encompasses social confidence, emotional resilience, venturesomeness, and similar constructs (e.g., fearless dominance). Meanness is characterized by emotional callousness, lack of affiliative capacity, low empathy, manipulativeness, and antagonism. Disinhibition entails impulsivity, weak constraint, hostility, and poor emotion regulation. These three factors have divergent relations with various psychological and social variables (Patrick et al., 2009), including general externalizing tendencies (e.g., antisocial behavior, substance abuse), recidivism, and psychopathology (for a review, see Patrick & Drislane, 2015).
Psychopathic Traits and Suicide
Psychopathic traits have historically been viewed as protective against suicide due to the egocentricity and low levels of negative emotionality presumed to be common among individuals high in psychopathic traits (Cleckley, 1976). However, recent research has shown more nuanced relations between psychopathic traits and suicidal thoughts and behaviors (see Dhingra et al., 2018). Research with various samples and assessment methods typically demonstrates a bifurcated relation, such that Factor 1 (interpersonal-affective traits) is orthogonal or negatively related to suicide attempt history (Douglas et al., 2006, 2008; Heirigs et al., 2018; Swogger et al., 2009; Verona et al., 2001, 2005) and current SI (Douglas et al., 2006, 2008; Gunter et al., 2011); whereas, Factor 2 (antisocial-lifestyle traits) is positively correlated with suicide attempt history (Douglas et al., 2006, 2008; Gunter et al., 2011; Smith et al., 2014; Swogger et al., 2009; Verona et al., 2001, 2005) and current SI (Douglas et al., 2006, 2008; Heirigs et al., 2018; Gunter et al., 2011; Smith et al., 2014). Greater detail on the relations between psychopathic traits and suicide risk can be found elsewhere (e.g., Dhingra et al., 2018; Douglas et al., 2006).
Recent research has also linked Patrick et al.’s (2009) triarchic constructs to SI. Specifically, Disinhibition and (low) Boldness have been found to positively predict SI when assessed via self-report and composite psychological/neurological (“psychoneurometric”) indices in samples of young adult men, adult twins, and adult psychiatric outpatients (Venables et al., 2015, 2018). In sum, research has indicated that psychopathic traits, depending on how they are conceptualized, are linked to suicidal thoughts and behaviors; however, it remains unclear how these findings may be conceptualized through a contemporary theoretical framework of suicidal behavior.
The Interpersonal Theory of Suicide (ITS)
The ITS (Joiner, 2005; Van Orden et al., 2010) has the potential to enhance our understanding of the relations between psychopathic traits and SI. The ITS suggests SI results from the combined presence of two interpersonal deficits: perceived burdensomeness (PB; indicated by feelings of liability and self-hatred) and thwarted belongingness (TB; indicated by feelings of social disconnectedness and low reciprocal care). SI is thought to develop when one is hopeless about the improvement of these cognitive-affective states (Van Orden et al., 2010). Furthermore, SI is posited to translate into action, in the form of suicide attempt, only in the presence of an additional third construct, capability for suicide (Joiner, 2007; Van Orden et al., 2010), which is consistent with other modern ideation-to-action theories of suicide (i.e., Integrated Motivational-Volitional Model [IMV; O’Connor & Kirtley, 2018], the Three-Step Theory of Suicide [3ST; Klonsky & May, 2015]).
Of note, the ITS postulates that TB and PB represent proximal predictors of SI and, as such, may account for (i.e., statistically mediate) the relations between various suicide risk factors and suicidal thoughts and behaviors (Van Orden et al., 2010). The ITS has been extensively researched and has gained empirical support (for a review, see Chu et al., 2017). Of particular relevance to the current research, in explicit tests of mediation, the ITS variables have been found to mediate the effect of other distal risk factors for suicide such as perfectionism and alcohol-related problems (e.g., Lamis & Malone, 2011; Rasmussen et al., 2012). The current study only focuses on the indirect effects of specific psychopathic traits (Egocentricity, Stimulus Seeking, and Antisocial Behaviors), through TB and PB given that SI is the outcome of interest. Therefore, suicide capability is not addressed in the current study.
Psychopathic Traits, Unmet Needs, and SI
There is limited information about psychopathic traits’ association with SI within the context of the ITS. Among undergraduates who completed the Levenson Self-Report Psychopathy Scales (LSRP; Levenson et al., 1995), Anestis et al. (2016) found that both the impulsive–antisocial factor (Factor 2) and the interpersonal–affective factor (Factor 1) were positively correlated with TB and PB; however, only Factor 2 was uniquely positively associated with TB and PB. Similarly, among male prisoners, Factors 1 and 2 were positively correlated with proxies of TB and PB; however, overall, Factor 2 was most often uniquely positively associated with proxies of TB and PB. In a military sample, Harrop et al. (2017) found that all three LSRP factors (Egocentricity, Callous, and Antisocial) uniquely positively predicted PB when controlling for other LSRP factors, whilst the LSRP-Antisocial and LSRP-Callous factors were unique positive predictors of TB, when controlling for other measure factors. Somewhat differently, in their undergraduate sample, Harrop et al. (2017) found that the LSRP-Egocentricity and LSRP-Antisocial factors each uniquely positively predicted PB, and the LSRP-Antisocial factor uniquely positively predicted TB.
Using Patrick et al.’s (2009) triarchic constructs in their undergraduate sample, Harrop et al. (2017) found an inverse relation between Boldness, and TB and PB; whereas, Meanness and Disinhibition were positively related to TB and PB. Similarly, Buchman-Schmitt et al. (2017) found that both Disinhibition and (low) Boldness were uniquely positively associated with PB and TB among young adults who endorsed a history of suicide attempts and/or SI. Further, they observed specific interactive effects whereby Boldness served as a protective factor against PB and TB. Finally, among gun-owning adults, Disinhibition, but not Meanness (which was negatively related), was positively related to PB, and both Meanness and Disinhibition were positively related to TB. Furthermore, Boldness exerted a buffering effect on the relation of Disinhibition to PB (Anestis et al., 2018).
It warrants mention that the various psychopathy measures used in previous research are not isomorphic. As such, associations between specific psychopathic traits and SI might depend on the operationalization of psychopathy. However, collectively, the above research suggests that both Factor 1/Boldness (dispositional fearfulness) and appears to confer protection against SI; whereas, Factor 2/Disinhibition confers risk towards the development of SI. Despite largely converging findings, there remains a relative lack of research investigating the theory-driven factors underlying this relation.
The Current Study
Although there is evidence supporting the idea that Factor 2/Disinhibition psychopathic traits are positively related to SI, there is a paucity of information on how interpersonal deficits may explain these associations. Such information could inform treatment initiatives for prisoners, who are at elevated risk for psychopathic traits (Coid et al., 2009) and suicidal thoughts and behaviors (e.g., Larney et al., 2012). The present study aimed to address this conceptual and empirical gap in the literature by investigating potential mechanisms underlying the relation between psychopathic traits and SI. Consistent with the ITS, which suggests that the simultaneous experience of TB and PB produces SI (Van Orden et al., 2010); we tested PB and TB as parallel mediators of the relation between psychopathic traits (Egocentricity, Stimulus Seeking, and Antisocial Behaviors) and SI. This allowed for the test of the total or additive indirect effects of TB and PB, as well as the specific or unique indirect effects of TB or PB when adjusting for the other mediator variable (Roush et al., 2018). This approach is consistent with previous research testing specific and total indirect effects with TB and PB as intervening variables (e.g., Brown et al., 2019).
We predicted that TB and PB, and two of the psychopathy facets (i.e., Stimulus Seeking and Antisocial Behaviors), representing Factor 2, would be positively correlated with SI, but the facet representing Factor 1 (i.e., Egocentricity) would be negatively correlated to SI. Given that all three psychopathic traits constructs are theoretically, and to some extent empirically, linked to SI via interpersonal deficits, we also hypothesized psychopathic traits would be indirectly linked to SI through TB and PB. Specifically, Factor 1 and 2 traits would be positively related to TB and PB, which would be consistent with previous literature (e.g., Buchman-Schmitt et al., 2017; Harrop et al., 2017). TB and PB would then, in turn, be positively associated with SI, which is consistent with previous literature as well (e.g., Chu et al., 2017).
Methods
Participants
Participants were 786 male prisoners aged between 18 and 73 years (M = 37.21, SD = 9.97). Participants were predominately White (80.8%), followed by Black (10.8%), multiracial (4.8%), Asian (3.3%), and “other” (0.1%); race data was missing for one participant. The majority of participants were single/never married (76.5%) and serving a life sentence (76.5%). The most common index offenses were murder (34.7%), robbery (13.5%), and rape (12.1%). On average, participants’ current sentence was 74.29 months (SD = 63.21 months), and they had 3.92 (SD = 4.37) previous custodial sentences. Additionally, 184 (23.5%) participants had been placed in segregation housing as a punishment during their current sentence. Participants had spent an average of 2.75 weeks (SD = 13.8 weeks) in segregated housing during the past year. Although psychiatric diagnosis data were not available for this sample, 39.1% of participants reported a suicide attempt history (31 participants were missing data), and 26.2% reported a history of non-suicidal self-injury (33 participants were missing data).
Procedure
Archival data were received from a category B (high security) prison2 in the South-East of the United Kingdom, that operates entirely as a democratic Therapeutic Community (TC)3. The prison is comprised of six TCs. This includes one assessment/treatment preparation unit and five residential communities, including one wing for men whose offending has been sexually motivated and one wing for men with learning disabilities. To be accepted into the prison, men must voluntarily apply and meet the following criteria: a) convicted of a crime and sentenced, b) have at least 18 months remaining on their sentence, c) demonstrate “treatment readiness” (as indicated by no recent involvement in violence, drug use or self-harm, as well as a willingness to change), and d) have no active symptoms of major mental illness (Bennett & Shuker, 2017). Upon reception, individuals undertake a comprehensive psychological assessment selected and administered by prison staff relating to his personality, background, and criminal history. Data from these reception batteries were de-identified and provided to the researchers for archival data analysis in the present study. Ethical approval was obtained from all necessary institutions (i.e., the prison and universities ethics boards). These data were archival, provided to the researchers by the prison. The data received by the researchers were deidentified and did not contain personally identifiable information. Thus, all data were anonymous.
Measures
Personality Assessment Inventory (PAI).
The PAI (Morey, 1991) is a 344-item self-report assessment of clinical variables, including symptoms, treatment response, and interpersonal style. Items are rated on a four-point ordinal response metric ranging from “false, not at all true” to “very true.” As discussed in depth below and consistent with previous studies (i.e., Anestis et al., 2016; Cramer et al., 2012), the current study uses the scales/subscales of Nonsupport (NON), Borderline Features–Self-Harm (BOR-S), Schizophrenia–Social Detachment (SCZ-S), and Depression–Cognitive (DEP-C) to construct proxy measures of the ITS constructs. Specifically, NON and SCZ-S contribute to the TB proxy and DEP-C to the PB proxy. Morey (1991) reported the following Cronbach’s alpha values in a combined community/student validation sample: NON = .78, BOR-S = .78, SCZ-S = .83, and DEP-C = .77. Additionally, we will use scales from the PAI for the assessment of psychopathic traits and SI.4
Thwarted belongingness (TB).
TB was assessed using the NON treatment scale and SCZ-S scale. The NON scale assesses a lack of perceived support (e.g., “My friends are available if I need them” [reversed]), quality of support (e.g., “People I’m close to are very supportive”), and an individual’s social interactions (e.g., “I spend most of my time alone”). The SCZ-S subscale assesses social isolation (e.g., “I don’t feel close to anyone”) and close relationships (e.g., “I just don’t seem to relate to people very well”). Therefore, greater higher scores on NON and SCZ-S were used to indicate elevated TB. Cramer et al. (2012) published a well-fitting model that included the NON and SCZ-S scales as manifest indicators of a latent TB variable, which is consistent with and provides support for the approach taken in our study.
Perceived burdensomeness (PB).
PB was assessed using the DEP-C subscale, which measures individuals’ sense of competence or self-efficacy (e.g., “I feel that I’ve let everyone down”). Thus, higher scores on DEP-C was used to indicate elevated PB. Given that DEP-C is a single indicator, and we lacked item-level data to model DEP-C as a latent variable, DEP-C scores were used to represent PB in our analyses. Again, our use of DEP-C as a proxy for PB is consistent with Cramer et al. (2012).
Psychopathic traits.
Psychopathic traits were assessed using the Antisocial Behaviors (ANT-A), Egocentricity (ANT-E), and Stimulus Seeking (ANT-S) scales. The ANT-A scale assesses one’s history of conduct problems and illegal behaviors. The ANT-E scale assesses self-centeredness and a lack of empathy or remorse. Higher scores on these scales indicate greater psychopathic traits. These scales have also been used as proxies for psychopathic traits where ANT-E represents Factor 1 and ANT-S and ANT-A represent Factor 2 (e.g., Douglas et al., 2008). Because we were particularly interested in the psychopathic traits scales separately, we did not model these scales as a latent variable. The PAI-ANT scores have been found to relate moderately to strongly to PCL-R and PPI total scores (r = .39 to .74; Douglas et al., 2008; Edens et al., 2000). Morey (1991) found a strong Cronbach’s alpha (.84) among men.
Suicide ideation.
SI was measured using the 12-item Suicide Ideation (SUI) treatment scale (Cronbach’s alpha = .85 to .93; Morey, 1991). Higher scores indicate greater suicidal thoughts and feelings. None of the items on SUI overlap with items from any other PAI subscale. Consistent with Cramer et al. (2012), SUI was not modeled as a latent variable given that SUI is a single indicator. We also lacked item-level data to model SUI as a latent variable. Among clinical and corrections samples, SUI scores have been associated with other self-report measures of SI, as well as suicide precaution status (Morey, 2014; Patry & Magaletta, 2015). In the current sample, 37.5% of participants had a score of 60 or greater, which is 1 SD above the average score of 50 on the PAI. Additionally, 22.1% had a score higher than 69T, which would high suicide risk (2 SD above the mean).
Data Analysis Plan
A structural equation model (SEM) was constructed to test the hypotheses using maximum likelihood estimation in Mplus version 8 (Muthén & Muthén, 2017). The psychopathic traits scales (ANT-A, ANT-E, ANT-S) were the predictor variables, the TB (NON and SCZ-S latent variable) and PB (DEP-C) variables were the mediating variables, and the SI scale (SUI) was the outcome variable. We used 10,000 bootstrapped samples to construct bias-corrected 95% confidence intervals. Direct and indirect effects were estimated using MODEL INDIRECT, where CI not containing zero indicated a significant indirect effect (Preacher & Hayes, 2008). Significant specific indirect effects indicate that there was a significant indirect effect through TB or PB when adjusting for the other (see Preacher & Hayes, 2009). Significant total indirect effects indicate a significant additive indirect effect of TB and PB (see Preacher & Hayes, 2008). This is consistent with the ITS proposition that TB and PB are risk factors for SI, and with previous research testing specific and total indirect effects with TB and PB as intervening variables (e.g., Brown et al., 2019).
Model fit was assessed using the goodness of fit χ2, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), the Tucker Lewis Index (TLI), and the standardized root mean square residual (SRMR). Good model fit is indicated by a nonsignificant χ2 statistic, an RMSEA value less than .06, a CFI and TLI greater than .95, and a SRMR value less than .08 (Hu & Bentler, 1999). It should be noted that with large samples, like in the current study, the χ2 statistic tends to be statistically significant even with good-fitting models; therefore, other fit indices were more strongly considered. Modifications indices were examined when model fit was poor, which is discussed in more detail below.
Results
Data Screening and Preparation
The data set originally contained data from 2,699 prisoners. We removed participants who were not administered the PAI, which yielded a sample of 985 prisoners. Next, we removed participants who had validity scale scores that indicated an invalid profile consistent with PAI profile clinical interpretation (Morey, 1991), which produced a sample of 786 participants.5 We compared demographic variables between those with valid or invalid profiles, which indicated were no significant differences by age (F[1, 893] = 1.12, p = .289), race (χ2[4, N = 984] = 1.14, p = .887), marital status (χ2[8, N = 935] = 3.70, p = .884), or if they were serving a life sentence (χ2[81, N = 985] = .56, p = .454). We identified six univariate outliers where a score was ± 3.29 SD from the mean; these participants’ scores were Winsorized and retained for analyses. We identified two multivariate outliers using Mahalanobis Distance scores, which were excluded from analyses; therefore, 784 participants were included in the analyses. Bivariate correlations and descriptive statistics are presented in Table 1.
Table 1.
Bivariate Correlations and Descriptive Statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. SUI | ---- | ||||||
| 2. DEP-C | .54** | ---- | |||||
| 3. SCZ-S | .42** | .58** | ---- | ||||
| 4. NON | .36** | .45** | .68** | ---- | |||
| 5. ANT-A | .07 | .17** | .08* | .16** | ---- | ||
| 6. ANT-E | .16** | .30** | .26** | .31** | .47** | ---- | |
| 7. ANT-S | .17** | .29** | .20** | .26** | .56** | .61** | ---- |
| M | 58.77 | 63.85 | 57.48 | 58.34 | 75.12 | 56.04 | 57.56 |
| SD | 16.29 | 12.22 | 12.42 | 12.90 | 9.99 | 12.54 | 14.85 |
| Observed Range | 43–112 | 37–104 | 36–94 | 37–99 | 41–93 | 39–99 | 37–104 |
Note. SUI = Suicide Ideation Scale; DEP-C = Depression-Cognitive Subscale (perceived burden proxy), SCZ-S = Social Detachment Scale (thwarted belonging proxy); NON = Non-Support Scale (thwarted belonging proxy); ANT-A = Antisocial Behaviors Subscale; ANT-E = Egocentricity Subscale; ANT-S = Stimulus-Seeking Subscale; All scales are from the Personality Assessment Inventory (PAI);
p < .05;
p < .01.
Primary Analyses
Figure 1 displays the final model with standardized path coefficients (STDYX), including the direct effects (i.e., the relation between the predictor and the outcome variable after adjusting for the mediating variables; Preacher & Hayes, 2008). To improve model fit, in accordance with the modification indices, we included the correlation between TB and PB residuals in our model (see Table 2 for model fit indices). Allowing residuals to correlate between mediators in multiple or parallel mediator SEM models has been recommended (Preacher & Hayes, 2008). Additionally, the correlation between the TB and PB residuals is also consistent with the ITS, which suggests that TB and PB are distinct, yet related constructs (Van Orden et al., 2010). A chi-square difference test (Δχ2 [Δdf = 1] = 255.49, p < .001) and the other fit indices indicated this modification produced a significant improvement in model fit; therefore, we retained the modified model. As seen in Table 2, the final model fit indices suggest that our model adequately fits the data overall. The Chi-square model fit static was significant; however, this is expected given the large sample size. RMSEA and TLI indicated mediocre model fit, whereas CFI and SRMR indicated good model fit. Therefore, we retained the final model that included the correlation between the TB and PB residuals, as presented in Figure 1.6
Figure 1.
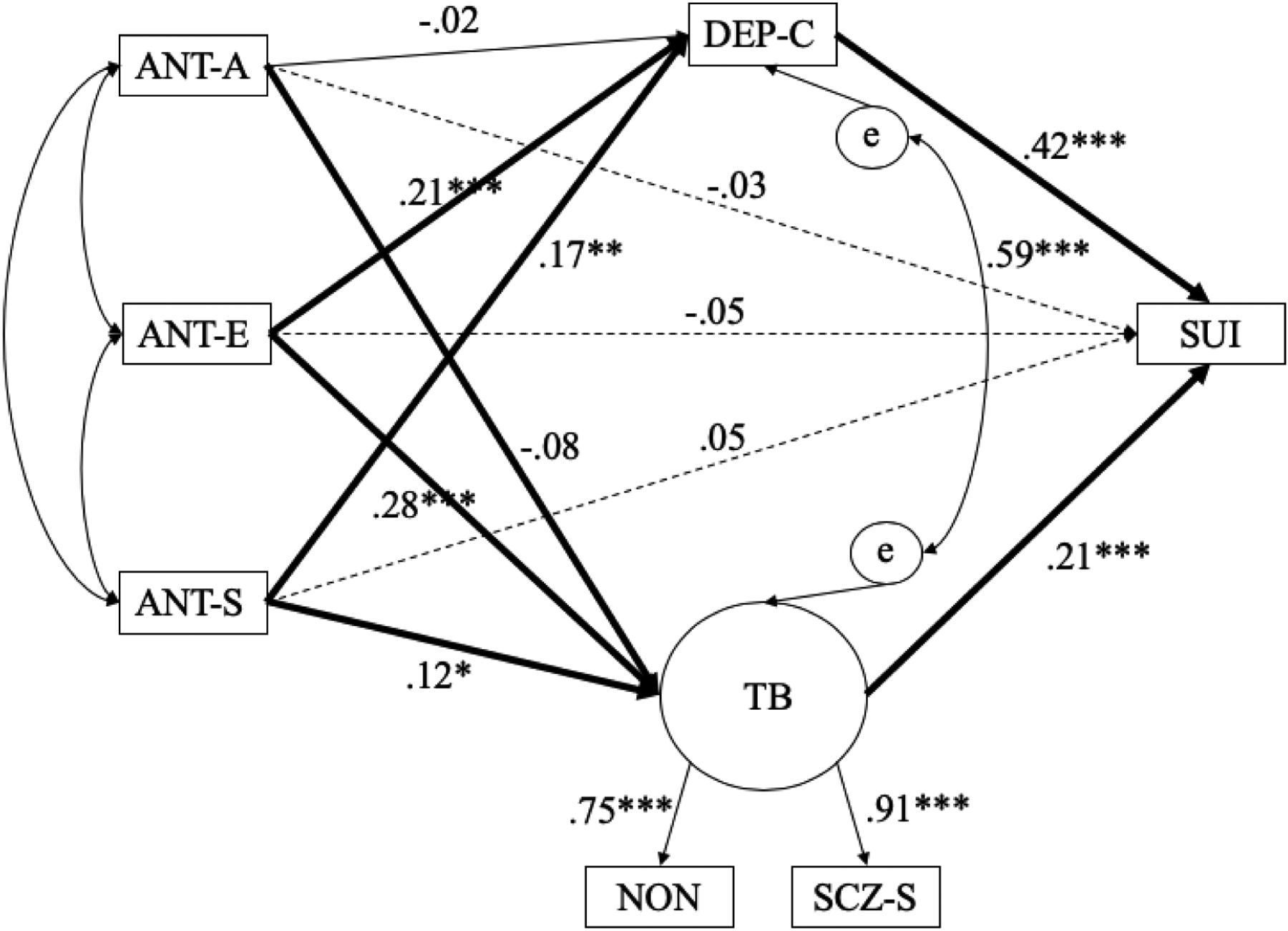
The indirect effects model of the relation between psychopathic traits and suicide ideation through thwarted belonging and perceived burden. Dashed lines indicate non-significant direct effects. Bolded lines indicate significant specific indirect effects pathways (also see Table 3). Model fit indices are presented in Table 2. All coefficients are standardized (STDYX). ANT-A = Antisocial Behaviors Subscale; ANT-E = Egocentricity Subscale; ANT-S = Stimulus-Seeking Subscale; SUI = Suicide Ideation Scale; DEP-C = Depression-Cognitive Subscale (perceived burden proxy), Thwarted belonging (TB) = latent variable with SCZ-S (Social Detachment Scale) and NON (Non-Support Scale) as indicators; All scales are from the Personality Assessment Inventory (PAI).
* p < .05; **p < .01; ***p < .001
Table 2.
Model Fit Indices Comparing the Original Model to the Modified Model
| Model | χ2 | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|
| Original | 280.66 (df = 5, p < .001) | .27 (90% CI = [.24, .29]) | .78 | 0.19 | 0.12 |
| Modified | 25.17 (df = 4, p < .001) | .08 (90% CI = [.05, .11]) | .98 | 0.92 | 0.02 |
Note. Original model = the model where the DEP-C and thwarted belonging residuals were not correlated; Modified model = the model where the DEP-C and Thwarted belonging residuals were correlated; RMSEA = Root mean square error of approximation; CFI = Comparative fit index; TLI = Tucker-Lewis Index; SRMR = Standardized root mean square residual.
Specific and total indirect effects estimates, and bias-corrected 95% CIs are presented in Table 3. Results indicated a significant specific indirect effect of Egocentricity (95% CI = [.05, .12]) and Stimulus Seeking (95% CI = [.04, .11]) on SI through PB. Specifically, Egocentricity (β = .21, p < .001) and Stimulus Seeking (β = .17, p = .001) were significantly positively associated with PB, which, in turn, was significantly positively associated with SI (β = .42, p < .001). Furthermore, Antisocial Behavior (95% CI = [−.04, −.002]), Egocentricity (95% CI = [.03, .10]), and Stimulus Seeking (95% CI = [.01, .05]) were specifically indirectly associated with SI through TB. Antisocial Behavior was not significantly associated with TB (β = −.08, p = .105), but TB was, in turn, associated with SI (β = .21, p < .001); therefore, it is likely that TB is primarily driving the specific indirect effect between Antisocial Behavior and SI through TB. Moreover, Egocentricity (β = .28, p < .001) and Stimulus Seeking (β = .12, p = .026) were significantly positively associated with TB, which, in turn, was significantly positively associated with SI (β = .21, p < .001). Total indirect effects indicated that only Egocentricity (95% CI = [.10, .19]) and Stimulus Seeking (95% CI = [.05, .14]) were indirectly associated with SI through PB and TB in combination. In this model, the PAI psychopathic traits scales predicted 10.9% (p < .001) of the variance in TB and 10.7% (p < .001) of the variance in PB. Additionally, this model explained 32.2% (p < .001) of the variance in SI.
Table 3.
Specific and Total indirect effects of Antisocial Traits on Suicide Ideation through Thwarted Belonging and Perceived Burden (DEP-C).
| Estimate | 95% Bias Corrected CI (Lower, Upper) | |
|---|---|---|
| Specific Indirect Effects of Thwarted Belonging | ||
| ANT-A to SUI | −.02 | −.04, −.002* |
| ANT-E to SUI | .06 | .03, .10* |
| ANT-S to SI | .03 | .01, .05* |
| Specific Indirect Effects of Perceived Burden (DEP-C) | ||
| ANT-A to SUI | −.01 | −.04, .02 |
| ANT-E to SUI | .09 | .05, .12* |
| ANT-S to SI | .07 | .04, .11* |
| Total Indirect Effects | ||
| ANT-A to SUI | −.02 | −.07, .02 |
| ANT-E to SUI | .15 | .10, .19* |
| ANT-S to SI | .09 | .05, .14* |
Note. SUI = Suicide Ideation Scale; DEP-C = Depression-Cognitive Subscale (perceived burden proxy), Thwarted belonging = latent variable with SCZ-S and NON as indicators); SCZ-S = Social Detachment Scale; NON = Non-Support Scale; ANT-A = Antisocial Behaviors Subscale; ANT-E = Egocentricity Subscale; ANT-S = Stimulus-Seeking Subscale; All scales are from the Personality Assessment Inventory (PAI);
CI not containing zero indicate a significant indirect effect.
Discussion
This study aimed to expand existing knowledge by testing potential mechanisms, derived from the ITS, underlying the relation between psychopathic traits and SI. Using data routinely collected at intake from male prisoners– a population for whom suicide is a leading cause of death (Konrad et al., 2007; Rabe, 2012)– we anticipated that TB and PB, and two of the psychopathy facets (Stimulus Seeking and Antisocial Behavior) would be positively correlated with SI, but Egocentricity would be negatively correlated to SI. We also hypothesized that psychopathic traits would be indirectly linked to SI through TB and PB. TB and PB would then, in turn, be positively associated with SI. Our preliminary results, in large part, supported our hypotheses, therefore adding to the growing body of research that implicates disrupted interpersonal functioning in the etiology of SI (Chu et al., 2017).
Consistent with our hypotheses, TB, PB, and Stimulus Seeking were significantly positively correlated with SI; however, Egocentricity was also significantly positively correlated with SI, and Antisocial Behavior was not significantly associated with SI. Also, largely consistent with our hypotheses, the relations between psychopathic traits (Egocentricity and Stimulus Seeking, but not Antisocial Behavior) and SI were significantly indirectly associated through the additive effect of TB and PB, such that greater psychopathic traits were associated with greater TB and PB and subsequently greater SI. This finding adds to the growing research implicating these ITS variables as mediators in the relation between other risk factors and SI (e.g., Buchmann-Schitt et al., 2017; Chu et al., 2016; Jahn et al., 2015). There were also several specific indirect effects, which indicate indirect associations between psychopathic traits and SI through TB and PB, uniquely. Egocentricity and Stimulus Seeking were indirectly associated with SI independently through PB. Antisocial Behavior, Egocentricity, and Stimulus Seeking were indirectly associated with SI independently through TB. However, the indirect effect between Antisocial Behavior and SI through TB were driven by the stronger association between TB and SI. Results, therefore, emphasize the importance of the ITS framework in understanding the pathways from psychopathic traits to SI.
The above results suggest that Antisocial Behavior and Stimulus Seeking facets of psychopathy, which are associated with reckless and impulsive behavior and dysregulated affect, may impact on an individual’s ability to engage in adaptive interpersonal interactions, preventing the development of significant relationships that buffer against the development of SI (Patrick & Drislane, 2015). These Factor 2 traits are associated, for example, with early behavior problems, impulsivity, irresponsibility, law-breaking, and substance abuse—and in connection with these adverse behavior patterns, an exploitative social style, employment problems, and difficulties in interpersonal relations. Consequently, Factor 2 traits may contribute over time to feelings of social disconnectedness and the absence of reciprocal care. Somewhat unexpectedly, since Egocentricity might reasonably be expected to shield an individual from concerns about one’s impact or imposition on others, these traits were found to positively relate to both PB and TB. This finding is difficult to explain and warrants further exploration and replication.
Our results not only bolster support for the ITS in prison populations (Mandracchia & Smith, 2015), but also provide an explanation of why individuals with heightened psychopathic traits, are at increased risk for SI. Specifically, male prisoners who report heightened psychopathic traits may be more likely to perceive themselves to be a burden on others and may also be likely to feel a sense of isolation from others. However, the findings and proportion of variance explained in these relations reveal that there are likely additional indirect mechanisms underlying the associations between psychopathic traits and SI (e.g., boldness/fearlessness; Anestis et al., 2018; Buchman-Schmitt et al., 2017), and therefore future studies should explore other possible mechanisms that may explain this relation.
Improving Treatment for SI in Prison
If further work in samples of male prisoners indicates that the IPT constructs are valid predictors of suicide risk, it will be critical to develop and empirically test the efficacy and effectiveness of interventions designed to target its constructs, particularly within the context of psychopathic traits (Baskin-Sommers et al., 2015; Skeem et al., 2011). Such treatments (e.g., Cognitive Therapy Techniques) may focus on the bolstering of interpersonal functioning to improve interpersonal relationship quality, restructuring maladaptive cognitions that underlie perceptions of isolation and/or burden, and improving engagement in social activities to build meaningful social connections (Beckner et al., 2010; Pratt et al., 2015; Stangier et al., 2011).
Limitations
Our study is limited by a cross-sectional design, which prohibits firm conclusions about causality and directionality of the relations examined. Second, the prison did not provide us with data to fully characterize the inmates psychiatric functioning and history (e.g., current or historical psychiatric diagnosis, hospitalizations, or treatment); therefore, our results are limited by the lack of these potentially relevant variables. Third, although several prior studies have used proxy variables to represent the ITS constructs when the ITS measures were not available (e.g., Joiner et al., 2009; Smith et al., 2012), the use of proxy measures is suboptimal. Consequently, future research should attempt to replicate these findings using other psychometrically-validated scales developed specifically to assess current feelings of PB and TB, as these would be expected to better capture variability in the proposed IPT mediators, resulting in less error and reducing the chance of inconsistent findings. Similarly, although PAI-ANT scales correlate moderately with psychopathic traits in prisoner samples, it is a stronger indicator of Factor 2 features (Edens & Ruiz, 2005). Thus, replication using other psychopathic traits measures is warranted. Relatedly, although we do not believe that demand characteristics played a prominent role in these measures, our assessment tools were vulnerable to dishonesty or lack of understanding; however, this may have been mitigated to removing individuals with invalid PAI profiles. The current study examined SI in a sample of male prisoners, but the findings do not speak to risk for suicidal behaviors and attempts. Given increased rates of suicide attempts, including severe attempts that require medical attention, among male prisoners (Fazel et al., 2017), future research should also examine whether mechanisms theorized by ITS to contribute to risk for suicide attempts (i.e., suicide capability) may account for these known disparities. Our findings also do not speak to SI among female prisoners or SI among other populations with varying levels, and expressions of psychopathic traits (e.g., individuals in clinical, military, or community settings; Debowska et al., 2018; Lee et al., 2010). Although our large sample of male prisoners is considered a study strength, further research is needed to enhance the generalizability of our findings. Use of only a single self-report measure to assess psychopathic traits and ITS constructs also leaves the results subject to potential monomethod bias; thus, relationships may have been artificially inflated. We further treated our participant group as a homogenous set of individuals. It may be the case that there are distinct subgroups of psychopathic traits (Dhingra et al., 2015) that differ in phenotypic expression, external correlates, etiology, and ability to experience PB, TB, and SI. Consequently, replication and extension of our findings is necessary. Finally, all of the conclusions reached above are with respect to a single therapeutic prison where residents have been described as among the most “damaged, disturbed and dangerous” men in the prison system (Shine & Newton, 2000, p. 23). Whether the results of this study apply elsewhere merits further investigation7.
Conclusion
Overall, the current study provides preliminary evidence for the role of thwarted interpersonal needs in the relations between specific psychopathic traits and suicidal thoughts in a high-risk population. Given that our results highlight potential mechanisms by which psychopathic traits and SI may be linked, our findings offer insight into targets for intervention. For healthcare professionals working in prison, therapeutically bolstering feelings of competence and connectedness may help to minimize suicide risk.
Acknowledgments
This work was supported, in part, by a grant from the National Institute of Mental Health (T32 MH020061).
Footnotes
Declarations of interest: none
Greater detail on the relationships between psychopathic traits and negative affect can be found elsewhere (e.g., Garofalo et al., 2019; Kosson et al., 2015).
Category B prisoners do not need to be held in the highest security conditions; however, for category B prisoners, the potential for escape should be made very difficult.
Democratic Therapeutic prisons provide group-based therapy within a social climate that promotes positive relationships, personal responsibility and social participation. Therapeutic Communities address a range of offender needs including interpersonal relationships, emotional regulation, self-management, and psychological wellbeing (see Bennett & Shuker, 2017).
Because the PAI was administered at the prison and only the scale T-scores were recorded, raw and item-level data were not available for analysis. Therefore, Cronbach’s alphas cannot be reported
The following criteria were used to determine invalid profiles: ICN > 73T, INF > 75T, NIM ≥ 92T, PIM > 68T. There were 199 participants who had an invalid profile based on at least one of the validity scales
To further identify sources of model misfit, the analyses were also conducted with the direct effects from the psychopathic traits to SI fixed to zero because these paths were not statistically significant (see Figure 1). Model fit indices when the direct effects were fixed to zero were: goodness of fit χ2 (df = 7) =27.88, p < .001; RMSEA = .06 (90% CI = [.04, .09]); CFI = .98; TLI = .96; SRMR = .02. These fit indices largely concur that the constrained model fit the data well; therefore, model misfit in the model present in Figure 1 was likely largely due to including nonsignificant direct effects in the model. We do not provide further detail on the model with zero-fixed direct effects because this could produce biased path coefficients and overinflate indirect effects (Preacher & Hayes, 2008). To prevent such biases, we retained the final model presented in Figure 1.
Although mean scores on the ANT-A are considerably higher in our sample (M = 75.12, SD = 9.99) than those reported in samples of maximum-security forensic psychiatric patients (M = 62.45, SD =12.21) and incarcerated sex offenders (M = 66.80, SD = 12.03), scores on the other two factors are similar (Edens et al., 2000).
References
- Anestis JC, Anestis MD, & Preston OC (2018). Psychopathic personality traits as a form of dispositional capability for suicide. Psychiatry Research, 262, 193–202. [DOI] [PubMed] [Google Scholar]
- Anestis JC, Anestis MD, Rufino KA, Cramer RJ, Miller H, Khazem LR, & Joiner TE (2016). Understanding the relationship between suicidality and psychopathy: An examination of the interpersonal-psychological theory of suicidal behavior. Archives of Suicide Research, 20(3), 349–368. [DOI] [PubMed] [Google Scholar]
- Baskin-Sommers AR, Curtin JJ, & Newman JP (2015). Altering the cognitive-affective dysfunctions of psychopathic and externalizing offender subtypes with cognitive remediation. Clinical Psychological Science, 3(1), 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett J, & Shuker R (2017). The potential of prison-based democratic therapeutic communities. International Journal of Prisoner Health, 13(1), 19–24. [DOI] [PubMed] [Google Scholar]
- Benning SD, Patrick CJ, Hicks BM, Blonigen DM, & Krueger RF (2003). Factor structure of the psychopathic personality inventory: validity and implications for clinical assessment. Psychological Assessment, 15(3), 340–350. [DOI] [PubMed] [Google Scholar]
- Brinkley CA, Diamond PM, Magaletta PR, & Heigel CP (2008). Cross-validation of Levenson’s Psychopathy Scale in a sample of federal female inmates. Assessment, 15(4), 464–482. [DOI] [PubMed] [Google Scholar]
- Brown SL, Mitchell SM, Roush JF, La Rosa NL, & Cukrowicz KC (2019). Rejection sensitivity and suicide ideation among psychiatric inpatients: An integration of two theoretical models. Psychiatry Research, 272, 54–60. [DOI] [PubMed] [Google Scholar]
- Buchman-Schmitt JM, Brislin SJ, Venables NC, Joiner TE, & Patrick CJ (2017). Trait liabilities and specific promotive processes in psychopathology: The example of suicidal behavior. Journal of Affective Disorders, 216, 100–108. [DOI] [PubMed] [Google Scholar]
- Chu C, Buchman-Schmitt JM, Stanley IH, Hom MA, Tucker RP, Hagan CR, … & Michaels MS (2017). The interpersonal theory of suicide: A systematic review and meta-analysis of a decade of cross-national research. Psychological Bulletin, 143(12), 1313–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleckley HM (1976). The mask of sanity. St Louis: Mosby. [DOI] [PubMed] [Google Scholar]
- Coid J, Yang M, Ullrich S, Roberts A, Moran P, Bebbington P, … & Singleton N (2009). Psychopathy among prisoners in England and Wales. International Journal of Law and Psychiatry, 32(3), 134–141. [DOI] [PubMed] [Google Scholar]
- Cramer RJ, Garza MJ, Henderson CE, Ribeiro JD, Silva C, Smith AR, … & White J (2012). A trait-interpersonal perspective on suicide risk in criminal offenders. Archives of Suicide Research, 16(4), 334–347. [DOI] [PubMed] [Google Scholar]
- Debowska A, Boduszek D, Dhingra K, Sherretts N, Willmott D, & DeLisi M (2018). Can we use Hare’s psychopathy model within forensic and non-forensic populations? An empirical investigation. Deviant Behavior, 39(2), 224–242. [Google Scholar]
- Dhingra K, Persson S, & Swogger MT (2018). Examining the relationship between suicidal behavior and psychopathic traits through the lens of the interpersonal–psychological theory of suicide In Routledge International Handbook of Psychopathy and Crime ( 544–558). Routledge. [Google Scholar]
- Dhingra K, Boduszek D, & Kola-Palmer S (2015). A latent class analysis of psychopathic traits in civil psychiatric patients: The role of criminal behaviour, violence, and gender. The Howard Journal of Criminal Justice, 54(3), 237–249. [Google Scholar]
- Douglas KS, Herbozo S, Poythress NG, Belfrage H, & Edens JF (2006). Psychopathy and suicide: A multisample investigation. Psychological Services, 3(2), 97–116. [Google Scholar]
- Douglas KS, Lilienfeld SO, Skeem JL, Poythress NG, Edens JF, & Patrick CJ (2008). Relation of antisocial and psychopathic traits to suicide-related behavior among offenders. Law and Human Behavior, 32(6), 511–525. [DOI] [PubMed] [Google Scholar]
- Edens JF, & Ruiz MA (2005). Personality assessment inventory interpretive report for correctional settings (PAI-CS) Psychological Assessment Resources, Odessa, FL. [Google Scholar]
- Fazel S, Ramesh T, & Hawton K (2017). Suicide in prisons: an international study of prevalence and contributory factors. The Lancet Psychiatry, 4(12), 946–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo C, Neumann CS, Zeigler-Hill V, & Meloy JR (2019). Spiteful and contemptuous: A new look at the emotional experiences related to psychopathy. Personality Disorders: Theory, Research, and Treatment, 10(2), 173–184. [DOI] [PubMed] [Google Scholar]
- Gunter TD, Chibnall JT, Antoniak SK, Philibert RA, & Hollenbeck N (2011). Predictors of suicidal ideation, suicide attempts, and self-harm without lethal intent in a community corrections sample. Journal of Criminal Justice, 39(3), 238–245. [Google Scholar]
- Hare RD & Neumann CS (2010). The role of antisociality in the psychopathy construct: Comment on Skeem and Cooke (2010). Psychological Assessment. 22, 446–454. [DOI] [PubMed] [Google Scholar]
- Hare RD, Neumann CS, & Mokros A (2018). The PCL-R assessment of psychopathy: Development, properties, debates, and new directions In Patrick CJ (Ed.), Handbook of Psychopathy ( 39–79). New York, NY, US: The Guilford Press. [Google Scholar]
- Harrop TM, Preston OC, Khazem LR, Anestis MD, Junearick R, Green BA, & Anestis JC (2017). Dark traits and suicide: Associations between psychopathy, narcissism, and components of the interpersonal–psychological theory of suicide. Journal of Abnormal Psychology, 126(7), 928–938. [DOI] [PubMed] [Google Scholar]
- Heirigs MH, DeLisi M, Fox B, Dhingra K, & Vaughn MG (2019). Psychopathy and suicidal thoughts and behaviors revisited: Results from a statewide population of institutionalized youth. International Journal of Offender Therapy and Comparative Criminology, 63(6), 874–895. [DOI] [PubMed] [Google Scholar]
- Hemphill JF, Hare RD, & Wong S (1998). Psychopathy and recidivism: A review. Legal and Criminological Psychology, 3(1), 139–170. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: a Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Jahn DR, & Cukrowicz KC (2011). The impact of the nature of relationships on perceived burdensomeness and suicide ideation in a community sample of older adults. Suicide and Life-Threatening Behavior, 41(6), 635–649. [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr, Van Orden KA, Witte TK, Selby EA, Ribeiro JD, Lewis R, & Rudd MD (2009). Main predictions of the interpersonal–psychological theory of suicidal behavior: Empirical tests in two samples of young adults. Journal of Abnormal Psychology, 118(3), 634–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner T (2007). Why people die by suicide. Harvard University Press. [Google Scholar]
- Klonsky ED, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. [Google Scholar]
- Kosson DS, Vitacco MJ, Swogger MT, Steuerwald BL, & Gacono CB (2015). Emotional experiences of the psychopath. The Clinical and Forensic Assessment of Psychopathy: A Practitioner’s Guide. [Google Scholar]
- Konrad N, Daigle MS, Daniel AE, Dear GE, Frottier P, Hayes LM, … & Sarchiapone M (2007). Preventing suicide in prisons, Part I: Recommendations from the International Association for Suicide Prevention Task Force on Suicide in Prisons. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 28(3), 113–121. [DOI] [PubMed] [Google Scholar]
- Lamis DA, & Malone PS (2011). Alcohol-related problems and risk of suicide among college students: The mediating roles of belongingness and burdensomeness. Suicide and Life-Threatening Behavior, 41(5), 543–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Topp L, Indig D, O’driscoll C, & Greenberg D (2012). A cross-sectional survey of prevalence and correlates of suicidal ideation and suicide attempts among prisoners in New South Wales, Australia. BMC public health, 12(1), 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Z, Salekin RT, & Iselin AMR (2010). Psychopathic traits in youth: is there evidence for primary and secondary subtypes?. Journal of Abnormal Child Psychology, 38(3), 381–393. [DOI] [PubMed] [Google Scholar]
- Levenson MR, Kiehl KA, & Fitzpatrick CM (1995). Assessing psychopathic attributes in a noninstitutionalized population. Journal of Personality and SocialPsychology, 68(1), 151–158. [DOI] [PubMed] [Google Scholar]
- Mandracchia JT, & Smith PN (2015). The interpersonal theory of suicide applied to male prisoners. Suicide and Life-Threatening Behavior, 45(3), 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC (1991). Personality assessment screener. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Morey LC (2014). The personality assessment inventory In Personality assessment ( 193–240). Routledge. [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus version 8 user’s guide. Los Angeles: Muthén & Muthén. [Google Scholar]
- O’Connor RC, & Kirtley OJ (2018). The integrated motivational–volitional model of suicidal behaviour. Philosophical Transactions of the Royal Society B: Biological Sciences, 373(1754), 20170268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Bradley MM, & Lang PJ (1993). Emotion in the criminal psychopath: startle reflex modulation. Journal of Abnormal Psychology, 102(1), 82–92. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, & Drislane LE (2015). Triarchic model of psychopathy: Origins, operationalizations, and observed linkages with personality and general psychopathology. Journal of Personality, 83(6), 627–643. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Fowles DC, & Krueger RF (2009). Triarchic conceptualization of psychopathy: Developmental origins of disinhibition, boldness, and meanness. Development and psychopathology, 21(3), 913–938. [DOI] [PubMed] [Google Scholar]
- Patry MW, & Magaletta PR (2015). Measuring suicidality using the Personality Assessment Inventory: A convergent validity study with federal inmates. Assessment, 22(1), 36–45. [DOI] [PubMed] [Google Scholar]
- Pratt D, Tarrier N, Dunn G, Awenat Y, Shaw J, Ulph F, & Gooding P (2015). Cognitive–behavioural suicide prevention for male prisoners: A pilot randomized controlled trial. Psychological Medicine, 45(16), 3441–3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Rabe K (2012). Prison structure, inmate mortality and suicide risk in Europe. International Journal of Law and Psychiatry, 35(3), 222–230. [DOI] [PubMed] [Google Scholar]
- Rasmussen KA, Slish ML, Wingate LRR, Davidson CL, & Grant DMM (2012). Can perceived burdensomeness explain the relationship between suicide and perfectionism?. Suicide and Life-Threatening Behavior, 42(2), 121–128. [DOI] [PubMed] [Google Scholar]
- Roush JF, Mitchell SM, Brown SL, & Cukrowicz KC (2018). Thwarted interpersonal needs mediate the relation between facets of mindfulness and suicide ideation among psychiatric inpatients. Psychiatry Research, 265, 167–173. [DOI] [PubMed] [Google Scholar]
- Sarchiapone M, Carli V, Giannantonio MD, & Roy A (2009). Risk factors for attempting suicide in prisoners. Suicide and Life-Threatening Behavior, 39(3), 343–350. [DOI] [PubMed] [Google Scholar]
- Schmitt WA, & Newman JP (1999). Are all psychopathic individuals low-anxious?. Journal of Abnormal Psychology, 108(2), 353–358. [DOI] [PubMed] [Google Scholar]
- Shine J & Newton M (2000). Damaged, disturbed and dangerous: a profile of receptionsto Grendon therapeutic prison 1995–2000, in Shine J (Ed.), A Compilation of Grendon Research, Leyhill Press, Leyhill, 23–35. [Google Scholar]
- Skeem JL, Polaschek DL, Patrick CJ, & Lilienfeld SO (2011). Psychopathic personality: Bridging the gap between scientific evidence and public policy. Psychological Science in the Public Interest, 12(3), 95–162. [DOI] [PubMed] [Google Scholar]
- Smith PN, Selwyn CN, Wolford-Clevenger C, & Mandracchia JT (2014). Psychopathic personality traits, suicide ideation, and suicide attempts in male prison inmates. Criminal Justice and Behavior, 41(3), 364–379. [Google Scholar]
- Stangier U, Schramm E, Heidenreich T, Berger M, & Clark DM (2011). Cognitive therapy vs interpersonal psychotherapy in social anxiety disorder: a randomized controlled trial. Archives of General Psychiatry, 68(7), 692–700. [DOI] [PubMed] [Google Scholar]
- Swogger MT, Conner KR, Meldrum SC, & Caine ED (2009). Dimensions of psychopathy in relation to suicidal and self-injurious behavior. Journal of Personality Disorders, 23(2), 201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venables NC, Sellbom M, Sourander A, Kendler KS, Joiner TE, Drislane LE, … & Patrick CJ (2015). Separate and interactive contributions of weak inhibitory control and threat sensitivity to prediction of suicide risk. Psychiatry Research, 226(2–3), 461–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venables NC, Yancey JR, Kramer MD, Hicks BM, Krueger RF, Iacono WG, … & Patrick CJ (2018). Psychoneurometric assessment of dispositional liabilities for suicidal behavior: phenotypic and etiological associations. Psychological Medicine, 48(3), 463–472. [DOI] [PubMed] [Google Scholar]
- Verona E, Hicks BM, & Patrick CJ (2005). Psychopathy and suicidality in female offenders: mediating influences of personality and abuse. Journal of Consulting and Clinical Psychology, 73(6), 1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verona E, Patrick CJ, & Joiner TE (2001). Psychopathy, antisocial personality, and suicide risk. Journal of Abnormal Psychology, 110(3), 462–470. [DOI] [PubMed] [Google Scholar]


