Abstract
Objectives:
to estimate the association of social disconnectedness and perceived social isolation with the risk of falls and also investigate whether depression mediated this association.
Method:
Biennial longitudinal survey data from 2006 to 2012 waves of the U.S. Health and Retirement Study of adults aged 65 and older (N = 22,153 observations) were examined. The outcome variable was number of self-reported falls over the observation period. Independent variables included social isolation (social disconnectedness, perceived social isolation) and number of depressive symptoms. Generalized Estimating Equation regressions were performed to address the research questions.
Results:
Regression models indicated that social disconnectedness is associated with a 5% increase in the risk of falls. Perceived social isolation (lack of perceived social support and loneliness combined) was associated with a 33% increase in falls risk. For each increase in the number of depressive symptoms, the risk of falls increased by 13%. Also, the number of depressive symptoms mediated the association between perceived social isolation and risk of falls.
Conclusion:
Our findings were suggestive of the need to consider the different components of social isolation when designing falls prevention programs. More research is needed with research designs that address potential endogeneity bias.
Keywords: Mental health, loneliness, social relationships, population-based study, Health and Retirement Study
Introduction
Falls among older adults represent a significant public health problem, with annual costs estimated to be $34 billion in 2013 (CDC, 2019). Consequences of falls include increased risk for disability, premature nursing-home admission, and mortality (Geusens, Milisen, Dejaeger, & Boonen, 2003; Hartholt, Lee, Burns, & van Beeck, 2019). Social isolation is as harmful for health outcomes and the general well-being of older adults as cigarette smoking and excessive alcohol consumption (Holt-Lunstad & Smith, 2016; Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015); yet, social isolation has only rarely been investigated in terms of its association with falls risk (Trevisan et al., 2019).
Social isolation is a complex, multi-dimensional concept and is defined as having a small social network and a lower likelihood of participating in social activities, as well as a self-perception of social isolation (sometimes referred to as loneliness). In this study, social isolation is defined based on two components: social disconnectedness and perceived social isolation (Cornwell & Waite, 2009). Social disconnectedness is defined as a lack of social interaction with others, such as having a small social network and limited or no participation in social activities. Perceived social isolation refers to a lack of companionship, including feeling lonely, and not feeling supported by others (Cornwell & Waite, 2009).
Scholars argue that the different components of social isolation should be examined separately because these components potentially represent different mechanisms for understanding risk factors for negative health outcomes (Hajek & Konig, 2017). However, previous research is limited and the different components of social isolation were not evaluated as risk factors for falls (Pohl, Cochrane, Schepp, & Woods, 2018). One contribution of this study is the evaluation of the association between two components of social isolation and risk of falls among older adults.
In this study, we used the social convoy model (Antonucci, 2001) as a framework for understanding the association between social isolation, depressive symptoms, and falls risk (Antonucci, 2001). The social convoy consists of social network members who have a relationship with older adults and who are prepared to provide support when needed (Antonucci, 2001). Social disconnectedness reduces the opportunity for older adults to receive support from social convoy members who may help manage falls risks associated with the physical environment and reduces the opportunity to receive support for maintaining medical therapies, also necessary for reducing falls risk. Further, perceived social isolation, including feelings of loneliness and sensing no social support in times of need, results in older adults not seeking out support that might help reduce the risk of falls. In other words, perceived social isolation represents a psychological state increasing the risk of falls. Therefore, we hypothesize that older adults who are socially disconnected and/or who perceive they are socially isolated will be at an increased risk for falling.
One pathway through which social isolation may be associated with falls is depression (or number of depressive symptoms). Previous studies indicated that there is an association between social isolation and depressive symptoms and depression is also associated with increased risk of falls (Kvelde et al., 2015). When older adults are isolated from their social convoy, it may lead to poor emotional support and increase depressive symptoms. Previous studies indicated that depression is associated with an increased risk of falls (Kvelde et al., 2015; Tinetti, Speechley, & Ginter, 1988).
The prevalence of depression among older adults is common; approximately 30% of older adults experience depression at any given time (Steffens et al., 2000). Depression may lead to falls because of various reasons related to biological, social and psychological factors. For instance, older adults fearful of falling reduce their mobility, which reduces conditioning and strength and, thus, increases the risk for falls. We hypothesize that depressive symptoms mediate the association between two components of social isolation (disconnectedness and perceived isolation) and falls.
Understanding whether these two components of social isolation are associated with falls risk along with investigation of the mediating effect of depression for these associations is important because it may help identify appropriate interventions. The research questions for this study include: (1) is there an association between the two components of social isolation and risk of falls? (2) Do depressive symptoms mediate the associations components of social isolation and risk of falls?
Methods
Data source
This study employed panel data from the HRS, a nationally representative, longitudinal survey of Americans (Servais, 2011) aged 65 years and older. The study followed one group of respondents with repeated measurements starting in 2006 and ending in 2012. The two components of social isolation, depressive symptoms, and the covariates were measured in 2006, 2008, and 2010 (RAND, 2014; Servais, 2011), while number of falls were reported in 2008, 2010, and 2012, yielding three two-year stacked sets of observations. The response rates of the HRS ranged from 88%—89% for all waves (HRS, 2017). Respondents who were lost to follow-up, proxy respondents, and those with missing data on any study variable were excluded (15%). Compared to study respondents, excluded respondents were older, disproportionately female, had lower education levels, and reported more chronic health conditions. The final study sample contained 22,153 observations (8464 in 2006, 7468 in 2008, and 6221 in 2010).
Measures
Falls were operationalized by responses to the following question: ‘How many times have you fallen in the last two years?’ (range = 0–50). Different dimensions of social isolation were defined based on the study by Cornwell and Waite (Cornwell & Waite, 2009). Social disconnectedness was determined by summing affirmative responses to the following items: (a) had good friends living nearby, (b) had relatives living nearby, (c) had one or more children living nearby, (d) attended religious services at least once per week, and (e) volunteered for a formal organization in the previous 12 months (range = 0–5). A previous study showed that Cronbach’s alpha for social disconnectedness was .71 (Cornwell & Waite, 2009). We generated a binary variable using the median value of the scale as the cut-off point (median = 3; social disconnectedness binary variable includes “Yes” = 3 or more or “No” = 2 or less).
Perceived social isolation was measured based on responses to two items: having someone who could help them, if needed, and feeling lonely for two weeks or more in the previous 12 months. A three-category perceived isolation variable was created to capture the subjective sense of isolation and included (a) perceived social support and no feeling of loneliness (reference group), (b) lacked perceived social support or felt lonely, and c) lacked perceived social support and felt lonely. A summed index of social isolation consisted of both social disconnectedness and perceived social isolation.
Depressive symptoms were measured with a modified short version of the CES-D index (non-clinical measure), capturing respondents’ emotional feelings and behavior during the past week (Radloff, 1977). This index included five negative mood items: (1) feeling depressed, (2) feeling sad, (3) could not get going, (4) trouble falling asleep, and (5) doing everything was an effort, as well as two positive emotion items: (6) enjoying life and (7) feeling happy. The positive items were reverse coded (range = 0–7). Because we used the loneliness item from the CES-D index to measure loneliness, this item was not included in our index of depressive symptoms. Previous studies showed that Cronbach’s alpha for CES-D index ranged from .80 to .86 (Smith et al., 2013).
Covariates
Socio-demographic covariates included age (range = 65–104), gender (1 = female, 0 = male), and race-ethnic status (1 = non-Hispanic white (reference group), 2 = non-Hispanic black, 3 = non-Hispanic other race groups, and 4 = Hispanic). Education included five groups (1 = no formal education, 2 = 1–12 years, 3 = s some college, 4 = college graduate, and 5 = post-graduate). Alcohol consumption was categorized as moderate to heavy drinker (two or more drinks/day), light drinker (1 drink/day), and non-drinker (reference group) (Lang, Guralnik, Wallace, & Melzer, 2007). Comorbidities were based on respondents’ self-report of eight physician-diagnosed conditions and were measured by a summative index of health conditions, including hypertension, diabetes, cancer, lung disease, heart disease, stroke, psychiatric problems, and arthritis (range = 0–8) (Sangha, Stucki, Liang, Fossel, & Katz, 2003).
Statistical strategy
Descriptive analyses of the sample were conducted first. Next, the association between social isolation or/and depressive symptoms with the number of falls were estimated with Generalized Estimating Equations (GEE) with a negative binomial distribution. The GEE technique took into account the unstructured correlation within each respondent when data were collected from the same respondent at different time points. Model 1 and 2 of the GEE regressions were performed to understand the relationship between each isolation measure with falls; Model 3 included both dimensions of social isolation; Model 4 showed the changes in the association between each dimensions of social isolation and falls when depression was added into Model 3. Mediation analyses were based on the Baron and Kenny method, comparing the direct effect coefficients of the social isolation measures with and without depressive symptoms in the models supporting material Table S1) (Baron & Kenny, 1986). Incidence rate ratios (IRR) and 95% confidence intervals (CI) were presented. All analyses were conducted with SAS (9.4).
Results
Descriptive characteristics of the sample are presented in Table 1. The mean social disconnectedness score was 2.6 (SD = 1.1). The combined perceived social isolation measure indicated that 52.7% of respondents were not isolated with respect to perception of social support if needed, or were not feeling lonely; 41% either reported not having any social support when needed, or reported feeling lonely during the past week; and 5.8% were very isolated socially, reported lacking social support and feeling lonely during the past week. The mean number of depressive symptoms was 1.2 (SD = 1.7).
Table 1.
Characteristics of the study sample (2006: N = 8,464).
| Exposure | Overall |
|
|---|---|---|
| N (%) | Mean (SD) | |
| Social disconnectedness indicators | ||
| Did not live with spouse/partner | 3481 (41.1) | |
| Had no children living within 10 miles | 3280 (42.0.) | |
| Did not have good friends living nearby | 2535 (30.0) | |
| Did not have relatives living nearby | 5974 (70.6) | |
| Did not attend religious services | 1878 (22.2) | |
| Did not volunteer | 5524 (65.3) | |
| Social Disconnectedness Index | 2.6 (1.1) | |
| Perceived social isolation indicators | ||
| Lacked perceived social support, if needed | 2618 (35.6) | |
| Felt lonely for two or more weeks | 1463 (17.3) | |
| Combined perceived social isolation variable | ||
| Perceived social support AND did not feel lonely | 4056 (52.7) | |
| Lacked perceived social support OR felt lonely | 3187 (41.4) | |
| Lacked perceived social support AND felt lonely | 447 (5.8) | |
| Depression scale | ||
| CESD (ranged from 0–7) | 1.2 (1.7) | |
| Covariates | ||
| Age (years) | 74.02 (7.0) | |
| Female | 4970 (58.7) | |
| Race-ethnic status | ||
| Non-Hispanic white | 6605 (78.0) | |
| Non-Hispanic black | 1061 (12.5) | |
| Hispanic | 656 (7.8) | |
| Non-Hispanic other race | 142 (1.7) | |
| Education (years) | 12.18 (3.3) | |
| Number of chronic health conditions | 2.24 (1.4) | |
Source: 2006–2012 Health and Retirement Study.
Depression scale: Center for Epidemiologic Studies Depression Scale (CESD) without feeling loneliness variable (range = 0–7).
SD, standard deviation.
Figure 1 indicates that the average number of falls was 55 per 100 person-years in 2008. Across the different waves, we observed that the number of falls was higher among respondents who perceived a lack of social support and felt lonely, compared to respondents who either perceived a lack of social support or felt lonely. Thus, those respondents with the greatest sense of social isolation reported the most falls in the observation period. The difference in the number of falls corresponding to social disconnectedness score only reached statistical significance in wave 1 (supporting material Figure S1).
Figure 1.
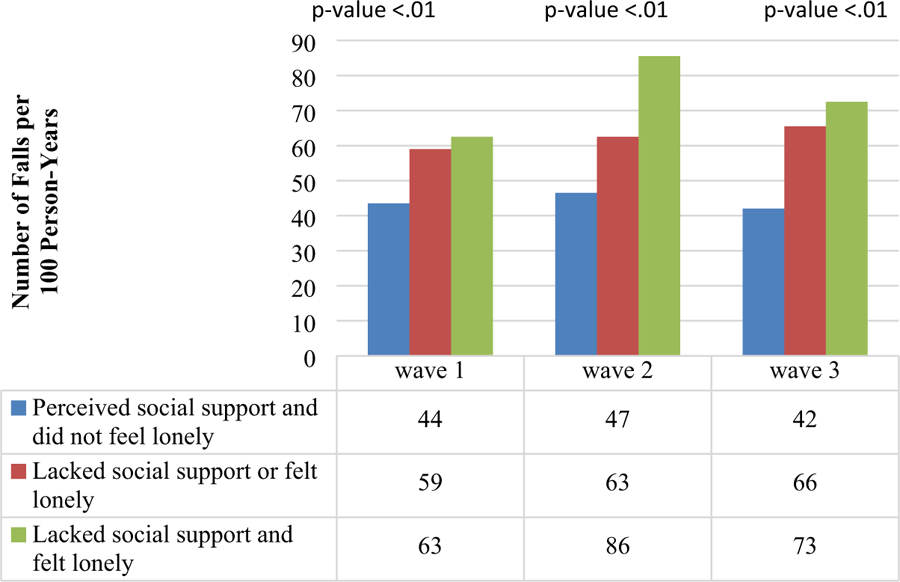
Average rate of falls by perceived social isolation status over three waves.
Table 2 shows the progression of models needed to test the direct effects of social isolation and the effect of the number of depressive symptoms, along with the indirect effect of the number of depressive symptoms, using an approach by Baron and Kenny (1986). Model 1 contains IRR’s for the combined perceived isolation variable showing that compared to respondents who were not isolated, the risk for falls was greater for those who either perceived a lack of social support or felt lonely (IRR = 1.20, 95% CI = 1.11–1.30) and for those who perceived a lack of social support and felt lonely (IRR = 1.34, 95% CI = 1.12–1.60). Model 2 shows that social disconnectedness was related to an increase in falls (IRR = 1.05, 95% CI = 1.01–1.09). Model 3 includes both perceived social isolation and social disconnectedness, where perceived isolation remained related to falls but social disconnectedness was no longer significantly related to falls. Model 4 includes both indicators of social isolation and depressive symptoms. In this final model, both types of social isolation were no longer associated with falls. For each increase in the number of depressive symptoms, the risk of falls increased by 13% (IRR = 1.13, 95% CI = 1.11–1.16). The association between the summed social isolation measure and the risk of falls was not statistically significant after adjusting for the covariates (IRR = 1.03, 95% CI = .99–1.06).
Table 2.
Incidence rate ratios (IRR) for the association between perceived social isolation and social disconnectedness and the rate of falls.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Perceived isolation | ||||
| No perceived isolation | Ref | Ref | Ref | Ref |
| Either no perceived support or felt lonely | 1.21 (1.11–1.31) | 1.20 (1.11–1.30) | 1.08 (1.00–1.17) | |
| Both no perceived support and felt lonely | 1.36 (1.14–1.63) | 1.33 (1.11–1.58) | 1.04 (0.87–1.25) | |
| Social disconnectedness index | 1.05 (1.01–1.09) | 1.03 (0.99–1.07) | 1.02 (0.98–1.06) | |
| CESD scale | 1.13 (1.11–1.16) |
Source: 2006–2012 Health and Retirement Study. Model 1: perceived isolation and the covariates. Model 2: social disconnectedness and the covariates. Model 3: both types of social isolation and the covariates. Model 4: both types of social isolation, depression and the covariates.
IRR, incidence rate ratio; CI, confident interval; depression scale, Center for Epidemiologic Studies Depression Scale (CESD) without feeling loneliness variable (range = 0–7); covariates, age, gender, race, education, alcohol consumption, and co-morbidities.
We engaged in sensitivity analysis to determine if a binary measure of social disconnectedness yielded the same results as the continuous measure. The results for the association between social disconnectedness and falls were similar when comparing both measurement approaches (see supporting material Table S3).
Discussion
The study indicated that perceived social isolation was independently associated with an increased falls risk. When both perceived isolation and social connectedness were in the model, depressive symptoms fully mediated the effects of both social isolation measures. The findings were important, in part, because each dimension of social isolation represented potential modifiable risk factors for falls that may need to be addressed when designing falls prevention programs. This study also contributes to the scientific literature regarding the association between social environment risk factors and falls risk, framed within the social convoy model.
Social disconnectedness and perceived social isolation are related to falls in different ways, demonstrating the importance of identifying and examining both structural and emotional social isolation characteristics. These findings confirm the assertion by Cornwell and Waite that there is likely more than one component responsible for the association between different dimensions of social isolation and falls (Cornwell & Waite, 2009). It is important to note that research showed that the relationship between social isolation and falls risk may be reciprocal (Hajek & Konig, 2017). Since no single-study results may be employed to generate new intervention strategies, more research is needed before a strong case can be made for falls intervention programs to include management of social isolation.
This study also illustrated that the association between depressive symptoms and falls was stable and in the same direction across the observation period. This finding was consistent with previous studies (Byers et al., 2008). Scholars have explained the association between depressive symptoms and falls from different perspectives. First, falls are influenced by psychological mechanisms, such as fear of falls. This results in older adults being more inactive, restricting their mobility, becoming physically weaker, leading to higher falls risk (van Haastregt, Zijlstra, van Rossum, van Eijk, & Kempen, 2008; Vellas, Wayne, Romero, Baumgartner, & Garry, 1997). Second, the association between the number of depressive symptoms and falls is influenced by physical decline and disability (Ariyo et al., 2000; Penninx et al., 1998). Third, the association between depression and falls is influenced by cognitive impairment that affects attention and reduces executive function, reaction time, and gait speed (Hajjar et al., 2009; McDermott & Ebmeier, 2009). Fourth, the association between the number of depressive symptoms and falls is related to medication use. Some prescription medications have side effects that can make older adults light-headed or dizzy and prone to fall. Antidepressants are known to contribute to osteoporosis, which is related to falls and fractures (Joo et al., 2002; Woolcott et al., 2009). Also, not following proper dosage recommendations for some medications is demonstrated to lead to higher risk of falls. Our findings suggested that depressive symptoms were not only directly associated with the risk of falls, but also were a mechanism that may link social isolation and falls risk. We note here that the data employed in this study (HRS) did not contain indicators of clinical depression; instead we relied on a number of depressive symptoms.
It is often assumed that depressive symptoms are a consequence of different types of social isolation (Taylor, Taylor, Nguyen, & Chatters, 2018). On the other hand, depressed older adults were often socially isolated or have limited social relationships. They may not have recognized the risks of falls or did not find ways to change or adapt to their environment. When older adults are isolated, they may not be able to access information and coping strategies that may help them evaluate and prevent their risk of falls. Reducing social environment risk factors for falls through increased social engagement, such as through formal volunteering, attending religious services, or joining clubs and interest or support groups, should be discussed during medical visits and home care services (Quach et al., 2019). Multiple approaches are needed to reduce the different types of social isolation to help depressed older adults avoid the risk of falls.
This study had several limitations. The HRS only recorded the number of falls and did not record information on other falls characteristics (e.g.whether the fall occurred inside or outside of the home). Since the measurement of falls was self-reported, it may not be reliable due to recall bias. Our findings suggest that further investigation is warranted of the relationship between different dimensions of social isolation and falls with a gold standard falls measure, such as a fall calendar or using the fall injury outcome. In addition, the inability to control for time-constant unobserved confounders in GEE models may have biased the results. Future research may benefit from the employment of fixed-effects models that may help address some of these issues. We did not make causal statements about the direction of the relationships given likely omitted variable bias and possible selection effects. It is possible that reverse causality was present, given that persons who have a history of falling may more likely be socially isolated (Hajek & Konig, 2017). More research is needed with designs that can address these issues. Also, panel attrition was a potential limitation since respondents lost to follow-up may bias the association between social isolation and risk of falls. The interpretation of mediation analysis should take into account that both social isolation and the number of depressive symptoms as measured at approximately the same time, so one cannot be certain which one comes first. Future studies should evaluate social isolation and the number of depressive symptoms at different time points, so the design of mediation analysis would be more certain.
Conclusions
The study demonstrates an association between two types of social isolation and falls risk. Specifically, perceived isolation was independently associated with falls risk. The results also contribute to the literature, stating that the relationship between social isolation and falls may be mediated by the number of depressive symptoms. The study drew on a large, national data file, incorporating a longitudinal design that evaluated falls risk using Generalized Estimating Equation (GEE) methods and negative binomial distribution. This approach accounted for the non-normal distribution of number of falls in the population and for the correlated error associated with multiple observations of the same subjects over time. Therefore, this approach reduced some of the bias associated with other modeling strategies. Social convoy theory was useful for understanding how social isolation might be associated to higher falls risk among older adults. Future research should investigate if the quality of social relationships is associated with falls to understand whether depressive symptoms may be one pathway through which social isolation and falls are associated.
Supplementary Material
Acknowledgements
The authors acknowledge the Health and Retirement Study research team and study participants for their time, effort, and dedication.
Funding
The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. This research was supported by the National Institutes of Health #1, under grant P2CHD065702, and the National Institutes on Aging #2, the Boston Claude D. Pepper Older Americans Independence Center, under grant P30-AG031679. The sponsors played no role in the content of this study.
Footnotes
Supplemental data for this article can be accessed online at https://doi.org/10.1080/13607863.2020.1732294
Ethics
This study used the data from the HRS in which personal information of human subjects was de-identified in the publicly available data; therefore, it was exempt by the Institutional Review Board (IRB). The Michigan IRB defines public use data as data disseminated by ICPSR, Roper and the following federal agencies (Census Bureau, NCHS, and NCES).
Disclosure statement
The authors report no conflict of interest.
References
- Antonucci TC (2001). Social relations - An examination of social networks, social support, and sense of control. In Birren JE & Schaie KW (Eds.), Handbook of the psychology of aging. Orlando, FL: Academic Press. [Google Scholar]
- Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, & Furberg CD (2000). Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation, 102(15), 1773–1779. [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Byers AL, Sheeran T, Mlodzianowski AE, Meyers BS, Nassisi P,& Bruce ML (2008). Depression and risk for adverse falls in older home health care patients. Research in Gerontological Nursing, 1(4), 245–251. 10.3928/19404921-20081001-03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2019). Web-based injury statistics query and reporting system. Atlanta, GA: Author. [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50(1), 31–48. 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geusens P, Milisen K, Dejaeger E, & Boonen S (2003). Falls and fractures in postmenopausal women: A review. The Journal of the British Menopause Society, 9(3), 101–106. [DOI] [PubMed] [Google Scholar]
- Hajek A, & Konig HH (2017). The association of falls with loneliness and social exclusion: Evidence from the DEAS German Ageing Survey. BMC Geriatrics, 17(1), 204. 10.1186/s12877-017-0602-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajjar I, Yang F, Sorond F, Jones RN, Milberg W, Cupples LA, & Lipsitz LA (2009). A novel aging phenotype of slow gait, impaired executive function, and depressive symptoms: Relationship to blood pressure and other cardiovascular risks. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 64(9), 994–1001. 10.1093/gerona/glp075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartholt KA, Lee R, Burns ER, & van Beeck EF (2019). Mortality from falls among US adults aged 75 years or older, 2000–2016. JAMA, 321(21), 2131–2133. 10.1001/jama.2019.41852735063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, & Smith TB (2016). Loneliness and social isolation as risk factors for CVD: Implications for evidence-based patient care and scientific inquiry. Heart, 102(13), 987–989. 10.1136/heartjnl-2015-309242heartjnl-2015-309242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/174569161456835210/2/227 [DOI] [PubMed] [Google Scholar]
- HRS. (2017). Sample sizes and response rates. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf.
- Joo JH, Lenze EJ, Mulsant BH, Begley AE, Weber EM, Stack JA, … Pollock BG (2002). Risk factors for falls during treatment of late-life depression. The Journal of Clinical Psychiatry, 63(10), 936–941. [DOI] [PubMed] [Google Scholar]
- Kvelde T, Lord SR, Close JCT, Reppermund S, Kochan NA, Sachdev P, … Delbaere K (2015). Depressive symptoms increase fall risk in older people, independent of antidepressant use, and reduced executive and physical functioning. Archives of Gerontology and Geriatrics, 60(1), 190–195. 10.1016/j.archger.2014.09.003 [DOI] [PubMed] [Google Scholar]
- Lang I, Guralnik J, Wallace RB, & Melzer D (2007). What level of alcohol consumption is hazardous for older people? Functioning and mortality in U.S. and English national cohorts. Journal of the American Geriatrics Society, 55(1), 49–57. 10.1111/j.1532-5415.2006.01007.x [DOI] [PubMed] [Google Scholar]
- McDermott LM, & Ebmeier KP (2009). A meta-analysis of depression severity and cognitive function. Journal of Affective Disorders, 119(1–3), 1–8. 10.1016/j.jad.2009.04.022 [DOI] [PubMed] [Google Scholar]
- Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, & Wallace RB (1998). Depressive symptoms and physical decline in community-dwelling older persons. JAMA, 279(21), 1720–1726. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9624025 [DOI] [PubMed] [Google Scholar]
- Pohl JS, Cochrane BB, Schepp KG, & Woods NF (2018). Falls and social isolation of older adults in the National Health and Aging Trends Study. Research in Gerontological Nursing, 11(2), 61–70. 10.3928/19404921-20180216-02 [DOI] [PubMed] [Google Scholar]
- Quach LT, Ward RE, Pedersen MM, Leveille SG, Grande L, Gagnon DR, & Bean JF (2019). The association between social engagement, mild cognitive impairment, and falls among older primary care patients. Archives of Physical Medicine and Rehabilitation, 100(8), 1499–1505. 10.1016/j.apmr.2019.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- RAND. (2014). RAND HRS family data documentation, version C. Retrieved from http://hrsonline.isr.umich.edu/modules/meta/rand/randfamilyc/randfamC.pdf.
- Sangha O, Stucki G, Liang MH, Fossel AH, & Katz JN (2003). The Self-Administered Comorbidity Questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis & Rheumatism, 49(2), 156–163. 10.1002/art.10993 [DOI] [PubMed] [Google Scholar]
- Servais M (2011). Overview of HRS public data files for cross-sectional and longitudinal analysis. Survey Research Center Institute for Social Research University of Michigan, Ann Arbor.https://hrs.isr.umich.edu/sites/default/files/biblio/OverviewofHRSPublicData.pdf [Google Scholar]
- Smith J, Fisher G, Ryan L, Clarke P, House J, & Weir D (2013). Psychosocial and lifestyle questionnaire 2006–2010.
- Steffens DC, Skoog I, Norton MC, Hart AD, Tschanz JT, Plassman BL, … Breitner JC (2000). Prevalence of Depression and Its Treatment in an Elderly Population: The Cache County Study. Archives of General Psychiatry, 57(6), 601–607. 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- Taylor HO, Taylor RJ, Nguyen AW, & Chatters L (2018). Social isolation, depression, and psychological distress among older adults. Journal of Aging and Health, 30(2), 229–246. 10.1177/0898264316673511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, & Ginter SF (1988). Risk factors for falls among elderly persons living in the community. The New England Journal of Medicine, 319(26), 1701–1707. 10.1056/NEJM198812293192604 [DOI] [PubMed] [Google Scholar]
- Trevisan C, Rizzuto D, Maggi S, Sergi G, Wang HX, Fratiglioni L, & Welmer AK (2019). Impact of social network on the risk and consequences of injurious falls in older adults. Journal of the American Geriatrics Society, 67(9), 1851–1858. 10.1111/jgs.16018 [DOI] [PubMed] [Google Scholar]
- van Haastregt JC, Zijlstra GA, van Rossum E, van Eijk JT, & Kempen GI (2008). Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. The American Journal of Geriatric Psychiatry, 16(3), 186–193. 10.1097/JGP.0b013e3181591c1e [DOI] [PubMed] [Google Scholar]
- Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, & Garry PJ (1997). Fear of falling and restriction of mobility in elderly fallers. Age and Ageing, 26(3), 189–193. [DOI] [PubMed] [Google Scholar]
- Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, & Marra CA (2009). Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Archives of Internal Medicine, 169(21), 1952–1960. 10.1001/archinternmed.2009.357 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


