Abstract
Peritoneal dialysis (PD), a home-based treatment for kidney failure, is associated with similar mortality, higher quality-of-life and lower costs compared to hemodialysis. Yet <10% of patients receive PD. Access to this alternative treatment, vis-à-vis providers’ supply of PD services, may be an important factor but has been sparsely studied in the current era of national payment reform for dialysis care. We describe temporal and regional variation in PD supply among Medicare-certified dialysis facilities in 2006–2013. The average proportion of facilities offering PD per hospital referral region (HRR) increased from 40% (2006) to 43% (2013). PD supply was highest in HRRs with higher percentage of facilities in urban areas (p=0.004), prevalence of PD use (p<0.0001), percentage of white ESRD patients (p=0.02), and per capita income (p=0.02). Disparities in PD access persist in rural, non-white, and low-income regions. Policy efforts to further increase regional PD supply should focus on these underserved communities.
Keywords: end-stage renal disease, peritoneal dialysis, access to care, hospital referral regions
INTRODUCTION
Over 500,000 Americans per year receive chronic dialysis for end-stage renal disease (ESRD) at considerable expense to the American healthcare system. Medicare is the primary payer of health services for ESRD patients, who make up <1% of the Medicare population but consume 7% of Medicare expenditures (US Renal Data System 2018). ESRD patients generally receive dialysis through one of two modalities: in-center hemodialysis (HD) or home-based peritoneal dialysis (PD), introduced as an alternative treatment modality over a decade after HD. Prior research has shown PD to be a clinically equivalent and less costly modality compared to HD, since patients on PD are trained to administer their dialysis treatments independently, outside of the dialysis clinic setting (Khawar, Kalantar-Zadeh, Lo, Johnson, and Mehrotra 2007; Wong et al. 2018; Mehrotra et al. 2011). While HD is typically performed by clinical staff in dialysis facilities three times per week, PD patients are trained to self-administer treatment several times daily and only have to visit their dialysis facilities monthly for maintenance.
PD offers several advantages to patients, payers, and providers. When patients are informed of their treatment options, they typically prefer PD, as it is associated with increased patient-reported independence, quality-of-life and satisfaction (Tong et al. 2013; Queeley and Campbell 2018; Stack 2002). Despite debates about the relative merits of HD and PD (Venkataraman and Nolph 1999), nephrologists report that PD is an appropriate therapy for roughly half of their patients (Mendelssohn, Mullaney, Jung, Blake, and Mehta 2001). The only absolute contraindication to initiating PD is a lack of a functional peritoneal membrane. For dialysis facilities, PD operating costs are lower relative to HD (De Vecchi, Dratwa, and Wiedemann 1999). For payers, PD is less costly: Medicare spent on average nearly $15,000 less per patient on PD compared to HD in 2016 (USRDS 2018).
Despite evidence of the benefits of PD, as well as patient and provider preferences, an overwhelming majority of US patients receive HD (90%), compared to PD (10%). This is in stark contrast to other North American, Asian, and European countries, where 20–70% of ESRD patients receive PD (USRDS 2018) (US Renal Data System 2017) (US Renal Data System 2017). Much of the literature examining the limited use of PD suggests that healthcare delivery system factors, rather than purely medical factors, drive PD’s limited uptake by patients (Blake and Finkelstein 2001; Golper et al. 2011; Mehrotra et al. 2007; Mehrotra et al. 2009). The limited availability of PD services at dialysis facilities likely plays a significant and under-appreciated role in influencing patients’ access to and choice of treatment (Wang et al. 2017).
Recent evidence has shown that PD supply at dialysis facilities has increased over the last decade, due in part to health reforms implemented during this period. Historically, Medicare reimbursed facilities for dialysis care in two parts: 1) a prospective payment for dialysis treatment regardless of modality, and 2) a separate, fee-for-service payment for drugs, laboratory tests and supplies. Over time, the separately billable items, which included injectable agents such as epoetin, comprised 40% of dialysis-associated costs (Hirth et al. 2013). These separately billable services were administered more frequently during HD, so operating margins significantly favored HD over PD (Hornberger and Hirth 2012; Hirth 2007; Hirth et al. 2013). In 2011, Medicare implemented a bundled payment for dialysis care, consolidating the prior 2-component payment into a single prospective payment (Centers for Medicare & Medicaid Services 2018). Coupled with changes to Food and Drug Administration labeling requirements for erythropoietin-stimulating agents, these reforms have decreased operating margins for HD and increased operating margins for and interest in PD services (Hornberger and Hirth 2012). Recent analysis conducted at the facility-level found a modest increase in dialysis facility PD service availability, from 36% of US facilities in 2006 to 42% in 2013 (Wang et al. 2017). But it is unclear whether increases in PD supply have been uniform across the country, because PD supply has wide regional variability. In this study, we describe trends in regional PD supply in the US between 2006 and 2013. Our findings may shed light on current era trends in PD supply and inform policies that address disparities in access to PD despite recent reforms.
NEW CONTRIBUTION
A number of studies have evaluated geographic variation in provision of non-dialysis care, but few have examined this in the context of dialysis care provision (Hao et al. 2015; Thomas et al. 2013; Wang et al. 2010). Recent facility- and patient-level analyses of PD found modest growth in PD service availability (Wang et al. 2018) and patient utilization (Lin et al. 2017; Turenne et al. 2018; Sloan et al. 2019) over the last 15 years. However, this growth is not likely geographically homogeneous.
In this study, we assess temporal and geographic trends in PD supply between 2006 and 2013, in the context of new federal efforts to improve kidney health (Centers for Medicare & Medicaid Services 2019; US Department of Health and Human Services 2019). Specifically, one goal of the Advancing American Kidney Health Initiative is to increase home dialysis utilization to 80% by the year 2025. Understanding geographic variation and time trends in PD supply is important, because sufficient PD supply is needed to ensure adequate access to this alternative treatment modality: patients cannot consider PD if the service is not available in their area. As federal and state policymakers consider further reforms to dialysis payment and other policies aimed at increasing patient access to PD services, it will be important for them to understand geographic variations in PD availability and what populations are most affected. Understanding the regional granularity in PD supply can help focus our attention on the regions and population groups that future national and local policies could target. Our findings will provide a useful foundation of contemporary trends for continued monitoring.
CONCEPTUAL FRAMEWORK
Our analysis was guided by the concept of supply-sensitive care, which posits that the utilization of certain health services depends greatly on the availability of those services (Bhattacharya, Hyde, and Tu 2014). Hospitals with higher bed densities, for example, tend to have higher hospitalization rates than hospitals with lower bed densities (Macinko et al. 2011; Wennberg and Cooper 1999), even when illness severity is similar. For patients with ESRD, PD access and utilization are likely driven by not only patient characteristics, but also supply-side factors. These include dialysis facility factors, characteristics of the regions they are located in, and changes in Medicare reimbursement over time.
Although reimbursement levels for PD and HD treatments have historically been similar, HD involves additional billable services that have tipped revenues and margins toward HD, thus discouraging PD use prior to Medicare payment reform (Hirth et al. 2013; Wang et al. 2010). The federal reforms implemented during our study period substantially increased the operating margins associated with PD from roughly -$185 to $201 per patient-month (compared with $76 to $86 per patient-month for HD) (Hirth et al. 2013; Hornberger and Hirth 2012). While this change may have increased facilities’ interest in offering PD services, facilities planning to establish new PD programs or switch from offering only HD to offering only PD face many supply-side administrative and logistical barriers. These barriers include the costs of buying PD equipment and getting rid of HD machines and chairs, training nurses and technicians to educate patients on PD administration, and setting up relationships with PD dialysate suppliers. Dialysis facilities might also be reluctant to take on the risk of establishing an entirely new patient base, especially since the proportion of patients on PD is currently so much lower than the proportion of patients on HD. If one or two PD facilities already exist in a given HRR, additional dialysis facilities may be even less likely to begin offering PD. Here, we posit that facilities expanded supply of PD in regions whose market conditions were expected to enable profit maximization via high demand, revenue, and market share. We expected greater PD supply in regions with a high density of ESRD patients with characteristics most common to PD patients (i.e. white, younger, employed) (Lin et al. 2017; Stack 2002), a high density of health care providers that could act as a consistent source of patient referrals (Wang, Lee, Patel, Maciejewski, and Ricketts 2011), and competitive regional markets. The presence of a PD program signals enhanced competency in dialysis care and diversifies a facility’s service mix, which may protect organizations from system shocks (e.g., payment reform) in the long-term.
METHODS
Study design, population, and data
We conducted a longitudinal retrospective study of US dialysis facilities at the regional level between 2006 and 2013. We defined PD markets as hospital referral regions (HRR). HRRs approximate the geographic extent of health care markets for tertiary care (Dartmouth Atlas of Health Care Working Group 2003) and reflect PD service areas because PD patients often travel outside county boundaries for monthly PD maintenance visits (Wang, Lee, Patel, Maciejewski, and Ricketts 2011). All data were aggregated to HRRs for each year of the study period.
The primary source of data came from the US Renal Data System (USRDS) (US Renal Data System 2016). We compiled yearly region-level data on non-federal dialysis facilities operating in the US between 2006 and 2013. Facilities were excluded if they were federally operated (e.g., Veterans Affairs), exclusively provided transplant services, did not report ever having served dialysis patients, or did not have valid zip codes in 2006–2013 (Supplemental Digital Content 1). Region-level dialysis facility characteristics were drawn from the Center for Medicare and Medicaid Services (CMS) Annual Facility Survey (CMS-2744, USRDS FACILITY file) and supplemented with the Medicare Provider of Service file (Centers for Medicare & Medicaid Services 2015), to account for facilities that opened or closed during the study period or changed facility ownership (Wang et al. 2018).
Region-level characteristics of ESRD prevalent patients were ascertained from the Medical Evidence Report (CMS-2728, various USRDS files), which providers are required to complete for all patients initiating, reentering, or changing ESRD services. We tracked changes in patient residence over time (e.g., zip code, USRDS RESIDENC file), to assign patients to HRRs each year. General region-level demographic characteristics were drawn from the Area Health Resource File. County-level demographic statistics were converted to the zip code-level using land-area weighting, and then aggregated to HRRs. Healthcare provider census data were obtained from the American Hospital Association’s Annual Hospital Survey.
Measurements
Our primary objective was to describe trends in regional supply of PD services, defined as the annual percentage of dialysis facilities in each HRR that offered PD services (either continuous ambulatory PD or continuous cyclic PD) in a particular year. There are no observable capacity parameters for home-based PD, in contrast to HD, for which it is possible to measure the number of HD stations. The proportion of facilities offering PD therapy is the most suitable method for representing utilization, while accounting for regional and market differences.
Explanatory variables included indicators of market conditions that maximize patient demand, revenue and market share conducive to PD service availability. Facility, patient and market characteristics were aggregated by HRR-year to create regional, time-varying explanatory covariates. Dialysis facility attributes, aggregated to reflect regional composition of providers, included proportions of facilities that were for-profit owned; freestanding vs hospital-based; affiliated with a chain vs independently-owned; and located in an urban vs non-urban area. Dialysis market competition was calculated using the Herfindahl-Hirschman Index (Folland, Goodman, and Stano 2001), which is equal to the sum of the square of each dialysis facility’s market share. Market share was based on the number of dialysis patients unique to each dialysis facility, regardless of chain affiliation. Index values range from 0 to 100, where a value of 0 reflects unconcentrated, competitive markets and values approaching 100 characterize concentrated, monopolistic markets.
Regional ESRD patient composition descriptors included ESRD incidence (number of new ESRD patients per 10,000 general population) and prevalence of PD use (number of patients on PD per 1,000 ESRD patient population) per HRR per year. Pre-existing prevalence of PD use reflects demand for PD and is likely associated with future PD availability and PD use: facilities may be more likely to offer PD in regions with higher pre-existing PD use. We also included measures of regional ESRD patient composition, to assess for characteristics commonly found among patients on PD that could be policy-relevant markers of health disparities: the percentage of ESRD patients in HRRs who were non-elderly (<65 years old) or employed (full or part-time) at dialysis initiation, and the percentage of patients who were non-Hispanic white (Lin et al. 2017; Stack 2002; Wang et al. 2010). Our analysis also evaluated other HRR-level predictors, including per capita income and regional hospital density (number of hospital beds per 100,000 general population). Facility, patient and market characteristics were averaged by year to create regional level time-varying covariates. We also included a pre-post indicator of the prior composite payment system (2006–2010) and the new inclusive ESRD PPS (2011–2013), because this was the most far-reaching dialysis-related reform implemented during our study period. All explanatory variables were lagged by one year because associations were unlikely to be instantaneous.
Analysis
Choropleth maps were generated to illustrate changes in the regional distribution of PD supply at the HRR level between 2006 and 2013 (Cromley and McLafferty 2002). We fit a linear mixed effects model with a random intercept to account for repeated HRR-level observations and to identify factors associated with regional PD provision (Verbeke and Molenbergh 2000). Continuous time-varying covariates contributed both cross-sectional and longitudinal sources of variation in our HRR-level PD outcomes and were decomposed into between-HRR and within-HRR components, respectively, for inclusion in the models (Fitzmaurice and al. 2011). The final model included an indicator for the PPS effect and linear terms for all between-HRR and within-HRR covariates defined above. Since prevalence of PD use may be strongly associated with PD supply, we performed a sensitivity analysis in which PD prevalence was excluded from analysis. Results were unchanged.
This study was approved by the Institutional Review Board of Duke University.
RESULTS
Regional characteristics
A total of 6,435 unique dialysis facilities operated at any point between 2006 and 2013. In 2006, there was an average of 16 facilities per HRR, ranging from as few as 1 to as many as 129 facilities per HRR. In 2013, there was an average of 20 facilities per HRR, ranging from as few as 1 to as many as 177 facilities per HRR (Supplemental Digital Content 1).
Observed PD supply in 2006 was generally higher in the Northeast, West, and areas with large metropolitan cities (Figure 1A), but there was considerable variation between regions. For example, in 2006, 20% of facilities offered PD in the region surrounding Rapid City, South Dakota, compared to 67% of facilities in the region surrounding Lynchburg, Virginia, both predominantly rural regions. In urban HRRs, 38% of facilities in the San Francisco, California area offered PD, compared to 87% of facilities in the Hartford, Connecticut area. In HRRs with 0–55% urban zip codes, an average of 34.3% of facilities offered PD, compared to 40.6% of facilities in HRRs with 56–85% urban zip codes, and 45.8% of facilities in HRRs with 86–100% urban zip codes (Figure 2).
Figure 1. Regional patterns of PD Provision in US Dialysis Facilities, 2006–2013.
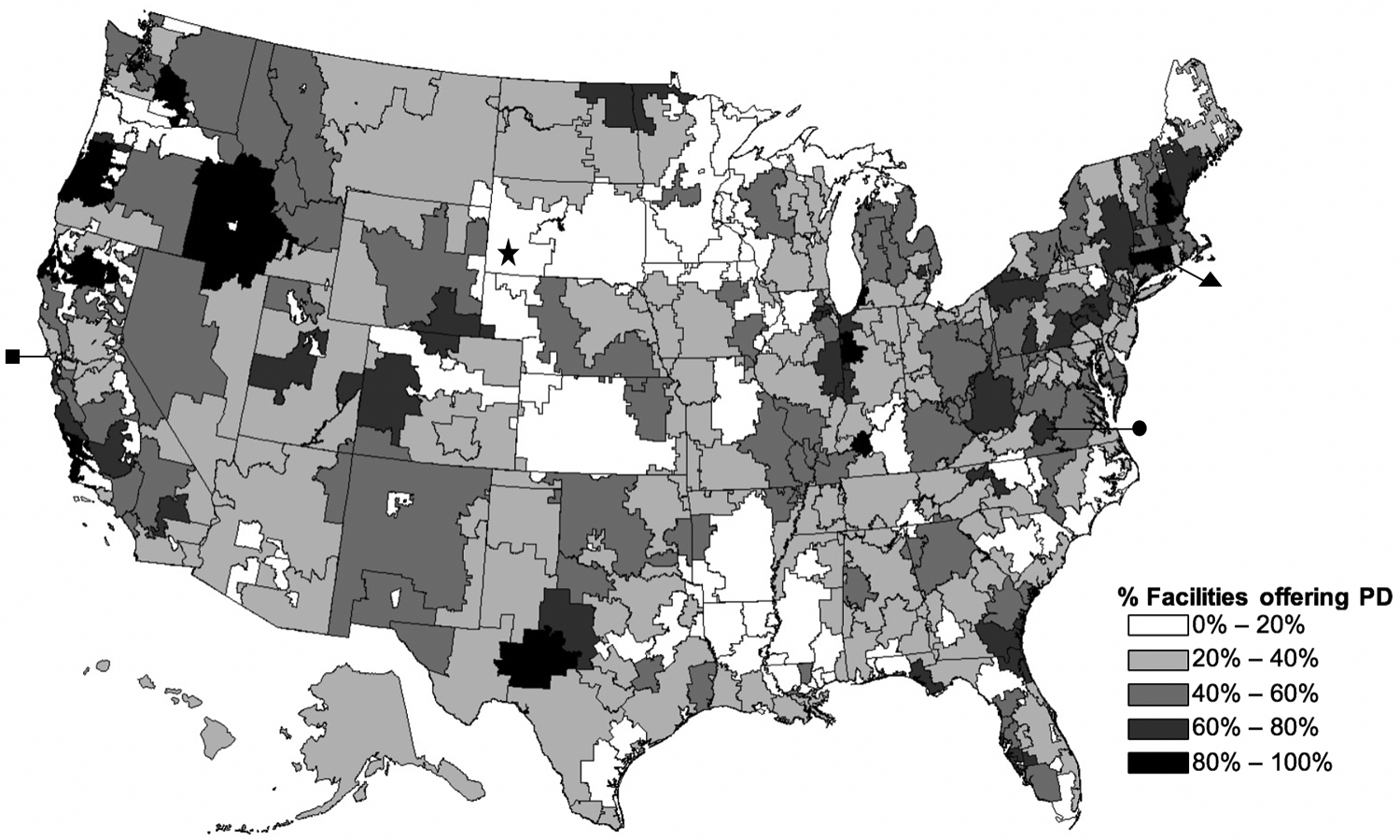
A. Proportion of facilities offering peritoneal dialysis in each hospital referral region in 2006.
Star: Rapid City, South Dakota HRR
Circle: Lynchburg, Virginia HRR
Square: San Francisco, California HRR
Triangle: Hartford, Connecticut HRR
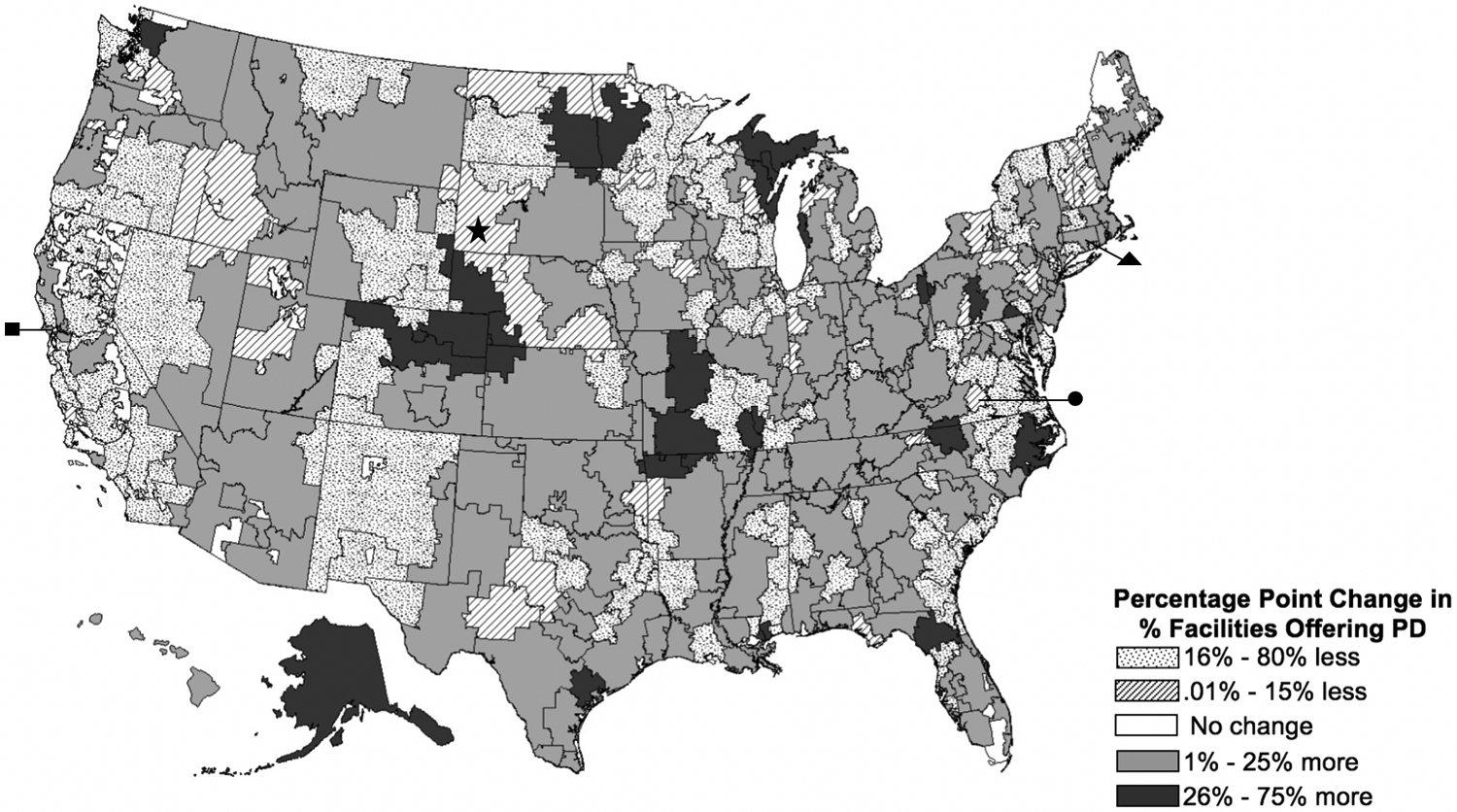
B. Change in proportion of facilities offering peritoneal dialysis in each hospital referral region between 2006 and 2013.
Star: Rapid City, South Dakota HRR
Circle: Lynchburg, Virginia HRR
Square: San Francisco, California HRR
Triangle: Hartford, Connecticut HRR
Figure 2. The percentage of facilities offering PD in predominantly rural regions increased, but did not catch up to levels in predominantly urban regions.
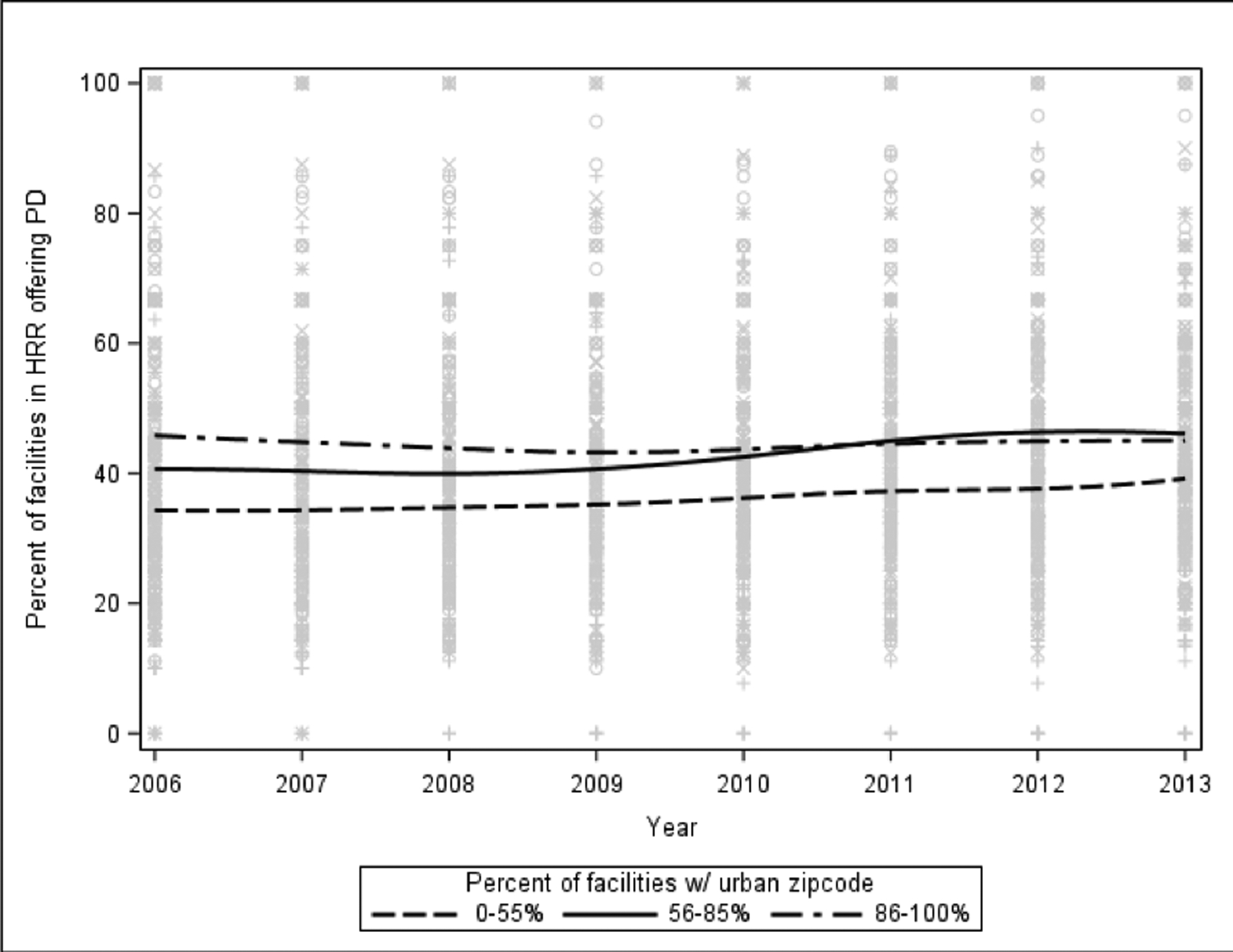
This figure represents the penalized B-spline trajectories of regional PD supply, stratified by urban zip code category. Each category contains roughly the same number of HRRs: 103–108 HRRs had 0–55% urban zip codes, 97–103 HRRs had 56–85% urban zip codes, and 99–105 HRRs had 86–100% urban zip codes. The number of HRRs in each group varied slightly by year, as some zip codes that were initially rural came to be defined as urban, and vice versa.
PD supply remained stable until 2010, when there was a gradual increase in the proportion of dialysis facilities offering PD services (Supplemental Digital Content 2). The proportion of facilities in each HRR that offered PD increased by an average of 3.2 percentage points, from 40.2% of facilities per HRR in 2006 to 43.4% in 2013 (Table 1). But this growth varied by HRR. Regionally, PD supply increased in 57% of HRRs, decreased in 34% of HRRs, and remained the same in only 9% of HRRs. PD supply increases can be attributed to both new facilities offering PD and pre-existing facilities adding PD services (Wang et al. 2018).
Table 1.
Descriptive characteristics of ESRD facility and patient composition in hospital referral regions, in 2006 and 2013
| N=306 hospital referral regions | 2006 Mean (SD) |
2013 Mean (SD) |
|---|---|---|
| Facilities offering PD, % | 40.2 (20.4) | 43.4 (18.4) |
| Dialysis facility composition | ||
| % For profit-owned | 74.9 (28.5) | 81.9 (23.6) |
| % Freestanding | 83.8 (23.7) | 89.3 (19.5) |
| % Chain affiliation | 80.4 (21.3) | 86.0 (20.4) |
| % in urban zip codes | 67.6 (28.4) | 67.9 (28.4) |
| Dialysis market competition, HHI | 20.5 (18.3) | 15.7 (14.0) |
| ESRD-patient composition | ||
| ESRD incidencea | 3.5 (1.4) | 3.4 (1.4) |
| PD prevalenceb | 83.6 (37.3) | 91.1 (35.6) |
| % White and non-Hispanic | 61.2 (22.8) | 59.3 (22.7) |
| % Age <65 years | 58.0 (5.6) | 57.1 (5.0) |
| % Employed | 16.4 (4.3) | 18.5 (4.6) |
| General market composition | ||
| Hospital densityc | 316.9 (123.1) | 293.6 (106.1) |
| Per capita income, $ | 33,886 (7,836) | 42,277 (8,647) |
SD: standard deviation; ESRD: end-stage renal disease; PD: peritoneal dialysis; HHI: Herfindahl-Hirschman Index of dialysis market competition.
ESRD incidence is defined as the number of ESRD patients, per 10,000 general population in HRR, per year.
PD prevalence is defined as the number of PD patients, per 1000 ESRD population in HRR, per year.
Hospital density is defined as the number of community hospital beds per 100,000 HRR general population
By 2013, PD supply had grown in the South, Midwest, and West, but again, trends varied widely between HRRs (Figure 1B). For example, the proportion of facilities offering PD decreased by 20 percentage points (20% to 0%) in Rapid City and by 27 percentage points (67% to 40%) in Lynchburg. Urban areas also exhibited variability: the proportion of facilities offering PD increased by 12.5 percentage points (37.5% to 50%) in San Francisco and by 3 percentage points (87% to 90%) in Hartford. In HRRs with 0–55% urban zip codes, the average percentage of facilities offering PD increased by 4.9 percentage points, to 39.3%. PD supply increased by 5.5 percentage points to 46.1% in HRRs with 56–85% urban zip codes, and decreased by 0.7 percentage points to 45.1% in HRRs with 86–100% urban zip codes (Figure 2). It is important to keep in mind that the proportional effects of small absolute changes in PD supply in HRRs with few dialysis facilities are greater than similar absolute changes in regions with large numbers of dialysis facilities. For example, if the number of facilities offering PD increased from 3 to 6 in a predominantly rural region with only 12 facilities, we would measure PD supply to have increased by 25 percentage points, from 25% to 50%, even though the absolute increase in PD supply was small. In contrast, if the number of facilities offering PD increased by 3 facilities, from 97 to 100, in a predominantly urban region with 200 facilities, we would measure PD supply to have increased by 1.5 percentage points, from 48.5% to 50%.
The rise in PD supply between 2006 and 2013 coincided with a 7.0% absolute increase in for-profit ownership, a 5.6% increase in chain affiliation, and a 5.5% increase in freestanding dialysis clinics (Table 1). Unadjusted annual trends in PD supply did not appear to align with White race and higher employment rates - characteristics previously found to favor PD use in patients with ESRD (Supplemental Digital Content 2) (Miskulin et al. 2002; Stack 2002).
Adjusted results
Over the study period, greater PD supply was associated with regions with greater representation of facilities not affiliated with chains in a region (p=0.01), higher proportions of urban zip codes in a region (p=0.004), less competitive dialysis markets (p=0.001), greater regional prevalence of PD use (p<0.0001), higher proportions of White ESRD patients (p=0.02), and higher per capita income (p=0.02). All covariates were lagged by one year. After adjustment for all covariates, we found an overall increase of 3.2% (95% CI 1.8–4.5; p<0.001) in regional PD supply after implementation of the PPS compared to the pre-PPS period (Table 2). A sensitivity analysis in which PD prevalence was excluded from analysis yielded similar results.
Table 2.
Between-region trends in peritoneal dialysis supply, adjusted for all covariates, 2006–2013
| β | 95% CI | p-value | |
|---|---|---|---|
| Dialysis facility composition | |||
| For profit-owned | 0.03 | −0.07 – 0.13 | 0.52 |
| Freestanding | 0.11 | −0.03 – 0.26 | 0.13 |
| Chain affiliation | −0.17 | −0.30 – −0.04 | 0.01 |
| Urban | 0.12 | 0.04 – 0.20 | 0.004 |
| Dialysis market competition, HHI | 0.20 | 0.09 – 0.32 | 0.001 |
| ESRD-patient composition | |||
| ESRD Incidenceb | 0.99 | −1.12 – 3.11 | 0.36 |
| PD Prevalencec | 0.16 | 0.10 – 0.21 | <0.0001 |
| White and non-Hispanic | 0.15 | 0.02–0.27 | 0.02 |
| Age <65 years | −0.13 | −0.59 – 0.34 | 0.58 |
| Employed | −0.27 | −0.83 – 0.29 | 0.34 |
| General market composition | |||
| Hospital Densityd | −0.02 | −0.04 – 0.00 | 0.06 |
| Per capita income | 0.37 | 0.05 – 0.68 | 0.02 |
| Post-PPS (2011–2013)a | 3.15 | 1.82–4.47 | <0.0001 |
95% CI: 95% confidence interval; ESRD: end-stage renal disease; PD: peritoneal dialysis; HHI: Herfindahl-Hirschman Index of dialysis market competition; PPS: Medicare’s ESRD prospective payment system.
In adjusted analysis, hospital referral region (HRR) covariates lag 1 year from outcome.
ESRD incidence is defined as number of ESRD patients, per 10,000 in HRR general population per year.
PD prevalence is defined as number of PD patients, per 1000 ESRD population in HRR per year.
Hospital density is defined as number of community hospital beds per 100,000 HRR general population.
Within-region effects on PD supply are reported in Supplemental Digital Content 3.
DISCUSSION
This study describes trends in regional PD supply in the US between 2006 and 2013. Overall, we found that PD supply increased modestly across HRRs, from 40.2% in 2006 to 43.4% in 2013 and that growth in PD supply varied considerably by region. This trend represents a reversal of the long decline that occurred in the era before recent federal policy changes (Wang et al. 2010; Wang et al. 2018). Our findings also indicate that the gap in access between rural and urban regions may be narrowing: communities that had lower PD supply in the early years of our study period (concentrated in rural areas) saw a larger increase in PD services than comparatively high PD supply regions. The unadjusted PD supply increased considerably in the HRRs with the fewest large cities, especially in the South, Midwest and West. This is an encouraging signal of improved access to PD. Patients on PD are more likely to be willing to travel farther to get to their assigned dialysis facility, as they do not need to be seen my medical professionals as often as patients on HD (O’Hare, Johansen, and Rodriguez 2006; Wang et al. 2017). PD supply in rural regions has increased, which is encouraging, as patients in these areas are more likely to initiate PD than urban patients (Hirth 2007). But it has still not caught up to PD supply levels in predominantly urban regions, suggesting that regional disparities remain.
Our adjusted results revealed that higher regional prevalence of white patients, higher per-capita income, higher PD prevalence and urban facility locations were associated with higher PD supply. These trends are consistent with previous studies (Wang, Lee, Patel, Maciejewski, and Ricketts 2011; Wang et al. 2010) conducted prior to Medicare payment reform, and persisted throughout all years of our study. Future research should explore the extent to which the PPS and other recent dialysis payment reforms have improved the alignment of patient preferences and dialysis modalities. Policy makers should develop effective levers to encourage growth in supply and patient access to PD to complement the incremental changes induced by the 2011 payment change, especially in the context of newly proposed federal policies that encourage a swift increase in patient access to and utilization of home-based dialysis within the next decade. Our findings elucidate the subgroups of ESRD patients who may benefit from or prefer home-based modalities.
Our results are consistent with prior findings that lower market competition and lower proportion of chain-affiliated facilities are associated with higher PD supply (Wang, Lee, Patel, Maciejewski, and Ricketts 2011; Wang et al. 2010). The lower overhead costs associated with PD treatment and the new reimbursement structure translates to substantially higher absolute and relative margins for PD compared to HD, an appealing financial incentive for dialysis providers (Hornberger and Hirth 2012) but perhaps not large enough for policy to translate to a groundswell of PD in the initial years of the 2011 payment reform. Startup costs and clinical logistics of developing a new type of dialysis program may require longer-term investment. It is also possible that our results reflect consolidation of PD services among chain-affiliated clinics. Large chains that already have standardized systems and processes for effectively delivering dialysis services across all of their facilities may be less likely to develop new dialysis programs and instead concentrate their PD services to only a few units with larger PD programs (Pulliam, Hakim, and Lazarus 2006). However, a recent analysis conducted at the facility-level suggests this may not be happening: PD program sizes did not vary by facility chain affiliation (Wang et al. 2018). Further studies, employing a more granular assessment of PD program consolidation within dialysis chains, could describe corporate regionalization strategies with better precision.
This study has several limitations. First, assessment of regional PD supply in this study was limited to the proportion of providers offering PD services. This variable may misclassify regional supply, as a small number of facilities may have increased the size of their PD programs, thereby increasing their capacity for treating PD patients. The likelihood of this, however, is small and would not affect our overall findings if it did occur. Second, we did not assess the extent to which some chain organizations may have consolidated their PD programs, which would appear as a lower or limited change in PD supply. Third, the quality of this study relies on the quality and accuracy of USRDS and CMS data. Changes in employment and comorbidities, for example, are not recorded. Finally, there are several factors that are potentially associated with changes in PD supply that we could not assess. For example, information on provider training and experience with PD, patient educational background, family support, and acuity of dialysis initiation (inpatient vs outpatient) was not available from the ESRD administrative data. These issues affect dialysis modality choices at the individual level and may affect dialysis modality supply at the regional level as well (Thamer et al. 2000; Mehrotra, Blake, Berman, and Nolph 2002; Furth et al. 2001).
Our study found that the historical decline in PD supply, which lasted from the 1990s to the early 2000s, has reversed: regional PD supply increased between 2006 and 2013. But PD supply continues to be lower in regions with fewer urban facilities, a greater proportion of non-white populations, and lower average incomes. While PD availability is increasing nationwide, patient disparities in access persist. Further research is needed to continue monitoring provider supply and patient utilization trends, and to explore the mechanisms underlying these trends. This research will be critical to informing strategies aimed at increasing PD supply in regions where more patients could benefit from this alternative, home-based dialysis modality, since the 2011 payment change may have been too incremental to overcome the supply- and demand-side barriers to greater PD supply.
Acknowledgements:
The authors thank Abby Hoffman and Kathryn Sleeman for scientific counsel and helpful comments on this manuscript; and Ms. JaNell Wylie and Ms. Nikita Shah for research assistance.
Funding: This research was supported by the National Institutes of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (R01DK097165). Dr. Maciejewski is supported by a Research Career Scientist award (RCS 10-391) from VA HSR&D. Dr. Sloan is supported by a VA Office of Affiliations Post-doctoral Fellowship.
Footnotes
Conflicts of interest: Dr. Maciejewski reports ownership of Amgen stock due to his spouse’s employment. The other authors (CS, CJC, LLS, SYDL, RH, and VW) report no relationship or financial interest with any entity that would pose a conflict of interest regarding the subject matter of this article.
REFERENCES
- Bhattacharya J, Hyde T, and Tu P. 2014. Health Economics. London, UK: Palgrave and MacMillan. [Google Scholar]
- Blake PG, and Finkelstein FO. 2001. Why is the proportion of patients doing peritoneal dialysis declining in North America? Perit Dial Int 21 (2):107–14. [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. 2015. Provider of Service Files. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/index.html. Baltimore, MD. [Google Scholar]
- Centers for Medicare & Medicaid Services. 2018. End Stage Renal Disease (ESRD) Prospective Payment System (PPS). Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ESRDpayment/index.html (accessed August 8, 2018). Baltimore, MD. [Google Scholar]
- Centers for Medicare & Medicaid Services. 2019. Medicare Program: Specialty Care Models To Improve Quality of Care and Reduce Expenditures (Proposed Rule CMS-5527-P). In Docket number CMS-2019–0101, edited by C. f. M. a. M. S. Department of Health and Human Services. Washington, DC: Federal Register. [Google Scholar]
- Cromley EK, and McLafferty SL. 2002. GIS and Public Health. New York, NY: Guilford Press. [Google Scholar]
- Dartmouth Atlas of Health Care Working Group. 2003. Geographic Boundary Files: Hospital Referral Region. Lebanon, NH: Center for the Evaluative Clinical Sciences. [Google Scholar]
- De Vecchi AF, Dratwa M, and Wiedemann ME. 1999. Healthcare systems and end-stage renal disease (ESRD) therapies--an international review: costs and reimbursement/funding of ESRD therapies. Nephrol Dial Transplant 14 Suppl 6:31–41. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, and et al. 2011. Applied longitudinal analysis. Hoboken, NJ: Wiley. [Google Scholar]
- Folland S, Goodman AC, and Stano M. 2001. The Economics of Health and Health Care, 3rd edition. Upper Saddle River, NJ: Prentice-Hall, Inc. [Google Scholar]
- Furth SL, Hwang W, Yang C, Neu AM, Fivush BA, and Powe NR. 2001. Relation between pediatric experience and treatment recommendations for children and adolescents with kidney failure. Jama 285 (8):1027–33. [DOI] [PubMed] [Google Scholar]
- Golper TA, Saxena AB, Piraino B, Teitelbaum I, Burkart J, Finkelstein FO, and Abu-Alfa A. 2011. Systematic barriers to the effective delivery of home dialysis in the United States: a report from the public policy/advocacy committee of the north american chapter of the international society for peritoneal dialysis. Am J Kidney Dis 58 (6):879–85. [DOI] [PubMed] [Google Scholar]
- Hao H, Lovasik BP, Pastan SO, Chang HH, Chowdhury R, and Patzer RE. 2015. Geographic variation and neighborhood factors are associated with low rates of pre-end-stage renal disease nephrology care. Kidney Int 88 (3):614–21. [DOI] [PubMed] [Google Scholar]
- Hirth RA 2007. The organization and financing of kidney dialysis and transplant care in the United States of America. Int J Health Care Finance Econ 7 (4):301–18. [DOI] [PubMed] [Google Scholar]
- Hirth RA, Turenne MN, Wheeler JR, Nahra TA, Sleeman KK, Zhang W, and Messana JA. 2013. The initial impact of Medicare’s new prospective payment system for kidney dialysis. Am J Kidney Dis 62 (4):662–9. [DOI] [PubMed] [Google Scholar]
- Hornberger J, and Hirth RA. 2012. Financial implications of choice of dialysis type of the revised Medicare payment system: an economic analysis. Am J Kidney Dis 60 (2):280–7. [DOI] [PubMed] [Google Scholar]
- Khawar O, Kalantar-Zadeh K, Lo WK, Johnson D, and Mehrotra R. 2007. Is the declining use of long-term peritoneal dialysis justified by outcome data? Clin J Am Soc Nephrol 2 (6):1317–28. [DOI] [PubMed] [Google Scholar]
- Lin E, Cheng XS, Chin KK, Zubair T, Chertow GM, Bendavid E, and Bhattacharya J. 2017. Home Dialysis in the Prospective Payment System Era. J Am Soc Nephrol 28 (10):2993–3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J, de Oliveira VB, Turci MA, Guanais FC, Bonolo PF, and Lima-Costa MF. 2011. The influence of primary care and hospital supply on ambulatory care-sensitive hospitalizations among adults in Brazil, 1999–2007. Am J Public Health 101 (10):1963–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra R, Blake P, Berman N, and Nolph KD. 2002. An analysis of dialysis training in the United States and Canada. Am J Kidney Dis 40 (1):152–60. [DOI] [PubMed] [Google Scholar]
- Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E, Mehrotra Rajnish, Chiu Yi-Wen, Kalantar-Zadeh Kamyar, Bargman Joanne, and Vonesh Edward. 2011. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Archives of Internal Medicine 171 (2):110–8. [DOI] [PubMed] [Google Scholar]
- Mehrotra R, Kermah D, Fried L, Kalantar-Zadeh K, Khawar O, Norris K, and Nissenson A. 2007. Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J Am Soc Nephrol 18 (10):2781–8. [DOI] [PubMed] [Google Scholar]
- Mehrotra R, Khawar O, Duong U, Fried L, Norris K, Nissenson A, and Kalantar-Zadeh K. 2009. Ownership patterns of dialysis units and peritoneal dialysis in the United States: utilization and outcomes. Am J Kidney Dis 54 (2):289–98. [DOI] [PubMed] [Google Scholar]
- Mendelssohn DC, Mullaney SR, Jung B, Blake PG, and Mehta RL. 2001. What do American nephrologists think about dialysis modality selection? Am J Kidney Dis 37 (1):22–29. [DOI] [PubMed] [Google Scholar]
- Miskulin DC, Meyer KB, Athienites NV, Martin AA, Terrin N, Marsh JV, Fink NE, Coresh J, Powe NR, Klag MJ, and Levey AS. 2002. Comorbidity and other factors associated with modality selection in incident dialysis patients: the CHOICE Study. Choices for Healthy Outcomes in Caring for End-Stage Renal Disease. Am J Kidney Dis 39 (2):324–36. [DOI] [PubMed] [Google Scholar]
- O’Hare AM, Johansen KL, and Rodriguez RA. 2006. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney Int 69 (2):343–9. [DOI] [PubMed] [Google Scholar]
- Pulliam J, Hakim R, and Lazarus M. 2006. Peritoneal dialysis in large dialysis chains. Perit Dial Int 26 (4):435–7. [PubMed] [Google Scholar]
- Queeley GL, and Campbell ES. 2018. Comparing Treatment Modalities for End-Stage Renal Disease: A Meta-Analysis. Am Health Drug Benefits 11 (3):118–127. [PMC free article] [PubMed] [Google Scholar]
- Sloan CE, Coffman CJ, Sanders LL, Maciejewski ML, Lee SD, Hirth RA, and Wang V. 2019. Trends in Peritoneal Dialysis Use in the United States after Medicare Payment Reform. Clin J Am Soc Nephrol 14 (12):1763–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack AG 2002. Determinants of modality selection among incident US dialysis patients: results from a national study. J Am Soc Nephrol 13 (5):1279–87. [DOI] [PubMed] [Google Scholar]
- Thamer M, Hwang W, Fink NE, Sadler JH, Wills S, Levin NW, Bass EB, Levey AS, Brookmeyer R, and Powe NR. 2000. US nephrologists’ recommendation of dialysis modality: results of a national survey. Am J Kidney Dis 36 (6):1155–65. [DOI] [PubMed] [Google Scholar]
- Thomas BA, Rodriguez RA, Boyko EJ, Robinson-Cohen C, Fitzpatrick AL, and O’Hare AM. 2013. Geographic variation in black-white differences in end-of-life care for patients with ESRD. Clin J Am Soc Nephrol 8 (7):1171–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A, Lesmana B, Johnson DW, Wong G, Campbell D, and Craig JC. 2013. The perspectives of adults living with peritoneal dialysis: thematic synthesis of qualitative studies. Am J Kidney Dis 61 (6):873–88. [DOI] [PubMed] [Google Scholar]
- Turenne M, Baker R, Pearson J, Cogan C, Mukhopadhyay P, and Cope E. 2018. Payment Reform and Health Disparities: Changes in Dialysis Modality under the New Medicare Dialysis Payment System. Health Serv Res 53 (3):1430–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. 2019. Advancing American Kidney Health, edited by Office of the Assistant Secretary for Planning and Evaluation. https://aspe.hhs.gov/system/files/pdf/262046/AdvancingAmericanKidneyHealth.pdf. (Accessed August 13, 2019). [Google Scholar]
- US Renal Data System. 2016. 2015 Annual Data Report and Researcher’s Guide to the USRDS Database. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. [Google Scholar]
- US Renal Data System. 2017. USRDS 2017 Annual Data Report: Atlas of End-stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. [Google Scholar]
- US Renal Data System. 2018. USRDS 2018 Annual Data Report: Atlas of End-stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. [Google Scholar]
- Venkataraman V, and Nolph KD. 1999. Socioeconomic aspects of peritoneal dialysis in North America: role of non medical factors in the choice of dialysis. Perit Dial Int 19 Suppl 2:S419–22. [PubMed] [Google Scholar]
- Verbeke G, and Molenbergh G. 2000. Linear mixed models for longitudinal data. New York: Spinger-Verlag. [Google Scholar]
- Wang V, Coffman CJ, Sanders LL, Lee SYD, Hirth RA, and Maciejewski ML. 2018. Medicare’s new prospective payment system on facility provision of peritoneal dialysis. Clin J Am Soc Nephrol (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang V, Coffman CJ, Sanders LL, Lee SD, Hirth RA, and Maciejewski ML. 2018. Medicare’s New Prospective Payment System on Facility Provision of Peritoneal Dialysis. Clin J Am Soc Nephrol 13 (12):1833–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang V, Lee SYD, Patel UD, Weiner BJ, Ricketts TC, and Weinberger M. 2010. Geographic and temporal trends in peritoneal dialysis services in the United States between 1995 and 2003. American Journal of Kidney Diseases 55 (6):1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang V, Lee SY, Patel UD, Maciejewski ML, and Ricketts TC. 2011. Longitudinal analysis of market factors associated with provision of peritoneal dialysis services. Med Care Res Rev 68 (5):537–58. [DOI] [PubMed] [Google Scholar]
- Wang V, Maciejewski ML, Coffman CJ, Sanders LL, Lee SD, Hirth R, and Messana J. 2017. Impacts of Geographic Distance on Peritoneal Dialysis Utilization: Refining Models of Treatment Selection. Health Serv Res 52 (1):35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg JE, and Cooper MA. 1999. The Dartmouth Atlas of Health Care in the United States. Chicago, IL: American Hospital Association. [Google Scholar]
- Wong B, Ravani P, Oliver MJ, Holroyd-Leduc J, Venturato L, Garg AX, and Quinn RR. 2018. Comparison of Patient Survival Between Hemodialysis and Peritoneal Dialysis Among Patients Eligible for Both Modalities. Am J Kidney Dis 71 (3):344–351. [DOI] [PubMed] [Google Scholar]


