Abstract
Objective:
Research has repeatedly demonstrated that parent foreign nativity has a protective effect on child asthma outcomes among Mexican Americans, but the mechanisms underlying this relationship are not well understood. The current study explored parent depression as a mediator and social support as a moderator of the parent nativity-child asthma control pathway.
Methods:
Data come from the baseline sample of a trial (NCT02481986) testing community interventions for 223 children aged 5–16 with uncontrolled asthma. We focused on parent/child dyads of Mexican heritage (N=165; mean age=9.08, SD=2.94; 57.3% with Mexico-born parent). Asthma control was defined using the child and adult versions of the Asthma Control Test (ACT). Psychosocial factors included parent depression symptoms and social (instrumental, informational, and emotional) support.
Results:
Mexican-born parents had fewer depressive symptoms (, ) and children with better asthma control (, ) than U.S.-born parents, p<.0001. Analyses suggested partial mediation of the nativity-ACT path via parent depression (p<.001). An interaction between Instrumental Support and Nativity was marginally significant (, , p=.07), with protective effects only observed at higher support levels. Last, among Mexico-born parents, the protective nativity effects on ACT declined with increasing residential years in the U.S. through 12 years.
Conclusions:
This study is novel in identifying parent depression as one mechanism underlying the effects of parent nativity on child asthma control, but results suggest that the health advantages may depend on availability of support. Providing resources for parent depression and instrumental support (transportation, childcare) can optimize asthma interventions in this population.
Keywords: Hispanic Health Paradox, Latino, Mexican Immigrants, Pediatric Asthma, Depression, Social Support
The Hispanic Health Paradox (HHP) describes the phenomenon that individuals of Hispanic heritage who immigrate to the United States experience better health outcomes across a variety of conditions compared to U.S.-born counterparts as well as other ethnic-racial groups with similar socioeconomic profiles in the U.S.1 In particular, the HHP has been well-documented in pediatric asthma and has important implications for optimizing asthma interventions.2,3 Childhood asthma prevalence in the U.S. remains high at six million, despite advances in medications and support interventions, and significant health disparities exist.4 Among youth of Mexican heritage, more than 1.4 million are diagnosed with asthma during childhood,5 but social and environmental influences on asthma risk among this population have received less attention. Research suggests that parent nativity may confer asthma protection, such that mainland U.S.-born children of foreign-born parents have better asthma outcomes than children of mainland U.S.-born parents2,6–8 with effects observed most robustly among persons of Mexican heritage.2,9 Protective effects of parent foreign nativity on child asthma outcomes have been shown to persist through the third generation (i.e., U.S.-born parents with foreign-born grandparents), suggesting a powerful health advantage.10 However, the mechanisms underlying these relationships are not well-understood.7,11 Similarly, the duration of effects across years lived in the U.S. has not been well established, but research suggests that protective effects may diminish with increased integration in American culture and lifestyle.12 Further understanding of the parent nativity-child asthma relationship is needed to inform interventions and guidelines to improve outcomes and reduce health disparities among minority youth.
Research demonstrating the HHP among psychosocial outcomes offers avenues for identifying factors that may contribute to the nativity effects observed in pediatric asthma. Notably, Mexico-born adults are less likely to have anxiety, depression and substance use disorders compared to counterparts born in the U.S.12,13 Evidence suggests a particularly strong HHP effect for depression in individuals of Mexican origin,13 with findings pointing to a three-fold increase in depression rates as well as earlier onset of depression in U.S.- versus Mexico-born Hispanics.14 In addition, social support – which may encompass cohesion and emotional support, information exchange, and instrumental help – has been shown to positively influence asthma control among Mexican and Puerto Rican children7 and may contribute to protective HHP effects on asthma. Indeed, the health advantages of nativity may depend on the levels of available social support. Cagney and colleagues found that the protective effects of foreign nativity on adult asthma were only observed in dense immigrant Latino, primarily Mexico-born, neighborhoods.15 Collectively, these findings highlight the importance of exploring the psychological and broader contextual influences to advance understanding of the HHP. Parent depression16,17 and social support7,16 have been associated with child asthma control and thus may serve as key pathways linking parent nativity and child asthma outcomes. However, limited research has examined the interplay of parent mental health, place of birth, and child asthma outcomes.
In our past work, we demonstrated how parent depression and family factors (chaos, low support) predict worse child asthma control.16 We expand on this work in the current study to explore the role of parent and family factors in the relationship between parent nativity and child asthma control in persons of Mexican heritage. Specifically, guided by studies suggesting links between nativity and depression as well as parent depression and asthma,13, 16–17 we examined parent depression as a mediator of the nativity-asthma relationship. We also explored family social support (including emotional, informational, and instrumental support) as moderators of this relationship in light of research demonstrating that nativity effects may be influenced by availability of support.15 We also explored the duration of parent nativity effects on child asthma across parent residential years in the U.S. These questions were examined among a sample of youth with uncontrolled asthma enrolled in the Asthma Action at Erie Trial (NCT02481986).18 Because the most robust effects of the HHP have been seen in populations of Mexican heritage,9 we focused exclusively on Mexican heritage families in the baseline cohort of the trial. We hypothesized that (1) children of Mexico-born parents would evidence better asthma control than children of U.S.-born parents; (2) parent depression would mediate the effects of parent nativity on child asthma control; (3) higher levels of social support would enhance the protective effects of nativity on child asthma control; and (4) protective nativity effects would decline across duration of parent residential time in the U.S. among children of Mexico-born parents.
Methods
Data were obtained from the baseline cohort of the Asthma Action at Erie trial, a randomized comparative effectiveness trial designed to compare certified asthma educator services (two in-clinic sessions) to a 10-session community health worker home intervention in families of children with uncontrolled asthma.18 The trial involves a partnership between the University of Illinois at Chicago and Erie Family Health Centers (Erie), a multi-site federally qualified health center serving mainly low-income minority families in Chicago. Participants were enrolled as parent/child dyads. Inclusion criteria for children were (1) patient at Erie, (2) aged 5–16 years, (3) live with caregiver at least five days/week, and (4) uncontrolled asthma. Multiple measures of asthma impairment and risk were used to determine asthma control following expert guidelines,19 defined as any of the following: >/=1.25 on the Asthma Control Questionnaire20,21 (ACQ) or <20 on the Asthma Control Test/childhood Asthma Control Test22–24 (ACT/cACT) or a report of at least one oral corticosteroid (OCS) burst for asthma in the past year. Exclusion criteria included: could not speak English or Spanish, did not have permanent housing, caregivers did not have permanent custody, or the child had significant developmental delays or co-morbidities that would significantly limit their ability to participate in the study. Recruitment occurred between March 2016-August 2017, and 223 families were enrolled and randomized to one of two interventions (N=223). For details regarding the study design, intervention conditions, and categorizations of asthma control within the sample, the reader is referred to Mosnaim et al., 2019.18 For this study, the sample was restricted to dyads of self-reported Mexican heritage (N=165).
Procedures and Measures
All study procedures were approved by Institutional Review Boards and the Erie Research Committee. Caregivers and children older than seven years provided signed consent and assent, respectively. Bilingual research assistants (RAs) collected data in participants’ homes via computer. Interviews were conducted in English (44.2%), Spanish (35.2%), or both English and Spanish (20.6%), depending on the preference of the family.
Our primary outcome of asthma control in this study was the ACT (children 12 and older) and cACT (children under 12); higher values on these continuous scales indicate better controlled asthma symptoms.22–24 The cACT/ACT include both child- and parent-report and have been validated in Spanish.25–26 Parent depression symptoms were measured via parent-report on the widely-used 9-item Patient Health Questionnaire (PHQ-9);27 total scores range from 0 to 27. The PHQ-9 has been published in Spanish and has demonstrated good psychometric properties for depression screening and diagnosis in Mexican populations.28 Parent social support was assessed using the Patient-Reported Outcomes Measurement Information System (PROMIS) Support scales,29 which were developed and validated to measure self-reported social health in English- and Spanish-speaking adults.30 Three 8-item subscales assessed Emotional Support (e.g., “I have someone to listen to me when I need to talk”), Instrumental Support (e.g., “Do you have someone to prepare your meals if you are unable to do it yourself;” “Is someone available to help you if you need it?”), and Informational Support (e.g., “I can get useful advice about important things in life”). Items are rated on a 1 (never) to 5 (always) scale; total scores are converted to T-scores. In addition, demographic characteristics potentially related to asthma outcomes or the nativity-asthma relationship (e.g., obesity3,31) were included in this study as covariates. Demographics, parent education, parent nativity, medications, and self-reported behaviors were assessed by the RAs through questions and observations; height and weight were also measured by the RAs. Body mass index was calculated according to age- and sex-specific percentiles and transformed into z-scores.32
Analytic Plan
Age-specific ACT measures were combined into a single measure to retain all subjects in the analyses by rescaling the ACT to the range of the cACT (hereafter referred to as ACT).16 We chose to combine scales rather than using the established cutoffs for poor control to allow for a continuous outcome measure, thus preserving statistical power to address our hypotheses. A series of linear regression models using generalized estimating equation (GEE) to account for clustering of observations in health clinics were estimated. The models examined the hypothesized effects of parent nativity, parent depression, and parent social support on child asthma control. Moderator analyses were examined by including the interaction term for each support subscale (emotional, instrumental, informational) by nativity on child asthma control. All models controlled for demographic characteristics identified a-priori based on prior work demonstrating a significant relationship to asthma outcomes (child age, child sex, BMI, maternal age, and maternal education).16 For brevity, only the effects of hypothesized predictors are discussed. Complete case analyses were implemented as there was no missing data in the sample.
To examine our hypothesis that parental depression may mediate the link between parent place of birth and child asthma control, we estimated a causal mediation model33 controlling for covariates described above. The average total, indirect, and direct causal mediation effects were estimated using the model-based approach implemented in the mediation package in R.34 The average mediation effects are estimated based on 10,000 simulations following the quasi-Bayesian Monte Carlo method based on normal approximation with cluster robust estimator for the covariance matrix.35 Of note, we considered the exposure-mediator interaction in the mediation model. However, given that the estimated magnitude of the interaction was very small and did not alter the direct and indirect effects, the exposure-mediator interaction was dropped from the final mediation model.33 Because the sequential ignorability assumption is untestable, we conducted a sensitivity analysis of the effects. Sensitivity analyses for the average indirect effect assessed the robustness of findings to the violation of the sequential ignorability assumption and was performed by varying the correlation between error terms of the mediator and outcome models.35 Lastly, to examine the duration of effects across years in the U.S., a model examined linear and quadratic effects for the number of residential years in the U.S. on ACT among Mexico-origin parents, controlling for demographic and site covariates as discussed above. Analyses were conducted in SAS 9.4 and statistical computing platform R v. 3.6.0.
Results
Sample Characteristics
Sample demographic characteristics are presented in Table 1. Children had a mean age of 9.08 (SD=2.94), were primarily born in the U.S. (97.6%), and 51.5% demonstrated uncontrolled asthma on the ACT. Youth had high rates of OCS bursts (63%), suggesting considerable asthma morbidity. Caregivers were predominantly parents (99.4%) and female (96.4%), with low educational attainment (70.9% high school diploma/GED or less). More than half of the parents were born in Mexico (57.3%). Additionally, one-third of parents endorsed mild to severe depressive symptoms. Social support was lower than the general U.S. population average.
Table 1.
Child and Parent Characteristics (N=165)
| Child | N = 165 | Parent | N = 165 |
|---|---|---|---|
| Place of Birth, n(%) | Place of Birth, n(%) | ||
| Mainland United States | 161 (97.6) | Mainland United States | 70 (42.7) |
| Mexico | 2 (1.2) | Mexico | 95 (57.3) |
| Puerto Ricoa | 2 (1.2) | ||
| Female Gender, n(%) | 72 (43.6) | Female Gender, n(%, | 159 (96.4) |
| Age, mean (SD) | 9.08 (2.9) | Age, mean (SD) | 35.42 (6.3) |
| 5–11 years, n (%) | 137 (83.0) | ||
| 12–16 years, n (%) | 28 (17.0) | ||
| BMI, n(%) | Education | ||
| Normal (< 85th%ile) | 69 (41.8) | Less than high school | 50 (30.3) |
| Overweight (85–95th%ile) | 29 (17.6) | High school graduate/GED | 67 (40.6) |
| Obese (>95 th%ile) | 67 (40.6) | Some college/college graduate | 48 (29.1) |
| Asthma Control Test (ACT), mean (SD) | 18.6 (4.6) | Years Lived in the US, Mean (SD) | 17.50 (6.6) |
| Median (range) | 17.00 (4.0–40.0) | ||
| Uncontrolled, n (%) | 85 (51.5) | ||
| Any oral corticosteroid use for asthma in past 12 months, n (%) | 104 (63.0%) | Depression symptoms, mean (SD) | 4.16 (5.1) |
| Minimal, n(%) | 112 (67.9) | ||
| Mild, n(%) | 29 (17.6) | ||
| Moderate-severe, n(%) | 24 (14.5) | ||
| Social Support, mean (SD) | |||
| Emotional | 33.43 (8.6) | ||
| Instrumental | 30.30 (9.5) | ||
| Informational | 31.51 (8.2) |
Note. Social support scale T-scores correspond to a mean of 50, SD = 10; below 40 = worse than average; above 60 = above average.
These families also reported Mexican heritage.
Parent Nativity Effects on Child Asthma Control and Parent Depression
Outcomes of the model examining parent nativity on ACT indicated that children of parents born in Mexico had better asthma control than children of U.S.-born parents, , , p<.0001. Estimated mean ACT scores of children of Mexico-born parents (19.37) were in the controlled range, versus children of U.S.-born parents with scores in the clinical range (17.60; >19 = controlled asthma). A separate model examined parent nativity on parent depression as the outcome and revealed a significant effect (, , p<.0001), with Mexico-born parents experiencing significantly fewer depressive symptoms (estimated M= 3.30, SE=0.10) than U.S.-born parents (estimated M=5.33, SE=0.14).
A series of models examined emotional support, instrumental support, and informational support as moderators of the nativity-ACT relationship, controlling for covariates. Findings revealed a trend for the interaction of parent nativity and instrumental support (, , p=.07), such that the association of nativity and ACT varied by level of support. Figure 1 illustrates the interaction, indicating that child asthma control is better in Mexico-born versus U.S.-born parents at high levels of instrumental support, but there are no differences in child asthma control at low levels of support. Emotional Support by Parent Nativity and Informational Support by Parent Nativity were not significant (, , p=.49 and , , p=.17).
Figure 1.
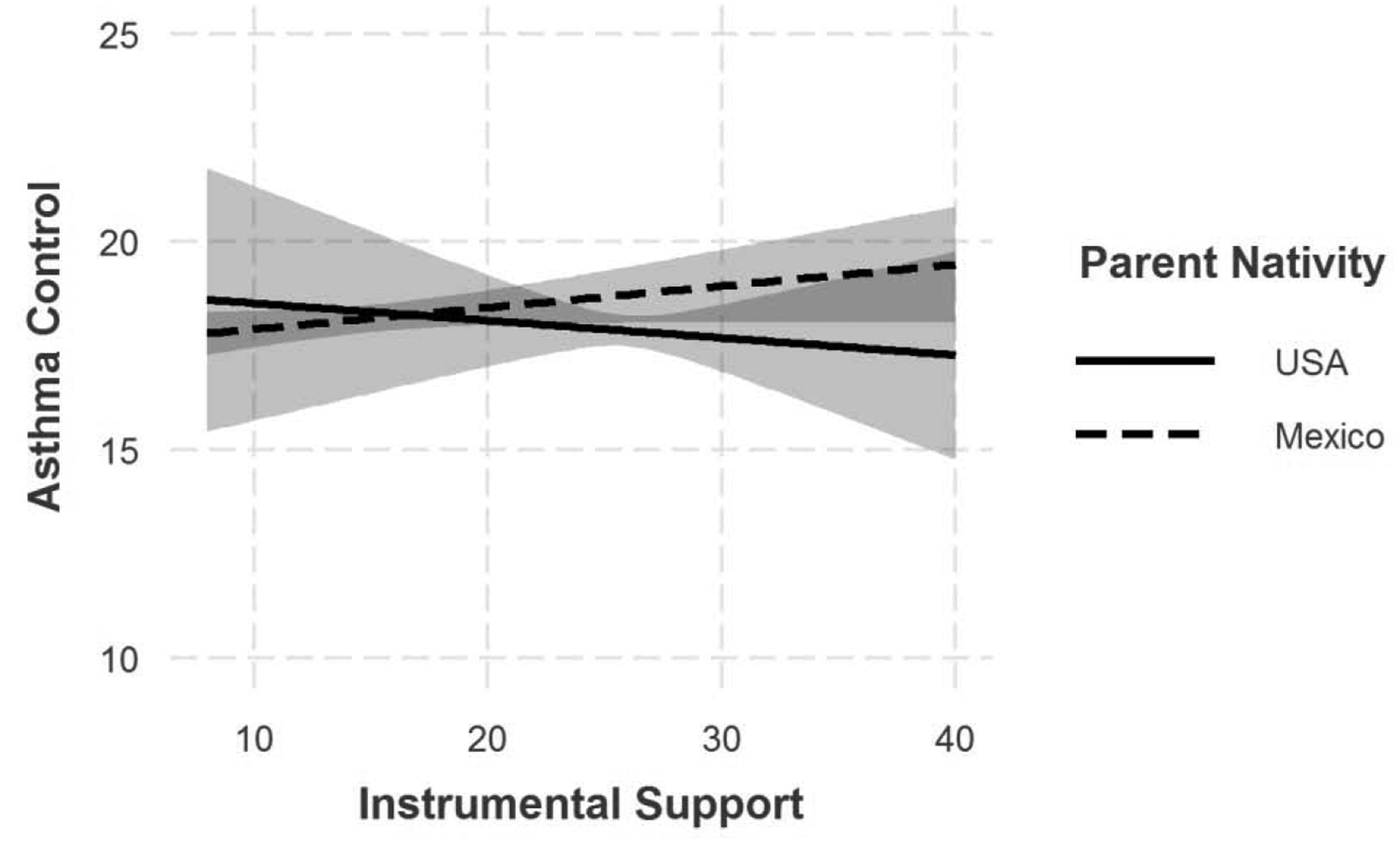
Child asthma control (ACT) as a function of Instrumental Support for parents born in the U.S. versus Mexico.
Mediation Analysis
Figure 2 displays the mediation model. Findings revealed a significant indirect path between parent nativity and ACT through parent depression (; CI= −0.87, −0.33; p<.0001). When controlling for parent depression, the nativity-ACT direct path became weaker, suggesting partial mediation (, CI = −2.06, −0.31, p=.01). The indirect effect contributed to 33% of total effect. Parents born in the U.S. endorsed higher rates of depressive symptoms and, in turn, had children with worse asthma control. Sensitivity analyses indicated that the mediation effects are zero for a ρ = −0.31 and the confidence intervals include zero for ρ = −0.22, which suggests robustness to assumption violations.
Figure 2.
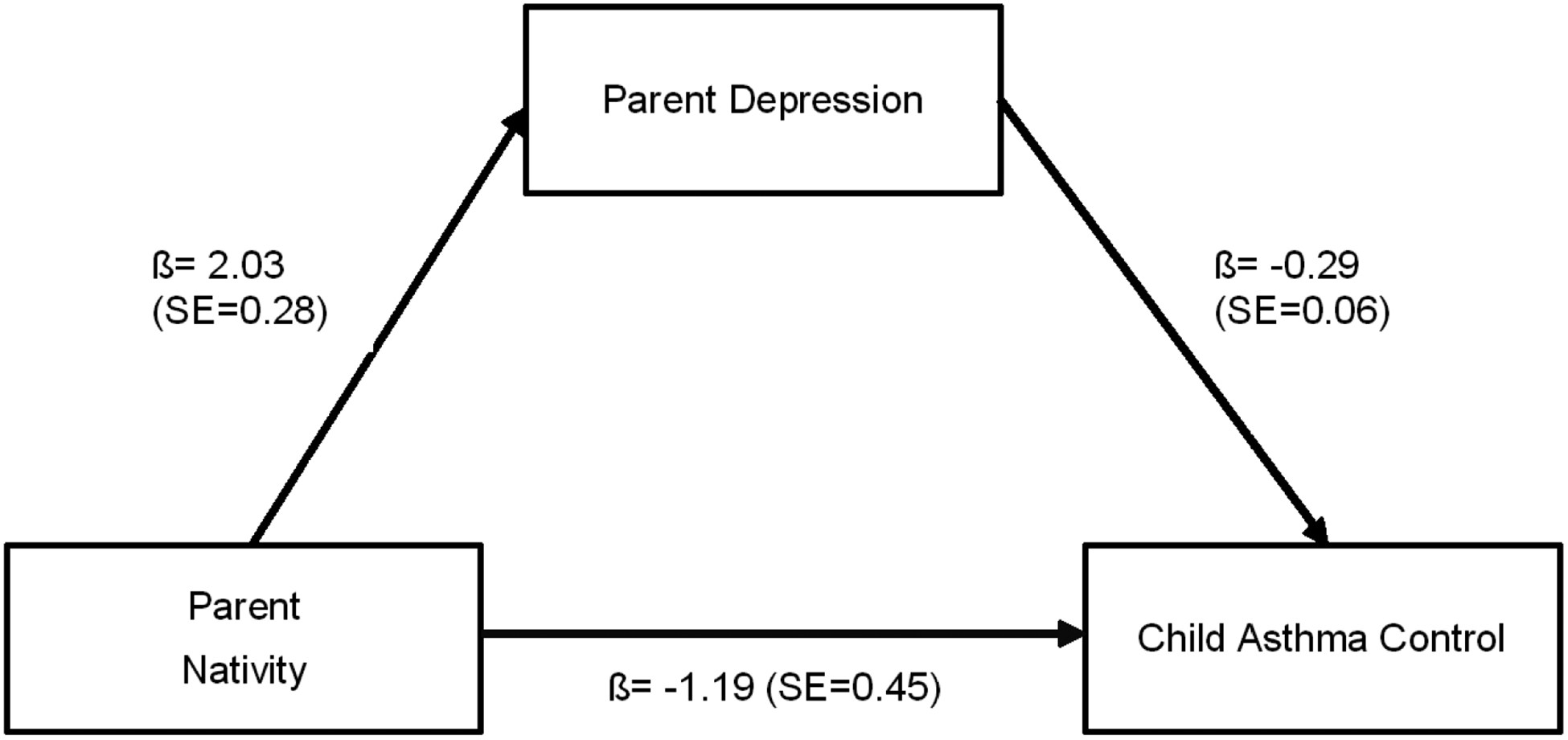
Mediation model of the effect of parent nativity on ACT via parent depression. Solid lines are significant (p < .05).
Duration of Nativity Effects on ACT
Last, we examined the duration of nativity effects on ACT among children of Mexico-born parents. Findings revealed a quadratic effect of years in the U.S. on ACT (linear , , p<0.0001; quadratic , , p<0.0001). Figure 3 depicts child ACT scores as a function of parent residential years in the U.S. and reveals that the protective nativity effect on ACT steadily declines across time until 12 years, at which point ACT scores improve. Findings correspond to a clinically meaningful worsening of asthma control over 12 years.36 To better understand this finding, post-hoc analyses explored instrumental support and parent depressive symptoms as a function of parent residential years in the U.S. However, neither linear nor quadratic effects for instrumental support or parent depression were significant.
Figure 3.
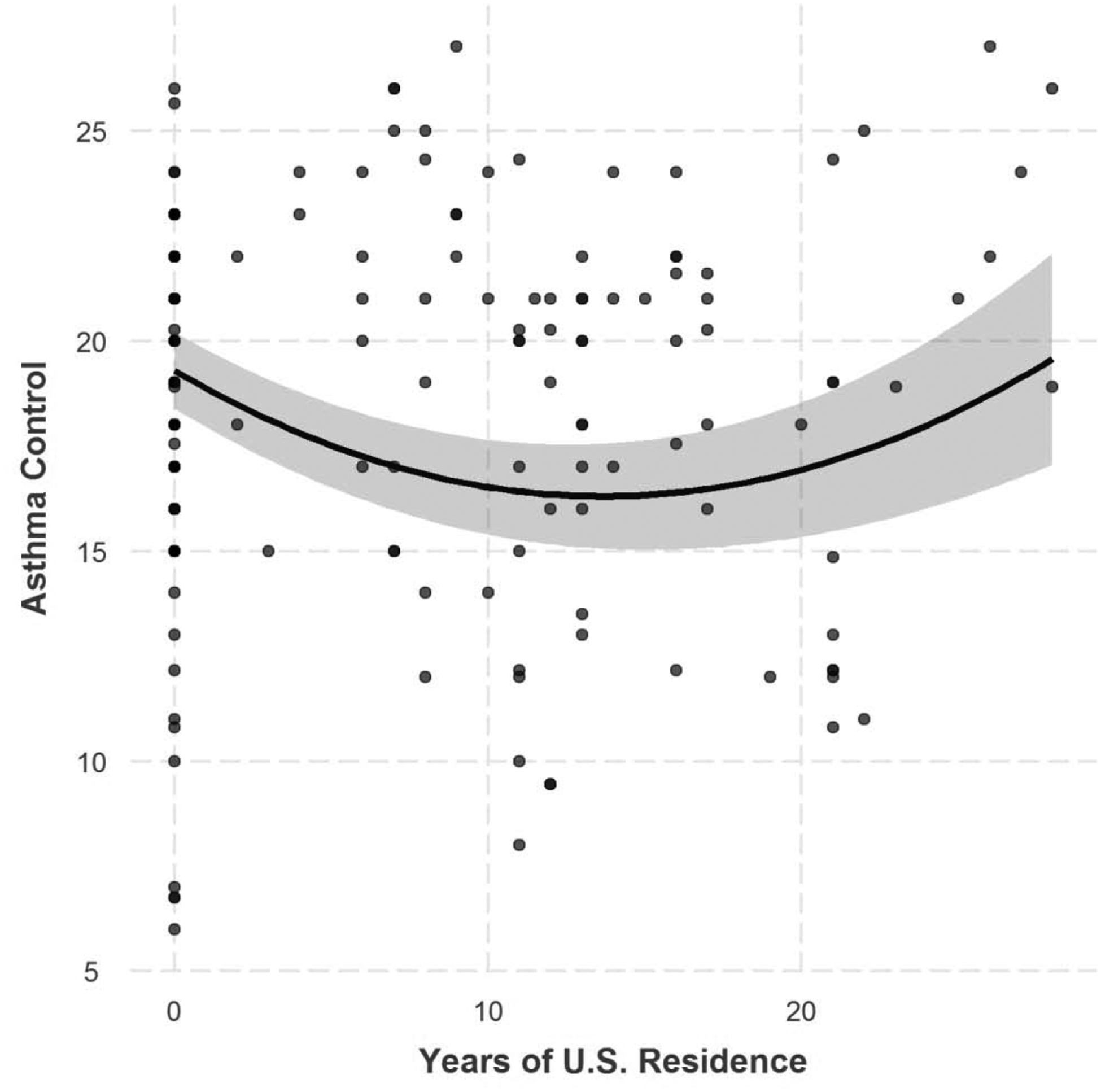
Estimated quadratic trend (with 95% CI) of child asthma control (ACT) as a function of Mexico-born parent residential years in the U.S.
Discussion
The present study sought to examine the psychosocial factors influencing the effects of parent nativity on child asthma control among families of Mexican heritage. In line with our hypotheses and prior research, nativity effects were evident: better child asthma control and lower parent depressive symptoms were observed among Mexico-versus U.S.-born parents. We demonstrated that parent depression, in part, mediated the relationship between parent place of birth and child asthma control, and instrumental support was found to moderate the parent nativity-child asthma pathway at a trend level. To our knowledge, this is the first study to examine parent depression as a mechanism underlying these relationships. We also showed that asthma control declined with more years living in the U.S. up until the 12-year mark, at which point asthma control improved.
Nativity Effects on Child Asthma
In our sample of high-risk youth with uncontrolled asthma, children of a Mexico-born parent evidenced significantly better asthma control as compared to their counterparts with US-born parents. Our findings are congruent with past studies demonstrating the protective relationships between parent nativity and child asthma prevalence and severity among individuals of Mexican heritage8,37 The bigger question is why this happens. Hillemeir and colleagues37 found that Mexican-American children with two U.S.-born parents experienced elevated behavioral and biological risk factors for asthma in early childhood as compared to children with one or more foreign-born parents (e.g., lower likelihood of being breastfed, greater chances of living with a smoker, family history of asthma, history of respiratory illness, and allergies) that may contribute to the parental nativity influence on child asthma prevalence. Prior studies have also explored the HHP in the context of broader measures of acculturation, with mixed findings. In a study of predominantly Mexican-American infants, fewer biological asthma risks were associated with lower caregiver acculturation, as defined by caregiver nativity and Spanish-language preference.38 Martin et al.2 examined the relationship between caregiver’s level of acculturation, defined by language preference, place of birth, and duration of residence in the U.S., and child asthma prevalence among families of Mexican heritage. Results demonstrated that place of birth may be more relevant for asthma outcomes than other dimensions of caregiver acculturation (language or time in the U.S.), which is consistent with the association between parent nativity and asthma control we found in our sample. However, further research is necessary to understand the complex psychosocial processes involved in acculturation to the U.S. among Mexico-born parents, and how this contributes to asthma burden.
Nativity Effects: Mediating and Moderating Factors
Our findings also indicated that parent depression was lower among Mexico- versus U.S.-born parents and may serve as a pathway linking parent nativity and child asthma control. Several studies have observed the HHP in depression in persons of Mexican heritage in the U.S.12,13 with findings suggesting that protective effects may be due, in part, to the level of acculturation and the preservation of ethnic identity. For example, Calzada and Sales13 found that more acculturated mothers (defined as born in or early immigration to the U.S. and English-speaking) were less likely to endorse a strong ethnic identity than less acculturated mothers (immigration to the U.S. at older ages, predominantly Spanish-speaking), which prospectively predicted higher depression symptoms at a one-year follow-up. Thus, although not examined in this study, the preservation of cultural characteristics may exert a protective influence on depressive symptoms among Mexico-born parents.
Parent depression emerged as a partial mediator of the parent nativity-child asthma link, such that Mexico-born parents had lower levels of depressive symptoms that, in turn, was related to better child asthma control. Caregiver depression is a key risk factor for child asthma severity16,17 as well as negative practices and beliefs surrounding the management of their child’s asthma.39 Our past work has also highlighted the family-level mechanisms that may underlie these relationships, indicating that parental depression may predict higher levels of family chaos that interfere with asthma management and control.16 These relationships are likely transactional; the stressors accompanying parenting a child with severe asthma may contribute to depression,39 and parent depression may influence the ability to care for a child with asthma.16, 40 Our findings suggest that parent nativity may protect against depression and serve as a pathway for better child asthma control among new immigrants. Together, our studies underscore the importance of screening and support for parent depression to improve child asthma outcomes, particularly for U.S.-born parents of Mexican-heritage.
We also found that parent nativity effects on child asthma control were pronounced at higher levels of instrumental support, whereas at low levels of support, there was no apparent nativity effect. These findings are consistent with past research demonstrating that the health advantages of foreign nativity may be contingent on the availability of local supportive networks.15 In past studies of Hispanic populations, social support predicts better child asthma control, possibly by reducing the burden of asthma management for caregivers.7 Indeed, our findings indicated that only instrumental support – which refers to tangible, local resources such as help with childcare, household tasks, and transportation – was relevant for asthma control, but emotional and informational support were not significant moderators. Although preliminary, these findings offer research and clinical implications, highlighting the need for studies examining behavioral asthma interventions involving the family and their community (e.g., Community Health Workers) focused on building systems of instrumental support. Interventions often focus on education or referrals (i.e., informational support), yet our results suggest that access to resources such as transportation vouchers to medical visits, meal services, or babysitting may yield an important return in terms of asthma control among families with foreign-born parents.
Duration of Nativity Effects
Despite observing protective effects of parent nativity on child asthma control, findings indicate that the advantages may diminish over time. Our findings are similar to past research demonstrating an increased risk of asthma in children after 10 years of residence in the United States8 and greater overall health among newly arrived immigrants of Hispanic heritage as compared to those who have spent more years in residence in the U.S.1 Notably, child asthma control declined across parent years of U.S. residence until reaching the lowest point at 12 years, but then reversed direction. This effect was not explained by changes in instrumental support or parent depressive symptoms as a function of residential years in the U.S., suggesting that other factors may contribute to the observed trajectory. Although not examined in this study, the downward trend followed by a reversal at 12 years may be explained by changes in access to healthcare and other supportive resources during this timeframe. Foreign-born Hispanics are less likely to have health insurance and health care access during the first 15 years in the U.S;41 thus, the reversal may reflect changes in access to treatment and decreased health-related stress. Additionally, although we did not find evidence of quadratic trend of instrumental support across duration of U.S. residence in our cross-sectional data, other work7,15 highlights the importance of social capital, including social support and integration in community networks, as an important determinant of health outcomes. Yet establishing social capital may take time; the strengthening of supportive community networks likely increases across duration of U.S. residence and may contribute to the reversal observed in our sample after 12 years of residence. Prospective research is warranted to explore the transactional relationships between health outcomes, acculturation and community supports, and access to socioeconomic resources across years of U.S. residence.
Limitations
Limitations of our study must be noted. Given that the study is cross-sectional, we are restricted in our ability to draw causal conclusions, and results must be interpreted with caution. Additionally, all measures were self-report. Our depression measure did not provide clinical diagnoses, and findings may not generalize to clinical samples. We also focused on parent place of birth rather than acculturation. Preliminary analyses separately examined the effects of place of birth and a measure of acculturation (defined as language use); consistent with past work, place of birth demonstrated more robust relationships with key outcome measures,2 and thus we chose to focus on nativity. Although findings cannot be generalized to broader constructs of acculturation, our examination allows for a finer-grained analysis of how nativity of Mexico-born parents can influence the health outcome of their children in the U.S.6
Conclusions
Our study offers insight into the psychosocial factors that may explain the protective effects of parent nativity on child asthma control among youth of Mexican heritage with uncontrolled asthma. The findings, albeit preliminary, have important implications for child asthma interventions. Results suggest that pediatric asthma interventions that incorporate a focus on parent depression assessment and treatment may be critical for enhancing asthma outcomes, particularly among Hispanic families born in the United States. Similarly, facilitating access to tangible resources and reliable support networks is paramount for families with foreign-born parents, and the first 12 years of residence in the U.S. may present a key window for intervention.
What’s New.
Parent depression may explain the link between parent foreign nativity and child asthma control in Mexican-heritage families, but protective nativity effects may depend on local supportive resources. Interventions should address parent depression and instrumental support to optimize child asthma outcomes.
Acknowledgments
We would like to thank the staff who collected these data: Gizelle Alvarez, Daisy Cintron, Jazmin Morales, and Genesis Rosales. We also want to recognize the Asthma Action at Erie Steering Committee who are not authors: Michael Berbaum, Ana Cesan, Hannah Chi, Andrea Fragoso, Denise Guerrero, Melissa Hernandez, Steven Rothschild, and Angkana Roy. The Chicago Asthma Consortium Asthma Community Advisory Board provides oversight for the study. We would like to thank everyone at Erie Family Health Center. This includes medical directors, providers and staff at the West Town Health Center, Evanston/Skokie Health Center, Erie Helping Hands Health Center, Erie Humboldt Park Health Center, Erie Westside Health Center at Laura S. Ward Elementary School, and Erie Johnson School-Based Health Center. Finally, we would like to thank all the families who made this research possible.
Funding source:
All phases of this study were supported by University of Illinois at Chicago and Erie Family Health Center. This work was supported by the National Heart, Lung, and Blood Institute [grant # 1R01HL123797 (PI Molly Martin)].
List of Abbreviations
- HHP
Hispanic Health Paradox
- U.S.
United States
- ACT
Asthma Control Test
- cACT
Child Asthma Control Test
- BMI
body mass index
- SD
standard deviation
- SE
standard error
- OR
odds ratio
- CI
confidence interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
All authors have indicated they have no potential conflicts of interest to disclose.
Clinical Trial Registration:
ClinicalTrials.gov Identifier NCT02481986, Asthma Action at Erie Trial, https://clinicaltrials.gov/ct2/show/NCT02481986?term=NCT02481986&rank=1
References
- 1.Teruya SA, Bazargan-Hejazi S. The Immigrant and Hispanic Paradoxes: A Systematic Review of Their Predictions and Effects. Hispanic Journal of Behavioral Sciences. 2013;35(4):486–509. doi: 10.1177/0739986313499004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin MA, Shalowitz MU, Mijanovich T, Clark-Kauffman E, Perez E, Berry CA. The effects of acculturation on asthma burden in a community sample of Mexican American schoolchildren. Am J Public Health. 2007;97(7):1290–6. doi: 10.2105/AJPH.2006.092239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thakur N, Borrell LN, Ye M, Oh SS, Eng C, Meade K, et al. Acculturation is associated with asthma burden and pulmonary function in Latino youth: The GALA II study. Journal of Allergy and Clinical Immunology. 2019;143(5):1914–22. doi: 10.1016/j.jaci.2018.12.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention; Most Recent National Asthma Data [internet]; 2017. [updated 2018 May 15; cited 2019 November 9]. Retrieved from https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm.
- 5.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2009. Vital Health Stat 10. 2010(247):1–82. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21563639. [PubMed] [Google Scholar]
- 6.Camacho-Rivera M, Kawachi I, Bennett GG, Subramanian SV. Revisiting the Hispanic health paradox: the relative contributions of nativity, country of origin, and race/ethnicity to childhood asthma. J Immigr Minor Health. 2015;17(3):826–33. doi: 10.1007/s10903-013-9974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scheckner B, Arcoleo K, Feldman JM. The effect of parental social support and acculturation on childhood asthma control. J Asthma. 2015;52(6):606–13. doi: 10.3109/02770903.2014.991969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eldeirawi KM, Persky VW. Associations of physician-diagnosed asthma with country of residence in the first year of life and other immigration-related factors: Chicago Asthma School Study. Annals of Allergy, Asthma & Immunology. 2007;99(3):236–43. doi: 10.1016/S1081-1206(10)60659-X. [DOI] [PubMed] [Google Scholar]
- 9.Jerschow E, Strizich G, Xue X, Hudes G, Spivack S, Persky V, et al. Effect of Relocation to the U.S. on Asthma Risk Among Hispanics. Am J Prev Med. 2017;52(5):579–88. doi: 10.1016/j.amepre.2016.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balcazar AJ, Grineski SE, Collins TW. The Hispanic health paradox across generations: the relationship of child generational status and citizenship with health outcomes. Public Health. 2015;129(6):691–7. doi: 10.1016/j.puhe.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carter-Pokras O, Zambrana RE, Yankelvich G, Estrada M, Castillo-Salgado C, Ortega AN. Health Status of Mexican-Origin Persons: Do Proxy Measures of Acculturation Advance our Understanding of Health Disparities? J Immigr Minor Health. 2008;10(6):475–88. doi: 10.1007/s10903-008-9146-2. [DOI] [PubMed] [Google Scholar]
- 12.Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165(3):359–69. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Calzada EJ, Sales A. Depression Among Mexican-Origin Mothers: Exploring the Immigrant Paradox. Cultural Diversity and Ethnic Minority Psychology. 2019(2):288–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(12):1226–33. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 15.Cagney KA, Browning CR, Wallace DM. The Latino paradox in neighborhood context: the case of asthma and other respiratory conditions. Am J Public Health. 2007;97(5):919–25. doi: 10.2105/AJPH.2005.071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinstein SM, Pugach O, Rosales G, Mosnaim GS, Walton SM, Martin MA. Family Chaos and Asthma Control. Pediatrics. 2019;144(2): e20182758. doi: 10.1542/peds.2018-2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feldman JM, Steinberg D, Kutner H, Eisenberg N, Hottinger K, Sidora-Arcoleo K, et al. Perception of pulmonary function and asthma control: the differential role of child versus caregiver anxiety and depression. J Pediatr Psychol. 2013;38(10):1091–100. doi: 10.1093/jpepsy/jst052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mosnaim GS, Weinstein SM, Pugach O, Rosales G, Roy A, Walton S, et al. Design and baseline characteristics of a low-income urban cohort of children with asthma: The Asthma Action at Erie Trial. Contemp Clin Trials. 2019;79:55–65. doi: 10.1016/j.cct.2019.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. In: National Heart L, and Blood Institute ed. Bethesda (MD) 2007. [Google Scholar]
- 20.Juniper EF, Gruffydd-Jones K, Ward S, Svensson K. Asthma Control Questionnaire in children: validation, measurement properties, interpretation. Eur Respir J. 2010;36(6):1410–6. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen JM, Holbrook JT, Wei CY, Gerald LB, Teague WG, Wise RA, et al. Validation and psychometric properties of the Asthma Control Questionnaire among children. J Allergy Clin Immunol. 2014;133(1):91–7 e1–6. doi: 10.1016/j.jaci.2013.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 23.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119(4):817–25. doi: 10.1016/j.jaci.2006.12.662. [DOI] [PubMed] [Google Scholar]
- 25.Vega JM, Badia X, Badiola C, López-Viña A, Olaguíbel JM, Picado C, et al. Validation of the Spanish Version of the Asthma Control Test (ACT). J Asthma. 2007; 44(10): 867–872. doi: 10.1080/02770900701752615. [DOI] [PubMed] [Google Scholar]
- 26.Rodríguez-Martínez CE, Melo-Rojas A, Restrepo-Gualteros SM, Sossa-Briceño MP, Nino G. Validation of the Spanish version of the childhood asthma control test (cACT) in a population of Hispanic children. J Asthma. 2014; 51(8): 855–862. doi: 10.3109/02770903.2014.921197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Ann. 2002;32(9):509–515. [Google Scholar]
- 28.Arrieta J, Aguerrebere M, Raviola G, Flores H, Elliott P, Espinosa A, et al. Validity and Utility of the Patient Health Questionnaire (PHQ)-2 and PHQ-9 for Screening and Diagnosis of Depression in Rural Chiapas, Mexico: A Cross-Sectional Study. J Clin Psychol. 2017; 73 (9)1076–1090. doi: 10.1002/jclp.22390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hahn EA, DeWalt DA, Bode RK, Garcia SF, DeVellis RF, Correia H, et al. and for the PROMIS Cooperative Group. New English and Spanish Social Health Measures Will Facilitate Evaluating Health Determinants. Health Psychol. 2014; 33(5): 490–499. doi: 10.1037/hea0000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000; 29: 470–477. [PubMed] [Google Scholar]
- 32.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002. May;(246):1–190. [PubMed] [Google Scholar]
- 33.VanderWeele TJ. Explanation in causal inference: methods for mediation and interaction. Oxford: Oxford University Press; 2015. [Google Scholar]
- 34.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014; 59(5), 1–38.26917999 [Google Scholar]
- 35.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010; 15(4): 309–34. doi: 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- 36.Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the Asthma Control Test. J Allergy Clin Immunol. 2009;124(4):719–23 e1. [DOI] [PubMed] [Google Scholar]
- 37.Hillemeier MM, Landale NS, Oropesa RS. Asthma in US Mexican-Origin Children in Early Childhood: Differences in Risk and Protective Factors by Parental Nativity. Acad Pediatr. 2015;15(4):421–9. doi: 10.1016/j.acap.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klinnert MD, Price MR, Liu AH, Robinson JL. Morbidity Patterns Among Low-Income Wheezing Infants. Pediatrics. 2003;112(1):49–57. doi: 10.1542/peds.112.1.49. [DOI] [PubMed] [Google Scholar]
- 39.Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–37. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- 40.Shalowitz MU, Mijanovich T, Berry CA, Clark-Kauffman E, Quinn KA, Perez EL. Context matters: a community-based study of maternal mental health, life stressors, social support, and children’s asthma. Pediatrics. 2006;117(5):e940–8. doi: 10.1542/peds.2005-2446. [DOI] [PubMed] [Google Scholar]
- 41.Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87(1):96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]


