Abstract
PURPOSE:
To evaluate and identify baseline factors associated with change in health-related quality of life (HRQOL) among patients with interstitial cystitis/bladder pain syndrome (IC/BPS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
METHODS:
A total of 191 men and 233 women with IC/BPS or CP/CPPS (collectively referred to as urologic chronic pelvic pain syndrome, or UCPPS) were followed for 12 months with bimonthly completion of the Short Form 12 (SF-12) to assess general mental and physical HRQOL, and with biweekly assessment of condition-specific HRQOL using the Genitourinary Pain Index. A functional clustering algorithm was used to classify participants as improved, stable, or worsened for each HRQOL measure. Ordinal logistic regression was used to determine baseline factors associated with change.
RESULTS:
Physical HRQOL improved in 22% of the participants, mental HRQOL improved in 25%, and condition-specific HRQOL improved in 47%. Better baseline physical HRQOL, older age, and the presence of non-urologic symptoms were associated with lower likelihood of improvement in physical HRQOL. Better baseline mental HRQOL, female sex, and greater baseline depression and stress were associated with lower likelihood of improvement in mental HRQOL. Better baseline condition-specific HRQOL and more severe baseline UCPPS pain symptoms were associated with lower likelihood of improvement in condition-specific HRQOL.
CONCLUSION:
While several non-UCPPS factors influenced the trajectory of general HRQOL over time, only condition-specific baseline HRQOL and UCPPS symptoms were associated with UCPPS-specific HRQOL change. Significant differences in how UCPPS impacts various aspects of HRQOL suggest a multidisciplinary approach to assessment and treatment of these patients.
MeSH: Interstitial cystitis, bladder pain syndrome, chronic prostatitis, bother
Brief Descriptive Running head
Quality of life change in urologic chronic pelvic pain syndrome
Introduction
Interstitial cystitis/bladder pain syndrome (IC/BPS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) are common and debilitating urologic pain conditions. IC/BPS is characterized by bladder pain, with symptoms that typically worsen with bladder filling and/or relieved by urination. CP/CPPS is characterized by male pelvic pain, which is localized to the perineum, genitalia, or suprapubic region. These two conditions share many similarities1,2, and can be collectively referred to as ‘urologic chronic pelvic pain syndrome (UCPPS)’3. Numerous cross-sectional studies have documented the dramatic impact of UCPPS symptoms on health-related quality of life (HRQOL)4–7. No studies, however, have evaluated changes in HRQOL prospectively among patients with UCPPS. Both generic and illness specific measures were used to examine illness impact on individuals’ HQOL. Generic measures provide data related to a wide array of physical and mental functioning and can be used to compare across chronic conditions, while disease-specific measures focus on areas of common symptoms for a particular disorder and are used to measure the efficacy of interventions and treatments8. Utilizing data from UCPPS participants enrolled in the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network’s Epidemiology and Phenotyping Study (EPS)9, we assessed general HRQOL and UCPPS disease-specific HRQOL over a 12-month period. We examined potential demographic, disease-related, and psychosocial characteristics that might be correlated with HRQOL change.
Methods
The MAPP Research Network consists of 6 Discovery Sites which recruit UCPPS participants into research studies, a Data Core, and a Tissue and Technology Core3. The study design, eligibility criteria and aims of the MAPP EPS protocol have been previously described9. A total of 191 male and 233 female participants with UCPPS were followed for one year and received usual care for their UCPPS symptoms. After an intensive baseline phenotyping evaluation, abridged in-person follow-up assessments were conducted at 6 and 12 months. Participants also completed a comprehensive battery of online questionnaires every 2 months, and a brief online questionnaire every 2 weeks.
Measurement of HRQOL
General HRQOL was evaluated bimonthly using the Medical Outcomes Study 12-item Short Form Health Survey (SF-12)10–13. The SF-12 comprises eight domains of health status: physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, energy/vitality, social functioning, role limitations due to emotional problems, and mental health. The SF-12 yields composite scores for physical functioning (PCS) and mental functioning (MCS) each ranging from 0–100, with higher scores indicating better functioning.
UCPPS condition-specific HRQOL was assessed biweekly using the QOL subscale of the Genitourinary Pain Index (GUPI)14. The GUPI is used to assess pelvic pain symptoms, urinary symptoms, and HRQOL in both men and women. The GUPI QOL subscale includes 3 items which are combined into a single QOL subscale score, ranging from 0–12, with higher scores indicating worse condition-specific HRQOL. The GUPI QOL items ask: ‘How much have your symptoms kept you from doing the kinds of things that you would usually do, over the last week?’ (None - 0, Only a little - 1, Some - 2, A lot - 3), ‘How much did you think about your symptoms, over the last week?’ (None - 0, Only a little - 1, Some - 2, A lot - 3), and ‘If you were to spend the rest of your life with your symptoms just the way they have been during the last week, how would you feel about that?’ (Delighted - 0, Pleased - 1, Mostly satisfied - 2, Mixed (about equally satisfied and dissatisfied) - 3, Mostly dissatisfied - 4, Unhappy - 5, Terrible - 6).
Other demographic and symptom variables
Additional variables assessed at baseline included: the baseline value of the respective HRQOL score, sex, age, composite UCPPS pain severity score15, composite UCPPS urinary symptom severity score15, UCPPS symptom duration, pain catastrophizing score (using the Coping Strategies Questionnaire)16, anxiety and depression (using the Hospital Anxiety and Depression Scale (HADS)17), perceived life stress (using the Perceived Stress Scale (PSS)18,19), sleep disturbance (using the NIH Patient Reported Outcomes Measurement Information System (PROMIS)20 questionnaire), degree of non-urological symptoms (using the Complex Multi-Symptom Inventory (CMSI)21), and spatial distribution of pain (using the sum of pain locations marked on a standardized body map)22,23.
Longitudinal HRQOL
A functional clustering procedure was applied to the three longitudinal HRQOL scores (SF-12 PCS, SF-12 MCS, and GUPI QOL) to classify the overall HRQOL trajectory for each participant as worsening, stable, or improving over the 52-week study period2. To decrease the influence of study entry effects (regression to the mean) on outcome classification, the first month of HRQOL scores were not used in the clustering algorithm24, and the HRQOL scores at study week 4 were used as the baseline values. Therefore, the maximum number of possible SF-12 scores (bimonthly) for analysis was 7, and the maximum number of GUPI QOL scores (biweekly) was 23. The analysis was limited to participants who completed the baseline assessment and at least one post-baseline assessment (n=376 for SF-12 and n=395 for GUPI QOL).
Statistical Analysis
Unadjusted and adjusted ordinal logistic regression models were used to determine baseline factors that were associated with change in each of the three HRQOL measures. For each analysis an odds ratio (OR) greater than 1 indicated a greater likelihood of HRQOL improvement (i.e., likelihood of being stable vs. worse, or improved vs. stable) with higher values of the given baseline characteristic; conversely, an OR <1 indicates a lower likelihood of improvement with higher values. Unadjusted models included baseline HRQOL and the indicated demographic or symptom measure. Adjusted models included all variables.
Results
For the SF-12, the mean number of bimonthly contacts per participant was 5.4, and 75% of participants completed at least 4 of the 7 contacts. For the GUPI, the mean number of biweekly contacts per participant was 15.8, and 73% completed at least 12 of the 23 contacts. Figure 1 shows the individual HRQOL trajectories by cluster, overlaid by the average HRQOL trajectory within the cluster. Physical HRQOL improved in 83 participants (22%), and worsened in 116 (30%). Mental HRQOL improved in 96 participants (25%), and worsened in 116 (30%). Condition-specific HRQOL improved in 187 participants (47%), and was stable/worsened in 208 (53%). Figure 2 is a Venn diagram which shows the overlap in participants who demonstrated improvement in any of the three HRQOL domains. There were 121 participants who did not improve in any of the categories, while only 14 improved in all three. A total of 32 participants improved only in the SF-12 PCS, while 36 participants improved only in the SF-12 MCS, and 100 participants improved only in the GUPI QOL assessment.
Figure 1.
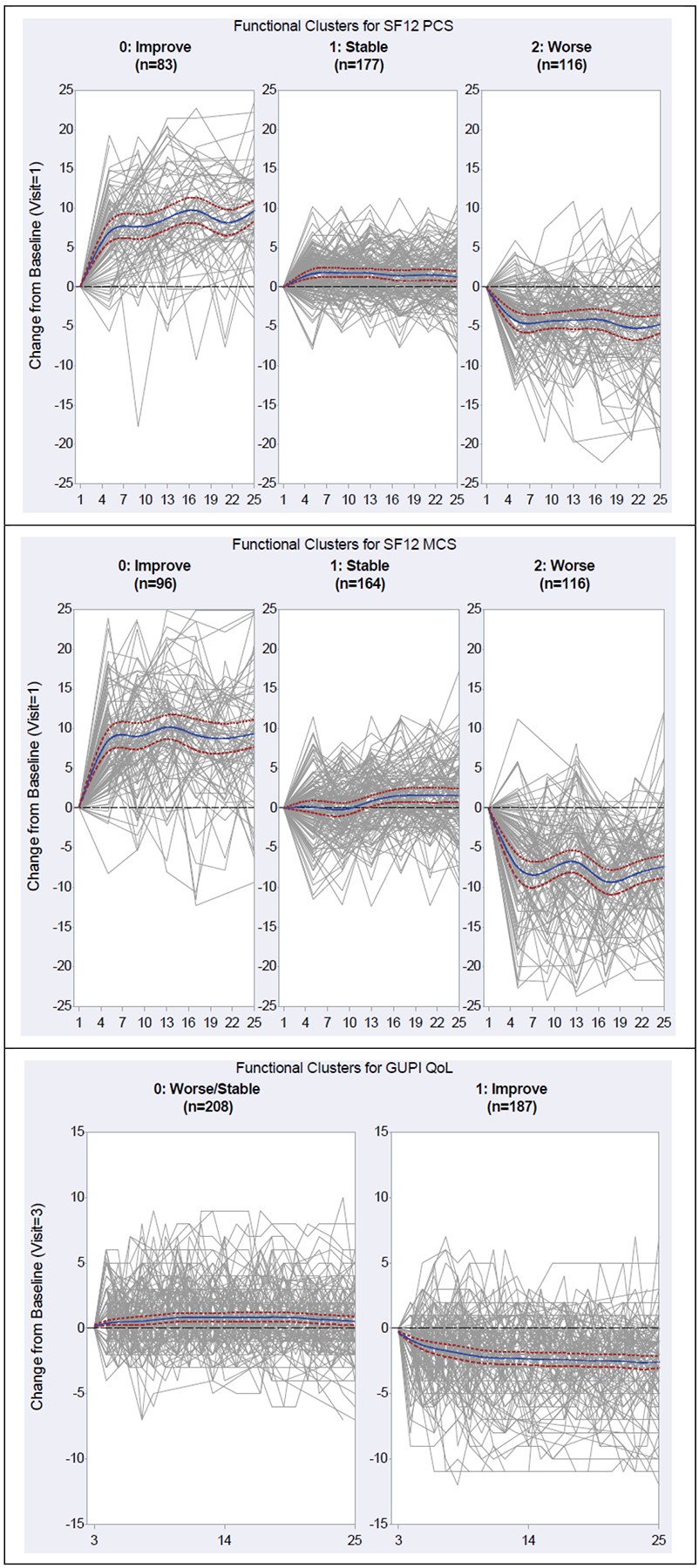
Functional clustering of participants based on longitudinal HRQOL ratings (in grey), classified into one of three clusters (Improved, Stable, Worse). Clustering was done separately for SF-12 PCS score (top), SF-12 MCS score (middle) and GUPI QOL subscale score (bottom). For the GUPI QOL scale, the analysis resulted in only two clusters (Stable vs Improved). Blue lines show the mean HRQOL scores for each cluster, and red lines show the 95% confidence interval for these mean values.
Figure 2.
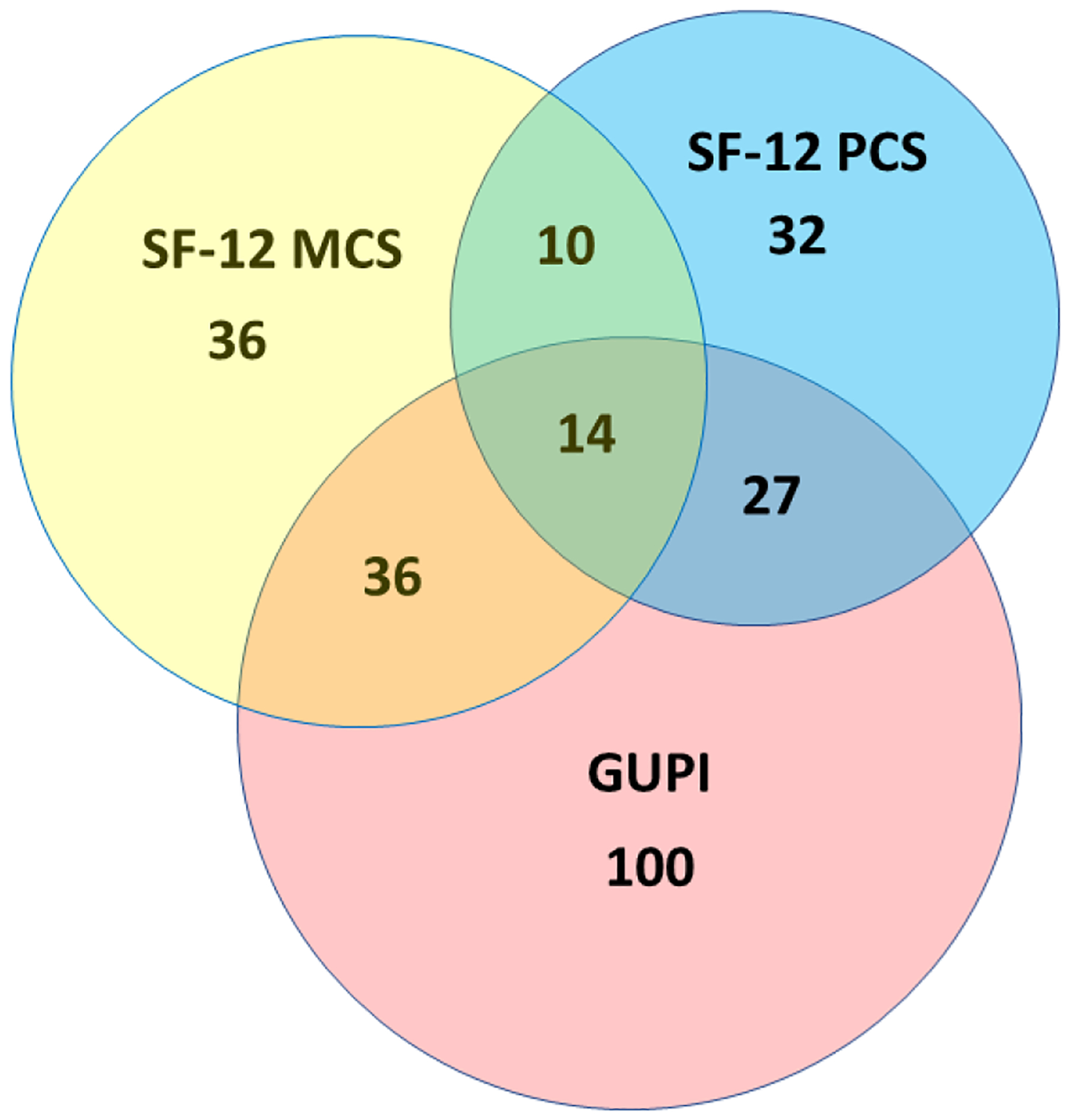
Overlap of HRQOL Improvement.
Results of the regression models are presented in Tables 1–3. Baseline HRQOL score was a strong predictor of HRQOL outcomes across all categories (C-statistic >0.7 SF-12 MCS and PCS; C-statistic=0.67 GUPI). Specifically, worse baseline physical HRQOL was associated with a greater likelihood of physical HRQOL improvement, worse baseline mental HRQOL was associated with a greater likelihood of mental HRQOL improvement, and worse baseline UCPPS condition-specific HRQOL was associated with a greater likelihood of condition-specific HRQOL improvement.
Table 1.
Association of baseline characteristics with change in physical health-related quality of life
| SF-12 PCS | n | Unadjusted1 | Adjusted2 | ||
|---|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | ||
| 0.914 (0.895–0.933) | <0.0001 | 0.892 (0.869–0.915) | <0.0001 | ||
| Sex (Female) | 376 | 0.724 (0.483–1.087) | 0.12 | 0.730 (0.476–1.119) | 0.15 |
| UCPPS Pain Score | 376 | 0.995 (0.957–1.034) | 0.80 | 0.997 (0.957–1.038) | 0.87 |
| UCPPS Urinary Symptom Score | 375 | 0.984 (0.951–1.018) | 0.34 | 0.991 (0.957–1.026) | 0.61 |
| Increased Age (per decade) | 376 | 0.894 (0.787–1.015) | 0.08 | 0.866 (0.760–0.987) | 0.0306 |
| Symptom Duration (per 5 years) | 368 | 0.950 (0.865–1.044) | 0.29 | 1.003 (0.906–1.111) | 0.95 |
| Catastrophizing Score | 374 | 1.011 (0.986–1.036) | 0.39 | 1.005 (0.979–1.031) | 0.73 |
| Depression Score | 374 | 0.971 (0.921–1.023) | 0.27 | 0.976 (0.923–1.031) | 0.38 |
| Anxiety Score | 374 | 0.988 (0.945–1.032) | 0.58 | 0.994 (0.948–1.043) | 0.81 |
| Perceived Stress | 373 | 0.987 (0.961–1.014) | 0.34 | 0.989 (0.960–1.019) | 0.49 |
| Sleep Disturbance Score | 375 | 0.977 (0.950–1.004) | 0.09 | 0.982 (0.954–1.011) | 0.22 |
| Non-Urologic Medical Symptoms | 374 | 0.947 (0.915–0.980) | 0.0018 | 0.958 (0.922–0.996) | 0.0300 |
| Body Map Sites | 376 | 0.846 (0.757–0.946) | 0.0033 | 0.899 (0.793–1.020) | 0.10 |
Includes baseline SF-12 PCS
Includes: baseline SF-12 PCS, Age, Non-Urologic Medical Symptoms, and Body Map Sites
Note: An Odds Ratio (OR) <1.0 indicates that this variable predicts a lower likelihood of HRQOL improvement
Table 3.
Association of baseline characteristics with change in UCPPS condition-specific health-related quality of life
| GUPI QOL Subscale | n | Unadjusted1 | Adjusted2 | ||
|---|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | ||
| 1.242 (1.154–1.336) | <0.0001 | 1.382 (1.257–1.518) | <0.0001 | ||
| Sex (Female) | 395 | 0.618 (0.405–0.946) | 0.0265 | 0.682 (0.442–1.053) | 0.08 |
| UCPPS Pain Score | 395 | 0.908 (0.867–0.952) | <0.0001 | 0.913 (0.870–0.957) | 0.0002 |
| UCPPS Urinary Symptom Score | 394 | 0.942 (0.906–0.979) | 0.0025 | 0.972 (0.931–1.015) | 0.19 |
| Age (per decade) | 395 | 1.026 (0.895–1.177) | 0.71 | 0.964 (0.834–1.115) | 0.62 |
| Symptom Duration (per 5 years) | 387 | 0.965 (0.874–1.065) | 0.48 | 0.975 (0.881–1.080) | 0.63 |
| Catastrophizing Score | 393 | 0.975 (0.948–1.002) | 0.07 | 0.988 (0.959–1.017) | 0.40 |
| Depression Score | 393 | 0.993 (0.937–1.053) | 0.82 | 1.007 (0.948–1.069) | 0.83 |
| Anxiety Score | 393 | 1.027 (0.978–1.079) | 0.29 | 1.038 (0.987–1.092) | 0.15 |
| Perceived Stress | 392 | 1.003 (0.975–1.033) | 0.81 | 1.011 (0.981–1.041) | 0.49 |
| Sleep Disturbance Score | 394 | 0.979 (0.950–1.008) | 0.15 | 0.995 (0.964–1.026) | 0.73 |
| Non-Urologic Medical Symptoms | 393 | 0.971 (0.940–1.002) | 0.07 | 0.989 (0.956–1.023) | 0.52 |
| Body Map Sites | 395 | 0.954 (0.885–1.066) | 0.41 | 0.986 (0.879–1.106) | 0.81 |
Includes baseline GUPI QOL
Includes: baseline GUPI QOL, Sex, and UCPPS Pain Score
Note: An Odds Ratio (OR) <1.0 indicates that this variable predicts a lower likelihood of HRQOL improvement
For physical HRQOL (Table 1), the unadjusted analysis showed that the presence of increased non-urologic medical symptoms and widespread pain on the body map were associated with a lower HRQOL improvement over time. The multivariable adjusted analysis found that the presence of non-urologic symptoms remained associated, while increased age also emerged as associated with a lower likelihood of improvement.
For mental HRQOL (Table 2), almost all variables were associated with symptom trajectory in unadjusted analysis. Female sex, more severe baseline pain and urinary scores, catastrophizing, depression, anxiety, stress, non-urologic symptoms, and widespread pain were all associated with a lower likelihood of mental HRQOL improvement. After adjustment, only female sex, depression, and stress were independently associated with changes in mental HRQOL.
Table 2.
Association of baseline characteristics with change in mental health-related quality of life
| SF-12 MCS | n | Unadjusted1 | Adjusted2 | ||
|---|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | ||
| 0.905 (0.885–0.925) | <0.0001 | 0.831 (0.800–0.863) | <0.0001 | ||
| Sex (Female) | 376 | 0.556 (0.372–0.830) | 0.0041 | 0.580 (0.380–0.885) | 0.0115 |
| UCPPS Pain score | 376 | 0.960 (0.924–0.997) | 0.0361 | 0.981 (0.941–1.023) | 0.38 |
| UCPPS Urinary Symptom score | 375 | 0.961 (0.930–0.993) | 0.0175 | 0.987 (0.952–1.024) | 0.49 |
| Age (per decade) | 376 | 1.138 (0.993–1.304) | 0.06 | 1.115 (0.963–1.290) | 0.14 |
| Symptom duration (per 5 years) | 368 | 0.943 (0.859–1.036) | 0.23 | 0.962 (0.872–1.060) | 0.43 |
| Catastrophizing Score | 374 | 0.958 (0.932–0.985) | 0.0022 | 0.996 (0.966–1.028) | 0.81 |
| Depression Score | 374 | 0.863 (0.806–0.924) | <0.0001 | 0.907 (0.840–0.980) | 0.0130 |
| Anxiety Score | 374 | 0.910 (0.860–0.963) | 0.0010 | 0.985 (0.918–1.057) | 0.67 |
| Perceived Stress | 373 | 0.907 (0.873–0.942) | <0.0001 | 0.932 (0.894–0.972) | 0.0010 |
| Sleep Disturbance Score | 375 | 0.948 (0.921–0.975) | 0.0002 | 0.974 (0.945–1.004) | 0.09 |
| Non-Urologic Medical Symptoms | 374 | 0.955 (0.927–0.985) | 0.0033 | 0.999 (0.965–1.035) | 0.97 |
| Body Map Sites | 376 | 0.871 (0.784–0.968) | 0.0105 | 0.949 (0.848–1.062) | 0.37 |
Includes baseline SF12 MCS
Includes: baseline SF12 MCS, Sex, Depression Score, Perceived Stress, and Sleep Disturbance Score
Note: An Odds Ratio (OR) <1.0 indicates that this variable predicts a lower likelihood of HRQOL improvement
For condition-specific HRQOL (Table 3), more severe baseline UCPPS pain and urinary scores and female sex were associated with less favorable HRQOL trajectory in univariable analysis. After adjustment, only the UCPPS pain score was independently associated with condition-specific HRQOL change.
Discussion
Like most chronic pain conditions, UCPPS is a non-lethal but potentially debilitating disorder for which effective treatments are lacking. Optimal management involves an individualized approach that focuses on patient well-being as well as reducing the UCPPS symptoms. Maximizing quality of life (the ability to function despite the UCPPS symptoms) is perhaps equally important as pain control. This is the first study to prospectively assess HRQOL over time in a group of men and women with UCPPS. Over 12 months, general HRQOL status (mental and physical) was stable in about 45–50% of participants, improved in about 25%, and worsened in about 30%. UCPPS-specific HRQOL improved in 47% and was stable or worsened in 53%. The greater proportion with improvement in UCPPS-specific HRQOL (as opposed to general HRQOL) may reflect the fact that study participants were recruited from UCPPS referral sites and were receiving ongoing UCPPS treatments during the study time period, while other concomitant health conditions may have received less attention.
Poorer initial HRQOL predicted greater improvement across all three categories. This may in part be due to regression to the mean or the result of some patients volunteering for the study during a period of particularly high symptoms and problems which decreased over the course of the study. The analysis of HRQOL predictors also emphasizes important differences across the HRQOL domains. Overall, higher levels of baseline problems most connected to the domain seemed to be the best predictors of declining outcome on that domain after controlling for initial HRQOL levels.
Worsening physical HRQOL outcome was associated with the presence of more widespread pain and greater non-urologic symptoms. These findings highlight the importance of recognizing and tracking generalized physical symptoms in UCPPS patients so that treatments for these symptoms may be offered or adjusted. Worsening HRQOL outcomes were also associated with increasing participant age. It is likely that this association is due to the presence of additional comorbidities in elderly patients, rather than specific UCPPS factors. This would explain why increased age was associated with less improvement in general HRQOL, while age was not associated with UCPPS-specific HRQOL trajectory.
Mental HRQOL outcomes were impacted by almost all measured variables including female sex, baseline UCPPS symptoms, widespread pain, non-urologic medical symptoms, and all measured psychosocial variables. Stress, depression, and female sex remained independently associated with poorer HRQOL outcomes after multivariable analysis. These findings primarily highlight the impact of psychosocial factors on the HRQOL of UCPPS patients. Clinicians who treat UCPPS should involve mental health care in the management of patients who exhibit symptoms of depression, stress, or poor coping.
As noted above, condition-specific HRQOL improved in almost 50% of participants. Very few of the examined variables, however, correlated with UCPPS HRQOL trajectory. Worse baseline UCPPS symptoms were associated with less favorable outcomes, while psychosocial variables and degree of widespread pain/symptoms were not associated. These findings reinforce the need for more effective UCPPS treatment approaches, as improved HRQOL is clearly tied to UCPPS symptom reduction.
These results can be compared with a previous MAPP study that used similar statistical methods to assess predictors of UCPPS symptom change over 12 months2. In that study, the primary predictors of declining UCPPS symptoms were the presence of widespread pain, greater non-urologic symptoms, and poorer overall health, while psychosocial variables had a minimal impact. Taken together, the findings provide empiric evidence that optimal outcomes require a reduction in UCPPS symptoms, widespread/nonurologic pain, and psychosocial symptoms.
The MAPP cohort study provides an enormous amount of prospective data with a very high retention rate, but the follow-up period was limited to 12 months. Therefore, any changes/trends were relatively short-term in nature, especially for a chronic disorder like UCPPS. Study participants, however, reported a broad range of symptom duration (range 1–54 years, mean 8 years)25, and the association between symptom duration and our HRQOL outcomes was not significant, suggesting that these findings may be applicable with longer-term follow-up. We also acknowledge that this was a ‘treated natural history’ study, in which UCPPS participants received usual care for their symptoms. These treatments may have varied considerably across providers and treatment sites. Individual treatment regimens were not closely tracked in this study, and therefore we are not able to correlate specific treatments with HRQOL data. A second MAPP cohort study is underway which will address some of these limitations. In this second study, participants will be followed for a longer time period (up to 3 years), and UCPPS treatment details will be collected longitudinally so that specific treatments effects can be correlated with individual participant phenotypes.
Conclusions
Over 1 year, nearly half of the participants demonstrated improved UCPPS-specific HRQOL while only a quarter showed improved general HRQOL. Poorer initial HRQOL predicted greater improvement across all three categories. Greater UCPPS pain predicted worse improvement in UCPPS-specific HRQOL while higher non-urological pain and stress predicted general physical and mental HRQOL, respectively. Additional research with longer follow-up is necessary to better understand the complexity of factors associated with improvement in UCPPS-specific HRQOL.
Funding
Funding for the MAPP Research Network was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (NIH) (DK82370, DK82342, DK82315, DK82344, DK82325, DK82345, DK82333, and DK82316.). In addition, this work was supported in part by: R01 DK117208 (stats methods grant).
Abbreviations
- CP/CPPS
Chronic Prostatitis/Chronic Pelvic Pain Syndrome
- EPS
Epidemiology and Phenotyping Study
- GUPI
Genitourinary Pain Index
- HRQOL
Health Related Quality Of Life
- IC/BPS
Interstitial Cystitis/Bladder Pain Syndrome
- MAPP
Multidisciplinary Approach to the Study of Chronic Pelvic Pain
- MCS
Mental Functioning
- PCS
Physical Functioning
- QOL
Quality of Life
- SP-12
Short Form Health Survey
- UCPPS
Urologic Chronic Pelvic Pain Syndrome
References
- 1.Suskind AM, Berry SH, Ewing BA, Elliott MN, Suttorp MJ, Clemens JQ. The prevalence and overlap of interstitial cystitis/bladder pain syndrome and chronic prostatitis/chronic pelvic pain syndrome in men: results of the RAND Interstitial Cystitis Epidemiology male study. J Urol. 2013;189(1):141–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naliboff BD, Stephens AJ, Lai HH, et al. Clinical and Psychosocial Predictors of Urological Chronic Pelvic Pain Symptom Change in 1 Year: A Prospective Study from the MAPP Research Network. J Urol. 2017;198(4):848–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clemens JQ, Mullins C, Kusek JW, et al. The MAPP research network: a novel study of urologic chronic pelvic pain syndromes. BMC Urol. 2014;14:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McNaughton Collins M, Pontari MA, O’Leary MP, et al. Quality of life is impaired in men with chronic prostatitis: the Chronic Prostatitis Collaborative Research Network. J Gen Intern Med. 2001;16(10):656–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tripp DA, Curtis Nickel J, Landis JR, Wang YL, Knauss JS, Group CS. Predictors of quality of life and pain in chronic prostatitis/chronic pelvic pain syndrome: findings from the National Institutes of Health Chronic Prostatitis Cohort Study. BJU Int. 2004;94(9):1279–1282. [DOI] [PubMed] [Google Scholar]
- 6.Michael YL, Kawachi I, Stampfer MJ, Colditz GA, Curhan GC. Quality of life among women with interstitial cystitis. J Urol. 2000;164(2):423–427. [PubMed] [Google Scholar]
- 7.Suskind AM, Berry SH, Suttorp MJ, et al. Health-related quality of life in patients with interstitial cystitis/bladder pain syndrome and frequently associated comorbidities. Qual Life Res. 2013;22(7):1537–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27(3 Suppl):S217–232. [DOI] [PubMed] [Google Scholar]
- 9.Landis JR, Williams DA, Lucia MS, et al. The MAPP research network: design, patient characterization and operations. BMC Urol. 2014;14(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ware JE Jr., Phillips J, Yody BB, Adamczyk J. Assessment tools: functional health status and patient satisfaction. Am J Med Qual. 1996;11(1):S50–53. [PubMed] [Google Scholar]
- 11.Ware JE Jr.. Patient-based assessment: tools for monitoring and improving healthcare outcomes. Behav Healthc Tomorrow. 1996;5(3):88, 87. [PubMed] [Google Scholar]
- 12.Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 13.Diaz-Arribas MJ, Fernandez-Serrano M, Royuela A, et al. Minimal Clinically Important Difference in Quality of Life for Patients With Low Back Pain. Spine (Phila Pa 1976). 2017;42(24):1908–1916. [DOI] [PubMed] [Google Scholar]
- 14.Clemens JQ, Calhoun EA, Litwin MS, et al. Validation of a modified National Institutes of Health chronic prostatitis symptom index to assess genitourinary pain in both men and women. Urology. 2009;74(5):983–987, quiz 987 e981–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffith JW, Stephens-Shields AJ, Hou X, et al. Pain and urinary symptoms should not be combined into a single score: psychometric findings from the MAPP Research Network. J Urol. 2016;195(4P1):949–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenstiel AK, Keefe FJ. The Use of Coping Strategies in Chronic Low-Back-Pain Patients - Relationship to Patient Characteristics and Current Adjustment. Pain. 1983;17(1):33–44. [DOI] [PubMed] [Google Scholar]
- 17.Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed). 1986;292(6516):344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 19.Cohen S, Williamson G. Perceived stress in a probability sample of the United States In: Spacapan S, Oskamp S, eds. The social psychology of health:Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 20.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams DA, Schilling S. Advances in the assessment of fibromyalgia. Rheum Dis Clin North Am. 2009;35(2):339–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tripp DA, Nickel JC, Wong J, et al. Mapping of pain phenotypes in female patients with bladder pain syndrome/interstitial cystitis and controls. Eur Urol. 2012;62(6):1188–1194. [DOI] [PubMed] [Google Scholar]
- 23.Lai HH, Jemielita T, Sutcliffe S, et al. Characterization of Whole Body Pain in Urological Chronic Pelvic Pain Syndrome at Baseline: A MAPP Research Network Study. J Urol. 2017;198(3):622–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stephens-Shields AJ, Clemens JQ, Jemielita T, et al. Symptom Variability and Early Symptom Regression in the MAPP Study: A Prospective Study of Urological Chronic Pelvic Pain Syndrome. J Urol. 2016;196(5):1450–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clemens JQ, Clauw DJ, Kreder K, et al. Comparison of baseline urological symptoms in men and women in the MAPP research cohort. J Urol. 2015;193(5):1554–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]


