Abstract
Background/Objectives
Studies show that in nursing homes (NHs) the prevalence of moderate-to-severe obesity has doubled in the last decade, and continues to increase. Obese residents are often complex and costly, and this increase in prevalence has come at a time when NHs struggle to decrease hospitalizations, particularly those that are potentially avoidable. This study examined the association between obesity and hospitalizations.
Design
We linked 2011–2014 national data using Medicare NH assessments, hospital claims, and the NH Compare.
Setting & Participants
Individuals age 65+, newly admitted to NHs, who became long-term residents between July 1st, 2011 and March 26th, 2014. The analytical sample included 490,086 residents.
Methods
NH-originating hospitalization was the outcome; a categorical variable defined as no hospitalization, potentially avoidable hospitalization (PAH) and other hospitalization (non-PAH). The main independent variable was body mass index (BMI) defined as normal weight (30>BMI>= 18.5kg/m2), mildly obese (35>BMI>=30kg/m2) or moderately-to-severely obese (BMI>=35kg/m2). Covariates included individual and NH characteristics. Multinomial models with NH random effects and state dummies were estimated.
Results
After adjusting for individual level covariates, the risk of non-PAH for the mildly and moderate/severely obese was not different from normal weight residents. But the risk of PAH remained significantly higher for the moderate/severely obese (RRR=1.055;95%CI 1.018,1.094). Several NH-level factors also influenced hospitalization risk.
Conclusions and Implications
Obese residents are more likely to experience PAH but not non-PAH. Efforts to improve care for these residents may need to broadly consider NHs’ ability to commit additional resources to fully integrate care for this growing segment of the population.
Keywords: obesity, potentially avoidable hospitalizations, nursing home
Brief summary
Obese nursing home residents are more likely to experience potentially avoidable hospitalizations than their non-obese counterparts. Caring for obese residents may place higher resource demands on nursing home resources.
Introduction
The prevalence of obesity among Americans age 65 and older exceeds 35% and is growing.1,2 In this age group, obesity is associated with greater functional decline, increased morbidity, higher hospitalization rates, longer length of stay, and increased risk of nursing home (NH) admissions.3,4 Recent studies have shown that in NHs the prevalence of moderate-to-severe obesity (Body Mass Index [BMI] >=35) has increased from 14.7% to 23.9% between 2000 and 2010,5 and to 28% in 2015.6
The increase in prevalence of obese residents whose care needs are often complex and costly7 comes at a time when NHs are increasingly struggling to decrease hospital readmissions8,9 and to reduce potentially avoidable hospitalizations.10 To date only two studies have examined the relationship between obesity and hospitalizations of NH residents. A study of patients with hip fracture receiving post-acute care in a skilled nursing facility (SNF) found obesity to be associated with increased readmission risk.11 Another recent study focusing on the general population of newly admitted SNF residents found the association between obesity and hospital readmissions to be complex and to vary by age and type of index hospitalization.12
These studies have suggested that care specifically targeted to obese residents may be needed to reduce readmissions in this vulnerable population. Others have pointed out that accommodating care needs of obese residents may require NHs to invest resources in special equipment, architectural modifications13,14, and staffing15,16, all of which are costly and difficult to achieve for most facilities. Without such accommodations, NHs may find it difficult not only to reduce hospital readmissions among obese residents, but they may also be less able to prevent or manage clinical conditions that result in otherwise potentially avoidable hospitalizations (PAH).
Our objective was to examine the association between obesity and PAH among long-stay NH residents. Because obesity-related accommodations are likely to be very infrequent in NHs, we hypothesized that obese long-stay residents experience significantly higher risk of PAH compared to residents of normal weight.
Methods
Data Sources
We used the following national data sets for CY2010–2014: Medicare Master Beneficiary Summary File (MBSF); Minimum Data Set (MDS) 3.0; Medicare Provider and Analysis Review (MedPAR) file; and Nursing Home Compare (NHC). The MDS is a federally mandated, comprehensive, clinical assessment database of all nursing home residents in Medicare or Medicaid certified NHs. The assessments are conducted at admission, quarterly, annually, when there is a significant change in health status, and at discharge. These assessments capture detailed information about residents’ socio-demographics, weight and height, comorbidities, health status, and other factors. We used the MBSF to identify individuals who were dually entitled for Medicare and Medicaid, excluding enrollees of Medicare Advantage plans for whom hospitalization data may not be complete.17 MedPAR was used to track inpatient admissions, and information on facility-level characteristics was obtained from the NHC. The Medicare beneficiary and provider identifiers were used to merge these databases.
The study protocol was reviewed and approved by the Institutional Research and Subjects Review Board.
Study Population
We first identified a cohort of Medicare fee-for-service (FFS) enrollees, age 65 or older who were newly admitted to free-standing NHs between January 1, 2011 and March 26, 2014, and became long-term residents (N=565,592). New admissions were defined for individuals who did not have any NH stays during the 180 days preceding their index admission (2010 data were used to track prior NH use and to identify new 2011 admissions). Admissions occurring after March 26, 2014 were truncated to allow for the follow-up period (180 days after starting long-stay status). Among the newly admitted only those who became long-stayers were included in the study population. Long-stay NH residents were defined as those whose care episode was at least 100 days, with the long-stay status beginning at 101st day of the episode.
We excluded underweight residents, body mass index (BMI) lower than 18.5 (N=47,219 or 8.3%), as they may have substantially different risks for being hospitalized. Also excluded were residents with missing BMIs (N=4,189 or 0.7%). After excluding observations with missing covariate values (N=24,098 or 4.3%) the final analytical sample included 490,086 (87%) of the long-stay residents admitted to 14,469 NHs.
Outcome Variables
We focused on two categorical outcomes, risk of hospitalizations deemed to be potentially avoidable (PAH) and risk of all other hospitalizations (non-PAH). Following the definition of PAH developed by RTI international,18 and recently used by CMS in their evaluation of the Initiative to Reduce Potentially Avoidable Hospitalizations,10 we focused on 17 conditions (Appendix) deemed as potentially manageable/preventable.19
Independent Variables
We used the MDS assessment closest to the date of becoming a long-stay resident as the index assessment for defining the obesity category and for all other individual covariates. Following the definition of the WHO, residents were categorized as non-obese (30>BMI>=18.5kg/m2), mildly obese (35>BMI>=30kg/m2), or moderate-to-severely obese (BMI>=35kg/m2).
Because conditions defined as PAH are based on diagnoses alone, and do not reflect the severity of illness, we also controlled for individual factors that manifest residents’ health condition and comorbidities. For example, we identified whether NH admission was post-acute or directly from the community. Functional status was measured by the level of Activities of Daily Living (ADL) impairments (score from 0-to-28).20 Cognitive Function Scale (CFS) measured cognitive impairment on a scale from intact to severely impaired.21 We controlled for co-morbid conditions and socio-demographic characteristics.12
We controlled for NH-level factors such as bed-size, percent of residents covered by Medicare and Medicaid, profit status, chain affiliation, nursing staffing levels (hours/resident/day), facility prevalence of obesity, and overall CMS star-rating. We also controlled for the year in which a resident became a long-stayer in order to account for any unobserved secular trends.
Statistical analyses
We first compared resident characteristics by obesity status. Chi-square and t-tests were employed for statistical inference. We then fit multinomial logistic regression models with NH random-effects and state dummies to explore the relationship between obesity and the risk of PAH and non-PAH. For each outcome three models were estimated. First, we estimated simple multinomial logit models with NH random-effect and state dummies (to control for state policies influencing hospitalizations) without adjusting for other covariates, in order to capture the overall relationship between obesity and NH-originating hospitalizations. We then estimated the second model to account for individual level covariates that may help to differentiate the effect of illness severity and comorbidities. In the third model we included both individual and NH-level characteristics as risk-adjustors. Normal weight residents were included as the reference group in all analyses. Analyses were performed using SAS, version 9.4@ (SAS Institute, Inc. Cary, NC), and STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP.).
Results
Our study cohort included 490,086 newly admitted, long-stay residents who experienced a total of 101,187 hospitalizations. Almost half (45%) of all hospitalizations were identified as potentially avoidable (Appendix). Regardless of the obesity status, the five most common conditions for PAH were pneumonia, falls and/or trauma, urinary tract infection, congestive heart failure (CHF), and dehydration; but the distribution of these conditions varied substantially with obesity. For example, while falls/trauma were common among the normal weight residents (20.2%), they were experienced at much lower rates among the mildly and moderate/severely obese (11.0% & 6.9%, respectively). On the other hand, CHF was most common among the moderate/severely obese (22.2%) but less so among the normal weight (14.8%).
Residents with moderate/severe obesity were more likely than those of normal weight to have any hospitalizations (23.5% vs. 20.2%), and had higher unadjusted rates of PAH (46.9% vs. 44.8%) (Table 1). Compared to normal weight, obese residents were younger, female, and with a higher proportion of blacks. They were much more likely to be Medicaid eligible (54.5% of moderate/severely obese, compared to 47.8% of mildly obese, and 41.8% among normal weight). Obese residents were more likely than those of normal weight to be cognitively intact (35.2% for the mildly and 49.9% for the moderate/severely obese vs. 25.2% for normal weight), but had substantially higher rates of co-morbidities such as hypertension, diabetes, and heart failure (for moderate/severely obese).
Table 1:
Descriptive Characteristics of the Study Population: By Obesity Status
| Characteristics | Normal weight N=380,650 (77.7%) | Mild obesity N=65,250 (13.3%) | Moderate/severe obesity N=44,186 (9.0%) |
|---|---|---|---|
| Hospitalizations | |||
| Pct. of residents with any hospitalization | 20.2% | 21.3%*** | 23.5%*** |
| Pct. of potentially avoidable hospitalizations | 44.8% | 45.7%*** | 46.9%*** |
| Socio-demographic factors | |||
| Age | 84.1 | 81.6*** | 78.2*** |
| Male | 34.8% | 32.1%*** | 23.8%*** |
| Race | *** | *** | |
| white | 83.3% | 83.9% | 83.3% |
| black | 8.5% | 9.1% | 10.6% |
| other | 8.3% | 7.0% | 6.1% |
| Medicare-Medicaid dual | 41.8% | 47.8%*** | 54.5%*** |
| Post-acute admission | 62.6% | 60.0%*** | 63.1%*** |
| Functional Status | |||
| ADL (score 0–28) | 15.8 | 15.0*** | 15.3*** |
| Cognitive Function Score | *** | *** | |
| Intact | 25.2% | 35.2% | 49.9% |
| Mildly impaired | 24.6% | 26.0% | 23.7% |
| Moderately impaired | 38.4% | 30.5% | 19.7% |
| Severely impaired | 8.6% | 5.0% | 2.9% |
| Missing | 3.2% | 3.3% | 3.8% |
| Major Diagnoses | |||
| Hypertension | 79.8% | 85.3%*** | 87.8%*** |
| Diabetes | 27.1% | 43.7%*** | 56.6%*** |
| Heart failure | 20.9% | 27.3%*** | 35.3%*** |
| Coronary artery disease (CAD) | 24.6% | 26.9% | 26.3%** |
| Peripheral vascular disease (PVD) | 8.0% | 8.9% | 10.5%*** |
| Alzheimer’s disease or related dementia (ADRD) | 59.2% | 51.2% | 36.0%*** |
| Asthma/COPD | 19.6% | 23.3% | 31.6%*** |
| Stroke | 18.6% | 19.5% | 16.9%*** |
| Anxiety | 27.6% | 27.6% | 28.6%*** |
| Depression | 44.8% | 49.6% | 52.6%*** |
P<0.001
P<0.05 – comparison of mild and moderate/severely obese to normal weight residents
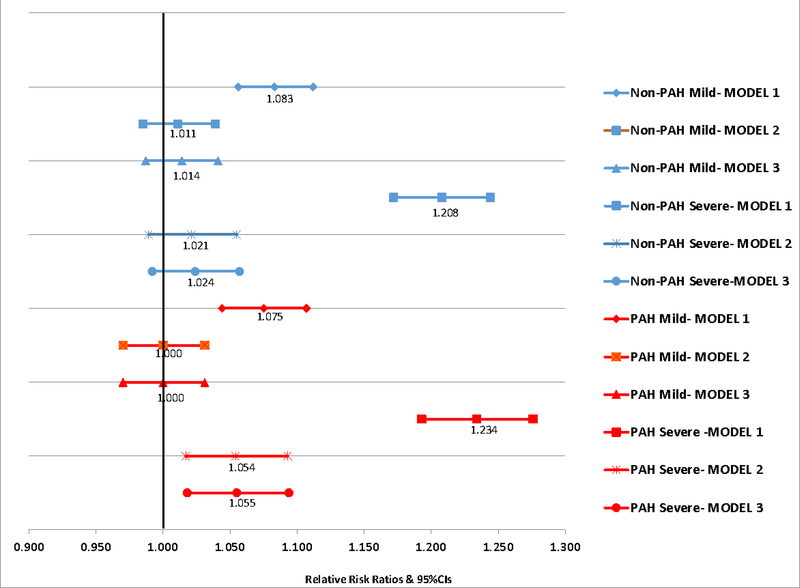
When unadjusted for other covariates (model 1, Figure 1), residents with mild and with moderate/severe obesity were statistically significantly more likely to be hospitalized for non-PAH (RRR=1.083 and RRR=1.208, respectively) and PAH (RRR=1.075 and RRR=1.234, respectively) than normal weight residents. After adjusting for individual level covariates, the risk of non-PAH, for the mildly obese and moderate/severely obese, became statistically not different from the risk for normal weight individuals, but the risk of PAH for the latter group remained higher (RRR=1.054) (model 2). After adjusting for individual and facility-level covariates (model 3), only the risk of PAH for the moderate/severely obese remained significantly higher (RRR=1.055; 95%CI=1.018,1.094) than for normal weight residents (Figure 1).
Figure 1:
Relative Risk and 95%CIs for Non-Avoidable (non-PAH) and Potentially Avoidable (PAH) Hospitalizations by Obesity Category: Simple and Risk-Adjusted Models*
NOTE: Lines that cross 1.0 depict parameters that are not statistically significant.
* Reference variable = normal weight
Model 1 = NH random effects and state dummies only
Model 2 = Model 1+ resident level characteristics
Model 3 = Model 2 + facility-level factors
In Table 2 we show a fully adjusted model (3) with individual and facility-level covariates, and year dummies, for the risk of PAH and non-PAH, independent of obesity. Most individual level factors, although statistically significantly associated with the risk of PAH (and non-PAH) were clinically quite insignificant, with a few notable exceptions. For example, dual eligibility for Medicare and Medicaid conferred a 17% higher risk (RRR=1.170) of PAH and 13% higher risk of non-PAH (RRR=1.133). Post-acute NH admissions increased the risk of PAH and non-PAH 24% and 28%, respectively. Among co-morbid conditions, heart failure and asthma/COPD had particularly strong incremental effects on PAH (RRR=1.530 and RRR=1.465, respectively) and a lower effect on non-PAH (RRR=1.210 and RRR=1.193, respectively).
Table 2:
Potentially Avoidable and All Other Hospitalizations by Obesity Status: Adjusted Relative Risk Ratios (RRR) and 95% Confidence Intervals (Note: Coefficients for state dummies are not shown)
| Characteristics | Non-Avoidable Hospitalizations | Potentially Avoidable Hospitalizations | ||||
|---|---|---|---|---|---|---|
| RRR | 95%CI | RRR | 95%CI | |||
| Individual Factors | ||||||
| Mild obesity (ref=normal) | 1.014 | 0.987 | 1.041 | 1.000 | 0.970 | 1.031 |
| Moderate/severe obesity | 1.024 | 0.992 | 1.057 | 1.055* | 1.018 | 1.094 |
| Age | 0.993* | 0.992 | 0.995 | 1.012* | 1.011 | 1.014 |
| Male (ref=female) | 1.301* | 1.277 | 1.327 | 1.063* | 1.040 | 1.088 |
| Race: black (ref=white) | 1.199* | 1.162 | 1.237 | 0.994 | 0.956 | 1.033 |
| Race: other | 1.082* | 1.045 | 1.121 | 0.950 | 0.911 | 0.992 |
| Dual status | 1.133* | 1.110 | 1.155 | 1.170* | 1.144 | 1.197 |
| Post-acute admission | 1.284* | 1.258 | 1.311 | 1.237* | 1.209 | 1.266 |
| ADL (score 0–28) | 1.026* | 1.025 | 1.028 | 1.008* | 1.007 | 1.010 |
| CFS:(ref=intact) Mildly impaired |
1.007 | 0.981 | 1.033 | 1.025 | 0.996 | 1.055 |
| Moderately impaired | 0.962* | 0.937 | 0.988 | 1.010 | 0.980 | 1.041 |
| Severely impaired | 1.005 | 0.965 | 1.046 | 0.958 | 0.911 | 1.006 |
| Missing | 3.451* | 3.310 | 3.600 | 3.773* | 3.602 | 3.953 |
| Hypertension | 1.098* | 1.072 | 1.126 | 1.125* | 1.093 | 1.157 |
| Diabetes | 1.209* | 1.186 | 1.233 | 1.223* | 1.196 | 1.251 |
| Heart failure | 1.210* | 1.184 | 1.236 | 1.530* | 1.495 | 1.566 |
| CAD | 1.085* | 1.063 | 1.108 | 1.130* | 1.104 | 1.157 |
| PVD | 1.184* | 1.149 | 1.221 | 1.092* | 1.054 | 1.132 |
| ADRD | 0.925* | 0.907 | 0.945 | 0.934* | 0.912 | 0.956 |
| Asthma/COPD | 1.193* | 1.168 | 1.219 | 1.465* | 1.431 | 1.500 |
| Stroke | 1.036* | 1.013 | 1.060 | 0.961* | 0.935 | 0.987 |
| Anxiety | 1.024 | 1.002 | 1.045 | 1.068* | 1.044 | 1.094 |
| Depression | 1.022 | 1.002 | 1.041 | 1.060* | 1.037 | 1.083 |
| Nursing Home Factors | ||||||
| NH rate: mild obesity | 0.997 | 0.994 | 1.000 | 1.000 | 0.996 | 1.003 |
| NH rate: mod/severe Obesity | 0.998 | 0.995 | 1.000 | 0.996* | 0.993 | 0.998 |
| Star rating: 1 star (ref=3 star) | 1.053* | 1.019 | 1.089 | 1.045 | 1.007 | 1.085 |
| Star rating: 2 star (ref=3 star) | 1.010 | 0.982 | 1.040 | 0.988 | 0.956 | 1.021 |
| Star rating: 4 star (ref=3 star) | 0.968 | 0.942 | 0.995 | 0.973 | 0.944 | 1.004 |
| Star rating: 5 star (ref=3 star) | 0.935* | 0.906 | 0.965 | 0.926* | 0.894 | 0.960 |
| CNA hours/resident/day | 1.021 | 1.000 | 1.042 | 1.047* | 1.023 | 1.072 |
| LPN hours/resident/day | 1.000 | 0.973 | 1.029 | 1.007 | 0.975 | 1.039 |
| RN hours/resident/day | 0.913* | 0.858 | 0.970 | 0.801* | 0.746 | 0.859 |
| Number of beds | 1.000 | 1.000 | 1.000 | 0.999* | 0.999 | 0.999 |
| Medicare% | 1.002* | 1.001 | 1.003 | 1.001* | 1.000 | 1.003 |
| Medicaid% | 1.004* | 1.003 | 1.004 | 1.005* | 1.004 | 1.006 |
| Chain | 0.969* | 0.947 | 0.991 | 0.950* | 0.926 | 0.974 |
| Profit | 1.039* | 1.011 | 1.068 | 1.018 | 0.988 | 1.049 |
| Year: 2012 (ref=2011) | 0.948* | 0.925 | 0.971 | 0.921* | 0.896 | 0.948 |
| Year: 2013 (ref=2011) | 0.883* | 0.860 | 0.906 | 0.833* | 0.809 | 0.858 |
| Year: 2014 (ref=2011) | 0.877* | 0.850 | 0.905 | 0.794* | 0.766 | 0.824 |
p-value <0.01
Residents in highest quality NHs (CMS 5-star rating) had 7.4% and 6.5% lower risk of PAH and non-PAH, respectively than residents in lower (3-star) quality NHs. The risk of both PAH and non-PAH was lower in NHs with higher RN staffing (RRR=0.801 and RRR=0.913, respectively). The risk of hospitalizations, both PAH and non-PAH, was statistically significantly lower in chain facilities and higher in the for-profit NHs, but only for non-PAH. Compared to CY2011, there has been a significant decline in PAH and non-PAH alike in the subsequent CY2012–2014 time period.
DISCUSSION
To the best of our knowledge this is the first study of the association between obesity and PAH among long-stay NH residents. In support of our hypothesis, we found that after controlling for individual covariates higher risk of PAH persisted for the moderate/severely obese but not for the mildly obese. Adjusting for facility factors did not change this pattern. However, we found no statistically significant differences in the risk of non-PAH among mildly or moderate/severely obese residents, compared to those of normal weight. Because caring for residents who are obese places higher demands on NH resources, such as higher staffing, weight-appropriate equipment and supplies, facilities may have less capacity in preventing or managing conditions that may result in PAH. Furthermore, the definition of what is preventable/manageable may be quite different when applied to obese residents. For example, residents who are obese have substantially higher rates of both CHF and COPD and experience much greater rates of hospitalizations for these conditions. The ability of NH staff to effectively recognize, prevent or manage exacerbations of these conditions in this population may be compromised by the complexity of their comorbid conditions. With increasing weight, edema or shortness of breath, all related to heart failure, may be more difficult to recognize in obese residents, and consequently harder to prevent or manage on site.
Consistent with the recent CMS reports of declines in PAH among NH residents,22 our study found similar declines in PAHs and non-PAHs alike. However, the disparities in PAH between obese and normal weight residents have persisted.
We acknowledge several limitations. While we have accounted for many individual covariates, as is true in other cohort studies, uncaptured health conditions may confound the relationship between obesity and PAH. Our study cohort did not include individuals who repeatedly used SNF services or those enrolled in Medicare Advantage, thus making our results not fully generalizable.
Conclusions and Implications
In conclusion, obese residents are more likely to experience PAH. Efforts to improve care for these residents may need to broadly consider NHs’ capacity to commit additional resources to fully integrate care for this growing segment of the population.
Supplementary Material
Acknowledgments
Funding source: National Institutes of Health / National Institute on Aging, grant R01AG052451.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- 1.Fakhouri THI, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS Data Brief. 2012. [PubMed] [Google Scholar]
- 2.Hales CM, Carroll MD, Fryay CD, Ogden CL. Prevalence of Obesity Among Adults and Youth:United States, 2015–2016. Washington, DC.; 2017. [PubMed] [Google Scholar]
- 3.Sturm R, Ringel JS, Andreyeva T. Increasing obesity rates and disability trends. Health Aff. 2004. doi: 10.1377/hlthaff.23.2.199 [DOI] [PubMed] [Google Scholar]
- 4.Zizza C, Herring A, Domino M, Haines P, Stevens J, Popkin BM. The effect of weight change on nursing care facility admission in the NHANES I Epidemiologic Followup Survey. J Clin Epidemiol. 2003. doi: 10.1016/S0895-4356(03)00142–2 [DOI] [PubMed] [Google Scholar]
- 5.Felix HC, Bradway C, Chisholm L, Pradhan R, Weech-Maldonado R. Prevalence of Moderate to Severe Obesity Among U.S. Nursing Home Residents, 2000–2010. Res Gerontol Nurs. 2015. doi: 10.3928/19404921-20150223-01 [DOI] [PubMed] [Google Scholar]
- 6.Zhang N, Field T, Mazor KM, Zhou Y, Lapane KL, Gurwitz JH. The Increasing Prevalence of Obesity in Residents of U.S. Nursing Homes: 2005–2015. Journals Gerontol Ser A. 2019. doi: 10.1093/gerona/gly265 [DOI] [PubMed] [Google Scholar]
- 7.Lapane KL, Resnik L. Obesity in nursing homes: An escalating problem. J Am Geriatr Soc. 2005. doi: 10.1111/j.1532-5415.2005.53420.x [DOI] [PubMed] [Google Scholar]
- 8.Associates A. Nursing Home Quality Measure Technical Specifications; 2016.
- 9.Centers for Medicare and Medicaid Services (CMS). The Skilled NUrsing Facility Value-Based Purchasing Program (SNF VBP). 2018. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/SNF-VBP/SNF-VBP-Page.html. Accessed June 17, 2019.
- 10.Ingber M, Feng Z, Khatutsky G, et al. Initiative to Reduce Avoidable Hospitalizations Among Nursing Facility Residents Shows Promising Results. Health Aff. 2017;36(3):441–450. [DOI] [PubMed] [Google Scholar]
- 11.Kosar CM, Thomas KS, Gozalo PL, Ogarek JA, Mor V. Effect of Obesity on Postacute Outcomes of Skilled Nursing Facility Residents with Hip Fracture. J Am Geriatr Soc. 2018. doi: 10.1111/jgs.15334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai S, Wang S, Mukamel DB, Caprio T, Temkin-Greener H. Hospital Readmissions Among Post-acute Nursing Home Residents: Does Obesity Matter? J Am Med Dir Assoc. 2019. doi: 10.1016/j.jamda.2019.01.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barr J, Cunneen J. Understanding the bariatric client and providing a safe hospital environment. Clin Nurse Spec. 2001. doi: 10.1097/00002800-200109000-00017 [DOI] [PubMed] [Google Scholar]
- 14.Piotrowski J, Romano M. Heavy costs. Hospitals pay high price to treat obese patients. Mod Healthc. 2003. [PubMed] [Google Scholar]
- 15.Felix HC. Personal Care Assistance Needs of Obese Elders Entering Nursing Homes. J Am Med Dir Assoc. 2008. doi: 10.1016/j.jamda.2008.01.011 [DOI] [PubMed] [Google Scholar]
- 16.Dimant J Bariatric programs in nursing homes. Clin Geriatr Med. 2005. doi: 10.1016/j.cger.2005.06.006 [DOI] [PubMed] [Google Scholar]
- 17.Kumar A, Rahman M, Trivedi AN, Resnik L, Gozalo P, Mor V. Comparing post-acute rehabilitation use, length of stay, and outcomes experienced by Medicare fee-for-service and Medicare Advantage beneficiaries with hip fracture in the United States: A secondary analysis of administrative data. PLoS Med. 2018. doi: 10.1371/journal.pmed.1002592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible medicare and medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc. 2012;60(5):821–829. doi: 10.1111/j.1532-5415.2012.03920.x [DOI] [PubMed] [Google Scholar]
- 19.Walsh E, Freiman M, Haber S, Bragg A, Ouslander J, Wiener J. Cost Drivers for Dually Eligible Beneficiaries: Potentially Avoidable Hospitalizations from Nursing Facility, Skilled Nursing Facility, and Home and Community-Based Services Waiver Programs. Waltham, MA; 2010. https://www.cms.gov/Research-Statistics-data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/costdriverstask2.pdf. [DOI] [PubMed] [Google Scholar]
- 20.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. Journals Gerontol - Ser A Biol Sci Med Sci. 1999. doi: 10.1093/gerona/54.11.M546 [DOI] [PubMed] [Google Scholar]
- 21.Thomas K, Dosa D, Wysocki A, Mor V. The Minimum Data Set 3.0 Cognitive Function. Med Care. 2015;(ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brennan N, Engelhardt T. Data Brief: Sharp Reductions in Avoidable Hospitalizations among Long-Term Care Facility Residents; 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.