Abstract
Objectives:
To understand how health status preceding traumatic brain injury (TBI) affects relative functional gain after inpatient rehabilitation using a data mining approach.
Design:
Population-based, sex-stratified, retrospective cohort study using health administrative data from Ontario, Canada (39% of the Canadian population).
Setting:
Inpatient rehabilitation.
Participants:
Patients 14 years or older (N=5,802; 63.4% males) admitted to inpatient rehabilitation within one-year of a TBI-related acute care discharge between April 1, 2008 and March 31, 2015.
Interventions:
Not applicable.
Main Outcome Measures:
Relative functional gain (RFG) in percent, calculated as [(Discharge FIM-Admission FIM)/(126-Admission FIM) × 100]. Health status prior to TBI was identified and internally validated using a data mining approach that categorized all International Classification of Diseases Version 10 codes for each patient.
Results:
The average RFG among males was 52.8±27.6% and among females, 51.6±27.1%. Sex-specific Bonferroni adjusted multivariable linear regressions identified 10 factors of pre-injury health status related to neurology, emergency medicine, cardiology, psychiatry, geriatrics, and gastroenterology that were significantly associated with reduced RFG in FIM for males. Only one pre-injury health status category, geriatrics, was significantly associated with RFG in female patients.
Conclusions:
Comorbid health conditions present up to five years preceding the TBI event were significantly associated with RFG. These findings should be considered when planning and executing interventions to maximize functional gain and to support an interdisciplinary approach. Best practices guidelines and clinical interventions for older males and females with TBI should be developed to account given the increasingly aging TBI population.
Keywords: Brain injuries, Comorbidity, Rehabilitation, Data mining, International Classification of Diseases
Traumatic brain injury (TBI) has been defined as “an alteration in brain function, or other evidence of brain pathology, caused by an external force”.1 As the population of patients with TBI in inpatient rehabilitation continue to rapidly age,2 an increasing number of patients is expected to enter rehabilitation with multiple comorbid health conditions that may have been present for a long time. Existing literature has provided strong evidence that comorbid health conditions negatively impact outcome after TBI. For example, research has indicated that higher burden of medical comorbidities and select conditions such as hypertension, diabetes, cancer, rheumatoid arthritis, chronic bronchitis anxiety, depression, and substance abuse were associated with lower functional outcome.3–5 While these studies provided key information to support clinical care for TBI, only select health conditions captured in surveys were included and as such, other comorbidities that may impact functional outcome were not assessed. Some studies also assess comorbidities based on self-reports,3,5 which may be affected by memory bias, or use pre-defined measures of comorbidities (e.g., Charlson Comorbidity Index, Aggregated Diagnosis Groups) that were neither developed for the TBI population nor for the purpose of measuring functional outcome,6,7 which may limit our understanding of the association between comorbidities among patients with TBI and functional outcome. Comprehensive data on all comorbid health conditions and related health experience must be identified to inform evidence-based client-centred rehabilitation services.
A recognized challenge in understanding how comorbidities affect rehabilitation outcomes is that TBI can happen to anyone, regardless of age, sex, and socioeconomic status. This heterogeneity makes it challenging to meaningfully categorize the health status of patients with TBI. The use of multiple testing and factor analyses on health administrative data have been demonstrated to be effective in addressing this challenge,8 as it can group complex comorbidities and social/environmental circumstances from volumes of data captured in health administrative datasets or electronic medical records. For TBI, 43 factors of health status preceding the TBI event have been identified to provide the foundation to overcome the challenge in sorting through complex medical conditions to understand how they affect outcomes after rehabilitation for TBI.
The objective of this population-based study was to determine how pre-injury health status (i.e., comorbid health conditions and personal, social, and environmental factors), present five years prior to the TBI event, affects relative functional gain during inpatient rehabilitation. Twelve years of health administrative data from the province of Ontario in Canada, home to 39% of the Canadian population,9 were used and all comorbid health conditions and related health problems were extracted.
Methods
Research ethics approval was received from KITE-Toronto Rehab, University Health Network and University of Toronto.
Data Source
Population-based health administrative data from Ontario, Canada were used for this study. Data on TBI-related acute care admissions were extracted from the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (DAD), which contains information on all demographic, clinical, and discharge, transfers, and deaths in Canada.10 Data on patients who were admitted to inpatient rehabilitation were obtained from the National Rehabilitation Reporting System (NRS), which contains information on all demographic, clinical, and rehabilitation activities from all adult inpatient rehabilitation beds within acute care and freestanding rehabilitation hospitals in Canada.11 These databases are assessed annually according to five dimensions of data quality as defined by the CIHI Data Quality Framework: accuracy, timeliness, comparability, usability and relevance.12
Sample
All patients aged 14 years and older admitted to inpatient rehabilitation within one-year of acute care discharge between April 1, 2008 and March 31, 2015 were identified. Even though the NRS collects data on adult inpatient rehabilitation beds, patients between age 14 and 18 years, inclusive (N=112; 1.9% of total sample), were identified in our dataset and as such, were included in this study.
Patients with a TBI-related acute care visit were identified in the DAD using the following ICD-10 codes: S02.0, S02.1, S02.3, S02.7, S02.8, S02.9, S06, S04.0, and S07.1. Literature reviews have identified an association between these codes and TBI and have been used extensively in Ontario to identify TBI in health administrative data.6,8,13–17 The patients’ first TBI-related acute care admission during the study period was identified from the DAD. Using unique de-identified patient IDs, their data were merged with the NRS to identify those who were admitted to inpatient rehabilitation within one-year of acute care discharge. This ensured that the acute care and inpatient rehabilitation records were matched to each patient, and that each patient was only captured once.
Variables
The outcome variable for this study was relative functional gain (RGF) in percent, defined as the total FIM at discharge minus the total FIM at admission, divided by the maximum possible change in FIM (i.e., 126 minus admit FIM score) in percent. The FIM (Functional Independence Measure) consists of 18 items, scored on a 7-point Likert scale, that measure the cognitive and physical disability of an individual.18 This outcome measure takes into account the maximum functional gain possible for each patient and has been applied in rehabilitation research across diverse health conditions.19 A negative 50% RFG was used a cut off for outliers (Supplementary File 1, Figure 1) and these outliers’ RFG was adjusted to −50% and remained in the sample.
Covariates included in this study were identified through previous research on TBI and inpatient rehabilitation.2–6,13,20–22 Demographic variables included: (a) age at acute care discharge; (b) rural residence (yes vs. no), determined based on the individual postal codes designated as being rural by the Canadian Postal Service; and (c) income quintile, defined as the relative household income adjusted for household size and community (1=lowest, 5=highest).
Injury-related variables included: (a) injury severity, measured using the Abbreviated Injury Severity (AIS) for head and face and categorized as mild (1–2), moderate (3), severe (4+) and unspecified (i.e., diagnosis code was not specific enough to determine severity of injury);23 (b) mechanism of injury, categorized as falls, motor vehicle collision, struck by/against an object, and other;24 (c) sports-related (yes vs. no);25 and (d) intent of injury, categorized as intentional, unintentional, and other.24
Acute care-related variables included (a) fiscal year of discharge; (b) acute care length of stay (LOS), defined as the number of days between acute care admissions and discharge, excluding alternate level of care (ALC) days; (c) special care days, defined as the number of days in an intensive care unit; and (d) alternate level of care days, defined as days in which a patient is still occupying an acute care bed when a physician or designated other has indicated that his/her acute care treatment has finished.26
Inpatient rehabilitation-related variables included (a) rehabilitation LOS, defined as the number of days from admission to discharge (in the multivariable linear regression, LOS was transformed to a quadratic effect due to a non-linear relationship with RFG; see Supplementary File 1, Figure 3); (b) admission delay, defined as the number of days between acute care discharge and admission to inpatient rehabilitation; (c) Rehabilitation Client Grouping of TBI (yes vs. no), defined as the primary reason for admission to a particular rehabilitation program;11 (d) TBI as the main diagnosis in inpatient rehabilitation; and (e) informal support, defined as unpaid assistance available to the patient through ones’ social and/or personal networks (required vs. not required).11
Analyses
Pre-injury health status is defined as comorbid health conditions and personal, social, and environmental factors identified in the emergency department, ambulatory care, or acute care settings up to five years prior to the TBI-related acute care admission. They were identified using ICD-10 codes and reduced into 43 factors using multiple testing and factor analysis.8 Briefly, matched McNemar test for all ICD-10 codes (N=2,600 codes based on the first three alphanumeric characters) were conducted to determine differences between patients with and without TBI (matched on age, sex, income quintile, and geographic area of residence). Benjamini-Yekutieli multiple testing method was used to identify ICD-10 codes that were significantly more likely to occur among patients with TBI compared to patients without TBI. Factor analysis was then conducted on these significant ICD-10 codes to reduce them into 43 factors, with some ICD-10 codes present in multiple factors because factor analyses identified these codes to be regularly coded with each, which may truly represent shared pathophysiological mechanisms of different systematic disorders (see Supplementary File, Table 1, for the list of ICD-10 codes that are captured in each of the factors). These 43 factors were internally validated by randomly splitting our data into training (50%), validation (25%), and testing (25%) datasets. Additional details are provided in a peer-reviewed manuscript.8
Sex-specific multivariable linear regressions were conducted for each of the 43 factors, controlling for all covariates (demographic, injury-related, acute care-related, inpatient rehabilitation-related, and pre-injury health status variables), with RFG as the outcome variable. In order to control for multiple testing, a Bonferroni correction was applied to each test of significance, resulting in a significance value of p<0.001. Besides reporting the usual 95% confidence intervals, Bonferroni adjusted confidence intervals (i.e., estimate±3.25*standard error) was also reported. All graphs and modelling were completed using SAS v9.4.
Results
Between April 1, 2008 and March 31, 2015, there were 38,619 patients, aged 14 years or older, with a TBI-related acute care visit, of whom 15% (N=5,806) were admitted to inpatient rehabilitation within one-year. Given that the outcome variable was RFG, three patients were excluded from this cohort because their admit FIM score was 126 (i.e., highest possible score and therefore, mathematically, their RFG cannot be computed because the denominator would be equal to zero). One patient was removed due to missing data on acute care length of stay. The final sample for this study was 5,802 patients, of whom 63.4% were males. Supplementary File 1, Figure 2 presents CONSORT flow diagram of sample inclusion. Table 1 presents the characteristics of patients by sex.
Table 1.
Profile of patients with TBI in inpatient rehabilitation within 1-year of acute care discharge by sample characteristics and sex, Ontario, Canada, 2008/09 – 2014/15 (inclusive).
| Male Patients N=3,677 | Female Patients N=2,125 | |
|---|---|---|
| Demographic | ||
| Age | ||
| Rural Residence (Yes) | 492 (13.4) | 189 (8.9) |
| Income Quintile | ||
| 1 (Lowest) | 786 (21.4) | 405 (19.1) |
| 2 | 793 (21.6) | 452 (21.3) |
| 3 | 705 (19.2) | 413 (19.4) |
| 4 | 715 (19.5) | 432 (20.3) |
| 5 (Highest) | 678 (18.4) | 423 (19.9) |
| Injury-Related | ||
| Injury Severity (AIS) | ||
| Unspecified | 552 (15.0) | 448 (21.1) |
| Mild | 125 (3.4) | 101 (4.8) |
| Moderate | 138 (3.8) | 105 (4.9) |
| Severe | 2,862 (77.8) | 1,471 (69.2) |
| Mechanism of Injury | ||
| Fall | 1,984 (54.0) | 1,338 (63.0) |
| Motor Vehicle Collision | 923 (25.1) | 565 (26.6) |
| Struck By/Against | 201 (5.5) | 51 (2.4) |
| Other | 569 (15.5) | 171 (8.0) |
| Sports-Related Injury (Yes) | 291 (7.9) | 57 (2.7) |
| Intent of Injury | ||
| Unintentional | 3,407 (92.7) | 2,076 (97.7) |
| Intentional | 198 (5.4) | 26 (1.2) |
| Other | 72 (1.9) | 23 (1.1) |
| Acute Care-Related | ||
| Fiscal Year of Discharge | ||
| 2008/09 | 415 (11.3) | 219 (10.3) |
| 2009/10 | 419 (11.4) | 256 (12.1) |
| 2010/11 | 494 (13.4) | 260 (12.2) |
| 2011/12 | 535 (14.6) | 313 (14.7) |
| 2012/13 | 567 (15.4) | 342 (16.1) |
| 2013/14 | 613 (16.7) | 361 (17.0) |
| 2014/15 | 634 (17.2) | 374 (17.6) |
| Acute Care LOS (Days) | ||
| Special Care Days (Yes) | 2,407 (65.5) | 1,098 (51.7) |
| ALC Days (Days) | ||
| Rehabilitation-Related | ||
| Total FIM Score | ||
| Admission | ||
| Discharge | ||
| RFG | ||
| Absolute Gain | ||
| Efficiency | ||
| Motor FIM Score | ||
| Admission | ||
| Discharge | ||
| RFG* | ||
| Absolute Gain | ||
| Efficiency | ||
| Cognitive FIM Score | ||
| Admission | ||
| Discharge | ||
| RFG* | ||
| Absolute Gain | ||
| Efficiency | ||
| Rehabilitation LOS (Days) | ||
| Admission Delay (Days) | ||
| RCG TBI (Yes) | 2,124 (57.8) | 931 (43.8) |
| TBI Main Diagnosis (Yes) | 2,123 (57.7) | 1,009 (47.5) |
| Informal Support (Required) | 3,174 (86.3) | 1,896 (89.2) |
Abbreviations.AIS: Abbreviated Injury Severity; ALC: Alternate Level of Care; FIM: Functional Independence Measure; IQR: Interquartile range; LOS: Length of Stay; RCG: Rehabilitation Client Grouping; RFG; Relative Functional Gain; SD: Standard Deviation; TBI: Traumatic Brain Injury.
Notes.All values are N (column %) unless otherwise specified; Absolute gain was calculated as discharge FIM minus admit FIM; Efficiency was calculated as discharge FIM minus admit FIM divided by rehabilitation LOS.
Patients with perfect motor FIM score at admission (N=67 males and N=7 females) were not included in the calculation of the motor RFG in Table 1 because the denominator of motor RFG is maximum possible motor FIM minus admit motor FIM; a perfect motor FIM score would result in a denominator of zero and mathematically, cannot be computed. Similarly, patients with perfect cognitive FIM score at admission (N=326 males and N=236 females) were not included in the calculation of cognitive RFG in Table 1, as the denominator of cognitive RFG is maximum possible cognitive FIM score minus admit cognition FIM. However, these patients remained in the cohort because the outcome of interest is the RFG for total FIM and their total FIM score at admission was not 126 (i.e., maximum possible FIM score).
The RFG was 52.8±27.6% and 51.6±27.1% for male and female patients, respectively. Sex-specific Bonferroni adjusted multivariable linear regressions identified 10 pre-injury health status factors significantly associated with reduced RGF in males compared to those without the factors. These factors were: (1) Alzheimer’s diseases and dementia: 16.8%; (2) epilepsy, seizures, brain lesions and other: 8.1%; (3) pulmonary, abdominal and other emergency: 7.7%; (4) stroke and emergencies involving the brain: 5.7%; (5) chronic cardiovascular pathology: 5.7%; (6) mental health disorders; functional inquiry: 5.3%; (7) disorders of elderly and medical issues: 5.1%; (8) conditions and symptoms of abdomen and pelvis: 4.4%; (9) metabolic disorders and abdominal symptoms: 3.5%; and (10) cardiovascular disorders and other: 3.4%.
One factor was significantly associated with reduced RFG among females: disorders of elderly and medical issues. Patients with this factor had a 4.7% lower RFG compared to patients without this factor. Table 2 presents the prevalence of each factor in male and female patients. Figure 1 reports the Bonferroni adjusted and unadjusted estimates with 95% confidence interval for the significant factors described above. Supplementary File 1, Table 2a and Table 2b lists the association between all 43 factors and RFG and Supplementary File 2 provides the multivariable linear regression models on the association between all covariates and RFG for all 43 factors, by sex.
Table 2.
Prevalence of pre-injury health status significantly associated with RFG between 5 years and 30 days prior to TBI-related acute care admission, by sex, Ontario, Canada.
| Male Patients N=3,677 | Female Patients N=2,125 | |
|---|---|---|
| Factor 01: Cardiovascular disorders and other | 1,121 (30.5) | 779 (36.7) |
| Factor 02: Mental health disorders; functional inquiry | 311 (8.5) | 197 (9.3) |
| Factor 03: Disorders of elderly and medical issues | 1,118 (30.4) | 897 (42.2) |
| Factor 10: Pulmonary, abdominal and other emergencies | 505 (13.7) | 395 (18.6) |
| Factor 11: Metabolic disorders and abdominal symptoms | 1,131 (30.8) | 854 (40.2) |
| Factor 12: Stroke and emergencies involving the brain | 717 (19.5) | 571 (26.9) |
| Factor 16: Conditions and symptoms of abdomen and pelvis | 476 (13.0) | 546 (25.7) |
| Factor 17: Chronic cardiovascular pathology | 448 (12.2) | 297 (14.0) |
| Factor 26: Epilepsy, seizures, brain lesions and other | 143 (3.9) | 65 (3.1) |
| Factor 29: Alzheimer’s diseases and dementia | 34 (0.9) | 35 (1.7) |
Notes.All values are N (column %); Multiple ICD-10 codes may be represented in each Factor and as such, patients with these ICD-10 codes may be counted in multiple Factors. Please see Supplementary File Table 1, for the list of ICD-10 codes that are captured in each of the factors.
Figure 1.
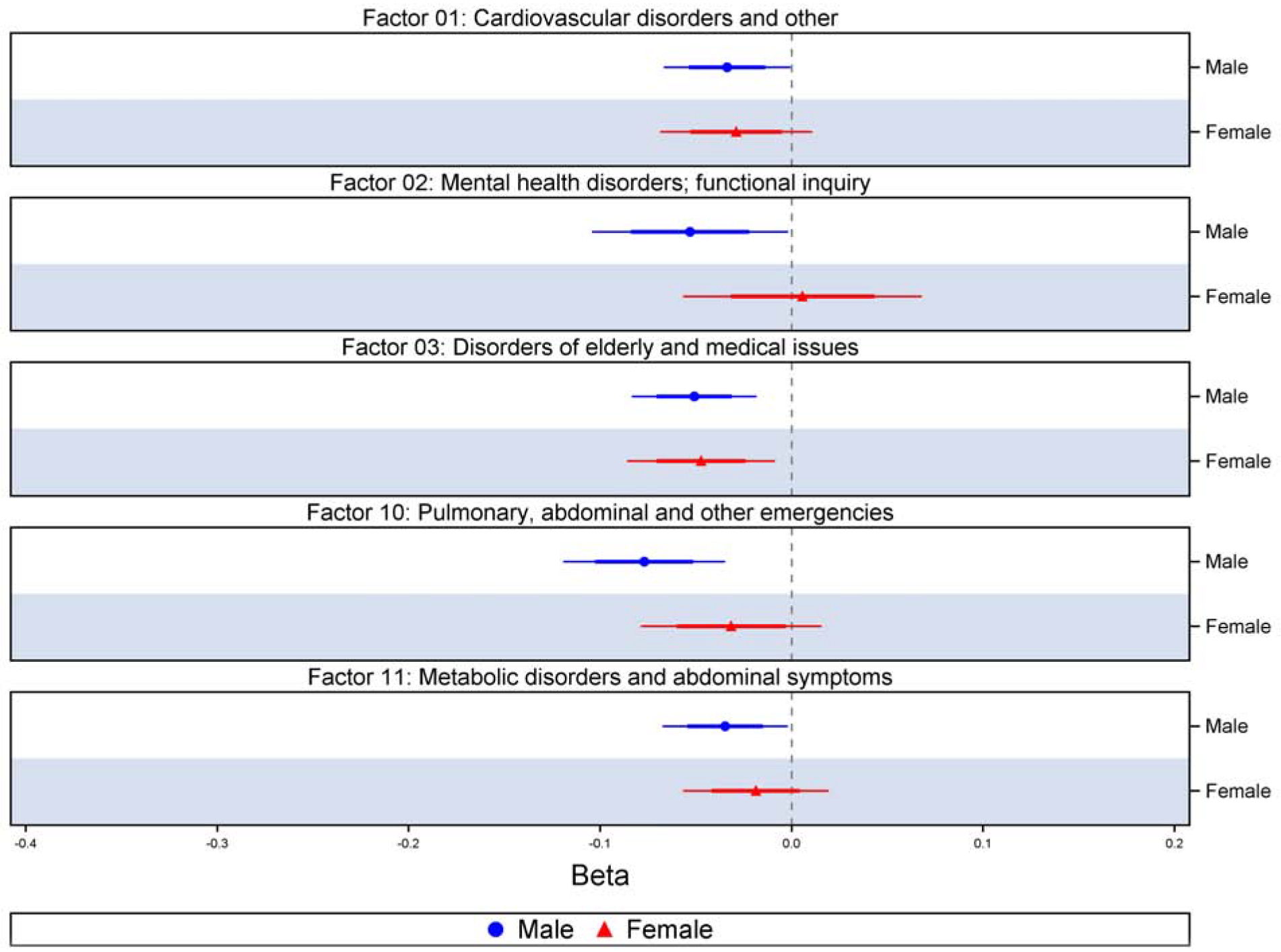
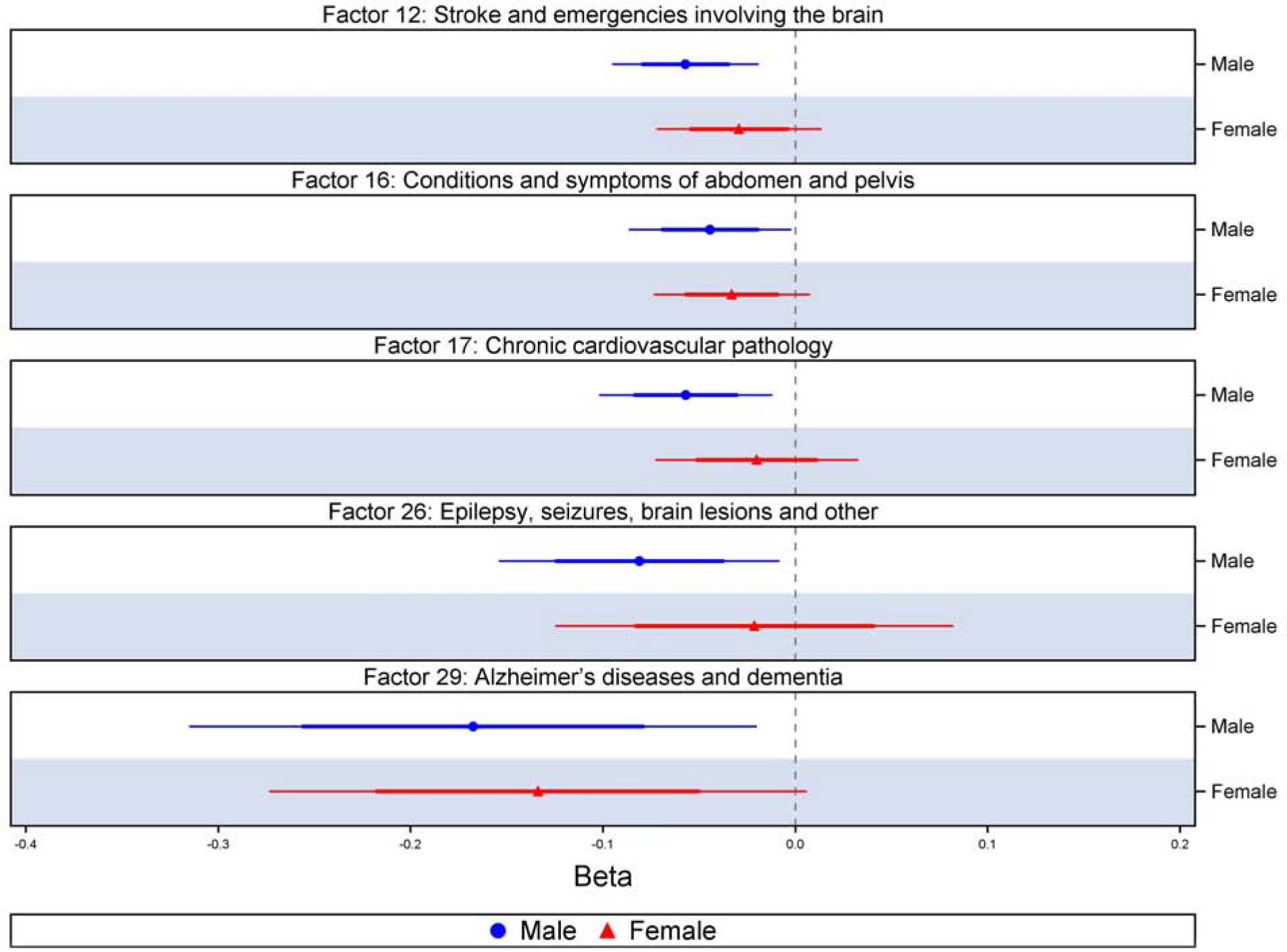
Multivariable linear regression results of pre-injury health status significantly associated with RFG (Bonferroni adjusted [thin line] and unadjusted estimates with 95% confidence interval [thicker line]).
Discussion
This study supports prior research showing that pre-injury health status impacts rehabilitation outcomes and extends existing knowledge by demonstrating that pre-injury health status present up to five years preceding TBI significantly reduced the RFG from 3.4% to 16.8%. A key finding is that there are sex differences in the number and types of pre-injury health status factors that affect RFG. Among males only, 10 factors related to psychiatry, neurology, cardiology, gastroenterology, and conditions related to the elderly were significantly associated with reduced RFG. Interestingly, even though the prevalence of all but one of the 10 factors was higher among females, they were statistically significant among males only. Further research into these health conditions is encouraged to understand the influence of sex and/or gender on the experiences of these conditions and impact on RFG. It is acknowledged the findings on sex differences presented in this study may be impacted by the smaller sample of female patients in this study compared to males (N=2,215 vs. N=3,677), particularly for some of the pre-injury health status factors. For example, five factors related to cardiology, emergency medicine, and neurology that were significantly associated with reduced RFG among males were also significant among females prior to Bonferroni adjustment. Nonetheless, findings highlight the importance of active identification and management of chronic conditions in both male and female patients with TBI in order to maximize functional gain during rehabilitation.
This study also identified the types of health conditions that warrant additional research to understand how pre-injury health status may be managed prior to and during inpatient rehabilitation. Of note is the finding that only one category of health status – disorders of the elderly and other medical conditions – was significantly associated with functional gain among female patients. This finding is important because the population of TBI in inpatient rehabilitation is rapidly aging,2 particularly among females. The median age of females in this study was 73 years and females who had experienced previous falls and conditions consistent with delirium, abnormality of gait and mobility, fatigue, hypertension, and osteoporosis, and Parkinson’s Disease, had a 4.7% lower change in FIM score compared to patients without the above conditions. These findings are consistent with previous research on comorbidities among patients with TBI5,13 and highlight the vulnerability of older females with these conditions to falls and TBI and its impact on functional outcome after rehabilitation. The future inpatient rehabilitation population for TBI will likely be older females, yet current best practices/clinical guidelines are predominately based on the pediatric or adult populations and to the best of our knowledge, none specifically on older adults that takes into consider the influence of sex and/or gender. As such, clinical practice, including the introduction of interdisciplinary teams with geriatric expertise, and interventions based on guidelines developed for the older males and females, must take into account this aging population to maximize functional outcome for older adults with TBI. Further in-depth research with clinicians and clients of inpatient rehabilitation is also encouraged to understand the clinical significance of these findings to support the co-creation of patient-oriented interventions that may mitigate the negative impacts of chronic conditions on adverse rehabilitation outcomes.
Finally, our study on the effects of comorbid health conditions preceding TBI is, to the best of our knowledge, novel. The data mining procedures used in this study can be successfully applied in rehabilitation research to comprehensively categorize thousands of diagnosis codes into meaningful groups that can be used to inform provision of services and supports. Importantly, it can overcome existing limitations in identifying and incorporating comorbidities in rehabilitation research, as current studies frequently capture comorbid health conditions using self-reports, pre-existing measures (e.g., ADGs, CCI), focus on select health conditions, or are of limited timespan.3–6 As the use of big data become increasingly common in research, data mining methodologies should be explored and applied to maximize its potential to inform evidence-based service delivery across all health conditions.
Strengths and Limitations
Limitations associated with using health administrative data are acknowledged. First, there is currently no consensus on the case definition for TBI across the lifespan, however, systematic reviews16,27 and published reports and peer-reviewed papers6,17,28 have used ICD-10 codes consistent with those applied in this study. The data available in this study are also limited to those captured in the DAD and NRS and as such, lack information on other measures, such as race/ethnicity and marital status.4,21,29 Methodological limitations include the use of 43 multivariable linear regressions, which do not account for concurrent pre-injury health statuses. However, the intent of this study is to provide the foundation for future research on the types of pre-injury comorbid health conditions warrant further research and as such, is an appropriate first step to this important area of research. Furthermore, it is acknowledged p-values are affected by large sample sizes like this present study and as such, interpretation of findings should also consider the 95% Confidence Intervals. Finally, the outcome variable for this study, RFG, is based on the difference, in raw scores, of the total FIM score at admission and discharge. The total FIM scores were also based on the summed, raw scores of the FIM motor and FIM cognitive measures. Future research is encouraged to apply Rasch analysis to generate estimates of each individual’s functional ability on an equal interval linear continuum to transform ordinal measures to interval-level scaling, which can improve accuracy of study findings.
Despite these limitations, there are considerable strengths to this study. A major strength is the use of population-based health administrative data from a publicly funded healthcare system where reporting of acute care and inpatient rehabilitation data are mandatory. As such, this study is virtually free of sampling bias (i.e., all Ontarian residents, regardless of socioeconomic status, who used inpatient rehabilitation services within one year of acute care discharge were included in this study). The use of these health administrative databases also eliminates recall bias as information on preceding health status were obtained directly from ICD-10 codes captured in all patients’ health records in the ED and acute care settings. Unique identifiers for each patient also enabled a longer look-back period (up to five years) compared to previous studies. Finally, we applied findings derived from a recent peer-reviewed study using data mining techniques to comprehensively categorize all ICD-10 codes present in patients’ health records up to five years prior to their TBI-related acute care admission.8
Conclusions
This is the first population-based, sex-stratified study, to the best of our knowledge, to comprehensively capture all pre-injury comorbid health conditions to understand how health status five years prior to TBI affects functional outcome. Among male patients, ten factors of pre-injury health status related to psychiatry, neurology, cardiology, gastroenterology, and conditions related to the elderly and medical issues were significantly associated with reduced RFG. Among females, only disorders of the elderly and other medical issues was significantly associated with reduced RFG after Bonferroni adjustment for multiple comparisons. Future research is encouraged to continue to leverage data mining methodologies to identify profiles of patients who are at risk of reduced RFG to support evidence-based planning of interdisciplinary teams and interventions to maximum rehabilitation for patients with TBI. Importantly, this study supplements prior research demonstrating sex differences in outcomes after inpatient rehabilitation, further strengthening the implication of sex-stratified analyses in research and healthcare planning.
Supplementary Material
Acknowledgements
We would like to thank Ms. Jingqian Liu for conducting a literature review that informed the development of the introduction of this manuscript.
This study was supported by the Eunice Kennedy Shriver National Institutes of Child Health & Human Development of the National Institutes of Health under Award Number R21HD089106. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. TM was supported by the postdoctoral research grant from the Alzheimer’s Association (AARF-16-442937). The funders had no role in the study design, data collection, decision to publish, or preparation of the manuscript.
This study made use of de-identified data from the ICES Data Repository, which is managed by the Institute for Clinical Evaluative Sciences with support from its funders and partners: Canada’s Strategy for Patient-Oriented Research (SPOR), the Ontario SPOR Support Unit, the Canadian Institutes of Health Research and the Government of Ontario. The opinions, results and conclusions reported are those of the authors. No endorsement by ICES or any of its funders or partners is intended or should be inferred. Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI.
Abbreviations:
- ADG
Aggregated Diagnosis Groupings
- AIS
Abbreviated Injury Severity
- ALC
Alternate level of care
- CCI
Charlson Comorbidity Index
- CIHI
Canadian Institute of Health Information
- DAD
Discharge Abstract Database
- ICD-10
International Classification of Diseases Version 10
- LOS
Length of stay
- NRS
National Rehabilitation Reporting System
- RFG
Relative functional gain
- TBI
Traumatic brain injury
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Menon DK, Schwab K, Wright DW, et al. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–1640. [DOI] [PubMed] [Google Scholar]
- 2.Lamm AG, Goldstein R, Giacino JT, Niewczyk P, Schneider JC, Zafonte R. Changes in Patient Demographics and Outcomes in the Inpatient Rehabilitation Facility Traumatic Brain Injury Population from 2002 to 2016: Implications for Patient Care and Clinical Trials. J Neurotrauma. 2019. [DOI] [PubMed] [Google Scholar]
- 3.Dahdah MN, Barnes S, Buros A, et al. Variations in Inpatient Rehabilitation Functional Outcomes Across Centers in the Traumatic Brain Injury Model Systems Study and the Influence of Demographics and Injury Severity on Patient Outcomes. Arch Phys Med Rehabil. 2016;97(11):1821–1831. [DOI] [PubMed] [Google Scholar]
- 4.Kucukboyaci NE, Long C, Smith M, Rath JF, Bushnik T. Cluster Analysis of Vulnerable Groups in Acute Traumatic Brain Injury Rehabilitation. Arch Phys Med Rehabil. 2018;99(11):2365–2369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malec JF, Ketchum JM, Hammond FM, et al. Longitudinal Effects of Medical Comorbidities on Functional Outcome and Life Satisfaction After Traumatic Brain Injury: An Individual Growth Curve Analysis of NIDILRR Traumatic Brain Injury Model System Data. J Head Trauma Rehabil. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan V, Mollayeva T, Ottenbacher KJ, Colantonio A. Sex-Specific Predictors of Inpatient Rehabilitation Outcomes After Traumatic Brain Injury. Arch Phys Med Rehabil. 2016;97(5):772–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahdah MN, Hofmann M, Pretz C, et al. Factors Associated With Rehabilitation Outcomes After Traumatic Brain Injury: Comparing Functional Outcomes Between TBIMS Centers Using Hierarchical Linear Modeling. J Head Trauma Rehabil. 2017;32(4):E1–E10. [DOI] [PubMed] [Google Scholar]
- 8.Mollayeva T, Sutton M, Chan V, Colantonio A, Jana S, Escobar M. Data mining to understand health status preceding traumatic brain injury. Sci Rep. 2019;9(1):5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Table 17–10-0005-01 Population estimates on July 1st, by age and sex. 2018. Accessed August 26, 2019.
- 10.Discharge Abstract Database Metadata (DAD). https://www.cihi.ca/en/discharge-abstract-database-metadata. Accessed August 26, 2019.
- 11.Rehabilitation Minimum Data Set Manual. Ottawa, ON: Canadian Institute for Health Informaiton; 2018. [Google Scholar]
- 12.National Rehabilitation Reporting System Data Quality Documentation 2017–2018. Ottawa: Canadian Institute of Health Information; 2018. [Google Scholar]
- 13.Chan V, Mollayeva T, Ottenbacher KJ, Colantonio A. Clinical profile and comorbidity of traumatic brain injury among younger and older men and women: a brief research notes. BMC Research Notes. 2017;10:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan V, Zagorski B, Parsons D, Colantonio A. Older Adults with Acquired Brain Injury: Outcomes After Inpatient Rehabilitation. Canadian Journal on Aging / La Revue canadienne du vieillissement. 2013;32(3):278–286. [DOI] [PubMed] [Google Scholar]
- 15.Chen A, Bushmeneva K, Zagorski B, Colantonio A, Parsons D, Wodchis WP. Direct cost associated with acquired brain injury in Ontario. BMC Neurol. 2012;12(76):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen AY, Colantonio A. Defining neurotrauma in administrative data using the International Classification of Diseases Tenth Revision. Emerg Themes Epidemiol. 2011;8(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saverino C, Swaine B, Jaglal S, et al. Rehospitalization After Traumatic Brain Injury: A Population-Based Study. Arch Phys Med Rehabil. 2016;97(2 Suppl):S19–25. [DOI] [PubMed] [Google Scholar]
- 18.Salter K, Teasell R, McIntrye A, Johnson D, Jutai. Assessment of Outcomes Following Acquired Brain Injury In: Teasell R, Cullen N, Marshall S, Janzen S, Bayley M, eds. Evidence-Based Review of Moderate to Severe Acquired Brain Injury 2017. [Google Scholar]
- 19.Koh GC, Chen CH, Petrella R, Thind A. Rehabilitation impact indices and their independent predictors: a systematic review. BMJ Open. 2013;3(9):e003483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corrigan JD, Horn SD, Barrett RS, et al. Effects of Patient Preinjury and Injury Characteristics on Acute Rehabilitation Outcomes for Traumatic Brain Injury. Arch Phys Med Rehabil. 2015;96(8 Suppl):S209–221 e206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graham JE, Radice-Neumann DM, Reistetter TA, Hammond FM, Dijkers M, Granger CV. Influence of sex and age on inpatient rehabilitation outcomes among older adults with traumatic brain injury. Arch Phys Med Rehabil. 2010;91(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu J, Roe C, Sigurdardottir S, Andelic N, Forslund M. Trajectory of Functional Independent Measurements during First Five Years after Moderate and Severe Traumatic Brain Injury. J Neurotrauma. 2018;35(14):1596–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abbreviated Injury Scale https://www.aaam.org/abbreviated-injury-scale-ais/. Accessed July 29, 2019.
- 24.ICD Injury Matrices https://www.cdc.gov/nchs/injury/injury_matrices.htm. Accessed July 29, 2019.
- 25.Recommended ICD-10-CA Codes for Injury Core Indicators. http://core.apheo.ca/index.php?pid=306. Accessed July 29, 2019.
- 26.Alternate Level of Care (ALC) Days http://www.health.gov.on.ca/en/pro/programs/ris/docs/alternate_level_of_care_days_en.pdf.Accessed July 29, 2019.
- 27.Chan V, Thurairajah P, Colantonio A. Defining pediatric traumatic brain injury using International Classification of Diseases Version 10 Codes: a systematic review. BMC Neurol. 2015;15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ng R, Maxwell CJ, Yates EA, et al. Brain Disorders in Ontario: Prevalence, Incidence and Costs from Health Administrative Data. Ontario, Canada: ICES; 2015. [Google Scholar]
- 29.Chang PF, Ostir GV, Kuo YF, Granger CV, Ottenbacher KJ. Ethnic differences in discharge destination among older patients with traumatic brain injury. Arch Phys Med Rehabil. 2008;89(2):231–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


