Abstract
Introduction:
Rates of adolescent substance use have decreased in recent years. Knowing whether nonmedical marijuana legalization for adults is linked to increases or slows desirable decreases in marijuana and other drug use or pro-marijuana attitudes among teens is of critical interest to inform policy and promote public health. This study tests whether nonmedical marijuana legalization predicts a higher likelihood of teen marijuana, alcohol, or cigarette use or lower perceived harm from marijuana use in a longitudinal sample of youth aged 10–20 years.
Methods:
Data were drawn from the Seattle Social Development Project-The Intergenerational Project, an accelerated longitudinal study of youth followed both before (2002–2011) and after nonmedical marijuana legalization (2015–2018). Analyses included 281 youth surveyed up to ten times and living in a state with nonmedical marijuana legalization between 2015 and 2018 (51% female, 33% white, 17% African American, 10% Asian/Pacific Islander, 40% mixed race or other).
Results:
Multilevel modeling (in 2019) showed that nonmedical marijuana legalization predicted a higher likelihood of self-reported past year marijuana (AOR=6.85, p=0.001) and alcohol use (AOR 3.38, p=0.034) among youth when controlling birth cohort, sex, race, and parent education. Nonmedical marijuana legalization was not significantly related to past-year cigarette use (AOR=2.43, p=0.279) or low perceived harm from marijuana use (AOR=1.50, p=0.236) across ages 10–20 years.
Conclusions:
It is important to consider recent, broad declines in youth substance use when evaluating the impact of nonmedical marijuana legalization. States that legalize non-medical marijuana for adults should increase resources for the prevention of underage marijuana and alcohol use.
INTRODUCTION
Since Washington State and Colorado first legalized nonmedical marijuana use for adults aged 21 years and older in 2012, multiple other states have followed suit. Use for teens remains illegal in all states, however. A key concern with the passage and expansion of nonmedical marijuana legalization (NML) for adults is that teen use may increase, perhaps through increased availability or the perception that marijuana use is not harmful because it is legal. Alternatively, NML may slow or stop recent, population-level decreases in the prevalence of teen substance use1; 2 via similar mechanisms. Given that marijuana use often co-occurs with alcohol and cigarette use,3–5 there also is concern that teen alcohol or cigarette use may increase following NML. Thus, information about whether NML is linked to changes in marijuana, alcohol, or cigarette use or perceived harm from marijuana among teens is of critical interest for policymakers, public health advocates, physicians, and other professionals who work with families and teens.
The limited available post-NML data from states with legalized marijuana provide mixed evidence about whether legalization is linked to increased marijuana use and lower perceived harm among teens. Data from Colorado show no effects of legalization on youth marijuana use, approval of use, or perceived harm.6–8 Washington State data from the nationally representative Monitoring The Future study spanning 2010–2015 showed significant increases in past-month marijuana use and regular use and decreases in perceived harm from marijuana use among 8th and 10th graders in Washington following legalization.6 Unfortunately, the Monitoring The Future Washington State cohort is not state representative, a key weakness.9 A replication using 2010–2016 statewide data from the Washington Healthy Youth Survey showed significant decreases in the prevalence of past-month marijuana use among 8th and 10th graders and no change among 12th graders following NML.9 Yet, response rates for older students in the Healthy Youth Survey were low (67%–69% for 10th grade, 49%–50% for 12th grade in 2014 and 2016), calling into question the representativeness of the data and the extent to which marijuana-using youth may have been missed. Further, although Monitoring The Future and the Healthy Youth Survey include large sample sizes and have many strengths, these studies rely on repeated cross-sections of youth, and therefore do not capture within-person change. Longitudinal, within-person data are rare, however, data from 8th and 9th graders in Oregon showed that adolescents who were already using marijuana used more frequently following legalization, but legalization did not predict increased prevalence of use.10
Given the paucity of and inconsistent findings in prior literature, additional studies of the impact of NML on youth cannabis use are sorely needed. Considering birth cohort may be particularly important, as national- and state-level trends in the prevalence of substance use have shown steady declines among recent cohorts.1; 2 Accounting for these declines may be critical for understanding the impact of NML, because even finding no change in levels of youth marijuana use after NML may be a concern if it indicates that NML is slowing ongoing population-level declines in youth marijuana use. For example, Washington State Healthy Youth Survey data and national data from the past decade show that the prevalence of alcohol and cigarette use are declining; however, the prevalence of marijuana use is generally holding steady.1; 11 Although repeated cross-sectional data are important to understand population-level trends, longitudinal studies that include multiple birth cohorts are needed to pull apart the influence of historic trends and developmental age, and advance understanding of the association between NML and youth marijuana use.
Adolescent marijuana use shows a high degree of overlap with alcohol and cigarette use.12–15 Thus, NML also may have implications for rates of teen alcohol and cigarette use. However, the literature on changes in rates of adolescent alcohol or cigarette use following NML is virtually nonexistent. One study using data from the Healthy Minds Study showed no change in past–30 day cigarette use or heavy alcohol use among undergraduates following NML in Oregon.16 Given the significant public health impacts of adolescent alcohol and cigarette use, it is important to know whether they are affected by NML.
This study examines the odds of adolescent marijuana, alcohol, and cigarette use and level of perceived harmfulness of marijuana use across ages 10–20 years. The study uses prospective longitudinal data from multiple birth cohorts of youth, born in 1989–2007 and surveyed repeatedly between 2002–2011 (before NML) and 2015–2018 (after NML). A higher probability of past-year marijuana use and lower levels of perceived harm are expected post- versus pre-NML. Analyses also test whether NML is associated with changes in the probability of alcohol or cigarette use.
METHODS
Study Sample
Data were drawn from the Seattle Social Development Project-The Intergenerational Project (SSDP-TIP). SSDP-TIP includes 426 families recruited from the ongoing, longitudinal SSDP study,17 which began in 1985 and includes 808 participants recruited from 18 Seattle area elementary schools. SSDP-TIP began in 2002, when SSDP participants were aged 27 (SD=0.52) years on average. Those SSDP participants who had become biological parents were asked to participate in SSDP-TIP, which includes the SSDP participating parent, the oldest biological child with whom they had regular contact, and a second caregiver, when available (usually the spouse). Parent and child interviews were conducted annually in 2002–2005 (Waves 1–4; pre-NML), 2009–2011 (Waves 5–7; pre-NML), and 2015–2018 (Waves 8–10; post-NML). The recruitment rate of eligible SSDP families into TIP was 72%, and retention from wave to wave averaged 90%. Parents and offspring aged ≥18 years provided informed consent at each data collection; parents provided permission for child participation, and children assented at each data collection. Study measures and procedures were approved by the University of Washington IRB. Each year, participants received an incentive between $10 (young children) and $50 (parents).
Although the SSDP parents in the study were all about the same age, they became parents at different times. Children ranged in age from 1 to 13 years when the study began (2002), and have been followed through 2018. The study used rolling enrollment, such that new families were recruited to SSDP-TIP as SSDP participants became parents for the first time. Child marijuana use was assessed beginning at age 10 years; by 2018, the study included 339 children who had been surveyed at least once between age 10 and 20 years (marijuana use becomes legal at age 21 years).
Although parents all originally lived in Washington State, some families had moved; by 2015, 25% of families were not living in a state with NML. Analyses were restricted to include youth who provided at least one data point between age 10 and 20 years and who lived in states with NML (i.e., legalization in effect and stores open) at some point between 2015 and 2018 (n=281 youth surveyed an average of 3.8 times; 1,068 person-years). NML states included Washington (stores open July 2014) and Oregon (stores open October 2015) in this sample; no respondents lived in Colorado or Alaska. California passed NML in 2016; however, stores did not open until January 2018; participants living in California were not included in analyses. Sensitivity analyses including only the 233 individuals who lived in an NML state as of 2015 yielded an identical pattern of significance and very similar parameter estimates to those reported below for all models. The study design and sample are described in detail elsewhere.18
Measures
At each data collection, children reported whether they had used marijuana, alcohol, and cigarettes in the past year (each coded 1=yes, 0=no).
At each wave, children were asked: Do you think it hurts people if they use marijuana regularly? (1=NO!, 2=no, 3=yes, 4=YES!). Responses were recoded such that higher scores indicate less perceived harm.
The legal status of adult nonmedical marijuana use at each assessment was dummy coded (1=legal, 0=not legal) based on the year that data were collected. Despite the October store opening date in Oregon, respondents living there were coded as experiencing NML in 2015 because the field period began in August; thus, participants in Oregon overwhelmingly were surveyed after stores opened.
Child age (in years) at each wave was calculated based on the child’s birth date and the survey completion date. Child birth cohort was coded based on the child’s year of birth; higher values indicate more recent birth cohorts. Child sex (1=female, 0=male) was based on parent report. Child race (white, African American, Asian/Pacific Islander, mixed/other) was coded based on consolidation of repeated child and parent reports. Parental education level (a proxy for SES; Results describe coding) was based on parent report.
Statistical Analysis
The accelerated longitudinal, or cohort-sequential, design (multiple birth cohorts followed over time) allowed estimation of the impact of NML on the odds of marijuana, cigarette, and alcohol use and level of perceived harm among youth who were surveyed at the same age, but who differed in exposure to legalization. Data were analyzed in 2019 using multilevel regression in HLM, version 6 to account for nesting of repeated measures within person. Figure 1 shows conceptually how aligning longitudinal data from the overlapping birth cohorts by age (short, thin lines) allowed estimation of the probability of cannabis use across age 10–20 years (long, thick lines). To estimate the association between NML and the odds of past-year youth marijuana, alcohol, and cigarette use and level of perceived harm from marijuana across age 10–20 years, a dichotomous NML indicator (0=no, 1=yes) was included in multivariable models as a time-varying predictor. This resulted in simultaneous estimation of two developmental trajectories of the probability of, for example, cannabis use (Figure 1). Overlapping cohort data collected before legalization were used to estimate a youth cannabis use trajectory from age 10 to 20 years without NML (thick, solid line). Concurrently, age-matched data collected in 2015–2018 were used to estimate a youth cannabis use trajectory from age 10 to 20 years with NML (thick, dashed line). This design delivers a great deal of statistical power, owing to the repeated measures of overlapping birth cohorts.19; 20 Child age, centered at 15 years, was included in regression models to index time. An age-squared term was included when significant to account for nonlinear change over time. Age X NML interaction terms were tested in each model, but were not significant. Logistic models of the dichotomous substance use outcome variables used a Bernoulli link function; the model of the ordered-categorical perceived harm outcome used a log link and restricted penalized quasi-likelihood estimation. Time-fixed controls in each model included child sex, race, and birth cohort, as well as parent education. To test the importance of controlling birth cohort to parse out downward trends in substance use, supplemental models without birth cohort also were tested.
Figure 1.
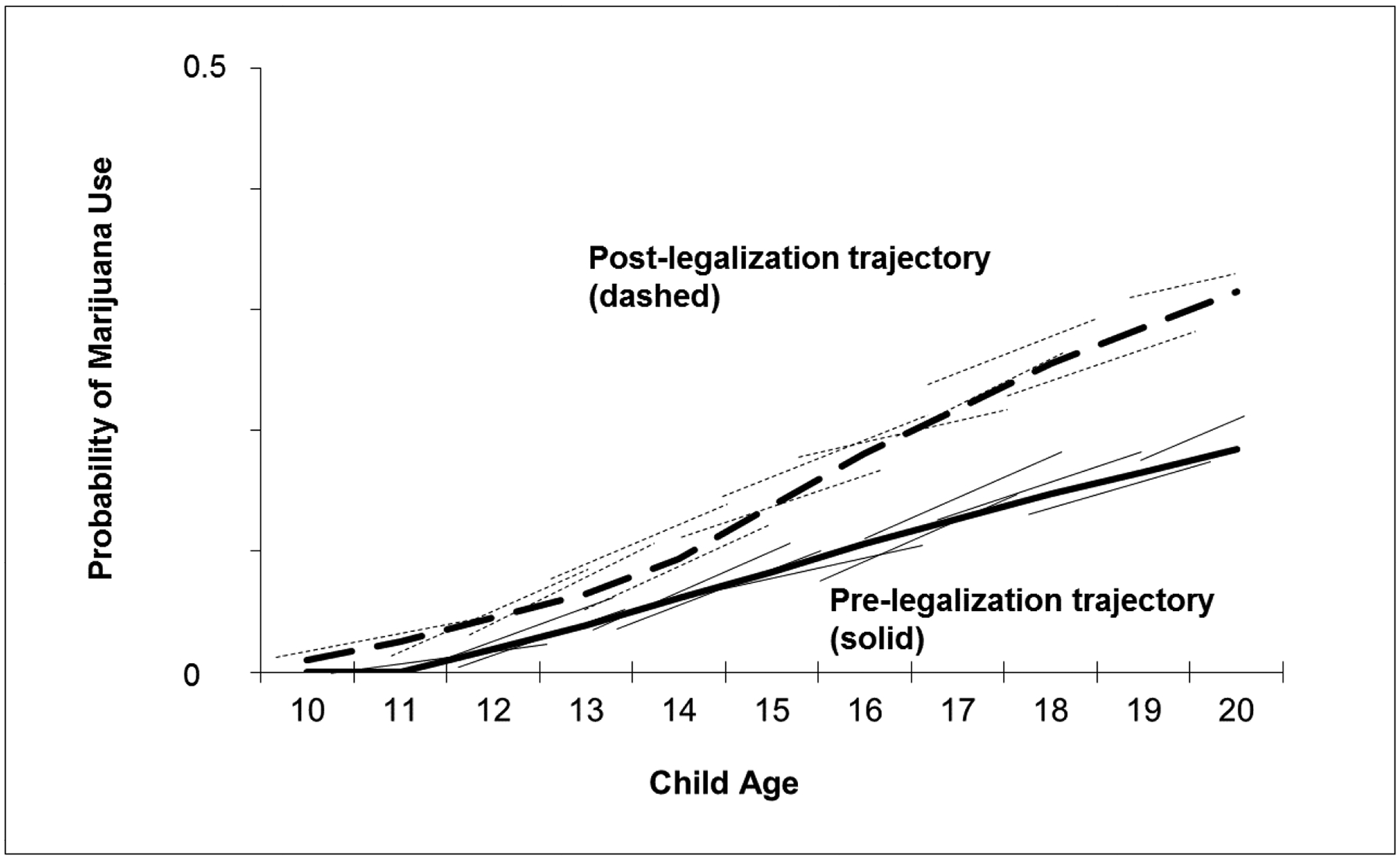
Conceptual model showing alignment of overlapping cohort data and resulting developmental trajectories.
RESULTS
About 51% (n=194) of children were female. With regard to race, 10% (n=27) of youth were Asian/Pacific Islander, 17% (n=49) were African American, 33% (n=93) were white, and 40% were mixed/other (n=112, including n=15 Native Americans). In terms of parental educational attainment, 14% of parents reported less than a completed high school diploma (individuals with GEDs were included in this category), 11% reported a high school diploma, 35% reported “some college” or attending vocational school, 11% reported completing 2-year college, 16% completed 4-year college, and 13% reported post-graduate training. About 94% (n=223) of youth included in analyses lived in Washington (66% of these in King County) and 4% (n=10) lived in Oregon in 2015.
Multilevel regression models showed that youth were more likely to report past-year marijuana and alcohol use (Table 1) following NML, but the odds of past-year cigarette use (Table 1) and level of perceived harm from marijuana use (Table 2) across ages 10–20 years did not change following NML. Increasing age predicted increased odds of substance use and less perceived harm from marijuana. Significant negative coefficients for the age squared terms suggested that the rate of age-based increases in substance use and norms slowed as youth got older. Compared with mixed race youth, white children were more likely to use cigarettes and alcohol, and African American youth were less likely to use alcohol. Being in a more recent birth cohort was associated with lower odds of use of each substance at age 15 years and greater perceived harm from marijuana use. Children of more educated parents were more likely to use alcohol and perceived less harm from marijuana use. Supplemental analyses (not shown) demonstrated that the associations between NML and marijuana and alcohol use were nonsignificant when excluding child birth cohort, indicating that birth cohort effects may bias analyses of NML impact if they are not modeled.
Table 1.
Results of Multilevel Models Predicting Youth Past Year Marijuana, Cigarette, and Alcohol Use
| Marijuana use | Cigarette use | Alcohol use | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors | B (SE) | AOR | p-value | B (SE) | AOR | p-value | B (SE) | AOR | p-value |
| Time-varying main effects | |||||||||
| Child age (slope) | 0.75 (0.15) | 2.11 | <0.001 | 0.66 (0.15) | 1.93 | <0.001 | 0.46 (0.08) | 1.59 | <0.001 |
| Child age squared | −0.11 (0.03) | 0.90 | 0.001 | −0.10 (0.03) | 0.91 | 0.005 | −0.05 (0.02) | 0.95 | 0.014 |
| Legal marijuana | 1.92 (0.71) | 6.85 | 0.007 | 0.89 (0.82) | 2.43 | 0.279 | 1.22 (0.57) | 3.38 | 0.034 |
| Time-fixed main effects | |||||||||
| Level at age 15 (intercept) | −0.76 (0.67) | 0.47 | 0.260 | −2.02 (0.81) | 0.13 | 0.014 | −0.97 (0.56) | 0.38 | 0.084 |
| Child is female | 0.04 (0.31) | 1.01 | 0.891 | 0.69 (0.40) | 2.00 | 0.083 | 0.33 (0.28) | 1.39 | 0.231 |
| Child is mixed race | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| Child is white | 0.43 (0.37) | 1.54 | 0.242 | 1.02 (0.46) | 2.79 | 0.028 | 0.80 (0.33) | 2.23 | 0.015 |
| Child is African American | −0.72 (0.43) | 0.49 | 0.092 | −0.60 (0.56) | 0.55 | 0.281 | −1.03 (0.40) | 0.36 | 0.011 |
| Child is Asian/Pacific Islander | −0.68 (0.69) | 0.51 | 0.325 | −0.32 (0.93) | 0.72 | 0.728 | −0.01 (0.56) | 0.99 | 0.985 |
| Child birth cohort | −0.32 (0.10) | 0.74 | 0.002 | −0.29 (0.13) | 0.75 | 0.029 | −0.28 (0.09) | 0.76 | 0.002 |
| Parent education | 0.03 (0.12) | 1.01 | 0.790 | 0.10 (0.15) | 1.10 | 0.530 | 0.24 (0.11) | 1.27 | 0.026 |
Note: Child age is centered at 15 years. Statistically significant parameters (p<0.05) are bolded.
Table 2.
Results of a Multilevel Model Predicting Low Perceived Harm From Marijuana Use
| Low perceived harm | |||
|---|---|---|---|
| Predictors | B (SE) | AOR | p-value |
| Time-varying main effects | |||
| Child age (slope) | −0.35 (0.04) | 0.71 | <0.001 |
| Legal marijuana | 0.41 (0.34) | 1.50 | 0.236 |
| Time-fixed main effects | |||
| Level at age 15 (intercept) | 0.01 (0.30) | 1.01 | 0.967 |
| Child is female | 0.12 (0.17) | 1.13 | 0.494 |
| Child is mixed race | ref | ref | ref |
| Child is white | −0.31 (0.21) | 0.74 | 0.146 |
| Child is African American | −0.34 (0.23) | 0.71 | 0.152 |
| Child is Asian/Pacific Islander | −0.19 (0.34) | 0.82 | 0.567 |
| Child birth cohort | −0.09 (0.04) | 0.91 | 0.044 |
| Parent education | 0.21 (0.07) | 1.24 | 0.002 |
| Threshold 2 | 1.16 (0.07) | 3.19 | <0.001 |
| Threshold 3 | 2.48 (0.11) | 11.98 | <0.001 |
Note: Child age is centered at 15. Statistically significant parameters (p<0.05) are bolded. The low perceived harm measure included 4 ordered categories and three thresholds (between response option 1 and 2, response option 2 and 3, and response option 3 and 4, respectively).
DISCUSSION
This longitudinal study is an important addition to the small extant literature that has produced mixed findings about the impact of NML on youth marijuana use. The current study suggests that modeling birth cohort to account for recent broad declines in substance use prevalence is important for understanding the impact of NML. Consistent with national- and state-level trend data, youth in this study from more recent birth cohorts were less likely to use marijuana and alcohol at age 15 years, compared with less recent cohorts.1; 2 Once accounting for the lower odds of substance use in more recent birth cohorts, however, the main effect of NML on youth marijuana and alcohol use emerged. This suggests that NML may be working against broad downward trends in substance use in general, and that contemporary youth may be more likely to use marijuana and alcohol following NML than they would otherwise be. Consistent with this hypothesis, the prevalence of alcohol and cigarette use are declining nationally and in Washington State; however, the prevalence of marijuana use is generally holding steady.1; 2; 21 Additional, larger-scale longitudinal studies including multiple birth cohorts are needed to understand not only whether NML predicts higher rates of youth marijuana use broadly, but also whether NML is working against reductions in use achieved through evidence-based preventive intervention and policy. Also very useful would be analyses of accelerated longitudinal data including youth from states both with and without NML to determine whether the probability of youth marijuana use is changing nationally in a post-NML era, or whether any changes are confined to states with NML.
The present study did not find an association between NML and youth cigarette use. The current results are consistent with findings from a study of college students in Oregon that found no increase in cigarette use following NML16 and with studies showing continued decreases in the prevalence of youth cigarette use in the run up to and following NML.2 Some studies have suggested that recent declines in the prevalence of teen cigarette use may explain why marijuana use has not increased dramatically given decreases in perceived harm and the advent of NML.22; 23 Given the risk of nicotine addiction and the important long-term health impact of adolescent cigarette use, continued monitoring to detect changes in youth cigarette use following NML is critical.
Contrary to expectations, analyses did not reveal a main effect of NML on perceived harm from marijuana use. It may be that reduced perception of harm in the general population contributes to NML, as opposed to NML driving perceptions.24–26 Nevertheless, low perceived harm continues to be linked to higher adolescent marijuana use after NML.22; 23 Thus, following NML, continued efforts to monitor perceived harm and relay accurate information about risks associated with use are warranted. Evidence-based preventive interventions developed before NML that target perceived harm from marijuana use should be tested in the context of NML to determine whether they remain effective, or whether development of new prevention approaches is needed.
Although multiple states have passed NML legislation, the specifics of legalization vary from state to state. For example, Washington caps the number of allowable retail marijuana outlets, but other states do not; multiple states allow individuals to grow nonmedical marijuana at home, whereas Washington does not. Washington had a thriving and poorly regulated medical marijuana industry prior to NML, which was much more strictly regulated beginning in 2016. Thus, the current results should be interpreted with these contextual factors in mind. For instance, changes in youth marijuana use following NML may be more dramatic in states that do not cap the number of retail outlets. Future studies aimed at understanding the role of variations in state and local policy and access are needed to inform youth prevention efforts.
Limitations
The primary limitations of the current study are that most participants were living in Washington State, and that the sample is somewhat small and not a statewide representative sample. Thus, replication of study findings to demonstrate generalizability, both to Washington State as a whole and to other states, will be important. In addition, the analysis of perceived harm relied on a single item, although one that is widely used. Outcome measures were dichotomized to capture any past-year use, which is of concern among youth aged 10–20 years; however, this precluded analyses of use frequency. These limitations are balanced by important strengths, including the longitudinal design and repeated measures that enabled both within- and between-person comparisons, as well as the modeling of individual development. The inclusion of multiple, overlapping birth cohorts provided a great deal of statistical power,19 and enabled the disentanglement of NML and the impact of declining rates of teen substance use in more recent birth cohorts.
CONCLUSIONS
Among teens, NML may be working against hard-won, population-level decreases in the prevalence of marijuana and alcohol use. Accounting for recent downward trends in adolescent substance use is important when testing the impact of NML. Continued monitoring of changes in the prevalence of youth marijuana, alcohol, and other substance use and perceived harm following NML is critical. States that legalize nonmedical marijuana use for adults should devote increased resources to evidence-based prevention programming for underage marijuana and alcohol use. Future studies should investigate potential moderators of the impact of NML, including sex, race/ethnicity, and SES.
Figure 2.
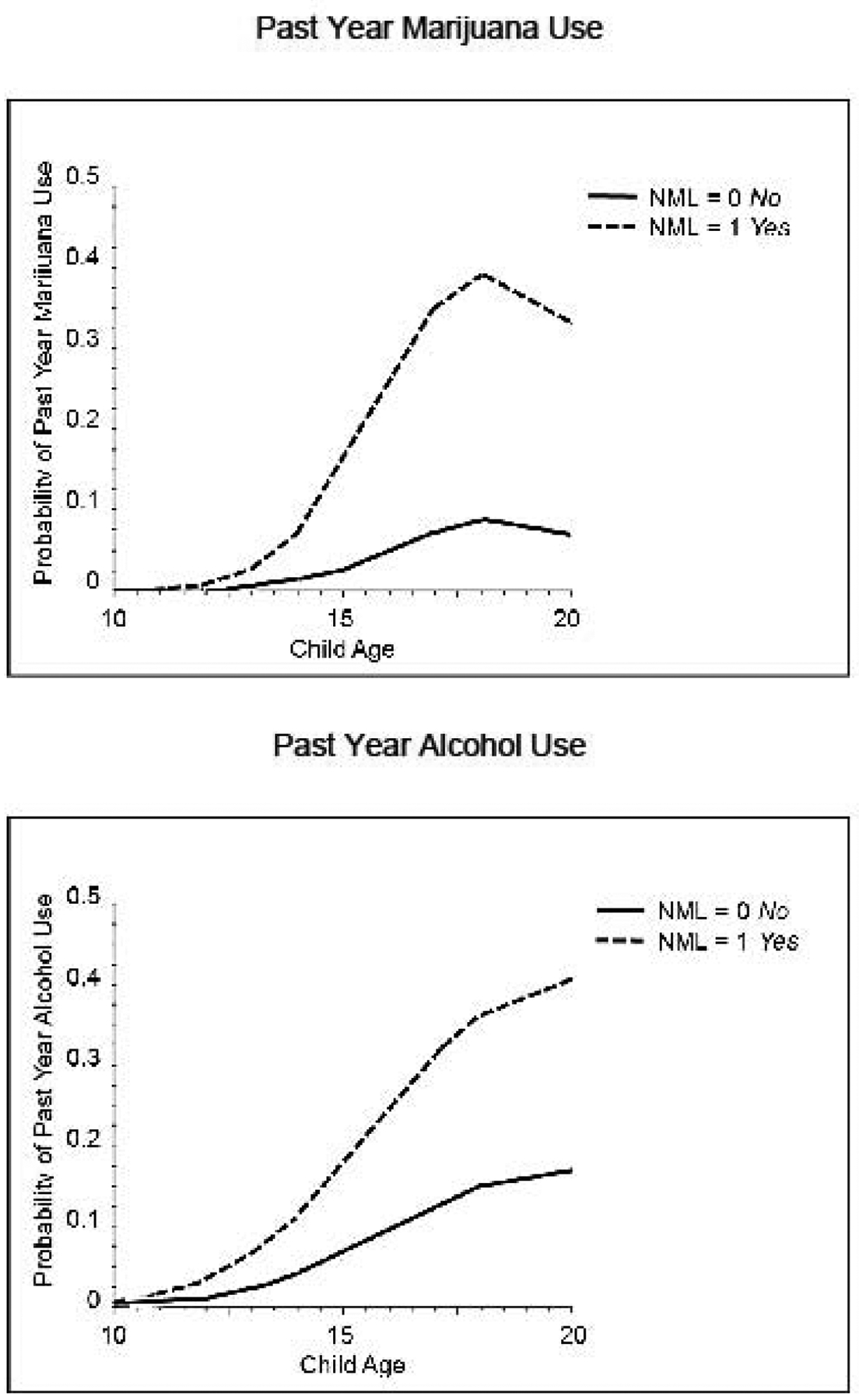
Graphs of models testing associations between nonmedical marijuana legalization (NML) and youth past year marijuana and alcohol use.
ACKNOWLEDGMENTS
We gratefully acknowledge the study participants for sharing their experiences and the Survey Research Division of the Social Development Research Group for their excellent data collection and management. Conclusions reflect the points of view of the authors and not the funding agency. This manuscript was supported by a grant from the National Institute on Drug Abuse (R01DA-023089). The funding agency had no role in the design of the study; collection, analysis, or interpretation of data; the writing of this report; or the decision to submit this manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of these findings were presented at the first cross-national symposium on Cannabis Legalization and Youth, November 2018, in Boulder, Colorado.
No financial disclosures or conflicts of interest were reported by the authors of this paper.
REFERENCES
- 1.Johnson RM, Fairman B, Gilreath T, et al. Past 15-year trends in adolescent marijuana use: Differences by race/ethnicity and sex. Drug Alcohol Depend. 2015;155:8–15. 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson RM, Fleming CB, Cambron C, Dean LT, Brighthaupt S-C, Guttmannova K. Race/ethnicity differences in trends of marijuana, cigarette, and alcohol use among 8th, 10th, and 12th graders in Washington State, 2004–2016. Prev Sci. 2019;20:194–204. 10.1007/s11121-018-0899-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey JA, Hill KG, Oesterle S, Hawkins JD. Linking substance use and problem behavior across three generations. J Abnorm Child Psychol. 2006;34(3):273–292. 10.1007/s10802-006-9033-z. [DOI] [PubMed] [Google Scholar]
- 4.Moss HB, Chen CM, Yi H. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51–62. 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Lanza S, Vasilenko S, Dziak J, Butera N. Trends among U.S. high school seniors in recent marijuana use and associations with other substances: 1976–2013. J Adolesc Health. 2015;57(2):198–204. 10.1016/j.jadohealth.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cerdá M, Wall M, Feng T, et al. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142–149. 10.1001/jamapediatrics.2016.3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones J, Jones KN, Peil J. The impact of the legalization of recreational marijuana on college students. Addict Behav. 2018;77:255–259. 10.1016/j.addbeh.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Harpin SB, Brooks-Russell A, Ma M, James KA, Levinson AH. Adolescent marijuana use and perceived ease of access before and after recreational marijuana implementation in Colorado. Subst Use Misuse. 2018;53(3):451–456. 10.1080/10826084.2017.1334069. [DOI] [PubMed] [Google Scholar]
- 9.Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerda M. Prevalence of cannabis use in youths after legalization in Washington State. JAMA Pediatr. 2019;173(2):192–193. 10.1001/jamapediatrics.2018.4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rusby JC, Westling E, Crowley R, Light JM. Legalization of recreational marijuana and community sales policy in Oregon: impact on adolescent willingness and intent to use, parent use, and adolescent use. Psychol Addict Behav. 2018;32(1):84–92. 10.1037/adb0000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnston LD, Miech R, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future national survey results on drug use 1975–2018: overview, key findings on adolescent drug use Ann Arbor, MI: Institute for Social Research, 2019. 10.3998/2027.42/150621. [DOI] [Google Scholar]
- 12.Badiani A, Boden JM, De Pirro S, Fergusson DM, Horwood LJ, Harold GT. Tobacco smoking and cannabis use in a longitudinal birth cohort: evidence of reciprocal causal relationships. Drug Alcohol Depend. 2015;150:69–76. 10.1016/j.drugalcdep.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 13.Patrick ME, Terry-McElrath YM, Lee CM, Schulenberg JE. Simultaneous alcohol and marijuana use among underage young adults in the United States. Addict Behav. 2019;88:77–81. 10.1016/j.addbeh.2018.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patrick ME, Kloska DD, Terry-McElrath YM, Lee CM, O’Malley PM, Johnston LD. Patterns of simultaneous and concurrent alcohol and marijuana use among adolescents. Am J Drug Alcohol Abuse. 2018;44(4):441–451. 10.1080/00952990.2017.1402335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kristman-Valente AN, Hill KG, Epstein M, et al. The relationship between marijuana and conventional cigarette smoking behavior from early adolescence to adulthood. Prev Sci. 2017;18(4):428–438. 10.1007/s11121-017-0774-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerr DC, Bae H, Phibbs S, Kern AC. Changes in undergraduates’ marijuana, heavy alcohol, and cigarette use following legalization of recreational marijuana use in Oregon. Addiction. 2017;112(11):1992–2001. 10.1111/add.13906. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch Pediatr Adolesc Med. 2005;159(1):25–31. 10.1001/archpedi.159.1.25. [DOI] [PubMed] [Google Scholar]
- 18.Bailey JA, Hill KG, Epstein M, Steeger CM, Hawkins JD. Seattle Social Development Project – The Intergenerational Project (SSDP-TIP) In: Eichelsheim V, van der Weijer S, eds. Intergenerational continuity of criminal and antisocial behavior. An international overview of studies. New York, NY: Routledge; 2019:186–206. 10.4324/9781315102788-11. [DOI] [Google Scholar]
- 19.Moerbeek M The effects of the number of cohorts, degree of overlap among cohorts, and frequency of observation on power in accelerated longitudinal designs. Methodology (Gott). 2011;7:11–24. 10.1027/1614-2241/a000019. [DOI] [Google Scholar]
- 20.Raudenbush SW, Bryk AS, Cheong YF, Congdon RT Jr. HLM 6: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- 21.Washington State Department of Health. Healthy Youth Survey Results. www.askhys.net/Home/Press. Accessed April 12, 2019.
- 22.Fleming CB, Guttmannova K, Cambron C, Rhew IC, Oesterle S. Examination of the divergence in trends for adolescent marijuana use and marijuana-specific risk factors in Washington State. J Adolesc Health. 2016;59(3):269–275. 10.1016/j.jadohealth.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miech R, Johnston L, O’Malley PM. Prevalence and attitudes regarding marijuana use among adolescents over the past decade. Pediatrics. 2017;140(6):e20170982 10.1542/peds.2017-0982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954–964. 10.1016/s2215-0366(16)30208-5. [DOI] [PubMed] [Google Scholar]
- 25.Khatapoush S, Halfors D. “Sending the wrong message”: did medical marijuana legalization in California change attitudes about and use of marijuana? J Drug Issues. 2004;34(4):751–770. 10.1177/002204260403400402. [DOI] [Google Scholar]
- 26.Wall M, Poh E, Cerda M, Keyes KM, Galea S, Hasin D. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–716. 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


